Abstract
Backgrounds
The severe acute respiratory syndrome-coronavirus 2 (SARS-CoV-2) has spread worldwide. Cardiac injury after SARS-CoV-2 infection is a major concern. The present study investigated impact of the biomarkers indicating cardiac injury in coronavirus disease 2019 (COVID-19) on patients' outcomes.
Methods
This study enrolled patients who were confirmed to have COVID-19 and admitted at a tertiary university referral hospital between February 19, 2020 and March 15, 2020. Cardiac injury was defined as an abnormality in one of the following result markers: 1) myocardial damage marker (creatine kinase-MB or troponin-I), 2) heart failure marker (N-terminal-pro B-type natriuretic peptide), and 3) electrical abnormality marker (electrocardiography). The relationship between each cardiac injury marker and mortality was evaluated. Survival analysis of mortality according to the scoring by numbers of cardiac injury markers was also performed.
Results
A total of 38 patients with COVID-19 were enrolled. Twenty-two patients (57.9%) had at least one of cardiac injury markers. The patients with cardiac injuries were older (69.6 ± 14.9 vs. 58.6 ± 13.9 years old, P = 0.026), and were more male (59.1% vs. 18.8%, P = 0.013). They showed lower initial oxygen saturation (92.8 vs. 97.1%, P = 0.002) and a trend toward higher mortality (27.3 vs. 6.3%, P = 0.099). The increased number of cardiac injury markers was significantly related to a higher incidence of in-hospital mortality which was also evidenced by Kaplan-Meier survival analysis (P = 0.008).
Conclusion
The increased number of cardiac injury markers is related to in-hospital mortality in patients with COVID-19.
Keywords: Coronavirus; COVID-19, Cardiac Injury Markers; In-hospital Mortality
Graphical Abstract
INTRODUCTION
The coronavirus disease 2019 (COVID-19) that is caused by the severe acute respiratory syndrome-coronavirus2 (SARS-CoV2) has spread worldwide.1,2 It has become a global crisis with a tremendous socio-economic impact.3 The case fatality rate worldwide exceeded 6% with higher mortality found mostly in patients with risk factors, such as age of > 60 years, and history of cardiovascular, respiratory, and metabolic disorders. Nevertheless, young patients without any medical history also can experience a fatal course of the disease.4,5
The mortality in COVID-19 was caused mainly by a respiratory failure due to severe acute pneumonia, but systemic inflammatory response syndrome, including cytokine storm, and myocardial damage, such as acute fulminant myocarditis with arrhythmic manifestations, can lead to a sudden cardiac death.6,7,8,9,10 In this regard, the cardiac injury related to SARS-CoV2 infection is considered as an important issue. However, owing to the risk of disease transmission during the diagnostic procedures and shortage of medical resources, a thorough examination of the cardiac injury using advanced diagnostic modalities is often not available for patients with COVID-19.7,11,12
Previous studies have defined the cardiac injury based on the cardiac biomarkers obtained by blood sampling and the abnormality on electrocardiography (ECG); these modalities are commonly available even in highly transmissible viral diseases.13 To date, the impact of each component indicating cardiac injury and heart failure in COVID-19 on the patients' outcome has never been studied.
The aim of this study was to evaluate the impact of cardiac injury markers including heart failure biomarker on the clinical outcome of patients with COVID-19 using a scoring system that utilized cardiac biomarkers and ECG findings.
METHODS
Study population
Between February 19, and March 15 in 2020, a total of 38 patients confirmed to have COVID-19 at the Keimyung University Dongsan Hospital in Daegu, Korea were consecutively included in the present study. Patients aged < 18 years were initially excluded. All the enrolled patients were confirmed to have SARS-CoV-2 infection by real-time reverse transcriptase-polymerase chain reaction (rRT-PCR) assay testing of nasal swabs. Electronic medical records, laboratory data, and ECG data of the patients were reviewed by two cardiologists.
Definition of cardiac injury and outcomes
Cardiac injury was defined when one of the following results is abnormal: 1) myocardial damage marker (creatine kinase-MB [CK-MB] or troponin-I > the 99th percentile upper reference limit); 2) heart failure marker (NT-proBNP ≥ 125 pg/mL); and 3) electrical abnormality marker (first detected or newly developed supraventricular tachycardia, ventricular tachycardia, ventricular fibrillation, atrial fibrillation, bundle branch block, ST-segment elevation/depression, T-wave flattening/inversion, and QT interval prolongation on ECG).4,6,11,13 The cardiac injury score was described using a 3-point scale (score 0 to 3) as giving each maker 1-point. Finally, we investigated the impact of cardiac injury markers or scoring on in-hospital mortality in the study population.
