Abstract
Objectives
To translate, cross-culturally adapt and validate a comprehensive evidence- and theoretically-based CR education intervention in Latin America.
Methods
First, best practices in translation and cross-cultural adaptation were applied through 6 steps. Then, the Spanish version was delivered to CR participants from programs in Colombia, Costa Rica and Peru for validation, such that the evaluation was pre-post, uncontrolled, pragmatic, observational, and prospective in design. Participants completed surveys assessing knowledge, health literacy, self-efficacy, and health behaviours. All outcomes were assessed pre-, and post-CR, as well as 6 months after CR completion.
Results
After translation of the patient guide from English to Spanish, 5 of the 9 booklets were culturally adapted. Two-hundred and forty-nine patients consented to participate, of which 184 (74 %) completed post-CR, and 121 (48 %) completed final assessments. There was a significant improvement in disease-related knowledge pre- to post-CR, as well as in health literacy, self-efficacy, and health behaviours (all p < 0.05). These gains were sustained 6 months post-program. With adjustment, CR attendance (i.e., exposure to the education) was associated with greater post-CR knowledge (ß = 0.026; p = 0.01).
Conclusion
A patient education intervention for CR patients in Latin America has been validated, and wider implementation is warranted.
Practice implications
Application of this first-ever validated CR education program for Spanish-speaking settings may result in secondary prevention.
Keywords: Cardiac rehabilitation, Patient education as topic, Follow-up studies, Latin America
1. Introduction
Cardiovascular diseases (CVD) are among the leading burdens of disease worldwide [1], with the highest rates of morbidity and mortality occurring in low-and middle-income countries (LMICs), such as in Latin America [2,3]. Cardiac rehabilitation (CR) is a well-established model of secondary prevention that mitigates this burden [4]. Despite the benefits, CR is only available in 40 % of LMICs [5], with grossly insufficient capacity even where it does exist. In Latin America for instance, there is only 1 spot each year for every 24 new ischemic heart disease cases [6].
CR has internationally-agreed core components such as structured exercise and patient education [7], which are also recommended in South American-specific CR guidelines [8]. Indeed, based on evidence of effectiveness [[9], [10], [11]], patient education is also a CR quality indicator [12]. In most Latin American countries however, patient education is not often delivered, and definitely not in a standardized way where it is [13]. This is despite our recent randomized controlled trial demonstrating it can be delivered in this region, and is effective [14].
Cardiac College™ is the only evidence-based and theoretically-informed comprehensive educational program for CR patients available globally, to our knowledge. The program specifically aims to help people learn about how cardiac disease is treated, to get active, eat healthy, feel well, and take control of their health. Cardiac College™ is mainly delivered in CR through a website (https://www.cardiaccollege.ca) and a patient guidebook (slides for group delivery also available upon request). The education program was developed by a multidisciplinary team of healthcare providers and patient partners, using a rigorous, theoretically-based process, as is described elsewhere [15]. Cardiac College™ has been tested in high- [16], as well as low- and middle-income settings [14], and shown to improve clinical outcomes, heart-health behaviours, and disease-related knowledge, as well as decrease morbidity, with maintenance of gains 1-year following CR. Cardiac College™ has been translated to 7 languages, but not Spanish.
Accordingly, the objectives of this study were (1) to develop and validate a Spanish version of Cardiac College™ for use in Latin American countries; this included consideration of satisfaction and adherence to sessions. Moreover, we aimed (2a) to assess the effects of this comprehensive educational program on knowledge (primary outcome); as well as (b) health behaviours (physical activity and diet) and exercise self-efficacy. It was hypothesized that there would be increases in these outcomes from pre- to post-CR, and that these improvements would be maintained through 6 months later.
2. Methods
2.1. Design
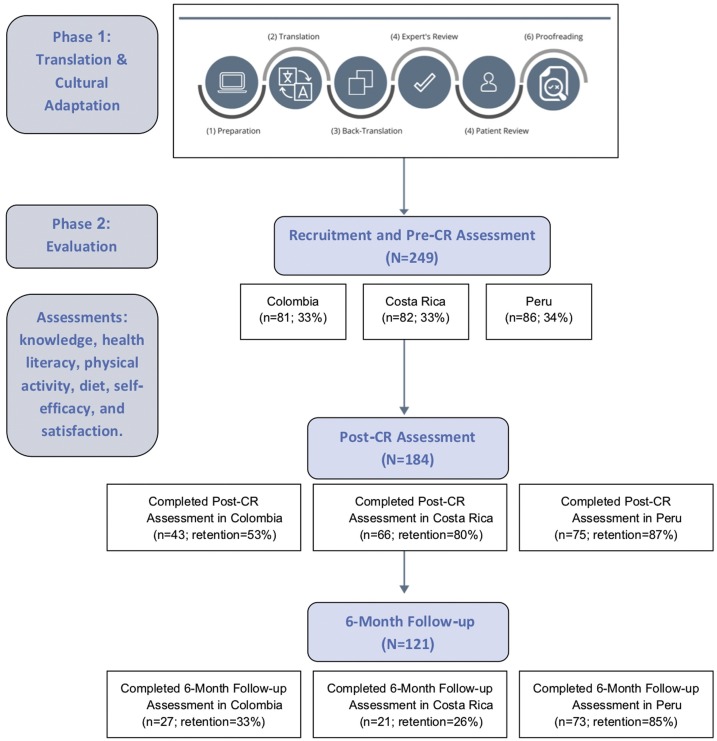
A multi-method design was used. Phase 1 comprised the translation and cultural adaptation of the educational intervention, and phase 2 comprised a multi-national observational and longitudinal study (Fig. 1 ). Ethics approval was obtained from the review board of all three hospitals where CR programs were located and the leading site in Canada. Phase 1 – translation and cultural adaptation – was undertaken between July 2017 and February 2018. Data for the evaluation (phase 2) were collected between June 2018 and December 2019. All participants provided written informed consent.
Fig. 1.
Flow Diagram of study Phases.
2.2. Procedure: translation and cultural adaptation
Best practices were followed in the translation and cross-cultural adaptation [17,18] of the Cardiac College™ guidebook. The process involved 6 steps (Fig. 1).
The first phase of preparation involved recruitment of key persons for the project (a team of healthcare providers in six countries (Brazil, Canada, Colombia, Costa Rica, Mexico and Peru), as well as two certified translators, and patient partners). The educational needs of the target audience were then considered, which involved an assessment of patient information needs (results reported elsewhere [19]; in brief, 184 participants from 3 Latin American countries completed the Information Needs in CR scale in Spanish, with results suggesting patients had high needs for education, particularly in the areas of emergency/safety. All areas where information needs were high were covered in Cardiac College™).
