Highlights
-
•
MS patients were more anxious, depressed and stressed during the COVID-19 pandemic than their caregivers and the general population.
-
•
Younger patients, those with high EDSS scores and those who believed that MS patients are at high risk for COVID-19 infection were more anxious.
-
•
The patients’ knowledge about the factors that may affect the risk for COVID-19 infection was poor.
-
•
Though they were more anxious, they were not more committed – in contrast to what would be expected - to follow the basic preventive measures for staying safe during the pandemic than the general population.
Abstract
Background
The novel coronavirus of 2019 (COVID-19), a pandemic of the kind not seen for a century, has caused global apprehension and distress.
Objectives
to evaluate whether the psychological state and behaviours of multiple sclerosis (MS) patients and their caregivers were different from the non-MS population or not during the pandemic.
Methods
A cross-sectional survey was conducted on 115 MS patients, 33 MS caregivers and 129 healthy controls. Depression anxiety stress score-21 (DASS-21) was used for evaluation of their psychological state.
Results
MS patients had significantly higher DASS-21 scores (51.48±29.62) than their caregivers (29.79±27.19) and non-MS population (32.91±23.39) (p = 0.005). Younger patients (r=-0.252, p<0.0001), those with high EDSS scores (r = 0.023, p = 0.013) and those who believed that MS patients are at high risk for COVID-19 infection (p = 0.009) had the highest anxiety scores. There was no difference between the three groups in the level of commitment to staying at home (p = 0.747), wearing facemask (p = 0.164), wearing gloves (0.225), avoiding crowd (p = 0.225) and frequent hand washing (p = 0.570). Anxious patients had more relapses (p = 0.002) and pseudorelapses (p = 0.008).
Conclusion
In this cohort, MS patients were more anxious, stressed and depressed during the COVID-19 pandemic than their caregivers and the non-MS population, but they were not more motivated to follow the basic preventive measures against infection.
1. Introduction
Coronavirus pandemic (COVID-19) has affected more than two 2.3 million individuals worldwide, and resulted in more than 150,000 deaths in 210 countries in less than four months (World Health Organization 2020). The rates of new confirmed cases and new deaths are exponentially increasing (European, 2020). As a result, the pandemic resulted in considerable anxiety and depression among people worldwide (Cao et al., 2020; Nemati et al., 2020; Qiu et al., 2020; Wang et al., 2020). Though several studies have been conducted to evaluate the psychological state of the general population and medical staff during the pandemic (Cao et al., 2020; Nemati et al., 2020; Qiu et al., 2020; Wang et al., 2020), the data is limited about risk of COVID-19 infection and increased risk of psychological dysfunction. Among the population at risk for COVID-19 infection as published by the Centers for Disease Control and Prevention (CDC) are patients with chronic diseases causing immune suppression and those taking immunosuppressants (CDC. Coronavirus Disease 2019). To date, there is no evidence that MS disease intrinsically increases the risk for viral infections including COVID-19 (Grigoriadis and van Pesch, 2015; Brownlee et al., 2020; Reder and Cipriana, 2020). Patients with MS do not seem to be at an increased risk for COVID-19 infection unless they are on disease-modifying therapies (DMTs) causing significant immune suppression (Brownlee et al., 2020; Reder and Cipriana, 2020; England, 2020; Giovannoni et al., 2020). Older MS patients and those with higher EDSS might be at a higher risk for COVID-19 infection and complications (Brownlee et al., 2020; Reder and Cipriana, 2020). In Egypt, the main sources of information about the COVID-19 infection transmission and protective measures were the news and the reports of the ministry of health. Prior to this study, the patients’ were not provided with any educational programs at the MS unit.
The aim of this research was to assess the psychological state of MS patients and their caregivers during the pandemic of COVID-19, to evaluate their perception about the risk of infection, and to assess their behaviors related to following the basic preventive measures against infection spread.
2. Patients and methods
This cross-sectional study was conducted on a cohort of registered MS patients at the MS unit in Alexandria University Hospital in Egypt and their caregivers and on non-MS/non-caregivers as a control group during the period from the 23rd of March 2020 to the 4th of April 2020. The control group had no relationship to the patients with MS, and had no immune-mediated diseases. This MS unit in Alexandria University Hospital serves four cities in Egypt with urban and rural populations. The study was conducted via an online survey that was distributed to MS patients and their caregivers through their registered e-mails or WhatsApp numbers in the medical records. Demographic (age, sex and level of education) and clinical data (phenotype of MS, duration of MS, number of relapses during the past year, EDSS and DMTs) were collected from the patients’ medical records.
The online survey was divided into five sections. The first section included demographic data and questions about exposure to COVID-19 cases. The second section included the 21 questions of a validated Arabic version of the depression anxiety stress scale 21 version (DASS-21) (Randall et al., 2017; Arabic DASS 21 2020). The scale comprised questions about symptoms of depression, anxiety and stress. Each question was to be rated on a scale from zero to three i.e. zero denotes never, 1 denotes sometimes, 2 denotes often, and 3 denotes almost always. The scores were manually calculated and ranked according to the DASS-21 scoring and interpretation manual (DASS 21 2020). Each of the three conditions (i.e. depression, anxiety and stress) was given a score that was ranked as normal, mild, moderate, severe or extremely severe (DASS 21 2020).
The third section included questions about the individuals’ behaviors towards the basic preventive measures for prevention of COVID-19 infection spread. They were asked about the extent of their commitment (on a Likert scale) to the basic preventive measures i.e. staying home, wearing a face mask on getting out, wearing gloves on getting out, avoiding crowd and keeping a social distance of at least one meter, and frequent handwashing.
The fourth section included questions related to their knowledge about the factors that may affect the risk for COVID-19 infection. Factors that increase the patients’ risk for viral infections including COVID-19 include old age, high EDSS, taking immunosuppressants, low vitamin D levels, smoking, stress, inadequate sleep, and sedentary life (Brownlee et al., 2020; Reder and Cipriana, 2020; England, 2020; Giovannoni et al., 2020; Vardavas and Nikitara, 2020; Cohen, 2020). Both correct and incorrect factors were included in the survey. The questions were ‘In your opinion, to what extent each of the following factors influence the risk for COVID-19 infection?’. The factors asked were the age of an individual, smoking, psychological state, sleep quality, foods/drinks, and taking vitamins/supplements. Each question was to be answered on a Likert scale from zero to 2, with zero denoting not at all and 2 denoting very much.