Statistical analysis
Mean ± standard deviation or median (interquartile range [IQR]) was presented for continuous variables. Independent Student's t-test and Pearson's correlation coefficient analysis were used to compare the groups. Categorical variables were compared using the χ2 test, Fisher's exact test, or Kruskal-Wallis test with post hoc pairwise test as appropriate. Variables that were non-normally distributed were compared using the Mann-Whitney U test. A Kaplan-Meier survival curve was analyzed with Breslow test to evaluate the impact of cardiac injury score on in-hospital mortality. All analyses were performed using the Statistical Package for Social Science version 20.0 (IBM SPSS Statistics for Windows, IBM Corp., Armonk, NY, USA). A P-value < 0.05 was considered significant.
Ethics statement
This study conforms to the ethical guidelines of the Declaration of Helsinki14 and was approved by the Institutional Review Bboard of Keimyung University Dongsan Hospital (No. 2020-04-028). Written informed consent was waived because of the retrospective nature of this study.
RESULTS
Baseline characteristics and clinical features of the study population
Among the 38 COVID-19 confirmed patients, 22 patients (57.9%) showed an abnormality in any of the cardiac injury markers. The patients' baseline characteristics, including patient demographics, previous medical history, and clinical presentation at admission, according to the presence and absence of the cardiac injury are shown in Table 1. Patients with cardiac injuries were older (69.6 ± 14.9 vs. 58.6 ± 13.9 years, P = 0.026), and were more likely to be male (59.1% vs. 18.8%, P = 0.013), and to have hypertension history (59.1% vs. 18.8%, P = 0.013) than those without cardiac injuries. The patients with cardiac injuries were more likely to be admitted to the intensive care unit (ICU) initially (22.7% vs. 0%, P = 0.041), and had lower oxygen saturation (92.8 ± 5.5% vs. 97.1 ± 2.1%, P = 0.002), and were more likely to use hydroxychloroquine (40.9% vs. 6.3%, P = 0.017) as well as steroids (54.5% vs. 6.3%, P = 0.002). The demographic and clinical characteristics of whole study patients according to the cardiac injury score were shown in Supplementary Table 1.
Table 1. Demographic and clinical characteristics of whole study patients according to the cardiac injury.
| Variables | Any cardiac injury (n = 22) | No cardiac injury (n = 16) | P value | |
|---|---|---|---|---|
| Age, yr | 69.6 ± 14.9 | 58.6 ± 13.9 | 0.026 | |
| Sex, male | 13 (59.1) | 3 (18.8) | 0.013 | |
| Height, cm | 163.4 ± 6.8 | 160.9 ± 7.8 | 0.415 | |
| Weight, kg | 68.0 ± 7.8 | 58.3 ± 9.8 | 0.012 | |
| BMI, kg/m2 | 25.3 ± 3.3 | 22.6 ± 3.8 | 0.075 | |
| Systolic BP, mmHg | 132.3 ± 22.6 | 132.7 ± 15.3 | 0.950 | |
| Diastolic BP, mmHg | 80.0 ± 11.7 | 86.1 ± 7.1 | 0.054 | |
| PR, beat per minute | 89.0 ± 9.9 | 85.4 ± 10.0 | 0.282 | |
| O2 saturation, % | 92.8 ± 5.5 | 97.1 ± 2.1 | 0.002 | |
| RR, respiration per min | 21.1 ± 1.9 | 20.2 ± 0.5 | 0.130 | |
| Body temperature, °C | 38.2 ± 0.8 | 37.8 ± 0.5 | 0.051 | |
| Medical history | ||||
| DM | 8 (36.4) | 4 (25.0) | 0.457 | |
| HTN | 13 (59.1) | 3 (18.8) | 0.013 | |
| CKD | 2 (9.1) | 0 (0) | 0.215 | |
| Dyslipidemia | 3 (13.6) | 2 (12.5) | 0.919 | |
| Old CVA | 1 (4.5) | 0 (0) | 0.387 | |
| CAD | 0 (0) | 1 (6.3) | 0.235 | |
| Heart failure | 1 (4.5) | 0 (0) | 0.387 | |
| Initial ICU admission | 5 (22.7) | 0 (0) | 0.041 | |
| Pneumonia at admission | 17 (77.3) | 12 (75.0) | 0.871 | |
| Lopinavir/Ritonavira | 9 (40.9) | 9 (56.3) | 0.350 | |
| Hydroxychloroquineb | 9 (40.9) | 1 (6.3) | 0.017 | |
| Steroidsc | 12 (54.5) | 1 (6.3) | 0.002 | |
| Mechanical ventilator | 7 (31.8) | 1 (6.3) | 0.106 | |
| ECMO | 1 (4.8) | 0 (0) | 0.376 | |
Data are presented as mean ± standard deviation or number (%).
