Highlights
-
•
Tornwald’s cyst is a rare benign disease of the nasopharynx.
-
•
The disease has a diverse clinical presentation, with the majority of cases being discovered incidentally.
-
•
Nasoendoscopy, imaging studies and pathological examination can be used to confirm the disease.
-
•
Endoscopic surgical removal is an excellent safe measure for disease management.
Abbreviations: TC, Tornwald’t cyst; CT, computerized tomography; MRI, magnetic resonance imaging
Keywords: Thornwaldt’s cyst, Nasoendoscopy, Nasopharyngeal cyst
Abstract
Background
Tornwaldt cyst (TC) is a relatively rare but benign disease. Although these lesions are asymptomatic and found incidentally during routine ENT examination, the can present with unexplained sinonasal symptoms, such as nasal obstruction, post nasal drip and occipital headache.
Aim
To study the clinical presentations and outcome of Tornwaldt nasopharyngeal cyst cases diagnosed and managed in our center.
Methods
Patients with symptomatic TC who were operated and followed up at our center were selected for this study.
Results
3 patients with a diagnosis of TC by naso-endoscopy, CT and MRI were included in this study. All patients were males, with age ranging from 54 to 86 years. A trans-nasal endoscopic surgical removal of the cyst was done for all patients with no intra or post-operative complications. All patients were free of symptoms and disease reassurance at follow up.
Conclusion
Although relatively rare, TC should be suspected in any patient complaining of unexplained sinonasal symptoms. Endoscopic surgical excision is a safe and effective maneuver with no cyst recurrence.
1. Introduction
Tornwaldt cyst (TC) is a relatively rare but benign disease. It is a developmental lesion within the midline of the nasopharynx [1]. An incidence of 1.4–3.3% was reported by some authors in the literature [2,3].
The disease usually presents between the age of 15–30 [4,5], with the majority of cysts being undiagnosed due to their small size and benign nature. If they grow, however, they can cause a verity of symptoms that might include, nasal obstruction, postnasal drip, headache, nick stiffness and Eustachian tube dysfunction [4].
This article aims to study the clinical presentations and outcome of Tornwaldt nasopharyngeal cyst cases diagnosed and managed in our center.
2. Subjects and methods
During the period from 2014 until 2019, 3 patients with symptomatic TC who were operated and followed up at our institution were included in this study. All patients were evaluated by nasoendoscopic examination, CT\MRI scans, and pathological examination prior to surgical management. All patients were followed up post operatively to assess resolution of symptoms and disease recurrence.
Ethical clearance was obtained from the Institutional Review Board (IRB) at our institution. Written consent was obtained from all patients prior to the involvement of the study.
The research work has been reported in line with the PROCESS criteria [6].
3. Results
3.1. 3 illustrative cases
3.1.1. Case1
An 86-year-old male patient, presented to our ENT clinic complaining of a 3 months history of left ear fullness. Other ear symptoms, including otalgia and otorrhea were denied by the patient.
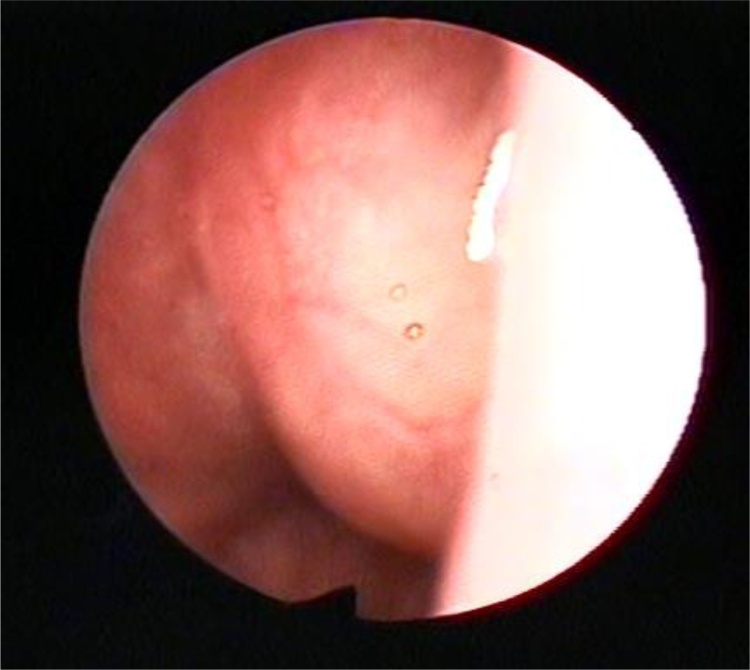
Nasoendoscopic examination revealed the presence of a well circumscribed, smooth nasopharyngeal mass (Graph 1). Autoscopic examination showed a dull tympanic membrane on left ear.
