Abstract
Background
Globally, mental health disorders and behavioural problems afflict persons with Down syndrome (DS) with a high prevalence reported in some studies. However, data on behavioural and emotional disorders in DS cohort in Asian countries are lacking.
Aims
To assess the mental health status of children and adults with DS, using the Strength and Difficulties Questionnaire (SDQ) and its impact on caregivers using the impact supplement.
Methods
The questionnaires were administered to caregivers of eligible participants aged ≥4 years. In addition, Down syndrome participant's ≥ 11 years old attempted the self-report. Scoring was done as per standard SDQ guidelines.
Results
The total difficulties score was observed to be at least borderline high in 30.6% (19/62) of the participants. Peer relationships and conduct subscale issues were rated high, with abnormal internalizing scores predominating over externalizing scores. From parents' perspective, behavioural issues impacted 41.9% (26/62) of participants' in areas of education, peer relationship and leisure. However, only 3.8% (1/26) of the caregivers whose children had behavioural issues perceived them as a burden.
Conclusions
Mental health difficulties are a significant morbidity in our DS cohort. SDQ is a useful user-friendly tool for identification of behavioural problems enabling timely referral for intervention and therapy.
Keywords: Disability, Epidemiology, Genetic disorders, Health promotion, Pediatrics, Quality of life, Down syndrome, Intellectual disability, Mental health disorder, Emotional and behavioural disorders, Internalizing and externalizing scores, Strength and difficulties questionnaire
Disability; Epidemiology; Genetic disorders; Health promotion; Pediatrics; Quality of life; Down syndrome, Intellectual disability; Mental health disorder; Emotional and behavioural disorders; Internalizing and externalizing scores; Strength and difficulties questionnaire
1. Introduction
The global prevalence of mental health disorders is estimated to be around 10.7% in the general population (Ritchie and Roser, 2020). In a multicultural society like Singapore, lifetime prevalence of mental health disorders is observed to be 13.8% in the general population (Subramaniam et al., 2020). Current global trends point to an increasing level of psychological abnormalities in youths and elderly (Subramaniam et al., 2020). In the intellectually disabled population, the prevalence of mental health disorders is higher, at about 45%, and in children, this is multifold as compared to that of typically developing children (Einfeld and Tonge, 1996; Kaptein et al., 2008; Oeseburg et al., 2010).
Down syndrome (DS), a common chromosomal disorder with intellectual disability (ID) as the most predominant feature, has a worldwide incidence of 1 in 1000 live births as per World Health Organization (WHO) statistics (2015). Children with DS have multiple areas of concern including medical, social, developmental and psychological issues. Advancement of medical care has led to a dramatic improvement in the survival and longevity of persons with DS with the current estimated life expectancy being 60 years in developed countries (Bittles et al., 2007). In this population, medical disorders are regularly screened for by laboratory tests and ultrasonography. However, a screening tool to identify psychological problems is not a routine practice especially in Asian countries. Glenn et al. (2013) reported a variety of problems in multiple domains in adults with DS when evaluated with the Strengths and Difficulties Questionnaire (SDQ). This tool has been widely validated and used in the intellectually disabled group as it addresses the 5 domains of behavioural concerns (emotional, conduct, hyperactivity, peer problems and prosocial behaviour). This questionnaire is simple to administer in clinic settings and has been found to have good reliability and validity (Goodman, 1997 & 2001).
In Singapore, the birth prevalence rate of DS was around 1 per 1000 live births in 1993 and 1998 (Lai et al., 2002), and the incidence of DS at our centre, KK Women's and Children's Hospital (KKH), was 1.13/1000 live births in 2019 (unpublished data, Figure 1). Locally, early intervention programmes (EIP) are in place in tertiary hospitals and in the community, to address the developmental issues in this population. However, no routine screening test for psychological problems are carried out. The current practice is to identify behavioural disorders based on parental or caregivers report during a clinic visit. We hypothesised that the use of a screening tool such as SDQ will be an objective method to identify and quantify children with psychological and behavioural problems. An effective screening tool will help to address the behavioural issues early and direct appropriate referrals to other specialities. The aim of this study was to determine the frequency of mental health disorders in children and adults with DS attending the outpatient clinic in our tertiary hospital, and also evaluate the impact on family and caregivers using the impact supplement of SDQ. We also wanted to test the ease of using SDQ as a screening tool in a clinic setting.
Figure 1.
