Abstract
Purpose:
The aim of this study was to compare breast imaging subspecialists’ follow-up recommendations for incidental liver lesions (ILLs) on breast MRI with abdominal subspecialty radiologists’ opinions informed by best-practice recommendations.
Methods:
In this retrospective study at an academic medical center, natural language processing identified reports with ILLs among 2,181 breast MRI studies completed in 2015. Electronic health record and radiology report reviews abstracted malignancy presence or absence, prior imaging, and breast subspecialists’ recommendations regarding ILLs for random sets of 30 patients: ILLs with follow-up recommendations, ILLs without recommendations, and without ILLs. Two abdominal radiologists evaluated MRI liver findings and offered follow-up recommendations in consensus. The primary outcome was agreement between breast and abdominal subspecialists in patients with ILL follow-up recommendations compared with those without (χ2 analysis). Secondary outcomes were agreement between subspecialists when ILLs were reported and referring clinicians’ adherence to follow-up recommendations.
Results:
ILLs were identified in 11.3% of breast MRI reports (247 of 2,181); breast subspecialists made follow-up recommendations in 12% of them (30 of 247). Abdominal subspecialists agreed with breast subspecialists when ILLs required no follow-up (29 of 30 cases) but disagreed with 28 of 30 breast subspecialists’ follow-up recommendations (agreement proportion 29 of 30 versus 2 of 30, P < .0001). Subspecialists agreed in 93% of cases (28 of 30) when breast imagers reported no ILLs. Overall, 16 of 30 breast subspecialists’ follow-up recommendations were performed; ILLs were benign in 15.
Conclusions:
Abdominal subspecialists disagreed frequently with breast subspecialists regarding follow-up recommendations for ILLs on breast MRI. Abdominal subspecialty consultation or embedding liver imaging decision support in breast imaging reporting workflow may reduce unnecessary imaging and improve care. Improvement opportunities may exist in other cross-subspecialty interpretation workflows.
Introduction
The importance of practicing consistent, high quality, and evidence-based radiology is promoted in the American College of Radiology (ACR) strategic initiative Imaging 3.0, which is based on the ideals of appropriateness, efficiency, quality, safety, and satisfaction.(1) Although the majority of radiologists in the United States are generalists, subspecialists are prevalent in larger and academic practices,(2) and breast imagers make up one of the top 3-5 subspecialty practices.(2,3) In radiology practices that embrace a subspecialty care model, radiologists may make follow-up recommendations when interpreting organ system imaging findings outside the primary organ of the subspecialist. In one example, the liver is incompletely imaged on breast MRI, however, follow-up recommendations may be made by breast imaging subspecialists when encountering incidental liver lesions (ILLs) while interpreting breast MRIs.
Several studies have looked at the incidence and implications of any extramammary findings on breast MRI (4–8), while others have focused specifically on ILLs (9, 10). In nearly all studies, hepatic lesions were the most common incidental finding (ranging from 44-60%), with reported incidence of 6-28% (4–8). Although most likely to be benign (7, 10), ILLs were also the most frequent indication for additional imaging follow-up (6). Knox et al reported additional imaging recommendations for ILLs in 37.3% of their study patients (9), but proposed the potential to achieve a reduction to 5.3% by employing more specific guidelines to MRI findings. Shah et al looked specifically at T2 hyperintense ILLs, finding only 2.7% were malignant, and all of those were associated with a new diagnosis of breast cancer (10). Other authors also noted that malignant incidental findings were found exclusively in patients with known breast malignancy (5, 6). Niell et al retrospectively categorized incidental findings on breast MRI as clinically unimportant (E2), incompletely characterized (E3), and potentially important (E4), using the computed tomography (CT) colonography reporting and data system (C-RADS). The majority, though not all lesions, were ILLs (6).
Although several authors have described the incidence/prevalence of ILLs -- one citing the high rate of false positive findings outside the breast (4), another reporting the low positive predictive value for breast MRI to detect a metastatic lesion within the liver (7) -- no one has addressed the common clinical scenario of having a breast imaging subspecialist address an abdominal finding. Therefore, the purpose of this study was to evaluate potential differences in follow-up recommendations for incidentally detected hepatic lesions between breast radiology subspecialists and abdominal radiology subspecialists in an academic radiology practice organized by subspecialty. We hypothesized that breast imaging subspecialists make significantly more follow-up recommendations than abdominal radiology subspecialists for ILLs found on breast MRI.
