Abstract
Bentall and valve-sparing root replacement (VSRR) procedures are established treatments for aortic root disease. We present a single-center retrospective analysis comparing outcomes of bioprosthetic Bentall (BB), mechanical Bentall (MB), and VSRR patients from November 2007 to October 2016. Survival analysis was performed to evaluate the composite endpoint of freedom from recurrent aortic insufficiency, reoperation, or death. Of the 170 patients, BB was performed in 36 patients, MB in 63 patients, and VSRR in 71 patients. For BB, MB, and VSRR, the mean age was 63.8, 45.5, and 49.2 years (P < 0.001), respectively. Additionally, significantly more patients in the MB group (n = 32, 50.8%, P < 0.001) than in the BB and VSRR groups had prior cardiac surgeries. Cardiopulmonary bypass time and cross-clamp time were significantly longer in the VSRR group (P = 0.04 and 0.0005, respectively). Despite the complexity of the procedure, VSRR patients had higher combined freedom from death and reoperation than patients in the BB or MB groups. Elective Bentall root replacement is an excellent option for patients with root disease. Patients undergoing Bentall tend to have more severe or emergent cases, making them unlikely candidates for VSRR. VSRR in experienced centers carries equivalent morbidity and mortality and improved survival.
Keywords: Bentall, root repair, root replacement, valve-sparing
The Bentall procedure has been considered the standard surgical technique for pathology of the sinuses of Valsalva and the aortic valve. 1 Two valve types are used for replacement of the pathologic valve: mechanical and bioprosthetic. The need for lifelong anticoagulation and the risks of structural valve deterioration and need for reoperation associated with bioprosthetic valves are major drawbacks of the Bentall procedure. Valve-sparing root replacement (VSRR) has emerged as a viable alternative to Bentall procedures for patients with aortic root aneurysms and favorable aortic cusp morphology. 2 , 3 VSRR is more technically demanding and has a higher risk of aortic insufficiency (AI) than Bentall procedures. 4 , 5 The aim of this study was to report the early and midterm outcomes of patients undergoing mechanical or bioprosthetic Bentall procedures or VSRR and determine if outcomes have improved.
METHODS
We reviewed data from November 2007 to October 2016 in 170 patients who underwent aortic root surgery at Baylor Scott & White–The Heart Hospital in Plano, Texas. The operative techniques were Bentall with bioprosthetic valve (BB) in 21.2% (n = 36), Bentall with mechanical valve (MB) in 37% (n = 63), and VSRR in 41.8% (n = 71).
All patients underwent surgical procedures via median sternotomy. Cardiopulmonary bypass was performed using single venous cannulation with mild hypothermia, unless mitral or tricuspid procedures were also planned. For myocardial protection, retrograde cardioplegia via direct coronary sinus cannulation and topical cooling with ice slush were used. Before closure of the aortotomy, low pressure testing was conducted on the left ventricular vent under direct vision and negative pressure. The surgeon also pressurized the aortic graft and gave pressurized cardioplegia to assess valve competence. Transesophageal echocardiogram off cardiopulmonary bypass was the final test used to fully assess valvular function.
The selection between the two root replacement techniques was generally based on the quality of the aortic valve leaflets and the surgeon’s opinion of the clinical situation. Generally, younger patients (<65 years) with normal aortic leaflets and a dilated aortic root underwent VSRR. The degree of preoperative AI was not a contributing factor in selection of operative technique. Patients with emergent cases and physiologic compromise, on the other hand, were less likely to receive VSRR. In the elective setting, operative techniques were discussed with the patient, and patient preferences were taken into consideration.
Survival analysis was performed to evaluate the composite endpoint of freedom from recurrent AI, reoperation, and death. Recurrence of AI postprocedure was defined as at least moderate AI. Follow-up mortality data were obtained from direct phone communication, electronic medical records, or query of the Social Security Death Index.
Categorical variables are presented as proportions, and continuous variables are presented as mean ± standard deviation or median with interquartile ranges. Comparisons were conducted using chi square or Fisher exact test for proportions and Student t test or Wilcoxon rank-sum test for continuous variables as applicable. P values < 0.05 were considered significant. Survival was estimated by Kaplan–Meier analysis with the log rank test for significance. The analyses were done using STATA 14.2. The Baylor Scott & White Health Research Institute institutional review board approved this study.
