Abstract
The ratio of subjects to variables (N/p), as a rule to calculate the sample size required in internal validity studies on measurement scales, has been recommended without any strict theoretical or empirical basis being provided. The purpose of the present study was to develop a tool to determine sample size for these studies in the field of psychiatry. First, a literature review was carried out to identify the distinctive features of psychiatric scales. Then, two simulation methods were developed to generate data according to: (1) the model for factor structure derived from the literature review and (2) a real dataset. This enabled the study of the quality of solutions obtained from principal component analysis or Exploratory Factor Analysis (EFA) on various sample sizes. Lastly, the influence of sample size on the precision of Cronbach's alpha coefficient was examined. The N/p ratio rule is not upheld by this study: short scales do not allow smaller sample size. As a rule of thumb, if one's aim is to reveal the factor structure, a minimum of 300 subjects is generally acceptable but should be increased when the number of factors within the scale is large, when EFA is used and when the number of items is small. Copyright © 2011 John Wiley & Sons, Ltd.
Keywords: sample size, validation studies, factor analysis, questionnaires, psychiatry
Introduction
One of the most critical methodological issues when designing a study and planning the statistical analysis, is the number of subjects to include. Generally, the sample size is based on the power of a statistical test of hypothesis. In descriptive studies, this approach cannot be used, and it is usually the range of the confidence interval of a given parameter which determines sample size. This is likely to be the case in internal validity studies of measurement scales in which, traditionally, two types of parameters are of interest: Cronbach's alpha coefficient (α) which assesses reliability, and factor analysis loadings which explore the dimensional structure of the scale. In practice, these loadings are estimated either by Principal Component Analysis (PCA) or by Exploratory Factor Analysis (EFA). A formula for the confidence interval of Cronbach's alpha coefficient was developed by Feldt in the 1960s (Fan and Thompson, 2001; Feldt, 1965). The sample size required for a desired precision of this coefficient can, therefore, be easily assessed. In fact, the difficulty in establishing a simple rule for sample size calculation in internal validity studies arises from the use of factor analysis.
Many recommendations regarding sample size in factor analysis have been made, but none are founded on a strict theoretical or empirical basis. The most widely used rule uses the ratio of the number of subjects (N) to the number of items (p), and this varies from three to 10 depending on authors (Cattell, 1978; Everitt, 1975; Gorsuch, 1983; Nunnaly, 1978). Other authors have suggested an absolute minimum sample size of 50 to 500 to enable factor analysis (Aleamoni, 1973; Comrey, 1978; Comrey and Lee, 1992; Loo, 1983). Given these various recommendations and their lack of documented explanation, some researchers have put them to the test by studying the consequences of using factor analysis on insufficient sample sizes. They all found that, in addition to N, two other parameters are important to obtain accurate and stable solutions: firstly the ratio of the number of variables to the number of factors (ratio p/M, which is an indicator of “factor overdetermination”, a concept defined by MacCallum et al. in 1999 as the degree to which each factor is clearly represented by a sufficient number of variables, at least three or four); and secondly the level of factor loadings (which reflects the level of communalities, the communality of a variable being the portion of the variance that a variable shares with the common factors). The lower the p/M ratio and the factor loading level, the larger the sample size required for a given accuracy and stability of solutions obtained from factor analysis (Guadagnoli and Velicer, 1988; Hogarty et al., 2005; MacCallum et al., 1999; Mundfrom et al., 2005; Velicer and Fava, 1998). All these studies have shown that sample size partly depends on the nature of the data: their “strength”. Strong data in factor analysis means uniformly high communalities without cross‐loadings, plus several variables loading strongly on each factor (Costello and Osborn, 2005; Fabrigar et al., 1999). The stronger the data, the smaller the sample size required. It does not therefore seem possible to recommend a general rule for sample size calculation that is valid in all the fields to which psychometric procedures apply.
However, in each field, there are distinctive features. In psychiatry, factor loading values are usually close to 0.6, the p/M ratio can vary from three to 20 or more, depending on scales, and the number of items is often different for each factor within a scale (Dawkins et al., 2006; Gabryelewicz et al., 2004; Iwata et al., 2000; Loza et al., 2003). Another characteristic observed in psychiatric scales is the shape of the scree plot. Unidimensionality is rare, and usually there is a first dimension representing a large part of the variance contained in the data (from 30 to 35%), and then there are one or more other dimensions explaining smaller and decreasing proportions of variance (from 15 to 5%) (Chapman et al., 2009; Sanchez‐Lopez and Dresch, 2008; Uslu et al., 2008; Villalta‐Gil et al., 2006). This factor structure can be explained by the presence of correlated factors or, likewise, by a two‐order factor model in which a second‐order factor explains the pattern of correlations among the first‐order factors.
The unresolved methodological issue about sample size in validation studies of measurement scales can lead to erroneous conclusions being drawn if the sample is too small. Conversely, the inclusion of too many subjects in a study wastes time and resources for researchers. The main purpose of this study is therefore to use the distinctive features encountered in psychiatric scales to develop a tool for the determination of the sample size required in internal validity studies on such scales in order to guarantee an acceptable level of precision for Cronbach's alpha coefficient and, above all, accuracy and stability of the factor solution. A secondary aim is to determine the influence of the choice of PCA or EFA on the sample size required and on the accuracy of the factor solution.
Material and methods
This study comprised three stages. The first consisted in a literature review to determine the shared characteristics of psychiatric scales. The second used simulations to study the influence of sample size on the stability and accuracy of the solutions obtained from PCA and EFA. These simulations were based, firstly, on artificial data generated according to the factor pattern observed in psychiatric scales from the literature review, and then on real data. Finally, the influence of sample size on the precision of Cronbach's alpha coefficient in the conditions encountered in psychiatry was studied.
Literature review
Ten psychiatric scales were selected taking account of the frequency of their use in clinical practice and their representativeness of different pathologies encountered in psychiatry:
Positive and Negative Syndrome Scale (PANSS – 30 items)
Brief Psychiatric Rating Scale (BPRS – 18 items)
Beck Anxiety Inventory (BAI – 21 items)
State–Trait Anxiety Inventory (STAI – 40 items)
Hamilton Anxiety Rating Scale (HAMA – 14 items)
Hamilton Rating Scale for Depression (HAMD – 17 items)
Montgomery–Asberg Depression Rating Scale (MADRS – 10 items)
Beck Depression Inventory (BDI – 21 items)
Hospital Anxiety and Depression Scale (HADS – 14 items)
General Health Questionnaire (GHQ – 12 items)
Articles including results of PCA or EFA concerning any of these 10 scales were sought in the Medline database using the following keywords: for each scale, the “name of the scale” and/or “its abbreviation”, the expressions “factor analysis” and/or “components analysis” and the article language “English” and/or “French”. A pre‐selection was carried out on the basis of the abstracts, and articles were then included if the following three criteria were met: the factor structure of one of the 10 scales was studied using PCA or EFA; eigenvalues or percentage of variance accounted for by each factor before rotation were specified; sample size was equal to or greater than 100.
In each article, the following data were collected: the method used for factor extraction (PCA or EFA), the rotation method used (orthogonal or oblique), the number of factors extracted, the eigenvalues or the percentage of variance accounted for by each factor before rotation, the number of items per factor and the values of the factor inter‐correlations. When the loading matrix was reproduced, the mean of the salient loadings was calculated by considering only the higher value in case of cross‐loadings. If several groups were studied, only the results from the largest group were considered. Likewise, if analyses were carried out on data collected at different times, only the results collected at the initial collection time were considered. All these data were recorded on the Microsoft®Office Excel 2007 spreadsheet program and descriptive statistical analyses for each of these variables were performed using R software 2.6.2 (R Development Core Team, 2008).
Simulation studies
Simulations based on artificial data
The simulation method developed here is based on the common factor model and is described in the Appendix. To summarize, certain important points should be noted. In this simulation model, two hypotheses are set. The first is the existence of a simple structure, i.e. each item loads on a single factor and all the non‐salient loadings are equal to zero. The second is that all salient loadings (λ) are equal. When a common factor model is used, responses have a normal distribution. To come closer to real‐life instruments, these responses were categorized into four‐class ordered variables as in a four‐point Likert response pattern. The response distribution was different for each item in the scale and non‐symmetrical so as to simulate floor and ceiling effects. Finally, parameters that can be controlled using this method are: the number of items (p), the number of factors (M), the number of items loading on each factor in the scale (pm, m = 1 to M), the value of salient loadings (λ), the level of the factor inter‐correlations (cor(Fm,Fm'), m ≠ m′) and the sample size (N).
