Abstract
Objective
To examine changes in outpatient visits for mental health and/or substance use disorders (MH/SUD) in an integrated healthcare organization during the initial Massachusetts COVID-19 surge and partial state reopening.
Methods
Observational study of outpatient MH/SUD visits January 1st-June 30th, 2018–2020 by: 1) visit diagnosis group, 2) provider type, 3) patient race/ethnicity, 4) insurance, and 5) visit method (telemedicine vs. in-person).
Results
Each year, January–June 52,907–73,184 patients were seen for a MH/SUD visit. While non-MH/SUD visits declined during the surge relative to 2020 pre-pandemic (−38.2%), MH/SUD visits increased (9.1%)—concentrated in primary care (35.3%) and non-Hispanic Whites (10.5%). During the surge, MH visit volume increased 11.7% while SUD decreased 12.7%. During partial reopening, while MH visits returned to 2020 pre-pandemic levels, SUD visits declined 31.1%; MH/SUD visits decreased by Hispanics (−33.0%) and non-Hispanic Blacks (−24.6%), and among Medicaid (−19.4%) and Medicare enrollees (−20.9%). Telemedicine accounted for ~5% of MH/SUD visits pre-pandemic and 83.3%–83.5% since the surge.
Conclusions
MH/SUD visit volume increased during the COVID surge and was supported by rapidly-scaled telemedicine. Despite this, widening diagnostic and racial/ethnic disparities in MH/SUD visit volume during the surge and reopening suggest additional barriers for these vulnerable populations, and warrant continued monitoring and research.
Keywords: Health care systems, COVID-19, Mental health, Substance use disorders, Disparities
1. Introduction
Disasters and recessions are associated with increases in distress and psychiatric disorders [[1], [2], [3], [4], [5], [6]]. Higher rates of depressive and anxiety disorders are a consistent finding [1,6]. Disasters are also associated with relapse among those with alcohol use disorders [4]; while economic recession has been associated with increased drug use disorders [6]. More recent research in the U.S. since the COVID-19 outbreak finds increased levels of psychological distress in terms of depression, anxiety, trauma, suicidal ideation [7,8] and substance use, including increased rates of opioid overdose [8,9].
Recognizing the imperative to assist providers in continuing to care for their patients, in March 2020 a variety of federal and state policies and regulations swiftly changed, aimed at facilitating rapid adoption of telemedicine [[10], [11], [12]]. In this context, telemedicine use increased significantly [10,13]. While there was early evidence suggesting that telemedicine was being quickly adopted in outpatient behavioral health care [13], at least one behavioral health provider type (psychiatrists) reported some challenging aspects of the transition to telemedicine [14].
Recent research documents the disproportionate health, health equity, socio-economic and psychological distress related to COVID-19 faced by racial and ethnic minorities in the U.S. [8,15]. While this new research related to COVID-19 highlights the additional vulnerability racial and ethnic minorities face in terms of mental health and/or substance use disorders (MH/SUD) and need for treatment access, this heightened need comes in the context of pre-existing documented racial and ethnic disparities in MH/SUD care. These include disparities in treatment access to or initiating MH/SUD care [[16], [17], [18], [19], [20], [21], [22], [23], [24]] and the adequacy and duration of that care [18,21,[25], [26], [27], [28]]. Further, the disparities have been observed even after controlling for clinical need, educational level, and poverty status [16,22].
In March 2020, Massachusetts became a focus of the COVID-19 pandemic, with an early and large COVID-19 outbreak—ranking third highest in U.S. cases per capita at the time [29]. Within weeks, a series of additional community stressors followed: state and federal declarations of emergency, closures of non-essential businesses, schools and child-care facilities, and a burgeoning unemployment rate [30]. The purpose of this research is to examine changes in outpatient visits for MH/SUD in a large Boston-area healthcare system before the initial COVID-19 pandemic medical surge, during the surge and community state of emergency, and initial state partial reopening periods, and to examine disparities by diagnosis and patient race/ethnicity. We examine outpatient visits for MH/SUD care across all providers in the health care system (i.e., specialty behavioral health, primary care, or non-behavioral health specialty care). Also, we examine the extent to which telemedicine was able to replace in-person MH/SUD care.
2. Methods
This study was approved by the Mass General Brigham Institutional Review Board. We used electronic health record (EHR) data to examine changes in outpatient visit volume in the healthcare system.
2.1. Setting
The provider organization is located primarily in Boston and surrounding communities in eastern Massachusetts. It includes academic medical centers, specialty hospitals (including a psychiatric hospital), community hospitals, community clinics and urgent care centers. It is the largest, non-profit healthcare system in Massachusetts and has an integrated EHR that includes all encounters occurring across its network of hospitals and community providers. On March 11th, 2020, the governor of Massachusetts declared a state of emergency and on March 16th, the system's clinics closed for non-urgent in-person care. On May 18th, 2020 the state began a partial reopening.
Prior to the pandemic, telemedicine was used for a small fraction of care in the healthcare system (~5%). In early March, the healthcare system was in the early stages of implementing EHR-integrated video visits using a vendor product. Recognizing that rapid, wide-scale adoption of EHR-integrated telemedicine visits was not feasible as part of imminent-pandemic planning, the organization instead provisioned stand-alone telemedicine accounts as an initial implementation strategy. Additionally, the initial vendor product that was planned for wide-scale EHR-integration could not accommodate group psychotherapy (i.e., connections with one or more providers and multiple patients/participants), an important treatment in MH/SUD care. Therefore, for group therapy sessions, the organization decided also to implement a second vendor product that was being used by the organization for non-clinical business purposes but for which the organization had in place a Health Insurance Portability and Accountability Act (HIPAA) complaint Business Associates Agreement (BAA). This second product could accommodate multiple participants in a meeting for group therapy. Therefore, at the outset of the pandemic there were two different telemedicine vendor products being implemented in the organization: one product for “1:1” (i.e., 1 provider and 1 patient) sessions, and another for group therapy sessions. Within the first week of wide-spread use of the 1:1 vendor product, providers across the organization (MH/SUD and non-MH/SUD providers) were experiencing frequent connectivity and technical difficulties that were disrupting outpatient patient care. Due to the difficulty in using the original 1:1 telemedicine vendor product, on March 25th the healthcare organization decided to discontinue its use and instead use only the second, stand-alone, product for all healthcare visits (i.e., 1:1 connections and group sessions), with a plan for eventual and phased integration of this second product into the EHR. Additionally, during the pandemic providers were encouraged to use either telephone or video visits to maintain patient care, if clinically appropriate.