The second phase was the translation. Here, the original language version (English) of the Cardiac College™ was translated to Spanish, by two certified translators, who worked together to create one version of the translations of the materials. It is considered best practice that more than one translation be carried out; However, due to budget restrictions, only one translation was undertaken. The two independent translators were from different countries, and they worked to reach a consensus on the best terminology that would be applicable across Latin America.
This first translation was then back-translated to English (3rd phase) by members of the team who were native speakers of the target language and fluent in the source language. Then we compared the back-translated version with the original, to identify and investigate discrepancies between versions.
The expert review phase aimed to detect and deal with any translation discrepancies that arose across language versions, thus ensuring conceptual equivalence between the source and the target language version. Experts also reviewed content accuracy and checked cultural relevance. Translated materials were given to healthcare providers and other experts in each of the specific content areas from the guidebook (for example, a dietitian reviewed the nutrition chapters). These experts were from 6 Spanish-speaking countries.
These reviewed, culturally-adapted materials were then given to a convenience sample of 12 CR patients, who read 1–2 booklets each and were informally asked about clarity of the materials. No major issues were identified. Finally, the last step was proofreading where all members of the research team read the guidebook and raised any issues and identified typos. After this step, the guide was final and ready for evaluation.
2.3. Evaluation setting
The evaluation of the Spanish Cardiac College™ was conducted in three CR centers in Latin America: Mediagnostica Tecmedi S.A.S in Boyacá, Colombia; Hospital San Vicente de Paúl in Heredia, Costa Rica; and the National Cardiovascular Institute Carlos Alberto Peschiera Carrillo in Lima, Peru. Table 1 presents the characteristics of the three CR programs. CR participants at all three sites were offered supervised exercise classes 3 times a week for 8–24 weeks, and provided a home exercise prescription for the other days of the week. As shown, none of the programs had a structured educational intervention.
Table 1.
Characteristics of the 3 CR programs involved in the study.
| Country | Year of establishment | Annual volumes (patients/year) | Duration of the CR program (months) | Frequency of supervised CR sessions (per week) | Duration of exercise component of CR sessions (minutes) | Patient education provided prior to this study |
|---|---|---|---|---|---|---|
| Colombia | 1999 | 180 | 3 | 3 | 60 minutes | The education was delivered in groups or one-on-one, with a duration of 20−90 min per session. Group classes were led by a doctor, every 6 weeks |
| Costa Rica | 1987 | 150 | 6 | 3 | 60 minutes | Educational content is provided by a nutritionist, psychologist, social workers, pharmacist, endocrinologists, and the core CR team, but not structured (i.e. no formal education delivered). |
| Peru | 1994 | 1200 to 1400 | 2 | 3 | 60 minutes | No education provided prior to this study. |
2.4. Evaluation procedure
At each center, patients were invited to participate in the study during their initial assessment. Consenting patients were invited to complete a self-administered survey in paper format (pre-CR survey) and wear a pedometer for 7 days. The survey included sociodemographic items, and psychometrically-validated scales to assess knowledge and health behaviours. Clinical data were extracted from patient records.
2.4.1. Intervention
Education was pragmatically delivered using the translated and culturally-adapted Spanish version of the Cardiac College™guidebook in 7–24 sessions (see Appendix for content offerings in each session by site), with session duration varying from 20−30 min. The education was provided by an interdisciplinary team of healthcare providers from each program and guided by the content of the guidebook. Sessions were delivered before or after exercise sessions in large or small groups. In accordance with the Health Action Process Approach and adult learning principles on which it is based [20,21], each section in the guidebook includes activities to support patient implementation of the information in Cardiac College™, including goal-setting and action planning, which were carried out in the sessions [15].
At the end of their CR program, patients were approached to complete the post-CR survey and asked to wear the pedometer again for 7 days. The post-CR survey assessed knowledge and health behaviours as per the initial survey, as well as patient satisfaction with the education received. Patient records were reviewed to ascertain degree of CR participation and completion (i.e., patient continued to attend sessions and completed post-program clinical assessment). Finally, 6 months after discharge from CR, participants were contacted by phone and invited to come to the CR centers to complete a follow-up survey, comprising the same assessments (Fig. 1).
2.5. Evaluation participants
CR patients (with coronary artery disease or multiple cardiovascular risk factors) recruited from the three CR programs in Latin America were included. The exclusion criteria were: lack of Spanish-language proficiency, and any visual, cognitive or serious psychiatric condition that would preclude the participant from completing the surveys.
Sample size was based on conservative calculations of an expected small-to-moderate effect size (d = 0.25) for knowledge, with a statistical power of 0.95 and alpha of 0.025. A total sample size of n = 50 at each site was deemed necessary based on these parameters. Calculations were made with GPower 3.1 using the following parameters: F-test, ANOVA repeated measures, within factors, number of groups = 1, number of measurements = 3, correlation among repeated measures = 0.5, and non-sphericity correction ε = 0.99. Anticipating a 60 % retention rate based on similar studies,1416 a minimum of 84 participants were required to achieve a final sample size of 50 per site. Patients were approached consecutively until the required sample size was achieved.
2.6. Measures
Clinical characteristics extracted from medical records included: CR referral indication and cardiac risk factors. All participant surveys were administered in Spanish. Participants self-reported their sociodemographic characteristics in the pre-CR assessment, which included ethnicity, highest educational attainment and family income.
Knowledge, health literacy, physical activity, diet, and exercise self-efficacy were assessed at pre-CR, post-CR (site-specific), and 6-month follow-up using psychometrically-validated scales as outlined below. Post-CR, all participants also completed a Cardiac College™ satisfaction survey created for purpose, which included Likert-type, yes/no and open-ended questions.
2.6.1. Primary outcome: knowledge
Knowledge was assessed using the short version of the Coronary Artery Disease Education Questionnaire (CADE-Q SV) which consists of 20 items- four in each of the following 5 domains: medical condition, risk factors, exercise, nutrition, and psychosocial risk. Response options are true/false/I don't know, with each correct answer equal to one point. Therefore, the maximum score possible is 20 overall, four for each domain, with higher scores indicating better knowledge. The CADE-Q SV is validated [22], including the Spanish version [23].
2.6.2. Other outcomes
CR utilization is described above. Health literacy was measured using both the Medical Term Recognition Test (METER) [24] and the Newest Vital Sign (NVS) survey which measures nutrition literacy specifically [25]. The METER consists of 40 medical terms and 30 non-words. Respondents are instructed to mark which words they recognize as actual words. Scores are based on the number of “true hits”, or actual medical terms the respondent correctly identified. Score ranges of 0–20, 21–34, and 35–40 indicate low, marginal and functional health literacy, respectively. In the NVS, respondents are asked to answer six questions regarding the information found on an accompanying nutrition label such as, “If you eat the entire container, how many calories will you eat?” Each correct response is worth one point, for a total of six points possible. Scores equal or greater than four are considered evidence of adequate health literacy.
