Abstract
To the best of our knowledge, there is no case report or data published regarding COVID pneumonitis presenting initially as pneumothorax.There are 3 case reports published to-date (May 30, 2020) reporting secondary pneumothorax as complication in later stages of Acute respiratory distress syndrome (ARDS) secondary to COVID-19 in non-ventilated patients. We present a case of COVID-19 disease presenting as tension pneumothorax after a week of symptoms and developing a second pneumothorax on the contralateral side post mechanical ventilation.
1. Background
Understanding of the nature of the SARS-CoV2 virus, giving rise to the COVID-19 pandemic, is rapid evolving. Several complications of COVID-19 have been described, which includes Acute respiratory distress syndrome, arrhythmias, acute cardiac injury and shock [1], thromboembolic complications [2,3], cytokine storm syndrome, liver injury, renal insufficiency and multiple organ dysfunction syndrome [4].
2. Case presentation
A 41-year-old british man was brought to the Accident and emergency department in respiratory distress with a 7 day history of shortness of breath and fevers. He was usually fit and well with no past medical history. He was an ex-smoker with a 25-pack year history, quitting smoking 10 years ago. On examination, his Oxygen saturations were 81% on air, picking up to 95% on 15L of oxygen administered by non-rebreathe bag. Respiratory rate 35 breaths per minute, heart rate 117 beats per minute, blood pressure 159/74 mmHg and temperature 39.7C. On chest auscultation, there was no audible air entry on left side. An urgent chest x-ray showed a large left sided tension pneumothorax (Fig. 1) with mediastinal shift. This was accompanied by a drop in systolic blood pressure to 107 mmHg. A 12Fr seldinger chest drain was inserted urgently.
Fig. 1.
Large Left sided Pneumothorax. Mild mediastinal shift to right. Right midzone consolidation also present.
This led to re-expansion of the left lung but a residual apical pneumothorax. Bloods showed CRP 117 mg/L, WCC 12.4 (10⁹L), lymphocytes 0.4 (10⁹L). Electrocardiogram showed sinus tachycardia with no ischaemic changes. After drain placement, he remained tachypnoeic with respiratory rate of 34 breaths per minute, but saturations were 96% on now decreased FiO2 of 40%. Overnight, he deteriorated clinically, with increased work of breathing, decreasing saturations, worsening type 1 respiratory failure and features suggestive of worsening pneumonitis clinically and radiologically. He was transferred to an intensive care unit (ICU) and intubated and mechanically ventilated on pressure support of 24 cmH2O and Positive end expiratory pressure (PEEP) of 10 cmH2O. The left sided seldinger chest drain stopped swinging and bubbling, therefore a new 20Fr surgical chest drain was inserted. The repeat chest x-ray showed re-expansion of left lung. He did not require any inotropic support. His nasopharyngeal swab results came back positive for SARS-CoV2.
Next day, patient underwent a further chest x-ray which showed a new right sided pneumothorax (Fig. 2).
Fig. 2.
New right sided Pneumothorax. Extensive bilateral patchy consolidation. Chest drain In situ on left side.
A seldinger chest drain was inserted and pressure support was decreased from 24 to 12cm H2O and PEEP decreased from 10 to 5 cmH20. The right lung re-expanded on chest x-ray (Fig. 3).
Fig. 3.
Bilateral chest drains in situ. The lung apices appears emphysematous. No definite residual pneumothorax. Bilateral mid and lower zone airspace shadowing.
The left chest drain for the initial pneumothorax continued to bubble suggestive of a persistent air leak. Two kPa of suction was applied. Given there were ongoing concerns about an air leak, the patient was ventilated on lower pressures which reduced alveolar recruitment and he subsequently needed a higher FiO2 of 85%–90% to keep pO2 over 8 kPa/oxygen saturations >90%.
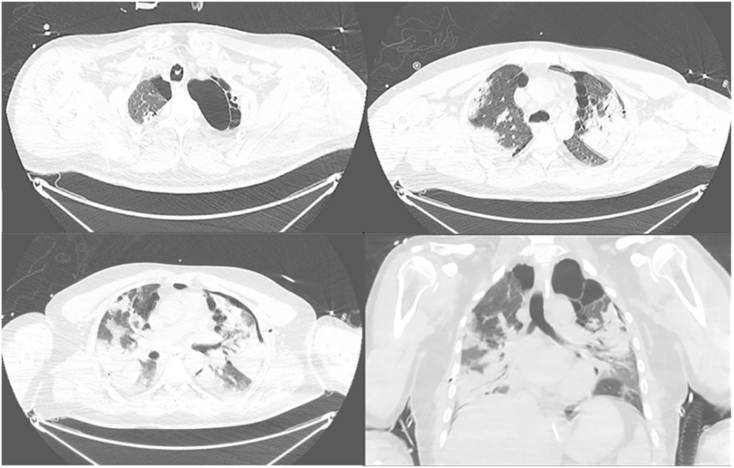
A CT chest scan (Fig. 4a–d) showed resolution of the right sided pneumothorax, but ongoing left mild anterior pneumothorax. There were bilateral apical air cysts, mainly subpleural, more so in the left lung, and paraseptal emphysema. There was extensive bibasal consolidation.
