Abstract
Background and aims:
Lung cancer patients suffer from deterioration in their physical and psychological function, which exerts a negative influence on their quality of life (QOL). Telemedicine has been proven to be an effective intervention for patients with several chronic diseases. The aim of this systematic review and meta-analysis was to investigate the efficacy of telemedicine in improving QOL in lung cancer patients.
Methods:
PubMed, Cochrane Library, EMBASE, Web of Science and Scopus databases were searched for randomized controlled trials that investigated the effectiveness of telemedicine in lung cancer patients. Review Manager 5.3 and Stata 15.1 were used to perform data analysis.
Results:
Our meta-analysis included eight clinical trials with a total of 635 lung cancer patients. The results showed that the telemedicine group had significantly higher QOL than the usual care group [standard mean difference (SMD) 0.96, 95% confidence interval (CI) 0.29–1.63, I2 = 91%]. In addition, the telemedicine group had lower anxiety (SMD −0.44, 95% CI −0.66 to −0.23, I2 = 3%) and depression scores (SMD −0.48, 95% CI −0.91 to −0.05, I2 = 66%) than the usual care group. However, no significant differences were found in fatigue and pain outcomes between the two groups.
Conclusion:
Telemedicine may be an effective method of improving QOL in lung cancer patients and the further development and use of telemedicine care is recommended.
Keywords: lung cancer, quality of life, symptom burden, telemedicine
Introduction
Lung cancer is one of the most common types of cancers and the leading cause of death from malignancy. At least 2.09 million people were newly diagnosed with lung cancer and the number of cancer-related deaths had reached up to 1.76 million in 2018 worldwide.1,2 The characteristics of tumour cells and certain cancer-related treatments are such that patients with lung cancer endure a high burden of symptoms such as fatigue and anxiety.3,4 As a result, preserving the quality of life (QOL) of patients as they decline has become an urgent concern.5–7
Telemedicine was defined by the World Health Organization (WHO) in 1997 as the delivery of health care services by information and communication technologies (ICTs) at a distance.8 Recommended as a type of safe, cost-effective and time-saving intervention, it has emerged in the last two decades as a non-invasive surveillance and follow-up method for patients discharged from hospital.9,10 ICTs such as websites, telephone and telemedicine systems have been established to detect and manage patients’ physical and psychological changes in a timely manner, improve communication between health care providers and patients or their families and allow patients to effectively self-manage.11,12 In addition, the value of telemedicine in chronic disease management has been confirmed in meta-analyses examining its use in conditions such as heart failure, chronic obstructive pulmonary disease and asthma.13–15 Telemedicine has been proven to have played an important role in dermatology during the 2019 novel coronavirus disease (COVID-19) pandemic.16
Few reviews have explored the effectiveness of telehealth in the management of malignant tumours, especially in improving QOL. In the past few years, several clinical trials have been conducted to examine the effectiveness of telemedicine in increasing the QOL of lung cancer patients, and mobile applications have even been developed to monitor their disease status.17–21 On the one hand, patients diagnosed with lung cancer demand an effective intervention to enable them to manage problems under their own initiative on a long-term basis in the follow-up period after initial treatment. On the other hand, interaction between health care providers and lung cancer patients has been a target for improving patients’ QOL.22 Telemedicine is acknowledged as a promising method for improving QOL by virtue of its unique advantages, and the results of several clinical trials have provided strong evidence for this view.23,24 However, due to high heterogeneity among these studies, the exact effect of telemedicine on the QOL of patients with lung cancer remains unknown. Thus, we conducted this meta-analysis to examine the superiority of telemedicine in lung cancer patients.
Methods
Search strategy
Two investigators (LP and ZL) independently searched for articles in the databases PubMed, Cochrane library, EMBASE, Web of Science and Scopus. Medical Subject Headings (MeSH) and free search terms were both used in the literature search. The search terms included telemedicine, telemonitor, e-health, telehealth, telecommunication, telemanagement, telecare, telephone monitoring, telepathology, remote and short message service, mobile health, telerehabilitation, lung neoplasm, lung neoplasms, lung carcinoma, lung cancer and lung tumour. The search strategy used for PubMed was as follows: (telemedicine OR telemonitor OR e-health OR telehealth OR telecommunication OR telemanagement OR telecare OR telephone monitoring OR telepathology OR remote and short message service OR mobile health OR telerehabilitation) AND (lung neoplasm OR lung neoplasms OR lung carcinoma OR lung cancer OR lung tumour). The final search date was 14 February 2020. In addition, we manually searched the references of the screened articles for further high-quality studies.
Study selection
Two investigators (LP and HL) independently skimmed the identified abstracts and selected articles to fully review. The same two investigators independently undertook full text review (including intensively reading appropriate articles after skimming the references of screened articles). A senior investigator (CC) adjudicated when eligibility could not be agreed.
Inclusion criteria were as follows: (1) patients diagnosed with lung cancer; (2) telemedicine intervention, defined as “the use of telecommunication systems to deliver health care at a distance”; (3) usual care referred to the usual oncology care; (4) reported outcomes including at least one of the following: QOL, anxiety, depression, fatigue or pain; (5) experimental studies, including randomized controlled trials (RCTs) and quasi-RCTs.
The following were excluded: (1) letters or reviews; (2) laboratory studies, case reports or animal experimental studies; (3) studies not published in English language; (4) studies with an absence of key information such as sample size.
Data extraction and outcome definitions
Two investigators (LP and HL) independently extracted data and any disagreements were discussed with the third investigator (ZL) or subsequently resolved via consensus. Extracted data included first author, publication year and country, number of participants and their characteristics (age, sex and disease status), interventions (technology, intervention providers), follow-up time and outcomes. If the necessary data could not be found in the published paper, investigators obtained them by emailing the original authors.
