Abstract
Sarcoidosis and lymphoma are two separate entities that need to be considered in the differential diagnosis of lymphadenopathy. Rarely these two diseases may coexist, in which case there may arise a diagnostic challenge, especially when the available sample is limited. We report a case of occult mantle cell lymphoma arising in an individual with a long history of sarcoidosis.
Keywords: Mantle cell lymphoma, sarcoidosis, sarcoidosis-lymphoma syndrome
Sarcoidosis and lymphoma are considered mutually exclusive diseases. There are rare situations when these diseases coexist, particularly in patients with hilar/mediastinal lymphadenopathy. We report a case of occult mantle cell lymphoma following a long history of sarcoidosis.
CASE REPORT
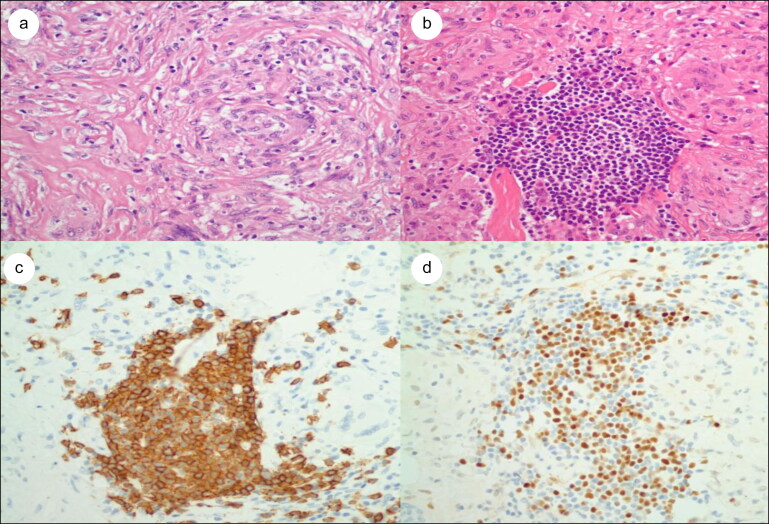
A 60-year-old woman had a 25-year history of sarcoidosis (initially diagnosed in a hilar lymph node) intermittently treated with steroids. In the 3 months prior to seeing her physician, she experienced a 15-pound weight loss with fatigue. She was mildly anemic with a hemoglobin of 10.3 g/dL and hematocrit of 30.8%. Her white blood cell count was 8.3 × 109/L with a normal differential. Her lactate dehydrogenase was elevated at 550 U/L (normal 140–280 U/L). A chest x-ray revealed calcified hilar nodes, mediastinal lymphadenopathy, and a new finding of a large pulmonary window lymph node. A core biopsy of this node (small biopsy) revealed noncaseating granulomas with a few interspersed lymphocytes and was consistent with sarcoid (Figure 1a). Flow cytometry revealed a minute 0.1% clonal population of CD20+, CD5+ B lymphocytes. Additional tissue was then requested, as the sample was too small to do further studies and a concurrent lymphoproliferative process needed to be further pursued. A subsequent biopsy again revealed predominantly noncaseating granulomas with small interspersed collections of lymphocytes, which were positive for CD20, CD5, and BCL1, indicative of mantle cell lymphoma (Figure 1b–d). The Ki-67 proliferation index was 20%, and the p53 stain was about 3%. Acid-fast stains were negative. No asteroid or Schaumann bodies were noted in the granulomas. A bone marrow biopsy revealed a small noncaseating granuloma but was negative for mantle cell lymphoma involvement. The lymphoma appeared to be limited to the mediastinal area. The patient is currently undergoing chemotherapy with hyper-CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone).
Figure 1.
(a) Granulomas with a few interspersed lymphocytes. Hematoxylin and eosin ×400. (b) Granulomas with a focal collection of lymphocytes. Hematoxylin and eosin ×400. (c) CD20 immunostain ×400. (d) BCL1 immunostain ×400.
DISCUSSION
Our patient had a 25-year history of sarcoidosis kept in control with intermittent steroid therapy. A 15-pound weight loss triggered an investigation, which resulted in a diagnosis of coexisting sarcoidosis and mantle cell lymphoma. This case was a diagnostic challenge as the initial biopsy showed largely noncaseating granulomas and obscured the neoplastic process. Only flow cytometry raised the suspicion of a possible concurrent lymphoma with a minute clonal B cell population, which was later confirmed as mantle cell lymphoma on a larger tissue specimen.