BMI = body mass index, BP = blood pressure, PR = pulse rate, RR = respiratory rate, DM = diabetes mellitus, HTN = hypertension, CKD = chronic kidney disease, CVA = cerebrovascular accident, CAD = coronary artery disease, ICU = intensive care unit, ECMO = extracorporeal membrane oxygenation.
aLopinavir/ritonavir 400/100 mg bid (7–10 days); bHydroxychloroquine 400 mg QD (Day 1) + 200 mg bid (Day 2–5); cSteroids: as an equivalent dose of methylprednisolone 1 mg/kg/day.
The symptoms at the initial presentation were not significantly different between the two groups; however, dyspneic symptoms were more likely to be noted in the cardiac injury group (50.0% vs. 18.8%, P = 0.049) (Table 2).
Table 2. Initial symptoms according to the cardiac injury.
| Variables | Any cardiac injury (n = 22) | No cardiac injury (n = 16) | P value |
|---|---|---|---|
| Febrile sensation | 11 (50.0) | 7 (43.8) | 0.703 |
| Myalgia | 1 (4.5) | 4 (25.0) | 0.066 |
| Coughing | 9 (42.9) | 7 (43.8) | 0.957 |
| Sputum | 7 (31.8) | 3 (18.8) | 0.366 |
| Sore throat | 1 (4.5) | 2 (12.5) | 0.369 |
| Rhinorrhea | 1 (4.5) | 0 (0) | 0.387 |
| Dyspnea | 11 (50.0) | 3 (18.8) | 0.049 |
| Chest pain | 1 (4.5) | 0 (0) | 0.387 |
| Diarrhea | 2 (9.1) | 2 (12.5) | 0.735 |
| Vomiting | 1 (4.5) | 0 (0) | 0.387 |
Data are presented as number (%).
Regarding the laboratory test results, the white blood cell count was significantly higher (7.9 ± 4.2 103/μL vs. 5.0 ± 2.2 103/μL, P = 0.018) in the patients with cardiac injuries than in those without cardiac injuries. Moreover, the cardiac injury group also showed a poor renal function (blood urea nitrogen: 30.1 ± 22.4 mg/dL vs. 15.3 ± 9.1 mg/dL, P = 0.009; creatinine: 1.54 ± 1.13 mg/dL vs. 0.81 ± 0.41 mg/dL, P = 0.009) (Table 3).
Table 3. Laboratory findings according to the cardiac injury.
| Variables | Any cardiac injury (n = 22) | No cardiac injury (n = 16) | P value |
|---|---|---|---|
| WBC, 103/µL | 7.90 ± 4.20 | 5.03 ± 2.24 | 0.018 |
| Hb, g/dL | 12.8 ± 1.7 | 12.0 ± 1.1 | 0.112 |
| Platelet, 103/µL | 204.0 ± 91.6 | 211.6 ± 85.1 | 0.796 |
| CRP, mg/dL | 13.5 ± 21.1 | 3.8 ± 4.9 | 0.090 |
| CK-MB, ng/mL | 6.13 ± 8.64 | 1.87 ± 0.18 | 0.411 |
| Tn-I, ng/mL | 0.26 ± 0.26 | 0.16 ± 0.00 | 0.615 |
| NT-proBNP, pg/mL | 1,475.2 ± 2,845.2 | 70.0 ± 53.7 | 0.196 |
| Total bilirubin, mg/dL | 0.60 ± 0.41 | 0.40 ± 0.19 | 0.056 |
| Total protein, g/dL | 6.86 ± 0.64 | 6.92 ± 0.73 | 0.801 |
| Albumin, g/dL | 3.66 ± 0.44 | 3.94 ± 0.45 | 0.059 |
| BUN, mg/dL | 30.1 ± 22.4 | 15.3 ± 9.1 | 0.009 |
| Creatinine, mg/dL | 1.54 ± 1.13 | 0.81 ± 0.41 | 0.009 |
| AST, U/L | 52.9 ± 46.6 | 28.6 ± 12.5 | 0.050 |
| ALT, U/L | 38.2 ± 60.3 | 20.9 ± 15.1 | 0.270 |
Data are presented as mean ± standard deviation.