Shows the incidence of Down syndrome from 2006 to 2019 (Unpublished data).
2. Methodology
This pilot study was conducted in KK Women's and Children's hospital, Singapore, which is a tertiary care hospital for women and children. SingHealth Centralized Institutional Review Board (CIRB 2019/2962) approved this study with a waiver of consent.
2.1. Participants
Participants were recruited from the outpatient DS clinic during routine outpatient visit from August 2019 to January 2020. After obtaining verbal consent, SDQ was administered to the parents of the recruited children aged 4–10, and to both parents and recruited participant with DS if aged 11 and above. Parents and DS patients who could not comprehend the questionnaire, had language barriers, or those who had been diagnosed with a psychiatric disorder or were on treatment were excluded. The SDQ version was conducted in English (UK). Briefly, the children were first asked to read and understand and attempt the questions. If they found it difficult, the parents would rephrase the sentence for them. If the child could not read or comprehend, they would be excluded from the study. No patient identifiers were used on the questionnaire and a case number was assigned to each responder. The results were entered into a database and analysed using IBM SPSS statistics version 19 for Windows.
2.2. Measures
The SDQ consists of 25 items describing positive and negative attributes of children and adolescents that can be allocated to 5 subscales of 5 items each: emotional, conduct, hyperactivity, peer problems and prosocial behaviour. Each item has to be scored on a 3-point scale with 0 = not true, 1 = somewhat true, and 2 = certainly true or vice versa for some positively worded problem items and for the prosocial subscale. Scores can be computed by summing the scores. Higher scores on the prosocial behaviour subscale reflect strengths, whereas higher scores on the other four subscales reflect difficulties. A total difficulties score is a total of all the 4 subscales excluding prosocial behaviour score. It ranges from 0-40 (www.sdqinfo.org). The higher the score, the higher the risk of developing a mental health disorder. A total difficulties score below 14 (parent scores) would warrant monitoring. However, a score between 14-16 (slightly raised) may need therapeutic services from a social worker, school nurse, educational psychologist or therapists. Scores of 17 and above warrant a referral to psychiatrist/primary mental health worker as described in the Decision Matrix of the SDQ (https://pdf4pro.com/file/41c38/Library_poilkj690.pdf.pdf).
Internalizing score is a summation of emotional and peer problems, and ranges between 0-20 (Goodman et al., 2010). High internalizing score reflects excessive controls of oneself, which in turn limits the social experiences of children and create obstacles for their psychological adjustment. Externalizing score (ranges 0–20) is the sum of conduct and hyperactivity scales. High score depicts impulsivity and conduct problems that manifests in children's outward behaviour. Higher externalizing scores interfere with daily routines like tooth brushing or eating. The children with higher scores are more susceptible to react negatively in an unfamiliar situation or environment, rendering them to act out or throw a temper tantrum. The prosocial score is excluded from the total difficulties score and it estimates the individuals' strengths. Higher prosocial score indicates good social skills, such as a person's ability to relate well with peers and favours actions that benefit the individuals with whom they live. This ability, however, does not include the ability to cope and overcome conflicts and adversities in their relationship (Silva et al., 2015).
The impact score included in the SDQ is an extended version and encompasses the respondent's perception of the child's overall distress. It provides useful information on the chronicity of the behavioural symptoms and its burden in areas of school, friendship, home and leisure. Impact score was calculated only for parents who perceived difficulties in one or more of the areas mentioned above for their child with DS.
Statistical analyses were carried out using Fisher's exact test for categorical variables.
