Abstract
Objective
We sought to understand how the coronavirus disease 2019 pandemic has affected the neurosurgical workforce.
Methods
We created a survey consisting of 22 questions to assess the respondent's operative experience, location, type of practice, subspecialty, changes in clinic and operative volumes, changes to staff, and changes to income since the pandemic began. The survey was distributed electronically to neurosurgeons throughout the United States and Puerto Rico.
Results
Of the 724 who opened the survey link, 457 completed the survey. The respondents were from throughout the United States and Puerto Rico and represented all practices types and subspecialties. Nearly all respondents reported hospital restrictions on elective surgeries. Most reported a decline in clinic and operative volume. Nearly 70% of respondents saw a decrease in the work hours of their ancillary providers, and almost one half (49.1%) of the respondents had had to downsize their practice staff, office assistants, nurses, schedulers, and other personnel. Overall, 43.6% of survey respondents had experienced a decline in income, and 27.4% expected a decline in income in the upcoming billing cycle. More senior neurosurgeons and those with a private practice, whether solo or as part of a group, were more likely to experience a decline in income as a result of the pandemic compared with their colleagues.
Conclusion
The coronavirus disease 2019 pandemic will likely have a lasting effect on the practice of medicine. Our survey results have described the early effects on the neurosurgical workforce. Nearly all neurosurgeons experienced a significant decline in clinical volume, which led to many downstream effects. Ultimately, analysis of the effects of such a pervasive pandemic will allow the neurosurgical workforce to be better prepared for similar events in the future.
Key words: COVID-19, Neurosurgery, Neurosurgery practice, Pandemic, Survey
Abbreviations and Acronyms: AANS, American Association of Neurological Surgeons; COVID-19, Coronavirus disease 2019; CSNS, Council of State Neurosurgical Societies
Introduction
As coronavirus disease 2019 (COVID-19) spread globally, the World Health Organization declared a global pandemic on March 11, 2020.1 , 2 The pandemic quickly altered all aspects of society and badly strained the healthcare system. The rapid increase in COVID-19 cases in the United States and the forecast shortfall of personal protective equipment, ventilators, and hospital beds led the American College of Surgeons to recommend the cessation of elective surgeries and triage of the remaining cases according to the level of acuity on March 13, 2020.3 , 4 The Centers for Medicare and Medicaid Services also released recommendations for a tiered framework for prioritizing surgeries and procedures.5 These recommendations were echoed in a joint statement from the American Association of Neurological Surgeons (AANS) and the Congress of Neurological Surgeons, and several templates were reported from institutions throughout the United States for triaging neurosurgery patients.6, 7, 8, 9, 10, 11, 12, 13, 14, 15 Neurosurgery practices around the United States adapted rapidly and variously, including canceling elective procedures, triaging of urgent cases, deploying telemedicine for office visits, and altering the traditional workflow of everyday practice. For many, productivity decreased, and neurosurgeons' practices and income have been affected.
To better understand how the COVID-19 pandemic has affected the neurosurgical workforce, we conducted an electronic survey of practicing neurosurgeons in various settings. Specifically, we sought to understand how the pandemic has affected neurosurgeons' case and clinic volume, compensation, changes in clinic structure, employment of support staff, and attitudes toward these changes.
Methods
Survey
An electronic survey (Supplementary Figure 1) was created (Qualtrics, Provo, Utah, USA) and distributed via e-mail to 9988 members of the AANS mailing list, including 5224 practicing neurosurgeons across the United States and Puerto Rico on April 15, 2020. A reminder e-mail with the survey link was sent 1 week later to this same group. The survey consisted of 22 questions, which were designed and vetted by us. Because of the rapid progression of the pandemic, the survey was not validated before distribution for use as a psychometric tool. The questions were designed to ascertain the respondent's operative experience, practice location, practice type, subspecialty, changes in clinic and operative volumes, changes to staff, and changes to income during the period since the pandemic began. The responses were collected anonymously via the Qualtrics interface. Although the survey link was sent twice to AANS and Council of State Neurosurgical Societies (CSNS) members, the electronic nature of the survey did not allow for duplicate entries. We received 457 responses from April 15, 2020 to May 1, 2020. Participation was strictly voluntary.