The fifth section of the survey was specified for the MS patients only. The section included additional questions about knowledge and behaviors related to the disease. They were asked if they think MS patients were at higher risk for COVID-19 infection, and to what extent they thought certain MS-related factors (e.g. MS phenotype, the degree of patients’ disability and DMT type) influence the risk for COVID-19 infection. Concerning their behaviors, they were asked if they stopped or reduced the dose of their DMTs because of the COVID-19, and if they have taken specific supplements or vitamins since the pandemic (and to detail them). Lastly, they were asked if they had pseudo-relapses (defined as exacerbation of symptoms lasting for less than 24 h) or true relapses (lasting for more than 24 h) since the beginning of pandemic, and if they have taken corticosteroids for their relapses.
2.1. Pilot study and sample size calculation
The survey questionnaire was piloted with 15 MS patients, 15 caregivers and 15 healthy controls initially, and the sample size was calculated by using G*power software version 3.1.9.4 at a level of significance of 5% and effect size of 0.67. A sample size of at least 25 individuals per group was accordingly decided, and the online survey was distributed to 200 MS patients, their caregivers, and 300 healthy controls.
2.2. Statistical analysis
All data were analyzed using IBM Statistical Package for the Social Sciences (SPSS) software version 22.0. Quantitative data were expressed as mean, median, standard deviation, minimum and maximum. Qualitative data were expressed as frequency and percentage. A comparative analysis was conducted to compare the demographics, knowledge, DASS-21 scores and behaviors among the three studied groups (MS patients, MS caregivers and healthy controls). Factors affecting the anxiety and the impact of anxiety on patients’ behaviors were studied. The specific tests used for each analysis were depicted in their specific tables.
2.3. Ethical considerations
Ethical approval was obtained from the Ethics Committee of the Alexandria Faculty of Medicine, which has a Federal wide Assurance (FWA) from 2010 and operates according to the International Conference on Harmonization Good Clinical Practice (ICH GCP) guidelines and applicable local and institutional regulations and guidelines (No 00,018,699) (ICH GCP 2011).
3. Results
Of 200 MS patients and 300 controls invited to participate in the study, 115 patients, 33 MS caregivers and 129 controls accepted to participate. Of the 277 participants, none had COVID-19 infection, a single healthy control was exposed to a definite case (0.4%), and 34 (12.3%) reported that they were exposed to probable cases.
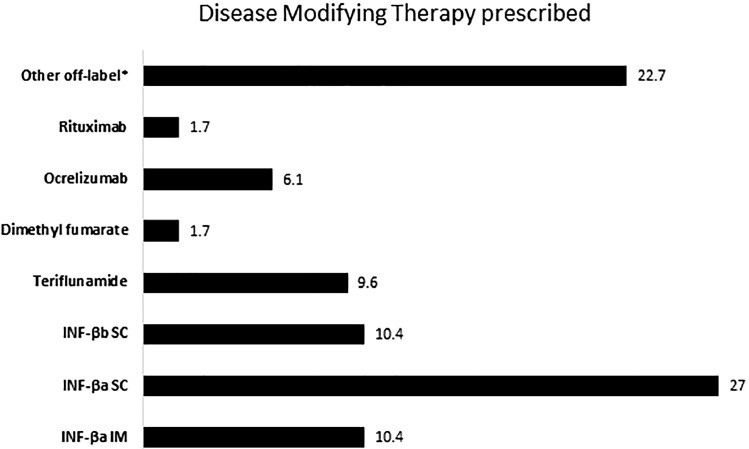
Of the 115 MS patients, 83.5% (n = 96) had relapsing remitting MS (RRMS), 13.9% (n = 16) had secondary progressive MS (SPMS) and 2.6% (n = 3) had primary progressive MS (PPMS) fulfilling the 2017 revised McDonald's criteria (McNicholas et al., 2018). The mean duration since disease onset was 6.8 ± 5.5 (0.5–24) years, and the mean EDSS score was 2.25±2.11 (0–8). Seventy-four percent (n = 54) of the patients were on interferons, whereas 21.7% (n = 25) were on DMTs causing lymphopenia (Fig. 1 ). The mean relapse rate was 1.7 ± 3.8 (0–6) during the past year. Meanwhile, 27% (n = 31) of patients reported they had a relapse since the beginning of the COVID-19 pandemic – which was announced in Egypt on the 15th of February i.e. about one month before filling the survey-, and an additional 51.3% (n = 59) reported transient exacerbations of their symptoms that lasted for less than 24 h. Of those, 20% (n = 23) did not seek medical advice and the mean number of healthcare visits was 0.5 ± 1.1 (0–7) visits.
Fig. 1.
Percentage of DMTs prescribed to MS patients recruited (*Off-label drugs included azathioprine, methotrexate and cyclophosphamide).
Table 1 details the demographic data and DASS-21 scores among the studied groups. Of note, the total DASS-21 scores were significantly higher among MS patients (51.48±29.62) than their caregivers (29.79±27.19) and the controls (32.91±23.39) (p = 0.005). Individual depression, anxiety and stress scores were also significantly higher among MS patients (17.76±11.39, 12.75±10.03 and 20.97±11.69, respectively) than their caregivers (12.24±10.94, 6.30±9.08 and 12.55±10.47, respectively) and controls (12.89±6.32, 9.33±6.71 and 10.69±8.45, respectively). Anxiety scores were the highest among MS patients, and at least one fifth of them had extremely severe grades of anxiety (28.7%), depression (22.6%), and stress (19.1%).
Table 1.
