Abstract
Purpose:
To retrospectively compare technical success and major complication rates of laparoscopically versus radiologically inserted jejunostomy tubes.
Materials and Methods:
In this single-institution retrospective study, 115 patients (60 men; mean age, 59.7 y) underwent attempted laparoscopic jejunostomy tube insertion as a standalone procedure during a 10-year period and 106 patients (64 men; mean age, 61.0 y) underwent attempted direct percutaneous radiologic jejunostomy tube insertion during an overlapping 6-year period. Clinical outcomes were retrospectively reviewed with primary focus on predictors of procedure-related major complications within 30 days.
Results:
Patients undergoing laparoscopic jejunostomy tube insertion were less likely to have previous major abdominal surgery (P <.001) or to be critically ill (P <.001) and had a higher body mass index (P =.001) than patients undergoing radiologic insertion. Technical success rates were 95% (110 of 115) for laparoscopic and 97% (103 of 106) for radiologic jejunostomy tube insertion (P =.72). Major procedural complications occurred in 7 patients (6%) in the laparoscopic group and in 5 (5%) in the radiologic group (P = 1.0). For laparoscopic jejunostomy tubes, only previous major abdominal surgery was significantly associated with a higher major procedure complication rate (14% [5 of 37] vs 3% [2 of 78] in those without; P = .039). In the radiologic jejunostomy group, only obesity was significantly associated with a higher major complication rate: 20% (2 of 10) vs 3% (3 of 96) in nonobese patients (P =.038).
Conclusions:
Laparoscopic and radiologic jejunostomy tube insertion both showed high success and low complication rates. Previous major abdominal surgery and obesity may be pertinent discriminators for patient selection.
Direct gastric feeding via a transabdominal gastrostomy tube is considered to be the first choice for long-term nutrition in patients who cannot receive oral alimentation (1). Although gastric feeding provides optimal physiologic benefit and practical bolus capabilities, there are numerous contraindications to gastrostomy tube insertion, including previous gastrectomy, gastric outlet obstruction, hiatal hernia, pancreatitis, gastroparesis, and severe reflux with aspiration (1–3). For patients who cannot receive transgastric access, a direct jejunostomy tube is typically the optimal route for nutrition. Historically, jejunostomy tubes have been inserted with open surgical techniques. More recently, laparoscopic jejunostomy tube insertion has gained popularity as a less invasive method that is considered to convey less morbidity and operative stress than open surgical jejunostomy (4–6).
Jejunostomy tube insertion has also been reported with the use of percutaneous radiologic techniques. Needle puncture of the jejunum can be performed with fluoroscopic, ultrasound, or computed tomographic (CT) guidance (7–13). The primary challenge to percutaneous radiologic jejunostomy tube insertion is successful puncture and securement of the mobile jejunal loop to the anterior abdominal wall, which is typically accomplished with the use of T-fasteners. One potential advantage of percutaneous radiologic insertion is the ability to use moderate sedation, whereas general anesthesia is typically required for open or laparoscopic insertion. Although both laparoscopic and radiologic jejunostomy tube insertion constitute minimally invasive techniques, comparative outcomes and factors that may influence patient selection are unknown. Therefore, the purpose of the present study was to compare outcomes after laparoscopic versus radiologic jejunostomy tube insertion, with analysis of factors that correlate with complications.
MATERIALS AND METHODS
Patient Population
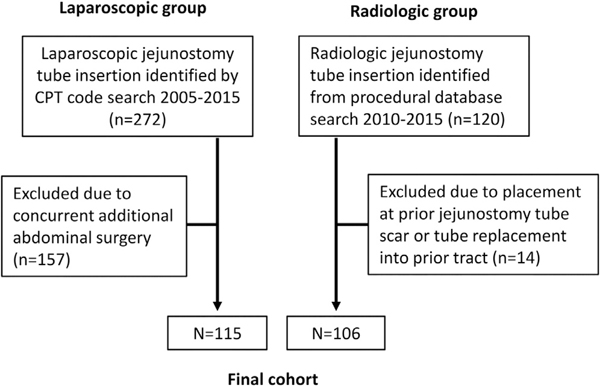
This retrospective study was approved by the institutional review board, and a waiver of the requirement for consent was obtained. Review of the surgical database from 2005 through 2015 revealed 115 adult patients (60 men and 55 women; mean age, 59.7 y; range, 18–89 y) who underwent primary laparoscopic jejunostomy tube insertion as a standalone procedure (ie, without adjunct abdominal surgery) by the general surgery or surgical oncology services (Fig). Review of the interventional radiology procedural database revealed 106 adult patients (64 men and 42 women; mean age, 61.0 y; range, 25–89 y) who underwent percutaneous radiologic jejunostomy tube insertion at a de novo site between 2010 and 2015. Insertions of radiologic jejunostomy tubes at the site of a previous jejunostomy tube were not included because the preexisting jejunopexy may impact outcomes. A portion of this cohort was previously reported (8). The decision to perform surgical versus radiologic jejunostomy tube insertion was primarily determined by the referring service, but, in some instances, one service declined or recommended the other service.