For M and p, we decided to study the values usually encountered in psychiatry, i.e. scales with two, three or four factors and a number of items varying between 10 and 45 (p = 10, 15, 20, 25, 30, 35, 40 or 45). The results from the literature review then enabled the determination of the value of λ and pm. Levels of factor inter‐correlations were chosen amongst the values encountered in the literature review, and also in order to obtain the percentage of variance accounted for by each factor that was nearest to the mean of this percentage found in the review. Once all these parameter values were determined, two sets of 10,000 samples were generated for each sample size studied (N = 50, 100, 150, 200, 300, 500, 1000) and for each condition defined by M and p. Then, PCA was performed on one set and EFA on the other. These two methods of factor extraction were followed by a promax rotation which is an oblique rotation method as recommended when factors are correlated with each other (Costello and Osborn, 2005; Fabrigar et al., 1999; Floyd and Widaman, 1995). To determine the adequate sample size, three criteria were used as a threshold for good quality of the factor solution:
standard deviation of the salient loadings obtained after rotation over the 10,000 simulations (σλ) below 0.05 (95% confidence interval of the salient loadings close to )
percentage of simulations in which all the items in the scale loaded on the right factor (i.e. that which is determined in the simulation model) after rotation (R%) greater than 90%
the mean of percentages of items loading on the wrong factor in the scale after rotation over the 10,000 simulations (W%) below 1%
When EFA was performed, the percentage of simulations where Heywood cases occurred (i.e. loading estimates greater than 1.0, which occurs only with EFA) was also estimated. Finally, for either method (PCA and EFA), the mean of the salient loadings over the 10,000 simulations (μλ) was computed.
Simulations based on real data
To offer a complementary perspective, a simulation study was also conducted by the aid of an important real data set of 1009 patients consecutively hospitalized between January 1988 and July 2004 in the Eating Disorder Unit of the Clinique des Maladies Mentales et de l'Encéphale at Sainte‐Anne Hospital, Paris, France. Patient characteristics and procedures have been described previously in Fedorowicz et al. (2007). We focused on two instruments, the 13‐item version of the BDI (Beck et al., 1961) and the 21‐item version of the HAMD (Hamilton, 1960). For each of these scales, a parallel analysis was performed to determine the number of factors to extract. Next, two sets of 10,000 samples were repeatedly drawn from the entire sample (with replacement) for each sample size: 100, 200, 300, 400, 500, 600, 700 and 800. Then, PCA was performed on one set and EFA on the other, followed by a promax rotation in the case of a multidimensional instrument. The mean of the standard deviations of the loadings was then calculated over the 10,000 samples for each sample size.
These analyses were performed using R software 2.6.2. The function princomp was used for PCA and the loading matrix obtained was rotated using promax with a constant set at four (Costello and Osborn, 2005; Jackson, 1991). For EFA, the function factanal (with the argument rotation = promax, which uses the maximum likelihood estimation procedure, was chosen for two reasons: it finds the solution with the optimal statistical properties and it is likely the most widely used method (Revelle, 2008). Finally, the draw was performed using the function sample and parallel analysis using the function scree.plot from the psy package.
Precision of Cronbach's alpha coefficient
The most widely cited minimum value considered as acceptable for the Cronbach's alpha coefficient is 0.7 (Fedorowicz et al., 2007; Nunnaly, 1978; Peterson, 1994). We therefore chose to study the half‐width of the confidence interval of this coefficient for three expected values (α = 0.7, 0.8 and 0.9) in relation to p and N (same values as previously). Feldt's formula for this confidence interval was used with type I error rate set at 0.05 (Fan and Thompson, 2001; Feldt, 1965).
where ddl1 = N − 1, ddl2 = (N − 1) × (p − 1) and represents the values of the F‐distribution for percentiles 0.025 and 0.975 respectively.
Results
Psychiatric scale characteristics
The keywords used for the search in Medline database enabled the identification of 827 studies. Amongst these, 232 articles were pre‐selected on the basis of the abstracts, and a total of 56 articles met the inclusion criteria. Five of these articles showed results from factor analysis on two of the scales selected for this review, which finally increased the total to 61 references. Table 1 contains, for each scale, the total number of references included and the number of references extracting the same number of factors for each.
Table 1.
References included and numbers of references extracting the same number of factors for each scale
| Scale | References | Total | Number of factors | |||||
|---|---|---|---|---|---|---|---|---|
| 2 | 3 | 4 | 5 | 6 | 7 | |||
| PANSS | (Bell et al., 1994; Fresan et al., 2005; Honey et al., 2003; Kay and Sevy, 1990; Lancon et al., 1999; Lee et al., 2003; Lindenmayer et al., 2004; Loza et al., 2003; Lykouras et al., 2000; Salokangas et al., 2002; Villalta‐Gil et al., 2006) | 11 | — | — | 1 | 8 | — | 2 |
| BPRS | (Adachi et al., 2000; Harvey et al., 1996; Lachar et al., 2001; Ventura et al., 2000) | 4 | — | — | 2 | 1 | 1 | — |
| BAI | (Beck, 1991; Chapman et al., 2009; Kabacoff et al., 1997; Steer et al., 1995; Steer et al., 1993) | 5 | 4 | — | 1 | — | — | — |
| STAI | (Iwata et al., 2000; Iwata et al., 1998; Kabacoff et al., 1997) | 3 | 2 | 1 | — | — | — | — |
| HAMA | (Beck, 1991; Serretti et al., 1999) | 2 | 2 | — | — | — | — | — |
| HAMD | (Grunebaum et al., 2005; Olden et al., 2009) | 2 | — | — | 1 | 1 | — | — |
| MADRS | (Gabryelewicz et al., 2004; Galinowski and Lehert, 1995; Lee et al., 2003; Parker et al., 2003; Serretti et al., 1999) | 5 | 3 | 2 | — | — | — | — |
| BDI | (Basker et al., 2007; Bonicatto et al., 1998; Bonilla et al., 2004; Gorenstein et al., 1999; Grunebaum et al., 2005; Helm and Boward, 2003; Jo et al., 2007; Killgore, 1999; Munoz et al., 2007; Powell, 2003; Salamero et al., 1994; Shek, 1990; Steer et al., 1989; Uslu et al., 2008; Wang et al., 2005) | 15 | 9 | 2 | 3 | — | — | 1 |
| HADS | (Dagnan et al., 2008; Dawkins et al., 2006; Friedman et al., 2001; Pallant and Bailey, 2005; Smith et al., 2002; Woolrich et al., 2006) | 6 | 4 | 2 | — | — | — | — |
| GHQ | (Castro‐Costa et al., 2008; Farrell, 1998; Hankins, 2008; Hu et al., 2007; Kilic et al., 1997; Lopez‐Castedo and Fernandez, 2005; Sanchez‐Lopez and Dresch, 2008; Werneke et al., 2000) | 8 | 5 | 3 | — | — | — | — |
| Total | 61 | 29 | 10 | 8 | 10 | 1 | 3 | |
In order to estimate a pattern of factor structure encountered in psychiatric scales, the descriptive statistical analyses were carried out over all the references without considering the number of factors found in the scales. The means of percentages of variance accounted for by each factor before rotation are shown in Table 2 for each scale and a box‐plot of these percentages over all the references is provided in Figure 1.
Table 2.