Definitions
The respondents could specify their practice as solo private practice, group private practice, hospital employed (nonacademic), academic, Veterans Affairs Medical Center, or locum tenens. Furthermore, respondents could specify their primary subspecialty as none, cerebrovascular/endovascular, spine, neurocritical care, pediatric, tumor/skull base, pain/functional, or peripheral nerve.
Statistical Analysis
Descriptive statistics were used to characterize the responses from the study cohort. Categorical variables were summarized using counts and proportions and were compared among the grouped variables such as subspecialty and geographic region (high volume vs. low volume) using the Fisher exact test. The Cochran-Armitage trend test was used to assess the relationship between the number of years in practice and the reduction in income during the COVID-19 pandemic. High-volume regions were defined as those states, districts, or territories with >10,000 cases of COVID-19. Low-volume regions were defined as those with ≤10,000 cases, as reported by the U.S. Centers for Disease Control and Prevention on May 18, 2020.16
All tests were 2-sided, and P < 0.05 was considered to indicate statistical significance. Statistical analysis was performed using SAS, version 9.4 (SAS Institute, Cary, North Carolina, USA).
Results
Demographics
The first e-mail was opened by 4088 AANS and CSNS members, with 704 opening the survey link. The second e-mail was opened by 3806 members, with 24 opening the survey link. A total of 457 responses were received from all 50 states, the District of Columbia, and Puerto Rico. The overall response rate was 8.7%. All practice types and subspecialties were represented (Figure 1 ). Of the 457 respondents, 80 were from low-volume regions, 340 were from high-volume regions, and 37 declined to give the location of their practice. Most respondents had been in practice for >20 years (45.2%), with the remainder evenly distributed in years of practice: 1–5 years, 15.8%; 6–10 years, 12.7%; 11–15 years, 13.2%; and 16–20 years, 13.2%.
Figure 1.
Graph showing the distribution of subspecialties among survey respondents. Most respondents were general or spine neurosurgeons. Two respondents did not state their primary subspecialty.
Clinical and Operative Volume
Nearly all respondents (97.1%) reported hospital restrictions on elective surgeries during the COVID-19 pandemic. Emergency neurosurgery was less affected, because only 22.5% of the respondents reported having difficulty admitting patients to the hospital, and 21.7% reported delays for emergent surgeries. Most respondents (64.1%) reported that the overall neurosurgical care of their patients had suffered as a result of the pandemic, although 25.2% reported that care was not negatively affected and 10.7% were unsure (Figure 2 ). No significant difference was found in the effects to neurosurgery care when comparing the respondents by their years in practice, type of practice, or subspecialty.
Figure 2.

Graph showing the respondent responses to the question of whether the respondents believed that the neurosurgical care of their patients had suffered significantly because of the coronavirus disease 2019 pandemic. Most respondents reported that the neurosurgical care of their patients had suffered during the pandemic.
Most respondents (93.0%) reported a decline in their clinical volume: 4.2% experienced a 1%–25% decline; 16.2%, a 26%–50% decline; 39.6%, a 51%–75% decline; and 33.0%, a 76%–99% decline. Of the 457 respondents, 24 (5.3%) had closed their practice completely during the pandemic, 6 (1.3%) had experienced no change in clinic volume, and 2 (0.4%) reported an increase in their clinic volume (Figure 3 ). Neurosurgeons in practice >20 years (8.3% vs. 2.8% for all others; P = 0.011), those in solo private practice (19.4% vs. 4.2% for all others; P = 0.003), and those with a primary subspecialty of spine (10.1% vs. 3.2% for all others; P = 0.001) were significantly more likely than their counterparts to have completely closed their outpatient clinics during the pandemic (Figure 4 ). Of those who had continued to see patients in the clinic, most had continued to do so remotely, because 93.6% had increased their use of telemedicine.
Figure 3.
Graph showing the change in clinic volumes among all respondents during the coronavirus disease 2019 pandemic. Most respondents had experienced a >50% decline in their clinic volume, and >5% of respondents had closed their clinic altogether during the pandemic.
Figure 4.
Graph showing the change in clinic volume stratified by the years in practice, type of practice, and subspecialty during the coronavirus disease 2019 pandemic. Those in practice >20 years were significantly more likely to have closed their clinic compared with the remainder of their colleagues (8.3% vs. 2.8%; P = 0.011). Those in solo private practice were significantly more likely to have closed their clinic than were those in other practice types (19.4% vs. 4.2%; P = 0.003). Those whose primary subspecialty was the spine were significantly more likely to close their clinic than were those in other subspecialties (10.1% vs. 3.2%; P = 0.001).