Figure.
Flow diagram of subject enrollment. CPT = Current Procedural Terminology.
Percutaneous Radiologic Jejunostomy Tube Insertion Technique
All radiologic jejunostomy tube insertion procedures were performed in the interventional radiology suites by an interventional radiology attending physician, under moderate sedation, according to a previously described technique (8). The majority of procedures were performed by an interventional radiologist with less than 10 years of experience, with a few performed by one with greater than 20 years of experience. Unless patients had previous colectomy or the colon was determined to be remote from potential target jejunal loops in the left lower quadrant on a previous CT scan, patients were administered barium orally or via nasoenteric tube the day before the procedure to opacify the transverse, left, and sigmoid colon or per rectum immediately before the procedure. Patients were administered 1 g ceftriaxone for antibiotic prophylaxis. If a nasojejunal feeding tube was not already present, a 5-F angled hydrophilic catheter (Terumo, Somerset, New Jersey) was advanced through the nostril into the proximal jejunum over a hydrophilic guide wire (Glidewire; Terumo) under fluoroscopic guidance.
Approximately 1 minute after administration of 1 mg intravenous glucagon, digital subtraction enterography was performed while rapidly insufflating the jejunum with air to distend and visualize air-filled jejunum until an adequate loop was identified. An adequate loop was defined as one that was well-distended with air, as proximal as possible, relatively linear in configuration, and very anterior (ie, just under the abdominal wall). A loop of jejunum was deemed anterior if it was easily deformable with gentle manual palpation and if air could be aspirated from the target loop with the use of the 25-gauge, 1.5-inch needle (BD Bio-sciences, San Jose, California) used for local anesthesia. After administration of local anesthesia and creation of a 5-mm incision, a T-fastener needle (Saf-T-Pexy; Halyard Health, Alpharetta, Georgia; or Cope Gastrointestinal Suture Anchor; Cook, Bloomington, Indiana) was used to access the bowel using a rapid thrust at a 45° angle toward the intended direction of bowel. Successful puncture was confirmed by injection of iodinated contrast medium. After the T-fastener was deployed, a guide wire (0.018-in for the Halyard T-fastener or 0.035-in for the Cook T-fastener) was inserted through the needle. Over the guide wire, a triaxial introducer system (AccuStick; Boston Scientific, Marlborough, Massachusetts) for the Halyard T-fastener or 4-F vascular sheath (Brite Tip; Cordis, Hialeah, Florida) for the Cook T-fastener was inserted. One or two additional T-fasteners were then deployed through the outer portion of the triaxial introducer or vascular sheath, respectively. After serial dilation, a custom-length 12-F balloon-retained MIC jejunostomy tube (Halyard Health) was inserted over the guide wire through a 15-F peel-away sheath. The balloon was inflated with 3 mL of a fluid mixture consisting of saline solution and approximately 0.5 mL of iodinated contrast medium (iopamidol 300; Bracco Diagnostics, Princeton, New Jersey). Injection of iodinated contrast medium into the tube was performed to confirm intraluminal positioning. The T-fastener sutures were then secured with the accompanying locking bolster (Halyard) or secured to the jejunostomy tube retention disc (Cook).
For at least 24 hours, the patient was maintained with nothing per mouth or tube, and daily abdominal radiographs were obtained. If, after 24 hours, the patient had a benign finding on abdominal examination without evidence of ileus on abdominal radiography, tube feeding was initiated.