Percentage of variance accounted for by each factor and numbers of references used to estimate the means for each scale
| Scale | Factors | |||||||
|---|---|---|---|---|---|---|---|---|
| F 1 | F 2 | F 3 | F 4 | F 5 | F 6 | F 7 | ||
| PANSS | Mean (Minimum–Maximum) | 25.8 (14.5–41.2) | 12.8 (8.7–18.6) | 8.8 (6.1–13.4) | 6.8 (3.9–11.1) | 5.8 (3.6–9.3) | 3.6 (3.6–3.7) | 3.6 (3.6–3.7) |
| Number of references | 11 | 11 | 11 | 11 | 10 | 2 | 2 | |
| BPRS | Mean (Minimum–Maximum) | 18.9 (12.8–23.3) | 14.0 (9.3–17.2) | 10.4 (8.7–11.7) | 8.3 (6.7–10.0) | 6.9 (6.1–7.8) | 6.7 (—) | |
| Number of references | 4 | 4 | 4 | 4 | 2 | 1 | ||
| BAI | Mean (Minimum–Maximum) | 37.6 (36.3–39.5) | 7.2 (4.4–7.7) | 6.2 (—) | 5.2 (—) | |||
| Number of references | 5 | 5 | 1 | 1 | ||||
| STAI | Mean (Minimum–Maximum) | 32.2 (29.8–34.3) | 9.6 (7.4–11) | 6.0 (—) | ||||
| Number of references | 3 | 3 | 1 | |||||
| HAMA | Mean (Minimum–Maximum) | 26.9 (20.4–33.5) | 8.2 (6.4–10) | |||||
| Number of references | 2 | 2 | ||||||
| HAMD | Mean (Minimum–Maximum) | 12.8 (12.6–13.0) | 11.3 (11.2–11.4) | 10.7 (10.4–11.0) | 8.5 (7.3–9.8) | 9.4 (—) | ||
| Number of references | 2 | 2 | 2 | 2 | 1 | |||
| MADRS | Mean (Minimum–Maximum) | 33.7 (25.1–41.1) | 15.6 (10.4–26.9) | 10.6 (10.2–1.0) | ||||
| Number of references | 5 | 5 | 2 | |||||
| BDI | Mean (Minimum–Maximum) | 29.4 (22.9–34.5) | 8.8 (5.9–25.1) | 6.8 (5.0–6.1) | 5.4 (4.9–6.1) | 6.0 (—) | 5.5 (—) | 4.9 (—) |
| Number of references | 15 | 15 | 6 | 4 | 1 | 1 | 1 | |
| HADS | Mean (Minimum–Maximum) | 34.3 (23.6–41.4) | 13.1 (11.4–16.4) | 8.4 (8.1–8.6) | ||||
| Number of references | 6 | 6 | 2 | |||||
| GHQ | Mean (Minimum–Maximum) | 39.6 (30.3–50.9) | 13.0 (8.5–25.9) | 9.2 (8.6–9.8) | ||||
| Number of references | 8 | 8 | 3 | |||||
| Total | Mean (Minimum–Maximum) | 30.4 (12.6–50.8) | 11.3 (4.4–26.9) | 8.7 (5.0–13.4) | 6.9 (3.9–11.1) | 6.3 (3.6–9.4) | 4.9 (3.6–6.7) | 4.0 (3.6–4.9) |
| Number of references | 61 | 61 | 32 | 22 | 14 | 4 | 3 | |
Figure 1.
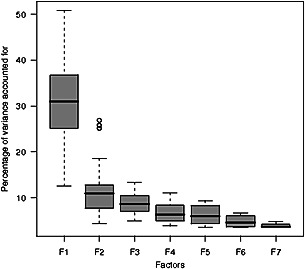
Box‐plot of the percentage of variance accounted for by each factor, according to the factor rank in the scale, in all the references.
The loadings matrix was present in 95.1% (58) of the references. The mean of the salient loadings was 0.626 with a median (med) of 0.636 and an interquartile range (IQR) of [0.587; 0.662]. This mean was 0.635 (med = 0.642, IQR = [0.601; 0.671]) when the method of factor extraction was PCA (80.3% – 49 – of the references) and 0.593 (med = 0.601, IQR = [0.545; 0.637]) in the case of EFA. The orthogonal rotation method was used in 63.9% (39) of the references and the values of factor inter‐correlations were reported in 34.4% (21) which represented 51 values (mean = 0.356, med = 0.33, IQR = [0.155; 0.535]). Concerning the p/M ratio, on average 7.1 items loaded on each factor in the scale (med = 6, IQR = [5; 10.5]) but this number varied depending on the number and the rank of the factors present within the scale as is shown in Table 3.
Table 3.
Mean of the percentages of items per factor (IQR, interquartile range)
| Number of factors in the scale | Factors | |||||||
|---|---|---|---|---|---|---|---|---|
| F 1 | F 2 | F 3 | F 4 | F 5 | F 6 | F 7 | ||
| 2 | Mean | 55.7 [50.0–59.2] | 39.0 [33.3–42.9] | |||||
| IQR | ||||||||
| 3 | Mean | 43.2 [40.4–49.4] | 34.8 [27.8–41.3] | 20.2 [16.7–24.1] | ||||
| IQR | ||||||||
| 4 | Mean | 29.1 [27.0–33.0] | 26.6 [22.9–32.2] | 19.3 [16.3–20.6] | 20.3 [14.8–23.7] | |||
| IQR | ||||||||
| 5 | Mean | 22.6 [20.0–25.8] | 20.1 [16.7–22.5] | 15.7 [13.3–19.2] | 16.7 [16.7–19.7] | 15.1 [12.7–16.7] | ||
| IQR | ||||||||
| 6 | Mean | 16.7 [—] | 22.2 [—] | 16.7 [—] | 16.7 [—] | 11.1 [—] | 16.7 [—] | |
| IQR | ||||||||
| 7 | Mean | 24.1 [19.5–26.7] | 22.4 [20.2–25.2] | 12.5 [10.5–15.5] | 15.2 [13.3–16.9] | 12.1 [9.8–13.3] | 6.5 [5.0–8.1] | 7.1 [4.0–9.0] |
| IQR | ||||||||
Sample size influence on the quality of solutions obtained using PCA or EFA
Results using artificial data
Choice of the parameter values for the simulation models: The determination of λ was based on the literature review so that λ was fixed at 0.6. Determination of the pm values was based on the percentages shown in Table 3. For example, in the three‐factor model, the largest integer not greater than p × 0.45 was chosen as the value for p 1, the largest integer not greater than p × 0.35 as the value for p 2 and the remaining items loaded on the third factor. As regards the values of factor inter‐correlations, they were set at 0.45 in the two‐factor model, at 0.45 for cor(F 1,F 2) and 0.35 for the two other inter‐correlations in the three‐factor model and finally, in the four‐factor model, at 0.45 for cor(F 1,F 2), cor(F 2,F 4) and cor(F 1,F 4) and 0.35 for the three other inter‐correlations. Figure 2 shows the path diagram for the three‐factor simulation model with 10 items.
Figure 2.
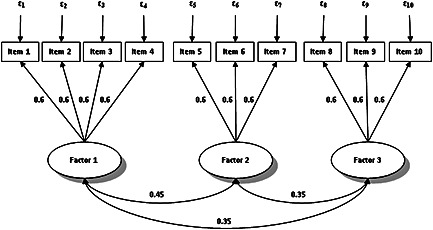
Path diagram for the three‐factor simulation model with 10 items.
Criteria of quality of the factor solutions: To reduce amounts of data presented in the results, only the details concerning the three criteria σλ, R% and W% in the case of a three‐factor scale are shown. Table 4 presents results when PCA was performed and Table 5 when it was EFA. All three criteria, σλ < 0.05, R% > 90% and W% < 1% were met when N = 500 if the scale contained less than 25 items, and when N = 300 if the scale contained 25 items or more in the case of PCA. When EFA was performed, N needed to be larger to reach the thresholds: 1000 if the scale contained less than 20 items, 500 if there were 25 items or more. For a two‐factor scale, on the whole, N could be smaller to meet the thresholds: 300 unless the scale contained less than 30 items and EFA was used, in which case N needed to be 500. In contrast, with both methods of factor analysis, a higher N value (500) was necessary when the scale contained four factors (and the criteria were not satisfied when N = 1000 in the case of EFA and p below 20). Concerning the percentage of simulations where Heywood cases occurred when EFA was performed, it was always under 2% whatever the number of factors in the scale with these values of N.
Table 4.
Values of the three criteria after PCA in the case of a three‐factor scale
| Sample size | Number of items | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 10 | 15 | 20 | 25 | 30 | 35 | 40 | 45 | ||
| 50 | σλ | 0.182 | 0.161 | 0.144 | 0.136 | 0.130 | 0.127 | 0.124 | 0.123 |
| R% | 48.4 | 48.5 | 51.1 | 50.7 | 51.3 | 51.5 | 50.6 | 49.5 | |
| W% | 9.3 | 6.5 | 4.4 | 3.4 | 2.7 | 2.3 | 2.1 | 1.9 | |
| 100 | σλ | 0.111 | 0.097 | 0.092 | 0.088 | 0.087 | 0.086 | 0.084 | 0.083 |
| R% | 88.8 | 92.6 | 94.6 | 95.9 | 96.4 | 97.1 | 96.9 | 97.1 | |
| W% | 1.5 | 0.6 | 0.3 | 0.2 | 0.1 | 0.1 | 0.1 | 0.1 | |
| 150 | σλ | 0.081 | 0.075 | 0.072 | 0.071 | 0.069 | 0.069 | 0.068 | 0.068 |
| R% | 97.8 | 99.4 | 99.5 | 99.7 | 99.8 | 99.7 | 99.8 | 99.8 | |
| W% | 0.3 | 0.1 | — | — | — | — | — | — | |
| 200 | σλ | 0.067 | 0.063 | 0.062 | 0.061 | 0.060 | 0.059 | 0.059 | 0.059 |
| R% | 99.5 | 99.9 | 99.8 | 99.8 | 99.9 | 99.9 | 99.9 | 99.8 | |
| W% | 0.1 | — | — | — | — | — | — | 0.1 | |
| 300 | σλ | 0.052 | 0.050 | 0.051 | 0.049 | 0.049 | 0.049 | 0.048 | 0.048 |
| R% | 99.9 | 100.0 | 99.8 | 99.9 | 99.9 | 99.8 | 100.0 | 99.8 | |
| W% | 0.1 | — | 0.1 | — | — | 0.1 | — | — | |
| 500 | σλ | 0.039 | 0.039 | 0.039 | 0.039 | 0.038 | 0.037 | 0.037 | 0.038 |
| R% | 99.9 | 100.0 | 99.9 | 99.9 | 99.9 | 99.9 | 99.9 | 99.9 | |
| W% | — | — | — | — | — | — | — | — | |
| 1000 | σλ | 0.029 | 0.027 | 0.027 | 0.027 | 0.027 | 0.027 | 0.026 | 0.026 |
| R% | 99.9 | 100.0 | 100.0 | 99.9 | 100.0 | 99.9 | 100.0 | 100.0 | |
| W% | 0.1 | — | — | — | — | — | — | — | |
Note : σλ, standard deviation of the salient loadings obtained after rotation over the 10,000 simulations; R%, percentage of simulations in which all the items in the scale load on the right factor; W%, mean of percentages of items loading on the wrong factor in the scale after rotation over the 10,000 simulations ; —, < 5 × 10–2.