Similarly, most respondents (91.4%) had reported a decline in their operative volume: 5.9% had experienced a 1%–25% decline; 11.8%, a 26%–50% decline; 28.1%, a 51%–75% decline; and 45.6%, a 76%–99% decline. Of the 457 respondents, 33 (7.2%) had stopped operating completely during the pandemic, 4 (0.9%) reported no change in their operative volume, and 2 (0.4%) reported an increase in their operative volume (Figure 5 ). Several groups were more likely than their counterparts to have stopped operating completely during the pandemic period. Those in practice >15 years were more likely to have stopped operating during the pandemic than were those in practice ≤15 years (9.4% vs. 3.7%; P < 0.001). Neurosurgeons in solo private practice were more likely to have stopped operating than were their peers in other practice types (19.4% vs. 6.4%; P = 0.007). Spine surgeons were more likely to have stopped operating compared with their colleagues in other subspecialties (15.1% vs. 3.8%; P < 0.001; Figure 6 ). Furthermore, the reduction in operative volume differed significantly (P = 0.03) between regions with high volumes of COVID-19 cases compared with the regions with low volumes of cases (Table 1 ).
Figure 5.
Graph showing the change in operative volumes among all respondents during the coronavirus disease 2019 pandemic. Most respondents had experienced a >50% decline in their operative volume, and >7% of respondents had stopped performing surgery altogether during the pandemic.
Figure 6.
Graph showing the change in the operative volume stratified by the years in practice, type of practice, and subspecialty during the coronavirus disease 2019 pandemic. Those in practice >15 years were significantly more likely to have completely stopped performing surgery compared with the remainder of their colleagues (9.4% vs. 3.7%; P < 0.001). Those in solo private practice were significantly more likely to have completely stopped performing surgery than were those in other practice types (19.4% vs. 6.4%; P = 0.007). Those whose primary subspecialty was the spine were significantly more likely to have completely stopped operating than were those in other subspecialties (15.1% vs. 3.8%; P < 0.001).
Table 1.
Neurosurgeons' Responses on Changes to Admission of Patients, Quality of Care, Clinic Volume, Operative Volume, and Income Stratified by Region Case Level
| Survey Question and Possible Response | Region Volume |
Nonparametric P Value∗ | |
|---|---|---|---|
| <10,000 Cases (n = 80) | >10,000 Cases (n = 340) | ||
| Q6. Have you had problems admitting neurosurgical patients because of high census secondary to the COVID-19 epidemic? | 0.077 | ||
| Yes | 9 (11.25) | 68 (20.18) | |
| No | 71 (88.75) | 269 (79.82) | |
| Q8. Do you feel that the neurosurgical care of your patients has suffered significantly because of the COVID-19 epidemic? | 0.444 | ||
| Definitely yes | 31 (38.75) | 114 (33.53) | |
| Probably yes | 18 (22.5) | 103 (30.29) | |
| Might or might not | 11 (13.75) | 32 (9.41) | |
| Probably not | 14 (17.5) | 70 (20.59) | |
| Definitely not | 6 (7.5) | 21 (6.18) | |
| Q9. How much reduction in volume have you experienced in your outpatient clinic/hospital consults since the start of the COVID-19 epidemic? | 0.633 | ||
| My clinic/hospital volume has increased | 0 (0) | 2 (0.59) | |
| No change in volume | 0 (0) | 4 (1.18) | |
| Volume decreased by 1%–25% | 4 (5) | 11 (3.24) | |
| Volume decreased by 26%–50% | 17 (21.25) | 51 (15) | |
| Volume decreased by 51%–75% | 33 (41.25) | 137 (40.29) | |
| Volume decreased by 76%–99% | 24 (30) | 117 (34.41) | |
| I have closed my outpatient clinic completely | 2 (2.5) | 18 (5.29) | |
| Q11. How much reduction in operative volume have you experienced since the start of the COVID-19 epidemic? | 0.03† | ||
| My operative volume has increased | 0 (0) | 2 (0.59) | |
| No change in volume | 1 (1.25) | 2 (0.59) | |
| Volume decreased by 1%–25% | 5 (6.25) | 15 (4.41) | |
| Volume decreased by 26%–50% | 9 (11.25) | 38 (11.18) | |
| Volume decreased by 51%–75% | 34 (42.5) | 85 (25) | |
| Volume decreased by 76%–99% | 26 (32.5) | 172 (50.59) | |
| I have stopped operating completely | 5 (6.25) | 26 (7.65) | |
| Q21. Have you experienced fluctuation in your income secondary to the COVID-19 epidemic? | 0.162 | ||
| No, I have a salaried position and do not expect my income to change | 22 (27.85) | 100 (29.67) | |
| No, but I expect that my income will decrease once the billing cycle catches up | 16 (20.25) | 99 (29.38) | |
| Yes | 41 (51.9) | 138 (40.95) | |
COVID-19, coronavirus disease 2019; Q, question.