WBC = white blood cell, Hb = hemoglobin, CRP = C-reactive protein, CK-MB = creatine kinase-MB, BUN = blood urea nitrogen, AST = aspartate transaminase, ALT = alanine transaminase.
Main findings and their incidences of the electrical abnormality were shown in Supplementary Table 2. Most common electrocardiographic abnormality was new-onset or first detected T inversion (46.7%).
Cardiac injury markers and in-hospital mortality
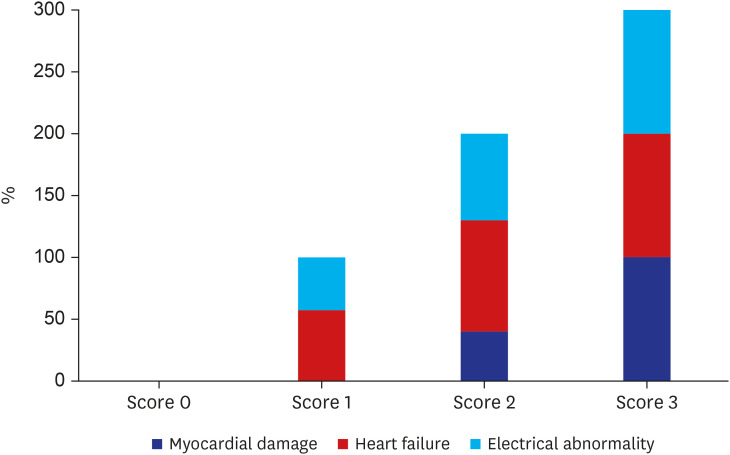
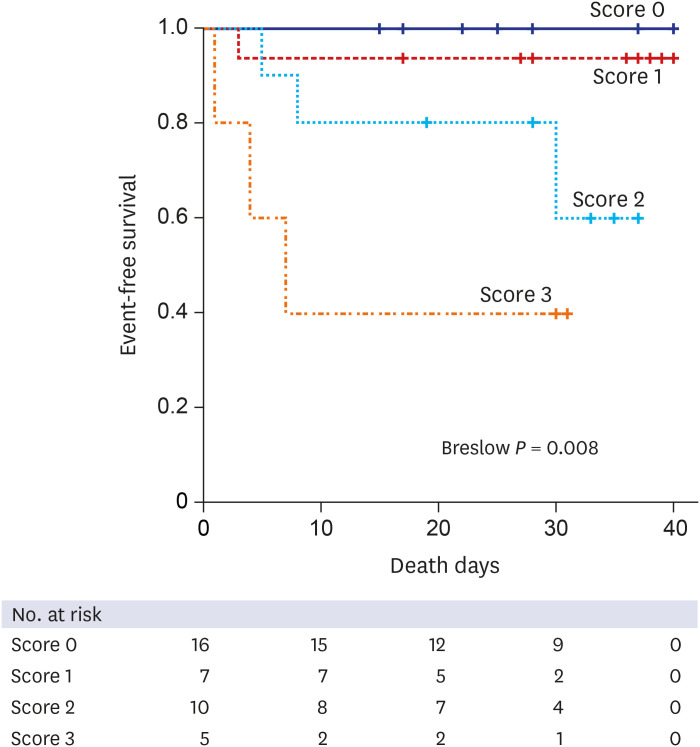
During the median follow-up of 28 days (interquartile range, 17–37 days), 7 patients (18.4%) had in-hospital mortality. Fig. 1 shows the proportion of each component of cardiac injury markers according to the cardiac injury score. The sum of the proportion in each cardiac injury marker is 100% for score 1, 200% for score 2, and 300% for score 3. Abnormal myocardial damage markers are noted only in the higher cardiac injury scores (scores 2 and 3). The proportions of ICU admissions and mechanical ventilator usage with higher mortality increased as the cardiac injury score increases (Table 4). The Kaplan-Meier survival analysis for event-free survival revealed the unfavorable prognosis in those with a high cardiac injury score during the follow-up period (Fig. 2).