Demographics and DASS-21 during the COVID-19 pandemic among the three studied groups (n = 277).
| %(n) | MS patients (n = 115) | MS caregivers (n = 33) | Controls (n = 129) | Test of significance p-value |
| Demographics | ||||
| Age (in years) | Kruskal Wallis | |||
| Mean±SD | 34.42±8.47 | 35.15±10.83 | 31.74±8.76 | X2=10.685 P = 0.005* |
| Median | 34.0 | 34.0 | 29.0 | |
| Min.-Max. | 21–57 | 19–62 | 19–60 | |
| Gender | Chi Square | |||
| Female | 77.4(89) | 72.7(24) | 72.1(93) | X2=0.948 P = 0.622 |
| male | 22.6(26) | 27.3(9) | 27.9(36) | |
| Educational level | Chi Square | |||
| School | 19.1(22) | 12.1(4) | 3.2(4) | X2=37.274 P=<0.001* |
| Faculty/institute | 70.4(81) | 72.7(24) | 57.9(73) | |
| Postgraduate | 10.4(12) | 15.2(5) | 38.9(49) | |
| To great extent | 95.7(110) | 90.9(30) | 94.5(121) | |
| DASS-21 scores | ||||
| Total score | Kruskal Wallis | |||
| Mean±SD | 51.48±29.62 | 29.79±27.19 | 32.91±23.39 | X2=10.685 P = 0.005* |
| Median | 46.0 | 20.0 | 30.0 | |
| Min.-Max. | 0–114 | 0–92 | 0–94 | |
| Depression grade | Chi Square | |||
| Normal | 28.7(33) | 54.4(18) | 46.9(60) | X2=26.287 P = 0.001* |
| Mild | 13.9(16) | 12.1(4) | 5.5(7) | |
| Moderate | 18.3(21) | 12.1(4) | 26.6(34) | |
| Severe | 16.5(19) | 0.0(0) | 8.6(11) | |
| Extremely severe | 22.6(26) | 21.2(7) | 12.5(16) | |
| Mean±SD | 17.76±11.39 | 12.24±10.94 | 12.89 | Kruskal Wallis X2=14.083 P = 0.001* |
| Median | 18.0 | 8.0 | 10.0 | |
| Min.-Max. | 0–42 | 0–36 | 0–38 | |
| Anxiety grade | Chi Square test | |||
| Normal | 38.3(44) | 66.7(22) | 40.6(52) | X2=30.126 P=<0.001* |
| Mild | 5.2(6) | 6.1(29) | 9.4(12) | |
| Moderate | 19.1(22) | 15.2(5) | 32.8(42) | |
| Severe | 8.7(10) | 0.0(0) | 8.6(11) | |
| Extremely severe | 28.7(33) | 12.0(4) | 8.6(11) | |
| Mean±SD | 12.75±10.03 | 6.30±8.08 | 9.33±6.71 | Kruskal Wallis X2=16.710 P=<0.001* |
| Median | 10.0 | 2.0 | 9.0 | |
| Min.-Max. | 0–40 | 0–28 | 0–34 | |
| Stress grade | Chi Square test | |||
| Normal | 20.0(23) | 56.3(18) | 56.5(73) | X2=58.058 P=<0.001* |
| Mild | 29.6(34) | 25.0(8) | 24.1(31) | |
| Moderate | 16.5(19) | 6.2(2) | 15.6(20) | |
| Severe | 14.8(17) | 6.2(2) | 3.8(5) | |
| Extremely severe | 19.1(22) | 6.3(3) | 0.0(0) | |
| Mean±SD | 20.97±11.69 | 12.55±10.47 | 10.69±8.45 | Kruskal Wallis X2=49.799 P=<0.001* |
| Median | 20.0 | 8.0 | 10.0 | |
| Min.-Max. | 0–42 | 0–38 | 0–32 | |
DASS: Depression, anxiety stress score; SD: standard deviation; Min: minimum; Max: maximum; MS: multiple sclerosis.
Significant at (P ≤ 0.05)
The degree to which the individuals were motivated to follow the basic preventive measures were not statistically significant among the three studied groups (Table 2 ), and the anxiety scores did not affect the degree of their commitment to the preventive measures (Table 3 ). Frequent hand washing was the most frequently followed protective measure among MS patients (95.7%), their caregivers (90.9%) and controls (94.5%) (p = 0.570), whereas wearing gloves was the least adopted (followed by 25.2%, 30.3% and 17.2% of the three groups, respectively (p = 0.369)).
Table 2.
Behaviours among the three studied groups during COVID-19 pandemic (n = 277).
| %(n) | MS patients (n = 115) | MS caregivers (n = 33) | Controls (n = 129) | Test of significance p-value |
| Behaviours (Following basic preventive measures against COVID-19 infection) | ||||
| Staying at home | Monte Carlo test | |||
| Not at all | 2.6(3) | 0.0(0) | 2.3(3) | X2MC=2.022 P = 0.747 |
| To little extent | 24.3(28) | 21.2(7) | 18.8(24) | |
| To great extent | 73.0(84) | 78.8(26) | 78.9(101) | |
| Wearing face mask on getting out | Chi Square test | |||
| Not at all | 36.5(42) | 42.4(14) | 40.6(52) | X2=6.519 P = 0.164 |
| To little extent | 31.3(36) | 12.1(4) | 31.3(40) | |
| To great extent | 32.2(37) | 45.5(15) | 28.1(37) | |
| Wearing gloves on getting out | Chi Square test | |||
| Not at all | 49.6(57) | 42.4(14) | 57.0(73) | X2=4.280 P = 0.369 |
| To little extent | 25.2(29) | 27.3(9) | 25.8(33) | |
| To great extent | 25.2(29) | 30.3(10) | 17.2(22) | |
| Avoiding crowd/keeping a social distance of at least one meter | Chi Square test | |||
| Not at all | 6.1(7) | 6.1(2) | 1.6(2) | X2=5.674 P = 0.225 |
| To little extent | 32.2(37) | 21.2(7) | 27.3(35) | |
| To great extent | 61.7(71) | 72.7(24) | 71.1(91) | |
| Frequent hand washing | Chi Square test | |||
| To little extent | 4.3(5) | 9.1(3) | 5.5(7) | X2=1.123 P = 0.570 |
| To great extent | 95.7(110) | 90.9(30) | 94.5(121) | |
| Median | 20.0 | 8.0 | 10.0 | |
| Min.-Max. | 0–42 | 0–38 | 0–32 | |
Table 3.