Methods
Study Setting and Population
Institutional Review Board approval was obtained for this retrospective, HIPAA-compliant study performed at a 793-bed urban tertiary academic medical center performing more than 800,000 annual radiological examinations, and an affiliated outpatient tertiary cancer center performing over 66,000 radiologic examinations annually. The initial sampling frame consisted of all female patients who underwent diagnostic breast MRI between 2010 and 2015. Of the 20,338 breast MRI examinations during the study period, 6,089 (30%) were performed at an outside institution and were thus excluded, leaving 14,249 examinations (Figure 1).
Figure 1:
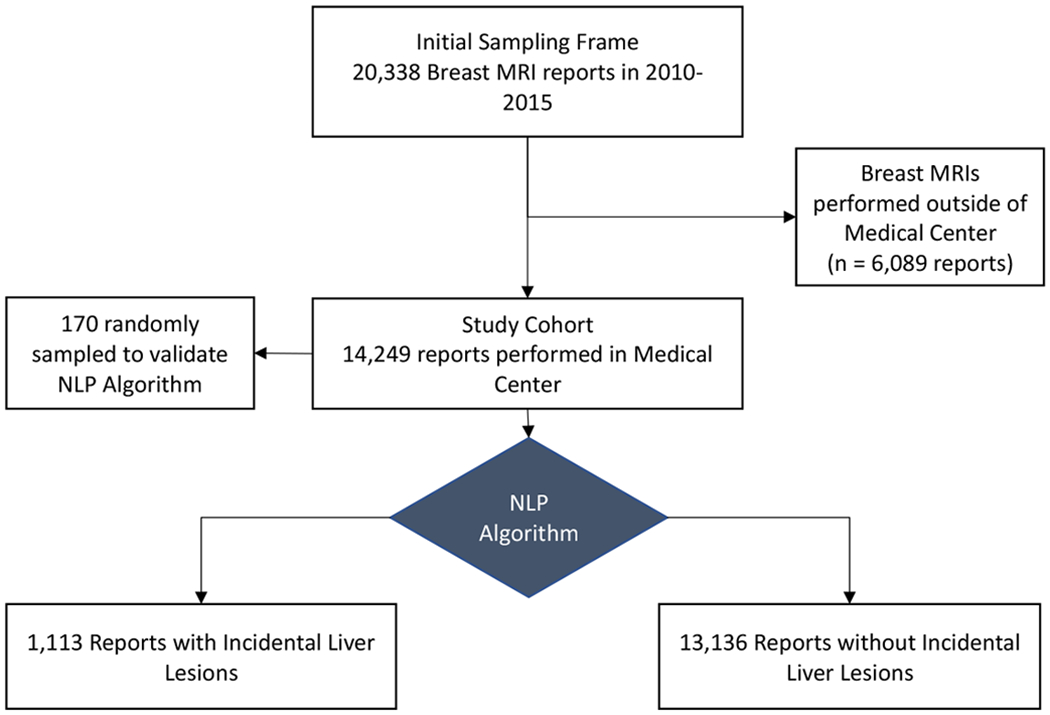
Flowchart of patient cohort selection.
Natural Language Processing Algorithm and Validation
ILLs on breast MRI were identified through CEBI-Miner, a natural language processing (NLP) algorithm that searched the breast MRI radiology reports for words relating to liver lesions and classified negations. The latter included the words ‘no’ and ‘not’ within 4 words before ‘liver’ or ‘hepatic’. Among the 14,249 reports, the NLP algorithm identified 1,113 (7.8%) that contained liver lesions (Table 1). A total of 170 reports were randomly sampled from those identified by NLP and manually reviewed to confirm the presence of ILLs. 100 reports were reviewed by a trained radiologist and 100 by a research assistant with 30 reports overlapping to assess inter-reviewer reliability.