Graph 1.
Nasopharyngeal endoscopic view showing a large smooth cystic mass filling the nasopharynx.
Audiogram revealed a left ear moderate to severe mixed hearing loss.
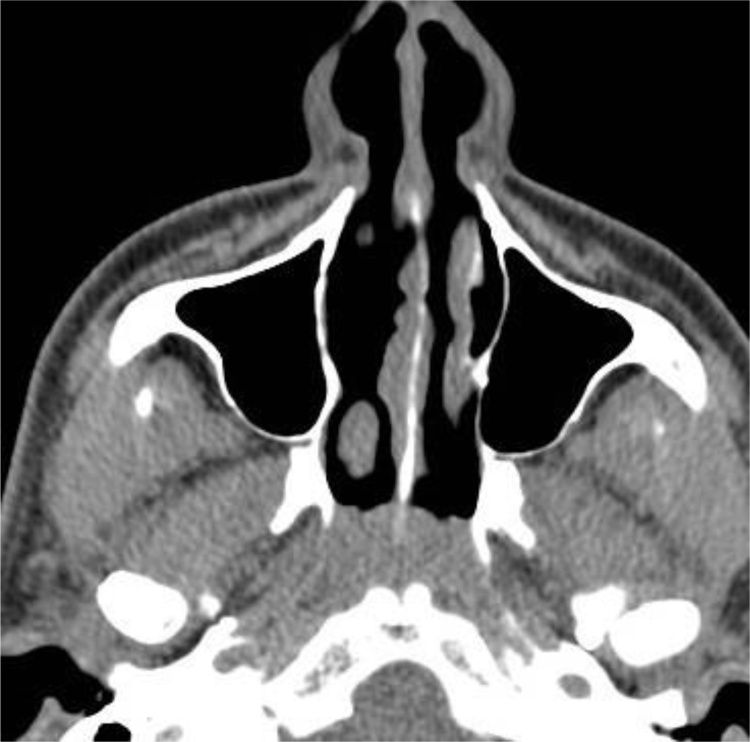
CT PNS, done outside in another facility revealed soft tissue in the nasopharynx (Graph 2).
Graph 2.
Plain axial CT scan showing the nasopharyngeal mass touching the posterior septum.
A biopsy was taken in the clinic, histopathology report showed multiple fragments with chronic inflammation and congested vessels. No evidence of malignancy.
Complete surgical excision was done endoscopically.
The patient remained symptoms free with no signs of recurrence at 2 years follow up.
3.1.2. Case2
A 54-year-old male patient, presented to our ENT clinc, a known case of chronic supporative otitis media with a surgical history of left ventilation tube insertion, complaining of left ear hearing loss.
Naso-endoscopic examination revealed the presence of a nasopharyngeal cystic lesion. Autoscopic examination showed adhesive tympanic membrane type IV.
Audiogram revealed a left ear moderate conductive hearing loss.