3. Results
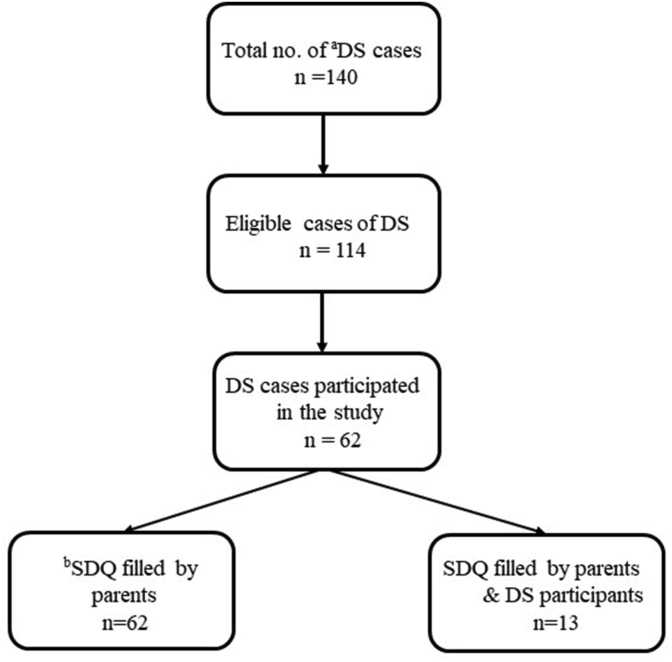
A total of 140 patients with DS were screened for recruitment during the study period and 114 were eligible. A total of 62 patients were recruited into the study (Figure 2). The demographic characteristics of the children and adults who participated in the study are shown in Table 1. The age range was 4–29 years with a mean of 12.6 (SD 6.0 years). The racial distribution was similar to the population demographics of Singapore (Table 1), and gender distribution was equal (male, 31/62 (50%)). A total of 35 (56%) patients (age ≥11) were eligible for self-reporting of SDQ. However, SDQ could only be completed by 13 (37%) of them. At the time of the study, we did not have the results of their Intelligence Quotient (IQ) assessment for the recruited patients. However the type of school they attended was documented (Table 1).
Figure 2.
Shows the recruitment process for this cohort. aDown syndrome. bStrengths and Difficulties Questionnaire.
Table 1.
Demographic characteristics of the participants (n = 62).
| Age distribution (years) | n (%) |
|---|---|
| 4–10 | 27 (43.5) |
| 11–17 | 24 (38.7) |
| ≥18 | 11 (17.7) |
| Race distribution | |
|---|---|
| Chinese | 36 (58.1) |
| Malay | 17 (27.4) |
| Indian | 7 (11.3) |
| Others | 2 (3.2) |
| School Type (Age in years) |
Normal n (%) |
APSNa n (%) |
MINDSb n (%) |
|---|---|---|---|
| 4–10 (n = 27)c | 1 (3.7) | 7 (25.9) | 19 (70.3) |
| 11–17 (n = 23) | 1 (4.3) | 7 (30.4) | 15 (65.2) |
| ≥18 (n = 11) | 0 | 5 (45.4) | 6 (54.5) |
Association for Persons with Special Needs (school for mild ID).
Movement for the Intellectually disabled of Singapore (school for the moderate to severe ID).
Children aged 4–6 years who were in early intervention programmes (EIPIC) were included in the MINDS cohort (n = 10).
Parents and DS subjects' responses to the questionnaire were stratified as per the pre-specified domains in the SDQ and are reported in Tables 2 and 3. Overall, as per parental reporting, 37.1% (23/62) of the cohort had at least a slightly raised total difficulty score, and 48.4% of our DS cohort had at least one domain in which the score was slightly raised. High or very high scores were reported by parents in the domains of peer problems in 34 (54.9%) and conduct in 13 (21%) followed by the emotional domain, 11 (17.7%). Prosocial behaviour was reported as normal in 37 (59.7%) of the cohort by the parents. The mean scores of the various domains demonstrated a high mean score in the hyperactivity and peer problem domain.
Table 2.
Results of Parent report on the 5 subscales, including total difficulties and impact score.
| Parent report (n = 62) | |||||
|---|---|---|---|---|---|
| Close to Average n (%) | Slightly raised n (%) | High n (%) | Very High n (%) | Mean Score (±SD) | |
| Emotional | 45 (72.6) | 6 (9.7) | 10 (16.1) | 1 (1.6) | 2.3 (2.1) |
| Conduct | 39 (62.9) | 10 (16.1) | 12 (19.4) | 1 (1.6) | 2.0 (1.7) |
| Hyperactivity | 48 (77.4) | 13 (21) | 1 (1.6) | 0 (0) | 3.6 (2.2) |
| Peer problems | 20 (32.3) | 8 (12.9) | 12 (19.4) | 22 (35.5) | 3.6 (2.1) |
| Prosocial | 37 (59.7) | 10 (16.1) | 4 (6.5) | 11 (17.7) | 7.8 (2.4) |
| Total Difficulties |
39 (62.9) |
8 (12.9) |
7 (11.2) |
8 (12.9) |
11.9 (7.0) |
| Impact scorea (n = 26) | 29 (7.6) | 1 (3.8) | 1 (3.8) | 22 (35.4) | |
Impact score filled by parents who perceived child's behavioural difficulties were a burden (n = 26/62).