Laparoscopic Jejunostomy Tube Insertion Technique
All laparoscopic jejunostomy tube insertion procedures were performed in the operating room under general endotracheal anesthesia. All patients received preoperative antibiotic agents according to Surgical Care Improvement Project guidelines (14). Intraabdominal access was obtained by using a 5-mm trocar in the left upper quadrant. Following initial insufflation with carbon dioxide, 3 additional trocars were placed, including a supraumbilical and 2 right-sided 5-mm ports. Lysis of adhesions was performed as needed. A selected loop of jejunum was presented to the left side of the abdomen, allowing transfascial placement of 4 sutures or T-fasteners under laparoscopic guidance. The bowel was then accessed with a 10-mL syringe and needle system, with intraluminal confirmation via air insufflation. A guide wire was passed into the distal jejunal limb, allowing placement of a peel-away sheath and then a 12-F jejunostomy tube (Flexiflo; Abbott, Abbott Park, Illinois) or 14-F balloon-retained MIC jejunal feeding tube (Halyard Health). For the balloon-retained tubes, the balloon was inflated with 2–3 mL of saline solution. The jejunal tube was anchored to the skin with nylon monofilament sutures, and trocar incisions were closed with buried absorbable sutures and surgical glue. The patient was maintained with nothing per mouth or tube for 24 hours, after which time tube feeding was initiated if the abdominal examination had benign findings.
Data Analysis
Patients were considered critically ill if they were admitted to the intensive care unit before the jejunostomy tube insertion during the same admission. Patients were considered to have undergone major abdominal surgery if any portion of stomach or bowel was operated on or if there was open exposure of the peritoneal cavity. Major surgeries are tabulated in Table 1. Patients with a body mass index of 30 kg/m2 or greater were considered to be obese.
Table 1.
Tabulation of All Major Surgeries in the Total Jejunostomy Tube Cohort
| Major Surgery Type | No. of Pts. |
|---|---|
| Exploratory laparotomy | 6 |
| Esophagectomy | 7 |
| Esophagogastrectomy | 24 |
| Gastrectomy | 11 |
| Gastric fundoplication | 3 |
| Gastric bypass | 6 |
| Gastrojejunostomy anastomosis | 4 |
| Pancreaticoduodenectomy | 7 |
| Other pancreatic surgery | 4 |
| Other Roux-en-Y surgery | 13 |
| Liver transplant | 5 |
| Open cholecystectomy | 3 |
| Prior jejunostomy tube (separate site) | 5 |
| Colectomy | 3 |
| Other | 10 |
Note-The table includes surgeries undergone by ≥3 patients.
Technical success was defined as successful insertion of the tube intraluminally within the jejunum. For laparoscopically inserted tubes, procedural abortion after insertion of laparoscopic trocars or conversion to open surgery constituted a technical failure. For radiologically inserted tubes, the inability to identify an appropriate loop of bowel for access and abortion of the procedure constituted a technical failure. Complications were divided into tube-specific complications and procedural complications, which were separately analyzed. Tube-specific complications included tube obstruction, peritube leakage, and tube dislodgment. Tube obstruction was defined as inability to infuse tube feedings, requiring tube exchange to restore function. Peritube leakage was defined as present if the patient was referred to the interventional radiology service for tube evaluation or exchange specifically as a result of persistent excessive leakage from around the outside of the tube. Tube dislodgment was defined as episodes of inadvertent tube removal requiring reinsertion. All events were analyzed during the total jejunostomy tube indwell time, which ended when the tube was removed and no longer needed. Procedural complications occurring within 30 days after insertion and meeting criteria as a major complication per Society of Interventional Radiology Clinical Practice Guidelines (ie, requiring therapy or hospitalization or resulting in permanent adverse sequelae or death) (15) were recorded and described.
Statistical Analysis
Statistical analysis was performed by using SPSS statistical software (version 22; IBM, Armonk, New York). For demographic variables, continuous variables were compared with the Student t test and categoric variables were compared between groups with the χ2 or Fisher exact test. Technical success and complication rates were compared between laparoscopic and radiologic jejunostomy tube insertions by χ2 or Fisher exact test. The rate of tube-specific complications was reported as events per 1,000 catheter indwell days. Predictors of major procedural complications were calculated for the entire cohort by using a univariate binomial logistic regression analysis. Additional analysis was performed for each group separately to determine whether there are predictors of major complications that are specific to either group. For any predictor with a P value less than or equal to .10, a multivariate analysis was performed for the respective group. The number of tube-related complications per 1,000 catheter indwell days was compared by Poisson regression with an overdispersion parameter. A P value less than or equal to .05 was considered statistically significant.