A report analyzing coexistent sarcoidosis and malignant lymphoproliferative disease suggests that this association is not fortuitous.1–5 Brincker and Wilbek6 reported an incidence of lymphoid disorders about 11.5 times higher than expected in a series of 2544 patients with sarcoidosis. The same authors in a subsequent study estimated that the incidence was 5.5 times higher than expected.1 The lymphoid disorders are thought to occur as a result of the immunologic abnormalities observed in sarcoid, including an increased number of CD4+ helper T cells in granulomatous tissue, decreased numbers of circulating T helper cells, and hyperactivity of the B cell system.7,8 There is also an increased antigenic presentation by dendritic cells with release of cytokine mediators such as interleukin-1 and tumor necrosis factor-α.7,8 The model that has been proposed is that sarcoid is a local mediated immune response induced by unknown antigens, resulting in activation of CD4+ T cells in an environment lacking significant regulatory CD8+ T cells. This response could lead to the formation of granulomas as cytokines released by the activated lymphocytes react and stimulate macrophages.1 An environment with defective regulation by suppressor T cells may result in the development of a lymphoid malignancy.2
Our case illustrates the difficulty that may exist in diagnosing a current lymphoma in the presence of sarcoidosis. Sarcoidosis can have prominent and extensive lymphadenopathy, and a “trigger event” may be necessary to justify a rebiopsy. The triggering point in our case was a 15-pound weight loss and fatigue, which prompted an x-ray that revealed the presence of a new large mediastinal lymph node. Even then the diagnosis was difficult, as the first biopsy revealed a predominantly granulomatous process and only flow cytometry suggested the presence of a minute monoclonal B cell process. Because of the presence of this small population of monoclonal B cells, a second biopsy was recommended, which resulted in a concurrent diagnosis of mantle cell lymphoma. In individuals with long-standing chronic active sarcoidosis, any significant change in the patient’s symptomatology, including new or expanding lymphadenopathy, might warrant further investigation.
References
- 1. Brincker H. The sarcoidosis-lymphoma syndrome. Br J Cancer. 1986;54(3):467–473. doi: 10.1038/bjc.1986.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Karakantza M, Matutes E, MacLennan K, O'Connor NT, Srivastava PC, Catovsky D.. Association between sarcoidosis and lymphoma revisited. J Clin Pathol. 1996;49(3):208–212. doi: 10.1136/jcp.49.3.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dunphy CH, Panella MJ, Grosso LE.. Low grade B cell lymphoma and concomitant extensive sarcoid-like granulomas. Arch Pathol Lab Med. 2000;124:1–6. [DOI] [PubMed] [Google Scholar]
- 4. Papanikolaou IC, Sharma OP.. The relationship between sarcoidosis and lymphoma. Eur Respir J. 2010;36(5):1207–1219. doi: 10.1183/09031936.00043010. [DOI] [PubMed] [Google Scholar]
- 5. Oskuei A, Hicks L, Ghaffar H, Hoffstein V.. Sarcoidosis-lymphoma syndrome: a diagnostic dilemma. BMJ Case Rep. 2017;10:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Brincker H, Wilbek E.. The incidence of malignant tumours in patients with respiratory sarcoidosis. Br J Cancer. 1974;29(3):247–251. doi: 10.1038/bjc.1974.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Müller-Quernheim J, Pfeifer S, Männel D, Strausz J, Ferlinz R.. Lung-restricted activation of the alveolar macrophage/monocyte system in pulmonary sarcoidosis . Am Rev Respir Dis. 1992;145(1):187–192. doi: 10.1164/ajrccm/145.1.187. [DOI] [PubMed] [Google Scholar]
- 8. Robinson BWS, Mclemore T, Crystal RG.. Gamma interferon is spontaneously released by alveolar macrophages and lung T lymphocytes in patients with pulmonary sarcoidosis. J Clin Invest. 1985;75(5):1488–1495. doi: 10.1172/JCI111852. [DOI] [PMC free article] [PubMed] [Google Scholar]