Abstract
Background
Tuberculosis is one of the ten major causes of mortality worldwide. The trend of increasing TB cases and drug resistance in India is very disturbing. The objectives of the study were to study the perspectives and opinions of different stakeholders on the status, challenges and the ways to tackle the issues of TB in India.
Methods
The online survey was done for the data collection from national and international experts. The data collection took place during October 2017. We received 46 responses.
Results
The experts had varied answers as to the menace of TB in India, effect of TB on individuals, family and society, failure of government plans in India, TB awareness campaign and ways to create awareness. Everyone believed that urgent action needs to be taken against the disease like improving the healthcare infrastructure of the country (improving the quality and quantity of medical facilities and doctors) and creating awareness about the TB.
Conclusion
Government of India is making lot of efforts to bring down the problems associated with TB through. In spite of this, there is a long way to go to achieve significant reduction in high incidence and prevalence of TB in India. Factors like lack of awareness and resources, poor infrastructure, increasing drug resistant cases, poor notification and overall negligence are the major challenges. If we eradicate poverty and undernourishment, educate the masses and eliminate the stigma attached with TB, we can hope for a disease free future.
Keywords: Awareness, Drug resistance, Health systems, India, Tuberculosis
Highlights
-
•
Tuberculosis is one of the ten major causes of mortality worldwide.
-
•
Many government plans have failed in bringing down the high incidence and prevalence of TB in India.
-
•
Major challenges: Lack of awareness, poor infrastructure, drug resistance, poor notification and overall negligence.
-
•
Eradication of poverty and undernourishment, education of people and elimination of stigma are must for a TB free future.
-
•
Current Covid-19 has given us an excellent opportunity to create awareness about TB in the community at various levels.
1. Introduction
Tuberculosis (TB), one of the most ancient diseases of mankind, is one of the ten major causes of mortality worldwide.1 It is an infectious disease caused by bacteria Mycobacterium tuberculosis. It usually affects lungs (Pulmonary TB) but can also affect other organs of the body. Pulmonary TB is an air borne disease. TB can be diagnosed by chest X-ray, sputum and other tests. Combinations of antibiotics are given for more than 6 months as a treatment. Vaccination with BCG (Bacille-Calmette-Guerin), early diagnosis and detection, proper and complete treatment, awareness, etc. can lower the burden of TB.
Poor socioeconomic status and living conditions are considered as strong risk factors linked with Latent Tuberculosis Infection in addition to malnourishment.2 BCG is the vaccine commonly available against TB. It does offer some protection against serious forms of TB in childhood but its protective effect wanes with age.1 Latent TB is also becoming a major issue in ageing population.
All countries and age groups are affected by TB but most cases (90%) in 2016 were in adults. Almost two-third was accounted for by eight developing countries with India contributing 27% of 10.4 million cases.3 , 4 In 2017, only 64% of the global estimated incident cases of TB were reported, the remaining 36% of ‘missing’ cases was undiagnosed, untreated or unreported. These ‘missing TB cases' have generated much hype for the challenges they present in achieving the End TB Strategy.5 Many people with TB (or TB symptoms) do not have access to adequate initial diagnosis. In many countries, TB diagnosis is still reliant on sputum microscopy, a test with known limitations.6
Wide spread misuse of anti-tubercular drugs has also resulted in emergence of drug resistant TB including Multi Drug Resistant TB (MDR-TB) and Extensively Drug Resistant TB (XDR-TB) globally. India has the highest incidence of new and MDR-TB cases in the world. It is difficult to diagnose MDR-TB and XDR-TB as compared to regular TB.7 , 8 TB treatment default, missing medical appointments for two consecutive months or more, is a serious problem not only for individuals but also for societies and health-care systems.9 An increasing burden of MDR-TB patients, especially in the young population with increased risk of transmission posing a major challenge in achieving TB elimination targets.10 In India, major challenges to control TB include poor primary health-care infrastructure in rural areas of many states, unregulated private health care, lack of political will and corrupt administration. WHO with its “STOP TB” strategy has given a vision to eliminate TB as a public health problem from the face of this earth by 2050.11
Since 2000, there has seen the emergence of new diagnostics and drugs for TB. A new and potent drugs such as Bedaquiline, Delamanid, Teixobactin have been evolved which may serve as a nice step forward, with a better outcome.12 However, these are yet to reach community, and access remains a major challenge for patients in low and middle income countries.13
The National Strategic Plan (2017–25) of India proposes bold strategies with commensurate resources to rapidly decline TB in the country by 2030. This is in line with the Global End TB targets and Sustainable Development Goals to attain the vision of a TB free India. The goal is to achieve a rapid decline in burden of TB, morbidity and mortality while working towards elimination of TB in India by 2025.14 India achieved the MDG targets of reducing the prevalence by half in 2015. In spite of this the trend of increasing TB cases and drug resistance in India is very disturbing. After collecting preliminary secondary information from the internet, journals, etc. about the disease, it was felt that there is a need to compile opinions of different stakeholders working in the healthcare field especially related to status and challenges of TB in India.