QOL was set as our primary outcome, with anxiety, depression score, fatigue and pain as secondary outcomes.
Risk of bias assessment
Two investigators (LP and HL) independently undertook a risk of bias assessment and any doubts were resolved by the third investigator (ZL).
We evaluated risk of bias of trials according to the Cochrane handbook of systematic reviews of interventions (http://handbook.cochrane.org). In addition, we applied the revised Jadad’s scale to assess the quality of each study.
Statistical analysis
Review Manager 5.3 (Cochrane) and Stata 15.1 were used for statistical analysis. For continuous variables such as QOL, we calculated standardized mean difference (SMD) with 95% confidence interval (CI). For discrete variables, we calculated odds ratio with 95% CI. Heterogeneity was evaluated using the Cochrane Q-statistic and I2 statistic. If the I2 statistic was above 50% and the Cochrane Q-statistic had a p value ⩽ 0.1, a random-effects model was used. However, if no considerable heterogeneity among studies was apparent, a fixed-effect model would be used. Subgroup analysis was conducted to explore high heterogeneity and pre-defined stratification including the follow-up time, type of QOL scale and technologies used. Funnel plots and Egger test were used to assess potential publication bias.
Results
Search process, study characteristics and quality assessment
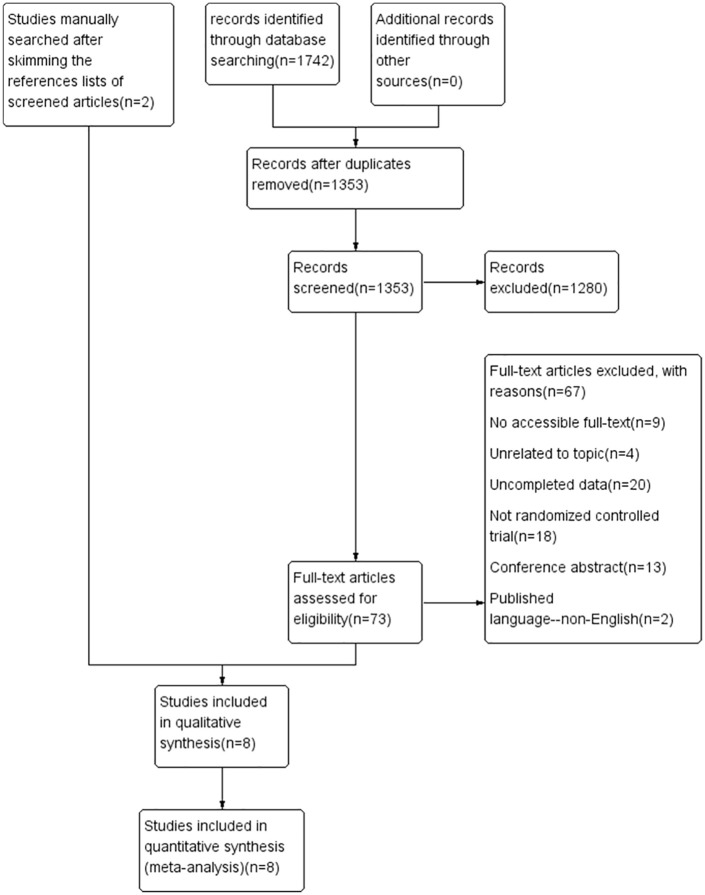
Based on the search criteria, we found 1742 articles. Of these, 1353 articles remained after removing duplications. We selected 73 of the articles for full consideration after reading the title and abstract. In addition, we manually searched two studies for intensive reading after skimming the references lists of the 73 articles. Finally, eight studies with a total of 635 patients were enrolled to our meta-analysis, all of which were experimental studies (six RCTs and two quasi-RCTs) published between 2014 and 2019.23–30 The process of selecting the included studies is presented in Figure 1.
Figure 1.
Flow diagram of the selection of the included studies.
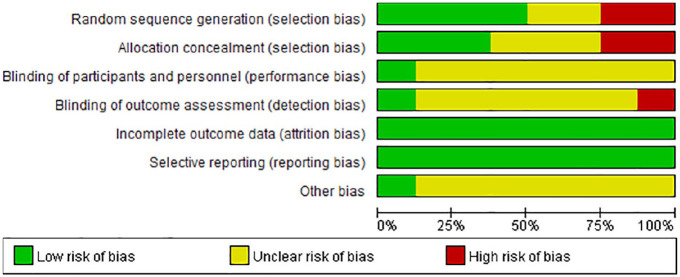
Table 1 shows the basic characteristics of the enrolled articles and the essential information of the participants. The studies were conducted in United States,23,26,27 China,28,30 United Kingdom,29 France24 and Turkey.25 Six23,25–27,29,30 of them had adopted a telephone-based intervention while the remaining studies were Web-based. Follow-up duration ranged from 3 weeks to 8 months. Scales to measure QOL included the WHO-QOL score and the Functional Living Index − Cancer, among others. Revised Jadad’s scale scores of the included studies are also presented in Table 1, and indicate that the studies were of high quality except for two. Figures 2 and 3 demonstrate the methodological quality of the included studies. In the domain of incomplete outcome data and selective reporting, all the included studies were judged as having low risk of bias. However, two studies (quasi-RCTs)23,25 failed to meet the criteria of random sequence generation and allocation concealment. Whether blinding was carried out was unclear in most of the studies.
Table 1.
