Abstract
Background
Breast cancer still is a topic. This overview of the literature aimed to update the current knowledge on quality of life in breast cancer patients.
Methods
A review of literature in MEDLINE, Cochrane Database of Systematic Reviews and Google Scholar were carried out to identify review papers on health-related quality of life in breast cancer during the 2008 to 2018. All publications were screened using the PRISMA guideline. The methodological quality of reviews was assessed using the AMSTAR. The findings were summarized and tabulated accordingly.
Results
Within over a decade, a total of 974 review papers were identified which according to the study selection criteria finally we have evaluated 82 reviews. Of these about 85% had a reasonable methodological quality. The findings were mainly summarized on several headings including instruments used to measure quality of life, treatment, supportive care, psychological distress, and symptoms. Questionnaires had a good performance to quantify quality of life in breast cancer patients. Most reviews were focused on the impact of treatment including endocrine therapy as well as integrating complementary and alternative medicine into the current practice. According to the reviews, yoga was the most recommended exercise to improve quality of life in breast cancer patients.
Conclusion
Overall, the findings from this overview indicated that quality of life in breast cancer patients enhanced during the last decade. Several simple but effective interventions such as physical activity and psychosocial interventions proved to be effective in improving quality of life in this population. However, management of symptoms such as pain, and lymphedema, issues related to worry, sexual function especially for young patients, and the future outlooks all are among topics that deserve further consideration. Also, this overview indicated that methodological issues in measuring quality of life in breast cancer patients improved greatly, but still there is a long way to go to understand what really matter to patients.
Keywords: Overview, Breast cancer, Quality of life, Review of reviews, Patient-reported outcome
Background
Breast cancer remains the most common cancer among women worldwide [1]. According to 2018 GLOBOCAN, approximately 2.1 million cases worldwide were diagnosed with breast cancer and about 630,000 died from the disease [2]. Due to the increasing in breast cancer incidence, advances in the treatment of the disease have been achieved. Local modalities and systemic anticancer therapies, therefore, lead to improve patients’ survival outcomes including disease-free survival and overall survival [3]. However, since the disease diagnosis and treatment have improved greatly over time, at present in addition to survival, quality of life has become an important outcome measure in breast cancer clinical investigations and survivorship studies [4, 5]. Hopefully, at present a compile of evidence exist on the topic and sometimes even it is very difficult to adhere to evidence in practice since conflicting findings are reported. Thus, to evaluate and summarize the existing evidence on quality of life in breast cancer patients a review of reviews was conducted.
Previously we have summarized all reviews on breast cancer patients’ quality of life that covered the literature from publication of the first review up to year 2008 [6]. The lists of those reviews are supplemented (see Additional file 1). Now we are updating the review by focusing on review papers which appeared in biomedical journals since then. Systematic review of reviews will allow the creation of a summary of reviews in a single document in order to enhance evidence-based knowledge and support well-informed clinical decision-making [7]. The present review of reviews aimed to address the primary question of whether the quality of life has been improved over the last decade and what factors have played the key role in patients’ quality of life. In fact, the goal of this review of reviews was to identify the impact of breast cancer and its treatment on quality of life and to determine ways to improve quality of life in breast cancer patients.
Methods
Definition
Quality of life or specifically health-related quality of life was defined as breast cancer patients’ perception of their own physical, mental and social health that influenced by diagnosis, treatment, post-treatment, and survivorship as assessed by using well validated instruments.
Search engines and time period
Studies identified through the available literature in MEDLINE (PubMed), and Goggle scholar to identify review papers on health-related quality of life in breast cancer. Also, an extra search was performed to check reviews indexed in the Cochrane Database of Systematic Reviews (CDSR). Current study covers all full review publications that appeared in English language biomedical journals between January 2008 and 31 December 2018.
Search strategy
This study used comprehensive evidence map of overview of systematic reviews introduced by Lunny et al. [8]. All databases were searched using the combination of keywords ‘quality of life’ and ‘breast cancer’ or ‘breast carcinoma’ in the titles of publications and limited to review articles. This provided the initial database for the review. Initial search was carried out in late January 2017, twice on March, and August 2017 and once for a final update on February 2019. A manual search also was performed for possible additional references. Key words and search strategy were as follows: (breast cancer [Title/Abstract]] AND quality of life [Title/Abstract] Filters: Review; Publication date from 2008/01/01 to 2018/12/31; English).