Fig. 4.
Bilateral predominantly apical lung air cysts mainly subpleural and more left sided. Bilateral extensive pneumonic consolidative patches more confluent in the bases. Residual left anterior pneumothorax.
After 6 days in ITU, he started to improve. The FiO2 of 90% was weaned down to 80%. Both chest drains were no longer swinging or bubbling, while on repeat chest x-rays, both lungs were fully re-expanded (Fig. 5).
Fig. 5.
Compared to previous CXR, mild reduction in consolidation. Both lungs fully expanded.
The drains were consecutively clamped for 24 hours and, with chest x-ray confirmation that the pneumothoraces had not recurred to suggest an air leak, the drains were then removed. A tracheostomy was inserted and he underwent weaning of ventilation.
3. Outcome and follow-up
Patient was successfully weaned off tracheostomy and was decannulated after 5 days. He was discharged home within a week after decannulation with a plan for follow up in clinic.
4. Discussion
Our patient initially presented with a left sided secondary spontaneous tension pneumothorax presumably secondary to undiagnosed emphysema as he had a 25 pack year smoking history but was asymptomatic. He was subsequently diagnosed with COVID pneumonitis progressing to ARDS requiring invasive ventilation. He then developed a right sided pneumothorax as a result of barotrauma secondary to mechanical ventilation.
Pneumothorax as a complication in COVID-19 has been reported in 1% of patients in 2 case series (1/91 and 1/99 patients), however its not clear if they were spontaneous or post mechanical ventilation [4,5].
Pneumothorax frequently complicates ARDS in mechanically ventilated patients or those with pre-existing lung disease (like emphysema) [6].
Duration of ARDS seems to be a factor in the incidence of pneumothorax, which can vary from 30% incidence within the early stages of ARDS (up to 1 week) to 46% in intermediate stage ARDS (between 1 and 2 weeks) and complicating a total of 87% of patients with late ARDS (beyond 2 weeks) [7].
The rising incidence of pneumothorax in relation to increasing duration of ARDS can perhaps be explained by underlying pathological mechanisms. Pathologically, ARDS evolves through three phases, Exudative (1–7 days), Proliferative (8–21 days) and Fibrotic (>21 days) [8]. Fibrotic phase is characterized by formation of microcystic airspaces, collagenous fibrosis and traction bronchiectasis [8].
These pathological phases can correlate with CT image findings. In Exudative/Acute stage, CT mainly shows wide-spread ground glass opacities and dense consolidations [9]. Proliferative/Intermediate stage is characterized by appearance of reticular opacities on background of alveolar opacities [11]. In Fibrotic/later stage, CT mainly shows air cysts, bullae, traction bronchiectasis and persistent ground glass opacities and reticulations [9].
The CT scan of our patient carried out after 2 weeks of illness also showed presence of bilateral air cysts and paraseptal emphysema. It is likely that rupture of these cysts was secondary to mechanical ventilation and resulted in a subsequent right sided pneumothorax.
An association with viral infection and pleural rupture has been described before. A study in Hong Kong of 123 SARS patients during a community outbreak of SARS-CoV in 2003 showed 13 patients developed spontaneous pneumomediastinum (including 1 with subcutaneous emphysema) which was thought to be due to free air leak from ruptured alveoli (due to diffuse alveolar damage) tracking up bronchovascular sheath towards the mediastinum [10]. Although pneumothorax is uncommon in pulmonary infection, it is reported in Pneumocystis Pneumonia (PCP) infection and cytomegalovirus pneumonitis [11,12].
Another study from Hong Kong during the coronavirus SARS outbreak of 2003 found that 6 out of 356 SARS-positive patients developed spontaneous pneumothorax at some point during hospital admission, occurring at a mean duration of hospital stay of 24.3 days [13]. All 6 cases had CT finding of diffuse bilateral infiltrates [13].
A review of 3 other case reports published during COVID-19 pandemic, with no pre-existing lung disease, and not treated with mechanical ventilation, revealed formation of cysts/Bullae complicated by pneumothorax after 3–4 weeks of illness [[14], [15], [16]].
These cases suggest that Pneumothorax in ARDS secondary to COVID19 presents after 3–4 weeks of illness, but can present early in patients with pre-existing lung disease. The cause is likely rupture of air cysts as seen previously in cases of ARDS.
It's not clear if this patient's first presentation as Tension pneumothorax has any relationship to COVID Pneumonitis or it was just co-incidental.
This data is very limited, but we are likely to learn more about the underlying pathological mechanisms and complications of COVID19 as our knowledge and experience of the condition advances.
CRediT authorship contribution statement
Ambreen Iqbal Muhammad: Conceptualization, Writing - original draft, Visualization. Emma Jane Boynton: Writing - original draft, Writing - review & editing. Samiha Naureen: Writing - review & editing.
Declaration of competing interest
None.