Table 3.
aComparison between parent and self-reports (n = 13).
| aSDQ domains | Parent report (n = 13) |
Self-report (n = 13) |
p-Value | ||||
|---|---|---|---|---|---|---|---|
| Slightly raised n (%) | High n (%) |
Very High n (%) |
Slightly raised n (%) | High n (%) |
Very High n (%) |
||
| Emotional | 2 (15.4) | 2 (15.4) | 1 (7.7) | 2 (15.4) | 3 (23.1) | 0 | 1.000 |
| Conduct | 3 (23.1) | 1 (7.7) | 1 (7.7) | 1 (7.7) | 0 | 1 (7.7) | 1.000 |
| Hyperactivity | 1 (7.7) | 0 | 0 | 0 | 1 (7.7) | 1 (7.7) | 0.22 |
| Peer problems | 2 (15.4) | 0 | 6 (46.2) | 4 (30.8) | 2 (15.4) | 3 (23.1) | 1.000 |
| Prosocial | 3 (23.1) | 0 | 1 (7.7) | 0 | 0 | 2 (15.4) | 1.000 |
| Total Difficulties | 1 (7.7) | 2 (15.4) | 1 (7.7) | 0 | 1 (7.7) | 2 (15.4) | 1.000 |
p value: Fisher's exact test performed only for high and very high scores.
SDQ categorized and scored as original.
Self-report was possible in 37% (13/35), of the eligible DS participants and there were no significant differences in the responses between the parents and self-report (Table 3). The patients reported a greater concern in the domain of peer problems as compared to their parents but this difference did not reach statistical significance (Table 3).
When we compared the incidence of abnormal internalizing and externalizing scores in our cohort, 13 (21%) of the parents reported abnormal internalizing scores as compared to only 4, (6.5%) of them reporting abnormal externalizing scores. Scores in self-report followed a similar trend with patients reporting more internalizing difficulties 4 (30.7%) as compared to externalizing difficulties 1 (7.7%). When we stratified the internalizing and externalizing score by age groups, the lower age group (4–17) demonstrated a higher externalizing score and a lower internalizing score as compared the higher age group of ≥18 years (Table 4).
Table 4.
Parent and self-report (for all ages) results of internalizing and externalizing scores.
| Internalizing |
Externalizing |
|||
|---|---|---|---|---|
| High n (%) |
Very High n (%) |
High n (%) |
Very High n (%) |
|
| Parents report n = 62 | 4 (6.5) | 9 (14.5%) | 4 (6.5) | 0 |
| Self-report n = 13 | 1 (7.7) | 3 (23.0) | 0 | 1 (7.7) |
| Parent and self-report results of internalizing and externalizing scores (age ≥18) | ||||||
|---|---|---|---|---|---|---|
| Internalizing |
Externalizing |
|||||
| High n |
Very High n |
Mean score | High n |
Very High n |
Mean score | |
| Parents report n = 11 | 0 | 3 (27%) | 6.9 | 0 | 0 | 4.1 |
| Self-report n = 4 | 1 (25%) | 1 (25%) | 8.25 | 0 | 0 | 3.8 |
| Parent and self-report results of internalizing and externalizing scores (age 4–17) | ||||||
|---|---|---|---|---|---|---|
| Internalizing |
Externalizing |
|||||
| High n |
Very High n |
Mean score | High n |
Very High n |
Mean score | |
| Parents report n = 51 | 3 (5.9%) | 8 (15.7%) | 5.0 | 4 (7.8%) | 0 | 5.5 |
| Self-report n = 9 | 0 | 2 (22.2%) | 6.2 | 0 | 1 (11.1%) | 5.5 |
Extended SDQ questionnaire with impact scores revealed that a total of 26 parents reported difficulties in areas of home life, friendships, classroom learning or leisure activities. The characteristics of these difficulties are reported in Table 5. The burden of the difficulties had been present for more than a year in 19 (73%) of the cohort, and in 18 (69%) of the cases caused at least a little distress to the child. These behavioural issues resulted in a greater impact on domains of friendships and classroom as compared to those at home or at leisure. Nine of the 26 (34.6%) parents reported that their child experienced a lot of difficulties in 1 or more of the domains. Only 1 (3.8%) parent felt that these difficulties were a burden to the family.
Table 5.