Anxiety scores relation to the MS patients’ behaviours, relapses, pseudo-relapses and corticosteroids intake for relapses.
| Anxiety score | Test of significance p-value | |||
| Mean±Standard deviation | Median | Minimum-maximum | ||
| Basic Preventive Measures Against COVID-19 Infection | ||||
|---|---|---|---|---|
| Staying at home | Mann Whitney | |||
| Yes (n = 112) | 12.9 ± 10.1 | 10.0 | 0–40 | z = 0.493 P = 0.622 |
| No (n = 3) | 8.7 ± 5.8 | 12.0 | 2–12 | |
| Wearing mask | Mann Whitney | |||
| Yes (n = 73) | 10.9 ± 10.7 | 10.0 | 0–40 | z = 0.647 P = 0.518 |
| No (n = 42) | 11.5 ± 8.6 | 10.0 | 0–30 | |
| Wearing gloves | Mann Whitney | |||
| Yes (n = 58) | 13.1 ± 10.6 | 10.0 | 0–40 | z = 0.149 P = 0.882 |
| No (n = 57) | 12.4 ± 9.4 | 10.0 | 0–32 | |
| Avoiding crowded places | Mann Whitney | |||
| Yes (n = 108) | 10.6 ± 10.1 | 10.0 | 0–40 | z = 0.997 P = 0.319 |
| No (n = 7) | 15.4 ± 8.8 | 12.0 | 2–30 | |
| Frequent hand washing | – | |||
| Yes (n = 115) | 12.8 ± 10.0 | 10.0 | 0–40 | |
| Behaviours related to the MS | ||||
|---|---|---|---|---|
| Stoppage or decrease DMT dosage | Kruskal Wallis | |||
| Yes (n = 5) | 21.2 ± 13.6 | 26.0 | 0–34 | X2=0.493 P = 0.622 |
| No (n = 18) | 13.8 ± 11.9 | 12.0 | 0–40 | |
| Decrease dose (n = 10) | 13.4 ± 10.3 | 13.0 | 2–28 | |
| Vitamins intake | Mann Whitney | |||
| Yes (n = 30) | 14.2 ± 11.6 | 14.0 | 0–40 | z = 0.647 P = 0.518 |
| No (n = 3) | 29.6 ± 12.8 | 26.0 | 6–30 | |
| Pseudo-relapses, relapses and corticosteroid intake | ||||
|---|---|---|---|---|
| Pseudo-relapse | Mann Whitney | |||
| Yes (n = 23) | 15.12±10.1 | 15.0 | 0–40 | z = 2.671 P = 0.008* |
| No (n = 10) | 10.25±9.5 | 9.0 | 0–30 | |
| Relapse | Mann Whitney | |||
| Yes (n = 17) | 18.32±8.6 | 18.0 | 0–40 | z = 3.128 P = 0.002* |
| No (n = 16) | 10.69±11.5 | 10.0 | 0–34 | |
| Received corticosteroids for relapses | Mann Whitney | |||
| Yes (n = 16) | 15.4 ± 12.7 | 14.0 | 0–40 | z = 0.997 P = 0.319 |
| No (n = 17) | 14.2 ± 10.9 | 16.0 | 0–34 | |
All MS patients frequently wash their hands,.
Significant at (P ≤ 0.05).
Since the beginning of COVID-19 pandemic, 12.2% of the patients stopped taking their DMTs and an additional 14.8% reduced their doses. However, neither the type of DMT used (p = 0.585), the patients’ belief about the influence of DMT on COVID-19 risk (p = 0.07), nor the anxiety score (0.622) were related to the DMT stoppage or dose reduction. Another noted behavior among MS patient was that 58.3% started to take new vitamins/supplements since the beginning of pandemic. Vitamin D (27%) and omega 3 (23.5%) were the most common supplements taken. Vitamin A, B, C and E were taken by 3.5%, 18.3%, 21.7%, and 5.2%, respectively.
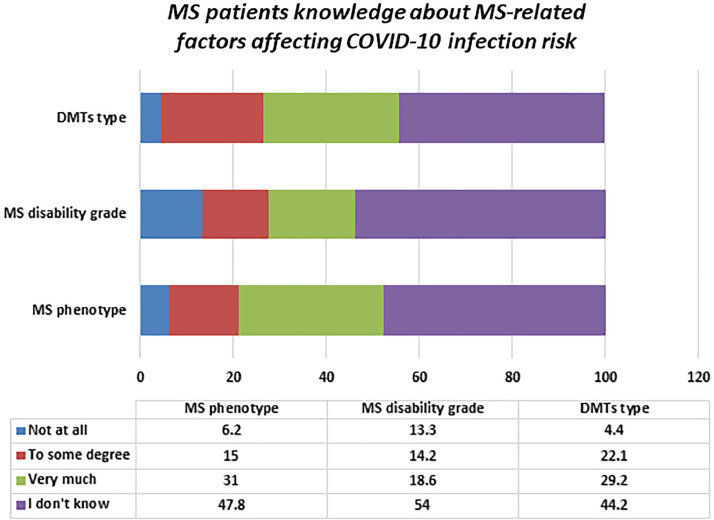
Knowledge about the factors that may influence the risk for COVID-19 infection was significantly variable among the studied groups (Table 4 ). Age, psychological state and vitamins intake were the most common reported factors to influence the risk for COVID-19 infection. Patients were less likely to report that smoking (0.007) and exercise (0.008) influence the risk for COVID-19 infection. MS caregivers were more likely to believe that foods/drinks have a great influence on the risk of COVID-19 infection than patients and controls (p = 0.01). About two-thirds of the patients (63.5%) believed that vitamins have a major role in COVID-19 risk determination, especially vitamins B (p = 0.003) and D (p<0.001). The percentage of MS patients who reported that they do not know whether the factors asked might influence the risk of COVID-19 infection or not were significantly higher than this of their caregivers and controls concerning several variables e.g. smoking (p = 0.007), exercise (p = 0.008), foods/drinks (p = 0.01) and vitamins (p = 0.005). Similarly, around half of the MS patients stated they did not know whether that MS-related factors i.e. MS phenotype (47.8%), MS disability grade (54%) and DMT type (44.2%) have an influence on COVID-19 risk determination or not (Fig. 2 ). More than one third of the MS patients (39%, n = 45) thought that MS patients were at higher risk for COVID-19, 2.6% (n = 3) thought that they are not, 23.5% (n = 27) stated that they did not know and only 33% (n = 38) knew that the risk depends on certain factors.
Table 4.