Table 5.
Values of the three criteria after EFA in the case of a three‐factor scale
| Sample size | Number of items | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 10 | 15 | 20 | 25 | 30 | 35 | 40 | 45 | ||
| 50 | σλ | 0.226 | 0.187 | 0.164 | 0.153 | 0.144 | 0.138 | 0.134 | 0.131 |
| R% | 31.1 | 34.9 | 40.9 | 43.7 | 45.3 | 47.3 | 47.1 | 46.7 | |
| W% | 14.9 | 10.5 | 6.6 | 4.8 | 3.5 | 2.8 | 2.4 | 2.1 | |
| 100 | σλ | 0.159 | 0.125 | 0.109 | 0.101 | 0.096 | 0.093 | 0.091 | 0.089 |
| R% | 70.7 | 86.3 | 92.7 | 95.0 | 95.8 | 96.5 | 96.6 | 96.9 | |
| W% | 4.4 | 1.3 | 0.4 | 0.2 | 0.1 | 0.1 | 0.1 | 0.1 | |
| 150 | σλ | 0.128 | 0.098 | 0.086 | 0.080 | 0.077 | 0.075 | 0.073 | 0.072 |
| R% | 89.8 | 98.7 | 99.4 | 99.7 | 99.6 | 99.8 | 99.7 | 99.8 | |
| W% | 1.3 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| 200 | σλ | 0.109 | 0.082 | 0.073 | 0.069 | 0.066 | 0.064 | 0.063 | 0.062 |
| R% | 96.4 | 99.8 | 99.8 | 99.9 | 99.9 | 99.9 | 99.9 | 99.9 | |
| W% | 0.4 | — | — | — | — | — | — | — | |
| 300 | σλ | 0.086 | 0.065 | 0.059 | 0.056 | 0.054 | 0.052 | 0.051 | 0.051 |
| R% | 99.6 | 99.9 | 99.9 | 99.9 | 99.9 | 99.9 | 100.0 | 99.9 | |
| W% | — | — | — | — | — | — | — | — | |
| 500 | σλ | 0.063 | 0.050 | 0.045 | 0.043 | 0.041 | 0.040 | 0.039 | 0.040 |
| R% | 99.9 | 99.9 | 100.0 | 99.9 | 100.0 | 99.9 | 100.0 | 99.8 | |
| W% | — | — | — | — | — | — | — | 0.1 | |
| 1000 | σλ | 0.043 | 0.034 | 0.032 | 0.030 | 0.029 | 0.028 | 0.028 | 0.027 |
| R% | 100.0 | 100.0 | 99.9 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | |
| W% | — | — | — | — | — | — | — | — | |
Note: σλ, standard deviation of the salient loadings obtained after rotation over the 10,000 simulations, R%, percentage of simulations in which all the items of the scale load on the right factor ; W%, mean of percentages of items loading on the wrong factor in the scale after rotation over the 10,000 simulations ; —, < 5 × 10–2.
In order to narrow the sample size required to meet the criteria, we interpolated values from the curves representing σλ in relation to N for the two methods of factor extraction, and each value of p and M. The junction between these curves and the line corresponding to σλ = 0.05 allowed the determination of the sample sizes required with a precision of 50 subjects. Results are summarized in Table 6. Numbers reported in Table 6 were always overestimated and at these sample sizes, the two other criteria were always met.
Table 6.
Sample size required to meet the three criteria thresholds for quality of factor solutions
| Method of factor extraction | Number of factors | Number of items | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 10 | 15 | 20 | 25 | 30 | 35 | 40 | 45 | ||
| PCA | 2 | 300 | 300 | 300 | 300 | 300 | 300 | 250 | 250 |
| 3 | 350 | 350 | 350 | 300 | 300 | 300 | 300 | 300 | |
| 4 | 400 | 400 | 350 | 350 | 350 | 350 | 350 | 350 | |
| EFA | 2 | 500 | 400 | 350 | 300 | 300 | 300 | 300 | 300 |
| 3 | 800 | 500 | 450 | 400 | 350 | 350 | 350 | 350 | |
| 4 | — | — | 600 | 500 | 450 | 400 | 400 | 400 | |
Note : —, >1000.
Accuracy of factor solutions: Figure 3 shows the relationship between μλ and N for each value of p and each method of factor extraction in the case of a three‐factor scale. When PCA was used, the smaller the number of items, the greater the distance from the expected value (λ = 0.6) μλ. There was little influence of N. Conversely, in the case of EFA, sample size had rather more influence and, whatever the number of items, all the curves tended towards the expected value as N increased. The shape of these curves was the same when there were two or four factors within the scale, but the overestimation of the value of the salient loadings was all the greater when M was greater in the case of PCA. Likewise, the sample size required to tend towards the expected value was also much greater when M was greater in the case of EFA.
Figure 3.
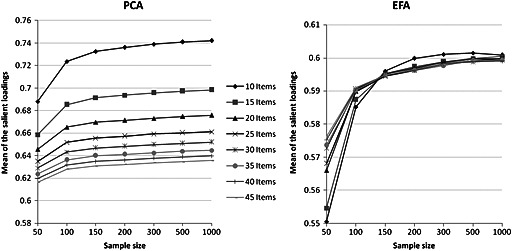
Mean of the values of the salient loadings after rotation on the 10,000 simulations in relation to sample size. Example of a three‐factor scale.
Standard deviation of the loadings using real data
Due to missing data, analyses were performed on 960 (95.1%) subjects for the BDI and 817 (81.0%) subjects for the HAMD. Parallel analysis suggested extracting one factor for the BDI and three factors for the HAMD. Figure 4 shows the mean of the standard deviations of the loadings over the 10,000 samples in relation to sample size in the case of PCA or EFA followed by a promax rotation for each scale. For the BDI, this mean was lower than 0.05 when the sample size was equal to or greater than 100 in the case of PCA. When EFA was used, the sample size needed to be larger, i.e. around 250, to obtain a mean lower than 0.05. In the case of the HAMD, even with 800 subjects the mean of the standard deviations of the loadings was higher than 0.05.
Figure 4.
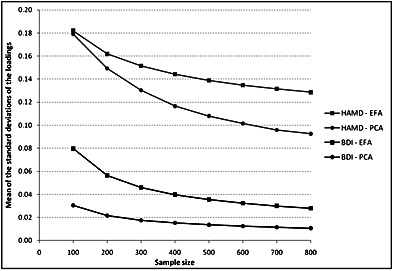
Mean of the standard deviations of the loadings over the 10,000 samples in relation to sample size in the case of Principal Component Analysis (PCA) or Exploratory Factor Analysis (EFA) followed by a promax rotation for the Beck Depression Inventory (BDI) and the Hamilton Depression Rating Scale (HAMD).
These rather unsatisfactory results found in the case of the HAMD, especially when EFA was performed, needed to be further investigated. We hypothesized that high standard deviations resulted from the possible presence of several underlying factor structures. To test this hypothesis, normal mixture modeling (function Mclust from the mclust package of the R software 2.6.2) was performed on the distribution of each salient loading of the HAMD for a sample size equal to 400 (10,000 samplings). The hypothesis of a unique component was systematically rejected and the number of components which optimized the Bayesian Information Criterion (BIC), ranged from two to six with a mode equal to three (the simulation program ruled out the possibility of an artificial phenomenon of label switching).