Calculated using the Fisher exact test.
Statistically significant.
Although, generally, fewer restrictions had been placed on outpatient surgery centers, 20.2% of the respondents had decreased their use of the outpatient surgery center, and nearly one tenth (9.4%) had continued to perform surgery at the same or greater volume. Most respondents (70.4%) had not performed surgery at outpatient surgery centers before or during the pandemic.
Trainee and Staff Education and Work Hours
Slightly more than one half of the respondents (51%) reported working with residents or fellows. Of those, 78.9% reported that the education of their residents and/or fellows had suffered as a result of the pandemic, and 17.7% reported that adequate adjustments had been made to the educational program such that their education would not suffer. Just >60% of the respondents noted a decrease in resident and fellow clinical work hours during this period.
Similarly, nearly 70% of the respondents saw a decrease in the work hours of their ancillary providers. Only 0.9% of the respondents reported increasing the work hours of their ancillary providers to compensate for the decrease in clinical hours worked by residents and fellows. Almost one half (49.1%) of the respondents had had to downsize their practice staff, office assistants, nurses, schedulers, and other personnel because of the pandemic, and 50.9% had not had to enact any changes to their staff.
Academic Pursuits
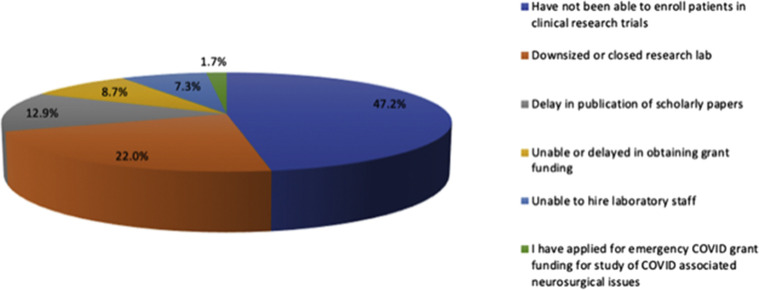
The pandemic has also had an effect on the academic pursuits of neurosurgeons. Of the respondents who participate in research, nearly one half (47%) stated that they were unable to enroll patients into clinical trials during the pandemic period. Many respondents also had had to downsize or close their research laboratories (22%) or were unable to hire laboratory staff (7.3%). Furthermore, many had experienced delays in the publication of scholarly papers (12.9%), and 8.7% were unable to obtain or had experienced delays in obtaining grant funding. A small group (1.7%) had applied for emergency grant funding to study COVID-19–associated neurosurgical issues (Figure 7 ).
Figure 7.
Pie chart showing how the coronavirus disease 2019 pandemic has affected the respondents' research efforts. These were not mutually exclusive categories (e.g., a respondent could select spending increased time conducting clinical research, watching remote didactic lectures, and spending time in the anatomy laboratory).
Exposure to COVID-19
Only 14.7% of the respondents reported that their practice had been affected because they or a partner had been exposed to, or had contracted, COVID-19, resulting in quarantine. Furthermore, only 26.8% of the respondents had been asked by their hospital to provide non-neurosurgical medical services to patients with COVID-19. Just more than 67% reported that they would be willing to provide non-neurosurgical medical care to patients with COVID-19 on a voluntary basis if needed, 10.5% stated they would not be willing to provide non-neurosurgical medical care, and another 22.4% stated they were not comfortable or qualified to provide these services. Neurosurgeons in practice <20 years were significantly more likely to be willing to provide non-neurosurgical care to COVID-19 patients than were those in practice >20 years (73.1% vs. 59.7%; P = 0.007).