Characteristics of the included studies and participants.
| First author | Country | Age* (years) | Patients, number* | Jadad’s score | Patients’ characteristics | Intervention* | Contact | Technology | Follow-up | Outcomes and outcome measures |
|---|---|---|---|---|---|---|---|---|---|---|
| Badr27 | United States | 68.17 ± 10.30 (average of all patients) | 20 versus 19 | 1+1+1+1 = 4 | Advanced LC patients who were within 1 month of treatment initiation | Telephone-based dyadic psychosocial intervention versus usual care | Mental health interventionist | Telephone | 6 weeks | Depression, anxiety (the six-item PROMIS short-form depression and anxiety measure) |
| Chang30 | Taiwan, China | 62.00 ± 12.15 versus 58.39 ± 13.39 | 32 versus 33 | 1+1+1+1 = 4 | LC patients recovering from lung lobectomy | Usual care plus once-daily additional brisk walking exercise and weekly telephone calls through week 12 versus usual care | Researcher | Telephone | 6 months | QOL [WHO QOL-BREF (Taiwanese)] |
| Chen23 | United States | 63 ± 8.9 versus 63 ± 11.3 | 26 versus 21 | 0+0+1+1 = 2 | LC patients in Appalachia | Wireless home-telemonitoring system, patient-centred phone coaching in addition to usual post-discharge care versus usual post-discharge care | Nurse | Telephone | 2 months | QOL (WHO-5) |
| Denis24 | France | 65.2 (35.7–86.9) versus 64.3 (42.7–88.1) | 60 versus 61 | 2+2+1+1 = 6 | Advanced-stage LC patients | A Web-mediated follow-up algorithm (experimental arm) based on weekly self-scored patient symptoms versus routine follow-up with computerized tomography scan (usual care) | Oncologist | Website | 6 months | Quality of life (FACT-L scores) |
| Hintistan25 | Turkey | ⩽49 years 8 versus 7 50–59 years 15 versus 8 ⩾60 years 7 versus 15 |
30 versus 30 | 0+0+1+1 = 2 | LC patients in the Ambulatory Chemotherapy Unit | The standard care plus follow-up call within a week after each chemotherapy session versus standard care | Nurse | Telephone | 3 weeks | QOL (FLIC) |
| Huang 28 | Taiwan, China | 61.00 ± 2.04 versus 58.68 ± 1.77 | 27 versus 28 | 2+1+1+1 = 5 | Patients receiving chemotherapy during the first 3 months after initial diagnosis of advanced NSCLC | A Web-based health education programme allowing patients to learn symptom management strategies biweekly versus usual care | Nurse | Website | 3 months | QOL (EORTC C30) |
| Mosher26 | United States | 63.47 ± 7.68 versus 61.96 ± 8.20 | 51 versus 55 | 2+2+2+1 = 7 | Symptomatic LC patients | Telephone-based symptom management consisting of cognitive–behavioural and emotion-focused therapy versus education/support condition (usual care) | Licensed clinical social workers | Telephone | 6 weeks | Depression, anxiety, fatigue (The Patient Health Questionnaire-8, GAD-7, Fatigue Symptom Inventory) |