Exercise self-efficacy was assessed using Bandura’s 18-item exercise self-efficacy (ESE) scale, which has been shown to be a valid measure of exercise beliefs in adults with chronic diseases [26]. Bandura’s original scale asked participants to rate how certain they were that they could perform their exercise routine regularly (three or more times per week), under a range of conditions. This was modified to reflect current physical activity guideline recommendations to exercise most days of the week [27]. A plain language expert reviewed the tool; the final administered version of the scale read: “How confident are you that you can exercise most days of the week?” Participants responded on a 5-point Likert scale ranging from 1= “not confident at all” to 5= “very confident”. These changes were made with the consent of the original author.
The health behaviours evaluated were physical activity and food intake. Number of steps per day was assessed using the PiezoRx® pedometer. Participants were asked to wear this device on their right hip for seven days (preferably seven consecutive days before CR intake and discharge) at all 3 assessments, from the time of waking up until the time of going to bed. They were provided a log to record their daily total number of steps. The PiezoRx® is a research-grade uniaxial accelerometer-based physical activity monitor that uses step rate thresholds to measure intensity related physical activity. It has been shown to be valid and reliable in different groups, including adults [28]. Mean steps per day were computed, with 7500 considered commensurate with guideline recommendations for 150 min/week in chronic disease populations [29].
Food intake was assessed by the Mediterranean Diet Score (MDS) tool [30], which consists of 13 questions on food consumption frequency and food intake habits considered characteristic of the Mediterranean diet. The total score ranges from 0 to 13; scores ≤ 5 are interpreted as low adherence to a MD and to ≥ 10 a high adherence to MD.
2.7. Statistical analysis
SPSS Version 26.0 (IBM Inc 2019, NYC) was used. First, descriptive statistics were computed to describe participants’ sociodemographic and clinical characteristics overall. Retention for the post-CR and 6-month follow-up was considered; differences in the sociodemographic and clinical characteristics of participants retained versus lost to follow-up were tested using t-tests or chi-square as appropriate.
Second, descriptive statistics were used to describe satisfaction with the education intervention, adherence to educational classes and drop-out. Pearson correlation coefficients were used to determine the associations between satisfaction, knowledge and adherence to educational classes. T-tests were used to test the difference in knowledge between participants that completed the CR program and drop-outs.
Third, paired t-tests were used to investigate outcome changes between assessments (i.e. pre- and post-CR when improvements were hypothesized based on exposure to the intervention, and post-CR and follow-up during which maintenance was hypothesized). Given that multiple tests were being performed to test each outcome, a more conservative p < 0.01 was applied to denote statistical significance. Finally, given the effect of education, health literacy among other factors on knowledge, multiple regression was performed to test whether an association between Cardiac College adherence and total knowledge was sustained with adjustment for these factors. Variables where p < 0.01 in binary analysis were included in the adjusted model.
3. Results
3.1. Translation and cultural adaptation of cardiac college to spanish
Through the 6-step translation and cross-cultural adaptation process (Fig. 1), the Spanish Cardiac College™ was developed. Five of the 9 booklets were culturally-adapted; a summary of these changes is reported in Table 2 . The final guidebook can be found online at: https://www.healtheuniversity.ca/es/CardiacCollege/Pages/default.aspx.
Table 2.
Summary of cultural adaptations to educational materials.
| Content Area | Booklet | Cultural Adaptations |
|---|---|---|
| Treat Heart Disease | 1. How your heart works and common types of heart problems | Risk factor profile tool was revised to reflect targets in national guidelines. |
| 2. Common tests and treatments for heart disease | No adaptations | |
| 3. Taking your heart medicines | Names and brands of medications were revised to reflect what is prescribed in each country. | |
| 4. Managing your symptoms | Emergency numbers were adapted to each country. Units were also revised to national measurement system. | |
| Get Active | 5. Staying active for a healthy heart | Some terms were adapted to Latin America culture (example: “weight training” replaced by “resistance training”). |
| In some countries, cardiopulmonary assessments are performed by medical doctors, physiotherapists or physical educators (not technicians), so this was revised accordingly. | ||
| Volunteers are not common in CR programs in Latin America, so reference to volunteers was removed. | ||
| Usually, exercise classes in these countries occur more than once a week, so reference to “weekly classes” was removed. | ||
| Eat Healthy | 6. Eating well for a healthy heart | Nutritional information was adapted to match Latin American food guide and national nutrition recommendation. Food examples were revised: some added and others deleted to reflect local eating habits. |
| Feel Well | 7. Managing stress for a healthy heart | No adaptations |
| 8. Enjoying a healthy relationship and sexual intimacy | No adaptations | |
| Take Control | 9. Setting goals for a healthy heart | No adaptations |
3.2. Evaluation
3.2.1. Participant characteristics
A flow diagram is shown in Fig. 1. Table 3 presents the sociodemographic and clinical characteristics of participants pre-CR, and Table 4 displays their baseline knowledge, health literacy and behaviours. Overall, 52 (21.1 %) had functional health literacy at pre-test. Participants were quite active.
Table 3.
Participants’ sociodemographic and clinical characteristics by assessment point and retention status.