Income
Overall, 43.5% of the survey responders had already experienced a decline in income, and 27.4% expected a decline in income in the upcoming billing cycle. The remainder (29.1%) reported they did not anticipate a change in their income. We found an inverse relationship between the years in practice and a change in income during the pandemic. More senior neurosurgeons reported a decline in income during this period compared with their more junior counterparts (P = 0.012). Those in private practice, whether solo or as part of a group, were more likely to have experienced a decline in income as a result of the pandemic compared with their hospital employed and academic counterparts (P < 0.001). Similarly, those surgeons who were hospital employed were more likely to have had a decline in income compared with those working in academic departments (P < 0.001). Among the neurosurgical subspecialties, 82.4% of functional neurosurgeons, 78.3% of spine surgeons, 73.4% of general neurosurgeons, 71.1% of vascular/endovascular neurosurgeons, 66.7% of neurocritical care neurosurgeons, 61.4% of tumor/skull base neurosurgeons, 48.8% of pediatric neurosurgeons, and 25% of peripheral nerve neurosurgeons had experienced or had expected to experience a decline in income. These differences across subspecialties were statistically significant (P = 0.003). Overall, no statistically significant difference was found in the income changes between the respondents practicing in high-volume versus low-volume states (P = 0.162; Table 1).
Effect on Morale
Overall, 20.4% of respondents had experienced a decreased value in their profession as a result of the pandemic, 15.1% an increased value, and 64.5% no change in the value of their profession. No differences were found in the sentiment toward their profession when comparing neurosurgeons by their years in practice, practice type, or subspecialty.
Discussion
The COVID-19 pandemic has resulted in unprecedented challenges to modern society and strains on the healthcare system. Hospitals have placed restrictions on elective surgery, clinic visits, visitors to the hospital, the use of personal protective equipment, and time spent in the hospital. Understandably, these measures have been enacted to limit the spread of COVID-19 and preserve scarce medical resources for the treatment of those infected with this often-deadly respiratory disease. However, the consequences of these measures have been far-reaching and have affected all aspects of the healthcare system.17, 18, 19, 20, 21, 22 Although some evidence has shown that COVID-19 might have some relationship to acute ischemic stroke, neurosurgeons have not otherwise been generally involved in the direct care of patients with COVID-19.23 Neurosurgical practices were much more likely to be affected by the measures in place to stop the spread of COVID-19, such as limitations on elective surgery and clinic visits, access to care, conservation of intensive care unit beds, and limitations on the hours worked by ancillary providers and residents. The revenue loss from halting elective surgery has likely had a profound effect on a neurosurgeon's income and ability to continue to run a practice and employ staff. These financial consequences could continue to hamper our profession. Our survey sought to elucidate the true effects of this pandemic on neurosurgeons, the practice of neurosurgery, and the care of our patients.
No events in recent memory have had such as pervasive effect on the daily practice of neurosurgery and medicine in general. Nearly all survey respondents (97.1%) were affected by the national and local restrictions placed on elective surgery. Emergency neurosurgery was less affected, with approximately one fifth of respondents reporting difficulties in admitting patients to the hospital and another one fifth reporting delays in getting emergent cases to the operating room. Nonetheless, nearly two thirds of the participating neurosurgeons reported that the care of their patients had suffered during this period, and these effects were similar for all neurosurgeons regardless of their seniority, type of practice, subspecialty, or practice location.
Overall, nearly three fourths of the neurosurgeons had experienced >50% decline in outpatient clinic volume, with just >5% of respondents closing their outpatient clinics during the pandemic. These changes in clinic volume were similar in all states and regions, regardless of the volume of COVID-19 cases. This decline in clinic volume created a major access problem for our patients and an ethical dilemma in deciding which patients had a condition serious enough to be considered “emergent” and require an in-person consultation or surgery. Those in solo private practices were disproportionately affected, because nearly 20% had closed their outpatient clinics in response to the pandemic, a statistically significant percentage compared with other practice types. Given that many solo practices were located in areas that were already underserved, this might serve to perpetuate the patient access problem. Although our survey had not specifically addressed the types of patients or cases that were delayed, it might be worth further study to determine which elective or semi-elective cases are universally considered “urgent” or “emergent.” For example, should surgery for a patient with newly diagnosed glioblastoma be delayed for a number of weeks because the condition is not truly emergent? The pandemic has also resulted in new approaches in how we practice neurosurgery. Nearly 94% of those who had responded to our survey reported that they had increased their use of telemedicine.