The authors whose names are listed immediately below certify that they have NO affiliations with or involvement in any organization or entity with any fi nancial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-fi nancial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
References
- 1.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in wuhan, China. JAMA. 2020 Mar 17;323(11):1061. doi: 10.1001/jama.2020.1585. [Internet] –9. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klok F.A., Kruip M.J.H.A., van der Meer N.J.M., Arbous M.S., Gommers D.A.M.P.J., Kant K.M. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020 Apr 10 doi: 10.1016/j.thromres.2020.04.013. https://pubmed.ncbi.nlm.nih.gov/32291094 Internet. S0049-3848(20)30120-1. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oxley T.J., Mocco J., Majidi S., Kellner C.P., Shoirah H., Singh I.P. Large-vessel stroke as a presenting feature of covid-19 in the young. N Engl J Med. 2020 Apr 28;(20):382. doi: 10.1056/NEJMc2009787. Internet. e60. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang F., Shi S., Zhu J., Shi J., Dai K., Chen X. Analysis of 92 deceased patients with COVID-19. J. Med. Virol. 2020 Apr 15;92:2511–2515. doi: 10.1002/jmv.25891. Internet. n/a(n/a). Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 395(10223):507–513. [DOI] [PMC free article] [PubMed]
- 6.Terzi E., Zarogoulidis K., Kougioumtzi I., Dryllis G., Kioumis I., Pitsiou G. Acute respiratory distress syndrome and pneumothorax. J. Thorac. Dis. October 2014;6(Suppl 4) doi: 10.3978/j.issn.2072-1439.2014.08.34. http://jtd.amegroups.com/article/view/3101 J Thorac Dis (Pneumothorax From Defin to Diagnosis Treat [Internet]. 2014; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gattinoni L., Bombino M., Pelosi P., Lissoni A., Pesenti A., Fumagalli R. Lung structure and function in different stages of severe adult respiratory distress syndrome. JAMA. 1994 Jun 8;271(22):1772–1779. doi: 10.1001/jama.1994.03510460064035. Internet. Available from: [DOI] [PubMed] [Google Scholar]
- 8.Tomashefski J.F. Pulmonary pathology OF acute respiratory distress syndrome. Clin Chest Med. 2000;21(3):435–466. doi: 10.1016/s0272-5231(05)70158-1. http://www.sciencedirect.com/science/article/pii/S0272523105701581 Internet. Available from: [DOI] [PubMed] [Google Scholar]
- 9.Zompatori M., Ciccarese F., Fasano L. Overview of current lung imaging in acute respiratory distress syndrome. Eur Respir Rev. 2014 Dec 1;23(134):519. doi: 10.1183/09059180.00001314. http://err.ersjournals.com/content/23/134/519.abstract Internet. LP – 530. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chu C.M., Leung Y.Y., Hui J.Y.H., Hung I.F.N., Chan V.L., Leung W.S. Spontaneous pneumomediastinum in patients with severe acute respiratory syndrome. Eur Respir J. 2004 Jun 1;23(6):802. doi: 10.1183/09031936.04.00096404. http://erj.ersjournals.com/content/23/6/802.abstract Internet. LP – 804. Available from: [DOI] [PubMed] [Google Scholar]
- 11.Tumbarello M., Tacconelli E., Pirronti T., Cauda R., Ortona L. Pneumothorax in HIV-infected patients: role of Pneumocystis carinii pneumonia and pulmonary tuberculosis. Eur Respir J. 1997 Jun 1;10(6):1332. doi: 10.1183/09031936.97.10061332. http://erj.ersjournals.com/content/10/6/1332.abstract Internet. LP – 1335. Available from: [DOI] [PubMed] [Google Scholar]
- 12.Olliff J.F.C., Williams M.P. Radiological appearances of cytomegalovirus infections. Clin Radiol. 1989;40(5):463–467. doi: 10.1016/s0009-9260(89)80245-4. http://www.sciencedirect.com/science/article/pii/S0009926089802454 Internet. Available from: [DOI] [PubMed] [Google Scholar]
- 13.Sihoe A.D.L., Wong R.H.L., Lee A.T.H., Lau L.S., Leung N.Y.Y., Law K.I. Severe acute respiratory syndrome complicated by spontaneous pneumothorax. Chest. 2004 Jun 1;125(6):2345–2351. doi: 10.1378/chest.125.6.2345. Internet. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang W., Gao R., Zheng Y., Jiang L. COVID-19 with spontaneous pneumothorax,pneumomediastinum and subcutaneous emphysema. J Travel Med. 2020 Apr 25 doi: 10.1093/jtm/taaa062. Internet. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun R., Liu H., Wang X. Mediastinal emphysema, giant Bulla, and pneumothorax developed during the course of COVID-19 pneumonia. Korean J Radiol. 2020 May;21(5):541–544. doi: 10.3348/kjr.2020.0180. Internet. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu K., Zeng Y., Xie P., Ye X., Xu G., Liu J. COVID-19 with cystic features on computed tomography: a case report. Medicine (Baltimore) 2020;99(18) doi: 10.1097/MD.0000000000020175. https://journals.lww.com/md-journal/Fulltext/2020/05010/COVID_19_with_cystic_features_on_computed.68.aspx Internet. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]