2.2. Patient population and data collection
The study population consisted of any patient (regardless of age) who received outpatient visits (in-person or via telemedicine [video, telephone, asynchronous e-visits or e-consults]) from January 1st to June 30th, 2020. Data from the same time period in 2018 and 2019 were used as a historical baseline. Using EHR data, we defined visits for MH/SUD as outpatient visits where a mental health and/or substance use disorder was the primary diagnosis (ICD-10 codes: MH–F20.xxx-F97.xxx and F99.xxx, excluding F70-F82; SUD–F10-F16, and F18.xxx-F19.xxx excluding F15.929, F15.93) (see Appendix Table 1), regardless whether the provider was a specialty MH/SUD provider, a primary care provider, or a non-MH/SUD specialty provider.
2.3. Main outcomes
Our main outcomes were outpatient visit counts, percentages and trends over time by: 1) visit type (MH/SUD or non-MH/SUD, also MH and SUD separately); 2) provider type (MH/SUD specialty [e.g., psychiatrist, psychologist, clinical social worker], primary care, or other); 3) patient race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic and Other/Unknown); 4) insurance type (commercial, Medicaid, Medicare, other, unknown); 5) visit method (in-person or telemedicine); and, 6) specific MH diagnostic groups (schizophrenia/bipolar disorder, depressive disorders, anxiety disorders, and other disorders).
2.4. Patient characteristics
Demographic characteristics examined were patient age (mean, standard deviation [SD]), patient-reported sex and race/ethnicity, and insurance type.
2.5. Statistical analysis
We described and compared demographics, MH/SUD diagnoses, provider type and insurance type of patients with a visit where the primary diagnosis was a MH/SUD, January–June 2018–2020 and pre-pandemic (January 1st-March 10th, 2020), during the COVID-19 surge emergency (March 25th-May 18th, 2020) and during the partial reopening (May 19th-June 30th, 2020). We calculated weekly number of outpatient visits for MH/SUD in the healthcare system, January–June 2018–2020 and compared and visualized the trends over time.
We conducted bivariate analyses of the outcomes (1–6 above) for the year 2020, comparing the mean [SD] of weekly visits pre-pandemic to pandemic surge and to partial reopening, using t-tests. For visit method we used two proportion z-tests. All statistical analysis was conducted on the Python statsmodels module, version 0.11.
3. Results
3.1. Patient characteristics
Each year between January–June, 52,907 (in 2018), 62,756 (in 2019) and 73,184 (in 2020) patients were seen for a MH/SUD visit (Table 1 ). Mean age was 40.5–41.0 [SD, 20.5–21.1] years. The majority of patients were female (58.0%–60.6%) and non-Hispanic White (76.5%–78.9%); approximately half were commercially insured (49.6%–53.7%). The fraction seen by primary care grew over time (34.4%–44.8%). In 2020 alone, 41,648 patients, 37,426 patients and 25,898 patients were seen for a MH/SUD visit during pre-COVID-19 surge, during-COVID-19 surge and partial reopening, respectively (Appendix Table 2).
Table 1.
Characteristics of patients with a visit in the health system where the primary diagnosis was a mental health and/or substance use disorder (MH/SUD), January–June 2018–2020 (unadjusted).ab
| Patient Characteristics | 2018 (N = 52,907) |
2019 (N = 62,756) |
2020 (N = 73,184) |
|---|---|---|---|
| Age, mean ± SD, yearc | 40.5 ± 21.1 | 40.6 ± 20.9 | 41.0 ± 20.5 |
| Female | 30,662 (58.0) | 36,675 (58.4) | 44,356 (60.6) |
| Race | |||
| Non-Hispanic White | 40,459 (76.5) | 48,272 (76.9) | 57,735 (78.9) |
| Non-Hispanic Black | 2334 (4.4) | 2626 (4.2) | 2830 (3.9) |
| Non-Hispanic Otherd | 4640 (8.8) | 5624 (9.0) | 6150 (8.4) |
| Hispanic | 5474 (10.3) | 6234 (9.9) | 6469 (8.8) |
| Psychiatric diagnoses | |||
| MH/SUD | 52,907 (100.0) | 62,756 (100.0) | 73,184 (100.0) |
| SUDe | 4245 (8.0) | 4877 (7.8) | 5450 (7.4) |
| MHe | 49,822 (94.2) | 59,299 (94.5) | 69,249 (94.6) |
| Schizophrenia/bipolar disorders | 5031(9.5) | 5559 (8.9) | 5931(8.1) |
| Anxiety disorders | 19,278 (36.4) | 23,979 (38.2) | 30,496 (41.7) |
| Depressive disorders | 15,722 (29.7) | 17,941 (28.6) | 20,269 (27.7) |
| Other disorders | 14,002 (26.5) | 16,464 (26.2) | 18,220 (24.9) |
| Provider typee | |||
| Specialty MH/SUD | 31,840 (60.2) | 33,668 (53.6) | 35,007 (47.8) |
| Primary care | 18,196 (34.4) | 24,437 (38.9) | 32,811 (44.8) |
| Other | 13,971 (26.4) | 16,174 (25.8) | 17,646 (24.1) |
| Insurance type | |||
| Commercial | 28,416 (53.7) | 31,139 (49.6) | 37,662 (51.5) |
| Medicaid | 11,935 (22.6) | 16,992 (27.1) | 17,654 (24.1) |
| Medicare | 10,002 (18.9) | 11,223 (17.9) | 11,687 (16.0) |
| Otherf | 731 (1.4) | 845 (1.3) | 827 (1.1) |
| Unknown | 4272 (8.1) | 5351 (8.5) | 11,511 (15.7) |
Data are reported as No. (%) of patients unless otherwise indicated.