Fig. 1. Proportion of the components of cardiac injury markers according to the cardiac injury score. Sum of the proportion in each cardiac injury marker is 100% for score 1, 200% for score 2, and 300% for score 3.
Table 4. Clinical manifestations according to the cardiac injury score.
| Variables | Score 0 (n = 16) | Score 1 (n = 7) | Score 2 (n = 10) | Score 3 (n = 5) | P value |
|---|---|---|---|---|---|
| Pneumonia | 12 (75) | 5 (71.4) | 8 (80) | 4 (80) | 0.745 |
| Initial Admission at ICU | 0 (0) | 0 (0) | 3 (30) | 2 (40) | 0.005 |
| Mechanical ventilator | 1 (6.2) | 1 (14.3) | 4 (40) | 2 (40) | 0.027 |
| Shock | 1 (6.2) | 1 (14.3) | 5 (50) | 3 (60) | 0.003 |
| ECMO | 0 (0) | 0 (0) | 0 (0) | 1 (20) | 0.081 |
| Death | 1 (6.2) | 0 (0) | 3 (30) | 3 (60) | 0.006 |
Data are presented as number (%).
ICU = intensive care unit, ECMO = extracorporeal membrane oxygenation.
Fig. 2. Kaplan-Meier survival curve for in-hospital mortality according to the cardiac injury score. Kaplan-Meier survival analysis showed significantly lower survival as the cardiac injury score increases.
DISCUSSION
The main findings of the current study are as follows; 1) among the 38 COVID-19 confirmed patients at a tertiary university referral hospital, 22 patients (57.9%) showed an abnormality in any of the markers of cardiac injury; 2) elderly and male patients with lower blood oxygen saturation had a higher incidence of cardiac injury; and 3) in-hospital mortality increased substantially as the cardiac injury score increased.
In a previous study, the incidence of cardiac injury that is associated with SARS-CoV-2 infection was reported to be 7.2% in the overall patients, 2% in non-ICU patients, and 22% in ICU patients.6 In other reports, the incidence of cardiac injury was reported to reach up to 27.8%–31% according to the definitions and patient's characteristics.4,15 Even though there are no definite criteria for the diagnosis of cardiac injury in COVID-19, the current consensus of the definition is based on the cardiac enzyme (CK-MB, Tn-I, Tn-T) by blood sampling and ECG (and echocardiography if feasible) examination, which are commonly feasible even during a viral outbreak.4,7,8,11 In this study, 57.9% of the patients had at least one component of cardiac injury marker. The reason for the two-fold higher incidence of cardiac injury in our study compared to the previous reports can be explained by the inclusion of an additional marker, NT-proBNP, to represent heart failure (HF), which is an important cardiac manifestation of SARS-CoV-2 infection indicating cardiac injury. The fact that the study patients were enrolled from the referral hospital with high-risk features is another cause of the higher incidence of cardiac injury in this study.
The evidence of myocardial damage during SARS-CoV-2 infection was evaluated by CK-MB, and troponin-I in this study. Previous studies used either one or two of the biomarkers (CK-MB, troponin-I and troponin-T) indicating myocardial injury depending on the laboratory setting of each hospital.16,17 Electrical abnormalities, which can be induced by the impairment of intracellular calcium function caused by the release of various inflammatory cytokines, or hypoxia-induced mitochondrial dysfunction was identified by ECG.7 We added NT-proBNP as a component of cardiac injury marker indicating HF. Among the biomarkers in HF, NT-proBNP is the most validated measure for the diagnosis, therapeutic guidance and prognostication in acute and chronic HF management.18,19,20,21,22 It can be used to evaluate the status of HF, especially for patients with a transmissible disease and when there is a shortage of medical resources, including the limited personal protective equipment (PPE) and the safety of health care providers is an important issue.23 In COVID-19 patients, the markers of myocardial injury, HF, and electrocardiographic abnormality indicating cardiac injury can be observed independently; however, if they are all observed in a patient with a serious disease, it may suggest a higher risk of mortality. Therefore, the scoring system giving each component one point to stratify risks in COVID-19 patients would be a good surrogate for the estimation of the mortality. Future investigation focusing on the different clinical impact of each cardiac injury marker could broaden the perspective of the prognostic implications in COVID-19.