| Walker29 | United Kingdom | 63.6 ± 8.8 versus 63.9 ± 8.7 | 68 versus 74 | 2+2+2+1 = 7 | Patients with LC and major depression | Depression care including telephone monitoring care versus usual care | Nurse, psychiatrist | Telephone | 8 months | QOL (EORTC-QLQ-C30), depression (SCL-20), anxiety (SCL-10) |
These items were recorded as experimental versus control group.
EORTC, European Organization for Research and Treatment of Cancer; FLIC, Functional Living Index-Cancer; GAD-7, Generalized Anxiety Disorder seven-item; LC, lung cancer; NSCLC, non-small cell lung cancer; PROMIS, Patient Reported Outcomes Measurement Information System; QOL, quality of life; SCL, Symptom Checklist; WHO, World Health Organization; WHO QOL-BREF, World Health Organization Quality of Life Questionnaire, brief version; FACT-L, Functional Assessmet of Cancer Therapy-lung.
Figure 2.
Risk of bias graph.
Figure 3.
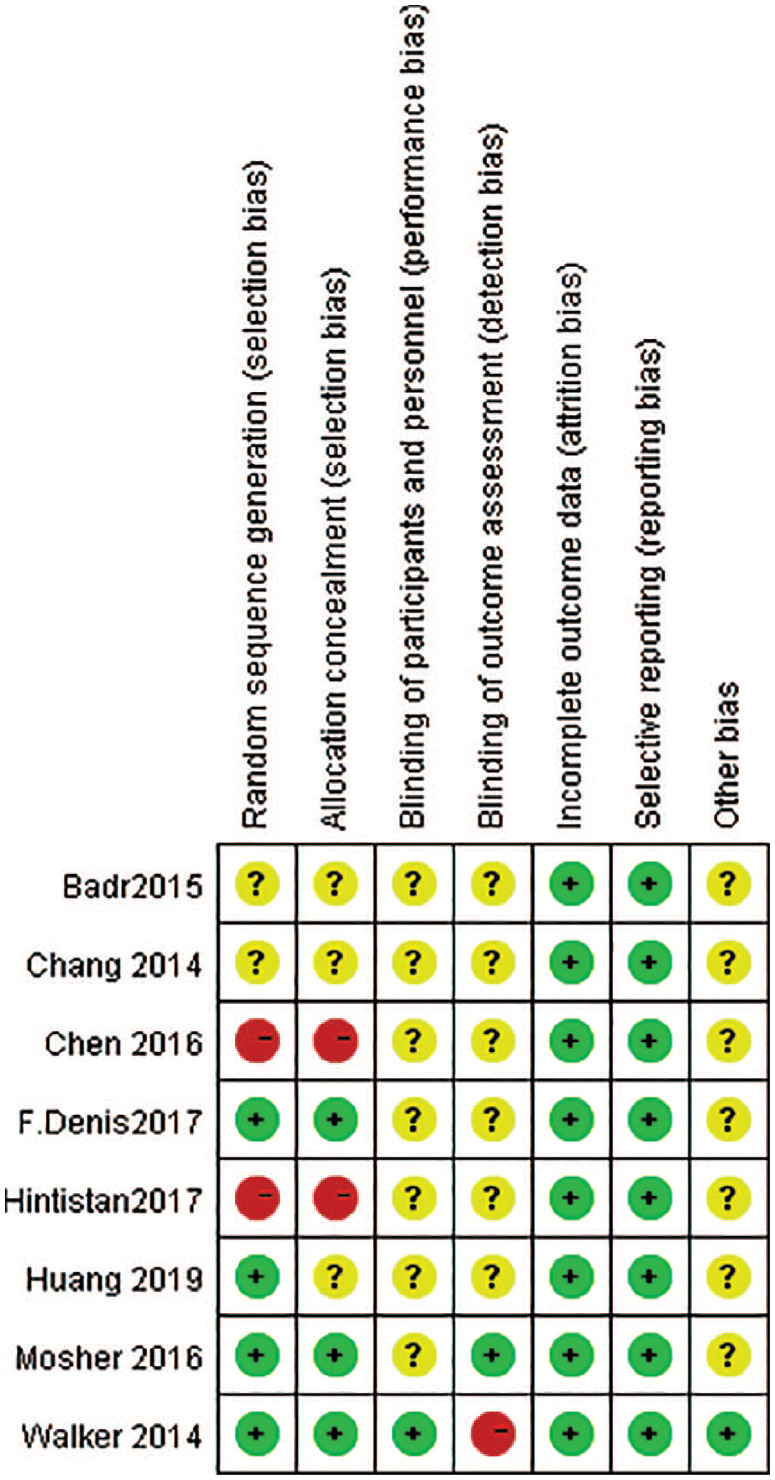
Risk of bias summary.
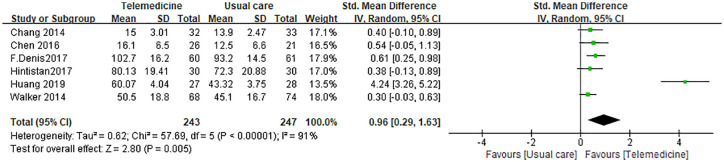
Quality of life
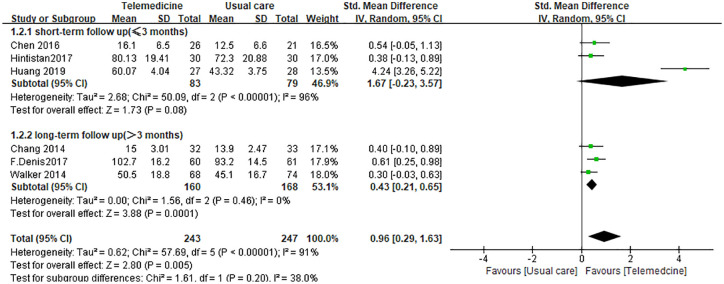
To compare telemedicine with usual care in the improvement of QOL, we enrolled data from six of the studies23–25,28–30 with a total of 490 patients. The results demonstrated that the telemedicine group reported a significantly higher QOL than the usual care group (SMD 0.96, 95% CI 0.29–1.63). Heterogeneity testing showed that I2 = 91%, indicating high heterogeneity (Figure 4). To address high heterogeneity, we conducted a subgroup analysis grouped by follow-up time (>3 months or not), type of scale (WHO-QOL or not) and type of technology (telephone-based or Web-based).
Figure 4.
Analysis comparing telemedicine versus usual care for quality of life in lung cancer patients.
CI, confidence interval; IV, inverse variance; Std., standardized
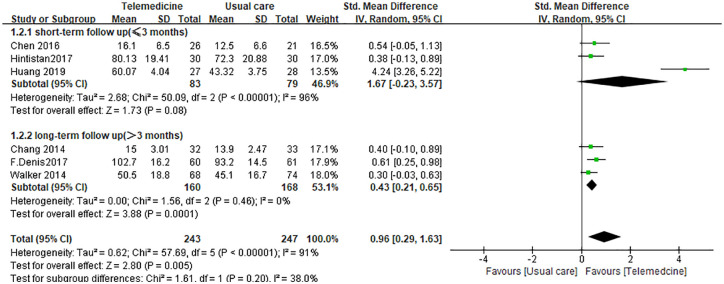
The subgroup analysis for follow-up time showed that the telemedicine group had significantly higher QOL than the usual care group for long-term follow-up (SMD 0.43, 95% CI 0.21–0.65, I2 = 0%), whereas no significant difference was observed in short-term follow-up (SMD 1.67, 95%CI −0.23 to 3.57, I2 = 96%; Figure 5).
Figure 5.
Subgroup analysis of quality of life comparing telemedicine with usual care grouped by follow-up time.
CI, confidence interval; IV, inverse variance; Std., standardized
In the subgroup analysis for type of scale, the telemedicine group had significantly higher QOL than the usual care group both in the WHO-QOL group (SMD 0.46, 95% CI 0.08–0.83, I2 = 0%) and the other types of QOL scale subgroup (SMD 1.26, 95% CI 0.25–2.28, I2 = 95%; Figure 6).
Figure 6.
Subgroup analysis of quality of life comparing telemedicine with usual care grouped by type of scale.