Start and end dates in each year: 2018/1/1–2018/7/1; 2019/1/1–2019/7/1; 2020/1/1–2020/6/30. There is an extra day in February 2020, i.e., 2/ 29, so 7/1 (instead of 6/30) was used for year 2018 and 2019 to obtain an equal duration across the 3 years.
Age range for 2018, 2019, and 2020 are 0–100 years, 0–103 years, and 0–106 years, respectively.
Other includes unknown and refused, which accounted for 980 patients in 2018, 1216 visits in 2019 and 1427 visits in 2020.
Columns sum to >100% since patients may have different MH/SUD diagnoses as the primary reason for visits during observation period, and they may see more than one provider type for a MH/SUD visit.
Other includes other government programs, international insurance, free care, auto insurance, CHAMPUS-Tricare and Workers Compensation.
3.2. Changes in visit volume by diagnosis group
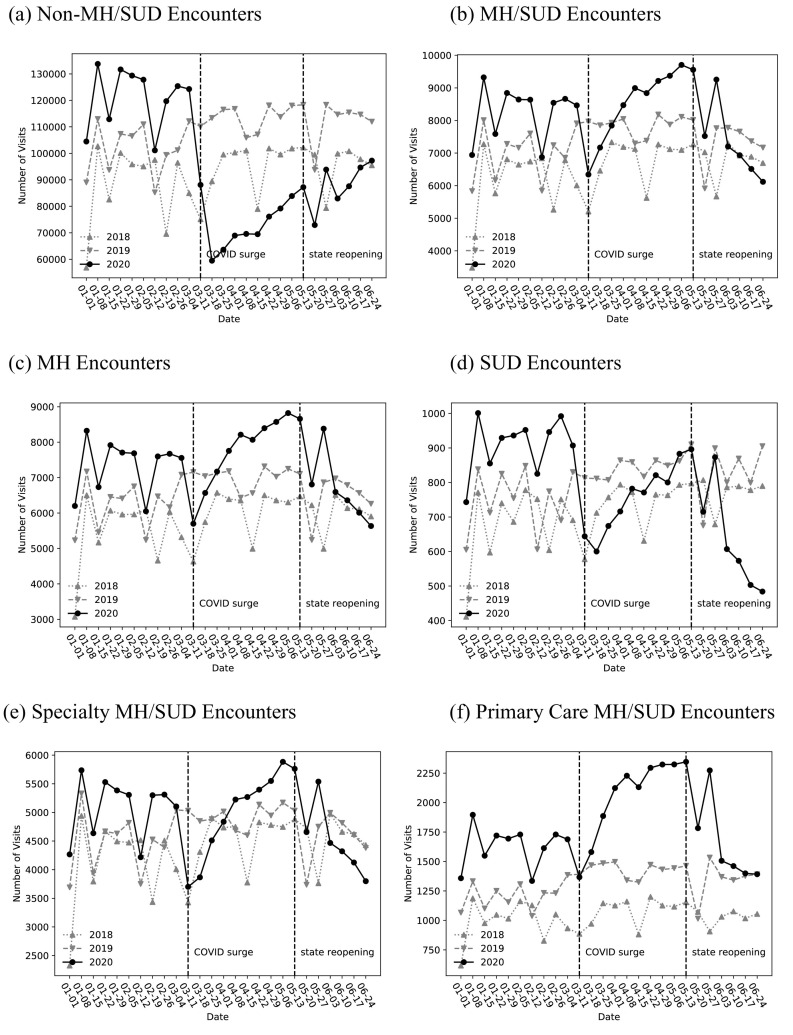
During the surge (March 25th-May 18th, 2020), non-MH/SUD visits declined by 38.2% (P < .001) relative to the pre-pandemic 2020 visit volume, while MH/SUD visits increased 9.1% above pre-COVID-19 levels (P < .05); however, during the partial reopening period (May 19th-June 30th, 2020) MH/SUD visits began to decrease, not statistically, to below pre-pandemic 2020 levels (−12.1%) ( Table 2 , Fig. 1a-b ). Non-MH/SUD visits began to increase during the partial reopening period, but were still low relative to the 2020 pre-pandemic volume (decreased by 27.1%, P < .001). The initial MH/SUD visit increase that occurred during the pandemic surge was for MH visits (9.1%, P < .05); SUD visits decreased to below the 2020 pre-pandemic volume during the surge by and continued to do so during the partial reopening, 12.7% and 31.1% respectively (P < .01) (Table 2 , Fig. 1c-d). During the surge, compared to pre-pandemic in 2020, most of the increase in visits were for anxiety disorders (a 24.2% increase, P < .001) and for schizophrenia/bipolar disorders (12.5% increase, P < .05) (Table 2 , Appendix
Table 2.