2. Methods
The objectives of the study were to study the perspectives and opinions of different stakeholders on the status, challenges and the ways to tackle the issues of TB in India. We decided to contact the clinicians, policy implementers and academic researchers as they play a pivotal role in controlling and preventing the disease. These stakeholders are also pioneers in reducing TB burden in India and their opinions will be useful in developing effective strategies.
A questionnaire for the survey was prepared and later on data was collected using available modern technology. The questionnaire was created on the online platform of www.surveymonkey.com. This online questionnaire made it easy for the survey to reach national and international experts. Social media (like email, Facebook, WhatsApp, etc) was utilized to send survey all across the world. The survey link (https://www.surveymonkey.com/r/H67S3YV) was sent to more than 1000 national as well as international experts and doctors working in diverse medical fields related to TB (academicians, researchers, clinicians, policymakers, implementers, etc). The online survey fulfilled the purpose of reaching out to many experts with variety of expertise like with the help of limited resources.
The data collection took place during October 2017. The responses were collected over the period of next 7–10 days. A semi-structured interview schedule was used comprising nine questions and mainly focusing on the effects of TB on society, the opinions of experts regarding what they felt was lacking in the country's efforts to reduce TB prevalence and the ways of creating more and better awareness about TB. The consent of each respondent was taken and the confidentiality was maintained as we did not ask them for their personal information.
The data was analyzed manually using MS Excel software. Data analysis largely followed the framework approach. The answers were entered in the worksheet. Data was coded, indexed and charted systematically to seek meaning from all of the data that was available. The data was categorized and sorted into patterns as the primary basis for organizing and reporting the study findings.
We received 46 responses. The respondents consisted of people from all age groups ranging from 24 years to 68 years and belonged to categories like Clinicians, Policy makers/implementers, Academic Researchers and others. Table 1 presents number of people belonging to various categories.
Table 1.
The category of respondents.
| Categories | No. of people |
|---|---|
| Clinician | 12 |
| Policy maker/implementer | 9 |
| Academician | 12 |
| Researcher | 8 |
| Other | 5 |
| Total | 46 |
Out of the 46 respondents, two were distinguished professors and academic researchers from USA. Three were from The World Health Organization (WHO) – Chief Medical Officer (TB) from an Asian country and two Medical Consultants from WHO–RNTCP (Revised National TB Control Program) India. The response was received from experts and specialists belonging to the Municipal Corporation of Greater Mumbai hospitals, District Health Officers, National Health Mission, The United Nations Children's Fund (UNICEF) and various other national and international organizations working actively in India. Apart from this, others were from diverse fields such as Neurologist, Laryngologist, Obstetrician and Gynecologists, Pathologists, Medical Students, PhD students, etc. from various reputed institutions like King's College (London), Holy Spirit Hospital, Bombay Hospital, Jaslok Hospital, Breach Candy Hospital, SRCC NH Children's Hospital, Wadia Children Hospital and so on.
3. Results
The experts had varied answers as to the menace of TB in India, effect of TB on individuals, family and society, failure of government plans in India, TB awareness campaign and ways to create awareness. The perspectives of policy makers, implementers and clinicians differed from that of the academicians and researchers but they also converged at a lot of points.
The respondents gave various perspectives to answer what made TB a menace all over the country. They mentioned social reasons like overcrowding, urbanization leading to congested cities, social problems like smoking and alcoholism, poor living conditions, unhygienic habits and poor nutrition are the major causes. On the other hand, few respondents stated that there are concerns related to health systems and services and said that poor public health conditions, lack of awareness about the TB amongst the masses, lack of universal access to healthcare, private sector malpractices, poor implementation of government health programs and poor drug supplies are the major problems. Few cited drug resistance as the cause of TB becoming a menace.