CI, confidence interval; IV, inverse variance; Std., standardized
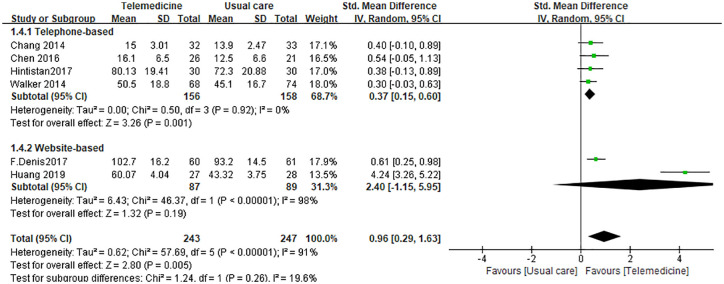
In the subgroup analysis stratified by type of technology, the telemedicine group had significantly higher QOL than the usual care group for telephone-based intervention (SMD 0.37, 95% CI 0.15–0.60, I2 = 0%). However, differences between the Web-based and usual care groups were not significant (SMD 2.40, 95%CI −1.15 to 5.95, I2 = 98%; Figure 7).
Figure 7.
Subgroup analysis of quality of life comparing telemedicine with usual care grouped by type of technology.
CI, confidence interval; IV, inverse variance; Std., standardized
The funnel plot shown in Figure 8 indicates potential publication bias. However, no significant potential publication bias was found using the Egger test (p = 0.072). This inconsistency may be due to the small number of enrolled studies.
Figure 8.
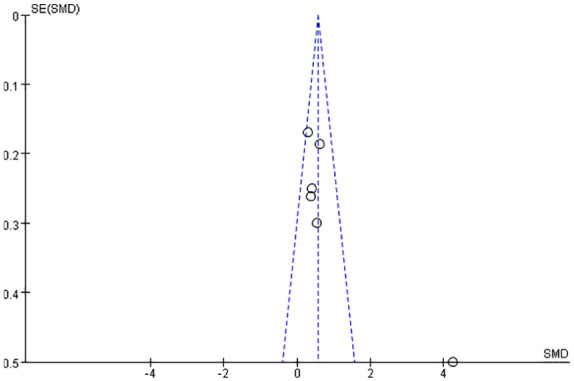
Funnel plot showing publication bias.
SE, standard error, SMD, standardized mean difference
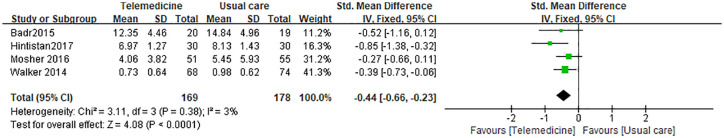
Anxiety
To investigate the efficacy of telemedicine in alleviating anxiety compared with usual care, we included four articles25–27,29 with 347 patients. Anxiety scores in the telemedicine group were lower than in the usual care group (SMD −0.44, 95% CI −0.66 to −0.23). Heterogeneity testing showed that I2 = 3%, indicating low heterogeneity (Figure 9).
Figure 9.
Analysis comparing telemedicine with usual care for managing anxiety in lung cancer patients.
CI, confidence interval; IV, inverse variance; Std., standardized
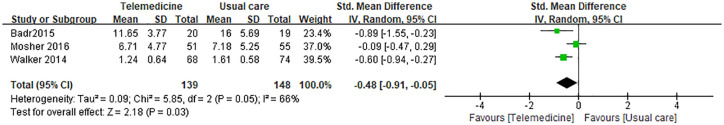
Depression
Our study enrolled three studies26,27,29 with a total of 287 patients to examine the superiority of telemedicine in easing depression in lung cancer patients. As shown in Figure 9, depression scores were lower in the telemedicine group than in the usual care group (SMD −0.48, 95% CI −0.91 to −0.05). Heterogeneity testing showed that I2 = 66%, indicating high heterogeneity (Figure 10).
Figure 10.
Analysis comparing telemedicine with usual care for managing depression in lung cancer patients.
CI, confidence interval; IV, inverse variance; Std., standardized
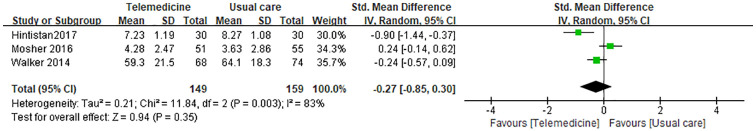
Fatigue
To comparing telemedicine and usual care in relieving fatigue in lung cancer patients, we enrolled three studies25,26,29 with a total of 308 patients. The results indicated no significant difference between telemedicine and usual care group in fatigue (SMD −0.27, 95% CI −0.85 to 0.30). Heterogeneity testing showed that I2 = 83%, indicating high heterogeneity (Figure 11).
Figure 11.
Analysis comparing telemedicine with usual care for managing fatigue in lung cancer patients.
CI, confidence interval; IV, inverse variance; Std., standardized
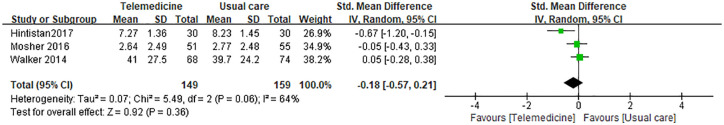
Pain
To examine whether telemedicine could alleviate pain in lung cancer patients compared with usual care, we included three studies25,26,29 with a total of 308 patients. These two groups did not have significantly different pain outcomes (SMD −0.18, 95% CI −0.57 to 0.21). Heterogeneity testing showed that I2 = 64%, indicating high heterogeneity (Figure 12).
Figure 12.
Analysis comparing telemedicine with usual care for managing pain in lung cancer patients.