Changes in average weekly mental health and/or substance use disorder (MH/SUD) visits in the healthcare organization during COVID surge emergency and partial reopening compared to pre-pandemic, January–June 2020 (unadjusted).a
| Visit Characteristics | Jan 1st-March 10th,2020a (N of weeks = 10) Pre-pandemic |
March 25th-May 19th, 2020b (N of weeks = 8) COVID Surge |
May 20th –June 30th, 2020b (N of weeks = 6) Partial Reopening |
||
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | % change in mean vs. Pre- COVID | Mean ± SD | % change in mean vs. Pre- COVID | |
| Diagnosis Category | |||||
| Non-MH/SUD | 121,043.6 ± 10,763.7 | 74,750.67680.9 | −38.2 *** | 88,200.8 ± 8336.3 | −27.1 *** |
| MH/SUD | 8251.3 ± 784.4 | 8998.9 ± 573.5 | 9.1 * | 7256.5 ± 1001.5 | −12.1 |
| Substance use disorders | 908.6 ± 75.7 | 792.9 ± 70.9 | −12.7 ** | 625.8 ± 133.8 | −31.1 ** |
| MH | 7344.0 ± 714.6 | 8206.8 ± 506.0 | 11.7 * | 6631 0.0 ± 870.6 | −9.7 |
| Schizophrenia/bipolar disorders | 816.3 ± 86.3 | 918.5 ± 64.9 | 12.5 * | 725.0 ± 98.4 | −11.2 |
| Anxiety disorders | 2532.4 ± 250.0 | 3146.2 ± 164.0 | 24.2 *** | 2436.0 ± 320.0 | −3.8 |
| Depressive disorders | 2105.2 ± 193.4 | 2257.6 ± 149.5 | 7.2 | 1832.7 ± 274.9 | −12.9 |
| Other disorders | 1428.2 ± 153.1 | 1479.2 ± 115.5 | 3.6 | 1258.3 ± 157.1 | −11.9 |
| Race | |||||
| Hispanic | 817.2 ± 97.5 | 838.1 ± 42.3 | 2.6 | 547.5 ± 144.8 | −33.0 ** |
| Non-Hispanic White | 6403.6 ± 578.9 | 7076.5 ± 473.8 | 10.5 * | 5838.3 ± 751.8 | −8.8 |
| Non-Hispanic Black | 338.9 ± 38.5 | 337.8 ± 20.6 | −0.3 | 255.5 ± 35.7 | −24.6 ** |
| Non-Hispanic Other/Unknown/Refusedc |
691.6 ± 76.7 | 746.5 ± 55.3 | 7.9 | 615.2 ± 86.7 | −11.1 |
| Provider type | |||||
| MH/SUD specialist | 5079.4 ± 497.9 | 5304.5 ± 428.6 | 4.4 | 4484.3 ± 542.4 | −11.7 |
| Primary care provider | 1631.1 ± 165.5 | 2207.0 ± 146.0 | 35.3 *** | 1635.7 ± 313.7 | 0.3 |
| Other specialist | 1938.9 ± 190.0 | 1971.2 ± 62.9 | 1.7 | 1544.5 ± 213.7 | −20.3 ** |
| Insurance | |||||
| Commercial | 3867.0 ± 376.5 | 4073.6 ± 455.5 | 5.3 | 3630.7 ± 407.2 | −6.1 |
| Medicaid | 2337.4 ± 230.0 | 2343.0 ± 206.3 | 0.2 | 1883.5 ± 304.5 | −19.4 * |
| Medicare | 1527.1 ± 153.1 | 1566.1 ± 180.8 | 2.6 | 1208.7 ± 239.7 | −20.9 * |
| Otherd | 146.7 ± 16.9 | 103.5 ± 14.4 | −29.4 *** | 89.2 ± 11.1 | −39.2 *** |
| Unknown | 373.1 ± 40.2 | 912.6 ± 276.6 | 144.6 ** | 444.5 ± 66.4 | 19.1 |
*P < .05 **P < .01 ***P < .001.
Due to the COVID-19 pandemic, on March 16th, 2020 clinics at the hospital system closed for non-urgent in-person care. We excluded visits between 3/11/2020 and 3/24/2020 from analysis, because during this period in-person non-urgent visits were halted and healthcare system was deploying telehealth.
t-test was used to compare to pre-COVID-19 surge (Jan 1st – March 10th).
Other includes unknown and refused, which accounted for 2350 visits in 2018, 2573 visits in 2019 and 3165 visits in 2020.
Other includes other government programs, international insurance, free care, auto insurance, CHAMPUS-Tricare and Workers Compensation.
Fig. 1.
Weekly number of mental health and/or substance use disorder (MH/SUD) outpatient visits in the healthcare system, January–June 2018–2020 (unadjusted).a
a X-axes shows the timeline from January 1st to June 30th 2020 and January 1st to July 1st, 2018 and 2019, scaled and measured in every seven days. We used the 2020 calendar date to align the date information across the three years (after 2/28 of 2018 and 2019, there is one day difference between 2020 and previous two years, i.e. 2/29/2020). Y-axes vary in scale. The first vertical line corresponds to the time period (between 3/11 and 3/17) when Massachusetts declared a state of emergency and provider organization began to discontinue most in-person ambulatory care and transition to telemedicine (i.e., video, phone, or other forms of virtual care [asynchronous e-visits or e-consults]); the second vertical line corresponding to the partial reopening week (between 5/13–5/19). Figures (a) and (b) show that while the number of visits for non-MH/SUD conditions decreased after COVID-19 surge and remained low but increased during the partial reopening in 2020, visits for MH/SUD increased during the surge but then declined. Figures (c) and (d) show that visits for MH increased during the surge and then decreased during reopening, but visits for SUD declined during the surge and reopening. Figures (e) and (f) show that the MH/SUD visit increase primarily occurred in primary care versus MH/SUD specialty during the surge, and then returned to pre-COVID volumes in primary care during reopening.
Fig. 1a-d). However, during the partial reopening there was no statistically significant change visits by diagnosis group, relative to the 2020 pre-pandemic period.
3.3. Changes in visit volume by provider type
In terms of the provider type, there was a significant increase (35.3%, P <. 001) in MH/SUD visits with primary care providers during the surge and it recovered to the normal volume (similar to pre-pandemic in 2020) during the partial reopening. The volume of MH/SUD visits with MH/SUD specialists had a slight but not significant increase (4.4%) during the surge and decreased non-significantly by 11.7% during the partial reopening, relative to pre-pandemic in 2020 (Table 2 , Fig. 1e-f).
3.4. Changes in visit volume by race/ethnicity and insurance type
During the surge, MH/SUD visits by non-Hispanic Whites increased by 10.5% relative to pre-pandemic in 2020 (P < .05); during the partial reopening; however, this increase among non-Hispanic Whites dissipated relative to pre-pandemic in 2020, and visits by Hispanics and non-Hispanic Blacks decreased (by 33.0% and 24.6% respectively; P < .01) ( Table 2 , Appendix Fig. 2a). Commercial insurance, Medicaid and Medicare visit volumes increased during the surge but were not statistically different than pre-pandemic 2020 levels; during reopening, Medicaid visits decreased by 19.4% and Medicare by 20.9% relative to pre-pandemic in 2020 (P < .05) ( Table 2 , Appendix Fig. 2b).
