Abstract
Malnutrition in patients with cancer is a ubiquitous but neglected problem that can reduce patient survival/quality of life and increase treatment interruptions, readmission rates, and healthcare costs. Malnutrition interventions, including nutrition support through dietary counseling, diet fortification, oral nutrition supplements (ONS), and enteral and parenteral nutrition can help improve health outcomes. However, nutritional care standards and interventions for cancer are ambiguous and inconsistently applied. The lack of systematic malnutrition screening and intervention in ambulatory cancer care has especially significant consequences and thus the nutrition support of patients with cancer represents an area for quality improvement. United States healthcare payment models such as the Oncology Care Model are linked to quality of care and health outcomes. Quality improvement programs (QIPs) can advance patient-centered care, perfect care processes, and help healthcare professionals meet their quality measure performance goals. Malnutrition QIPs like the Malnutrition Quality Improvement Initiative (MQii) have been shown to be effective in identifying and treating malnutrition. However, little is known about or has been reported on nutrition or malnutrition-focused QIPs in cancer care. This paper provides information to support translational research on quality improvement and outlines the gaps and potential opportunities for QIPs in the nutrition support of patients with cancer.
Keywords: malnutrition, ambulatory cancer care, quality improvement programs, malnutrition screening, nutrition interventions, quality care, health outcomes
1. Introduction
Malnutrition in patients with cancer is a ubiquitous but neglected problem that continues to remain the “elephant in the room” [1]. Indeed, up to 80% of patients with solid tumors develop malnutrition—most often protein-energy undernutrition—during the course of their cancer care [2,3,4]. Malnutrition negatively impacts many health outcomes. Two decades ago, it was identified that the loss of even 5% of body weight decreased survival in patients with cancer [5], and multiple studies have since corroborated the association between weight loss and poor cancer outcomes [6,7,8]. The Evidence Analysis Library of the Academy of Nutrition and Dietetics (Academy) has documented strong evidence (Grade 1) of an association between poor nutrition status in adult oncology patients and decreased tolerance to radiation treatment, decreased tolerance to chemotherapy treatment, increased length of hospital stay, lower quality of life, and mortality [9]. Malnutrition in patients with cancer is also associated with higher healthcare costs [10].
Malnutrition interventions, including nutrition support through dietary counseling, diet fortification, oral nutrition supplements (ONS), and enteral and parenteral nutrition, can help improve health outcomes [11]. However, in the American outpatient setting, where nearly all oncology patients receive treatment, ambulatory nutritional care standards and interventions for cancer are ambiguous and inconsistently applied [10]. This is further complicated by the fact that registered dietitian nutritionists (RDNs) are not routinely employed in outpatient cancer centers and the medical nutritional therapy that they provide is not consistently a part of multidisciplinary outpatient cancer care or adequately reimbursed [12]. The lack of systematic malnutrition screening and intervention in ambulatory cancer care has especially significant consequences for both patient and healthcare outcomes and thus the nutrition support of patients with cancer represents an important area for quality improvement.
In the United States (U.S.), healthcare payment models are increasingly linked to quality of care and health outcomes. For example, the U.S. Oncology Care Model (OCM) is a specialty payment program that aims to provide greater quality, more highly coordinated cancer care at the same or lower cost. Physician practices participating in the OCM commit to providing enhanced services to their Medicare patients. Such services can include care coordination, navigation, and aligning with national treatment guidelines [13]. Systematic malnutrition screening and intervention are not required but are a good fit with these enhanced services, particularly because malnutrition impacts health outcomes. The OCM also includes performance against specific quality measures, including unnecessary Emergency Department (ED) visits and patient satisfaction, as well as total cost of care thresholds. Poor health outcomes related to malnutrition, such as hospital readmissions and ED visits, can reduce physicians’ Medicare payments.
As improving quality of care continues to gain momentum in all care segments, healthcare professionals are using quality improvement programs (QIPs) to advance patient-centered care, perfect care processes, and meet their quality measure performance goals. Malnutrition QIPs have been shown to be effective in identifying and treating malnutrition [14]. However, little is known about or has been reported on nutrition or malnutrition-focused QIPs in cancer care, even though the Oncology Nutrition Dietetic Practice Group of the Academy has identified quality improvement as one area where more translational research is needed [10].
This paper provides information to support translational research on quality improvement and the development of malnutrition-focused QIPs for cancer care. First, this paper briefly reviews the healthcare quality improvement process, including the Malnutrition Quality Improvement Initiative (MQii). Next, the paper reports on various quality frameworks for nutrition in adult cancer care, identifying international and U.S. nutrition-specific oncology care guidelines as well as the presence or absence of nutrition in general U.S. cancer care guidelines, standards, quality measures, and initiatives. Finally, the paper describes the evidence for malnutrition and nutrition QIPs in cancer care. In summary, this review—intended for individual teams and healthcare organizations—outlines the gaps and potential opportunities for QIPs in the nutrition support of patients with cancer.
2. The Healthcare Quality Improvement Process
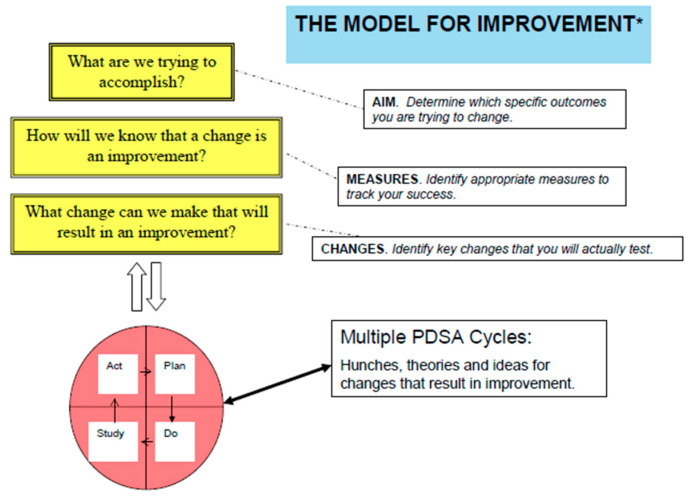
The healthcare quality improvement process can seem overwhelming, but it does not have to be. Healthcare quality improvement is patient-focused and thus the goal of a QIP is to identify how care processes can be improved to benefit patient health outcomes. Ideally, the process starts with a single care team or small unit of caregivers, such as a cancer care or nutrition support team, and then often evolves to include behavior and practice changes across multiple levels of a healthcare organization. QIP models vary in their approach and methods; however, all reflect the common principle that quality improvement is a continuous activity, not a single event. Thus, as changes are implemented, ongoing issues are addressed, and further changes are made to perfect the targeted patient care process. In healthcare, the most common QIP is the Model for Improvement (MFI), which uses a rapid cycle process called Plan Do Study Act (PDSA) (Figure 1) [15].