The cardiac injury related to SARS-CoV-2 infection can be explained by several mechanisms. The first mechanism is the angiotensin converting enzyme 2 (ACE2)-mediated direct damage can be suggested.13,24 ACE2 has been identified as a functional receptor for coronaviruses. SARS-CoV-2 infection is triggered by the binding of the spike protein of the virus to ACE2, which is highly expressed in the heart and lungs. The second one is the hypoxia-induced myocardial injury. Oxidative stress, intracellular acidosis, and mitochondrial damage followed by hypoxia might result in cardiac injury. A significantly lower oxygen saturation levels and higher incidence of dyspneic symptoms was noted in the cardiac injury group in this study. The third is the cardiac microvascular damage caused by vessel hyperpermeability and angio-spasm under the condition of inflammation. The fourth mechanism is the systemic inflammatory response syndrome, such as the cytokine storm, caused by the inadequate responses of type 1 and type 2 helper T cells, which may contribute to the myocardial injury.25 Fulminant myocarditis can be related to the immunologic response during a viral infection.26,27,28 Acute plaque rupture at the epicardial coronary artery and stress-induced cardiomyopathy are other contributors of cardiac injury.7,25,29,30 Cardiac injury in COVID-19 might be a direct cause of mortality by an arrhythmic manifestation combined with the left ventricular systolic dysfunction or might be a result of the multi-organ failure in the setting of systemic inflammatory response by SARS-CoV-2 infection.12,24 Accordingly, it is comprehensible that the patients with an increased number of cardiac injury markers have a higher incidence of mortality, since they have greater signs of cardiac damage and combined multiple organ dysfunction.
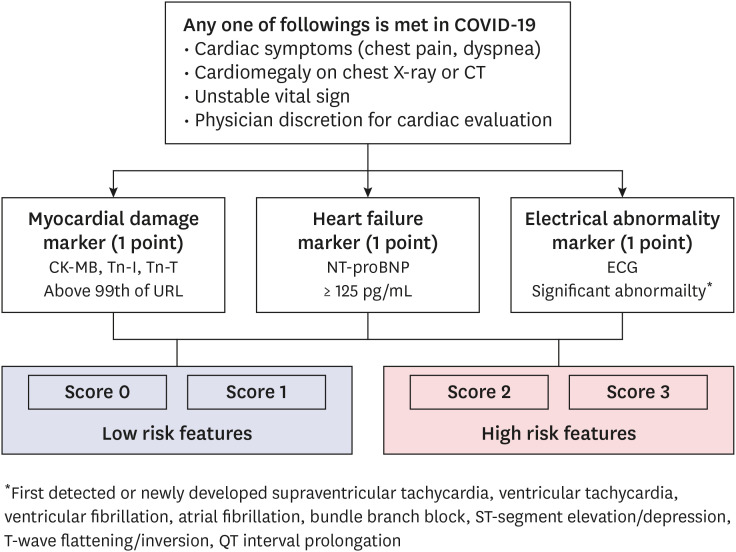
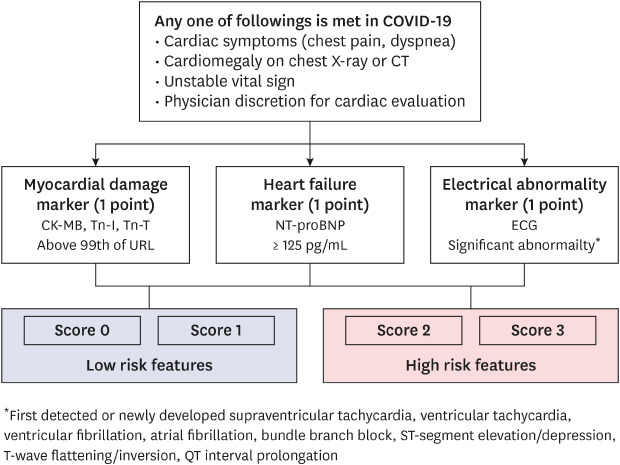
After the cardiac evaluation according to the physician's discretion based on the patient's condition, the cardiac injury score was calculated for the risk stratification. When the patient has one of the following conditions: cardiac symptoms (chest pain, dyspnea); cardiomegaly on chest X-ray or CT; unstable vital sign; and physician discretion for cardiac evaluation, possible cardiac evaluation markers need to be evaluated (Fig. 3). If a patient has at least two positive components (score ≥ 2), the patient is suggested to have a higher risk, which requires special attention with intensive treatment.