RESULTS
A total of 170 patients underwent aortic root procedures during the study period, with 36 patients undergoing BB, 63 undergoing MB, and 71 undergoing VSRR. Patients in the MB group were younger than those in the other two groups. The prevalence of Marfan syndrome was higher in the VSRR group (12.9%) compared with the other two groups. A total of 10 (15.9%) acute type A dissection patients underwent MB procedures, and none underwent VSRR. Median aortic root diameter was 51.5 mm (range, 31–90) in the VSRR group (Table 1).
Table 1.
Baseline characteristics of patients undergoing the Bentall procedure vs valve-sparing aortic root replacement a
| Variable | Bioprosthetic Bentall (n = 36) | Mechanical Bentall (n = 63) | VSRR (n = 71) | P value |
|---|---|---|---|---|
| Age (years) | 63.8 ± 10.4 | 45.5 ± 12.4 | 49.2 ± 12.0 | <0.001 |
| Men | 28 (78%) | 49 (78%) | 58 (82%) | 0.83 |
| BMI (kg/m2) | 26.8 ± 4.1 | 30.3 ± 6.0 | 28.5 ± 4.7 | 0.005 |
| Ejection fraction (%) | 57.5 (45–67.5) | 55 (15–62.5) | 60 (40–75) | 0.003 |
| Bicuspid aortic valve | 12 (33%) | 22 (35%) | 18 (25%) | 0.44 |
| Marfan syndrome | 1 (3%) | 1 (2%) | 9 (13%) | 0.02 |
| Acute aortic dissection | 5 (14%) | 10 (16%) | 0 | <0.001 |
| Aortic insufficiency | 0.22 | |||
| None | 3 (8%) | 12 (19%) | 12 (17%) | |
| Trace/trivial | 1 (3%) | 2 (3%) | 10 (14%) | |
| Mild | 4 (11%) | 9 (14%) | 12 (17%) | |
| Moderate | 10 (28%) | 14 (22%) | 14 (20%) | |
| Severe | 18 (50%) | 26 (41%) | 22 (32%) | |
| Aortic stenosis | 8 (22%) | 12 (19%) | 2 (3%) | 0.001 |
| Aortic root diameter (mm) | 50 (34–70) | 45.8 (25–67) | 51.5 (31–90) | 0.03 |
| Previous Ross | 1 (3%) | 9 (15%) | 7 (10%) | 0.18 |
| Previous CABG | 4 (11%) | 4 (6%) | 1 (1%) | 0.07 |
| Prior AV repair/replacement | 2 (6%) | 17 (27%) | 0 | <0.001 |
AV indicates aortic valve; BMI, body mass index; CABG, coronary artery bypass grafting; VSRR, valve-sparing root replacement.
Data are n (%), median (interquartile range), or mean (± 1 standard deviation).
Table 2 reviews operative data. Most procedures were performed electively (BB 83.3%, MB 77.8%, VSRR 95.8%; P = 0.007). Half of the patients (50.8%) had prior cardiac surgeries in the MB group, which was significantly higher than in the BB and VSRR groups (P < 0.001). Cardiopulmonary bypass time and cross-clamp time were significantly longer in the VSRR group (P = 0.04 and 0.0005, respectively).
Table 2.
Operative details of patients undergoing the Bentall procedure vs valve-sparing aortic root replacement*
| Variable | Bioprosthetic Bentall (n = 36) | Mechanical Bentall (n = 63) | VSRR (n = 71) | P value |
|---|---|---|---|---|
| Status | 0.007 | |||
| Elective | 30 (83%) | 49 (78%) | 68 (96%) | |
| Emergent | 3 (8%) | 8 (13%) | 0 | |
| Urgent | 3 (8%) | 6 (10%) | 3 (4%) | |
| Prior cardiac surgery | 4 (11%) | 32 (51%) | 11 (16%) | <0.001 |
| MV repair/replace | 0 | 3 (5%) | 0 | 0.11 |
| Pulmonic valve replacement | 1 (3%) | 2 (3%) | 2 (3%) | 1 |
| CABG | 4 (11%) | 4 (6%) | 1 (1%) | 0.06 |
| Aortic arch replacement | 0.2 | |||
| Hemiarch replacement | 9 (25%) | 17 (27%) | 9 (13%) | |
| Total arch replacement | 1 (3%) | 3 (5%) | 2 (3%) | |
| CPB (min) | 178 (102–403) | 175 (106–390) | 201 (68–323) | 0.04 |
| Cross-clamp time (min) | 137 (82–255) | 147.5 (81–354) | 179 (55–271) | 0.0005 |
CABG indicates coronary artery bypass grafting; CPB, cardiopulmonary bypass; MV, mitral valve; VSRR, valve-sparing root replacement.