Influence of sample size on the precision of Cronbach's alpha coefficient
The half‐width of the 95% confidence interval of Cronbach's alpha coefficient in relation to N for the three expected values (α = 0.7, 0.8 and 0.9) is shown in Figure 5. Only the two extreme values for the number of items (p = 10 and 45) are represented because, as can be seen from Figure 5, there was little influence of p on the precision of Cronbach's alpha coefficient in the conditions studied here. A half‐width of 0.05 was reached when N = 300 for α = 0.7, 150 for α = 0.8 and only 50 for α = 0.9.
Figure 5.
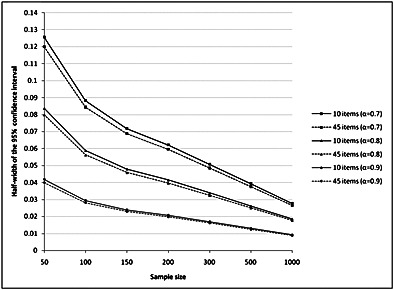
Half‐width of the 95% confidence interval of Cronbach's alpha coefficient for three expected values (α) in relation to the sample size and the number of items.
Discussion
These simulation studies, approaching as closely as possible the conditions usually met in practice during an internal validity study on a psychiatric scale, provide an answer to researchers facing the unavoidable issue of sample size in this field. When the factor structure underlying the instrument is clear, Table 6 gives the estimates for the numbers of subjects required to obtain stable and accurate solution in factor analysis in various usual conditions, defined by the number of items and the number of factors present within a psychiatric scale. These estimates can then be adapted to the results set out in Figure 5 according to the desired precision of the Cronbach's alpha coefficient.
As shown by the simulation study using artificial data, a sample size of 300 is generally required, but it needs to be increased in three cases: when the number of factors within the scale is large, when EFA is chosen as the method for factor extraction and when the number of items is small. One of the most important results of this study is this last point. Indeed, it shows how the use of the N/p ratio rule can be deleterious, particularly for scales with a small number of items. This is consistent with the conclusions drawn by other recent simulation studies on sample size in factor analysis. These studies did not however provide a simple answer to the sample size issue because of the wide ranges of the parameter values (λ, p, M) studied (Guadagnoli and Velicer, 1988; Hogarty et al., 2005; MacCallum et al., 1999; Mundfrom et al., 2005; Velicer and Fava, 1998). Another important result concerns the choice between the two different methods of factor extraction. Criticisms have been voiced in the literature against the use of the PCA. The common factor model rests on the assumption of the existence of latent variables that explain the inter‐item correlations observed. It is often remarked that PCA is not fully compatible with this assumption (Costello and Osborn, 2005; Fabrigar et al., 1999; Floyd and Widaman, 1995). Another criticism concerns the part of variance taken into account to estimate the loadings. In the common factor model, the shared variance of each item is partitioned from its unique variance and error variance whereas in PCA, this distinction is not made (Fabrigar et al., 1999; Ford et al., 1986; Widaman, 1993). Relationships between items are therefore overestimated and in the conditions occurring in psychiatry, loading estimates obtained by PCA are all the more overestimated when p is small and M large; and when N is large, this bias does not diminish (Figure 3). The use of EFA is therefore recommended in this field to obtain factor solutions with a lesser bias.
Considering the difficulty in recommending a general rule for sample size calculation valid in all the fields to which psychometric procedures apply, the literature review made it possible to determine an “average” pattern of factor structure characteristic of psychiatric scales. While a review is not as accurate as a formal meta‐analysis, it suggested that, in psychiatry, a particular factor structure is generally observed. Factors are correlated, salient loadings are close to 0.6 and there is a rather good factor overdetermination with an average p/M ratio greater than seven. The simulation of the categorical data was then performed on the basis of these characteristics and took into account different levels of floor and ceiling effects for each item. This was not the case in the previous simulation studies exploring sample size in factor analysis (Guadagnoli and Velicer, 1988; Hogarty et al., 2005; MacCallum et al., 1999; Mundfrom et al., 2005; Velicer and Fava, 1998; Velicer et al., 1982). The conditions encountered in psychiatry were therefore nearly reproduced in the artificial data. This helped to obtain results appropriate to this field that can be easily used in practice.
Concerning the limitations of the present results, two assumptions were made that could have artificially increased the strength of the artificial data as compared to real psychiatric data. One of these assumptions concerns the equality of the salient loadings. The absence of any significant influence of this on the quality of the factor solutions has been highlighted in a simulation study conducted by Velicer and Fava in 1998. The other assumption relates to simple structure (absence of cross‐loadings and non‐salient loadings set at zero). The simulation study based on real data suggests that the sample sizes recommended here could be underestimated. This is not certain. Different factor solutions were observed after resampling from the real data set. The standard deviations of loadings were thus high because of the melded fluctuations due to sampling and to the mixture of factor solutions. The interpretation of these standard deviations is not straightforward and, obviously, future studies are needed to further explore this area. At this point, we can conclude that sample sizes presented in the Table 6 represent minimal values determined from an idealized situation in which the common factor model is true. In practice, the stability of a solution obtained from real data can require a larger sample size. Of course, the present results are based on an “average” psychiatric scale and can vary according to the properties of a given instrument. However, certain elements of knowledge concerning p and M could help to obtain a clearer idea. For example, determination of the internal validity of a five‐factor psychiatric scale requires at least 400 subjects if PCA is chosen as the method of factor extraction, and 450 in the case of EFA. Finally, we chose to study the influence of sample size on the precision of Cronbach's alpha coefficient, but recent developments suggest more appropriate methods for reliability estimation, such as those based on non‐linear structural equation modeling (Green and Yang, 2009) or estimation of the greatest lower bound (Sijtsma, 2009a). However, debate is still open concerning which method should be used (Sijtsma, 2009b) and the Cronbach's alpha coefficient is by far the most used in practice.
Conclusion
The rule of the N/p ratio, which has already been criticized in previous studies on required sample sizes for factor analysis, is not upheld by the results of this simulation study, and researchers should refrain from using it. The validation of short scales (i.e. with a small number of items) does not warrant smaller sample size. If one's aim is to reveal the factor structure, under the hypothesis that the underlying common factor model is true, a minimum of 300 subjects is generally acceptable in the conditions encountered in the field of psychiatry. This sample size needs, however, to be larger when the expected number of factors within the scale is large. Furthermore, this study shows that, to obtain more accurate solutions, researchers should choose EFA as the method for factor extraction.
Declaration of interest statement
The authors have no competing interests.
Acknowledgements
The authors wish to thank the two reviewers for their helpful suggestions especially concerning the addition of simulations based on real data.
The common factor model postulates that each observed variable is a linear function of one or more common factors and one unique factor. Its fundamental equation can be written:
where yj is the vector of the N subjects' answers to the item j (j = 1 to p) and Fm the vector of the N subjects' non‐observable scores on the common factor m (m = 1 to M). Each item j loads on each common factor m with the factor loading λjm. The unique factor εj, for each item j is independent (⊥) from all the Fm and from the other ε(j'≠j) (Brown, 2006). In our simulation model, two hypotheses are set out. The first is the existence of a simple structure, i.e. each item loads on a single factor and all the non‐salient loadings are equal to zero. The second is that all salient loadings (λ) are equal. Therefore, if the p 1 first items load only onto the first factor F 1, the p 2 following items load onto F 2, …, the pm following onto Fm, …, and the pm last items onto FM, , then all the answers to a p item scale can be modeled as:
where ∀ j ∈ [1, p], εj ~ N(0,1) and εj ⊥ ε(j'≠j) and ∀ m ∈ [1, M], Fm ~ N(0,1) and Fm ⊥ εj
In this model, the coefficient λ′ is not directly equal to the salient loadings. Indeed, in order to preserve the variances of the yj equal to unity, standardization is required using the factor . Individual data can therefore be simulated in a matrix where each row represents the answers of one individual to all p items in the scale and each column represents the answers of the N individuals to one item. If i represents subjects (i = 1 to N), the answer of the subject i to the item j is:
To introduce correlations between factors in this simulation model, each factor is modeled using a term specific to each factor (fm ~ N(0,1)) and a term common to all factors (C ~ N(0,1)):
Thus, the proportions of each of these terms, am and bm, make it possible to control for the factor inter‐correlation levels with solely the constraint that to preserve the variances of factors equal to unity. A last stage is necessary to obtain a non‐symmetrical distribution of categorical data, as for data encountered in a real internal validity study on a psychiatric scale, for example, answers to a four‐point Likert scale. The conversion of the yij into integral numbers from one to four is performed using three breakpoints in their distribution N(0,1). For each item j, these three breakpoints are (−1 + δj), (0 + δj), and (1 + δj) where δj is drawn from a uniform distribution between [−0.5, 0.5] to introduce asymmetry and thus simulate floor and ceiling effects. The data simulation was performed using R software 2.6.2.; vectors εj, fm and C were generated using the function rnorm and δj using runif.