Figure 1.
The Model for Improvement [16] used in healthcare quality improvement. * The Plan Do Study Act (PDSA) cycle was developed by W. Edwards Deming [17].
To begin the PDSA cycle, the team
Establishes improvement goals
Identifies possible strategies
Chooses specific interventions to implement
Prepares a written action plan.
Through successive PDSA cycles, clinicians arrive at a final process change which they believe is most effective in producing the desired results. Subsequently, they may work to implement and spread this process change through their broader healthcare organization. Ultimately, it is the small changes perfected through the PDSA cycle which provide an opportunity for larger and more lasting effects on the healthcare system’s quality of patient care [15].
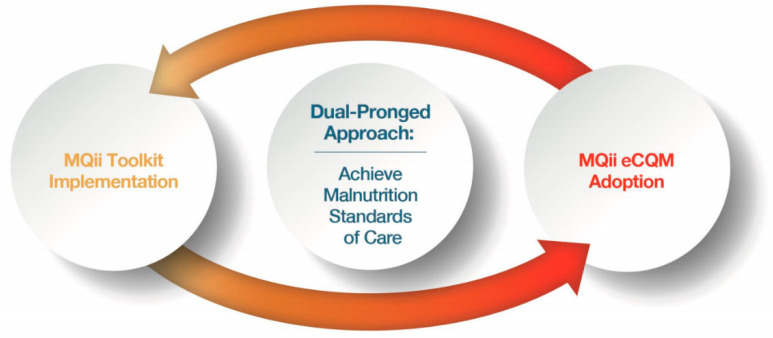
The Malnutrition Quality Improvement Initiative (MQii) is a malnutrition-specific QIP framework using the PDSA cycle that could serve as a model for nutrition-focused QIPs in cancer care. The MQii began in 2013, when a variety of stakeholder organizations highlighted gaps in existing malnutrition care and the impact of these gaps on patient outcomes. Following literature reviews, landscape assessments, engagements with key opinion leaders, and best practice research, the MQii was established in partnership with the Academy, Avalere Health, and other stakeholders. Support for the MQii has been provided by Abbott. MQii innovations include the development of an evidence-based malnutrition quality improvement toolkit and a set of malnutrition electronic clinical quality measures (eCQMs) (Figure 2) [14]. The MQii toolkit is interdisciplinary and open-access [18]; further details on the four malnutrition eCQMs are available on the Academy’s website [19].
Figure 2.
The Malnutrition Quality Improvement Initiative (MQii) dual-pronged approach to helping hospitals achieve malnutrition standards of care [14].
The MQii initially focused on advancing evidence-based, high-quality, patient-centered care for hospitalized older adults (aged 65 years and older). To help healthcare institutions achieve malnutrition standards of care, the MQii also established a learning collaborative, which currently boasts a membership of over 250 U.S. healthcare institutions. Results from the learning collaborative demonstrated that hospital teams which implemented the MQii improved the timely identification, quality of care, and treatment of older adults who were malnourished or at risk of malnutrition. RDNs and their interdisciplinary colleagues have led this implementation process. Furthermore, the MQii is helping to expand learning collaborative hospitals’ leadership into transitions of care, securing nutrition quality measures in core data sets and national data registries, and implementing the MQii model in other care settings and with other patient populations [20]. Specific applications of the MQii model to cancer care alone have not yet been reported.
3. Quality Frameworks for Nutrition in Cancer Care
QIPs such as the MQii often focus on improving patient care processes by more closely aligning the processes with recommended clinical guidelines, standards, quality measures, best practices, and other quality frameworks. For example, one way in which physician practices participating in the OCM can enhance their services is by following national treatment guidelines. However, in nutrition-specific oncology care, the standards and guidelines are inconsistent and may be of limited quality [21]. Furthermore, nutrition is frequently not included in general oncology standards, guidelines, quality measures, and initiatives. The following summarizes existing nutrition-specific oncology care quality frameworks and describes where nutrition is or is not included in the quality frameworks of general oncology care. The gaps may be helpful for individual teams to identify possible areas for malnutrition QIPs and for healthcare organizations to identify opportunities for improvement in national cancer care guidelines, standards, and quality programs.
3.1. International Nutrition-Specific Oncology Care Guidelines
A recent international review of nutrition care procedures in nutrition-specific guidelines for patients with cancer identified 17 guidelines [21]. Using the Appraisal of Guidelines for Research and Evaluation (AGREE II) methodology to evaluate the quality of those guidelines, Zhao et al. rated the European Society for Clinical Nutrition and Metabolism (ESPEN) [11] guidelines and Australian guidelines [22] as having the highest total quality scores (>60%). They further evaluated 12 of the guidelines and found heterogeneity in the content/tools of nutrition screening and/or assessment, application of immune nutrients, and selection of nutrition support pathways, and they concluded that the quality of nutrition guidelines for patients with cancer was highly variable [21].
3.2. U.S. Nutrition-Specific Oncology Care Standards and Guidelines
Of the 17 nutrition-specific oncology care guidelines evaluated by Zhao et al., only two were from the U.S. [9,23]. However, in broadening the approach to include nutrition-specific standards of practice, several additional U.S. nutrition-specific quality frameworks for cancer care can be identified (Table 1).
Table 1.
U.S. nutrition-specific oncology care standards and guidelines.
| Organization and Developer | Title and Target Audience | Methodology and Scope |
|---|---|---|
| Academy of Nutrition and Dietetics (the Academy) Oncology Workgroup |
Oncology Evidence-Based Nutrition Practice Guideline for Adults [9] Registered Dietitian Nutritionists (RDNs) |
|
| Academy Oncology Nutrition Dietetic Practice Group, with guidance from Academy Quality Management Committee |
Academy of Nutrition and Dietetics: Revised 2017 Standards of Practice and Standards of Professional Performance for Registered Dietitian Nutritionists (Competent, Proficient, and Expert) in Oncology Nutrition [24] RDNs |
|
| American Society for Parenteral and Enteral Nutrition (ASPEN) ASPEN Members |
Review of American Society for Parenteral and Enteral Nutrition (ASPEN) Clinical Guidelines for Nutrition Support in Cancer Patients: Nutrition Screening and Assessment [25] Multidisciplinary teams |
|
| ASPEN ASPEN Members |
Nutrition Support in Surgical Oncology [26] Multidisciplinary teams |
|
| ASPEN ASPEN Members and Board of Directors |
ASPEN Clinical Guidelines: Nutrition Support Therapy During Adult Anticancer Treatment and in Hematopoietic Cell Transplantation [23] Multidisciplinary teams |
|
3.3. Nutrition in U.S. General Oncology Care Standards and Guidelines
Nutrition is lacking in many of the U.S. general oncology care standards and guidelines. However, specific sections on nutrition are part of the American College of Surgeons (ACS) Commission on Cancer (CoC) Accreditation Standards, the Association of Community Cancer Centers (ACCC) Cancer Program Guidelines, several Enhanced Recovery after Surgery (ERAS®) Society guidelines, and in the National Cancer Institute’s Physicians Data Query® resources (Table 2).