Data are n (%) or median (interquartile range).
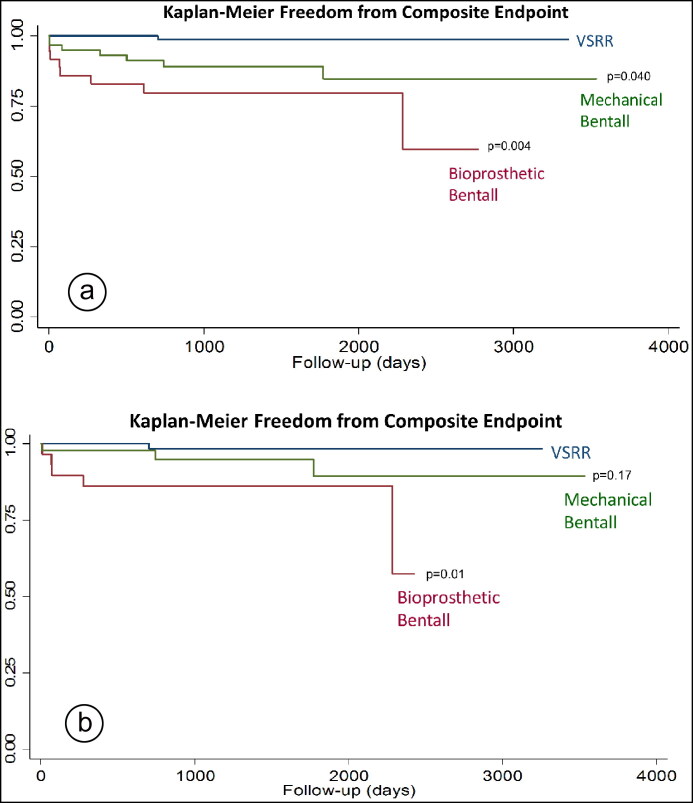
Clinical outcomes were evaluated as a whole and then specifically in the elective setting (Table 3). As a whole, both BB and MB groups had more cases of new-onset dialysis, permanent neurologic dysfunction, operative mortality (P = 0.04), pacemaker implantation, prolonged ventilator usage ≥ 24 h (P = 0.005), length of stay (P = 0.0001), and re-exploration for bleeding. In the elective setting, increased length of stay (P = 0.001) for the BB and MB cohorts was the only significant difference. Kaplan–Meier analysis for all three groups demonstrated a significant decrease in composite endpoint events in the VSRR group compared with the BB (P = 0.004) and MB (P = 0.04) groups during the follow-up period (Figure 1a). For those receiving elective operations, there was a trend for decreased composite endpoint events for VSRR compared with MB (P = 0.17) and a significant decrease when compared with BB (P = 0.01) during the follow-up period (Figure 1b).
Table 3.