RESULTS
Demographic Data
During the study period, a total of 221 patients underwent jejunostomy tube insertion as a standalone procedure, of which 115 were performed laparoscopically and 106 were performed with percutaneous radiologic technique (Table 2). A significantly higher proportion of patients in the radiologic group (29%) were critically ill (ie, requiring intensive care stay during procedural admission) compared with the laparoscopic group (1%; P <.001). Previous major abdominal surgery was significantly more common in the radiologic jejunostomy tube group than in the laparoscopic group (70% vs 32%; P <.001). Patient body mass index was significantly higher in the laparoscopic group (23.8 kg/m2 vs 21.8 kg/m2; P = .001). There were no significant differences between groups in age, sex, cancer diagnosis, previous lung transplantation, diabetes, or ascites. In the laparoscopic group, 30 patients (26%) required intraoperative lysis of adhesions. Patients in the laparoscopic group with previous major surgery were significantly more likely to require lysis of adhesions compared with patients with no previous surgery (50% vs 15%; P = .002).
Table 2.
Demographic Information for Laparoscopic and Radiologic Jejunostomy Tube Groups
| Variable | Laparoscopic (n = 115) | Radiologic (n = 106) | P Value |
|---|---|---|---|
| Male sex | 61 (53) | 63 (59) | .34 |
| Age | 59.7 | 61.0 | 1.0 |
| BMI | 23.8 | 21.8 | .001 |
| Obesity (BMI ≥30 kg/m2) | 19 (17) | 10 (9) | .16 |
| Cancer | 75 (65) | 60 (57) | .21 |
| Lung transplant | 4 (3) | 10 (9) | .1 |
| Diabetes | 13 (11) | 17 (16) | .33 |
| Ascites | 5 (4) | 6 (6) | .76 |
| Critical illness | 1 (1) | 31 (29) | < .001 |
| Prior major abdominal surgery | 37 (32) | 75 (71) | < .001 |
Note-Values in parentheses are percentages.
BMI = body mass index.
Technical Success
The technical success rate for laparoscopic jejunostomy tube insertion was 96% (110 of 115). Four surgeries were converted from laparoscopic to open because of excessive intraabdominal adhesions. In one patient, the surgery was aborted as a result of peritoneal carcinomatosis. In the radiologic jejunostomy tube group, the technical success rate was 97% (103 of 106). In one patient, an acceptable loop of jejunum could not be identified for puncture. In 2 patients, T-fasteners were deployed into a target loop, but the tube could not be inserted as a result of loss of guide wire access. There was no difference in technical success rate between modalities (P = .72).
Tube-Specific Complications
The mean and median follow-up times for laparoscopically placed jejunostomy tubes were 202 and 109 days, respectively, and 221 and 97 days, respectively, for radiologically placed jejunostomy tubes. Rates of jejunostomy tube exchange as a result of tube obstruction were 0.8 per 1,000 catheter days for the laparoscopic group and 1.6 per 1,000 catheter days for the radiologic group. Rates of jejunostomy tube exchange as a result of pericatheter leakage were 0.8 per 1,000 catheter days for the laparoscopic group and 1.6 per 1,000 catheter days for the radiologic group. Rates of catheter dislodgment requiring replacement were 2.8 per 1,000 catheter days for the laparoscopic group and 1.7 per 1,000 catheter days for the radiologic group. Statistical analysis of tube complication frequency rates revealed no significant differences between laparoscopically and radiologically inserted tubes for all 3 categories (P =.13, P =.18, and P = .07, respectively).
Procedural Complications
The occurrence of major procedural complications was similar between groups: 5 in the radiologic jejunostomy tube group (5%) and 7 in the laparoscopic jejunostomy tube group (6%; P = 1.0). Table 3 describes all major complications. The 30-day rate of mortality as a result of major complication was 3% for each group, with 3 deaths each. Univariate analysis of factors correlated with major complications for the combined cohort demonstrated that only obesity was significantly associated with higher incidence of major complications (5 of 29 [17%] vs 7 of 192 [4%]; P = .006; odds ratio [OR], 5.5; 95% confidence interval [CI], 1.6–18.7; Table 3). Based on multivariate analysis, along with previous major abdominal surgery and history of cancer, obesity persisted as a significant predictor (P = .016; OR, 4.9; 95% CI, 1.3–18.1).
Table 3.