Details of Impact score based on parent rating of behaviour problems in learning and relationship (n = 26)∗.
| Perception of difficulties as burden | ||||
|---|---|---|---|---|
| n (%) |
Not at all 8 (30.8) |
Little 17 (65.4) |
A lot 1 (3.8) |
Greatly 0 |
| Duration of behavioural difficulties | ||||
| Duration | <1 month | 1–5months | 6–12months | >1 year |
| n (%) |
1 (3.8) |
5 (19.2) |
1 (3.8) |
19 (73.1) |
| Areas where it affected child the most | ||||
| Not at all n (%) |
Little n (%) |
A lot n (%) |
Greatly n (%) |
|
| Home | 10 (38.5) | 15 (57.7) | 1 (3.8) | 0 |
| Friendships | 11 (42.3) | 9 (34.6) | 5 (19.2) | 1 (3.8) |
| Classroom | 6 (23.1) | 14 (53.8) | 5 (19.2) | 1 (3.8) |
| Leisure |
11 (42.3) |
13 (50) |
2 (7.7) |
0 |
| Distress to child | ||||
| Distress to child | Not at all | Little | A lot | Greatly |
| n (%) | 8 (30.8) | 13 (50) | 5 (19.2) | 0 |
Scores calculated based on parents who perceived that the child's behavioural symptoms caused distress (26/62; 41.9%).
All the parents and caregivers were asked regarding the ease of completing SDQ, and they reported finding the questionnaire easy to complete. They cited relatability and positive strengths in the SDQ as added advantages to answering the questionnaire.
4. Discussion
In this pilot study conducted on DS participants, we observed that SDQ was a useful screening tool in an outpatient setting and helped us in identifying DS persons with psychological problems requiring further monitoring or care. In addition, use of impact scores helped us to establish the burden of behavioural problems on parents/caregivers and enabled us to channel support and to institute appropriate remedial therapies.
Mental health issues are not often addressed in this population especially in Asian countries.
In this study, we found that 23/62 (37.1%) of the cohort has at least a slightly raised total difficulties score (Table 2). In addition, 15/62 (24.1%) of the study cohort had a high or very high total difficulties score. This is similar to the point prevalence of 23.7% of an abnormal total difficulty score (scores ≥17) reported by Mantry et al. (2008) and a score of 25.6% by Sarimski (2018) in both pre-school children and adults.
Overall, we found that 48.4% of the children had high or very high scores in at least one of the domains in the SDQ screening. This is similar to the results by Määttä et al. (2006), who reported 61% of their DS cohort experienced either behavioural difficulties or mood and anxiety related problems. In addition, Rice et al. (2018) in Australia (NSW) had quoted a total difficulty mean score of 14.1 (age group 4–17) in children with DS, and it is comparable to our cohort mean of 11.9.
In our study, the two main domains affected significantly in the SDQ were peer relationships and conduct as compared to prosocial behaviour and hyperactivity problems in the DS subgroup of the NSW cohort (Rice et al., 2018). The mean prosocial score was 7.8 ± 2.4 in our cohort as compared to 5.3 ± 3.0 in the NSW cohort, and the hyperactivity score was lower in our cohort (3.6 ± 2.2 Vs. 5.7 ± 2.5). This might be due to a difference in culture and parental upbringing in the populations, as our population is mainly Asian as compared the mainly Caucasian population in the other study (Stolk et al., 2017).
Among the young adults and children aged 11 and above, 22 (62.9%) were unable to participate in the self-report questionnaire. This is likely due to moderate to severe intellectual disability, resulting in an inability to comprehend, as most of them were also unable to read or write, therefore lacking capacity to self-report. We analysed the type of school the participants were attending at the time of the study, as we did not have the cognitive assessments available to us. Majority were in the school for moderate to severe ID. This is the likely reason for the inability to self-report.
Where children were able to self-report, we found peer issues being the predominant concern (Table 3). In addition, the parents also reported more impact on friendships and classroom (Table 5). This might be due to the fact that at home and during leisure activities, the parents and siblings are more tolerant of the child's behaviour and may not anticipate peer problems. In addition, the child might, therefore, perceive the home environment more favourably as compared to being in classroom or with peers.
In this pilot study, we found internalizing issues scoring higher than externalizing issues. Woo et al. (2007) in his survey on normal preschool children in Singapore reported higher internalizing issues (12.5%) as compared to externalizing problems (4.9%). Weisz et al. (1993), studied across different cultures and showed that Asian children exhibit more internalizing behaviours as compared to Caucasian American children who exhibit more externalizing behaviours. The author suggested that cultural differences and parental upbringing greatly influence children's manifestation of their behavioural symptoms. Aggression is usually discouraged in Asian culture, while self-control, emotional restraint and social inhibition are encouraged. Hence, Asian children are likely to internalize rather than externalize their behaviour.