Table 2.
U.S. general oncology care standards and guidelines including nutrition.
| Organization | Reference | Methodology and Scope |
|---|---|---|
| American College of Surgeons (ACS) ACS Multidisciplinary Commission on Cancer |
Commission on Cancer. Optimal Resources for Cancer Care (2020 Standards) [27] Accredited U.S. cancer programs |
|
| Enhanced Recovery After Surgery (ERAS®) Society Joint efforts of the ERAS® Society and authors from the international ERAS® Gynecology chapters |
Guidelines for Perioperative Care in Gynecologic/Oncology: Enhanced Recovery After Surgery (ERAS®) Society Recommendations-2019 Update [28] Surgical teams |
|
| ERAS® Society Endorsed by ERAS® Society and international panel of experts in major head/neck cancer surgery and enhanced recovery after surgery |
Optimal Perioperative Care in Major Head and Neck Cancer Surgery with Free Flap Reconstruction, a Consensus Review and Recommendations from the Enhanced Recovery After Surgery Society [29] Surgical teams |
|
| ERAS® Society ERAS® Society working group |
Guidelines for Perioperative Care after Radical Cystectomy for Bladder Cancer: Enhanced Recovery After Surgery (ERAS®) Society recommendations [30] Surgical teams |
|
| National Cancer Institute PDQ® Supportive and Palliative Care Editorial Board |
PDQ® Nutrition in Cancer Care [31] Clinicians |
|
The National Comprehensive Cancer Network (NCCN) is an alliance of 28 leading U.S. cancer centers focused on improving the quality of cancer care. NCCN guidelines are evidence-based, consensus-driven, and reported to be the most thorough and frequently updated clinical practice guidelines in any area of medicine [32], but most contain limited if any nutrition recommendations or information (Table 3 and Supplementary Materials). Not surprisingly, the diagnoses with more frequent nutrition mentions in the NCCN guidelines all involve some part of the gastrointestinal tract. The most common references to nutrition are related to nutrition status, nutrition counseling, and nutrition support. Further details of the frequencies and types of references to nutrition in the NCCN guidelines are provided in the appended Supplementary Materials.
Table 3.
Summary of nutrition mentions in adult National Comprehensive Cancer Network (NCCN) guidelines [32] *.
| Type of NCCN Guideline (N) | Number (%) of NCCN Guidelines with Nutrition Mentions | NCCN Guidelines with Specific Nutrition Section |
|---|---|---|
| Diagnosis-specific guidelines (53) | 19 (36%) 1–10 nutrition mentions 3 (6%) 11–25 nutrition mentions 3 (6%) >25 nutrition mentions |
Head and neck cancer |
| Population-specific guidelines (2) | 1 (50%) 1–10 nutrition mentions 1 (50%) >25 nutrition mentions |
Older adult oncology |
| Supportive care guidelines (12) | 6 (50%) 1–10 nutrition mentions 3 (25%) >25 nutrition mentions |
Cancer-related fatigue Survivorship |
| Patient-directed guidelines (39) | 9 (23%) 1–10 nutrition mention 2 (5%) 11–25 nutrition mentions |
Nasopharyngeal cancer Oral cancers Stomach cancer |
* Complete count of nutrition mentions by guideline provided in Supplementary Materials.
Compared to NCCN guidelines, the American Society of Clinical Oncology (ASCO) guidelines have even fewer mentions of nutrition. One new ASCO Management of Cancer Cachexia guideline has a significant focus on nutrition. However, of the other more than 90 ASCO guidelines, nutrition is mentioned in just two guidelines; once in the Management of Osteoporosis in Survivors of Adult Cancers with Nonmetastatic Disease guideline and twice in the Practical Assessment and Management of Vulnerabilities in Older Patients Receiving Chemotherapy guideline [33]. In summary, few U.S. general oncology care standards and guidelines mention nutrition and even fewer include it as a specific area of focus.
3.4. Nutrition in U.S. Cancer Care Quality Measures, Initiatives, and Data Sources
Nutrition is nearly absent in U.S. cancer care quality measures and initiatives. In the oncology quality care measures developed by national organizations, specifically ASCO’s more than 150 quality measures [34], CoC’s 23 quality measures [35], the National Quality Forum (NQF)’s 16 quality measures [36], and the Oncology Nursing Society’s 10 quality measures [37], no quality measures are specific to or mention nutrition. Furthermore, nutrition is not part of any of ASCO’s cancer care quality initiatives [38], such as the Quality Training Program (QTP), Quality Oncology Practice Initiative (QOPI), and Quality Certification Program (QCP), and there is just one project specific to nutrition in the more than 80 QTP projects listed in the ASCO Quality Improvement Library. Additionally, the American College of Surgeon and American Cancer Society’s National Cancer Database [39], a hospital data registry used for quality benchmarking, does not include nutrition as a variable in the publicly available data.
4. Review of Malnutrition and Nutrition-Focused QIPs in Cancer Care
To review the evidence base on malnutrition and nutrition-focused QIPs in cancer care, we conducted a search in Embase® and Medline® on research from developed countries published in English between 1 January 2000 to 31 December 2019. Our search was exclusive to research in the adult population (aged 18 years and older), in inpatient and outpatient settings, and for all active cancer diagnoses (we excluded patients in hospice/palliative care). The search terms are detailed in Table 4. Key words were linked using “OR” as a Boolean function and the results of the components were combined using the “AND” Boolean function. All study designs were included and duplicate studies were removed from the final abstract count. A total of 228 abstracts were identified and then screened independently by two reviewers to distinguish which publications were specific to malnutrition and nutrition-focused QIPs or quality effectiveness process initiatives in cancer care. The two reviewers then met and agreed that seven abstracts satisfied the criteria. Of these, only one was a peer-reviewed article; the remaining six were conference abstracts.
Table 4.