Effects of TB could be felt at individual, family, society and country level. Immunity of the person contracted with TB reduces which makes him/her susceptible to other diseases as well and reduces life expectancy. According to the respondents, the main effect of TB on the family was loss of income of the family due to which the family is slipped into poverty and their quality of life is affected. If the sole breadwinner of the family contracts the disease, then the family loses its only source of income and is forced to spend all its meager monetary resources on the treatment of the person. The family of the infected person also is at a high risk of contracting the contagious disease. Also, the social stigma attached to the disease can't be ignored. The effect of TB on society and country is such that it affects the National Economy at the macro level mainly due to decreased workforce. This leads to lower per capita income and a lower GDP.
According to the experts, the TB eradication programme of government has failed because of inadequate budgetary allocation to the programs, lack of proper infrastructure and manpower and poor implementation of programs. The various policies of the government fail to address the root cause of the problem. Also, the corruption in the healthcare system is hindering the policies from reaching the population. The Government policies need proper management. The TB program of the government will sink or swim with the Primary health program. Unless Primary Healthcare is improved and the problem of malnutrition is addressed, the program will fail to make any difference.
The experts say that each and every person in the country needs TB awareness and no section of the population must be exempted. But they feel that a special emphasis must be given on the poor and the marginalized sections of the society as these sections survive in poor and congested living conditions and the rate of malnutrition is high among them. The respondents feel that for the TB Awareness Campaign to reach every nook and corner of the country, innovative and creative methods have to be used so that the campaign catches everyone's attention. Use of mass media and social media will help in reaching the whole country. The use of local language for promoting the campaign will help in reaching out to the remotest places of India. The Awareness Campaign needs to be promoted by a celebrity or a famous personality so that people respond to the campaign. Also, awareness workshops should be held in schools and colleges so that the young generation is well informed about the disease. As one respondent mentioned, “The government should start an educational series on TB along the lines of “Mann ki Baat” by the Prime Minister of India.”
The additional efforts required to reduce the menace of TB include improving the overall scenario of public and primary healthcare in India. Universal access to healthcare and treating MDR-TB efficiently can substantially reduce the prevalence of TB. Improving the general health facilities, improved standard of living conditions, proper nutrition are some of the ways to tackle this deadly disease. Access to free or cheaper drugs and treatment, usage of quicker and more accurate diagnosis technology, involving private sector in the management of the TB Program will help to improve the existing infrastructure and healthcare services. These are some of the measures which will help tackle the problem of TB in the long run.
Finally, all the experts believe that urgent action needs to be taken against the disease. Improving the healthcare infrastructure of the country (improving the quality and quantity of medical facilities and doctors) should be the main motto the Government. Awareness and mass education about the various killer diseases is the need of the hour. TB is just like any other communicable disease. It needs to be tackled in a rational and scientific way. This is possible only if the whole country takes part in the campaign against TB menace.
4. Discussion
TB along with Acquired Immune Deficiency Syndrome (AIDS) and malaria rank among the top three fatal infectious diseases which pose threat to global public health, especially in middle and low income countries.15 Asia has the highest burden of TB in the world. Optimizing the diagnosis and treatment of TB is one of the key strategies for achieving the WHO ‘End TB’ targets.16 Majority of TB cases of resource-poor settings experience food insecurity, which impacts treatment adherence and outcomes. Additional food or cash assistance for this subgroup might improve food insecurity and thereby nutritional status.17 But again, this is a temporary measure. The root causes of TB, like poverty, poor socio-economic conditions, and improper hygienic practices are still neglected. Most of the developed countries have eliminated diseases like TB before the advent of anti-tubercular drugs through socio-economic improvement. India is earmarking funding for prevention and control of TB, but it is still mainly for diagnosis and treatment and not for primary prevention.