Collacott et al. (1992) had described in his study that older adolescents with DS show fewer externalizing symptoms and a subtle increase in withdrawal compared to their younger counterparts. Disruptive behaviours, anxiety disorders and repetitive behaviours were common in those aged under 20. In our cohort, we noted similar findings, where internalizing behaviours had a higher mean (6.9) compared to externalizing (4.1) in the age group of 18 years and older as per the parent report. In the age group of 4–17 years, externalizing behaviours were more predominant (5.5 compared to 5.0) (Table 4). However, the difference was not statistically significant.
In our study, we observed that the impact of the difficulties had been present for more than a year in 19 (73.1%) of the cohort (Table 5). It is unclear as to why parents and caregivers were not identifying these issues earlier. A possible explanation is that the families become used to the behavioural symptoms over time and fail to seek medical attention when these behaviours become disruptive. Another reason is perhaps that the parents are caught up with their other responsibilities, and that they find the behaviours manageable and may not want to accept another diagnosis following evaluation by another subspecialty e.g. psychology. Parents may also be wary of commencing a new medication or becoming more aware due to social stigma of a psychiatric diagnosis.
4.1. Limitations and future implications
This pilot study has some limitations, one being the small sample size. Replication of a larger sample size across institutions is desirable. It would also be useful to attain SDQ differences related to age, gender and socio-economic status. Inclusion of teacher reports will also be beneficial as majority are in special schools and have a formal education. In addition, including DS with psychiatric problems would have added more weight to the study. Despite these limitations, this pilot study has shown that SDQ is a valuable screening tool for identification of emotional and behavioural problems in a DS population.
4.2. Conclusion
We find the SDQ a feasible and practical tool for identification of emotional and behavioural problems in a DS population. Our study reinforces the need for a user-friendly screening tool in the outpatient setting for early identification of mental health disorders in children and adolescents with DS as the incidence of mental health issues can be as high as 30%. This will facilitate onward referral and help in addressing parental and patient's concerns early.
Declarations
Author contribution statement
K. Sothirasan: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
A. Anand: Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
R. Mittal: Analyzed and interpreted the data; Wrote the paper.
S. Chandran: Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
P. Khoo: Contributed reagents, materials, analysis tools or data.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- Bittles A.H., Bower C., Hussain R., Glasson E.J. The four ages of Down syndrome. Eur. J. Publ. Health. 2007;17(2):221–225. doi: 10.1093/eurpub/ckl103. [DOI] [PubMed] [Google Scholar]
- Collacott R.A., Cooper S., McGrother C. Differential rates of psychiatric disorders in adults with Down syndrome compared with other mentally handicapped adults. Br. J. Psychiatry. 1992;161:671–674. doi: 10.1192/bjp.161.5.671. [DOI] [PubMed] [Google Scholar]
- Einfeld S.L., Tonge B.J. Population prevalence of psychopathology in children and adolescents with intellectual disability. II. Epidemiological findings. J. Intellect. Disabil. Res. 1996;40(Pt2):99–109. doi: 10.1046/j.1365-2788.1996.768768.x. [DOI] [PubMed] [Google Scholar]
- Glenn S., Cunningham C., Nananidou A., Prasher V., Glenholmes P. Using the strengths and difficulties questionnaire with adults with Down syndrome. Res. Dev. Disabil. 2013;34(10):3343–3351. doi: 10.1016/j.ridd.2013.06.034. [DOI] [PubMed] [Google Scholar]