Key search terms for research review of malnutrition and nutrition-focused quality improvement programs (QIPs) and quality effectiveness process initiatives in cancer care.
| String | Terms |
|---|---|
| Cancer | Cancer, neoplasm, tumor, oncology, carcinoma, sarcoma |
| Nutrition | Food, diet, nutrition |
| Care | Assessment, care plan, plan, counsel, council, diagnosis, consult, discharge education, education, evaluation, index, intervention, monitoring, oral nutrition supplement (ONS), screening, therapy, treatment |
| Efficacy | Efficacy, effectiveness, efficient, efficiency, effectiveness, effectivity |
| Quality | Improvement of quality, improvement of care, improvement of treatment, improvement of therapy |
Two conference abstracts summarized specific quality improvement programs; both aimed to increase the rate of RDN-documented nutrition assessment and plan of care through successive PDSA cycles. Brown et al. had a goal of increasing the rate of an RDN-documented nutrition assessment to 65%; at baseline, 41.1% of new patients had RDN-documented nutrition plans within 90 days of their first appointment. Multiple causes of the low nutrition plan baseline rates were identified, including those related to patient or family characteristics/needs, clinical dietitian resources, physician limitations, process flaws, and difficulty with the electronic medical record [40]. Levonvak et al. reported that the rate of a documented nutrition care plan doubled after a month of starting the second PDSA cycle intervention [41].
The other five abstracts described the evaluation of the effectiveness of new nutrition-related clinical processes, pathways, models of care, and/or roles [42,43,44,45,46]. One conference abstract and the one article evaluated the benefit of training a nutrition assistant to perform nutrition screening and intervention for oncology patients and found that the role of nutrition assistants could benefit patient outcomes [42,46]. Further information about the seven abstracts is summarized in Table 5.
Table 5.
Summary of abstracts identified through a research review of malnutrition and nutrition-focused quality improvement program (QIPs) and quality effectiveness process initiatives in cancer care.
| Publication Type and Cancer Diagnosis | Title | Methodology | Conclusions |
|---|---|---|---|
| Article Head and neck cancer |
Evaluating the effectiveness of a nutrition assistant role in a head and neck cancer clinic [42] |
|
|
| Conference abstract Neuroendocrine tumor (NET) |
Evaluation of nutritional deficiencies in a new gastroenterology-led South Wales neuroendocrine tumor (NET) service [43] |
|
|
| Conference abstract Gastrointestinal (GI) cancer |
A nutrition-focused quality improvement program to improve rate of documented nutrition plan at a safety-net hospital gastrointestinal (GI) oncology clinic [41] |
|
|
| Conference abstract Gastrointestinal (GI) cancer |
Development of a nutrition-focused quality improvement program for new patients with cancer seen at the UTSW Simmons Comprehensive Cancer Center (SCCC) outpatient gastrointestinal (GI) oncology clinic [40] |
|
|
| Conference abstract Not specified |
Onconut®: Nutritional care optimization for cancer patients [44] |
|
|
| Conference abstract Lung cancer |
Evaluation of an evidence-based nutrition care pathway for lung cancer patients undergoing radiotherapy [45] |
|
|
| Conference abstract Not specified |
Nutrition assistants and malnutrition in a cancer setting: Exploring an integrated model of care [46] |
|
|
5. Discussion
Malnutrition has long been linked to poor patient and health outcomes, including reducing patient survival and quality of life and increasing treatment interruptions, readmission rates, and healthcare costs. Evidence indicates that early nutrition intervention can reduce complication rates, lengths of hospital stay, readmission rates, mortality, and costs of care [10]. However, for many patients, malnutrition continues to go unrecognized and untreated [47]. Similarly, while nutrition support is recognized as critical for oncology care, and recent evidence continues to show that specific interventions such as enteral and parenteral feeding are associated with positive survival benefits in patients with metastatic disease [48], malnutrition remains a frequent comorbid condition for patients with cancer [49]. During the last decade, the collaborative and visionary leadership of the MQii and the implementation of malnutrition and nutrition-focused QIPs nationwide have helped to advance malnutrition care for hospitalized patients in the U.S. Unfortunately, there has been less progress in malnutrition care in oncology and at present there are few reported models of well-developed U.S. patient care programs providing optimal malnutrition care. There may be several reasons for this gap in care and thus potential opportunities for individual teams and healthcare organizations to advance malnutrition care in the nutrition support of patients with cancer.
Firstly, there are no quality models specific to malnutrition or nutrition care in oncology that provide a framework for comprehensive care. The MQii was initially developed to target hospital patients and older adults specifically. Only recently has there been a focus by RDNs and other healthcare professionals to promote MQii learnings across the continuum of care and with different patient populations [20]. One U.S. teaching hospital has reported using elements of the MQii Toolkit to measure and improve quality, and as a part of their initiative, they began providing free, early immunonutrition supplements and nutrition education to high-risk patients with colorectal cancer during preadmission testing. Overall, they reported significant reductions in length of stay (LOS) (from 8 to 6 days, p < 0.01) and infection rates (from 14% to 9%, p < 0.01) for patients who were malnourished or at risk of malnutrition, although they did not report specific results for the cancer subpopulation [50]. Similar to this institution, cancer care teams could readily adapt MQii tools and processes for use in oncology clinics to provide more inclusive care. The broader implementation of ERAS® is also an opportunity to model quality malnutrition care and impact outcomes. ERAS® is not a single, rigid protocol but rather a comprehensive new way for multidisciplinary teamwork to make changes as knowledge evolves [51]. ERAS® includes a significant nutrition component and ERAS® has been shown to decrease complications, reduce LOS, and save costs for oncology patients undergoing surgery [52,53,54]. Another recommendation to incentivize more comprehensive care is for healthcare organizations to advocate for the addition of malnutrition care to future updates of the OCM. The Academy has recently strongly encouraged the inclusion of medical nutrition therapy into the care design and payment for CMS’ next proposed payment model—the Oncology Care First model. It reinforced that “there is strong (grade I) evidence for evaluation of nutritional status as a key component of the oncology patient care process” [55].