A significant proportion of the general population has incomplete knowledge on the routes of the spread of TB infection. Social stigma, such as reluctance to disclose about a family member being infected with the disease to others, also remains high. Imminent need for appropriate policy mechanisms for involving the private sector and raising consciousness through suitable advocacy measures is re-emphasized.18 Quality of TB care is suboptimal and must urgently be addressed; merely focusing on coverage of TB services is no longer sufficient. While the world awaits revolutionary vaccines, drugs and diagnostics, programmatic data indicate that much can be done to accelerate the decline of TB.5 Efforts are also being made to understand the genetic/molecular basis of target drug delivery and mechanisms of drug resistance.19
TB during childhood is also quite under diagnosed and under reported in India. Increased detection of childhood TB cases is essential to control TB in general population.20 Social determinants like overcrowding, lack of awareness and knowledge about TB, and malnutrition have to be tackled in order to combat TB. There is urgent need for advocating educational activities among the patients and the more vulnerable population about the cause, transmission, preventive measures, duration and dosage of therapy of TB with the help of DOTS providers and apt IEC (Information Education and Communication) materials. Very few patients i.e., only 3 lakh out of estimated 15 lakh are notified by private sector making the issue underrated.21 The current National Strategic Plan for TB Elimination (NSP 2017–25) has been worked out to provide nutrition support and reduce out of pocket expenditure of the patients and is aimed at ending TB by 2025.14 , 22
Successful control of TB globally will depend on strengthening TB control programs, wider access to rapid diagnosis and provision of effective treatment. Therefore, political and fund provider commitment is essential to curb the spread of TB.7 There is a pressing need for systematic monitoring of ongoing TB treatment in the private sector: both to cast light on the true scale of the problem, and to help monitor the progress of interventions currently being planned to address this problem.23 While transformative tools are being developed, high-burden countries like India will need to improve the efficiency of their health care delivery systems and ensure better uptake of new technologies. National TB programs must scale up the best diagnostics currently available, and use implementation science to get the maximum impact.6 It has been shown that Active Case Finding (ACF) as compared to Passive case finding significantly averts catastrophic costs due to TB among patients. ACF as a strategy could ensure financial protection of TB patients and limit their risk of poverty.24 In addition, TB elimination efforts need to focus on all forms of TB, including Extra Pulmonary TB, leaving no one behind, in order to realise the dream of ending TB.25
The End TB Strategy by WHO envisions a world free of tuberculosis by 2035. This requires reducing the global tuberculosis incidence from >125 cases per lakh people to <10 cases per lakh people within the next 15 years, which is quite a herculean task. Expanding testing and treatment of tuberculosis infection is critical to achieving this goal. India will require cost-effective and sustainable interventions aimed at tuberculosis.26 The WHO End TB Strategy also calls for a global reduction in the case fatality ratio below 5%. India accounts for a third of global TB deaths. Case fatality is a critical measure of the quality of TB care. Increased high-quality reporting on patient outcomes will help improve the evidence base on this topic.27
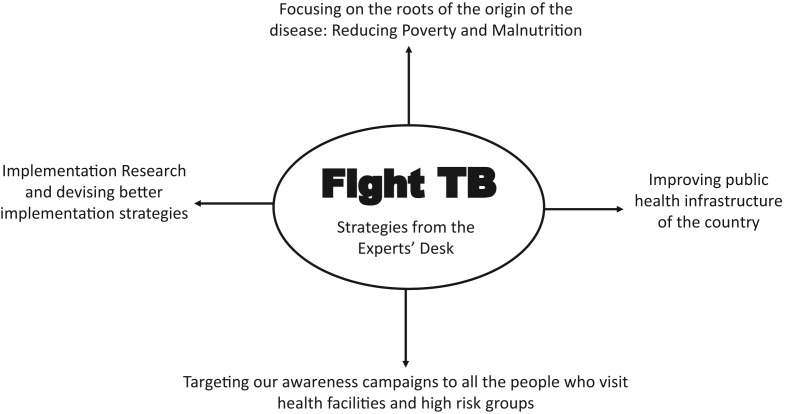
The foundation of end TB strategy includes integrated patient centric care and prevention, bold policies, supportive statement, intensified research and innovation which requires engaging a wide range of collaborators across government, communities and private sector.28 India needs to sustain the existing DOTS based program while introducing new components including services to address TB/HIV, treatment for MDR-TB, strengthening laboratory services and integrating TB services in both public and private healthcare sectors. Fig. 1 summarizes the strategies given by all the stakeholders/experts to Fight and End TB in India. The effectiveness of the program can be increased with focused efforts undertaken by Government of India in strengthening the primary healthcare system under National Health Mission through careful planning, thorough implementation, stable funding and innovations.