CI, confidence interval; IV, inverse variance; Std., standardized
Discussion
With the further development of cancer treatment, clinic staff are increasingly focused on not only patients’ lifespan but also their QOL. It is acknowledged that patients with lung cancer experience a greater symptom burden than patients with any other type of cancer.4,7 Previous studies have reported that lung cancer patients have severe symptoms, including anxiety, depression, pain and fatigue.3,7 Moreover, these symptoms have been confirmed to exert a negative influence on their QOL.31 Several studies have investigated the excellent capability of non-invasive intervention to improve their QOL and alleviate their psychological burden.32–34 A meta-analysis conducted by Chen et al.35 demonstrated that telehealth care had advantages over usual care in improving QOL in breast cancer patients, proving the positive effects of e-health technologies in the management of malignancy.
Our study explored the effectiveness of telemedicine on the management of patients with lung cancer. We showed that a telemedicine group had a significantly better QOL than a usual care group. Subgroup analysis stratified by type of technology indicated that QOL in the telemedicine group was significantly better than that of the usual care group when telephone-based intervention was used. Moreover, the telemedicine group had a significantly better QOL than the usual care group during long-term follow-up. The telemedicine group also had lower anxiety and depression scores than the usual care group.
One reason for these results about QOL is the unique superiority of telemedicine in overcoming the obstacle of distance between patients and clinic staff. Follow-up time was also subjected to subgroup analysis, with the results suggesting that telemedicine might be more effective than usual care in the long-term management of patients. This implies that the advantages of telehealth intervention over usual care need a relatively long time to be observed. Compared with website-based technology, lung cancer patients were more likely to benefit from telephone-based interventions. As the lung cancer patient population is mostly elderly, the assumption is that they may be more familiar with telephone technology than with the internet.
Lung cancer patients who undergo surgery spend a lot of time recovering from trauma and with deteriorated pulmonary function.36 Patients unfit for surgery may experience considerable discomfort and distress during chemotherapy or radiotherapy.37,38 Instant and ongoing feedback from their physicians about their suffering may provide them with significant comfort and support. Consequently, e-health web systems and applications have been devised to ensure that clinic staff and patients can contact each other conveniently, potentially contributing to improving patients’ QOL.18,19 Nevertheless, one RCT has reported that symptom telemonitoring combined with active feedback from patients was not superior to the relatively passive method of symptom telemonitoring only in maintaining the well-being of lung cancer patients.39 This suggests further investigation and more research are necessary.
In terms of symptom burden, anxiety and depression scales scores were lower in the telemedicine group than those in the usual care group. However, there were no significant differences in fatigue and pain outcomes between the two groups. Khue et al.40 has demonstrated that depression and anxiety pose risks to the QOL of lung cancer patients, which is consistent with our findings. However, a telehealth-based pulmonary rehabilitation intervention for advanced lung cancer patients was reported to be capable of alleviating fatigue, depression and anxiety, which was not completely concordant with our results.20 In addition, an enrolled study conducted by Hintistan et al.25 did not report the scales used for the assessment of pain and other symptoms.
The use of telemedicine to improve the QOL of lung cancer patients is relatively new and the publication year of all our enrolled studies was 2014 or later. Chang et al.30 conducted an RCT in 2014 on an early postoperative walking exercise programme in which the intervention was incorporated with a weekly telephone call. Since this, a number of telehealth systems designed to maintain QOL in lung cancer patients have emerged with technologies not limited to telephone but also including websites. Therefore, more high-quality RCTs are encouraged to explore the promising value of telemedicine in the maintenance of QOL in patients with lung cancer.
Our study had some limitations. First, the number of enrolled articles and participants was small, with recent clinical studies still underway. However, this study was, to our knowledge, the first meta-analysis to investigate the efficacy of telehealth care in lung cancer patients. Second, two of the enrolled studies were quasi-RCTs that did not implement random sequence generation, impairing the quality of this meta-analysis. Moreover, interventions in the telemedicine group were not limited to only telephone or internet, but also incorporated other types of non-invasive interventions, such as exercise programmes and depression care. Finally, the form of interventions varied considerably among studies in terms of follow-up time, technology medium and the intervention providers with whom patients were in contact, leading to the high heterogeneity of the enrolled studies.
Conclusion
Overall, telemedicine has an advantage in improving the QOL and psychological outcomes (including reported anxiety and depression) in patients with lung cancer. Telemedicine may be an effective intervention in managing the well-being of lung cancer patients. We suggest that more resources are put into the development of telehealth care and more high-quality RCTs are conducted to explore the value of telemedicine in the management of lung cancer patients.
Acknowledgments
We acknowledge all the contributed authors. We also acknowledge Dr Fabrice Denis and Dr Yea-Jyh Chen for their kindness to provide the necessary data in their studies.
Footnotes
Author contributions: QZ, CC designed the study. LP designed the search strategy. LP and ZL performed the search. LP and HL performed the abstract screening, full text screening, data extraction, and risk of bias assessment. ZL, SL, ZL helped in the revision process. All the authors drafted and revised the manuscript.
Availability of data and materials: The datasets used in this study are available from the corresponding author upon request. All data generated or analysed in this study are included in the published articles or obtained from the authors who published the enrolled articles.
Conflict of interest statement: The authors declare that there is no conflict of interest.
Consent for publication: All the contributed authors have agreed to the publication of this manuscript.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iDs: Lanlan Pang  https://orcid.org/0000-0002-4932-8117
https://orcid.org/0000-0002-4932-8117
Chongxiang Chen  https://orcid.org/0000-0002-2079-881X
https://orcid.org/0000-0002-2079-881X
Contributor Information
Lanlan Pang, Department of Intensive Care Unit, Sun Yat-sen University Cancer Centre, State Key Laboratory of Oncology in South China, Collaborative Innovation Centre for Cancer Medicine, Guangzhou, China; Zhongshan School of Medicine, Sun Yat-sen University, Guangzhou, Guangdong Province, China.
Zefu Liu, Department of Urology, Sun Yat-sen University Cancer Centre, State Key Laboratory of Oncology in South China, Collaborative Innovation Centre for Cancer Medicine, Guangzhou, China.