Table 1:
Rate of Incidental Liver Lesions on Breast MRI by Study Year
| Year | Number of Breast MRI Reports | Reports with Incidental Liver Lesion | Percent |
|---|---|---|---|
| 2010 | 2560 | 112 | 4.4 |
| 2011 | 2933 | 172 | 5.9 |
| 2012 | 2313 | 183 | 7.9 |
| 2013 | 2065 | 183 | 8.9 |
| 2014 | 2197 | 216 | 9.8 |
| 2015 | 2181 | 247 | 11.3 |
| TOTAL | 14,249 | 1113 | 7.8 |
Cohort Selection and Data Collection
Over the study period, there was a continued rise in reported ILLs (Table 1). To focus on the most recent data at our institution, the 247 reports in 2015 with ILLs were manually reviewed to collect patient-specific data (presence/absence of malignancy, availability of prior studies) and hepatic lesion-specific (size, location, multiplicity, and follow-up recommendation) variables.
Among the 247 breast MRI reports in 2015 with ILLs, 12% (30/247) had follow-up recommendations made by the interpreting breast imaging subspecialist. Three groups of 30 cases each were then identified. Group One consisted of the 30 cases with an ILL and follow-up recommendations, Group Two consisted of 30 randomly-selected cases with an ILL and no follow-up recommendation, and Group Three consisted of 30 cases randomly sampled from the 1,934 cases in 2015 without an ILL characterized in the report.
Best Practice Recommendations and Abdominal Subspecialist Review
Local best practice recommendations for the study were based on consensus opinion of two Board-certified abdominal subspecialty radiologists who reviewed the breast MRI cases in Groups One, Two and Three. They independently reviewed each case and noted their recommendation for the liver lesion when one was present. When the two abdominal subspecialists’ recommendations differed, the case was reviewed together, and a consensus decision was made. The abdominal radiologists independently reviewed the American College of Radiology White Paper for ILLs detected at CT before beginning the image review process. However, they were not required to follow the white paper’s recommendations in their independent image review or during the consensus discussion.
Referring Clinician Adherence to Follow-Up Recommendations
For each case containing a follow-up recommendation, the electronic health record was searched for follow-up imaging studies, or their reports when performed at an outside institution. All subsequent pertinent radiologic imaging through August 2019 was reviewed for stability, change, or further characterization of ILLs.
Outcome Measures
The primary study outcome was agreement between breast imaging subspecialists’ recommendations and abdominal subspecialist consensus recommendations for ILLs noted on breast MRI, comparing agreement when follow-up recommendations were present and absent. Secondary outcomes were agreement of abdominal subspecialists with breast imaging subspecialists when no lesion was reported, and adherence to/acquisition of recommended follow-up studies by referring clinicians.
Statistical Analysis
The reported proportion of ILLs identified in imaging exams is 10.6%.(11) Sample size for the assessment of the NLP algorithm’s performance was calculated based on a prevalence of ILLs of 10-12.5% with a precision of 0.05, to arrive at a sample size of 170. The sample size calculation formula was used for prevalence estimation.(12) To evaluate breast and abdominal subspecialists’ agreement, Fisher’s Exact test of proportions was used to compare the proportion of concordance in ILLs with follow-up recommendations versus those without. Percentage agreement was calculated between the two reviewers who manually reviewed reports for liver lesions. Statistical analysis was done in R version 3.4.2 (R Foundation for Statistical Computing, Vienna, Austria). Statistical significance was set at p<0.05.
Results
Study Cohort
The study cohort included 90 total reports in Groups One, Two and Three. Upon review, in Group One, two cases had no liver lesions; one was a pulmonary nodule, and the other was correctly characterized as susceptibility artifact, though for which further imaging evaluation was recommended (Figure 2).
