Abstract
In recent years, e-cigarette use has become more popular. Until recently, it was considered safer than smoking. We report two cases of acute pulmonary illness associated with vaping, focusing on their histologic patterns.
Keywords: Acute lung injury, e-cigarettes, vaping
In recent years, the use of e-cigarettes has grown among young and adolescent populations in the USA. E-cigarettes are battery-operated devices that produce aerosol, and their use is referred to as vaping. This aerosol is generated by heating a liquid that usually contains nicotine, flavorings, and other chemicals. 1 Only a few recent reports discuss the histopathological changes in pulmonary illness caused by vaping. We report two cases with acute pulmonary illness associated with vaping, focusing on their histologic patterns.
CASE PRESENTATIONS
The first patient was a 31-year-old man with abdominal pain, nausea, and symptoms of pneumonia (fever, cough, and shortness of breath) with perihilar infiltrates on imaging for 2 weeks. He was vaping methamphetamines at the time of presentation. The second patient was a 27-year-old man with fever and cough for 4 days and extensive ground-glass opacities bilaterally on imaging. He had a recent history of using a vaping device. Serology and microbiology cultures for infectious etiology were negative in both cases. The first patient was discharged home on levofloxacin and the second on prednisone.
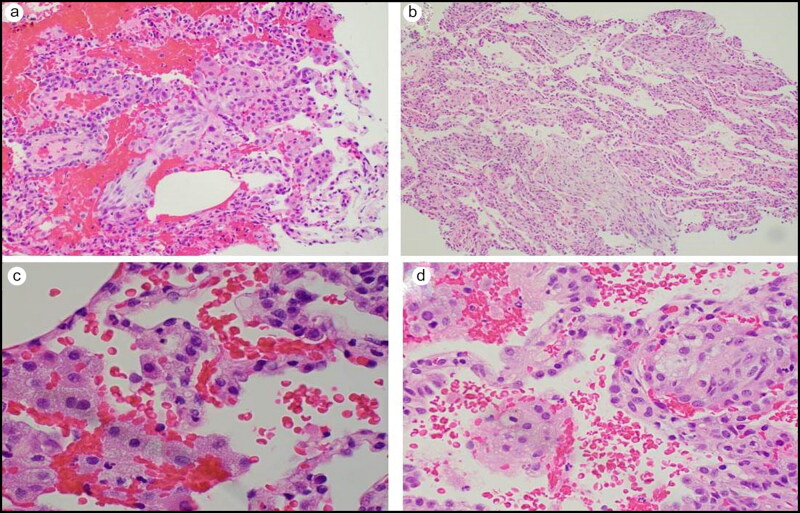
The biopsies from both patients had very similar histomorphology. Sections of the transbronchial lung biopsies showed fragments of alveolar lung parenchyma with an increased number of intra-alveolar macrophages, many of which had variable-sized clear vacuoles in the cytoplasm. In addition, there was slight thickening of the alveolar septa with increased fibroblasts. Fragments of intra-alveolar granulation tissue (fibroblast plugs) consistent with an organizing pneumonia were seen in several areas (Figure 1). Patchy areas with residual intra-alveolar organizing fibrin were also seen in both cases. Type II pneumocyte hyperplasia was present, as was focal, mild acute inflammation. There was no granulomatous reaction or significant eosinophilic infiltrate. Overall, the findings indicated an organizing pattern of acute lung injury with the distinct feature of vacuolated macrophages. Acid-fast and Gomori methenamine silver stains were negative for microorganisms in both cases.
Figure 1.
(a, b) Organizing pneumonia (fibroblast plugs in airspace, hematoxylin and eosin 200×). (c, d) Foamy macrophages in airspaces (hematoxylin and eosin 400×).
DISCUSSION
Commercially successful e-cigarettes were first introduced in 2003 and became available in the USA in 2006. 2 Since then, the popularity of e-cigarettes has risen dramatically, especially in recent years. 3 Compared to cigarettes, e-cigarettes were considered safer. 4 , 5 Recently, vaping has been identified as a public health issue. 1 , 6 E-cigarette–associated lung injury, also called vaping-associated pulmonary injury, was initially described in 2019 and is an acute or subacute respiratory illness that can be severe and life threatening. 7–9 Recently, published case series on lung biopsy in vaping discussed the Centers for Disease Control and Prevention criteria for a “confirmed case,” which are as follows:
Use of an e-cigarette or dabbing during the 90 days before symptom onset.
Presence of a pulmonary infiltrate on chest radiograph or ground-glass opacities on chest computed tomography.
Absence of pulmonary infection on initial workup. Minimum criteria include negative respiratory viral panel, influenza polymerase chain reaction, or rapid test if local epidemiology supports testing. All other clinically indicated respiratory infectious disease testing (e.g., urine antigen for Streptococcus pneumoniae and Legionella, sputum culture if productive cough, bronchoalveolar lavage culture if done, blood culture, human immunodeficiency virus–related opportunistic respiratory infections if appropriate) must be negative.
No evidence in the medical record of a plausible alternative diagnosis (e.g., cardiac, rheumatologic, or neoplastic process). 1
Both patients met the criteria.