Fig. 3. Algorithm for the evaluation of the cardiac injury and risk stratification in COVID-19. After the cardiac evaluation according to the physician's discretion based on the patient's condition, the cardiac injury score was calculated for the stratification of the risk.
COVID-19 = coronavirus disease 2019, CT = computed tomography, URL = upper reference limit, ECG = electrocardiography.
This study has several limitations. First, this is a retrospective observational study with a limited patient population. Further validation of this scoring system in a larger patient population is necessary. Second, the protocol for the evaluation of cardiac injury was not controlled. The attending physician decided each category of the test according to the patient's condition at the time of the management. When the test was not performed, it is assumed as a negative result because the physician considered it as an unnecessary test or the result might be negative. Third, the cut-off value of NT-proBNP was set at the conventional threshold for chronic HF diagnosis (125 pg/mL). Some of the patients might be in an acute HF condition at the time of the evaluation; the cut-off value of 300 pg/mL might be considered. However, to increase its sensitivity of diagnosing cardiac injury, it is better to lower the threshold value.18,19,21 Furthermore, many of the patients are still in a chronic HF condition, which can be evaluated by using 125 pg/mL as the cut-off value.
In conclusion, the increased number of cardiac injury markers including heart failure biomarker is related to a higher in-hospital mortality in patients with COVID-19. The non-invasive cardiac triage algorithm using the scoring system could guide a physician for the strategy of treatment in SARS-CoV-2 infection.
ACKNOWLEDGMENTS
The authors thank A Young Cho (Registered Nurse), Min Kyung Park (Research Coordinator) and So Hee Ahn (Registered Nurse and Research Coordinator) for their sincere contribution to this work.
Footnotes
Funding: This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: H18C1234).
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Kim IC, Kim HA, Youn JC, Hwang J, Lee CH, Cho YK, Park HS, Nam CW, Han S, Hur SH, Eisen HJ, Kim H.
- Data curation: Kim IC, Song JE, Lee HJ, Park JH, Hyun M, Lee JY, Kim HA, Kwon YS, Park JS, Hwang J, Park HS, Eisen HJ, Kim H.
- Formal analysis: Kim IC, Kim H.
- Investigation: Kim IC, Youn JC, Lee CH, Nam CW, Kim H.
- Methodology: Kim IC, Hwang J, Park HS, Nam CW, Kim H.
- Project administration: Youn JC.
- Resources: Kim IC, Kim HA, Yoon HJ.
- Supervision: Youn JC, Han S, Hur SH, Eisen HJ, Kim H.
- Validation: Kim IC, Cho YK, Han S, Kim H.
- Visualization: Kim IC, Kim H.
- Writing - original draft: Kim IC.
- Writing - review & editing: Kim IC, Kim H.