The reduction in operative volume was greater than previously reported during the early pandemic period.24 Nearly three fourths of the respondents had experienced a decline of >50% in operative volume, with 7.3% stopping surgery completely. Although the reduction in operative volume was not significantly different across neurosurgeons with different experience or type of practice, we found a statistically significant decline in operative volume in the regions with a higher number of COVID-19 cases. Furthermore, spine surgeons were more likely to stop operating completely during the pandemic period. This decrease in inpatient operative volume did not translate to a proportional increase in outpatient surgery center use, because only 9.4% of respondents had continued to perform surgery at the same or greater volume at the outpatient surgery center and more than double that proportion had decreased their use of the outpatient surgery center during the same period (20.2%).
The pandemic has not only affected neurosurgeons and their patients, but has also had a similar effect on neurosurgery trainees and ancillary providers. More than 60% of the respondents noted a decrease in resident and fellow clinical work hours, and nearly 80% expressed concern that their residents' and fellows' education had suffered as a result.25 The shortfall in work by residents was not compensated for by an increased use of ancillary providers because <1% reported an increase in their ancillary providers' work hours. Rather, 69.3% of survey responders saw a decrease in their ancillary providers work hours and almost one half had had to decrease their practice staff. These limitations in residents and ancillary providers might have resulted in a larger role for staff neurosurgeons in call coverage and inpatient hospital work, which could have further limited patient access.
Given the decline in clinic and operative volumes, it can be expected that most neurosurgeons had experienced a decline in income during the pandemic. Overall, 71% of the respondents had experienced or expected to experience a decline in income during the pandemic and the remaining 29% had not. Neurosurgeons who practiced in a private practice setting were more likely to have experienced a decline in income compared with those who were hospital employed (P < 0.001). Those who were hospital employed were more likely to experience a decline in income than were those employed in an academic setting (P < 0.001). This might have been because academic neurosurgeons often have other nonclinical components of the compensation plan that were less likely to be affected by the COVID-19 pandemic (i.e., research, teaching). The more senior neurosurgeons had experienced a greater decline in income during the pandemic. This likely had resulted because senior neurosurgeons will have well-developed elective referral bases and mature practices that are more likely to be strongly affected by any limitation in elective work. It is also possible that the more senior neurosurgeons were more vigilant about practicing social distancing measures. It is also important to consider that although the incoming revenues had significantly declined, the practice expenses (i.e., payroll, insurance, office expenses) have continued unchanged. This led 39.9% of the respondents in our study to downsize their practice in an effort to limit these expenses. This, in turn, could lead to issues for patient access in the future.
Overall, approximately two thirds of respondents (67.1%) were willing to assist in the non-neurosurgical care of COVD-19 patients if needed. Neurosurgeons who had been in practice >20 years stated they were less willing to provide non-neurosurgical medical care than their counterparts in practice for <20 years. Most neurosurgeons, however, were not asked by their hospital to assist in the non-neurosurgical care of these patients, because only 26.8% of respondents reported they had been asked by their hospital to do so.
Although our survey was useful in describing the effects of the pandemic on the average neurosurgeon, a number of limitations still exist. We acknowledge that the results of our study might only represent the opinions of a percentage of practicing neurosurgeons. Our survey was sent to 5224 practicing neurosurgeons who are members of the AANS and/or the CSNS across the United States and Puerto Rico, with 457 members completing the survey, for a response rate of 8.7%. From these respondents, we obtained the data presented in our report. We believe that although this does not constitute all opinions, our survey results represent significant exposure to the opinions of practicing neurosurgeons during the pandemic. A joint statement by the AANS, Congress of Neurological Surgeons, American Board of Neurological Surgery, and Society of Neurological Surgeons reported an estimated 3689 practicing board-certified neurosurgeons in the United States as of 2012.26 However, our survey was also sent to non–board-certified neurosurgeons; therefore, it reasonable to expect that the survey was sent to most practicing neurosurgeons in the United States and Puerto Rico. As with any survey, the opportunity for a response bias exists. Our selected population was not random, and it is quite possible that the neurosurgeons most affected by the pandemic did not respond owing to their increased responsibilities working on the front lines caring for COVID-19 patients. Additionally, because of the rapid progression of the pandemic, the survey could not be validated as a psychometric analysis tool before distribution. Therefore, the results should be interpreted more descriptively.