Figure 2:
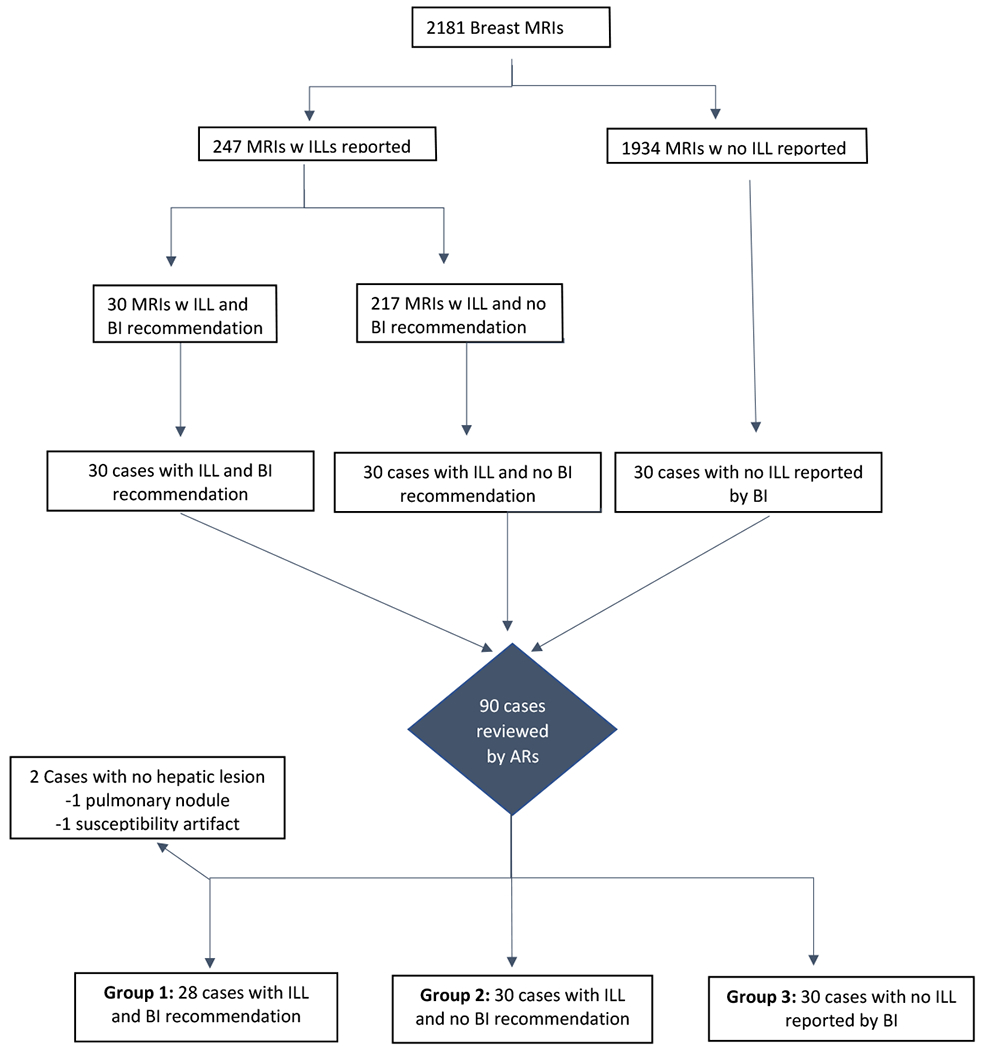
Review of cases. AR = abdominal subspecialty radiologist; BR = breast subspecialty radiologist; ILL = incidental liver lesion
Tests of Data Quality
Percentage agreement between the two reviewers for identifying liver lesions in reports was 100%. Recall and precision of the NLP algorithm were 100%. Of the 170 cases, NLP accurately predicted 159 without liver lesions, and 11 with liver lesions.
Agreement between Breast and Abdominal Subspecialists
A total of 8 of the 90 cases across the three groups (8/90=8.9%) required consensus agreement between the abdominal radiologists. Among the 30 cases in Group One where breast subspecialists made a follow-up recommendation for an ILL, abdominal subspecialists agreed with 2 (7%). One included recommendation for correlation with a pre-scheduled same day PET-CT scan. The other was for a 1.6 cm indeterminate liver lesion in a patient with newly diagnosed triple negative breast cancer, who did not undergo further imaging evaluation at the time, but received chemotherapy, and presented 1 year later with widespread metastatic disease, including liver involvement. In two cases, abdominal subspecialists recommended MRIs (1 immediately, and 1 in 3-6 months), while breast subspecialists recommended ultrasound evaluation. Of these, 1 had no follow-up of a probable hemangioma, but has continued to undergo screening mammograms, the last in 2019. The other patient, for which 3-6 month follow-up was recommended by the abdominal subspecialists, underwent the recommended ultrasound which was non-diagnostic, with subsequent MRI, revealing a probable biliary cystadenoma, last followed at 4 years (2/2019), and stable.
