Abstract
Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) is a rare inflammatory disorder featured by pontocerebellar dysfunctions and, in some cases, later cognitive disturbances. Here, we describe an atypical presentation of CLIPPERS, characterized by clinical onset with neuropsychiatric and cognitive symptoms. A 45-year-old man was referred to our Memory Clinic due to difficulties at work for over a month, caused by confusion and asthenia. Furthermore, insomnia and mood changes appeared. These disturbances were unresponsive to antipsychotic and antidepressant drugs. At admission, the patient presented also with severe cognitive impairment, urinary incontinence, ataxic gait, and limitation of lateral conjugate gaze. During the hospitalization, the patient underwent cerebrospinal fluid analysis, serum systemic autoimmune disorders laboratory research, neoplastic markers analysis, and brain MRI scan. The radiological and laboratory findings were compatible with the diagnosis of CLIPPERS. The sudden clinical and radiological improvement of the patient's conditions, after only a week of steroid therapy, further confirmed our clinical suspicion. The present case enhances the necessity to consider CLIPPERS in the differential diagnosis of pre-senile cognitive impairment, even in the absence of early pontocerebellar neurological signs. Before the spreading of the neuroinflammatory and degenerative processes, CLIPPERS represents one among the few possible reversible causes of cognitive decline.
Keywords: CLIPPERS, Early-onset dementia, Reversible dementia, Autoimmune diseases, Magnetic resonance imaging
Introduction
Reversible causes of cognitive impairment are underestimated conditions, often resulting from endocrine, infective, or nutritional deficiency and account for up to 19% of the cases of dementia-like disorders [1]. The diagnosis of dementia, and the possibility to rule out reversible causes of cognitive impairment, is particularly challenging in young patients. Neuroinflammation plays a significant role in producing cognitive impairment in the youngest. According to Kelley et al. [2], inflammatory diseases account for 21% of the cases of cognitive impairment found in young individuals.
Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) is a rare central nervous system inflammatory disorder [3]. CLIPPERS features an array of symptoms driven by the underlying T cell-mediated pathology affecting the brainstem, as well as characteristic magnetic resonance imaging (MRI) findings of punctate and curvilinear gadolinium pontocerebellar enhancements [3]. Since its first description in 2010 [4], several unusual presentations, including occipital headache [5], seizures [6], and trigeminal neuropathy [7], have been reported. We here describe an atypical presentation of CLIPPERS characterized by neuropsychiatric and cognitive symptoms at onset.
Case Presentation
A 45-year-old man came to our observation, reporting to have suffered for more than a month from asthenia and confusion, in combination with neuropsychiatric symptoms (i.e., depression, irritability, and insomnia), which had affected his work performance. The patient had been diagnosed by a psychiatrist with pseudodementia and treated, without significant improvement, with olanzapine (5 mg/day) and escitalopram (20 mg/day). At admission to our ward, the patient exhibited signs of cognitive impairment (MMSE: 22/30), urinary incontinence, ataxic gait, and limitation of the lateral conjugate gaze. The patient's medical history was unremarkable, besides the presence of benign ileal lymphoid hyperplasia and amblyopia.
During the hospitalization, the patient had a diagnostic workup (Table 1) which included a lumbar puncture that revealed increased protein levels (283 mg/dL) and lymphocytic pleocytosis (195 leucocytes, 97% lymphocytes) with a significant prevalence of CD4+CD3+ T cells in the cerebrospinal fluid (CSF). CSF glucose levels were only slightly decreased (37.3% of blood glucose). The cytological examination and clonality testing revealed a polyclonal pattern of T-cell receptors, thereby ruling out the possibility of an underlying lymphoma. The link index was normal and no oligoclonal bands were observed in the CSF. The laboratory workup excluded tuberculosis, syphilis, Borrelia, and infections by cytomegalovirus, HIV, HSV, or VZV. Serum markers of systemic autoimmune disorders, neoplastic markers, as well as onconeural, anti-AQ4, anti-glycolipids, and anti-sulfatides antibodies were negative. Only an aspecific positivity for anti-myelin oligodendrocyte glycoprotein antibodies (anti-MOG) was found in the CSF. Markers of neurodegeneration and amyloid deposition were negative. A total-body computed tomography was normal. A brain and spinal MRI scan (Fig. 1; top row) finally revealed, along with spinal central holocord enhancement, a pattern of widespread perivascular dot-shaped and curvilinear enhancements, mostly affecting the pontocerebellar region, compatible with CLIPPERS.
Table 1.