Secondly, while there are several nutrition-specific oncology care guidelines, they are inconsistent and nutrition is usually not included in general oncology care standards and guidelines; in contrast to other countries, U.S. oncology care guidelines do not recommend frequent interaction or access to oncology nutrition services [56]. This can make it more difficult to initiate nutrition-focused QIPs to optimize patient and health outcomes. U.S. oncology care guidelines could benefit from education and awareness building, starting with medical education, although changing guidelines is a lengthy process. There are examples of nutrition support for patients with cancer included as a part of medical school nutrition curriculum [57] but, unfortunately, the adoption of such nutrition curriculum has not been widespread. In a recent systematic review, Crowley et al. identified insufficient inclusion of nutrition in medical education, regardless of country, setting, or year of medical education [58]. Walsh et al. noted that only 25% of medical schools have a dedicated nutrition curriculum and few meet the National Academy of Science’s recommended 25 h of nutrition education. Furthermore, Walsh et al. have pointed out that the American Board of Internal Medicine’s Maintenance of Certification for Medical Oncology Fellows does not have any requirements related to nutrition [1]. Malnutrition advocates have purposely targeted the inclusion of nutrition in medical standards and guidelines. For example, the Malnutrition Quality Collaborative in their National Blueprint: Achieving Malnutrition Care in Older Adults, 2020 Update makes the specific recommendation to “Develop core materials and integrate malnutrition care training modules into school and university curriculums for physicians” [59]. Another approach could be to engage clinicians directly. For example, the Prevalence of Malnutrition in Oncology (PreMiO) study was conducted at 22 medical oncology centers across Italy to raise oncologists’ awareness of the “pressing need for early assessment of nutrition status in cancer patients and the need for providing appropriate nutritional care.” In the model, oncologists—rather than RDNs—evaluated the nutrition status of patients at their first medical oncology visit and results demonstrated that oncologists could be effectively trained to perform assessments that identified malnutrition and its risks [3]. The role of the oncologist in interdisciplinary nutrition care is further delineated in a review by Muscaritoli et al., where they outline a roadmap for oncologists to move from guidelines to clinical practice [60]. To date, no such initiatives seem to have been undertaken in the U.S., although the need to develop a “culture of nutrition” among all cancer care staff has been identified [56]. Cancer care teams can help bring precedence to the need for including nutrition in general oncology recommendations and standards by implementing and publishing the results of malnutrition and nutrition-focused QIPs.
Thirdly, based on the evaluation of NCCN guidelines, patient recommendations have limited focus on nutrition. Mentions of nutrition in the NCCN guidelines are more frequent in the clinical diagnosis-specific guidelines compared to the patient guidelines. This is of concern because, at its core, healthcare quality improvement and comprehensive cancer care are patient-focused. Rauh et al. have stated that “Nutrition is a major issue for most patients with cancer and their families, and its impact will often lead to highly emotionalised discussions in our daily practice. For all participants, there often is an unpronounced underlying fear: that their cancer may already have ‘consumed’ the patient, and thus ‘won’. On the other hand, nutrition is one factor they potentially (think they) can influence.” Rauh et al. go on to describe the Cancer Patient’s Nutritional Bill of Rights, which was based on ESPEN’s guidelines for nutrition in cancer patients, published by the European Cancer Patient Coalition, and presented to the European Parliament in November 2017 [61]. Cancer care teams and healthcare organizations could consider creating and adopting a similar Bill of Rights in the U.S. to empower patients, their families, and healthcare providers to systematically identify and intervene for malnutrition in cancer care which could help improve both patient and healthcare system outcomes.
Fourthly, there is a complete lack of U.S. nutrition quality measures for oncology. In the over 200 distinct quality measures for cancer care identified, none were specific to nutrition. The Academy, in describing their first ever malnutrition eCQMs, recognized the availability of these eCQMs as a “tremendous opportunity to advance patient/client nutrition care.” They further underscored that “the development of the eCQMs and tools to support implementation is one of the most innovative initiatives undertaken by the Academy of Nutrition and Dietetics” [62]. Consistent malnutrition screening is critical for the early identification and treatment of malnutrition; however, in a survey of U.S. ambulatory oncology settings, only about half reported screening for malnutrition [12]. Targeting the development of malnutrition quality measures specific to cancer care should be a priority for nutrition and oncology organizations because eCQMs are an effective tool to help identify where malnutrition screening is not occurring as well as to document the burden of malnutrition and the positive outcomes that are realized when malnutrition is better identified and treated.
Lastly, there is a void of malnutrition and nutrition-focused QIPs and data sources for nutrition support in cancer care. In our review, we found very few published QIPs for malnutrition and nutrition care in oncology and all but one were conference abstracts vs. peer-reviewed articles. Published QIPs can help provide examples for other clinicians to mirror, particularly as there are few published best practice models in the U.S. of oncology-focused patient care programs to prevent and treat malnutrition. The Journal of the Academy of Nutrition and Dietetics recently published a special supplement on the MQii to “provide a guide or template for individuals and organizations interested in continually improving the nutrition care in their respective facility regardless of their particular situations and resources” [14]. There are also nutrition-focused QIPs where the study population includes patients with cancer. In one such study, oncology patients using ONS as part of the QIP were associated with 46.1% fewer 30-day hospital readmissions after controlling for other covariates and confounding variables (p < 0.001) [63]. Similarly, a secondary analysis of at-risk or malnourished hospital patients with cancer in a nutrition-focused QIP documented statistically significant reductions in 30-day hospital readmission rates and lengths of stay, with potential cost savings of >$3800 per patient treated [64]. As clinicians develop and implement malnutrition and nutrition-focused QIPs, they should work to publish their results and include the QIPs in ASCO’s Quality Improvement Library to help increase visibility among interdisciplinary care teams nationwide. There is also a need for benchmarking data that can be used for quality care comparisons for oncology malnutrition care. Thus, it is recommended that healthcare organizations consider how data sources, such as the National Cancer Database, can be expanded to include specific data points relevant to malnutrition and nutrition care.
6. Conclusions
Existing literature shows that poor nutrition remains a challenge for both patients with cancer and healthcare providers, adversely impacting morbidity and mortality, decreasing quality of life, and driving substantial cost burdens for the healthcare system. The lack of emphasis on nutrition in oncology treatment guidelines in the U.S. suggests that nutrition is an under-utilized tool in cancer treatment. The nature of much of cancer care taking place in outpatient clinics makes this an ideal setting for the successful execution of a QIP. Specifically, patients have regular office visits for treatment and follow-up, and, during these visits, their nutrition status and risk for malnutrition could be monitored, recommendations made, and compliance verified. Such a coordinated effort would require the involvement of multiple patient care disciplines but could yield significant improvements in patient outcomes and quality of life. There is an opportunity for individual teams and healthcare organizations to help fill such existing gaps in malnutrition care in oncology clinics and, as documented in this paper, implement and then leverage QIPs focused on improving the nutrition support of patients with cancer.
Acknowledgments
We would like to thank Elaine B. Trujillo for her review of and suggestions for this manuscript.
Supplementary Materials
The following are available online at https://www.mdpi.com/2227-9032/8/3/227/s1. Table S1: NCCN Guidelines for Treatment of Cancer by Site, Table S2: NCCN Guidelines for Treatment of Cancer by Specific Patient Population, Table S3: NCCN Guidelines for Supportive Care, Table S4: NCCN Guidelines for Patients.