Description of Major Procedural Complications
| Type | Description |
|---|---|
| Lap | 69-y-old woman with prior hysterectomy and appendectomy underwent JT insertion; converted to open for excessive adhesions. On POD 5, abdominal pain developed with acidosis and hemodynamic instability. Exploratory laparotomy showed diffuse small-bowel ischemia of uncertain etiology. Condition rapidly worsened; patient died. |
| Lap | 42-y-old woman with prior liver transplantation and adhesions underwent JT insertion. On POD 1, CT scan performed for pain and acute anemia showed hemoperitoneum and large intraperitoneal hematoma centered on JT site requiring transfusions. Hematoma subsequently became infected and improved with antibiotic treatment. |
| Lap | 51-y-old woman with multiple prior abdominal surgeries and extensive adhesions underwent JT insertion. Resistance with injection on POD 1; patient underwent fluoroscopic tube check that showed tube tip was not intraluminal. Patient underwent repeat operation for laparoscopic JT insertion. |
| Lap | 71-y-old man with recent stroke and malnutrition. On POD 2, after laparoscopic JT insertion, septic shock of unknown source developed; patient died on POD4. Abdominal CT noted unremarkable. |
| Lap | 65-y-old man with esophageal cancer underwent JT insertion. On POD 12, patient noted to have purulence at exit site, with CT showing large abscess with gas-producing organizing adjacent to tube. After incision and drainage, patient recovered uneventfully. |
| Lap | 34-y-old woman with prior gastric bypass surgery underwent JT insertion; extensive adhesions noted. On POD 2, patient had severe abdominal pain with flushing of tube, with CT showing tip in peritoneum. Repeat operation for laparoscopic JT insertion. |
| Lap | 49-y-old man with large diaphragmatic hernia underwent attempted radiologic JT attempt aborted for failure to find suitable loop for access. Surgical insertion recommended. During laparoscopic JT insertion, adhesions encountered and iatrogenic enterotomy noted; converted to open surgery for repair. JT insertion performed. Patient exhibited septic shock on POD 2 and died on POD 5. |
| Rad | 36-y-old woman with diffusely metastatic colon cancer with peritoneal carcinomatosis and gastric outlet obstruction receiving constant opioid infusion for chronic pain underwent JT insertion. On PPD 10, patient admitted in unresponsive state with leukocytosis of uncertain etiology; died 2 d later. |
| Rad | 51-y-old man with large hiatal hernia, multiple prior bowel obstructions, and repetitive GJ tube tip migration into stomach underwent JT insertion. Patient presented at PPD 6 with obstruction of distal ileum (remote from JT site) and septic shock. Laparotomy showed frank spillage from JT site. Patient underwent bowel resection and died at PPD 10. |
| Rad | 54-y-old woman underwent ventral hernia repair 2 weeks before JT insertion. Leukocytosis developed on PPD 4. CT showed large fluid collection in dissected facial space from recent ventral hernia repair through which JT traversed. Percutaneous drainage performed with resolution. |
| Rad | 77-y-old man with metastatic GIST treated with gastrectomy underwent JT insertion. Hemodynamic instability developed on PPD 3 with deteriorating mental status. CT showed unremarkable JT in bowel but with new free peritoneal fluid and air with stranding around duodenum remote from JT site. Percutaneous drain revealed thick yellow fluid in peritoneum, suspected to be leakage of enteric contents from JT site vs perforated duodenal ulcer given CT findings. Died on PPD 5. |
| Rad | 64-y-old man with severe pancreatitis and recurrent GJ tube tip migration into stomach. During JT attempt, guide wire access to jejunum was lost during tract dilation. Procedure aborted; T-fasteners secured to skin to minimize leakage. Nausea and vomiting developed on PPD 2; CT showed jejunal obstruction at T-fastener site. Laparotomy on PPD 5. T-fasteners found traversing both walls of a loop of nontarget bowel before entering target loop. T-fasteners removed, enterotomies repaired, open jejunostomy tube inserted. Patient recovered uneventfully. |
GIST = gastrointestinal stromal tumor; JT = jejunostomy tube; Lap = laparoscopic; POD = postoperative day; PPD = postprocedure day; Rad = radiologic.
Analysis of the laparoscopic jejunostomy group demonstrated that previous major abdominal surgery and lysis of adhesions during jejunostomy tube insertion were associated with a significantly higher rate of major procedural complications (Table 4). In patients with previous major abdominal surgery, 5 of 37 (14%) had major complications, compared with 2 of 78 (3%) of those without (P = .039; OR, 5.9; 95% CI, 1.1–32.2). Patients who underwent lysis of adhesions had a 15% rate of major complications (5 of 33), compared with 2% (2 of 83) of those who did not (P = .023; OR, 7.1; 95% CI, 1.3–38.9). Multivariate analysis including previous major abdominal surgery and obesity revealed that previous major abdominal surgery persisted as a significant predictor of major complications (P = .035; OR, 6.5; 95% CI, 1.1–36.7).