In the remaining 26 cases, the abdominal subspecialists recommended no follow-up as lesions were not present or were identified as benign, most commonly cysts or hemangiomas. Among the 30 cases in Group Two with ILLs for which the breast imagers did not make a follow-up recommendation, the abdominal subspecialists agreed that no follow-up recommendation was necessary in 29 (97%;) but made a recommendation for the remaining case with a 1.6 cm ILL (which has remained stable for at least 4 years). Fisher’s exact test showed a significantly greater agreement proportion with breast subspecialists’ recommendations when no follow-up recommendation was necessary (agreement proportion 29/30 vs. 2/30; p<0.0001).
Among the 30 cases in Group Three where the breast subspecialist detected no liver lesions, abdominal subspecialists noted 2 lesions (agreement 93% [28/30]). One was a 4 mm cyst requiring no additional follow-up. The other was an indeterminate 1.2 cm left hepatic lesion which remained unchanged for over 2 years on repeat breast MRI.
Adherence to Breast Subspecialists’ Recommendations
Of the 30 cases in Group One where breast subspecialists made a follow-up recommendation for an ILL on breast MRI, referring clinicians obtained examinations in 53% (16/30). Of these, 94% (15/16) of ILLs were proven benign, and 1 malignant. An additional 10 cases were shown to most likely be benign (characterized on a subsequent study, stable for >3 years, or patient continued screening for at least 2 years), resulting in overall probable benignity in at least 83% (25/30) of cases for which additional imaging was recommended. One patient presented with widespread metastatic disease 1 year later (no immediate follow-up was obtained), and 3 patients were lost to follow up.
Discussion
In this study, abdominal subspecialists’ follow-up recommendations regarding ILLs noted on breast MRI agreed with only 7% of those recommendations made by breast subspecialists. However, abdominal subspecialists agreed in 97% of cases where breast subspecialists noted an ILL and made no follow-up recommendation, and in 93% of interpretations where a breast subspecialist detected no ILL. Among cases where referring clinicians followed breast imager recommendations and obtained follow-up for an ILL, 94% (15/16) were characterized as benign. These findings suggest that at our institution, breast imagers may recommend potentially unnecessary imaging for ILLs, an area outside the scope of their subspecialty practice.
Our finding of 11.3% of breast MRI reports with ILLs in 2015 is similar to reported incidences of 6-28% (6–10) in other studies. Using Medicare reimbursement rates, Niell et al concluded that incompletely characterized or potentially important extramammary findings warrant additional imaging, adding only a small incremental increase in cost. However, based on our study results, breast subspecialists often made unnecessary recommendations for benign incidental hepatic findings that should have required no additional cost. Given the findings at our institution, an educational intervention regarding best practice recommendations may be helpful to breast imagers reading MRIs that contain liver findings. A recent publication by Shinagare et al showed that imbedding ACR white paper guidelines regarding follow-up of incidental adnexal lesions into the radiologist workflow can improve adherence to guidelines. (13) A similar workflow incorporation for breast subspecialists interpreting MRI may improve patient care and avoid unnecessary examinations of the liver.
This study has several limitations. The design was retrospective and used natural language processing to identify breast MRI studies where an ILL was noted, which may have underestimated the prevalence of such lesions. The study was performed at a single academic medical center and its affiliated outpatient cancer center, and therefore results may not be generalizable. Only a representative 90 studies from one year were directly evaluated by abdominal subspecialists. We used local best practice follow-up recommendations based on consensus opinion of 2 abdominal subspecialty radiologists which may differ from other practices. We did not have follow-up data on all lesions for which follow-up was recommended.
In summary, variability exists in follow-up recommendations between breast imaging subspecialists and abdominal subspecialists when ILLs are detected on breast MRI. Additional studies are not infrequently recommended that may be unnecessary. Abdominal subspecialty consultation, or educational interventions including embedding liver imaging best practice as decision support in breast imaging reporting workflow, may reduce unnecessary imaging and improve experience and care for patients undergoing breast MRI. Future studies should assess whether similar improvement opportunities exist in other cross-subspecialty interpretation workflows.