Author Contributions
Conceptualization, M.B.A., J.R. and K.K.; approach and analysis, M.B.A., J.R., J.B., K.K. and R.H.; resources, M.B.A. and J.R.; writing—original draft preparation, M.B.A.; writing—review and editing, M.B.A., J.R., J.B., K.K. and R.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
M.B.A., K.K. and R.H. are employees of the Abbott Nutrition Division of Abbott and shareholders in Abbott. J.R. is a nutrition consultant for the Abbott Nutrition Division of Abbott. J.B. is an employee of Kaiser Permanente and has received honorariums as a speaker for the Abbott Nutrition Division of Abbott.
References
- 1.Walsh D., Szafranski M., Aktas A., Kadakia K.C. Malnutrition in cancer care: Time to address the elephant in the room. J. Oncol. Pract. 2019;15:357–359. doi: 10.1200/JOP.19.00165. [DOI] [PubMed] [Google Scholar]
- 2.Von Haehling S., Anker S.D. Cachexia as a major underestimated and unmet medical need: Facts and numbers. J. Cachexia Sarcopenia Muscle. 2010;1:1–5. doi: 10.1007/s13539-010-0002-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Muscaritoli M., Lucia S., Farcomeni A., Lorusso V., Saracino V., Barone C., Plastino F., Gori S., Magarotto R., Carteni G., et al. Prevalence of malnutrition in patients at first medical oncology visit: The PreMiO study. Oncotarget. 2017;8:79884–79896. doi: 10.18632/oncotarget.20168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Caillet P., Liuu E., Raynaud Simon A., Bonnefoy M., Guerin O., Berrut G., Lesourd B., Jeandel C., Ferry M., Rolland Y., et al. Association between cachexia, chemotherapy and outcomes in older cancer patients: A systematic review. Clin. Nutr. Edinb. Scotl. 2017;36:1473–1482. doi: 10.1016/j.clnu.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 5.Dewys W.D., Begg C., Lavin P.T., Band P.R., Bennett J.M., Bertino J.R., Cohen M.H., Douglass H.O., Engstrom P.F., Ezdinli E.Z., et al. Prognostic effect of weight loss prior to chemotherapy in cancer patients. Eastern Cooperative Oncology Group. Am. J. Med. 1980;69:491–497. doi: 10.1016/S0149-2918(05)80001-3. [DOI] [PubMed] [Google Scholar]
- 6.Martin L., Senesse P., Gioulbasanis I., Antoun S., Bozzetti F., Deans C., Strasser F., Thoresen L., Jagoe R.T., Chasen M., et al. Diagnostic criteria for the classification of cancer-associated weight loss. J. Clin. Oncol. 2015;33:90–99. doi: 10.1200/JCO.2014.56.1894. [DOI] [PubMed] [Google Scholar]
- 7.Wong H.C.Y., Lam K.Y., Chong C.C.N., Chan A.W.H., Chan S.L. Impact of weight loss during chemotherapy in Chinese patients with unresectable pancreatic cancer. Nutr. Cancer. 2019;71:954–970. doi: 10.1080/01635581.2019.1595047. [DOI] [PubMed] [Google Scholar]
- 8.Takayoshi K., Uchino K., Nakano M., Ikejiri K., Baba E. Weight loss during initial chemotherapy predicts survival in patients with advanced gastric cancer. Nutr. Cancer. 2017;69:408–415. doi: 10.1080/01635581.2017.1267774. [DOI] [PubMed] [Google Scholar]
- 9.Thompson K.L., Elliott L., Fuchs-Tarlovsky V., Levin R.M., Voss A.C., Piemonte T. Oncology evidence-based nutrition practice guideline for adults. J. Acad. Nutr. Diet. 2017;117:297–310. doi: 10.1016/j.jand.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 10.Trujillo E.B., Dixon S.W., Claghorn K., Levin R.M., Mills J.B., Spees C.K. Closing the gap in nutrition care at outpatient cancer centers: Ongoing initiatives of the Oncology Nutrition Dietetic Practice Group. J. Acad. Nutr. Diet. 2018;118:749–760. doi: 10.1016/j.jand.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 11.Arends J., Bachmann P., Baracos V., Barthelemy N., Bertz H., Bozzetti F., Fearon K., Hutterer E., Isenring E., Kaasa S., et al. ESPEN guidelines on nutrition in cancer patients. Clin. Nutr. Edinb. Scotl. 2017;36:11–48. doi: 10.1016/j.clnu.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 12.Trujillo E.B., Claghorn K., Dixon S.W., Hill E.B., Braun A., Lipinski E., Platek M.E., Vergo M.T., Spees C. Inadequate nutrition coverage in outpatient cancer centers: Results of a national survey. J. Oncol. 2019;2019:7462940. doi: 10.1155/2019/7462940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Medicare & Medicaid Services Oncology Care Model. [(accessed on 1 June 2020)]; Available online: https://innovation.cms.gov/innovation-models/oncology-care.
- 14.McCauley S.M., Barrocas A., Malone A. Hospital nutrition care betters patient clinical outcomes and reduces costs: The Malnutrition Quality Improvement Initiative story. J. Acad. Nutr. Diet. 2019;119:S11–S14. doi: 10.1016/j.jand.2019.05.027. [DOI] [PubMed] [Google Scholar]
- 15.Agency for Healthcare Research and Quality Practice Facilitation Handbook, Module Approaches to Quality Improvement. [(accessed on 1 June 2020)]; Available online: https://www.ahrq.gov/ncepcr/tools/pf-handbook/mod4.html.
- 16.Langley G., Nolan T., Provost L., Norman C., Moen R., Nolan K. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. Jossey-Bass; San Francisco, CA, USA: 1996. [Google Scholar]
- 17.Deming W.E. The New Economics for Industry, Government, Education. Massachusetts Institute of Technology; Cambridge, MA, USA: 1994. [Google Scholar]
- 18.Malnutrition Quality Improvement Initiative (MQii) [(accessed on 1 June 2020)]; Available online: http://malnutritionquality.org/
- 19.Electronic Clinical Quality Measures (eCQMs) [(accessed on 1 June 2020)]; Available online: https://www.eatrightpro.org/practice/quality-management/quality-improvement/malnutrition-quality-improvement-initiative.
- 20.McCauley S.M., Mitchell K., Heap A. The Malnutrition Quality Improvement Initiative: A multiyear partnership transforms care. J. Acad. Nutr. Diet. 2019;119:S18–S24. doi: 10.1016/j.jand.2019.05.025. [DOI] [PubMed] [Google Scholar]
- 21.Zhao X.H., Yang T., Ma X.D., Qi Y.X., Lin Y.Y., Chen X.Z., Duan Y.Q., Sun D.L. Heterogeneity of nutrition care procedures in nutrition guidelines for cancer patients. Clin. Nutr. 2020;39:1692–1704. doi: 10.1016/j.clnu.2019.08.022. [DOI] [PubMed] [Google Scholar]
- 22.Evidence-Based Practice Guidelines for the Nutritional Management of Adult Patients with Head and Neck Cancer Clinical Guidelines Wiki. [(accessed on 1 June 2020)]; Available online: https://wiki.cancer.org.au/australia/COSA:Head_and_neck_cancer_nutrition_guidelines.