| n (%) / mean ± SD | Pre-CR (N = 249) | Post-CR |
6-Month Follow-up |
|||||
|---|---|---|---|---|---|---|---|---|
| Retained (n = 184) | Lost to follow-up (n = 65) | p | Retained (n = 121) | Lost to follow-up (n = 128) | p | |||
| Sociodemographic | ||||||||
| Sex (% male) | 185 (74.3) | 139 (75.5) | 46 (70.8) | 0.47 | 96 (79.3) | 89 (69.5) | 0.08 | |
| Age (years) | 61.3 ± 11.8 | 61.0 ± 11.2 | 62.4 ± 13.4 | 0.45 | 61.1 ± 12.3 | 61.5 ± 11.4 | 0.79 | |
| Education (% low*) | 60 (24.2) | 40 (21.9) | 20 (30.8) | 0.18 | 25 (20.7) | 35 (27.3) | 0.21 | |
| Monthly income (% low†) | 114 (53.3) | 75 (48.7) | 39 (65.0) | 0.03 | 54 (50.5) | 60 (56.1) | 0.41 | |
| Clinical | ||||||||
| CR indication (% yes) | ||||||||
| Myocardial infarction | 133 (53.4) | 100 (54.3) | 33 (50.8) | 0.62 | 63 (52.1) | 70 (54.7) | 0.68 | |
| PCI | 131 (52.6) | 96 (52.2) | 35 (53.8) | 0.82 | 63 (52.1) | 68 (53.1) | 0.87 | |
| Bypass surgery | 34 (13.7) | 27 (14.7) | 7 (10.8) | 0.41 | 25 (20.7) | 9 (7.0) | <0.01 | |
| Angina | 47 (18.9) | 36 (19.6) | 11 (16.9) | 0.63 | 23 (19.0) | 24 (18.8) | 0.96 | |
| HF | 28 (11.2) | 21 (11.7) | 7 (10.8) | 0.88 | 14 (11.7) | 14 (10.9) | 0.86 | |
| Risk factors (% yes) | ||||||||
| Hypertension | 158 (63.5) | 121 (65.8) | 37 (56.9) | 0.22 | 75 (62.0) | 83 (64.8) | 0.64 | |
| Dyslipidemia | 175 (70.3) | 125 (67.9) | 50 (76.9) | 0.16 | 71 (58.7) | 104 (81.3) | <0.001 | |
| Obesity | 109 (43.8) | 70 (38.0) | 39 (60.0) | <0.01 | 43 (35.5) | 66 (51.6) | 0.01 | |
| Diabetes type 1 | 6 (2.4) | 3 (1.6) | 3 (4.6) | 0.29 | 2 (2.5) | 2 (2.3) | 0.95 | |
| Diabetes type 2 | 54 (21.7) | 36 (19.6) | 18 (27.7) | 0.20 | 22 (18.2) | 32 (25.0) | 0.19 | |
| Smoking (% current) | 48 (19.3) | 39 (21.2) | 9 (13.8) | 0.17 | 33 (27.3) | 15 (11.7) | <0.01 | |
| Alcohol consumption | 21 (8.4) | 15 (8.2) | 6 (9.2) | 0.80 | 12 (9.9) | 9 (7.0) | 0.42 | |
| Depression | 19 (7.6) | 16 (8.7) | 3 (4.6) | 0.23 | 12 (9.9) | 7 (5.5) | 0.19 | |
| Sleep apnea | 16 (6.4) | 12 (6.5) | 4 (6.2) | 0.92 | 7 (5.8) | 9 (7.0) | 0.69 | |
SD, standard deviation; PCI, percutaneous coronary intervention; HF, heart failure; CR, cardiac rehabilitation.
Did not complete high school.
Less than US$700 per month.
Table 4.
Impact of education intervention.
| mean ± SD | Maximum Score | Pre-CR (N = 249) | Post-CR (n = 184) | Change | 6 Month Follow-up (n = 121) | Change |
|---|---|---|---|---|---|---|
| Knowledge | 20 | 13.64 ± 2.73 | 15.38 ± 2.36 | 1.74** | 15.41 ± 1.96 | 0.03 |
| Medical | 4 | 2.48 ± 0.75 | 2.63 ± 0.67 | 0.15* | 2.65 ± 0.59 | 0.02 |
| Risk factors | 4 | 2.68 ± 0.59 | 2.81 ± 0.55 | 0.13 | 2.83 ± 0.51 | 0.02 |
| Exercise | 4 | 2.55 ± 1.07 | 3.22 ± 0.90 | 0.67** | 3.16 ± 0.93 | −0.06 |
| Nutrition | 4 | 3.29 ± 0.83 | 3.64 ± 0.66 | 0.35** | 3.73 ± 0.56 | 0.09 |
| Psychosocial risk | 4 | 2.63 ± 0.96 | 3.08 ± 0.83 | 0.45** | 3.04 ± 0.83 | −0.04 |
| Health literacy - METER | 40 | 26.41 ± 12.25 | 30.37 ± 9.60 | 3.96** | 29.31 ± 11.41 | −1.06 |
| Health literacy - NVS | 6 | 2.59 ± 1.97 | 3.26 ± 2.08 | 0.67** | 3.05 ± 2.15 | −0.21 |
| Exercise self-efficacy | 5 | 3.14 ± 0.95 | 3.54 ± 0.87 | 0.40** | 3.48 ± 0.82 | −0.06 |
| Exercise (steps / day) | – | 7752.43 ± 3635.31 | 9180.39 ± 4497.24 | 1427.96** | 9502.83 ± 4223.91 | 322.44 |
| Diet | 13 | 7.85 ± 2.16 | 9.10 ± 2.20 | 1.25** | 9.25 ± 2.09 | 0.15 |
Differences between first and second assessment, and second and third assessment using paired t-test: *p < 0.01**p < 0.001.
SD, standard deviation; METER, Medical Term Recognition Test; NVS, Newest Vital Sign.
A comparison of characteristics among those retained versus lost to follow-up post-CR and at the 6-month follow-up is found also in Table 3. As shown, there was minimal retention bias, only with regard to income, bypass surgery as CR indication, and having obesity, dyslipidemia as well as smoking as risk factors.
3.2.2. Satisfaction and adherence
The mean percentage of adherence to scheduled CR exercise sessions was 83.0 ± 12.1 % (standard deviation). The mean percentage of adherence to educational sessions was 65.2 ± 26.9 %. Sixty-five (26.1 %) participants dropped out of CR (Table 3).