Clinical outcomes of patients undergoing the Bentall procedure vs valve-sparing aortic root replacement*
| Variable | Bioprosthetic Bentall | Mechanical Bentall | VSRR | P value |
|---|---|---|---|---|
| All patients | 36 | 63 | 71 | |
| Reexploration for bleeding | 2 (6%) | 6 (10%) | 1 (1%) | 0.09 |
| Prolonged ventilator >24 h | 2 (6%) | 10 (16%) | 1 (1%) | 0.005 |
| New dialysis required | 1 (3%) | 3 (5%) | 0 | 0.16 |
| Permanent neurologic dysfunction | 0 | 1 (2%) | 0 | 0.58 |
| Pacemaker implantation | 1 (3%) | 5 (8%) | 3 (5%) | 0.56 |
| Length of stay (days) | 6 (0–17) | 6 (2–42) | 5 (3–35) | 0.0001 |
| Operative mortality | 3 (8%) | 2 (3%) | 0 | 0.04 |
| Elective only | 30 | 49 | 68 | |
| Re-exploration for bleeding | 2 (7%) | 2 (4%) | 1 (2%) | 0.29 |
| Prolonged ventilator >24 h | 2 (7%) | 4 (8%) | 1 (2%) | 0.19 |
| New dialysis required | 1 (3%) | 2 (4%) | 0 | 0.21 |
| Permanent neurologic dysfunction | 0 | 1 (2%) | 0 | 0.54 |
| Pacemaker implantation | 1 (4%) | 4 (9%) | 3 (5%) | 0.63 |
| Length of stay (days) | 6 (4–17) | 6 (4–42) | 5 (3–35) | 0.001 |
| Operative mortality | 1 (3%) | 1 (2%) | 0 | 0.29 |
VSRR indicates valve-sparing root replacement.
Data are n (%) or median (interquartile range).
Figure 1.
Kaplan–Meier freedom from composite endpoint for (a) all patients and (b) elective patients only. Composite endpoint included recurrent aortic insufficiency, reoperation, and mortality.
DISCUSSION
For patients with various aortic root pathologies, the composite graft procedure presented by Bentall and DeBono has been the gold standard. 1 Given technological and surgical advancements over the past several decades, the procedure is performed widely with low operative risk and good clinical outcomes. Although the Bentall procedure has been successful, associated factors including systemic thromboembolic events, need for lifelong anticoagulation, endocarditis, and gradual degeneration of bioprosthetic valves make it a less desirable choice. 6 This is particularly true for younger patients who will presumably have a longer postoperative lifespan. Valve-sparing aortic root procedures, originally introduced by David and Fiendel 2 and Sarsan and Yacoub, 3 are a viable alternative to the traditional Bentall procedure and have increased in use over the last few decades for patients with near-normal cusp structure. 7 , 8 By maintaining the native valve, VSRR reduces the associated morbidities of the classic Bentall procedure, which has led to its increased adoption, particularly with younger patients. 6 , 9
In our study, we evaluated 170 patients: 36 BB, 63 MB, and 71 VSRR. More patients undergoing VSRR had Marfan syndrome (12.9%) compared with the Bentall procedures (MB = 1.6%, BB 2.8%). Patients with acute aortic dissection exclusively underwent the Bentall procedures: 13.9% BB (n = 5) and 15.9% MB (n = 10) (Table 1). Operative mortality for all patients was also higher in the BB (8.3%) and MB (3.2%) cohorts compared with the VSRR (0%) cohort (Table 3). Our Bentall cohorts had more cases of new-onset dialysis, permanent neurologic dysfunction, pacemaker implantation, prolonged ventilator usage ≥ 24 h (P = 0.005), and re-exploration for bleeding (Table 3). Few of these differences reached statistical significance, so they likely reflect the presentation and overall physiologic state of patients selected for the procedure, which had a negative effect on perioperative outcomes. Patients in the Bentall cohorts had higher age and higher body mass index (Table 1). These patients also had higher percentages of prior cardiac surgery and acute cases (Table 2). VSRR is contraindicated in patients with aortic stenosis, and thus patients with that condition had to undergo one of the Bentall procedures. Conversely, the longer cross-clamp time and cardiopulmonary bypass time observed in the VSRR cohort can pose problems for low-volume centers or patients with multiple comorbidities and is likely due to the increased surgical difficulty and technical complexity of the procedure. 5 , 9 With the understanding of the observed differences in patient characteristics between the three cohorts, as well as the nature of the VSRR procedure, the VSRR cohort still outperformed the other cohorts in our composite outcome measure.