- 23.August D.A., Huhmann M.B., American Society for Parenteral and Enteral Nutrition (ASPEN) Board of Directors ASPEN. clinical guidelines: Nutrition support therapy during adult anticancer treatment and in hematopoietic cell transplantation. J. Parenter. Enteral Nutr. 2009;33:472–500. doi: 10.1177/0148607109341804. [DOI] [PubMed] [Google Scholar]
- 24.Macris P.C., Schilling K., Palko R. Academy of Nutrition and Dietetics: Revised 2017 standards of practice and standards of professional performance for registered dietitian nutritionists (competent, proficient, and expert) in oncology nutrition. J. Acad. Nutr. Diet. 2018;118:736–748. doi: 10.1016/j.jand.2018.01.012. [DOI] [PubMed] [Google Scholar]
- 25.Huhmann M.B., August D.A. Review of American Society for Parenteral and Enteral Nutrition (ASPEN) Clinical Guidelines for Nutrition Support in Cancer Patients: Nutrition screening and assessment. Nutr. Clin. Pract. 2008;23:182–188. doi: 10.1177/0884533608314530. [DOI] [PubMed] [Google Scholar]
- 26.Huhmann M.B., August D.A. Nutrition support in surgical oncology. Nutr. Clin. Pract. 2009;24:520–526. doi: 10.1177/0884533609335375. [DOI] [PubMed] [Google Scholar]
- 27.Optimal Resources for Cancer Care. [(accessed on 14 July 2020)]; Available online: https://www.facs.org/-/media/files/quality-programs/cancer/coc/optimal_resources_for_cancer_care_2020_standards.ashx.
- 28.Nelson G., Bakkum-Gamez J., Kalogera E., Glaser G., Altman A., Meyer L.A., Taylor J.S., Iniesta M., Lasala J., Mena G., et al. Guidelines for perioperative care in gynecologic/oncology: Enhanced Recovery After Surgery (ERAS®) Society recommendations—2019 update. Int. J. Gynecol. Cancer. 2019;29:651–668. doi: 10.1136/ijgc-2019-000356. [DOI] [PubMed] [Google Scholar]
- 29.Dort J.C., Farwell D.G., Findlay M., Huber G.F., Kerr P., Shea-Budgell M.A., Simon C., Uppington J., Zygun D., Ljungqvist O., et al. Optimal perioperative care in major head and neck cancer with free flap reconstruction: A consensus review and recommendations form the Enhanced Recovery After Surgery Society. JAMA Otolaryngol. Head Neck Surg. 2017;143:292–303. doi: 10.1001/jamaoto.2016.2981. [DOI] [PubMed] [Google Scholar]
- 30.Yannick C., Valerio M., Persson B., Jichlinski P., Ljungqvist O., Hubner M., Kassouf W., Muller S., Galdini G., Carli F., et al. Guidelines for perioperative care after radical cystectomy for bladder cancer: Enhanced Recovery After Surgery (ERAS®) society recommendations. Clin. Nutr. 2013;32:879–887. doi: 10.1016/j.clnu.2013.09.014. [DOI] [PubMed] [Google Scholar]
- 31.Nutrition in Cancer Care PDQ®. [(accessed on 14 July 2020)]; Available online: https://www.cancer.gov/about-cancer/treatment/side-effects/appetite-loss/nutrition-hp-pdq#_AboutThis_1.
- 32.National Comprehensive Cancer Network (NCCN) Guidelines. [(accessed on 1 June 2020)]; Available online: https://www.nccn.org/professionals/physician_gls/default.aspx.
- 33.Guidelines, Tools & Resources. [(accessed on 1 June 2020)]; Available online: https://www.asco.org/research-guidelines/quality-guidelines/guidelines.
- 34.QOPI® 2020 Reporting Tracks. [(accessed on 14 July 2020)]; Available online: https://practice.asco.org/sites/default/files/drupalfiles/QOPI-2020-Round-2-Reporting-Tracks-Public-Posting.pdf.
- 35.CoC Quality of Care Measures. [(accessed on 14 July 2020)]; Available online: https://www.facs.org/quality-programs/cancer/ncdb/qualitymeasurescocweb.
- 36.Cancer Measures. [(accessed on 14 July 2020)]; Available online: http://www.qualityforum.org/Projects/c-d/Cancer/Cancer.aspx.
- 37.Quality Resources and Improvement Activities. [(accessed on 14 July 2020)]; Available online: https://www.ons.org/make-difference/quality-improvement/quality-improvement-registry.
- 38.Quality Programs. [(accessed on 14 July 2020)]; Available online: https://practice.asco.org/quality-improvement/quality-programs.
- 39.National Cancer Database. [(accessed on 14 July 2020)]; Available online: https://www.facs.org/quality-programs/cancer/ncdb.