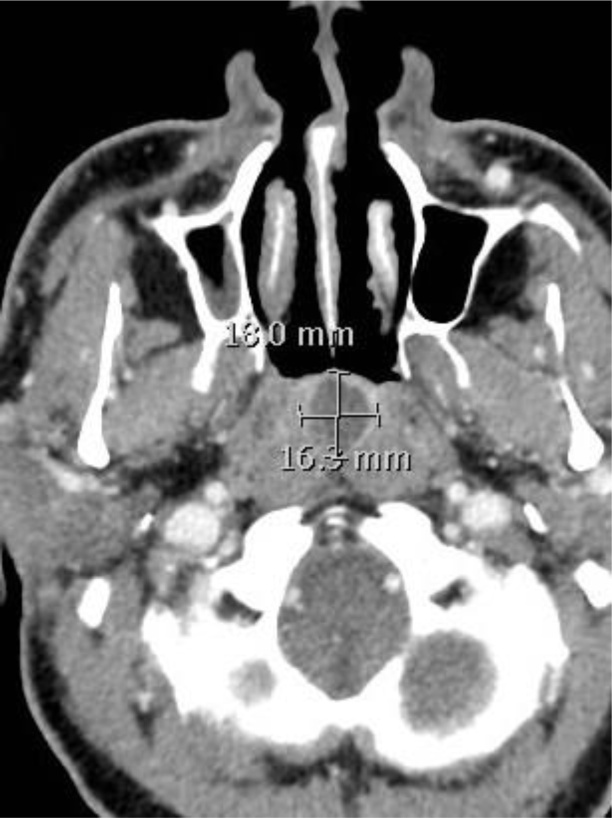
A CT scan was done, which revealed the presence of a nasopharyngeal cyst occupying the roof and posterior nasopharyngeal wall (Graph 3).
Graph 3.
Sagittal CT scan showing the nasopharyngeal cyst measuring 23.6 mm × 21.5 mm occupying the roof and posterior wall nasopharynx.
A biopsy was taken in the clinic, histopathology report showed benign lymphoid hyperplasia. No evidence of malignancy.
Complete surgical excision was done endoscopically.
On the one month-follow up, patient reported complete resolution of symptoms with no evidence of recurrence of the cyst upon examination.
3.1.3. Case3
A 55-year-old male patient, presented to our ENT clinic, complaining of long term cough with excessive throat secretions.
Nasoendoscopic examination revealed the presence of an anterior septal perforation with a cystic mass originating from the roof of the nasopharynx.
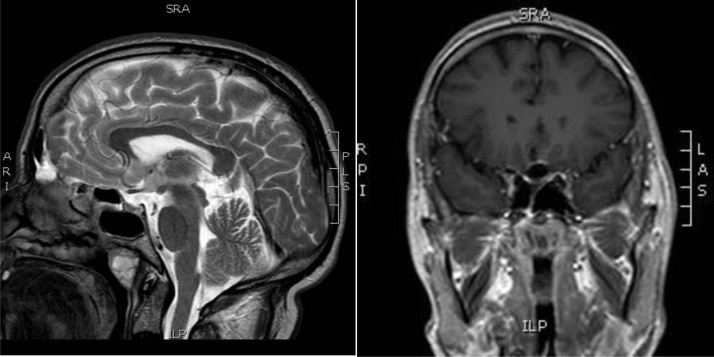
An MRI and a CT scan were done. The CT scan revealed the presence of a localized cystic nasopharyngeal mass with peripheral enhancement (Graph 4), while he MRI revealed the presence of a nasopharyngeal cyst occupying the roof and posterior nasopharyngeal wall (Graph 5).
Graph 4.
Axial ct scan with contrast showing a localized cystic nasopharyngeal mass with peripheral enhancement.
Graph 5.
Sagittal and coronal MRI scans of the nasopharynx showing the nasopharyngeal cyst measuring 23.6 mm × 21.5 mm occupying the roof and posterior wall nasopharynx.
A biopsy was taken in the clinic, histopathology report showed chronic inflammation. No evidence of malignancy.
Surgical marsupialization was done endoscopically. Patient remained symptoms free with no recurrence for 3 years.