3.5. Changes in 2020 visit volume by visit method (i.e., in-person, telephone, video)
During the COVID-19 surge, telemedicine use predominated in the healthcare system—particularly for MH/SUD visits (MH/SUD = 83.5% vs. non-MH/SUD = 73.1%; P < .001) (Table 3 , Appendix Fig. 3). During the partial reopening, telemedicine use for MH/SUD visits remained similar as during the surge, whereas for non-MH/SUD visits it was used in a smaller fraction of visits (83.3% vs. 48.0%, respectively; P < .001). Video visits specifically (versus phone) were also more commonly used in MH/SUD care during the surge and partial opening periods (surge video visits: MH/SUD = 82.1% vs. non-MH/SUD = 62.4%, P < .001). Video visits remained the predominant mode of MH/SUD outpatient care during the partial reopening, while being used in a minority of non-MH/SUD visits during this same period (partial reopening video visits: MH/SUD = 81.5% vs. non-MH/SUD =36.8%, P < .001). During the COVID surge, among
Table 3.
Number and percent of visits by telemedicine and type of telemedicine during the COVID-19 pandemic surge emergency (March 25th-May 19th, 2020) and the reopening period (May 20th-June 30th, 2020) (unadjusted).a
| Types of Telemedicine | March 25th-May 19th COVID Surge N of MH/SUD = 71,991 N of Non-MH/SUD = 598,005 |
P Valueb | May 20th-June 30th Partial Reopening N of MH/SUD = 43,539 N of Non-MH/SUD = 529,205 |
P Valueb |
|---|---|---|---|---|
| Any type of telemedicine (video, phone, or otherc) | ||||
| MH/SUD visit | 60,140 (83.5) | < 0.001 | 36,273 (83.3) | < 0.001 |
| Non-MH/SUD visit | 437,324 (73.1) | 254,227 (48.0) | ||
| Video visit only | ||||
| MH/SUD visit | 59,083 (82.1) | < 0.001 | 35,503 (81.5) | < 0.001 |
| Non-MH/SUD visit | 373,206 (62.4) | 194,527 (36.8) |
Abbreviation: MH, mental health; SUD, substance use disorders.
Data are reported as No. (%) of visits unless otherwise indicated.
Two proportion z-test was used to compare MH/SUD and Non-MH/SUD visit.
Other includes asynchronous e-visits or e-consults.
MH/SUD visits delivered by telemedicine, telephone visits initially predominated but declined mid-surge and then declined precipitously by mid-partial reopening period as video visits grew (Appendix Fig. 4). Also during the surge, video visits integrated with the EHR initially increased, then plateaued during the period of performance difficulties with the initial integrated vendor; during this period standalone video visits increased. Video visits integrated with the EHR continued to rise (as the system transitioned to integrating the second vendor product) during the surge and partial reopening periods. As the partial reopening period began, integrated video visit volumes for MH/SUD visits surpassed those of standalone video visits.
4. Discussion
During the initial Massachusetts COVID-19 surge, in a large multi-specialty healthcare system, outpatient MH/SUD visits increased—due to increased MH visits, largely occurring in primary care. During the surge and state's partial reopening, SUD visits decreased below pre-COVID-19 levels. MH visits, while not statistically lower, appear to be on a downward trend as well; primary care MH/SUD visits decreased to pre-pandemic levels. These changes in MH/SUD visits were in the context of a dramatic decrease in non-MH/SUD visits (during the pandemic surge) and still low but recovering volume of non-MH/SUD visits (during the partial reopening).
It is perhaps not surprising that primary care would be the initial setting for increased MH treatment-seeking during the surge. Specialty behavioral health providers are in short supply [31], and in a recently published national qualitative study, early in the pandemic surge at least one type of MH/SUD specialist—psychiatrists—described being able to continue care of existing patients but that was more difficult to see new patients due to challenges in learning and navigating the rapid transition to virtual care [14]. Also, patients commonly receive MH care in primary care [32]. Under these circumstances, contacting one's primary care provider is an understandable response to initial increased psychiatric distress. Primary care providers can assess a patient's MH/SUD clinical needs, and either treat and/or assist in triage and referral to specialty care if needed. Different communities are undergoing COVID-19 surges at different time points in the U.S.; knowing that initial increases in demand for mental health services may be concentrated in primary care provides important information for healthcare systems looking to prepare for these needs. For example, integrating primary care with behavioral healthcare [33,34] could help organizations to better address the needs of these patients. However, transitioning quickly to supporting primary care with integrated behavioral health care may not be easy for organizations. Some services in integrated care are not routinely reimbursed by insurance, which could pose as a barrier in some organizations, absent alternative payment model contracting (such as accountable care organizations (ACOs)) that could encourage care that is not solely tied to fee-for-service care in the organization [35].
The decrease in visits for SUD to below pre-COVID-19 levels during the surge, and further still during initial partial opening period, is worrisome. Also, while MH visit volume during the partial reopening was not statistically lower than prior to the surge, nonetheless, the continued pattern of decreased visits in the remaining weeks of observation raise concerns that we are seeing the beginning of a downward trend of MH visits, relative to pre-pandemic. It is unlikely that there was less need for MH/SUD care relative to pre-pandemic, given evidence from prior disasters or recessions, and early literature emerging about the impact of COVID-19 on psychological distress in general and MH/SUD in particular [1,4,6,7,9]. While possible that patients sought care outside of the health system, it seems unlikely that community providers would have the capacity to absorb a greater proportion of MH/SUD care during the surge or partial opening, relative to pre-COVID. The large relative decrease in SUD visits in both periods is particularly concerning given reports of increases substance use and opioid overdose during the pandemic [8,9]. Further, the pandemic has disrupted self-help groups such as Alcoholics Anonymous and Narcotics Anonymous [36], important recovery supports for individuals with SUD. These reductions in visit requires further evaluation and monitoring.