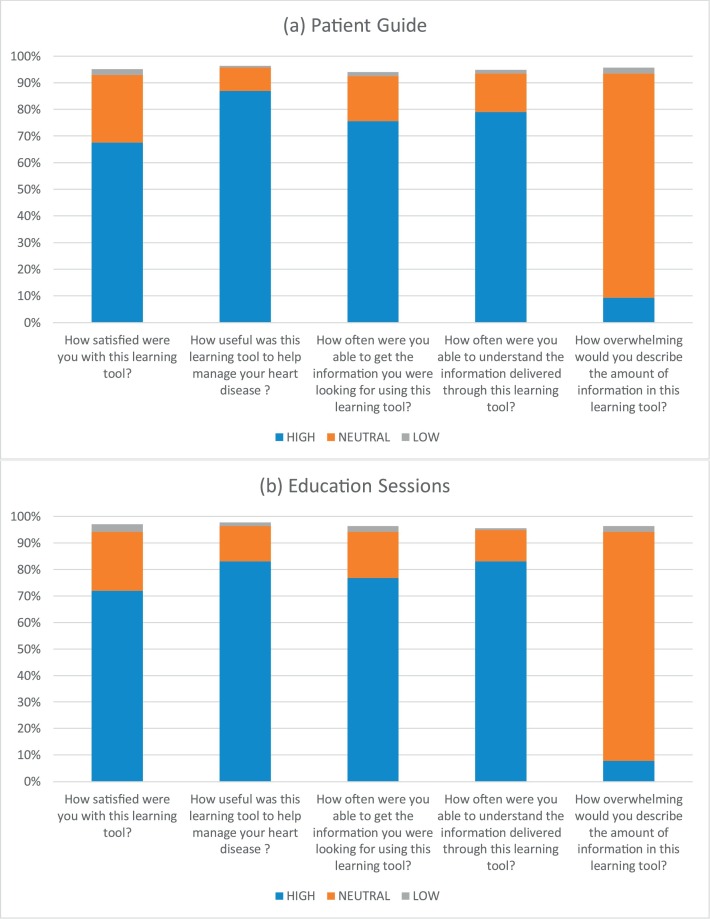
Participants’ satisfaction with the patient guidebook and education sessions provided is reported in Fig. 2 . Overall, participants were very satisfied with both, confirming both the printed materials and sessions as very useful to them in getting the information they were looking for and helping them manage their condition. The topic (see Appendix) with which patients had the highest satisfaction was healthy eating (2.75 ± 0.48/4); the lowest satisfaction was with relapse prevention (2.22 ± 0.90/4). When asked how many times participants used the patient guide in the past month outside of CR classes, 75 (41.0 %) responded they used it between 5 and 10 times, and 55 (30.0 %) more than 10 times. Finally, 46 (25.2 %) participants responded that if they had a question about heart disease and healthy living, the first thing they would do was to read the patient guidebook.
Fig. 2.
Participants’ satisfaction with the Spanish (a) patient guide and (b) education sessions, N = 184 (Note: the last item on right is reverse-worded).
Simple linear regression analysis (Table 5 ) revealed that education level, pre-CR knowledge, and attendance at the CR education sessions were associated with post-CR knowledge. The multiple regression analysis model was significant (F = 13.51, p < 0.001), but with low power (R2 = 0.21). This model showed that with adjustment, attendance at the education sessions remained associated with post-CR knowledge.
Table 5.
Simple and multiple regression analysis testing association with total post-CR knowledge.
| Simple regression |
Multiple regression |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables | β | SE | p | 95 % CI Lower Bound | 95 % CI Upper Bound | β | SE | p | 95 % CI Lower Bound | 95 % CI Upper Bound |
| Age | −0.015 | 0.016 | 0.34 | −0.046 | 0.016 | – | – | – | – | – |
| Sex | −0.489 | 0.403 | 0.23 | −1.285 | 0.307 | – | – | – | – | – |
| Highest Education | 0.512 | 0.102 | <0.001 | 0.310 | 0.713 | 0.430 | 0.102 | <0.001 | 0.229 | 0.630 |
| Family income | −0.152 | 0.156 | 0.33 | −0.460 | −0.157 | – | – | – | – | – |
| Pre-CR knowledge | 0.205 | 0.064 | 0.002 | 0.078 | 0.331 | 0.188 | 0.061 | 0.002 | 0.068 | 0.309 |
| Satisfaction – patient guide | −0.004 | 0.002 | 0.12 | −0.008 | 0.001 | – | – | – | – | – |
| Satisfaction - education sessions | −0.004 | 0.002 | 0.11 | −0.008 | 0.001 | – | – | – | – | – |
| # education sessions attended | 0.026 | 0.01 | 0.01 | 0.045 | 0.007 | 0.02 | 0.009 | 0.01 | 0.04 | 0.005 |
SE, standard e.
3.2.3. Impact of education intervention
Mean scores of all outcome measures at each time point are presented in Table 4. Pre-program, nutrition knowledge was highest, and medical lowest. As shown, there was a significant increase from pre- to post-CR in the primary outcome total knowledge, as well as in 4/5 knowledge areas, namely medical content, exercise, nutrition, and psychosocial risk. The biggest increase in knowledge was in the area of exercise. This did not decay 6 months later.
With regards to the two measures of health literacy (METER and NVS), both increased significantly at post-CR when compared to pre-CR (Table 4). The number of participants with functional health literacy measured by METER increased to 65 (35.7 %) post-program, and by NVS increased to 93 (54.4 %). As above, participants maintained these gains at the 6-month follow-up assessment.
As also shown in Table 4, self-efficacy increased was significantly greater post-CR when compared to pre-CR. Participants maintained these gains at the 6-month follow-up assessment. With regards to heart-health behaviors, mean steps per day increased significantly from pre- to post-CR, and these results were maintained at the 6-month follow-up assessment. Participants that were reaching the recommended 7500 steps per day increased from 47.8 % pre-CR, to 64.2 % post-CR, and 70.0 % at the 6-month follow-up assessment. With regard to food intake, MDS scores also increased significantly from pre- to post-CR, and these results were also maintained at the 6-month follow-up assessment. The percentage of participants with high adherence to the Mediterranean diet increased from 22.0 % pre-CR to 46.3 % post-CR.
4. Discussion and conclusion
4.1. Discussion
Consistent with prior studies on structured educational interventions for cardiac patients [14,16,31,32], our findings confirm their benefit in supporting patients’ adherence to CR programs, and increasing knowledge and behaviour change as well, but in a Spanish-speaking setting for the first time to our knowledge. Previous studies have also demonstrated an effect of this education intervention on lower morbidity up to 12 months later in LMICs [33], which could be cost-saving to health systems, as well as on improvements in cardiorespiratory fitness [14], which is associated with lower mortality. The results of this study are also particularly encouraging considering previous studies have shown that improvements achieved during CR are not well-maintained in the short- and long-term, including exercise [34,35] and diet [36]; we found no decay through 6 months. This too could result in lower mortality and morbidity over the long-term.
An important finding of this study was related to health literacy, which is critical since it enables patients to understand their treatments, communicate with healthcare providers, and navigate the complexities of the healthcare system [37,38]. Although several studies have reported a direct association between health literacy and knowledge in cardiac patients [38], increases in health literacy after education interventions are not commonly observed, as they are with knowledge levels. This may be because most studies are performed in high-income countries, where CR participants are more health-literate and educated [39]. In the present study, patient scores on both validated measures of health literacy increased significantly from pre to post-CR, and these gains were maintained at the 6-month follow-up assessment. That this intervention supported improvements of health literacy in patients in LMICs is a novel finding, and whether this can support patients in optimally navigating their future cardiac and other chronic disease care (and potentially then even receive better care as they understand and hence ask questions and follow-up on physician recommendations), and also better self-manage, with resulting benefits in morbidity and mortality, warrant investigation.