Diagnostic workup
| Infectious disease markers | Primitive autoimmune neurological disorder markers | |
| HSV, VZV, EBV, CMV DNA PCR test | Routine CSF physical and chemical examination | |
| Borrelia Ab | CSF oligoclonal bands | |
| Anti-treponema Ab, VDRL, TPHA | Anti-AQ4, anti-aquaporin 4 Ab | |
| Ziehl-Neelsen stain, Quantiferon | Anti-MOG, anti-myelin oligodendrocyte glycoprotein Ab (sometimes positive also in CLIPPERS) | |
| HIV markers | ||
| Neurodegenerative disease markers | ± other anti-sulfatides and anti-glycolipids Ab (anti-GM1, anti-GM2, anti-GD1a, anti-GD1b, anti-GM3) | |
| CSF Aβ 42, total-tau, phospho-tau, protein 14.3.3 | ||
| Systemic autoimmune disorder markers | Neoplastic/paraneoplastic disease markers | |
| ANA, anti-nuclear antigen antibodies (Ab) | Ca19-9 | Anti-SOX1 Ab |
| ENA, extractable nuclear antigen | Ca15-3 | Anti-titin Ab |
| Anti-DNA Ab | NSE, neuron specific enolase | Anti-Zic4 Ab |
| ASMA, anti-smooth muscle Ab | αFP, α-fetoprotein | Anti-GAD65 Ab |
| AMA, anti-mitochondrial Ab | CEA, carcinoembryonic antigen | Anti-Tr Ab |
| Rheumatoid factor | Anti-Ma1 Ab | Anti-VGKC Ab |
| Anti-CCP, anti-cyclic citrullinated peptide Ab | Anti-Ma2/Ta Ab | Anti-NMDAr Ab |
| Anticentromere Ab | Anti-CV2 Ab | Routine CSF physical and chemical examination (cell count, proteins, glucose) |
| p-ANCA, perinuclear antineutrophil cytoplasmic Ab | Anti-Hu Ab | |
| c-ANCA, cytoplasmic antineutrophil cytoplasmic Ab | Anti-Ri p54 Ab | |
| Anticardiolipin Ab | Anti-Yo Ab | Cytologic exam on CSF white cells |
| Anti-β2-glycoprotein I Ab | Anti-amphiphysin Ab | Clonality test on CSF white cells |
| Anti-phospholipid Ab | Anti-recoverin Ab | |
| Anti-prothrombin Ab | ||
| C3, complement component 3 | ||
| C4, complement component 4 | ||
Fig. 1.
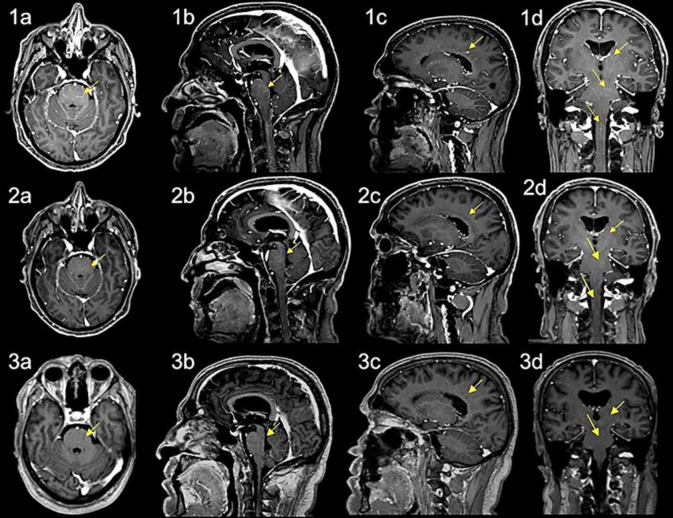
Brain MRI scan at admission, after 1 week of steroid therapy, and after 1 month of steroid therapy. Gd-enhanced MRI scans of the brain. The arrows indicate the main sites of the widespread pattern of perivascular dot-shaped and curvilinear enhancement, mostly within the pontocerebellar region, but also surrounding the lateral ventricles. Also, central spinal enhancement can be observed. The scan on the first line was acquired before the therapy. The scan on the middle line was obtained after 1 week of high-dose steroid therapy. The scan on the lower line shows complete resolution of the picture after 1 month of steroid therapy. First column (a), axial section; second and third column (b, c), sagittal sections; fourth column (d), coronal section.
The clinical presentation together with the MRI and laboratory findings were in line with a CLIPPERS diagnosis. High-dose steroid therapy with methylprednisolone 1 g/day was administered for 5 days and followed by a course of prednisone 1 mg/kg/day. The steroid therapy resulted in a rapid improvement of gait and gaze as well as the resolution of the cognitive deficits (MMSE: 30/30) and psychiatric signs. Brain and spinal MRI scans were repeated after 1 week of steroid therapy and documented a dramatic improvement of the imaging findings (Fig. 1; middle row). The neurological exam, lumbar puncture, and MRI scan, repeated after 1 month (Fig. 1; bottom row), documented the complete resolution of the symptoms and signs. In the following 4 months, prednisone therapy was gradually discontinued, while azathioprine was introduced. At the fifth month of follow-up, the patient exhibited signs of clinical and radiological relapse, so a second course of steroid therapy, along with rituximab, was started. The patient has been asymptomatic since then.