Take-home Points.
At our institution, breast subspecialists made significantly more follow-up recommendations than abdominal subspecialists for incidental liver lesions seen on breast MRI.
Direct abdominal subspecialist consultation or access to guidelines during breast MRI interpretation may eliminate many unnecessary follow-up examinations in practices such as ours where discrepant recommendations are made between breast and abdominal imaging subspecialists.
Similar opportunities for improvement may exist in other cross-subspecialty workflows.
Acknowledgments:
The authors thank Laura E. Peterson for editorial assistance and Isha Gujrathi for assistance with reviewing reports.
Funding Support: Dr Lacson was funded through grant R01 HS24722 from the Agency for Healthcare Research and Quality.
References
- 1.Ellenbogen PH. Imaging 3.0: What Is It? Journal of the American College of Radiology. 2013;10(4):229. [DOI] [PubMed] [Google Scholar]
- 2.Rosenkrantz AB, Wang W, Hughes DR, Duszak R. Generalist versus Subspecialist Characteristics of the U.S. Radiologist Workforce. Radiology. 2018;286(3):929–937. [DOI] [PubMed] [Google Scholar]
- 3.Bender CE, Bansal S, Wolfman D, Parikh JR. 2018 ACR Commission on Human Resources Workforce Survey. Journal of the American College of Radiology. 2019;16(4, Part A):508–512. [DOI] [PubMed] [Google Scholar]
- 4.Padia SA, Freyvogel M, Dietz J, Valente S, O’Rourke C, Grobmyer SR. False-positive Extra-Mammary Findings in Breast MRI: Another Cause for Concern. Breast J. 2016;22(1):90–95. [DOI] [PubMed] [Google Scholar]
- 5.Alduk AM, Prutki M, Stern-Padovan R. Incidental extra-mammary findings in breast MRI. Clinical Radiology. 2015;70(5):523–527. [DOI] [PubMed] [Google Scholar]
- 6.Niell BL, Bennett D, Sharma A, Gazelle GS. Extramammary Findings on Breast MR Examinations: Frequency, Clinical Relevance, and Patient Outcomes. Radiology. 2015;276(1):56–64. [DOI] [PubMed] [Google Scholar]
- 7.Rinaldi P, Costantini M, Belli P, et al. Extra-mammary findings in breast MRI. Eur Radiol. 2011;21(11):2268–2276. [DOI] [PubMed] [Google Scholar]
- 8.Iodice D, Di Donato O, Liccardo I, et al. Prevalence of extramammary findings on breast MRI: a large retrospective single-centre study. Radiol Med. 2013;118(7):1109–1118. [DOI] [PubMed] [Google Scholar]
- 9.Knox M, Slanetz P, Phillips J, et al. Incidental liver lesions seen on Breast MRI: When is additional imaging warranted? European Journal of Radiology. 2017;95:319–324. [DOI] [PubMed] [Google Scholar]
- 10.Shah PK, Kafer IA, Grimaldi GM. Incidental hepatic lesions detected on breast MRI: Rate of malignancy and implications for utilization. Clin Imaging. 2018;51:93–97. [DOI] [PubMed] [Google Scholar]
- 11.Zygmont ME, Shekhani H, Kerchberger JM, Johnson J-O, Hanna TN. Point-of-Care Reference Materials Increase Practice Compliance With Societal Guidelines for Incidental Findings in Emergency Imaging. J Am Coll Radiol. 2016;13(12 Pt A):1494–1500. [DOI] [PubMed] [Google Scholar]
- 12.Naing L, Winn T, Rusli BN. Practical Issues in Calculating the Sample Size for Prevalence Studies. Archives of Orofacial Science 2006:1:9–14. [Google Scholar]
- 13.Shinagare AB, Alper E, Wang A, Ip IK, Khorasani R. Impact of a Multifaceted Information Technology–Enabled Intervention on the Adoption of ACR White Paper Follow-Up Recommendations for Incidental Adnexal Lesions Detected on CT. American Journal of Roentgenology. 2019;213(1):127–133. [DOI] [PubMed] [Google Scholar]