Caution is warranted in interpreting the findings of this study. The first limitation is related to design. This was not a randomized study, so no causal conclusions can be drawn. Moreover, the design did not incorporate a control or comparison condition, so one cannot rule out that improvements may have been seen without the intervention (e.g., the exercise sessions alone) or due to the natural recovery from a cardiovascular event and informal education that people are exposed to from friends, family, CR staff and other patients. However, we tested the association between number of sessions attended and knowledge, and the significant association suggests the intervention was effective. Moreover, our randomized controlled trial with the Portuguese version demonstrated exposure to the education intervention resulted in improvements in several outcomes, over and above both usual care and exercise alone [15,33]. In addition, without a comparison or control group, we cannot rule out practice effects for the knowledge and health literacy scales. There was a considerable period of time between testing however, and as per our previous research where we have had a control group and randomization, we found significantly greater knowledge using the same scale in intervention participants compared to controls (health literacy was not an outcome, so this does require testing) [40].
The second limitation is related to generalizability of results, which is limited for several reasons. Although this study was undertaken in three different countries, it is unknown how generalizable this intervention and the effects would be to other Spanish-speaking countries (especially those outside Latin America or those that are higher-income). Moreover, there may have been selection bias, because patients who access CR are likely more advantaged than those who do not. However, we cannot establish if selection bias exists, because centers did not track individual participant recruitment and response rate. Finally, retention post-CR was strong, but was not sustained at the subsequent follow-up, resulting in some retention bias. Replication is warranted, using a more generalizable sample, control group, randomization, and financial incentives for retention.
4.2. Conclusions
In conclusion, this first-ever structured, comprehensive and theory-based education intervention for Spanish-speaking cardiac patients developed based on local guidelines [8] and patients’ information needs [19] was highly satisfactory to patients. Through this study, the effectiveness of this education intervention was also demonstrated; it significantly increased knowledge across multiple domains, health literacy, as well as exercise and diet (all outcomes assessed), and these increases were maintained through 6 months. The encouraging results of this study support the value of implementing tailored educational initiatives to patients in low-resource settings, where need for information and secondary prevention are greatest.
4.3. Practice implications
Results from this study support the implementation of this translated, culturally-adapted and validated education intervention, in various Spanish-speaking settings. Results showed that the content can be adapted across different CR model/program constellations, in low-resource settings, and still be effective. Indeed, implementation fidelity in these LMICs was high; despite differences in frequency of sessions and duration of programs across these countries, all three centers successfully delivered all content, adapted to their program models. This demonstrates the feasibility of implementing this education intervention in “real-world” LMIC settings (i.e. adapted to 3 different CR programs), with efficacy. CR programs should consider this educational program (available also in Portuguese and French at same URL), then adapt and implement it based on their resources, as well as patient needs and preferences. Indeed, the greatest need for CR exists in India and China [41]; we are currently evaluating translations to Hindi, Punjabi and simplified Chinese.
Even before the COVID-19 pandemic, the English version of Cardiac College™ was adapted to an online mode of delivery, to enable greater access and reach. Patients could complete modules independently weekly, including the implementation activities, and CR supervisors could monitor progress(https://www.healtheuniversity.ca/EN/CardiacCollege/THRIVE/). Indeed, previous reviews have demonstrated the equivalence of eCR [42]. During the COVID-19 pandemic [43], the sessions are being delivered free, openly weekly to patients online in a live, group setting (see: https://www.healtheuniversity.ca/EN/CardiacCollege/Pages/learn-online.aspx; past sessions also posted). Evaluation is underway. Given penetration of technology in LMICs, this may prove to be a promising delivery modality in terms of reach and cost-efficiency.
Authorship statement
GLMG, CVA, XG, RF, DQ: substantial contributions to the conception or design of the work; the acquisition, analysis and interpretation of data for the work. SLG, PO: substantial contributions to the conception and interpretation of data for the work. BAL, PR, EC, RSM, JFC, MHN, RPV: substantial contributions to the acquisition and interpretation
Funding
This work was supported by Toronto Rehab Foundation.
CRediT authorship contribution statement
Gabriela Lima de Melo Ghisi: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing - original draft, Writing - review & editing. Sherry L. Grace: Formal analysis, Writing - original draft, Writing - review & editing. Claudia V. Anchique: Conceptualization, Data curation, Investigation, Project administration, Resources, Supervision, Writing - review & editing. Ximena Gordillo: Project administration, Resources, Writing - review & editing. Rosalía Fernandez: Conceptualization, Data curation, Investigation, Project administration, Resources, Supervision, Writing - review & editing. Daniel Quesada: Conceptualization, Data curation, Investigation, Project administration, Resources, Supervision, Writing - review & editing. Blanca Arrieta Loaiciga: Project administration, Resources, Writing - review & editing. Patricia Reyes: Project administration, Resources, Writing - review & editing. Elena Chaparro: Project administration, Resources, Writing - review & editing. Renzo Soca Meza: Project administration, Resources, Writing - review & editing. Julia Fernandez Coronado: Project administration, Resources, Writing - review & editing. Marco Heredia Ñahui: Project administration, Resources, Writing - review & editing. Rocio Palomino Vilchez: Project administration, Resources, Writing - review & editing. Paul Oh: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing - review & editing.
Declaration of Competing Interest
The authors reported no declarations of interest.
Acknowledgements
We would like to acknowledge Dr Oscar Javier López León Murguía and Dr Tania Hinojosa López from Universidad de Guadalajara (Mexico) for their help with the cultural adaptation of the educational materials. The team is Peru would like to acknowledge the following professionals that helped with the study: Olga Orosco, Lorenzo Baez, Ruth Cañari, Winston Dávila, and Christian Arriola.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.pec.2020.10.008.