Table 4.
Predictors of Major Complications Based on Patient Characteristics
| Characteristic | Overall (N = 221) | P Value | Laparoscopic (n = 115) | P Value | Radiologic (n = 106) | P Value |
|---|---|---|---|---|---|---|
| No. of major complications | 12/221 (5) | – | 7/115 (6) | – | 5/106 (5) | – |
| Male sex | 6/125 (5) | .64 | 3/61 (5) | .58 | 3/64 (5) | .99 |
| Mean age (y) | 55.9 | .28 | 54.6 | .33 | 57.8 | .63 |
| Mean BMI (kg/m2) | 24.2 | .96 | 23.5 | .83 | 25.1 | .163 |
| Obesity | 5/29 (17) | .006 | 3/19 (16) | .07 | 2/10 (20) | .038 |
| Prior major abdominal surgery | 9/112 (8) | .01 | 5/37 (14) | .039 | 4/75 (5) | .65 |
| Cancer | 4/133 (3) | .06 | 3/74 (4) | .23 | 1/59 (2) | .14 |
| Lung transplant | 0/14 | 1.0 | 0/4 | 1.0 | 0/10 | 1.0 |
| Diabetes mellitus | 1/30 (3) | .59 | 1/13 (8) | .80 | 0/17 | 1.0 |
| Ascites | 1/11 (9) | .59 | 0/5 | 1.0 | 1/6 (17) | .19 |
| Critical illness | 1/32 (3) | .54 | 0/1 | 1.0 | 1/31 (3) | .65 |
| Lysis of adhesions | – | – | 5/33 (15) | .023 | – | – |
Note-For listed ratios (percentages), the denominator is the number of patients with the characteristic of interest and the numerator is the number of patients with a major complication who had the characteristic of interest. P values describe the preceding column based on univariate binomial logistic regression analysis.
BMI = body mass index.
Analysis of the radiologic jejunostomy tube group demonstrated only obesity to be predictive of major complications (2 of 10 [20%] in obese patients vs 3 of 96 [3%] in nonobese patients; P =.038; OR, 7.8; 95% CI, 1.1–53.4). There was no association between previous major surgery and major complications: 4 of 75 (5%) in the radiologic jejunostomy group versus 1 of 31 (3%; P = .65) in the laparoscopic jejunostomy group. No other variables met the criteria for inclusion in a multivariate analysis.
DISCUSSION
For patients who need long-term enteral nutrition, laparoscopic and radiologic techniques for jejunostomy tube insertion have demonstrated high technical success rates and low rates of major complications. Previous abdominal surgeries were associated with challenges for laparoscopic jejunostomy tube insertion, including a significantly higher need for lysis of adhesions and a higher major complication rate, whereas no correlation was found with radiologic jejunostomy tube insertion. Obesity was a significant risk factor for radiologic jejunostomy tube insertion but not for laparoscopic insertion. These findings suggest that previous major abdominal surgery and obesity may serve as discriminators in the choice of the optimal technique.
The high success rate for radiologic tube insertion in the present study is similar to those reported in the literature. Multiple studies of percutaneous radiologic jejunostomy tube insertion in sample sizes of 14–51 patients (4–10) report technical success rates ranging from 87% to 100%. Mortality rates resulting from radiologic jejunostomy tube placement have been reported at 0%–5%, which are similar to that found in the present study, despite 29% of patients undergoing radiologic jejunostomy tube placement in the present study being categorized as critically ill, compared with only 1% in the laparoscopic insertion group. Although critically ill intensive-care patients are typically considered at high risk for general anesthesia and surgery, this factor did not correlate with major complications in the radiologic placement group in the present study.
The high technical success rate for laparoscopic jejunostomy tube insertion in the present study was also similar to the 88%–100% range reported in the literature (4–6,16,17). In the present study and others, the primary reason for technical failure was conversion to open surgery as a result of excessive intraabdominal adhesions, with previous abdominal surgery correlating with a significantly higher rate of lysis of adhesions and major complications in the present study. Lysis of adhesions has been reported to be a factor not only for a high conversion rate from laparoscopic to open insertion, but also unintentional enterotomies (16). Accordingly, studies with no technical failures may be related to exclusion of patients in whom severe adhesions were expected (18). In a systematic review of laparoscopic jejunostomy tube insertions (5), the overall complication rate was 17%, with 1.8% requiring repeat laparotomy. The severity of complications was not delineated in that study (5).