Sheng Lin, Department of pulmonary and critical care medicine, Shengli Clinical Medical College of Fujian Medical University, Fujian Provincial Hospital, Fuzhou, Fujian, China.
Zhidong Liu, Zhongshan School of Medicine, Sun Yat-sen University, Guangzhou, Guangdong Province, China.
Hengyu Liu, Zhongshan School of Medicine, Sun Yat-sen University, Guangzhou, Guangdong Province, China.
Zihang Mai, Zhongshan School of Medicine, Sun Yat-sen University, Guangzhou, Guangdong Province, China.
Zhuowei Liu, Department of Urology, Sun Yat-sen University Cancer Centre, State Key Laboratory of Oncology in South China, Collaborative Innovation Centre for Cancer Medicine, Guangzhou, China.
Chongxiang Chen, Department of Intensive Care Unit, Sun Yat-sen University Cancer Centre, State Key Laboratory of Oncology in South China, Collaborative Innovation Centre for Cancer Medicine, Dongfeng East Road 651, Guangzhou 510060, China; Guangzhou Institute of Respiratory Health, State Key Laboratory of Respiratory Disease, the First Affiliated Hospital of Guangzhou Medical University, Guangzhou 510120, China.
Qingyu Zhao, Department of Intensive Care Unit, Sun Yat-sen University Cancer Centre, State Key Laboratory of Oncology in South China, Collaborative Innovation Centre for Cancer Medicine, Guangzhou 510060, China.
References
- 1. Feng R-M, Zong Y-N, Cao S-M, et al. Current cancer situation in China: good or bad news from the 2018 Global cancer statistics? Cancer Commun (Lond) 2019; 39: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ferlay J, Colombet M, Soerjomataram I, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer 2019; 144: 1941–1953. [DOI] [PubMed] [Google Scholar]
- 3. Sung MR, Patel MV, Djalalov S, et al. Evolution of symptom burden of advanced lung cancer over a decade. Clin Lung Cancer 2017; 18: 274–280.e6. [DOI] [PubMed] [Google Scholar]
- 4. Iyer S, Roughley A, Rider A, et al. The symptom burden of non-small cell lung cancer in the USA: a real-world cross-sectional study. Support Care Cancer 2014; 22: 181–187. [DOI] [PubMed] [Google Scholar]
- 5. Jung JY, Lee JM, Kim MS, et al. Comparison of fatigue, depression, and anxiety as factors affecting posttreatment health-related quality of life in lung cancer survivors. Psychooncology 2018; 27: 465–470. [DOI] [PubMed] [Google Scholar]
- 6. Polanski J, Jankowska-Polanska B, Rosinczuk J, et al. Quality of life of patients with lung cancer. Onco Targets Ther 2016; 9: 1023–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Morrison EJ, Novotny PJ, Sloan JA, et al. Emotional problems, quality of life, and symptom burden in patients with lung cancer. Clin Lung Cancer 2017; 18: 497–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. World Health Organization. Telehealth and telemedicine will henceforth be part of the strategy for health-for-all. (Press release). Geneva, Switzerland: World Health Organization, 1997. [Google Scholar]
- 9. Johnston B, Wheeler L, Deuser J, et al. Outcomes of the Kaiser Permanente tele-home health research project. Arch Fam Med 2000; 9: 40–45. [DOI] [PubMed] [Google Scholar]
- 10. Alonso A. A new model for home care for COPD. Stud Health Technol Inform 2004; 103: 368–373. [PubMed] [Google Scholar]
- 11. Radhakrishnan K, Xie B, Jacelon CS. Unsustainable home telehealth: a Texas qualitative study. Gerontologist 2016; 56: 830–840. [DOI] [PubMed] [Google Scholar]
- 12. Horwitz CM, Mueller M, Wiley D, et al. Is home health technology adequate for proactive self-care? Methods Inf Med 2008; 47: 58–62. [DOI] [PubMed] [Google Scholar]
- 13. Hong Y, Lee SH. Effectiveness of tele-monitoring by patient severity and intervention type in chronic obstructive pulmonary disease patients: a systematic review and meta-analysis. Int J Nurs Stud 2019; 92: 1–15. [DOI] [PubMed] [Google Scholar]
- 14. Zhao J, Zhai Y-K, Zhu W-J, et al. Effectiveness of telemedicine for controlling asthma symptoms: a systematic review and meta-analysis. Telemed J E Health 2015; 21: 484–492. [DOI] [PubMed] [Google Scholar]
- 15. Knox L, Rahman RJ, Beedie C. Quality of life in patients receiving telemedicine enhanced chronic heart failure disease management: a meta-analysis. J Telemed Telecare 2017; 23: 639–649. [DOI] [PubMed] [Google Scholar]
- 16. Jakhar D, Kaul S, Kaur I. WhatsApp messenger as a teledermatology tool during coronavirus disease (COVID-19): from bedside to phone-side. Clin Exp Dermatol 2020; 45: 739–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Timmerman JG, Dekker-van Weering MGH, Stuiver MM, et al. Ambulant monitoring and web-accessible home-based exercise program during outpatient follow-up for resected lung cancer survivors: actual use and feasibility in clinical practice. J Cancer Surviv 2017; 11: 720–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sui Y, Wang T, Wang X. The impact of WeChat app-based education and rehabilitation program on anxiety, depression, quality of life, loss of follow-up and survival in non-small cell lung cancer patients who underwent surgical resection. Eur J Oncol Nurs 2019; 45: 101707. [DOI] [PubMed] [Google Scholar]