References
- Adachi N., Onuma T., Nishiwaki S., Murauchi S., Akanuma N., Ishida S., Takei N. (2000) Inter‐ictal and post‐ictal psychoses in frontal lobe epilepsy: A retrospective comparison with psychoses in temporal lobe epilepsy. Seizure, 9 (5), 328–335, DOI: 10.1053/seiz.2000.0413S1059-1311(00)90413-8 [pii] [DOI] [PubMed] [Google Scholar]
- Aleamoni L.M. (1973) Effects of size of sample on eigenvalues, observed communalities, and factor loadings. Journal of Applied Psychology, 58 (2), 266–269, DOI: 10.1037/h0035429 [DOI] [Google Scholar]
- Basker M., Moses P.D., Russell S., Russell P.S. (2007) The psychometric properties of Beck Depression Inventory for adolescent depression in a primary‐care paediatric setting in India. Child and Adolescent Psychiatry and Mental Health, 1 (1), 8–14, DOI: 1753‐2000‐1‐8 [pii]10.1186/1753‐2000‐1‐8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A.T. (1991) Relationship between the Beck Anxiety Inventory and the Hamilton Anxiety Rating Scale with anxious outpatients. Journal of Anxiety Disorders, 5 (3), 213–223, DOI: 10.1016/0887-6185(91)90002-B [DOI] [Google Scholar]
- Beck A.T., Ward C.H., Mendelson M., Mock J., Erbaugh J. (1961) An inventory for measuring depression. Archives of General Psychiatry, 4 (6), 561–571. [DOI] [PubMed] [Google Scholar]
- Bell M.D., Lysaker P.H., Beam‐Goulet J.L., Milstein R.M., Lindenmayer . J.P. (1994) Five‐component model of schizophrenia: Assessing the factorial invariance of the positive and negative syndrome scale. Psychiatry Research, 52 (3), 295–303, DOI: 0165‐1781(94)90075‐2 [pii] [DOI] [PubMed] [Google Scholar]
- Bonicatto S., Dew A.M., Soria J.J. (1998) Analysis of the psychometric properties of the Spanish version of the Beck Depression Inventory in Argentina. Psychiatry Research, 79 (3), 277–285, DOI: S0165‐1781(98)00047‐X [pii] [DOI] [PubMed] [Google Scholar]
- Bonilla J., Bernal G., Santos A., Santos D. (2004) A revised Spanish version of the Beck Depression Inventory: Psychometric properties with a Puerto Rican sample of college students. Journal of Clinical Psychology, 60 (1), 119–130, DOI: 10.1002/jclp.10195 [DOI] [PubMed] [Google Scholar]
- Brown T.A. (2006) Confirmatory Factor Analysis for Applied Research, New York, The Guilford Press. [Google Scholar]
- Castro‐Costa E., Uchoa E., Firmo J.O., Lima‐Costa M.F., Prince M. (2008) Association of cognitive impairment, activity limitation with latent traits in the GHQ‐12 in the older elderly. The Bambui Health and Aging Study (BHAS). Aging Clinical and Experimental Research, 20 (6), 562–568, DOI: 5323 [pii] [DOI] [PubMed] [Google Scholar]
- Cattell R.B. (1978) The Scientific Use of Factor Analysis in Behavioral and Life Sciences, New York, Plenum Press. [Google Scholar]
- Chapman L.K., Williams S.R., Mast B.T., Woodruff‐Borden J. (2009) A confirmatory factor analysis of the Beck Anxiety Inventory in African American and European American young adults. Journal of Anxiety Disorders, 23 (3), 387–392, DOI: S0887‐6185(08)00218‐1 [pii]10.1016/j.janxdis.2008.12.003 [DOI] [PubMed] [Google Scholar]
- Comrey A.L. (1978) Common methodological problems in factor analytic studies. Journal of Consulting and Clinical Psychology, 46 (4), 648–659, DOI: 10.1037/0022-006X.46.4.648 [DOI] [Google Scholar]
- Comrey A.L., Lee H.B. (1992) A First Course in Factor Analysis, Hillsdale, NJ, Lawrence Erlbaum Associates. [Google Scholar]
- Costello A.B., Osborn J.W. (2005) Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Practical Assessment, Research & Evaluation, 10 (7), 1–9. http://pareonline.net/getvn.asp?v=10&n=7 [13th October 2011]. [Google Scholar]
- Dagnan D., Jahoda A., McDowell K., Masson J., Banks P., Hare D. (2008) The psychometric properties of the Hospital Anxiety and Depressions Scale adapted for use with people with intellectual disabilities. Journal of Intellectual Disability Research, 52 (11), 942–949, DOI: JIR1053 [pii]10.1111/j.1365‐2788.2008.01053.x [DOI] [PubMed] [Google Scholar]
- Dawkins N., Cloherty M.E., Gracey F., Evans J.J. (2006) The factor structure of the Hospital Anxiety and Depression Scale in acquired brain injury. Brain Injury, 20 (12), 1235–1239, DOI: V041611313646066 [pii]10.1080/02699050601076414 [DOI] [PubMed] [Google Scholar]
- Everitt B.S. (1975) Multivariate analysis: The need for data, and other problems. The British Journal of Psychiatry, 126 (3), 237–240, DOI: 10.1192/bjp.126.3.237 [DOI] [PubMed] [Google Scholar]
- Fabrigar L.R., Wegener D.T., MacCallum R.C., Strahan E.J. (1999) Evaluating the use of exploratory factor analysis in psychological research. Psychological Methods, 4 (3), 272–299, DOI: 10.1037/1082-989X.4.3.272 [DOI] [Google Scholar]
- Fan X., Thompson B. (2001) Confidence intervals about score reliability coefficients, please: An EPM guideline editorial. Educational and Psychological Measurement, 61 (4), 517–531, DOI: 10.1177/0013164401614001 [DOI] [Google Scholar]
- Farrell G.A. (1998) The mental health of hospital nurses in Tasmania as measured by the 12‐item General Health Questionnaire. Journal of Advanced Nursing, 28 (4), 707–712, DOI: 10.1046/j.1365-2648.1998.00735 [DOI] [PubMed] [Google Scholar]
- Fedorowicz V.J., Falissard B., Foulon C., Dardennes R., Divac S.M., Guelfi J.D., Rouillon F. (2007) Factors associated with suicidal behaviors in a large French sample of inpatients with eating disorders. International Journal of Eating Disorders, 40 (7), 589–595, DOI: 10.1002/eat.20415 [DOI] [PubMed] [Google Scholar]
- Feldt L.S. (1965) The approximate sampling distribution of Kuder–Richardson reliability coefficient twenty. Psychometrika, 30 (3), 357–570, DOI: 10.1007/BF02289499 [DOI] [PubMed] [Google Scholar]
- Floyd F.J., Widaman K.F. (1995) Factor analysis in the development and refinement of clinical assessment instruments. Psychological Assessment, 7 (3), 286–299, DOI: 10.1037/1040-3590.7.3.286 [DOI] [Google Scholar]
- Ford J.K., MacCallum R.C., Tait M. (1986) The application of exploratory factor analysis in applied psychology: A critical review and analysis. Personnel Psychology, 39 (2), 291–314, DOI: 10.1111/j.1744-6570.1986.tb00583.x [DOI] [Google Scholar]
- Fresan A., De la Fuente‐Sandoval C., Loyzaga C., Garcia‐Anaya M., Meyenberg N., Nicolini H., Apiquian R. (2005) A forced five‐dimensional factor analysis and concurrent validity of the Positive and Negative Syndrome Scale in Mexican schizophrenic patients. Schizophrenia Research, 72 (2–3), 123–129, DOI: 10.1016/j.schres.2004.03.021 [DOI] [PubMed] [Google Scholar]
- Friedman S., Samuelian J.C., Lancrenon S., Even C., Chiarelli P. (2001) Three‐dimensional structure of the Hospital Anxiety and Depression Scale in a large French primary care population suffering from major depression. Psychiatry Research, 104 (3), 247–257, DOI: S0165‐1781(01)00309‐2 [pii] [DOI] [PubMed] [Google Scholar]
- Gabryelewicz T., Styczynska M., Pfeffer A., Wasiak B., Barczak A., Luczywek E., Androsiuk W., Barcikowska M. (2004) Prevalence of major and minor depression in elderly persons with mild cognitive impairment – MADRS factor analysis. International Journal of Geriatric Psychiatry, 19 (12), 1168–1172, DOI: 10.1002/gps.1235 [DOI] [PubMed] [Google Scholar]
- Galinowski A., Lehert P. (1995) Structural validity of MADRS during antidepressant treatment. International Clinical Psychopharmacology, 10 (3), 157–161, DOI: 10.1097/00004850-199510030-00004 [DOI] [PubMed] [Google Scholar]