- Goodman R. The strengths and difficulties questionnaire: a research note. JCPP (J. Child Psychol. Psychiatry) 1997;38(5):581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J. Am. Acad. Child Adolesc. Psychiatr. 2001;40(11):1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- Goodman A., Lamping D.L., Ploubidis G.B. When to use broader internalising and externalising subscales instead of the hypothesised five subscales on the Strengths and Difficulties Questionnaire (SDQ): data from British parents, teachers and children. J. Abnorm. Child Psychol. 2010;38(8):1179–1191. doi: 10.1007/s10802-010-9434-x. [DOI] [PubMed] [Google Scholar]
- Kaptein S., Jansen D.E., Vogels A.G., Reijneveld S.A. Mental health problems in children with intellectual disability: use of the Strength and Difficulties Questionnaire. J. Intellect. Disabil. Res. 2008;52(Pt 2):125–131. doi: 10.1111/j.1365-2788.2007.00978.x. [DOI] [PubMed] [Google Scholar]
- Lai F.M., Woo B.H., Tan K.H., Huang J., Lee S.T., Tan B.Y., Chew S.K., Yeo G.S.H. Birth prevalence of Down syndrome in Singapore from 1993 to 1998. Singap. Med. J. 2002;43(2):70–76. [PubMed] [Google Scholar]
- Määttä T., Tervo-Määttä T., Taanila A., Kaski M., Iivanainen M. Mental health, behaviour and intellectual abilities of people with Down syndrome. Down Syndrome Res. Pract. 2006;11(1):37–43. doi: 10.3104/reports.313. [DOI] [PubMed] [Google Scholar]
- Mantry D., Cooper S.A., Smiley E., Morrison J., Allan L., Williamson A., Finlayson & J., Jackson A. The prevalence and incidence of mental ill-health in adults with Down syndrome. J. Intellect. Disabil. Res. 2008;52(Pt 2):141–155. doi: 10.1111/j.1365-2788.2007.00985.x. [DOI] [PubMed] [Google Scholar]
- Oeseburg B., Jansen D.E., Groothoff J.W., Dijkstra G.J., Reijneveld S.A. Emotional and behavioural problems in adolescents with intellectual disability with and without chronic diseases. J. Intellect. Disabil. Res. 2010;54(1):81–89. doi: 10.1111/j.1365-2788.2009.01231.x. [DOI] [PubMed] [Google Scholar]
- Rice L.J., Emerson E., Gray K.M., Howlin P., Tonge B.J., Warner G.L., Einfeld S.L. Concurrence of strengths and difficulties questionnaire and developmental behaviour checklist among children with an intellectual disability. J. Intellect. Disabil. Res. 2018;62(2):150–155. doi: 10.1111/jir.12426. [DOI] [PubMed] [Google Scholar]
- Ritchie H., Roser M. 2020. Mental health.OurWorldIndata.orghttps://ourworldindata.org/mental-health Published online at. [Google Scholar]
- Sarimski K. Verhaltensauffalligkeiten von Kindern mit Down-Syndrom im Vorschulalter [Behaviour problems of children with Down syndrome in preschool-age- Results from the Heidelberg Down syndrome study] Z. Kinder JugenPsychiatr. Psychother. 2018;46(3):194–205. doi: 10.1024/1422-4917/a000523. [DOI] [PubMed] [Google Scholar]
- Subramaniam M., Abdin E., Vaingankar J.A., Shafie S., Chua B.Y., Sambasivam R., Zhang Y.J., Shahwan S., Chang S., Chua H.C., Verma S., James L., Kwok K.W., Heng D., Chong S.A. Tracking the mental health of a nation: prevalence and correlates of mental health disorders in the second Singapore mental health study. Epidemiol. Psychiatr. Sci. 2020;29(e29):1–10. doi: 10.1017/S2045796019000179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stolk Y., Kaplan I., Szwarc J. Review of the strengths and difficulties questionnaire translated into languages spoken by children and adolescents of refugee background. Int. J. Methods Psychiatr. Res. 2017;26(4) doi: 10.1002/mpr.1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva Thaysa B.F., Osorio Flavia L., Loureiro Sonia R. SDQ: discriminative validity and diagnostic potential. Front. Psychol. 2015;6:811. doi: 10.3389/fpsyg.2015.00811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz J.R., Suwanlert S., Chaiyasit W., Weiss B., Achenbach T.M., Eastman K.L. Behavioral and emotional problems among Thai and American adolescents: parent reports for ages 12-16. J. Abnorm. Psychol. 1993;102(3):395–403. doi: 10.1037//0021-843x.102.3.395. [DOI] [PubMed] [Google Scholar]
- World Health Organization . 2015. World Health Statistics 2015.https://www.who.int/gho/publications/world_health_statistics/2015/en/ [Google Scholar]
- Woo B.S., Ng T.P., Fung D.S., Chan Y.H., Lee Y.P., Koh J.B.K., Cai Y. Emotional and behavioural problems in Singaporean children based on parent, teacher and child reports. Singap. Med. J. 2007;48(12):1100–1106. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.