Several studies have shown either similar or slightly improved clinical outcomes when comparing VSRR with Bentall. Ouzounian et al analyzed 616 patients who underwent aortic root procedures over a 20-year period, with 251 cases of VSRR, 180 BB, and 183 MB. 10 They found that BB and MB cohorts experienced more long-term major adverse valve-related events (hazard ratio [HR] 3.4, P = 0.005; HR 5.2, P < 0.001, respectively) and increased cardiac mortality (HR 7.0, P = 0.001; HR 6.4, P = 0.003, respectively) when compared with the VSRR cohort. They also noted that patients undergoing VSRR (43.9%) had higher rates of Marfan syndrome when compared to BB (5.6%) and MB (10.4%) cohorts. 10 Although more patients with Marfan syndrome in our study underwent VSRR (12.9%, P = 0.02) compared with both BB and MB, clinical outcomes were relatively similar across operative techniques.
Many surgeons have also shown durable aortic valve function in patients undergoing VSRR for aortic root pathology; 11–16 however, there are still concerns about postoperative valvular function since limited long-term outcome data with large cohorts are available in the literature. 5 , 17 , 18 Lim et al analyzed 120 patients from 1999 to 2009 with moderate to severe preoperative AI, comparing VSRR (n = 48) to Bentall (n = 72). 19 They showed no operative mortality in the VSRR cohort, but 7 VSRR patients (14.6%) had to undergo reoperation for recurrent AI, and a significant number of other patients had AI ≥ grade 3 on echocardiography (P = 0.001). As a whole, the results at our hospital are comparable to those in the literature and support the idea that the benefits of VSRR outweigh the associated surgical risks. Additionally, the results present the characteristics of patients who were selected for each type of procedure.
Our study was a retrospective, nonrandomized, single-center study, and has all the limitations associated with this design. Given the limited sample size, we also were not able to perform a propensity-matched comparison while maintaining statistical power in our analyses; however, we attempted to minimize differences between cohorts and their length of follow-up. The VSRR cohort was not segmented into reimplantation and remodeling groups, although most procedures were reimplantation. Lower frequencies in the composite outcome measure for the BB and MB cohorts could be attributed to the preferential use of the Bentall procedure in high-risk patients or acute cases. 20 VSRR is a suitable treatment method in patients with aortic root dilation, with or without AI, surpassing all other operative techniques using our composite outcome measure. These results came in spite of the high technical difficulty and longer operation time. However, BB presents a viable alternative for patients in the elective setting with similar clinical outcomes. VSRR is ideal in subsets of patients where the associated factors of the Bentall procedure, including lifelong anticoagulants and thromboembolic events, are undesirable.
ACKNOWLEDGMENTS
Mohanad Hamandi and C. Ikenna Nwafor were supported by a generous grant from the Satish and Yasmin Gupta Family Foundation.
References
- 1. Bentall H, De Bono A.. A technique for complete replacement of the ascending aorta. Thorax. 1968;23(4):338–339. doi: 10.1136/thx.23.4.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. David TE, Feindel CM.. An aortic valve-sparing operation for patients with aortic incompetence and aneurysm of the ascending aorta. J Thorac Cardiovasc Surg. 1992;103(4):617–621, discussion 622. doi: 10.1016/S0022-5223(19)34942-6. [DOI] [PubMed] [Google Scholar]
- 3. Sarsam MA, Yacoub M.. Remodeling of the aortic valve anulus. J Thorac Cardiovasc Surg. 1993;105(3):435–438. [PubMed] [Google Scholar]
- 4. Price J, Magruder JT, Young A, et al. Long-term outcomes of aortic root operations for Marfan syndrome: a comparison of Bentall versus aortic valve-sparing procedures. J Thorac Cardiovasc Surg. 2016;151(2):330–338. doi: 10.1016/j.jtcvs.2015.10.068. [DOI] [PubMed] [Google Scholar]