Conclusion
The COVID-19 pandemic will likely have lasting effects on many aspects of the practice of medicine. Our survey has provided more information on the particular vulnerabilities of different practice types and subspecialties to disasters of this nature. Nearly all neurosurgeons have seen a significant decrease in clinical volume. This was most pronounced for more senior surgeons who have well-established elective practices and more likely for those subspecializing in the spine. As expected, this decrease in volume has led to decreased income for neurosurgeons and their practices, which, in many cases, has led to restructuring of the practice itself. In the future, this could lead to reduced patient access. Little doubt exists that the lessons learned will shape our clinical practice patterns, compensation models, and preparedness for future pandemics or other disasters.
CRediT authorship contribution statement
Panayiotis E. Pelargos: Investigation, Data curation, Writing - original draft, Writing - review & editing, Visualization. Arpan R. Chakraborty: Writing - original draft, Writing - review & editing. Owoicho Adogwa: Data curation, Writing - review & editing. Karin Swartz: Writing - review & editing. Yan D. Zhao: Validation, Formal analysis, Visualization. Zachary A. Smith: Writing - original draft, Writing - review & editing. Ian F. Dunn: Writing - review & editing. Andrew M. Bauer: Conceptualization, Methodology, Investigation, Data curation, Writing - original draft, Writing - review & editing, Project administration, Supervision.
Acknowledgments
The authors would like to acknowledge the support and collaboration from the Council of State Neurosurgical Societies Workforce Committee. Without their assistance in survey distribution, this work would not have been possible and certainly would not have been as complete. Finally, the authors appreciate and acknowledge the willing participation of survey respondents nationally in this difficult time.
Footnotes
Conflict of interest statement: The present study was provided support by the Council of State Neurosurgical Societies. The statistical analysis performed by Yan D. Zhao, Ph.D., was partially supported by National Institutes of Health, National Institute of General Medical Sciences (grant 1 U54GM104938; principal investigator, Judith James).
Appendix A. Supplementary Data
The 22-question survey distributed electronically to neurosurgery attending members of the American Association of Neurological Surgery and Council of State Neurosurgical Societies.
References
- 1.Zhu N., Zhang D., Wang W., et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American College of Surgeons COVID-19: Guidance for Triage of Non-Emergent Surgical Procedures. https://www.facs.org/covid-19/clinical-guidance/triage Available at:
- 4.American College of Surgeons COVID-19: Recommendations for Management of Elective Surgical Procedures. https://www.facs.org/covid-19/clinical-guidance/elective-surgery Available at:
- 5.Centers for Medicare and Medicaid Services Non-Emergent, Elective Medical Services and Treatment Recommendations. https://www.cms.gov/files/document/cms-non-emergent-elective-medical-recommendations.pdf Available at:
- 6.Kalkanis S.N., Shaffrey C.I. COVID-19 Impacts Delivery of Neurosurgical Care—A Message from the CNS President and the AANS President. https://www.cns.org/covid-19 Available at:
- 7.Shaffrey C.I., Kalkanis S.N. COVID-19 Impacts Delivery of Neurosurgical Care — A Message from the AANS and the CNS Presidents. https://www.aans.org/en/COVID-19-Update/Presidents-Message Available at:
- 8.Burke J.F., Chan A.K., Mummaneni V., et al. Letter: the coronavirus disease 2019 global pandemic: a neurosurgical treatment algorithm. Neurosurgery. 2020;87:E50–E56. doi: 10.1093/neuros/nyaa116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lucas T. Letter: neurosurgical triage in the pandemic era. Neurosurgery. 2020;87:E69–E73. doi: 10.1093/neuros/nyaa127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arnaout O., Patel A., Carter B., Chiocca E.A. Letter: adaptation under fire: two Harvard neurosurgical services during the COVID-19 pandemic. Neurosurgery. 2020;87:E173–E177. doi: 10.1093/neuros/nyaa146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.LoPresti M.A., McDeavitt J.T., Wade K., et al. Letter: telemedicine in neurosurgery—a timely review. Neurosurgery. 2020;87:E208–E210. doi: 10.1093/neuros/nyaa175. [DOI] [PubMed] [Google Scholar]