Fig. 1.
Experts' opinion on fight TB in India.
In India, TB is still one of the most commonly prevalent diseases as far as both morbidity and mortality is concerned. The incidence is quite high but it is only the tip of the iceberg. There are many missed cases either due to non-reporting by private sector or due to misdiagnosis. The next issue is inadequate and improper treatment of identified cases leading to increasing burden of drug resistant TB. Availability and affordability of sound diagnostic technology which helps in early diagnosis of TB cases (both non DR-TB and DR-TB cases) is missing from many parts of country. TB has a tremendous effect at individual, family and community level. This way it even affects the economy of a country. Also it is still neglected as India is more concentrating towards other conditions like Non Communicable Diseases and other emerging health issues.
5. Conclusion
Government of India is making lot of efforts to bring down the problems associated with TB through revised plans and their implementation across the country. In spite of this, there is a long way to go to achieve significant reduction in high incidence and prevalence of TB in India. Factors like lack of awareness and resources, poor infrastructure, increasing drug resistant cases (MDR TB and XDR TB), poor notification and overall negligence are the major challenges. Contagious disease like TB can victimize anyone. Even vaccinations do little to reduce its impact. If we eradicate poverty and undernourishment, educate the masses and eliminate the stigma attached with TB, we can hope for a disease free future. The current Coronavirus pandemic in 2020 has also given us excellent opportunity to create awareness about TB in the community at various levels.
Conflicts of interest
The authors have none to declare.
References
- 1.Yadav J., Verma S., Chaudhary D., Jaiwal P.K., Jaiwal R. Tuberculosis: current status, diagnosis, treatment and development of novel vaccines. Curr Pharmaceut Biotechnol. 2019;20(6):446–458. doi: 10.2174/1389201020666190430114121. [DOI] [PubMed] [Google Scholar]
- 2.Kashyap R.S., Nayak A.R., Husain A.A. Impact of socioeconomic status and living condition on latent tuberculosis diagnosis among the tribal population of Melghat: a cohort study. Lung India. 2016;33(4):372–380. doi: 10.4103/0970-2113.184868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pai M., Bhaumik S., Bhuyan S.S. India's plan to eliminate tuberculosis by 2025: converting rhetoric into reality. BMJ Glob Health. 2017;2(2) doi: 10.1136/bmjgh-2017-000326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO . World Health Organization; Geneva: 2016. Global Tuberculosis Report 2016. [Google Scholar]
- 5.Padayatchi N., Daftary A., Naidu N., Naidoo K., Pai M. Tuberculosis: treatment failure, or failure to treat? Lessons from India and South Africa. BMJ Glob Health. 2019;4(1) doi: 10.1136/bmjgh-2018-001097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pai M., Nicol M.P., Boehme C.C. Tuberculosis diagnostics: state of the art and future directions. Microbiol Spectr. 2016;4(5) doi: 10.1128/microbiolspec.TBTB2-0019-2016. [DOI] [PubMed] [Google Scholar]
- 7.Dash M. Drug resistant tuberculosis: a diagnostic challenge. J Postgrad Med. 2013;59(3):196–202. doi: 10.4103/0022-3859.118038. [DOI] [PubMed] [Google Scholar]
- 8.Thakur H. Drug resistance in TB control – a global & Indian situation. J Prevent Med. 2008;16(3–4):3–9. [Google Scholar]
- 9.Jittimanee S.X., Madigan E.A., Jittimanee S., Nontasood C. Treatment default among urban tuberculosis patients, Thailand. Int J Nurs Pract. 2007;13(6):354–362. doi: 10.1111/j.1440-172X.2007.00650.x. [DOI] [PubMed] [Google Scholar]