Appendix A. Supplementary data
The following is supplementary data to this article:
References
- 1.Mendis S., Puska P., Norrving B. World Health Organization; Geneva: 2011. Global Atlas on Cardiovascular Disease Prevention and Control. [Google Scholar]
- 2.Roth G.A., Johnson C., Abajobir A., Abd-Allah F., Abera S.F., Abyu G., Ahmed M., Aksut B., Alam T., Alam K. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017;70:1–25. doi: 10.1016/j.jacc.2017.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fernando L., Pamela S., Alejandra L. Cardiovascular disease in Latin America: the growing epidemic. Prog. Cardiovasc. Dis. 2014;57:262–267. doi: 10.1016/j.pcad.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 4.Oldridge N., Taylor R.S. Cost-effectiveness of exercise therapy in patients with coronary heart disease, chronic heart failure and associated risk factors: a systematic review of economic evaluations of randomized clinical trials. Eur. J. Cardiovasc. Prev. Rehabil. 2020;27:1045–1055. doi: 10.1177/2047487319881839. [DOI] [PubMed] [Google Scholar]
- 5.Pesah E., Turk-Adawi K., Supervia M., Lopez-Jimenez F., Britto R., Ding R., Babu A., Sadeghi M., Sarrafzadegan N., Cuenza L. Cardiac rehabilitation delivery in low/middle-income countries. Heart. 2019;105:1806–1812. doi: 10.1136/heartjnl-2018-314486. [DOI] [PubMed] [Google Scholar]
- 6.Chacin Suarez A., Grace S.L., Supervia M. Cardiac rehabilitation availability and characteristics in Latin America and the Caribbean: a global comparison. Rev. Esp. Cardiol. 2020 doi: 10.1016/j.ahj.2021.05.010. [under review] [DOI] [PubMed] [Google Scholar]
- 7.Grace S.L., Turk-Adawi K.I., Contractor A., Atrey A., Campbell N.R.C., Derman W., Ghisi G.L.M., Sarkar B.K., Yeo T.J., Lopez-Jimenez F. Cardiac rehabilitation delivery model for low-resource settings: an international council of cardiovascular prevention and rehabilitation consensus statement. Prog. Cardiovasc. Dis. 2016;59:303–322. doi: 10.1016/j.pcad.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 8.Herdy A., López-Jiménez F., Terzic C., Milani M., Stein R., Carvalho T., Serra S., Araujo C., Zeballos P., Anchique C. South American guidelines for cardiovascular disease prevention and rehabilitation. Arq. Bras. Cardiol. 2014;103:1–31. doi: 10.5935/abc.2014s003. [DOI] [PubMed] [Google Scholar]
- 9.de G.L., Ghisi M., Abdallah F., Grace S.L., Thomas S., Oh P. A systematic review of patient education in cardiac patients: do they increase knowledge and promote health behavior change? Patient Educ. Couns. 2014;95:160–174. doi: 10.1016/j.pec.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 10.Anderson L., Brown J.P., Clark A.M., Dalal H., Rossau H.K.K., Bridges C., Taylor R.S. Patient education in the management of coronary heart disease. Cochrane Database Syst. Rev. 2017;6 doi: 10.1002/14651858.CD008895.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barnason S., White-Williams C., Rossi L.P., Centeno M., Crabbe D.L., Lee K.S., McCabe N., Nauser J., Schulz P., Stamp K. Evidence for therapeutic patient education interventions to promote cardiovascular patient self-management: a scientific statement for healthcare professionals from the American Heart Association. Circ. Cardiovasc. Qual. Outcomes. 2017;10 doi: 10.1161/HCQ.0000000000000025. [DOI] [PubMed] [Google Scholar]
- 12.Moghei M., Oh P., Chessex C., Grace S.L. Cardiac rehabilitation quality improvement: a narrative review. J. Cardiopulm. Rehabil. Prev. 2019;39:226–234. doi: 10.1097/HCR.0000000000000396. [DOI] [PubMed] [Google Scholar]
- 13.Chaves G., Turk-Adawi K., Supervia M., Santiago de Araújo Pio C., Abu-Jeish A., Mamataz T., Tarima S., Lopez Jimenez F., Grace S.L. Cardiac rehabilitation dose around the world. Circ. Cardiovasc. Qual. Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.119.005453. [DOI] [PubMed] [Google Scholar]
- 14.Chaves G.S.S., Ghisi G.L.M., Grace S.L., Oh P., Ribeiro A.L., Britto R.R. Effects of comprehensive cardiac rehabilitation on functional capacity in a middle-income country: a randomized trial. Heart. 2019;105:406–413. doi: 10.1136/heartjnl-2018-313632. [DOI] [PubMed] [Google Scholar]
- 15.Ghisi G.L.M., Scane K., Sandison N., Maksymiu S., Skeffington V., Oh P. Development of and educational curriculum for cardiac rehabilitation patients and their families. J. Clin. Experiment Cardiol. 2015;6:5. doi: 10.4172/2155-9880.1000373. [DOI] [Google Scholar]
- 16.Ghisi G.L.M., Rouleou F., Ross M.K., Dufoir-Doiron M., Belliveau S.L., Brideau J.R., Aultman C., Thomas S., Colella T., Oh P. Effectiveness of an education intervention among cardiac rehabilitation patients in Canada: a multi-site study. Can. J. Cardiol. Open. 2020;4(March) doi: 10.1016/j.cjco.2020.02.008. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nierkens V., Hartman M.A., Nicolaou M., Vissenberg C., Beune E.J.A.J., Hosper K., van Valkengoed I.G., Stronks K. Effectiveness of cultural adaptations of interventions aimed at smoking cessation, diet, and/or physical activity in ethnic minorities. A systematic review. PLoS One. 2013;8:e73373. doi: 10.1371/journal.pone.0073373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ace Concern England . 2006. Communicating With Diverse Audience: a Practical Guide to Producing Translated Materials in Appropriate Languages and Formats for People From Minorities Ethnic Communities.https://www.ageuk.org.uk/documents/en-gb/for-professionals/equality-and-human-rights/379_1105_communicating_with_diverse_audiences_2006_pro.pdf?dtrk=true [Google Scholar]
- 19.de M. Ghisi G.L., Anchique C.V., Fernandez R., Quesada-Chaves D., Gordillo M.X., Acosta S., Fernandez J., Arrieta-Loaiciga B., Heredia M., Oh P. Validation of a spanish version of the information needs in cardiac rehabilitation scale to assess information needs and preferences in cardiac rehabilitation. J. Cardiovasc. Nurs. 2018;33:E29–E34. doi: 10.1097/JCN.0000000000000505. [DOI] [PubMed] [Google Scholar]
- 20.Ghisi G.L.M., Grace S.L., Thomas S., Oh P. Behavior determinants among cardiac rehabilitation patients receiving educational interventions: an application of the health action process approach. Patient Educ. Couns. 2015;98:612–621. doi: 10.1016/j.pec.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 21.Zhang C.Q., Zhang R., Schwarzer R., Hagger M.S. A meta-analysis of the health action process approach. Health Psychol. 2019;38:623–637. doi: 10.1037/hea0000728. [DOI] [PubMed] [Google Scholar]