- 19. Ciani O, Cucciniello M, Petracca F, et al. Lung Cancer App (LuCApp) study protocol: a randomised controlled trial to evaluate a mobile supportive care app for patients with metastatic lung cancer. BMJ Open 2019; 9: e025483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Park S, Kim JY, Lee JC, et al. Mobile phone app-based pulmonary rehabilitation for chemotherapy-treated patients with advanced lung cancer: pilot study. JMIR Mhealth Uhealth 2019; 7: e11094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Paul CL, Boyes AW, O’Brien L, et al. Protocol for a randomized controlled trial of proactive web-based versus telephone-based information and support: can electronic platforms deliver effective care for lung cancer patients? JMIR Res Protoc 2016; 5: e202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nipp RD, Greer JA, El-Jawahri A, et al. Coping and prognostic awareness in patients with advanced cancer. J Clin Oncol 2017; 35: 2551–2557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chen YJ, Narsavage GL, Frick KD, et al. Home-telemonitoring lung cancer intervention in Appalachia: a pilot study. Int J Chronic Dis Ther 2016; 2: 21–30. [PMC free article] [PubMed] [Google Scholar]
- 24. Denis F, Lethrosne C, Pourel N, et al. Randomized trial comparing a web-mediated follow-up with routine surveillance in lung cancer patients. J Natl Cancer Inst 2017; 109. [DOI] [PubMed] [Google Scholar]
- 25. Hintistan S, Nural N, Cilingir D, et al. Therapeutic effects of nurse telephone follow-up for lung cancer patients in Turkey. Cancer Nurs 2017; 40: 508–516. [DOI] [PubMed] [Google Scholar]
- 26. Mosher CE, Winger JG, Hanna N, et al. Randomized pilot trial of a telephone symptom management intervention for symptomatic lung cancer patients and their family caregivers. J Pain Symptom Manage 2016; 52: 469–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Badr H, Smith CB, Goldstein NE, et al. Dyadic psychosocial intervention for advanced lung cancer patients and their family caregivers: results of a randomized pilot trial. Cancer 2015; 121: 150–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Huang C-C, Kuo H-P, Lin Y-E, et al. Effects of a web-based health education program on quality of life and symptom distress of initially diagnosed advanced non-small cell lung cancer patients: a randomized controlled trial. J Cancer Educ 2019; 34: 41–49. [DOI] [PubMed] [Google Scholar]
- 29. Walker J, Hansen CH, Martin P, et al. Integrated collaborative care for major depression comorbid with a poor prognosis cancer (SMaRT Oncology-3): a multicentre randomised controlled trial in patients with lung cancer. Lancet Oncol 2014; 15: 1168–1176. [DOI] [PubMed] [Google Scholar]
- 30. Chang N-W, Lin K-C, Lee S-C, et al. Effects of an early postoperative walking exercise programme on health status in lung cancer patients recovering from lung lobectomy. J Clin Nurs 2014; 23: 3391–3402. [DOI] [PubMed] [Google Scholar]
- 31. Choi S, Ryu E. Effects of symptom clusters and depression on the quality of life in patients with advanced lung cancer. Eur J Cancer Care (Engl). Epub ahead of print 26 April 2018. DOI: 10.1111/ecc.12508. [DOI] [PubMed] [Google Scholar]
- 32. Rueda J-R, Solà I, Pascual A, et al. Non-invasive interventions for improving well-being and quality of life in patients with lung cancer. Cochrane Database Syst Rev 2011; 2011: CD004282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chan CW, Richardson A, Richardson J. Managing symptoms in patients with advanced lung cancer during radiotherapy: results of a psychoeducational randomized controlled trial. J Pain Symptom Manage 2011; 41: 347–357. [DOI] [PubMed] [Google Scholar]
- 34. Arbane G, Tropman D, Jackson D, et al. Evaluation of an early exercise intervention after thoracotomy for non-small cell lung cancer (NSCLC), effects on quality of life, muscle strength and exercise tolerance: randomised controlled trial. Lung Cancer 2011; 71: 229–234. [DOI] [PubMed] [Google Scholar]
- 35. Chen Y-Y, Guan BS, Li Z-K, et al. Effect of telehealth intervention on breast cancer patients’ quality of life and psychological outcomes: a meta-analysis. J Telemed Telecare 2018; 24: 157–167. [DOI] [PubMed] [Google Scholar]
- 36. Jiao W, Zhao Y, Wang M, et al. A retrospective study of diaphragmatic motion, pulmonary function, and quality-of-life following video-assisted thoracoscopic lobectomy in patients with nonsmall cell lung cancer. Indian J Cancer 2015; 51(Suppl. 2): e45–e48. [DOI] [PubMed] [Google Scholar]
- 37. Spigel DR, McCleod M, Jotte RM, et al. Safety, efficacy, and patient-reported health-related quality of life and symptom burden with nivolumab in patients with advanced non-small cell lung cancer, including patients aged 70 years or older or with poor performance status (CheckMate 153). J Thorac Oncol 2019; 14: 1628–1639. [DOI] [PubMed] [Google Scholar]
- 38. Reck M, Brahmer J, Bennett B, et al. Evaluation of health-related quality of life and symptoms in patients with advanced non-squamous non-small cell lung cancer treated with nivolumab or docetaxel in CheckMate 057. Eur J Cancer 2018; 102: 23–30. [DOI] [PubMed] [Google Scholar]
- 39. Yount SE, Rothrock N, Bass M, et al. A randomized trial of weekly symptom telemonitoring in advanced lung cancer. J Pain Symptom Manage 2014; 47: 973–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Khue PM, Thom VT, Minh DQ, et al. Depression and anxiety as key factors associated with quality of life among lung cancer patients in Hai Phong, Vietnam. Front Psychiatry 2019; 10: 352. [DOI] [PMC free article] [PubMed] [Google Scholar]