Although previous major abdominal surgery was found to be associated with a higher major complication rate for laparoscopic jejunostomy tube insertion in the present study and others (16), there was no association found in the percutaneous radiologic jejunostomy tube insertion cohort. The presence of intraabdominal adhesions may be a potential explanation for this observation. One of the primary challenges for percutaneous radiologic insertion is jejunal loop mobility, which causes needle access of the target loop to be technically difficult (1). Bowel adhesions, however, may serve to decrease bowel loop mobility and thereby enable more reliable needle access.
Obesity, which has been shown to be a general risk factor for surgical complications (19), was a significant risk factor for major complications in the overall cohort and in the radiologic jejunostomy tube group, but not in the laparoscopic group. Although the reason or this difference is uncertain, it is possible that pannus mobility may exert more stress and cause more movement at the single-site T-fastener jejunopexy, which is theoretically less secure than the circumferential jejunopexy achieved laparoscopically.
There are several limitations to the present study. Given its retrospective nature, there was selection bias, as evidenced by several factors with significantly different distributions, including a significantly lower proportion of patients in the laparoscopic group with previous major abdominal surgery, which is known to be a risk factor for technically challenging laparoscopic jejunostomy tube insertion (16). Conversely, adhesions may be beneficial for percutaneous radiologic insertion. Therefore, if the groups were equivalently represented, there could theoretically be higher complication rates in both groups. Another limitation of the study is the relatively high level of experience with percutaneous radiologic jejunostomy tubes in the authors’ institution, meaning the results may not be generalizable to other operators. However, the success and complication rates in the present study are similar to those in existing literature. Finally, the low number of complications and modest number of patients in this study limit robust analysis of factors associated with complications.
In conclusion, the present study found that laparoscopic and percutaneous radiologic insertion of jejunostomy tubes both have a high technical success rate and acceptable complication rates. Although the 2 groups had different population characteristics, the finding of different risk factors for major procedural complications suggests that certain patients may be better suited for one or the other modality. Therefore, a randomized controlled trial to determine which modality is superior for “all-comer” patients may not be helpful. The present data suggest that patients expected to have extensive intraabdominal adhesions may be better served with percutaneous radiologic jejunostomy tube insertion. Conversely, patients without previous abdominal surgery, particularly those who are obese, may be better suited for laparoscopic jejunostomy tube insertion. Therefore, availability of both methods for jejunostomy tube insertion may be ideal for achieving optimal outcomes for patients in need of long-term enteral feeding.
EDITORS’ RESEARCH HIGHLIGHTS.
This large single-center retrospective study compares outcomes of laparoscopic versus radiologic placement of jejunostomy tubes in 211 patients. Rates of technical success (95% and 97%) and major complications (6% and 5%) were similar for laparoscopic and radiologic placement, respectively.
Previous major abdominal surgery was a risk factor for major complications in the laparoscopic insertion group, whereas obesity was associated with major complications in the radiologic insertion group.
Interventional radiologic approaches are valid primary approaches to routine jejunostomy tube placement. Obesity or previous major abdominal surgery may further guide patient allocation for laparoscopic versus radiologic jejunostomy tube placement.
ABBREVIATIONS
- CI
confidence interval
- OR
odds ratio
Footnotes
None of the authors have identified a conflict of interest.