SUPPLEMENTARY MATERIALS
Demographic and clinical characteristics of whole study patients according to the cardiac injury score
Main findings and incidences of the electrical abnormality
References
- 1.World Health Organization. Coronavirus disease (COVID-19) outbreak. [Updated 2020]. [Accessed June 5, 2020]. https://covid19.who.int/
- 2.Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cho DH, Yoo BS, Son JW, Kim IC, Park SM, Choi DJ. COVID-19 — implications for patients with heart failure: the Korean Society of Heart Failure's Clinical Recommendations. Int J Heart Fail. 2020;2(2):2. doi: 10.36628/ijhf.2020.0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5(7):811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics. 2020;145(6):e20200702 [Google Scholar]
- 6.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clerkin KJ, Fried JA, Raikhelkar J, Sayer G, Griffin JM, Masoumi A, et al. Coronavirus disease 2019 (COVID-19) and cardiovascular disease. Circulation. 2020;141(20):1648–1655. doi: 10.1161/CIRCULATIONAHA.120.046941. [DOI] [PubMed] [Google Scholar]
- 8.Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5(7):819–824. doi: 10.1001/jamacardio.2020.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xiong TY, Redwood S, Prendergast B, Chen M. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J. 2020;41(19):1798–1800. doi: 10.1093/eurheartj/ehaa231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5(7):802–810. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gao C, Wang Y, Gu X, Shen X, Zhou D, Zhou S, et al. Association between cardiac injury and mortality in hospitalized patients infected with avian influenza A (H7N9) virus. Crit Care Med. 2020;48(4):451–458. doi: 10.1097/CCM.0000000000004207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim IC, Kim HA, Park JS, Nam CW. Updates of cardiovascular manifestations in COVID-19: Korean experience to broaden worldwide perspectives. Korean Circ J. 2020;50(7):543–554. doi: 10.4070/kcj.2020.0205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sandoval Y, Januzzi JL, Jaffe AS. Cardiac Troponin for Assessment of Myocardial Injury in COVID-19: JACC review topic of the week. J Am Coll Cardiol. 2020;76(10):1244–1258. doi: 10.1016/j.jacc.2020.06.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 15.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bodor GS. Biochemical markers of myocardial damage. EJIFCC. 2016;27(2):95–111. [PMC free article] [PubMed] [Google Scholar]
- 17.Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018) Circulation. 2018;138(20):e618–51. doi: 10.1161/CIR.0000000000000617. [DOI] [PubMed] [Google Scholar]
- 18.Kim MS, Lee JH, Kim EJ, Park DG, Park SJ, Park JJ, et al. Korean Guidelines for diagnosis and management of chronic heart failure. Korean Circ J. 2017;47(5):555–643. doi: 10.4070/kcj.2017.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 20.Morrow DA, Velazquez EJ, DeVore AD, Prescott MF, Duffy CI, Gurmu Y, et al. Cardiovascular biomarkers in patients with acute decompensated heart failure randomized to sacubitril-valsartan or enalapril in the PIONEER-HF trial. Eur Heart J. 2019;40(40):3345–3352. doi: 10.1093/eurheartj/ehz240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee JH, Kim MS, Kim EJ, Park DG, Cho HJ, Yoo BS, et al. KSHF Guidelines for the management of acute heart failure: part i. definition, epidemiology and diagnosis of acute heart failure. Korean Circ J. 2019;49(1):1–21. doi: 10.4070/kcj.2018.0373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128(16):1810–1852. doi: 10.1161/CIR.0b013e31829e8807. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization. Shortage of personal protective equipment endangering health workers worldwide. [Updated 2020]. [Accessed June 5, 2020]. http://www.who.int/news-room/detail/03-03-2020-shortage-of-personal-protective-equipment-endangering-health-workers-worldwide.
- 24.Akhmerov A, Marbán E. COVID-19 and the heart. Circ Res. 2020;126(10):1443–1455. doi: 10.1161/CIRCRESAHA.120.317055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17(5):259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hu H, Ma F, Wei X, Fang Y. Coronavirus fulminant myocarditis saved with glucocorticoid and human immunoglobulin. Eur Heart J. 2020:ehaa190. doi: 10.1093/eurheartj/ehaa190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Doremalen N, Bushmaker T, Munster VJ. Stability of Middle East respiratory syndrome coronavirus (MERS-CoV) under different environmental conditions. Euro Surveill. 2013;18(38):20590. doi: 10.2807/1560-7917.es2013.18.38.20590. [DOI] [PubMed] [Google Scholar]
- 28.Kim IC, Kim JY, Kim HA, Han S. COVID-19-related myocarditis in a 21-year-old female patient. Eur Heart J. 2020;41(19):1859. doi: 10.1093/eurheartj/ehaa288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alhogbani T. Acute myocarditis associated with novel Middle east respiratory syndrome coronavirus. Ann Saudi Med. 2016;36(1):78–80. doi: 10.5144/0256-4947.2016.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maisch B, Portig I, Ristic A, Hufnagel G, Pankuweit S. Definition of inflammatory cardiomyopathy (myocarditis): on the way to consensus. A status report. Herz. 2000;25(3):200–209. doi: 10.1007/s000590050007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Demographic and clinical characteristics of whole study patients according to the cardiac injury score
Main findings and incidences of the electrical abnormality