We observed racial/ethnic disparities in MH/SUD visits. Increased volume (during the surge) occurred only among non-Hispanic Whites; and decreases (during reopening) occurred among Hispanics and non-Hispanic Blacks. Both findings are concerning, particularly in the context of already existing disparities in access to MH/SUD care for racial and ethnic minorities pre-pandemic [[16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28],[37], [38], [39]], and increasing evidence of the disproportionate medical and psychological distress burden borne by racial and ethnic minorities during the pandemic [8,15]. Prior research finds a digital divide in terms of access to computer, smartphone and broadband availability to individuals who are racial and ethnic minorities [40]. In a clinical context where only virtual care (phone or video) is available, disparities in access to digital technology will also make care more difficult for these populations.
Decreased visits could reflect lower access to employer-sponsored commercial insurance as part of rising unemployment. There is recent evidence that the rise in unemployment has left more individuals and households without health insurance [41,42]. We explored whether visits associated with commercial insurance decreased, but this was not the case. However, visits associated with Medicaid and Medicare plans decreased during reopening phase. It is unlikely the decrease in Medicaid visits during the partial reopening reflects disruptions in Medicaid eligibility in the population; Massachusetts suspended Medicaid terminations and initiated a premium waiver for hardship during the pandemic emergency [43]. More likely is that the decrease in visits from individuals who are enrolled in Medicaid and Medicare reflects the additional challenges faced by individuals who are poor, disabled and/or elderly in terms of the “digital divide” in access to digital technology, broadband, and/or ability or proficiency in using these tools [[44], [45], [46]]. While more research is needed, this finding suggests that other factors, likely related to social determinants of health, may be influencing access to MH/SUD care.
Telemedicine, particularly video visits, scaled quickly for MH/SUD care—and more so than for non-MH/SUD visits. Our results are consistent with recent research describing that as telemedicine visits increased during the pandemic, MH/SUD visits experienced the least decline among medical specialties [13]. The rapid diffusion of telemedicine occurred in the context of more permissive policy, licensure and reimbursement changes by federal and state governments, and health plans. Its future use will depend upon to what extent these policies revert back to the pre-pandemic state. Our study finds that telemedicine enabled a rapid, system-wide ability to maintain and early on increase access to MH care. Still, our findings of decreased MH/SUD visit volume and racial/ethnic disparities during the surge and reopening suggest additional access to care challenges that future research needs to address. While telemedicine can preserve access to MH/SUD care for some patients, these results suggest that it is unlikely to overcome other barriers related to structural inequalities/disparities and social determinants of health.
There are several limitations to note in this study. First, not all patients with MH/SUD diagnoses associated with visits may meet diagnostic criteria for these disorders. Also, MH/SUD visits are undercounted for patients with visits outside of the organization. We defined visits for MH/SUD as being limited to those with a primary diagnosis that is a MH/SUD condition because we were interested in understanding what was happening with visits for MH or SUD. While some MH/SUD treatment may occur in outpatient visits for which a MH/SUD is not the primary diagnosis/reason for the visit, absent review of the clinical content of notes, the focus or active management of MH/SUD in a given visit is less clear when it is not the primary diagnosis. Additionally, while visit counts may not reflect the total MH/SUD care received by these patients, they do reflect important changes in MH/SUD care that are occurring in the healthcare system. Another limitation to consider is that our findings of rapid and sustained implementation of telehealth for outpatient MH/SUD care in this healthcare organization may not generalize to other healthcare organizations or U.S. regions. For example, recent analysis of Medicare data from April 2020 finds that urban areas saw greater growth in telemedicine primary care visits compared to rural areas (likely due to urban areas having greater broadband access), and that even among urban areas, there was wide variation in telemedicine use—with Boston having the highest proportion of Medicare fee-for-service primary care telemedicine visits compared to other urban areas [10]. Important strengths of this study are that the healthcare organization is large, includes a diverse array of settings, and has an integrated EHR system. Other strengths are that our data include visits from patients of diverse insurance types (e.g., commercial, Medicare, and Medicaid), and our use of several years of data available as comparisons to pre-COVID healthcare use.
5. Conclusions
MH/SUD visits increased during the COVID surge, largely in primary care. Telemedicine can be rapidly scaled across a healthcare system to address what would otherwise be drastic decreases in patient access to MH/SUD care, particularly during the pandemic surge. However, as the pandemic and its associated economic crisis continue to unfold, subsequent decreases in MH/SUD visits suggest additional barriers to care. In particular, we found concerning disparities of care for patients with SUD, those who are racial and ethnic minorities, and patients from vulnerable, underserved populations. These findings highlight the importance of future research aimed at better understanding barriers to MH/SUD care during the pandemic, particularly for populations that appear to be especially vulnerable to disruptions in care such as individuals with SUD, as well as those who are racial/ethnic minorities or for whom structural health equity and/or digital divide challenges may be affecting access to care.
Author statement
Dr. Yang: Conceptualization, methodology, software, validation, formal analysis, investigation, resources, data curation, writing-review & editing, visualization. Dr. Landrum: methodology, writing-review & editing. Dr. Zhou: Conceptualization, methodology, data curation, writing-review & editing, visualization. Dr. Busch: Conceptualization, methodology, writing-original draft, writing-review & editing, visualization.
Source of funding
This work was supported by the National Institutes of Health: NIDA P30 DA035772 and R01DA048533, NIMH R01MH112829 (Dr. Busch), NIAID R01AI150295 and AHRQ R01HS025375 (Dr. Zhou).
Declaration of Competing Interest
Drs. Yang, Zhou, and Busch have not conflict of interest disclosures; Dr. Landrum discloses husband's income from the on-going opioid litigation representing plaintiffs seeking damages.
Acknowledgments
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.genhosppsych.2020.09.004.