REFERENCES
- 1.Itkin M, DeLegge MH, Fang JC, et al. ; Society of Interventional Radiology, American Gastroenterological Association, American Gastroenterological Association Institute, Canadian Interventional Radiological Association, Cardiovascular, Interventional Radiological Society of Europe. Multidisciplinary practical guidelines for gastrointestinal access for enteral nutrition and decompression from the Society of Interventional Radiology and American Gastroenterological Association (AGA) Institute, with endorsement by Canadian Interventional Radiological Association (CIRA) and Cardiovascular and Interventional Radiological Society of Europe (CIRSE). J Vasc Interv Radiol 2011; 22:1089–1106. [DOI] [PubMed] [Google Scholar]
- 2.Heyland DK, Drover JW, MacDonald S, Novak F, Lam M. Effect of postpyloric feeding on gastroesophageal regurgitation and pulmonary microaspiration: results of a randomized controlled trial. Crit Care Med 2001; 29:1495–1501. [DOI] [PubMed] [Google Scholar]
- 3.Jabbar A, McClave SA. Pre-pyloric versus post-pyloric feeding. Clin Nutr 2005; 24:719–726. [DOI] [PubMed] [Google Scholar]
- 4.Young MT, Troung H, Gebhart A, Shih A, Nguyen NT. Outcomes of laparoscopic feeding jejunostomy tube placement in 299 patients. Surg Endosc 2016; 30:126–131. [DOI] [PubMed] [Google Scholar]
- 5.Han-Geurts IJ, Lim A, Stijnen T, Bonjer HJ. Laparoscopic feeding jejunostomy: a systematic review. Surg Endosc 2005; 19:951–957. [DOI] [PubMed] [Google Scholar]
- 6.Senkal M, Koch J, Hummel T, Zumtobel V. Laparoscopic needle catheter jejunostomy: modification of the technique and outcome results. Surg Endosc 2004; 18:307–309. [DOI] [PubMed] [Google Scholar]
- 7.Hu HT, Shin JH, Song HY, et al. Fluoroscopically guided percutaneous jejunostomy with use of a 21-gauge needle: a prospective study in 51 patients. J Vasc Interv Radiol 2009; 20:1583–1587. [DOI] [PubMed] [Google Scholar]
- 8.Kim CY, Engstrom BI, Horvath JJ, Lungren MP, Suhocki PV, Smith TP. Comparison of primary jejunostomy tubes versus gastrojejunostomy tubes for percutaneous enteral nutrition. J Vasc Interv Radiol 2013; 24:1845–1852. [DOI] [PubMed] [Google Scholar]
- 9.Yang ZQ, Shin JH, Song HY, et al. Fluoroscopically guided percutaneous jejunostomy: outcomes in 25 consecutive patients. Clin Radiol 2007; 62: 1061–1065. [DOI] [PubMed] [Google Scholar]
- 10.Richard HM, Widlus DM, Malloy PC. Percutaneous fluoroscopically guided jejunostomy placement. J Trauma 2008; 65:1072–1077. [DOI] [PubMed] [Google Scholar]
- 11.Sparrow P, David E, Pugash R. Direct percutaneous jejunostomy–an underutilized interventional technique? Cardiovasc Intervent Radiol 2008; 31:336–341. [DOI] [PubMed] [Google Scholar]
- 12.van Overhagen H, Ludviksson MA, Lameris JS, et al. US and fluoroscopic-guided percutaneous jejunostomy: experience in 49 patients. J Vasc Interv Radiol 2000; 11:101–106. [DOI] [PubMed] [Google Scholar]
- 13.Evans AL, Uberoi R. CT-guided jejunostomy tube insertion. AJR Am J Roentgenol 2005; 185:1369. [DOI] [PubMed] [Google Scholar]
- 14.Rosenberger LH, Politano AD, Sawyer RG. The surgical care improvement project and prevention of post-operative infection, including surgical site infection. Surg Infect (Larchmt) 2011; 12:163–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sacks D, McClenny TE, Cardella JF, Lewis CA. Society of Interventional Radiology clinical practice guidelines. J Vasc Interv Radiol 2003; 14(suppl): S199–S202. [DOI] [PubMed] [Google Scholar]
- 16.Hotokezaka M, Adams RB, Miller AD, McCallum RW, Schirmer BD. Laparoscopic percutaneous jejunostomy for long term enteral access. Surg Endosc 1996; 10:1008–1011. [DOI] [PubMed] [Google Scholar]
- 17.Speer EA, Chow SC, Dunst CM, et al. Clinical burden of laparoscopic feeding jejunostomy tubes. J Gastrointest Surg 2016; 20:970–975. [DOI] [PubMed] [Google Scholar]
- 18.Duh QY, Senokozlieff-Englehart AL, Siperstein AE, et al. Prospective evaluation of the safety and efficacy of laparoscopic jejunostomy. West J Med 1995; 162:117–122. [PMC free article] [PubMed] [Google Scholar]
- 19.Bamgbade OA, Rutter TW, Nafiu OO, Dorje P. Postoperative complications in obese and nonobese patients. World J Surg 2007; 31:556–560. [DOI] [PubMed] [Google Scholar]