- 5. Lee H, Cho YH, Sung K, et al. Clinical outcomes of root reimplantation and Bentall procedure: propensity score matching analysis. Ann Thorac Surg. 2018;106(2):539–547. doi: 10.1016/j.athoracsur.2018.02.057. [DOI] [PubMed] [Google Scholar]
- 6. Hammermeister K, Sethi GK, Henderson WG, Grover FL, Oprian C, Rahimtoola SH.. Outcomes 15 years after valve replacement with a mechanical versus a bioprosthetic valve: final report of the Veterans Affairs randomized trial. J Am Coll Cardiol. 2000;36(4):1152–1158. doi: 10.1016/S0735-1097(00)00834-2. [DOI] [PubMed] [Google Scholar]
- 7. Pacini D, Settepani F, De Paulis R, et al. Early results of valve-sparing reimplantation procedure using the Valsalva conduit: a multicenter study. Ann Thorac Surg. 2006;82(3):865–871, discussion 871–872. doi: 10.1016/j.athoracsur.2006.04.018. [DOI] [PubMed] [Google Scholar]
- 8. Aicher D, Langer F, Adam O, Tscholl D, Lausberg H, Schäfers H-J.. Cusp repair in aortic valve reconstruction: does the technique affect stability? J Thorac Cardiovasc Surg. 2007;134(6):1533–1538, discussion 1538–1539. doi: 10.1016/j.jtcvs.2007.08.023. [DOI] [PubMed] [Google Scholar]
- 9. Sabol F, Kolesar A, Jankajova M, et al. Aortic valve-sparing operation versus Bentall and mechanical aortic valve replacement-midterm results. Bratisl Lek Listy. 2014;115(5):292–299. doi: 10.4149/bll_2014_060. [DOI] [PubMed] [Google Scholar]
- 10. Ouzounian M, Rao V, Manlhiot C, et al. Valve-sparing root replacement compared with composite valve graft procedures in patients with aortic root dilation. J Am Coll Cardiol. 2016;68(17):1838–1847. doi: 10.1016/j.jacc.2016.07.767. [DOI] [PubMed] [Google Scholar]
- 11. David T. Aortic valve sparing operations: outcomes at 20 years. Ann Cardiothorac Surg. 2013;2(1):24–29. doi: 10.3978/j.issn.2225-319X.2012.11.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. David TE. Aortic valve sparing in different aortic valve and aortic root conditions. J Am Coll Cardiol. 2016;68(6):654–664. doi: 10.1016/j.jacc.2016.04.062. [DOI] [PubMed] [Google Scholar]
- 13. Matalanis G, Perera N.. Aortic valve sparing root surgery for Marfan syndrome. Ann Cardiothorac Surg. 2017;6(6):682–691. doi: 10.21037/acs.2017.11.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. de Kerchove L, Mosala NZ, Boodhwani M, El Khoury G.. How to perform valve sparing reimplantation in a tricuspid aortic valve. Ann Cardiothorac Surg. 2013;2:105–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Badiu CC, Deutsch MA, Sideris C, et al. Aortic root replacement: comparison of clinical outcome between different surgical techniques. Euro J Cardiothorac Surg. 2014;46(4):685–692. doi: 10.1093/ejcts/ezt647. [DOI] [PubMed] [Google Scholar]
- 16. Kerendi F, Guyton RA, Vega JD, Kilgo PD, Chen EP.. Early results of valve-sparing aortic root replacement in high-risk clinical scenarios. Ann Thorac Surg. 2010;89(2):471–478. doi: 10.1016/j.athoracsur.2009.10.030. [DOI] [PubMed] [Google Scholar]
- 17. Gaudino M, Lau C, Munjal M, Avgerinos D, Girardi LN.. Contemporary outcomes of surgery for aortic root aneurysms: a propensity-matched comparison of valve-sparing and composite valve graft replacement. J Thorac Cardiovasc Surg. 2015;150(5):1120–1129 .e1. doi: 10.1016/j.jtcvs.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 18. Zehr KJ, Orszulak TA, Mullany CJ, et al. Surgery of aneurysms of the aortic root: a 30-year experience. Circulation. 2004;110(11):1364–1371. doi: 10.1161/01.CIR.0000141593.05085.87. [DOI] [PubMed] [Google Scholar]
- 19. Lim JY, Kim JB, Jung S-H, Choo SJ, Chung CH, Lee JW.. Surgical management of aortic root dilatation with advanced aortic regurgitation: Bentall operation versus valve-sparing procedure. Korean J Thorac Cardiovasc Surg. 2012;45(3):141–147. doi: 10.5090/kjtcs.2012.45.3.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Patel ND, Weiss ES, Alejo DE, et al. Aortic root operations for Marfan syndrome: a comparison of the Bentall and valve-sparing procedures. Ann Thorac Surg. 2008;85(6):2003–2011. doi: 10.1016/j.athoracsur.2008.01.032. [DOI] [PubMed] [Google Scholar]