Appendix A. Supplementary data
Supplementary data
Data availability
The data that has been used is confidential.
References
- 1.Beaglehole B., Mulder R.T., Frampton C.M., Boden J.M., Newton-Howes G., Bell C.J. Psychological distress and psychiatric disorder after natural disasters: systematic review and meta-analysis. B J Psych. 2013;2018:716–722. doi: 10.1192/bjp.2018.210. [DOI] [PubMed] [Google Scholar]
- 2.Keyes K.M., Hatzenbuehler M.L., Hasin D.S. Stressful life experiences, alcohol consumption, and alcohol use disorders: the epidemiologic evidence for four main types of stressors. Psychopharmacology. 2011;218:1–17. doi: 10.1007/s00213-011-2236-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.North C.S. A tale of two studies of two disasters: comparing psychosocial responses to disaster among Oklahoma City bombing survivors and Hurricane Katrina evacuees. Rehabil Psychol. 2010;55:241–246. doi: 10.1037/a0020119. [DOI] [PubMed] [Google Scholar]
- 4.North C.S., Ringwalt C.L., Downs D., Derzon J., Galvin D. Postdisaster course of alcohol use disorders in systematically studied survivors of 10 disasters. Arch Gen Psychiatry. 2011;68:173–180. doi: 10.1001/archgenpsychiatry.2010.131. [DOI] [PubMed] [Google Scholar]
- 5.Bor J., Basu S., Coutts A., McKee M., Stuckler D. Alcohol use during the great recession. Alcohol Alcohol. 2013;48:343–348. doi: 10.1093/alcalc/agt002. [DOI] [PubMed] [Google Scholar]
- 6.Forbes M.K., Krueger R.F. The great recession and mental health in the United States. Clin Psychol Sci. 2019;7:900–913. doi: 10.1177/2167702619859337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGinty E.E., Resskreischer R., Han H., Barry C.L. Psychological distress and lonliness reported by U.S. adults in 2018 and April 2020. JAMA. 2020;324:93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Czeisler M.E., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. Morb Mortal Wkly Rep. 2020;69 doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alter A., Yeager C. COVID-19 Impact on U.S. National Overdose Crisis. Overdose Detection Mapping Application Program (ODMAP) June 2020. http://www.odmap.org/Content/docs/news/2020/ODMAP-Report-June-2020.pdf
- 10.Bosworth A., Ruhter J., Samson L.W., Sheingold S., Taplin C., Tarazi W., et al. July 28, 2020. Mediciare beneficiary use of telehealth vistis: early data from the start of the COVID-19 pandemic. Issue Brief. Washington, D.C.: Office of the Assistant Secretary for Planning and Evaluation, Department of Health and Human Services. [Google Scholar]
- 11.Verma S. 2020. Early Impact Of CMS Expansion Of Medicare Telehealth During COVID-19, Health Affairs Blog. July 15. [DOI] [Google Scholar]
- 12.Center for Connected Health Policy COVID-19 Related State Actions. https://www.cchpca.org Accessed: September 10, 2020.
- 13.Mehrotra A. 2020. The impact of the COVID-19 pandemic on outpatient visits: a rebound emerges. To the Point (blog). Commonwealth Fund. May 19. [DOI] [Google Scholar]
- 14.Uscher-Pines L., Sousa J., Raja P., Mehrotra A., Barnett M., Huskamp H.A. 2020. Suddenly becoming a “Virtual Doctor”: experiences of psychiatrists transitioning to telemedicine durin the COVID-19 pandemic. Psychiatric Services Published September 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Raifman M., Raifman J. Disparities in the population at risk of severe mental illness from COVID-19 by race/ethnicity and income. Am J Public Health. 2020;59:137–139. doi: 10.1016/j.amepre.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cook B.L., Zuvekas S.E., Carson N., Wayne G.F., Vesper A., McGuire T.G. Assessing racial/ethnic disparities in treatment across episodes of mental health care. Health Serv Res. 2014;49:206–229. doi: 10.1111/1475-6773.12095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alegria M., Chatterji P., Wells K.B., Cao Z., Takeuchi D., Jackson J., et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatr Serv. 2008;59:1264–1272. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ault-Brutus A.A. Changes in racial-ethnic disparities in use and adequacy of mental health care in the United States. Psychiatr Serv. 1990-2003;63:531–540. doi: 10.1176/appi.ps.201000397. [DOI] [PubMed] [Google Scholar]
- 19.Blanco C., Patel S.R., Liu L., Jiang H., Lewis-Fernandez R., Schmidt A.B., et al. National trends in ethnic disparities in mental health care. Med Care. 2017;45:1012–1019. doi: 10.1097/MLR.0b013e3180ca95d3. [DOI] [PubMed] [Google Scholar]
- 20.Cummings J.R., Wen H., Ko M., Druss B.G. Race/ethnicity and geographic access to Medicaid substance use disorder treatment facilities in the United States. JAMA Psychiat. 2014;71:190–196. doi: 10.1001/jamapsychiatry.2013.3575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stockdale S.E., Lagomasino I.T., Siddique J., McGuire T.G., Miranda J. Racial and ethnic disparities in detection and treatment of depression and anxiety among psychiatric and primary health care visits, 1995-2005. Med Care. 2008;46:668–677. doi: 10.1097/MLR.0b013e3181789496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cook B.L., Zuvekas S.E., Chen J., Progovac A., Lincoln A.K. Assessing the individual, neighborhood, and policy predictors of disparities in mental health care. Med Care Res Rev. 2017;74:404–430. doi: 10.1177/1077558716646898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goedel W.C., Shapiro A., Cerda M., Tsai J.W., Hadland S.E., Marshall B.D.L. Association of racial/ethnic segregation with treatment capacity for opioid use disorder in counties in the United States. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haffajee R.L., Lin L.A., Bohnert A.S.B., Goldstick J.E. Characteristics of US counties with high opioid overdose mortality and low capacity to deliver medications for opioid use disorder. JAMA Netw Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.6373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Quality National Healthcare, Report Disparities. Appendix A. Rockville, M.D.: Agency for Healthcare Quality and Research. US Dept of Health and Human Services. 2018;2019 [Google Scholar]
- 26.Busch A.B., Huskamp H.A., Neelon B., Manning T., Normand S.-L.T., McGuire T.G. Longitudinal racial/ethnic disparities in antimanic medication use in bipolar-I disorder. Med Care. 2009;47:1217–1228. doi: 10.1097/MLR.0b013e3181adcc4f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Phillips K.L., Copeland L.A., Zeber J.E., Stock E.M., Tsan J.Y., MacCarthy A.A. Racial/ethnic disparities in monitoring metabolic parameters for patients with schizophrenia receiving antipsychotic medications. Am J Geriatr Psychiatry. 2015;23:596–606. doi: 10.1016/j.jagp.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 28.Busch A.B., Lehman A.F., Goldman H.G., Frank R.G. Changes over time and disparities in schizophrenia treatment quality. Med Care. 2009;47:1990207. doi: 10.1097/MLR.0b013e31818475b7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Datar S., Huddle R. Charts: Massachusetts's coronavirus outbreak compared to other states. Boston Globe Boston: John W Henry April 18. 2020. https://www.bostonglobe.com/2020/04/18/metro/look-coronavirus-impact-massachusetts-versus-other-states/
- 30.Massachusetts Executive Office of Labor and Workforce Development Massachusetts Unemployment and Job Estimates for April 2020. https://www.mass.gov/news/massachusetts-unemployment-and-job-estimates-for-april-2020 Accessed May 22, 2020.