4. Discussion
Tornwaldt cyst (TC) was first described in literature by of Dr. Gustoff L. Tornwaldt in the 19th century as one of the causes of pharyngeal discomfort [7]. This cyst develops as a result of defected embryological development at the point where the notochord retains its union with the pharyngeal ectoderm [8]. It may also be required by means of surgical trauma, in particular nasopharyngitis, chemoradiation or adenoidectomy [9,10], which has been implicated as the etiological factor in approximately 75% of cases [11].
Tornwaldt’s cyst is mainly classified based on drainage to one of two categories, crusting and cystic. The cystic type has an obstructed drainage pathway resulting in a cyst formation, while the crusting type drains spontaneously into the nasopharynx [12].
The vast majority of these cysts are asymptomatic, and may go decades undiagnosed. If these cysts get larger in size or become infected, a variety of symptoms can manifest. These include occipital headache, seizures, dizziness/vertigo, pharyngeal discomfort, estuation tube dysfunction, pharyngitis, halitosis and post nasal drip [[13], [14], [15], [16]].
Naso-endoscopic examination of the nasopharynx typically reveals a well encapsulated lesion, stationed in the posterior Midline in the superior recess of the nasopharynx [17].
Imaging studies can be used to confirm the diagnosis, if in doubt. MRI is the gold standard modality. It is the most sensitive modality for detecting the cyst, evaluating its size, content and anatomical relationship to surrounding structures [17]. The cyst has a high signal intensity on T1-weighted, T2-weighted and fluid-attenuated inversion-recovery, with no enhancement with gadolinium contrast [18]. Computerized tomography can be used as well, with the TC appearing as a well circumscribed, low density lesion [19].
As long as the cyst is asymptomatic, not intervention is required. If symptomatic, however, the cyst can be managed surgically by means of excision or marsupialization [14]. Surgical management can lead to complete resolution of symptoms in the vast majority of patients [1].
5. Conclusion
This paper delineates the diverse clinical presentation of Torwaldt’s cyst. The cyst can be easily diagnosed by means of nasoendoscopy or imaging studies, supported by histopathological examination. Long term follow up for our patients have proven the effectiveness and safety of endoscopic surgical excision with no recurrence detected up to 3 years post operatively. Although relatively rare, TC should be suspected in any patient complaining of such symptoms and be managed accordingly.
Declaration of Competing Interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Funding
There is no financial support and sponsorship.
Ethical approval
This research has been approved by the IRB committee at KFSH Dammam.
Consent
Written informed consent was obtained from all patients for publication of this case series.
Author’s contribution
ZAINAB ALSHUHAYB: conceptualization, validation, data curation, writing - original draft. Writing.
HUSSAIN ALKHAMIS, BAYAN ALSHUHAYB, MAJED ALDOSSARY, ZAHRA ALMOUMEN, AMIRAH ALDHURAIS: review and editing, visualization, funding acquisition.
Ali A AlMOMEN: Writing - review and editing, supervision, project administration.
Registration of research studies
-
1.
Name of the registry: ResearchRegistry UIN
-
2.
Unique identifying number or registration ID: researchregistry5872
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked):
Guarantor
Dr. Ali A Almomen. Senior Consultant, Rhinology and Skull Base Surgery at King Fahad Specialist Hospital, Dammam, KSA.
Data availability
The data used to support the findings of this study are included within the article. They are available from the corresponding author upon request.