- Gorenstein C., Andrade L., Vieira Filho A.H., Tung T.C., Artes R. (1999) Psychometric properties of the Portuguese version of the Beck Depression Inventory on Brazilian college students. Journal of Clinical Psychology, 55 (5), 553–562, DOI: [pii] [DOI] [PubMed] [Google Scholar]
- Gorsuch R.L. (1983) Factor Analysis, London, Lawrence Erlbaum Associates. [Google Scholar]
- Green S.A., Yang Y. (2009) Reliability of summed item scores using structural equation modeling: An alternative to coefficient alpha. Psychometrika, 74 (1), 155–167, DOI: 10.1007/S11336-008-9099-3 [DOI] [Google Scholar]
- Grunebaum M.F., Keilp J., Li S., Ellis S.P., Burke A.K., Oquendo M.A., Mann J.J. (2005) Symptom components of standard depression scales and past suicidal behavior. Journal of Affective Disorders, 87 (1), 73–82, DOI: S0165‐0327(05)00073‐X [pii] 10.1016/j.jad.2005.03.002 [DOI] [PubMed] [Google Scholar]
- Guadagnoli E., Velicer W.F. (1988) Relation of sample size to the stability of component patterns. Psychological Bulletin, 103 (2), 265–275, DOI: 10.1037/0033-2909.103.2.265 [DOI] [PubMed] [Google Scholar]
- Hamilton M. (1960) A rating scale for depression. Journal of Neurology, Neurosurgery & Psychiatry, 23 (1), 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankins M. (2008) The factor structure of the twelve item General Health Questionnaire (GHQ‐12): the result of negative phrasing? Clinical Practice and Epidemiology in Mental Health, 4 (4), 10, DOI: 1745‐0179‐4‐10 [pii]10.1186/1745‐0179‐4‐10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey P.D., Davidson M., White L., Keefe R.S., Hirschowitz J., Mohs R.C., Davis K.L. (1996) Empirical evaluation of the factorial structure of clinical symptoms in schizophrenia: Effects of typical neuroleptics on the brief psychiatric rating scale. Biological Psychiatry, 40 (8), 755–760, DOI: 0006‐3223(95)00486‐6 [pii]10.1016/0006‐3223(95)00486‐6 [DOI] [PubMed] [Google Scholar]
- Helm H.W. Jr., Boward M.D. (2003) Factor structure of the Beck Depression Inventory in a university sample. Psychological Reports, 92 (1), 53–61. [DOI] [PubMed] [Google Scholar]
- Hogarty K.Y., Hines C.V., Kromrey J.D., Ferron J.M., Mumford K.R. (2005) The quality of factor solutions in exploratory factor analysis: The influence of sample size, communality, and overdetermination. Educational and Psychological Measurement, 65 (2), 202–206, DOI: 10.1177/0013164404267287 [DOI] [Google Scholar]
- Honey G.D., Sharma T., Suckling J., Giampietro V., Soni W., Williams S.C., Bullmore E.T. (2003) The functional neuroanatomy of schizophrenic subsyndromes. Psychological Medicine, 33 (6), 1007–1018, DOI: 10.1017/S0033291703007864 [DOI] [PubMed] [Google Scholar]
- Hu Y., Stewart‐Brown S., Twigg L., Weich S. (2007) Can the 12‐item General Health Questionnaire be used to measure positive mental health? Psychological Medicine, 37 (7), 1005–1013, DOI: 10.1017/S0033291707009993 [DOI] [PubMed] [Google Scholar]
- Iwata N., Mishima N., Okabe K., Kobayashi N., Hashiguchi E., Egashira K. (2000) Psychometric properties of the State‐Trait Anxiety Inventory among Japanese clinical outpatients. Journal of Clinical Psychology, 56 (6), 793–806, DOI: [pii] [DOI] [PubMed] [Google Scholar]
- Iwata N., Mishima N., Shimizu T., Mizoue T., Fukuhara M., Hidano T., Spielberger C.D. (1998) Positive and negative affect in the factor structure of the State‐Trait Anxiety Inventory for Japanese workers. Psychological Reports, 82 (2), 651–656, DOI: 10.2466/PR0.82.2.651-656 [DOI] [PubMed] [Google Scholar]
- Jackson J.E. (1991) A User's Guide to Principal Components, New York, John Wiley & Sons. [Google Scholar]
- Jo S.A., Park M.H., Jo I., Ryu S.H., Han C. (2007) Usefulness of Beck Depression Inventory (BDI) in the Korean elderly population. International Journal of Geriatric Psychiatry, 22 (3), 218–223, DOI: 10.1002/gps.1664 [DOI] [PubMed] [Google Scholar]
- Kabacoff R.I., Segal D.L., Hersen M., Van Hasselt V.B. (1997) Psychometric properties and diagnostic utility of the Beck Anxiety Inventory and the State‐Trait Anxiety Inventory with older adult psychiatric outpatients. Journal of Anxiety Disorders, 11 (1), 33–47, DOI: S0887618596000333 [pii] [DOI] [PubMed] [Google Scholar]
- Kay S.R., Sevy S. (1990) Pyramidical model of schizophrenia. Schizophrenia Bulletin, 16 (3), 537–545, DOI: 10.1016/0165-1781(94)90075-2 [DOI] [PubMed] [Google Scholar]
- Kilic C., Rezaki M., Rezaki B., Kaplan I., Ozgen G., Sagduyu A., Ozturk M.O. (1997) General Health Questionnaire (GHQ12 &GHQ28): Psychometric properties and factor structure of the scales in a Turkish primary care sample. Social Psychiatry and Psychiatric Epidemiology, 32 (6), 327–331, DOI: 10.1007/BF00805437 [DOI] [PubMed] [Google Scholar]
- Killgore W.D. (1999) Empirically derived factor indices for the Beck Depression Inventory. Psychological Reports, 84 (3 Pt 1), 1005–1013. [DOI] [PubMed] [Google Scholar]
- Lachar D., Bailley S.E., Rhoades H.M., Espadas A., Aponte M., Cowan K.A., Gummattira P., Kopecky C.R., Wassef A. (2001) New subscales for an anchored version of the Brief Psychiatric Rating Scale: Construction, reliability, and validity in acute psychiatric admissions. Psychological Assessment, 13 (3), 384–395, DOI: 10.1037/1040-3590.13.3.384 [DOI] [PubMed] [Google Scholar]
- Lancon C., Reine G., Llorca P.M., Auquier P. (1999) Validity and reliability of the French‐language version of the Positive and Negative Syndrome Scale (PANSS). Acta Psychiatrica Scandinavica, 100 (3), 237–243, DOI: 10.1111/j.1600-0447.1999.tb10851.x [DOI] [PubMed] [Google Scholar]
- Lee K.H., Harris A.W., Loughland C.M., Williams L.M. (2003) The five symptom dimensions and depression in schizophrenia. Psychopathology, 36 (5), 226–233, DOI: 10.1159/000073447 PSP2003036005226 [pii] [DOI] [PubMed] [Google Scholar]
- Lindenmayer J.P., Czobor P., Volavka J., Lieberman J.A., Citrome L., Sheitman B., McEvoy J.P., Cooper T.B., Chakos M. (2004) Effects of atypical antipsychotics on the syndromal profile in treatment‐resistant schizophrenia. The Journal of Clinical Psychiatry, 65 (4), 551–556. [DOI] [PubMed] [Google Scholar]
- Loo R. (1983) Caveat on sample sizes in factor analysis. Perceptual and Motor Skills, 56 (2), 371–374. [Google Scholar]
- Lopez‐Castedo A., Fernandez L. (2005) Psychometric properties of the Spanish version of the 12‐item General Health Questionnaire in adolescents. Perceptual and Motor Skills, 100 (3 Pt 1), 676–80. [DOI] [PubMed] [Google Scholar]
- Loza B., Kucharska‐Pietura K., Kopacz G., Debowska G. (2003) Factor structure of paranoid schizophrenia: A prospective study. Psychopathology, 36 (3), 132–141, DOI: 10.1159/000071258 PSP2003036003132 [pii] [DOI] [PubMed] [Google Scholar]
- Lykouras L., Oulis P., Psarros K., Daskalopoulou E., Botsis A., Christodoulou G.N., Stefanis C. (2000) Five‐factor model of schizophrenic psychopathology: How valid is it? European Archives of Psychiatry and Clinical Neuroscience, 250 (2), 93–100, DOI: 10.1007/s004060070041 [DOI] [PubMed] [Google Scholar]
- MacCallum R.C., Widaman K.F., Zhang S., Hong S. (1999) Sample size in factor analysis. Psychological Methods, 4 (1), 84–99, DOI: 10.1037/1082-989X.4.1.84 [DOI] [Google Scholar]