- 40.Brown T.J., Wolfe H.R., Hardy S., Bhulani N., Hong C., Khosama L., Cheedella N., Hobbs S., Froehlich T.W., Kamal A., et al. Development of a nutrition-focused quality improvement program for new patients with cancer seen at the UTSW Simmons Comprehensive Cancer Center (SCCC) outpatient gastrointestinal (GI) oncology clinic. J. Clin. Oncol. 2018;36:143. doi: 10.1200/JCO.2018.36.30_suppl.143. [DOI] [Google Scholar]
- 41.Levonyak N., Hodges M.P., Broome N., Beg M.S., Kainthla R., Sanjeevaiah A., Sadeghi N., Pandey N., Mhoon V., Cox J.V., et al. A nutrition-focused quality improvement program to improve rate of documented nutrition plan at a safety-net hospital gastrointestinal (GI) oncology clinic. J. Clin. Oncol. 2019;37:289. doi: 10.1200/JCO.2019.37.27_suppl.289. [DOI] [Google Scholar]
- 42.Kiss N., Gilliand S., Quinn P., Atkins L., Black J., Frowen J. Evaluating the effectiveness of a nutrition assistant role in a head and neck cancer clinic. Nutr. Diet. 2019;76:21–27. doi: 10.1111/1747-0080.12462. [DOI] [PubMed] [Google Scholar]
- 43.Pranoy S., Reynolds M., Lim S. Evaluation of nutritional deficiencies in a new gastroenterology-led South Wales neuroendocrine tumour (NET) service. Neuroendocrinology. 2019;108:S87. [Google Scholar]
- 44.Jacquelin-Ravel N., Pugliesi-Rinaldi A., Joly C., Ho S., Mareschal J., Dietrich P.Y., Dulguerov P., Miralbell R., Pichard C. Onconut: Nutritional care optimization for cancer patients. Clin. Nutr. 2014;33:S4. doi: 10.1016/S0261-5614(14)50009-X. [DOI] [Google Scholar]
- 45.Hill A., Kiss N. Evaluation of an evidence-based nutrition care pathway for lung cancer patients undergoing radiotherapy. J. Thorac. Oncol. 2012;7:S172. [Google Scholar]
- 46.Loeliger J., Hodgson B. Nutrition assistants and malnutrition in a cancer setting: Exploring an integrated model of care. Asia Pac. J. Clin. Oncol. 2010;3:S137. [Google Scholar]
- 47.Tappenden K.A., Quatrara B., Parkhurst M.L., Malone A.M., Fanjiang G., Ziegler T.R. Critical role of nutrition in improving quality of care: An interdisciplinary call to action to address adult hospital malnutrition. JPEN J. Parenter. Enteral Nutr. 2013;37:482–497. doi: 10.1177/0148607113484066. [DOI] [PubMed] [Google Scholar]
- 48.Pedrazzoli P., Caccialanza R., Cotogni P., Esposti L.D., Perrone V., Sangiorgi D., DiCostanzo F., Gavazzi C., Santoro A., Pinto C. The advantages of clinical nutrition use in oncologic patients in Italy: Real world insights. Healthcare. 2020;8:125. doi: 10.3390/healthcare8020125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ravasco P. Nutrition in cancer patients. J. Clin. Med. 2019;8:1211. doi: 10.3390/jcm8081211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pratt K.J., Hernandez B., Blancato R., Blankenship J., Mitchell K. Impact of an interdisciplinary malnutrition quality improvement project at a large metropolitan hospital. BMJ Open Qual. 2020;9:e000735. doi: 10.1136/bmjoq-2019-000735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Taurchini M., Del Naja C., Tancredi A. Enhanced Recovery After Surgery: A patient centered process. J. Vis. Surg. 2018;4:1–4. doi: 10.21037/jovs.2018.01.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Boitano T.K.L., Smith H.J., Rushton T., Johnston M.C., Lawson P., Leath C.A., Xhaja A., Guthrie M.P., Straughn J.M. Impact of Enhanced Recovery After Surgery (ERAS®) protocol on gastrointestinal function in gynecologic oncology patients undergoing laparotomy. Gynecol. Oncol. 2018;151:282–286. doi: 10.1016/j.ygyno.2018.09.009. [DOI] [PubMed] [Google Scholar]
- 53.Bisch S.P., Wells T., Garmlich L., Faris P., Wang X., Tran D.T., Thanh N.X., Glaze S., Chu P., Ghatage P., et al. Enhanced Recovery After Surgery (ERAS®) in gynecologic oncology: System-wide implementation and audit leads to improved value and patient outcomes. Gynecol. Oncol. 2018;141:117–123. doi: 10.1016/j.ygyno.2018.08.007. [DOI] [PubMed] [Google Scholar]
- 54.Pisarska M., Torbicz G., Gajewska N., Rubinkiewicz M., Wierdak M., Major P., Budzynski A., Ljungqvist O., Pedziwiatr M. Compliance with ERAS® protocol and 3-year survival after laparoscopic surgery for non-metastatic colorectal cancer. World J. Surg. 2019;43:2552–2560. doi: 10.1007/s00268-019-05073-0. [DOI] [PubMed] [Google Scholar]
- 55.Include MNT into Care Design and Payment for Future Oncology Model. [(accessed on 1 June 2020)]; Available online: https://www.eatrightpro.org/news-center/on-the-pulse-of-public-policy/regulatory-comments/include-mnt-into-care-design-and-payment-for-future-oncology-model.
- 56.Food and Nutrition Board. Health and Medicine Division. National Academies of Sciences, Engineering, and Medicine . Examining Access to Nutrition Care in Outpatient Cancer Centers: Proceedings of a Workshop. National Academies Press; Washington, DC, USA: 2016. [(accessed on 1 June 2020)]. Available online: https://www.ncbi.nlm.nih.gov/books/NBK379326/ [PubMed] [Google Scholar]
- 57.Adams K.M., Kohlmeier M., Powell M., Zeisel S.H. Nutrition in medicine: Nutrition education for medical students and residents. Nutr. Clin. Pract. 2010;25:471–480. doi: 10.1177/0884533610379606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Crowley J., Ball L., Hiddink G.J. Nutrition in medical education: A systematic review. Lancet Planet. Health. 2019;3:e379. doi: 10.1016/S2542-5196(19)30171-8. [DOI] [PubMed] [Google Scholar]
- 59.The Malnutrition Quality Collaborative . National Blueprint: Achieving Quality Malnutrition Care for Older Adults. Avalere Health and Defeat Malnutrition Today; Washington, DC, USA: 2020. [(accessed on 14 July 2020)]. Available online: https://www.defeatmalnutrition.today/sites/default/files/National_Blueprint_MAY2020_Update_OnlinePDF_FINAL.pdf. [Google Scholar]
- 60.Muscaritoli M., Arends J., Aapro M. From guidelines to clinical practice: A roadmap for oncologists for nutrition therapy for cancer patients. Ther. Adv. Med. Oncol. 2019;11 doi: 10.1177/1758835919880084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rauh S., Antonuzzo A., Bossi P., Eckert R., Fallon M., Frobe A., Gonella S., Giusti R., Lakatos G., Santini D., et al. Nutrition in patients with cancer: A new area for medical oncologists? A practising oncologist’s interdisciplinary position paper. ESMO Open. 2018;3:e000345. doi: 10.1136/esmoopen-2018-000345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.eCQMs Frequently Asked Questions. [(accessed on 1 June 2020)]; Available online: https://www.eatrightpro.org/practice/quality-management/quality-improvement/ecqms-frequently-asked-questions.
- 63.Mullin G.E., Fan L., Sulo S., Partridge J. The association between oral nutrition supplements and 30-day hospital readmissions of malnourished patients at a US academic medical center. J. Acad. Nutr. Diet. 2019;119:1168–1174. doi: 10.1016/j.jand.2019.01.014. [DOI] [PubMed] [Google Scholar]
- 64.Arensberg M.B., Sulo S., Drawert S. United States value-based payment programs provide framework for developing nutrition-focused quality improvement programs (QIPs) to address malnutrition in outpatient cancer care. J. Clin. Nutr. Food Sci. 2020 accepted. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.