Knowledge about factors that may influence the risk for COVID-19 infection among the three studied groups (n = 277).
| %(n) | MS patients (n = 115) | MS caregivers (n = 33) | Controls (n = 129) | Test of significance p-value |
| Knowledge about factors that may influence the risk for COVID-19 | Chi Square test | |||
| Age of the individual | X2=3.236 P = 0.779 | |||
| Not at all | 5.2(6) | 3.0(1) | 4.7(6) | |
| To little extent | 18.3(21) | 27.3(9) | 18.6(24) | |
| To great extent | 71.3(82) | 69.7(23) | 72.9(94) | |
| Don't know | 5.2(6) | 0.0(0) | 3.9(5) | |
| Smoking | X2=17.734 P = 0.007* | |||
| Not at all | 3.5(4) | 0.0(0) | 1.6(2) | |
| To little extent | 19.1(22) | 12.1(4) | 12.4(16) | |
| To great extent | 50.4(58) | 72.7(24) | 74.4(96) | |
| Don't know | 27.0(31) | 15.2(5) | 11.6(15) | |
| Psychological state | X2=11.186 P = 0.083 | |||
| Not at all | 4.3(5) | 15.2(5) | 7.0(9) | |
| To little extent | 27.0(31) | 36.4(12) | 37.2(48) | |
| To great extent | 56.5(65) | 45.5(15) | 49.6(64) | |
| Don't know | 12.2(14) | 3.0(1) | 6.2(8) | |
| Adequate sleep | X2=10.176 P = 0.115 | |||
| Not at all | 11.3(13) | 15.2(5) | 9.3(12) | |
| To little extent | 30.4(35) | 39.4(13) | 45.7(59) | |
| To great extent | 36.5(42) | 30.3(10) | 34.9(45) | |
| Don't know | 21.7(25) | 15.2(5) | 10.1(13) | |
| Physical exercise | X2=17.270 P = 0.008* | |||
| Not at all | 18.3(21) | 18.2(6) | 9.3(12) | |
| To little extent | 33.9(39) | 45.5(15) | 41.9(54) | |
| To great extent | 18.3(21) | 18.2(6) | 33.3(43) | |
| Don't know | 29.6(34) | 18.2(6) | 15.5(20) | |
| Certain foods/drinks | X2=16.752 P = 0.010* | |||
| Not at all | 12.2(14) | 12.1(4) | 18.6(24) | |
| To little extent | 31.3(36) | 33.3(11) | 46.5(60) | |
| To great extent | 27.0(31) | 36.4(12) | 22.5(29) | |
| Don't know | 29.6(34) | 18.2(6) | 12.4(16) | |
| Taking vitamins | X2=18.550 P = 0.005* | |||
| Not at all | 0.9(1) | 9.1(3) | 6.2(8) | |
| To little extent | 23.5(27) | 27.3(9) | 40.3(52) | |
| To great extent | 63.5(73) | 51.5(17) | 48.8(63) | |
| Don't know | 12.2(14) | 12.1(4) | 4.7(6) | |
| Vitamin A | 10.4(12) | 6.1(2) | 4.7(6) | X2=3.055 P = 0.217 |
| Vitamin B | 13.9(16) | 18.2(6) | 3.1(4) | X2=11.634 P = 0.003* |
| Vitamin C | 64.3(74) | 60.6(20) | 65.6(128) | X2=0.290 P = 0.865 |
| Vitamin D | 33.9(39) | 24.2(8) | 10.9(14) | X2=18.673 P=<0.001* |
| Vitamin E | 7.0(8) | 6.1(2) | 2.3(3) | X2=3.024 P = 0.220 |
Significant at (P ≤ 0.05).
Fig. 2.
MS patients’ knowledge about MS-related factors affecting COVID-19 infection risk i.e. DMT type, MS disability grade and MS phenotype.
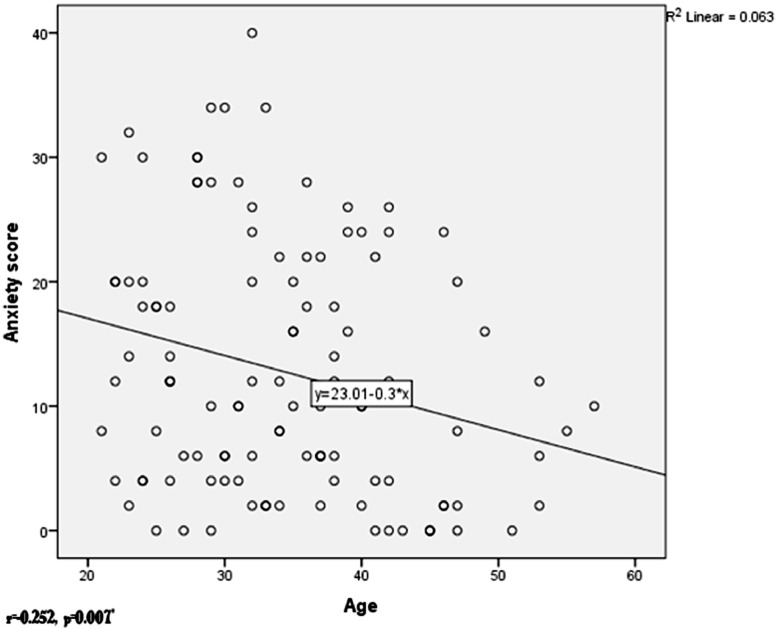
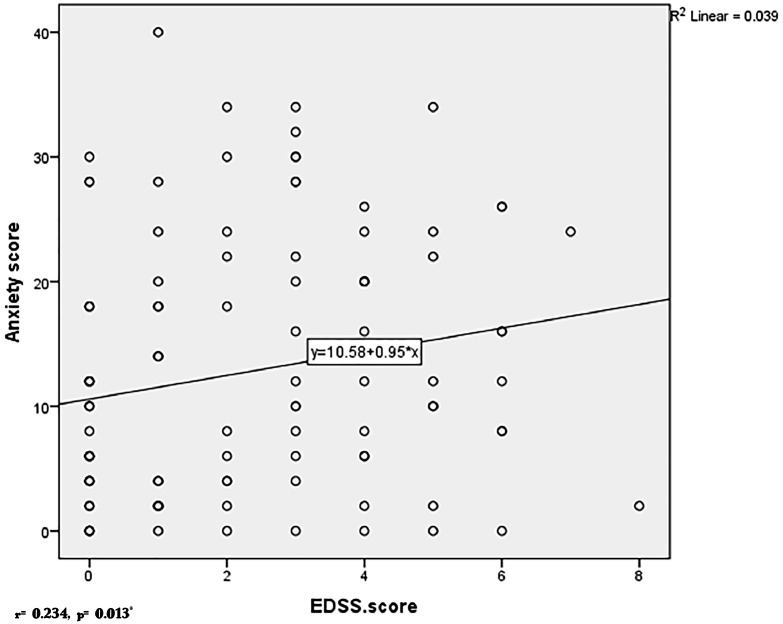
The factors that might affect the anxiety scores i.e. age, disease duration, MS phenotype, EDSS, DMT type, patients’ belief about MS risk to COVID-19 and exposure to a probable COVID-19 case were analysed (Table 5 ). Younger patients (r=−0.252, p = 0.007, Fig. 3 ), those with high EDSS scores (r = 0.0234, p = 0.013, Fig. 4 ) and the patients who believe that MS patients are at high risk for COVID-19 infection (0.009) were more anxious. Anxiety scores were significantly higher among patients who had relapses (18.32±8.6 versus 10.6911.5, p = 0.002) and pseudorelapses (15.12±10.1 versus 10.25±9.5, p = 0.008) during the past month (Table 3).