- 10.Sharma N., Khanna A., Chandra S. Trends & treatment outcomes of multidrug-resistant tuberculosis in Delhi, India (2009-2014): a retrospective record-based study. Indian J Med Res. 2020;151(6):598–603. doi: 10.4103/ijmr.IJMR_1048_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sandhu G.K. Tuberculosis: current situation, challenges and overview of its control programs in India. J Global Infect Dis. 2011;3(2):143–150. doi: 10.4103/0974-777X.81691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rawal T., Butani S. Combating tuberculosis infection: a forbidding challenge. Indian J Pharmaceut Sci. 2016;78(1):8–16. doi: 10.4103/0250-474x.180243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pai M., Furin J. Tuberculosis innovations mean little if they cannot save lives. Elife. 2017;6 doi: 10.7554/eLife.25956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khaparde S. The national strategic plan for tuberculosis step toward ending tuberculosis by 2025. J Mahatma Gandhi Inst Med Sci. 2019;24:17–18. [Google Scholar]
- 15.Singh R., Dwivedi S.P., Gaharwar U.S., Meena R., Rajamani P., Prasad T. Recent updates on drug resistance in Mycobacterium tuberculosis. J Appl Microbiol. 2020;128(6):1547–1567. doi: 10.1111/jam.14478. [DOI] [PubMed] [Google Scholar]
- 16.Paton N.I., Borand L., Benedicto J. Diagnosis and management of latent tuberculosis infection in Asia: review of current status and challenges. Int J Infect Dis. 2019;87:21–29. doi: 10.1016/j.ijid.2019.07.004. [DOI] [PubMed] [Google Scholar]
- 17.Ayiraveetil R., Sarkar S., Chinnakali P. Household food insecurity among patients with pulmonary tuberculosis and its associated factors in South India: a cross-sectional analysis. BMJ Open. 2020;10(2) doi: 10.1136/bmjopen-2019-033798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mazumdar S., Satyanarayana S., Pai M. Self-reported tuberculosis in India: evidence from NFHS-4. BMJ Glob Health. 2019;4(3) doi: 10.1136/bmjgh-2018-001371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sheikh B.A., Bhat B.A., Mehraj U., Mir W., Hamadani S., Mir M.A. Development of new therapeutics to meet the current challenge of drug resistant tuberculosis. Curr Pharmaceut Biotechnol. 2020;21 doi: 10.2174/1389201021666200628021702. [DOI] [PubMed] [Google Scholar]
- 20.Ruchi, Thakur H. Characteristics of childhood tuberculosis patients registered under RNTCP in Varanasi, Uttar Pradesh. Indian J Publ Health. 2013;57(1):36–39. doi: 10.4103/0019-557X.111367. [DOI] [PubMed] [Google Scholar]
- 21.Thakur H., Toshniwal M., Rangan S., Dholakia Y. National workshop on public private participation (PPP) for TB control in India--a brief review. Indian J Tubercul. 2008;55(4):224–226. [PubMed] [Google Scholar]
- 22.Saha I., Paul B. Private sector involvement envisaged in the national strategic plan for tuberculosis elimination 2017-2025: can tuberculosis health action learning initiative model act as a road map? Med J Armed Forces India. 2019;75(1):25–27. doi: 10.1016/j.mjafi.2018.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arinaminpathy N., Batra D., Maheshwari N. Tuberculosis treatment in the private healthcare sector in India: an analysis of recent trends and volumes using drug sales data. BMC Infect Dis. 2019;19(1):539. doi: 10.1186/s12879-019-4169-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muniyandi M., Thomas B.E., Karikalan N. Catastrophic costs due to tuberculosis in South India: comparison between active and passive case finding. Trans R Soc Trop Med Hyg. 2020;114(3):185–192. doi: 10.1093/trstmh/trz127. [DOI] [PubMed] [Google Scholar]
- 25.Lohiya S., Tripathy J.P., Sagili K. Does drug-resistant extrapulmonary tuberculosis hinder TB elimination plans? A case from Delhi, India. Trav Med Infect Dis. 2020;5(3) doi: 10.3390/tropicalmed5030109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moonan P.K., Nair S.A., Agarwal R. Tuberculosis preventive treatment: the next chapter of tuberculosis elimination in India. BMJ Glob Health. 2018;3(5) doi: 10.1136/bmjgh-2018-001135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huddart S., Svadzian A., Nafade V., Satyanarayana S., Pai M. Tuberculosis case fatality in India: a systematic review and meta-analysis. BMJ Glob Health. 2020;5(1) doi: 10.1136/bmjgh-2019-002080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.WHO . World Health Organization; Geneva: 2014. The End TB Strategy. [Google Scholar]