- 12.Zacharia B.E., Eichberg D.G., Ivan M.E., et al. Letter: surgical management of brain tumor patients in the COVID-19 era. Neurosurgery. 2020;87:E197–E200. doi: 10.1093/neuros/nyaa162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ghogawala Z., Kurpad S., Falavigna A., et al. Editorial: COVID-19 and spinal surgery. https://doi.org/10.3171/2020.4.SPINE20468 [e-pub ahead of print]. J Neurosurg Spine. [DOI] [PMC free article] [PubMed]
- 14.Weiner H.L., Adelson P.D., Brockmeyer D.L., et al. Editorial: pediatric neurosurgery along with Children's Hospitals' innovations are rapid and uniform in response to the COVID-19 pandemic. https://doi.org/10.3171/2020.4.PEDS20240 [e-pub ahead of print]. J Neurosurg Pediatr. [DOI] [PMC free article] [PubMed]
- 15.Wellons J.C., Grant G., Krieger M.D., et al. Editorial: early lessons in the management of COVID-19 for the pediatric neurosurgical community from the leadership of the American Society of Pediatric Neurosurgeons. https://doi.org/10.3171/2020.3.PEDS20215 [e-pub ahead of print]. J Neurosurg Pediatr. [DOI] [PMC free article] [PubMed]
- 16.Centers for Disease Control and Prevention Coronavirus Disease 2019 (COVID-19): Cases in the U.S. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html?fbclid=IwAR2YGdSiJ1zk6mktakCLsCqjU-tEq9XsvLMK2fGG0vmHPIsAdMgl8C13cOU Available at:
- 17.COVIDSurg Collaborative Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. https://doi.org/10.1002/bjs.11746 [e-pub ahead of print]. Br J Surg. [DOI] [PMC free article] [PubMed]
- 18.Hemingway J.F., Singh N., Starnes B.W. Emerging practice patterns in vascular surgery during the COVID-19 pandemic. J Vasc Surg. 2020;72:396–402. doi: 10.1016/j.jvs.2020.04.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pesce A., Palmieri M., Armocida D., Frati A., Santoro A. Letter: neurosurgery and coronavirus (COVID-19) epidemic: doing our part. Neurosurgery. 2020;87:E48–E49. doi: 10.1093/neuros/nyaa115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salenger R., Etchill E.W., Ad N., et al. The surge after the surge: cardiac surgery post-COVID-19. https://doi.org/10.1016/j.athoracsur.2020.04.018 [e-pub ahead of print]. Ann Thorac Surg. [DOI] [PMC free article] [PubMed]
- 21.Tomlinson S.B., Hendricks B.K., Cohen-Gadol A.A. Editorial: innovations in neurosurgical education during the COVID-19 pandemic: is it time to reexamine our neurosurgical training models. https://doi.org/10.3171/2020.4.JNS201012 [e-pub ahead of print]. J Neurosurg. [DOI] [PMC free article] [PubMed]
- 22.Zoia C., Bongetta D., Veiceschi P., et al. Neurosurgery during the COVID-19 pandemic: update from Lombardy, northern Italy. Acta Neurochir. 2020;162:1221–1222. doi: 10.1007/s00701-020-04305-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sweid A., Hammoud B., Weinberg J.H., et al. Letter: thrombotic neurovascular disease in COVID-19 patients. https://doi.org/10.1093/neuros/nyaa254 [e-pub ahead of print]. Neurosurgery. [DOI] [PMC free article] [PubMed]
- 24.Jean W.C., Ironside N.T., Sack K.D., Felbaum D.R., Syed H.R. The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir. 2020;162:1229–1240. doi: 10.1007/s00701-020-04342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pelargos P.E., Chakraborty A., Zhao Y.D., Smith Z.A., Dunn I.F., Bauer A.M. An evaluation of neurosurgical resident education and sentiment during the COVID-19 pandemic: a North American Survey. World Neurosurg. 2020;140:e381–e386. doi: 10.1016/j.wneu.2020.05.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Statement of the American Association of Neurological Surgeons, American Board of Neurological Surgery, Congress of Neurological Surgeons, and Society of Neurological Surgeons Before the Institute of Medicine on the Subject of Ensuring an Adequate Neurosurgical Workforce for the 21st Century. https://www.aans.org/pdf/Legislative/Neurosurgery%20IOM%20GME%20Paper%2012%2019%2012.pdf Available at:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The 22-question survey distributed electronically to neurosurgery attending members of the American Association of Neurological Surgery and Council of State Neurosurgical Societies.