Table 5.
Factors proposed to have a potential effect on anxiety among patients.
| Factors affecting anxiety | Anxiety score | Test of significance (p-value) | ||
| Mean±Standard deviation | Median | Minimum-maximum | ||
| Phenotype of MS | Kruskal Wallis | |||
| RRMS (n = 96) | 12.5 ± 10.2 | 10.0 | 0–40 | X2=0.762 P = 0.683 |
| SPMS (n = 16) | 13.9 ± 7.9 | 11.0 | 2–26 | |
| PPMS (n = 3) | 14.7 ± 17.5 | 10.0 | 0–34 | |
| DMT type | Mann Whitney z = 0.127 P = 0.899 | |||
| Lymphopenia (n = 25) | 12.8 ± 10.0 | 10.0 | 0–30 | |
| Non-lymphopenia (n = 54) | 12.9 ± 10.1 | 11.0 | 0–40 | |
| MS patients at high risk of COVID⁎⁎ | Kruskal Wallis X2=11.515 P = 0.009* | |||
| Yes (n = 45) | 14.0 ± 11.0 | 12.0 | 0–34 | |
| It depends on certain factors (n = 38) | 10.5 ± 8.7 | 9.0 | 0–30 | |
| Don't know (n = 27) | 15.3 ± 9.5 | 16.0 | 0–40 | |
| Exposure to a probable case of COVID-19 | Mann Whitney z = 0.642 P = 0.521 | |||
| No (n = 102) | 12.5 ± 9.9 | 10.0 | 0–40 | |
| Yes (n = 13) | 14.6 ± 11.1 | 12.0 | 0–30 | |
| Correlation coefficient (r) | p-value | |||
| Patients’ age | −0.0.252 | 0.007* | ||
| MS disease duration | −0.123 | 0.196 | ||
| EDSS | 0.234 | 0.013* | ||
r: spearman coefficient,.
Significant at (P ≤ 0.05),.
the participants who answered no (n = 3) were normal as regards anxiety.
Fig. 3.
Correlation between anxiety and age.
Fig. 4.
Correlation between anxiety and EDSS.
4. Discussion
The novel COVID-19, a pandemic of the kind not seen for a century, has caused global apprehension and distress. The aim of this research was to evaluate the psychological state of MS patients and their caregivers, their knowledge, and behaviours during the COVID-19 pandemic. Patients recruited to this study were significantly anxious, depressed and stressed in comparison to their caregivers and their counterparts from the general population. In absence of a pandemic, patients with MS do have anxiety and depression. The point prevalence of depressive symptoms in MS patients is about 30% (Oliver Tobin, 2019), and the point prevalence of anxiety ranges from 14% to 41% (Korostil and Feinstein, 2007). Depression prevalence among Egyptian MS patients was reported to be higher (52.5%) (Pinkston and Alekseeva, 2006). In our study, however, the percentage of patients with depression and anxiety were significantly higher than what was reported in literature i.e. about 70% of the patients had depression (13.9% mild, 18.3% moderate, 16.5% severe and 22.6% extremely severe) and about 62% had anxiety (5.2% mild, 19.1% moderate, 8.7% severe and 28.7% extremely severe). Though a definite causal effect relationship between the COVID-19 pandemic and anxiety and/or depression cannot be established in the current cross-sectional model, such high prevalence and high grades of severity in comparison to the numbers reported in literature are likely attributed to the pandemic.
Though being highly anxious, MS patients did not seem to be more committed – in contrast to what would be expected - to follow the basic preventive measures for staying safe during the COVID-19 pandemic than the non-MS population, and their anxiety scores did not influence the degree of their commitment. This means that their anxiety is not beneficial or productive. Moreover, more than one quarter (27%) of the patients experienced relapses during the past month (i.e. since the beginning of pandemic), which is relatively high in comparison to a mean annualized relapse rate of 1.7 during the past 12 months. The anxiety scores were significantly higher among patients who experienced relapses and pseudorelapses during the past month. Thus, not only was the anxiety unbeneficial for the patients, but also harmful with regards to the high relapse rates. Thus, efforts are needed to reduce the patients’ anxiety and to deal with the factors that increase the anxiety. Anxiety was not significantly correlated with DMTs stoppage/dose reduction or corticosteroid intake.
In our cohort, younger age, higher EDSS scores and the perception about the risk of MS for COVID-19 risk were the factors significantly correlated with high anxiety scores. The patients who did not know whether the MS patients were at risk for COVID-19 infection and those who thought that they are at risk had significantly high anxiety scores. High EDSS scores were reported to be positively correlated with anxiety scores in literature (Tsivgoulis et al., 2007), and patients with high EDSS scores might be at higher risk or COVID-19 infection and complications (Brownlee et al., 2020; Reder and Cipriana, 2020). In contrast, older MS patients in our sample were less anxious than young patients whereas they might be at a higher risk for COVID-19 infection and complications (Brownlee et al., 2020; Reder and Cipriana, 2020). This can be attributed to probable better cognitive functions among the young patients and better access to social media and news warning the community against the potential dangerous hazards of the pandemic. The anxiety scores were not related to the MS phenotype, duration of the disease or the type of DMT prescribed. This emphasize the importance of adequate education of the MS patients about their actual risk for COVID-19 infection and complications.