- 22.de G.L., Ghisi M., Sandison N., Oh P. Development, pilot testing and psychometric validation of a short version of the coronary artery disease education questionnaire: the CADE-Q SV. Patient Educ. Couns. 2016;99:443–447. doi: 10.1016/j.pec.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 23.Ghisi G.L.M., Fernandez R., Quesada D., Anchique C., Gordillo Z., Loaiciga B.A., Reyes P., Oh P. Translation, adaptation, and psychometrically validation of an instrument to assess disease-related knowledge in Spanish-speaking cardiac rehabilitation participants: the Spanish CADE-Q SV. Heart Lung. 2020 doi: 10.1016/j.hrtlng.2020.07.016. [under review] [DOI] [PubMed] [Google Scholar]
- 24.Rawson K.A., Gunstad J., Hughes J., Spitznagel M.B., Potter V., Waechter D., Rosneck J. The METER: A brief, self-administered measure of health literacy. J. Gen. Intern. Med. 2009;25:67–71. doi: 10.1007/s11606-009-1158-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singh R., Coyne L.S., Wallace L.S. Brief screening items to identify spanish-speaking adults with limited health literacy and numeracy skills. BMC Health Serv. Res. 2015;15:374. doi: 10.1186/s12913-015-1046-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bandura A. Information Age Publishing; Greenwich: 2006. Guide for Constructing Self-efficacy Scales; pp. 307–337. [Google Scholar]
- 27.Piercy K.L., Troiano R.P., Ballard R.M., Carlson S.A., Fulton J.E., Galuska D.A., George S.M., Olson R.D. The physical activity guidelines for americans. J. Am. Med. Assoc. 2018;320:2020–2028. doi: 10.1001/jama.2018.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O’Brien M.W., Wojcik W.R., DÉntremont L., Fowles J.R. Validation of the PiezoRx® step count and moderate to vigorous physical activity times in free living conditions in adults: a pilot study. Int. J. Exerc. Sci. 2018;11:541–551. [PMC free article] [PubMed] [Google Scholar]
- 29.Tudor-Locke C., Craig C.L., Aoyagi Y., Bell R.C., Croteau K.A., De Bourdeaudhuij I., Ewald B., Gardner A.W., Hatano Y., Lutes L.D., Matsudo S.M., Ramirez-Marrero F.A., Rogers L.Q., Rowe D.A., Schmidt M.D., Tully M.A., Blair S.N. How many steps/day are enough? For older adults and special populations. Int. J. Behav. Nutr. Phys. Act. 2011;8:1–19. doi: 10.1186/1479-5868-8-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ghisi G.L.M., Mahajan A., Chaves G.S.S., Rouse V., Brum M., Ajwani F., Aultman C., Ricupero M., Oh P., Colella T.J.F. Validation of a self-administered version of the Mediterranean Diet Scale (MDS) for cardiac rehabilitation patients in Canada. Int. J. Food Sci. Nutr. 2019;70:202–211. doi: 10.1080/09637486.2018.1486392. [DOI] [PubMed] [Google Scholar]
- 31.Bellman C., Hambraeus K., Lindbäck J., Lindahl B. Achievement of secondary preventive goals after acute myocardial infarction. J. Cardiovasc. Nurs. 2009;24:362–368. doi: 10.1097/JCN.0b013e3181a9bf72. [DOI] [PubMed] [Google Scholar]
- 32.Tawalbeh L.I., Ahmad M.M. The effect of cardiac education on knowledge and adherence to healthy lifestyle. Clin. Nurs. Res. 2014;23:245–258. doi: 10.1177/1054773813486476. [DOI] [PubMed] [Google Scholar]
- 33.Chaves G.S.S., Lima de Melo Ghisi G., Britto R.R., Grace S.L. Maintenance of gains, morbidity, and mortality at 1 year following cardiac rehabilitation in a middle‐income country: a wait‐list control crossover trial. J. Am. Heart Assoc. 2019;8 doi: 10.1161/JAHA.118.011228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bock B.C., Carmona-Barros R.E., Esler J.L., Tilkemeier P.L. Program participation and physical activity maintenance after cardiac rehabilitation. Behav. Modif. 2003;27:37–53. doi: 10.1177/0145445502238692. [DOI] [PubMed] [Google Scholar]
- 35.Pinto B.M., Goldstein M.G., Papandonatos G.D., Farrell N., Tilkemeier P., Marcus B.H., Todaro J.F. Maintenance of exercise after phase II cardiac rehabilitation. Am. J. Prev. Med. 2011;41:274–283. doi: 10.1016/j.amepre.2011.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Twardella D., Merx H., Hahmann H., Wusten B., Rothenbacher D., Brenner H. Long term adherence to dietary recommendations after inpatient rehabilitation: prospective follow up study of patients with coronary heart disease. Heart. 2006;92:635–640. doi: 10.1136/hrt.2005.067611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mantwill S., Monestel-Umaña S., Schulz P.J. The relationship between health literacy and health disparities: a systematic review. PLoS One. 2015;10 doi: 10.1371/journal.pone.0145455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.de G.L., Ghisi M., da G.S., Chaves S., Britto R.R., Oh P. Health literacy and coronary artery disease: a systematic review. Patient Educ. Couns. 2018;101:177–184. doi: 10.1016/j.pec.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 39.Beauchamp A., Sheppard R., Wise F., Jackson A. Health literacy of patients attending cardiac rehabilitation. J. Cardiopulm. Rehabil. Prev. 2020;40:249–254. doi: 10.1097/HCR.0000000000000473. [DOI] [PubMed] [Google Scholar]
- 40.Ghisi G., Chaves G., Ribeiro A.L., Oh P., Britto R.R., Grace S.L. Comprehensive cardiac rehabilitation effectiveness in a middle-income setting: a RANDOMIZED CONTROLLED TRIAL. J. Cardiopulm. Rehab. Prev. 2020 doi: 10.1097/HCR.0000000000000512. [DOI] [PubMed] [Google Scholar]
- 41.Turk-Adawi K., Supervia M., Lopez-Jimenez F., Pesah E., Ding R., Britto R.R., Bjarnason-Wehrens B., Derman W., Abreu A., Babu A.S. Cardiac rehabilitation availability and density around the globe. EClinicalMedicine. 2019;13:31–45. doi: 10.1016/j.eclinm.2019.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jin K., Khonsari S., Gallagher R., Gallagher P., Clark A.M., Freedman B., Briffa T., Bauman A., Redfern J., Neubeck L. Telehealth interventions for the secondary prevention of coronary heart disease: a systematic review and meta-analysis. Eur. J. Cardiovasc. Nurs. 2019;18:260–271. doi: 10.1177/1474515119826510. [DOI] [PubMed] [Google Scholar]
- 43.Thomas E., Gallagher R., Grace S.L. Future-proofing cardiac rehabilitation: transitioning services to telehealth during COVID-19. Eur. J. Prev. Cardiol. 2020 doi: 10.1177/2047487320922926. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.