Methods
This work has been reported in line with the SCARE criteria.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Moody M.W. Tornwaldt’s cyst: incidence and case report. Ear Nose Throat J. 2007;86:45–47. [PubMed] [Google Scholar]
- 2.Rodgers G.K., Chan Khl, Dahl R.E. Antral choanal polyp presenting as obstructive sleep apnea syndrome. Arch. Otolaryngol. Head Neck Surg. 1991;117:914–916. doi: 10.1001/archotol.1991.01870200108019. [DOI] [PubMed] [Google Scholar]
- 3.Salib R.J., Sadek S.A., Dutt S.N., Pearman K. Antrochoanal polyp presenting with obstructive sleep apnea and cachexia. Int. J. Pediatric Otorhnolaryngol. 2000;54:163–166. doi: 10.1016/s0165-5876(00)00353-0. [DOI] [PubMed] [Google Scholar]
- 4.Eloy P., Watelet J.B., Hartert A.S., Bertrand B. Thornwaldt’s cyst and surgery with powered instrumentation. B-ENT. 2006;2:135–139. [PubMed] [Google Scholar]
- 5.Baisakhiya N., Deshmukh P., Pawar V. Thornwaldt’s cyst: a cause of neck pain and stiffness. Indian J. Otolaryngol. Head Neck Surg. 2011;63:147–148. doi: 10.1007/s12070-011-0185-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., SCARE Group The PROCESS 2018 statement: updating consensus preferred reporting of CasE series in surgery (PROCESS) guidelines. Int. J. Surg. 2018;60:279–282. doi: 10.1016/j.ijsu.2018.10.031. [DOI] [PubMed] [Google Scholar]
- 7.Chong V.F., Fan Y.F. Radiology of the nasopharynx: pictorial essay. Australas. Radiol. 2000;44:5–13. doi: 10.1046/j.1440-1673.2000.00765.x. [DOI] [PubMed] [Google Scholar]
- 8.Miller R.H., Sneed W.F. Thornwalt’s bursa. Clin. Otolaryngol. Allied Sci. 1985;10:21–25. doi: 10.1111/j.1365-2273.1985.tb01160.x. [DOI] [PubMed] [Google Scholar]
- 9.Miyahara H., Matsunaga T. Tornwaldt’s disease. Acta Otolaryngol. 1994:29–36. doi: 10.3109/00016489409124336. [DOI] [PubMed] [Google Scholar]
- 10.Ikushima I. MRI imaging of Tornwaldt’s cysts. Am. J. Roentgenol. 1999:1663–1665. doi: 10.2214/ajr.172.6.10350312. [DOI] [PubMed] [Google Scholar]
- 11.Eagle W.W. Pharyngeal bursa (Thornwaldt’s bursae): report of 64 cases. Laryngoscope. 1939;56:199–207. [Google Scholar]
- 12.Miyahara H., Matsunaga T. Tornwaldt’s disease. Acta Otolaryngol. Suppl. 1994;517:36–39. doi: 10.3109/00016489409124336. [DOI] [PubMed] [Google Scholar]
- 13.Miyahara H., Matsunaga T. Tornwaldt’s disease. Acta Oiolaryngol. Suppl. 1994;517:36–39. doi: 10.3109/00016489409124336. [DOI] [PubMed] [Google Scholar]
- 14.Weissman J.L. Thornwaklt cysts. Am. J. Otolaryngol. 1992;13:381–385. doi: 10.1016/0196-0709(92)90080-d. [DOI] [PubMed] [Google Scholar]
- 15.Magliulo G., Fusconi M., D’Amico R., de Vincentiis M. Tornwaldt’s cyst and magnetic resonance imaging. Ann. Otol. Rhinol. Laryngol. 2001;110:895–896. doi: 10.1177/000348940111000916. [DOI] [PubMed] [Google Scholar]
- 16.Weber A.L. Computed tomography and magnetic resonance imaging of the nasopharynx. ISR J. Med. Sci. 1992;28:161–168. [PubMed] [Google Scholar]
- 17.Yanagisawa E., Yanagisawa K. Endoscopic view of Thornwaldt’s cyst of the nasopharynx. Ear Nose Throat J. 1994;73:884–885. [PubMed] [Google Scholar]
- 18.Marom T., Russo E., Salem D., Roth Y. Nasopharyngeal cysts. Int. J. Pediatr. Otorhinolaryngol. 2009;73:1063–1070. doi: 10.1016/j.ijporl.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 19.El-anwar 5 years follow up after transnasal endoscopic surgery of Thornwaldt’s cyst with powered instrumentation. Auris Nasus Larynx. 2015;42:29–33. doi: 10.1016/j.anl.2014.08.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are included within the article. They are available from the corresponding author upon request.