Another point we addressed in this study was the knowledge about the factors that may influence COVID-19 risk. The patients’ knowledge about these factors was poor. Age more than 65 years, smoking, poor sleep and psychological stress were reported to increase the risk for COVID-19 infection (CDC. Coronavirus Disease 2019; Zhou et al., 2020; Jordan et al., 2020; Bai et al., 2020). Moderate physical exercise is known to boost the immune system, and is recommended for protection against viral infections including COVID-19 (Owen et al., 2010; Chen et al., 2020). To date, there is no evidence that certain foods/drinks or vitamins/supplements have an influencing role in determining the risk of viral respiratory infection or COVID-19 infection (Gasmi et al., 2020). An exception to this is vitamin D, where some evidence exists that it can reduce the COVID-19 infection risk (Grant et al., 2020). MS patients were less likely to know the role of most of these factors in determination of the COVID-19 infection risk, and they were more likely to report that they do not know in most of the questions about the risk factors. An exception to this was the knowledge about vitamin D role. MS patients and their caregivers were more likely to know the role of vitamin D intake in COVID-19 risk determination than the non-MS population, and more than one fourth (27%) of them started to take vitamin D after the beginning of the pandemic. Patients’ knowledge about MS risk for COVID-19 was also poor. One point to be mentioned here is that MS patients in our study were less educated than the controls (p<0.0001). Though the educational level only does not account for poor knowledge about risk for COVID-19, the lack of knowledge may be partly attributed to the different educational levels. Lower education is one of several factors that influence health literacy such as history of depression and/or anxiety, gender, age, disability, and culture and language (Moeini et al., 2019; Lee et al., 2015; Corona et al., 2008; Rowlands et al., 2017; Nguyen and Gilbert, 2019; Protheroe et al., 2017). Such lack of knowledge necessitate implementing health education programs by the local health authorities and health care providers to reduce anxiety, depression and stress and to educate MS patients and their caregivers about their disease.
The last point we wanted to focus the light on was the MS caregivers. We wanted to evaluate whether they were also more psychologically affected and more keen on following the basic preventive measures to protect themselves and their patients from COVID-19 infection or not. Though about 47% of the MS caregivers had depression and 33% had anxiety, their mean levels were comparable to the non-MS population. This also applies to their behaviours during the pandemic.
One of the limitations of this study was the non-availability of pre-COVID-19 scores to know if the current high scores are due to COVID19 solely, or having MS or some other reason. The cross-sectional design of the study also limits absolute attribution of the change in the DASS-21 to COVID-19. It is also to be noted that the DASS21 is not a diagnostic tool for anxiety, depression or stress. It was just used to screen for these conditions, a followed-up with formal clinical review and other assessments would have been valuable. However, this was not accessible during the COVID-19 pandemic. Another limitation is that the Likert scale used was a three-point scale rather than a five or seven-point scale. Limiting a Likert scale to three reduces validity of the scale and forces the participant to commit to an answer that is not necessarily right because there is no other option. Future studies are needed to also evaluate the health-related quality of life and the patients’ perception of health during the pandemic.
In conclusion, MS patients, in this cohort, were more psychologically affected during COVID-19 pandemic than MS care givers and healthy controls. They were less aware about the risk factors for COVID-19 infection, and their knowledge was poor about the factors that may affect the MS risk to develop COVID-19 infection. A considerable proportion of them reduced the doses/stopped taking their immunomodulatory DMTs without indication. Thus, efforts from the healthcare sectors and psychiatrists are needed to provide health education and assurance for MS patients during the pandemic.
Funding
No funds were received for this research
CRediT authorship contribution statement
Farouk Talaat: Supervision, Project administration, Writing - review & editing. Ismail Ramadan: Conceptualization, Supervision, Writing - review & editing. Salma Aly: Software, Validation, Software, Visualization. Eman Hamdy: Methodology, Validation, Investigation, Resources, Data curation, Writing - original draft, Visualization.
Declaration of Competing Interest
The authors have no conflicts of interest
Acknowledgements
None to be declared.
References
- World Health Organization. Coronavirus disease 2019 (COVID-19): situation Report – 91 [Internet]. 2020 [cited 2020 Apr 21]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200420-sitrep-91-covid-19.pdf?sfvrsn=fcf0670b_4.
- European CDC. Situation update worldwide, as of 5 April 2020 [Internet]. 2020 [cited 2020 Apr 16]. Available from: https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases.
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res [Internet] 2020;287 doi: 10.1016/j.psychres.2020.112934. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemati M., Ebrahimi B., Nemati F. Assessment of Iranian Nurses’ Knowledge and Anxiety Toward COVID-19 During the Current Outbreak in Iran. Arch Clin Infect Dis. 2020 In Press(In Press. [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry. 2020;33(2):19–21. doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. Coronavirus Disease COVID-19): people who are at higher risk for severe illness. Centers for Disease Control and Prevention. 2019;2020 https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-at-higher-risk.html [Internet] [cited 2020 Apr 11]. Available from. [Google Scholar]
- Grigoriadis N., van Pesch V. A basic overview of multiple sclerosis immunopathology. Eur. J. Neurol. 2015;22:3–13. doi: 10.1111/ene.12798. [DOI] [PubMed] [Google Scholar]
- Brownlee W., Bourdette D., Broadley S., Killestein J., Ciccarelli O. Treating multiple sclerosis and neuromyelitis optica spectrum disorder during the COVID-19 pandemic. Neurology. 2020 doi: 10.1212/WNL.0000000000009507. [DOI] [PubMed] [Google Scholar]
- Reder A., Cipriana V. COVID-19 and multiple sclerosis [Internet] MedLink Neurology. 2020 https://www.medlink.com/page/covid_19_and_multiple_sclerosis [cited 2020 Apr 16]. Available from. [Google Scholar]
- England P.H. Guidance on shielding and protecting people defined on medical grounds as extremely vulnerable from COVID-19 [Internet] Public Health England. 2020 https://www.gov.uk/government/publications/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19 [cited 2020 Apr 16]. Available from. [Google Scholar]
- Giovannoni G., Hawkes C., Lechner-Scott J., Levy M., Waubant E., Gold J. The COVID-19 pandemic and the use of MS Disease-Modifying Therapies. Mult Scler Relat Disord. 2020 doi: 10.1016/j.msard.2020.102073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randall D., Thomas M., Whiting D., McGrath A. Depression anxiety stress scales (DASS-21): factor structure in traumatic brain injury rehabilitation. J Head Trauma Rehabil. 2017;32(2):134–144. doi: 10.1097/HTR.0000000000000250. [DOI] [PubMed] [Google Scholar]
- Arabic DASS 21 [Internet]. [cited 2020 Apr 17]. Available from: http://www2.psy.unsw.edu.au/dass/Arabic/Arabic DASS-21.pdf.