Only a few articles have described the pathology in vaping-associated injury. From a histologic standpoint, the patterns commonly seen are diffuse alveolar damage and organizing pneumonia. 1 A spectrum of acute lung injury can be observed, including mucopolysaccharide-rich intraluminal plugs of proliferating fibroblasts within alveolar spaces and distal bronchioles (organizing pneumonia); diffuse alveolar septal thickening, type II pneumocyte hyperplasia, and hyaline membranes (diffuse alveolar damage); and abundant intra-alveolar fibrin accompanied by alveolar septal edema and variable degrees of organization with acute fibrinous and organizing pneumonia. Other patterns associated with vaping include acute alveolar hemorrhage, acute eosinophilic pneumonia, and hypersensitivity pneumonia. Some nonspecific findings such as foamy macrophages and foamy pneumocytes are also seen, which could also be due to other causes such as toxic fume injury or use of amiodarone. Some neutrophils and eosinophils were reported in recent case series. 1 , 6 , 10
Endogenous lipoid pneumonia is associated with macrophages with fine intracytoplasmic vacuoles within alveolar spaces. Exogenous lipoid pneumonia is associated with macrophages with coarse intracytoplasmic vacuoles in histology and involves interstitium by lipid vacuoles surrounded by foreign body–type giant cells. 1 No large lipid inclusions or other features of exogenous lipoid pneumonia have been observed in published cases. 1 , 6 A bronchoalveolar lavage fluid finding of lipid-laden macrophages staining positive for Oil Red O, suggestive of lipoid pneumonia, has been reported in a few cases. 11–13 This finding could be due to aspiration, obstruction, infection, adverse drug reaction, or some other causes and therefore is nonspecific and should not be used to diagnose acute lung injury associated with vaping. 14 , 15 Due to the nonspecific findings, lung biopsy might not be indicated in diagnosing vaping but can be a useful tool in ruling out other etiologies. 1
References
- 1. Mukhopadhyay S, Mehrad M, Dammert P, et al. Lung biopsy findings in severe pulmonary illness associated with e-cigarette use (vaping). Am J Clin Pathol. 2020;153:30–39. doi: 10.1093/ajcp/aqz182. [DOI] [PubMed] [Google Scholar]
- 2. Hajek P, Etter JF, Benowitz N, Eissenberg T, McRobbie H.. Electronic cigarettes: review of use, content, safety, effects on smokers and potential for harm and benefit. Addiction. 2014;109:1801–1810. doi: 10.1111/add.12659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Khan MS, Khateeb F, Akhtar J, et al. Organizing pneumonia related to electronic cigarette use: a case report and review of literature. Clin Respir J. 2018;12:1295–1299. doi: 10.1111/crj.12775. [DOI] [PubMed] [Google Scholar]
- 4. Itoh M, Aoshiba K, Herai Y, Nakamura H, Takemura T.. Lung injury associated with electronic cigarettes inhalation diagnosed by transbronchial lung biopsy. Respirol Case Rep. 2018;6:e00282. doi: 10.1002/rcr2.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Agustin M, Yamamoto M, Cabrera F, Eusebio R.. Diffuse alveolar hemorrhage induced by vaping. Case Rep Pulmonol. 2018; 2018:9724530. doi: 10.1155/2018/9724530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Butt YM, Smith ML, Tazelaar HD, et al. Pathology of vaping-associated lung injury. N Engl J Med. 2019;381:1780–1781. doi: 10.1056/NEJMc1913069. [DOI] [PubMed] [Google Scholar]
- 7. Ayden JE, Ghinai I, Pray I, et al. Pulmonary illness related to e-cigarette use in Illinois and Wisconsin—final report. N Engl J Med. 2020;382:903–916. doi: 10.1056/NEJMoa1911614. [DOI] [PubMed] [Google Scholar]
- 8. Centers for Disease Control and Prevention. Clinician outreach and communication activity. https://emergency.cdc.gov/newsletters/coca/081619.htm. Published August 2019. Accessed March 25, 2020.
- 9. Kligerman S, Raptis C, Larsen B, et al. Radiologic, pathologic, clinical, and physiologic findings of electronic cigarette or vaping product use–associated lung injury (EVALI): evolving knowledge and remaining questions. Radiology. 2020;294):491–505. doi: 10.1148/radiol.2020192585. [DOI] [PubMed] [Google Scholar]
- 10. Arter ZL, Wiggins A, Hudspath C, Kisling A, Hostler DC, Hostler JM.. Acute eosinophilic pneumonia following electronic cigarette use. Respir Med Case Rep. 2019;27:100825. doi: 10.1016/j.rmcr.2019.100825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dicpinigaitis PV, Trachuk P, Fakier F, Teka M, Suhrland MJ.. Vaping-associated acute respiratory failure due to acute lipoid pneumonia. Lung. 2020;198:31–33. doi: 10.1007/s00408-019-00277-6. [DOI] [PubMed] [Google Scholar]
- 12. Maddock SD, Cirulis MM, Callahan SJ, et al. Pulmonary lipid-laden macrophages and vaping. N Engl J Med. 2019;381:1488–1489. doi: 10.1056/NEJMc1912038. [DOI] [PubMed] [Google Scholar]
- 13. Viswam D, Trotter DS, Burge PS, Walters GI.. Respiratory failure caused by lipoid pneumonia from vaping e-cigarettes. BMJ Case Rep. 2018;2018:bcr-2018-224350. doi: 10.1136/bcr-2018-224350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rossi G, Cavazza A, Spagnolo P, et al. The role of macrophages in interstitial lung diseases. Eur Respir Rev. 2017;26(145):170009. doi: 10.1183/16000617.0009-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Colby TV. Pathologic aspects of bronchiolitis obliterans organizing pneumonia. Chest. 1992;102(1 Suppl):38S–43S. doi: 10.1378/chest.102.1_supplement.38s. [DOI] [PubMed] [Google Scholar]