- Mundfrom D.J., Shaw D.G., Ke T.L. (2005) Minimum sample size recommendations for conducting factor analyses. International Journal of Testing, 5 (2), 159–168, DOI: 10.1207/s15327574ijt0502_4 [DOI] [Google Scholar]
- Munoz D.J., Chen E., Fischer S., Roehrig M., Sanchez‐Johnson L., Alverdy J., Dymek‐Valentine M., le Grange D. (2007) Considerations for the use of the Beck Depression Inventory in the assessment of weight‐loss surgery seeking patients. Obesity Surgery, 17 (8), 1097–1101, DOI: 10.1007/s11695-007-9185-0 [DOI] [PubMed] [Google Scholar]
- Nunnaly J.C. (1978) Psychometric Theory, New York, McGraw‐Hill. [Google Scholar]
- Olden M., Rosenfeld B., Pessin H., Breitbart W. (2009) Measuring depression at the end of life: Is the Hamilton Depression Rating Scale a valid instrument? Assessment, 16 (1), 43–54, DOI: 1073191108320415 [pii] 10.1177/1073191108320415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pallant J.F., Bailey C.M. (2005) Assessment of the structure of the Hospital Anxiety and Depression Scale in musculoskeletal patients. Health and Quality of Life Outcomes, 3 (12), 82, DOI: 1477‐7525‐3‐82 [pii] 10.1186/1477‐7525‐3‐82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker R.D., Flint E.P., Bosworth H.B., Pieper C.F., Steffens D.C. (2003) A three‐factor analytic model of the MADRS in geriatric depression. International Journal of Geriatric Psychology, 18 (1), 73–77, DOI: 10.1002/gps.776 [DOI] [PubMed] [Google Scholar]
- Peterson R.A. (1994) A meta‐analysis of Cronbach's coefficient alpha. Journal of Consumer Research, 21 (2), 381–391, DOI: 10.1086/209405 [DOI] [Google Scholar]
- Powell R. (2003) Psychometric properties of the Beck Depression Inventory and the Zung Self Rating Depression Scale in adults with mental retardation. Mental Retardation, 41 (2), 88–95, DOI: 10.1352/0047‐6765(2003)041 < 0088: PPOTBD > 2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- R Development Core Team . (2008) R: A Language and Environment for Statistical Computing, Vienna, R Foundation for Statistical Computing. [Google Scholar]
- Revelle W. (2008) R Documentation: Procedures for Personality, Psychometric, and Psychological Research, help pages for package ‘psych’ version 1.0‐58: Principal Axis Factor Analysis (function : fa): CRAN. http://www.r‐project.org/ [13th October 2011].
- Salamero M., Marcos T., Gutierrez F., Rebull E. (1994) Factorial study of the BDI in pregnant women. Psychological Medicine, 24 (4), 1031–1035. [DOI] [PubMed] [Google Scholar]
- Salokangas R.K., Honkonen T., Stengard E., Koivisto A.M. (2002) Symptom dimensions and their association with outcome and treatment setting in long‐term schizophrenia. Results of the DSP project. Nordic Journal of Psychiatry, 56 (5), 319–327, DOI: 10.1080/080394802760322079 [DOI] [PubMed] [Google Scholar]
- Sanchez‐Lopez M.P., Dresch V. (2008) The 12‐Item General Health Questionnaire (GHQ‐12): Reliability, external validity and factor structure in the Spanish population. Psicothema, 20 (4), 839–843. [PubMed] [Google Scholar]
- Serretti A., Jori M.C., Casadei G., Ravizza L., Smeraldi E., Akiskal H. (1999) Delineating psychopathologic clusters within dysthymia: A study of 512 out‐patients without major depression. Journal of Affective Disorders, 56 (1), 17–25, DOI: S0165‐0327(99)00056‐7 [pii] [DOI] [PubMed] [Google Scholar]
- Shek D.T. (1990) Reliability and factorial structure of the Chinese version of the Beck Depression Inventory. Journal of Clinical Psychology, 46 (1), 35–43, DOI: [DOI] [PubMed] [Google Scholar]
- Sijtsma K. (2009a) On the use, the misuse, and the very limited usefulness of Cronbach's alpha. Psychometrika, 74 (1), 107–120, DOI: 10.1007/S11336-008-9101-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sijtsma K. (2009b) Reliability beyond theory and into practice. Psychometrika, 74 (1), 169–173, DOI: 10.1007/S11336-008-9103-Y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A.B., Selby P.J., Velikova G., Stark D., Wright E.P., Gould A., Cull A. (2002) Factor analysis of the Hospital Anxiety and Depression Scale from a large cancer population. Psychology and Psychotherapy, 75 (Pt 2), 165–176. [DOI] [PubMed] [Google Scholar]
- Steer R.A., Beck A.T., Brown G. (1989) Sex differences on the revised Beck Depression Inventory for outpatients with affective disorders. Journal of Personal Assessment, 53 (4), 693–702, DOI: 10.1207/s15327752jpa5304_6 [DOI] [PubMed] [Google Scholar]
- Steer R.A., Kumar G., Ranieri W.F., Beck A.T. (1995) Use of the Beck Anxiety Inventory with adolescent psychiatric outpatients. Psychological Reports, 76 (2), 459–65. [DOI] [PubMed] [Google Scholar]
- Steer R.A., Rissmiller D.J., Ranieri W.F., Beck A.T. (1993) Structure of the computer‐assisted Beck Anxiety Inventory with psychiatric inpatients. Journal of Personal Assessment, 60 (3), 532–542, DOI: 10.1207/s15327752jpa6003_10 [DOI] [PubMed] [Google Scholar]
- Uslu R.I., Kapci E.G., Oncu B., Ugurlu M., Turkcapar H. (2008) Psychometric properties and cut‐off scores of the Beck Depression Inventory‐II in Turkish adolescents. Journal of Clinical Psychological Medicine S15 (3), 225–233, DOI: 10.1007/s10880-008-9122-y [DOI] [PubMed] [Google Scholar]
- Velicer W.F., Fava J.L. (1998) Effects of variable and subject sampling on factor pattern recovery. Psychological Methods, 3 (2), 231–251, DOI: 10.1037/1082-989X.3.2.231 [DOI] [Google Scholar]
- Velicer W.F., Peacock A.C., Jackson D.N. (1982) A comparison of component and factor patterns: A Monte Carlo approach. Multivariate Behavioral Research, 17 (3), 371–388, DOI: 10.1207/s15327906mbr1703_5 [DOI] [PubMed] [Google Scholar]
- Ventura J., Nuechterlein K.H., Subotnik K.L., Gutkind D., Gilbert E.A. (2000) Symptom dimensions in recent‐onset schizophrenia and mania: A principal components analysis of the 24‐item Brief Psychiatric Rating Scale. Psychiatry Research, 97 (2–3), 129–135, DOI: S0165178100002286 [pii] [DOI] [PubMed] [Google Scholar]
- Villalta‐Gil V., Vilaplana M., Ochoa S., Dolz M., Usall J., Haro J.M., Almenara J., Gonzalez J.L., Lagares C. (2006) Four symptom dimensions in outpatients with schizophrenia. Comprehensive Psychiatry, 47 (5), 384–388, DOI: S0010‐440X(06)00019‐8 [pii] 10.1016/j.comppsych.2006.01.005 [DOI] [PubMed] [Google Scholar]
- Wang Y.P., Andrade L.H., Gorenstein C. (2005) Validation of the Beck Depression Inventory for a Portuguese‐speaking Chinese community in Brazil. Brazilian Journal of Medical and Biological Research, 38 (3), 399–408, DOI: S0100‐879X2005000300011 [pii] /S0100‐879X2005000300011 [DOI] [PubMed] [Google Scholar]
- Werneke U., Goldberg D.P., Yalcin I., Ustun B.T. (2000) The stability of the factor structure of the General Health Questionnaire. Psychological Medicine, 30 (4), 823–829, DOI: 10.1017/S0033291799002287 [DOI] [PubMed] [Google Scholar]
- Widaman K.F. (1993) Common factor analysis versus principal component analysis: Differential bias in representing model parameters? Multivariate Behavioral Research, 28 (3), 263–311, DOI: 10.1207/s15327906mbr2803_1 [DOI] [PubMed] [Google Scholar]
- Woolrich R.A., Kennedy P., Tasiemski T. (2006) A preliminary psychometric evaluation of the Hospital Anxiety and Depression Scale (HADS) in 963 people living with a spinal cord injury. Psychology, Health & Medicine, 11 (1), 80–90, DOI: J07M627G23552610 [pii] 10.1080/13548500500294211 [DOI] [PubMed] [Google Scholar]