- DASS 21 Scoring and Interpretation [Internet]. [cited 2020 Apr 16]. Available from: https://www.bristol.ac.uk/media-library/sites/sps/documents/c-change/dass-twenty-one-scoring-and-interpretation.pdf.
- Vardavas C.I., Nikitara K. COVID-19 and smoking: a systematic review of the evidence. Tob Induc Dis. 2020;18 doi: 10.18332/tid/119324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S. Psychosocial Vulnerabilities to Upper Respiratory Infectious Illness: implications for Susceptibility to Coronavirus Disease 2019 (COVID-19) Perspect Psychol Sci. 2020 doi: 10.1177/1745691620942516. [Internet][cited 2020 Sep 25]; Available from: /pmc/articles/PMC7345443/?report=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ICH GCP (Good Clinical Practice) Training Course [Internet]. 2011 [cited 2020 Apr 4]. Available from: https://ichgcp.net/.
- McNicholas N., Hutchinson M., McGuigan C., Chataway J. 2017 McDonald diagnostic criteria: a review of the evidence. Mult Scler Relat Disord. 2018;24:48–54. doi: 10.1016/j.msard.2018.05.011. [DOI] [PubMed] [Google Scholar]
- Oliver Tobin W. Management of multiple sclerosis symptoms and comorbidities. Contin Lifelong Learn Neurol. 2019;25(3):753–772. doi: 10.1212/CON.0000000000000732. [DOI] [PubMed] [Google Scholar]
- Korostil M., Feinstein A. Anxiety disorders and their clinical correlates in multiple sclerosis patients. Mult Scler. 2007;13(1):67–72. doi: 10.1177/1352458506071161. [DOI] [PubMed] [Google Scholar]
- Pinkston J.B., Alekseeva N. Neuropsychiatric manifestations of multiple sclerosis. Neurol. Res. 2006;28:284–290. doi: 10.1179/016164106X98170. [DOI] [PubMed] [Google Scholar]
- Tsivgoulis G., Triantafyllou N., Papageorgiou C., Evangelopoulos M.E., Kararizou E., Sfagos C. Associations of the Expanded Disability Status Scale with anxiety and depression in multiple sclerosis outpatients. Acta Neurol Scand. 2007;115(1):67–72. doi: 10.1111/j.1600-0404.2006.00736.x. [DOI] [PubMed] [Google Scholar]
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan R.E., Adab P., Cheng K.K. Covid-19: risk factors for severe disease and death. BMJ. 2020;368:m1198. doi: 10.1136/bmj.m1198. [DOI] [PubMed] [Google Scholar]
- Bai Y., Wang X., Huang Q., Wang H., Gurarie D., Ndeffo-Mbah M. SARS-CoV-2 infection in health care workers: a retrospective analysis and a model study. medRxiv. 2020 doi: 10.1016/j.sleepx.2020.100028. 2020 Apr 103.29.20047159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen N., Sparling P.B., Healy G.N., Dunstan D.W., Matthews C.E. Vol. 85. Mayo Clinic Proceedings; 2010. pp. 1138–1141. (Sedentary behavior: Emerging evidence For a New Health Risk). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen P., Mao L., Nassis G.P., Harmer P., Ainsworth B.E., Li F. Wuhan coronavirus (2019-nCoV): the need to maintain regular physical activity while taking precautions. J Sport Health Sci. 2020;9:103–104. doi: 10.1016/j.jshs.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasmi A., Noor S., Tippairote T., Dadar M., Menzel A., Bjørklund G. Individual risk management strategy and potential therapeutic options for the COVID-19 pandemic. Clin Immunol. 2020 doi: 10.1016/j.clim.2020.108409. https://linkinghub.elsevier.com/retrieve/pii/S1521661620302254 [Internet]Apr [cited 2020 Apr 17];108409. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant W.B., Lahore H., McDonnell S.L., Baggerly C.A., French C.B., Aliano J.L. Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients. 2020;12(4):988. doi: 10.3390/nu12040988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moeini B., Rostami-Moez M., Besharati F., Faradmal J., Bashirian S. Adult Functional Health Literacy and its Related Factors: a Cross-Sectional Study. Int J Epidemiol Res. 2019;6(1):24–29. http://ijer.skums.ac.iroriginalarticle [Internet]Jan 19 [cited 2020 Sep 26]Available from. [Google Scholar]
- Lee H.Y., Lee J., Kim N.K. Gender Differences in Health Literacy Among Korean Adults: do Women Have a Higher Level of Health Literacy Than Men? Am J Mens Health. 2015;9(5):370–379. doi: 10.1177/1557988314545485. https://pubmed.ncbi.nlm.nih.gov/25122719/ [Internet]Sep 13 [cited 2020 Sep 26]Available from. [DOI] [PubMed] [Google Scholar]
- Corona G., Casetta B., Sandron S., Vaccher E., Toffoli G. Rapid and sensitive analysis of vincristine in human plasma using on-line extraction combined with liquid chromatography/tandem mass spectrometry. Rapid Commun Mass Spectrom. 2008;22(4):519–525. doi: 10.1002/rcm.3390. http://www.euro.who.int/pubrequest [Internet].[cited 2020 Sep 26]Available from. [DOI] [PubMed] [Google Scholar]
- Rowlands G., Shaw A., Jaswal S., Smith S., Harpham T. Health literacy and the social determinants of health: a qualitative model from adult learners. Health Promot Int. 2017;32(1):130–138. doi: 10.1093/heapro/dav093. https://academic.oup.com/heapro/article/32/1/130/2950953 [Internet]Feb 1 [cited 2020 Sep 26]Available from. [DOI] [PubMed] [Google Scholar]
- Nguyen J., Gilbert L. Health Literacy among Individuals with Disabilities: a Health Information National Trends Survey Analysis. Perm J. 2019:23. doi: 10.7812/TPP/19.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Protheroe J., Whittle R., Bartlam B., Estacio E.V., Clark L., Kurth J. Health literacy, associated lifestyle and demographic factors in adult population of an English city: a cross-sectional survey. Heal Expect. 2017;20(1):112–119. doi: 10.1111/hex.12440. [Internet]Feb 1 [cited 2020 Sep 26]Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]