- 31.Health Resources and Services Administration/National Center for Health Workforce Analysis; Substance Abuse and Mental Health Services Administration/Office of Policy, Planning and Innovation . 2015. National projections of supply and demand for selected behavioral health practitioners: 2013–2025. Rockville, MD. [Google Scholar]
- 32.Wang P.S., Lane M., Olfson M., Pincus H.A., Wells K.B., Kessler R.C. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 33.Kroenke K., Unutzer J. Closing the false divide sustainable approaches to integrating mental health services into primary care. J Gen Intern Med. 2016;32:404–410. doi: 10.1007/s11606-016-3967-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Blasi P.R., Cromp D., McDonald S., Hsu C., Coleman K., Flinter M., et al. Approaches to behavioral health integration at high performing primary care practices. J Am Board Fam Med. 2018;31:691–701. doi: 10.3122/jabfm.2018.05.170468. [DOI] [PubMed] [Google Scholar]
- 35.Stewart M.T., Horgan C.M., Quinn A., Garnick D.W., Reif S., Creedon T.B., et al. The role of health plans in supporting behavioral health integration. Adm Policy Ment Health. 2017;44:867–977. doi: 10.1007/s10488-017-0812-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Santhanam L. 2020. Why COVID-19 can be 'toxic' for people in alcohol recovery. PBS Newhour.https://www.pbs.org/newshour/health/why-covid-19-can-be-toxic-for-people-in-alcohol-recovery [Google Scholar]
- 37.Substance Abuse and Mental Health Administration (SAMHSA) Double Jeopardy: COVID-19 and Behavioral Health Disparities for Black and Latino Communities in the U.S. Office of Behavioral Health Equity, Substance Abuse and Mental Health Administration (SAMHSA) 2020. https://www.samhsa.gov/sites/default/files/covid19-behavioral-health-disparities-black-latino-communities.pdf Accessed July 10, 2020.
- 38.Horvitz-Lennon M., McGuire T.G., Alegria M., Frank R.G. Racial and ethnic disparities in the treatment of a Medicaid population with schizophrenia. Health Serv Res. 2009;44:2106–2122. doi: 10.1111/j.1475-6773.2009.01041.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mennis J., Stahler G.J. Racial and ethnic disparities in outpatient substance use disorder treatment episode completion for different substances. J Subst Abuse Treat. 2016;63:25–33. doi: 10.1016/j.jsat.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 40.Perrin A., Turner E. Smartphones help blacks, Hispanics bridge some-but not all-digital gaps with Whites Fact Tank: News in the Numbers Pew Research Center August 20. 2019. https://pewrsr.ch/2Z1PKPf
- 41.Collins S.R., Gunja M.Z., Aboulafia G.N., Czyzewicz E., Kline C.H., Rapoport R., et al. Commonwealth Fund; June: 2020. An early look at the potential implications of the COVID-19 pandemic for health insurance coverage.https://www.commonwealthfund.org/publications/issue-briefs/2020/jun/implications-covid-19-pandemic-health-insurance-survey [Google Scholar]
- 42.Dorn S. The COVID-19 Pandemic and Resulting Economic Crash. The National Center for Coverage Information, Families USA. July 13. 2020. https://familiesusa.org/wp-content/uploads/2020/07/COV-254_Coverage-Loss_Report_7-17-20.pdf
- 43.MassHealth Eligibility Flexibilities for COVID-19 June 2020. https://www.mass.gov/doc/masshealth-eligibility-flexibilities-for-covid-19-0/download
- 44.Anderson M., Kumar M. Digital divide persists even as lower-income Americans make gains in tech adoption. Fact Tank: News in the Numbers Pew Research Center May 7. 2019. https://www.pewresearch.org/fact-tank/2019/05/07/digital-divide-persists-even-as-lower-income-americans-make-gains-in-tech-adoption/
- 45.Anderson M., Perrin A. Vol. 7. 2017. Disabled Americans are less likely to use technology. Fact Tank: News in the Numbers Pew Research Center April.https://www.pewresearch.org/fact-tank/2017/04/07/disabled-americans-are-less-likely-to-use-technology/ [Google Scholar]
- 46.Gray D.M., Joseph J.J., Olayiwola J.N. 2020. Strategies for Digital Care of Vulnerable Patients in a COVID-19 World—Keeping in Touch. JAMA Health Forum. 1(6) [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data
Data Availability Statement
The data that has been used is confidential.