Discussion and Conclusions
This is the first report of a CLIPPERS case exhibiting cognitive and psychiatric disturbances as first symptoms of the disease, an uncommon finding given that these clinical features usually occur later, in the disease course, and are mild [8]. If identified before the spreading of the neuroinflammatory process and the ensuing of brain and cerebellar atrophy, CLIPPERS represents a reversible cause of cognitive decline [8]. From a prognostic viewpoint, CLIPPERS relapses, typically occurring in patients who have not been treated with long-term courses of high doses of corticosteroids or alternative immunosuppressants [9], can lead to sequelae, disability, and even to death [10]. As a final remark, CLIPPERS is associated with a high prevalence of malignancies [4, 10]; therefore, a prompt diagnosis is needed to allow appropriate therapy, prevent irreversible lesions [11, 12], and put in place an appropriate workflow of long-term clinical and radiological follow-ups.
Statement of Ethics
The patient's written informed consent was acquired for publication of medical records, including images.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. This study is not industry sponsored.
Funding Sources
No targeted funding reported.
Author Contributions
M.R.: Management of the patient, first diagnosis, paper writing, Figure and Table creation. A.P.: Paper writing. C.C.: Management of the patient, first diagnosis, paper writing. F.D.: Management of the patient, paper writing, Figure and Table creation. M.V.D.: Management of the patient, first diagnosis. S.L.S.: Manuscript revision and process supervision. M.O.: Manuscript revision and process supervision. L.B.: Manuscript revision and process supervision.
Acknowledgement
The authors want to acknowledge Prof. Massimo Caulo for MRI scan acquisition and for the contribution to its first interpretation.
References
- 1.Bello VM, Schultz RR. Prevalence of treatable and reversible dementias: A study in a dementia outpatient clinic. Dement Neuropsychol. 2011 Jan-Mar;5((1)):44–7. doi: 10.1590/S1980-57642011DN05010008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kelley BJ, Boeve BF, Josephs KA. Young-onset dementia: demographic and etiologic characteristics of 235 patients. Arch Neurol. 2008 Nov;65((11)):1502–8. doi: 10.1001/archneur.65.11.1502. [DOI] [PubMed] [Google Scholar]
- 3.Tobin WO, Guo Y, Krecke KN, Parisi JE, Lucchinetti CF, Pittock SJ, et al. Diagnostic criteria for chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) Brain. 2017 Sep;140((9)):2415–25. doi: 10.1093/brain/awx200. [DOI] [PubMed] [Google Scholar]
- 4.Pittock SJ, Debruyne J, Krecke KN, Giannini C, van den Ameele J, De Herdt V, et al. Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) Brain. 2010 Sep;133((9)):2626–34. doi: 10.1093/brain/awq164. [DOI] [PubMed] [Google Scholar]
- 5.Cordano C, López GY, Bollen AW, Nourbakhsh B. Occipital Headache in Chronic Lymphocytic Inflammation With Pontine Perivascular Enhancement Responsive to Steroids (CLIPPERS) Headache. 2018 Mar;58((3)):458–9. doi: 10.1111/head.13232. [DOI] [PubMed] [Google Scholar]
- 6.Okune S, Ishii K, Ouchi S, Sakakura K, Matsuda M, Tamaoka A. A cerebral phenotype of chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids: A case report and review of the literature. Mult Scler Relat Disord. 2018 Feb;20:159–63. doi: 10.1016/j.msard.2018.01.017. [DOI] [PubMed] [Google Scholar]
- 7.Bobba S, Narasimhan M, Zagami AS. Isolated painful trigeminal neuropathy as an unusual presentation of chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids: A case report. Cephalalgia. 2019 Feb;39((2)):316–22. doi: 10.1177/0333102418781789. [DOI] [PubMed] [Google Scholar]
- 8.Simon NG, Parratt JD, Barnett MH, Buckland ME, Gupta R, Hayes MW, et al. Expanding the clinical, radiological and neuropathological phenotype of chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) J Neurol Neurosurg Psychiatry. 2012 Jan;83((1)):15–22. doi: 10.1136/jnnp-2011-301054. [DOI] [PubMed] [Google Scholar]
- 9.Wijntjes J, Wouda EJ, Siegert CE, Karas GB, Vlaar AM. Need for prolonged immunosupressive therapy in CLIPPERS—a case report. BMC Neurol. 2013 May;13((1)):49. doi: 10.1186/1471-2377-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Graaff HJ, Wattjes MP, Rozemuller-Kwakkel AJ, Petzold A, Killestein J. Fatal B-cell lymphoma following chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids. JAMA Neurol. 2013 Jul;70((7)):915–8. doi: 10.1001/jamaneurol.2013.2016. [DOI] [PubMed] [Google Scholar]
- 11.Zalewski NL, Tobin WO. CLIPPERS. Curr Neurol Neurosci Rep. 2017 Sep;17((9)):65. doi: 10.1007/s11910-017-0773-7. [DOI] [PubMed] [Google Scholar]
- 12.Dudesek A, Rimmele F, Tesar S, Kolbaske S, Rommer PS, Benecke R, et al. CLIPPERS: chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids. Review of an increasingly recognized entity within the spectrum of inflammatory central nervous system disorders. Clin Exp Immunol. 2014 Mar;175((3)):385–96. doi: 10.1111/cei.12204. [DOI] [PMC free article] [PubMed] [Google Scholar]