Selection criteria
Eligibility criteria for inclusion were: all review papers that published in English language, and reviewed quality of life as a main outcome in breast cancer patients. All other papers were excluded. All publications were screened using the PRISMA guideline. The AMSTAR checklist is used to assess the quality of reviews [9].
Data synthesis
Data obtained from each single review were synthesized by providing descriptive tables reporting authors’ names, publication year, type of review, number of databases and studies included, analysis, and whether performed quality appraisal and risk of bias assessments. The findings were presented chronologically.
Results
Statistics
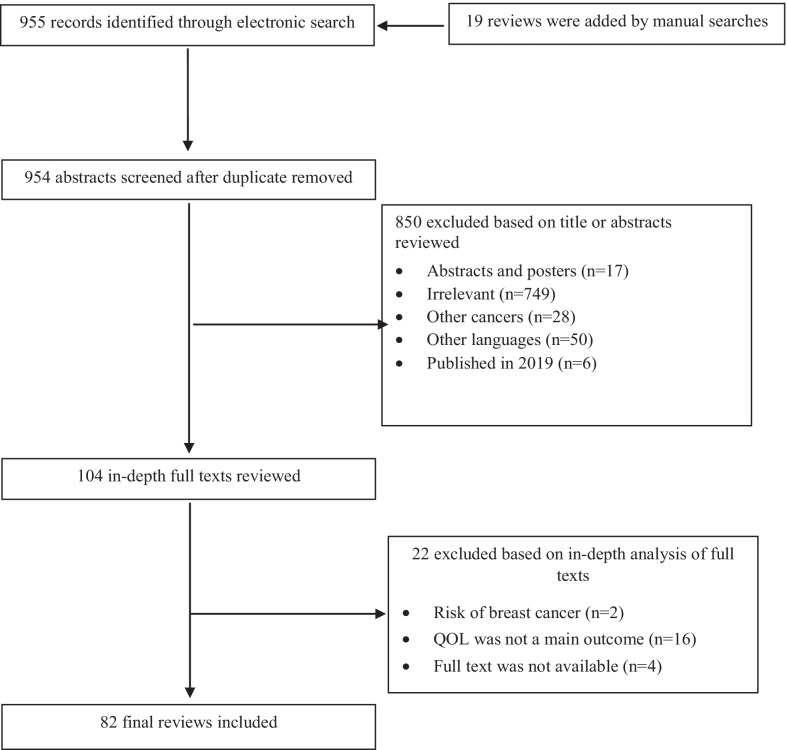
A total of 955 unique review articles were identified. In addition, 19 citations were found via manual search (n = 974). After removing duplicates, commentaries and brief communications, 104 reviews seemed relevant for further evaluation. Finally, of these 81 quantitative and one qualitative review were found eligible and included in the study. The study flowchart is shown in Fig. 1. According to the AMSTAR checklist, approximately 85% of the publications had value of 4 or more for methodological quality (Fig. 2).
Fig. 1.
The study flowchart
Fig. 2.
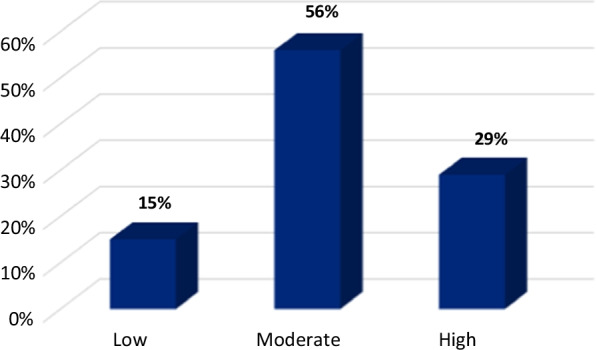
Quality scoring according to the AMSTAR checklist
Overall outlook of reviews
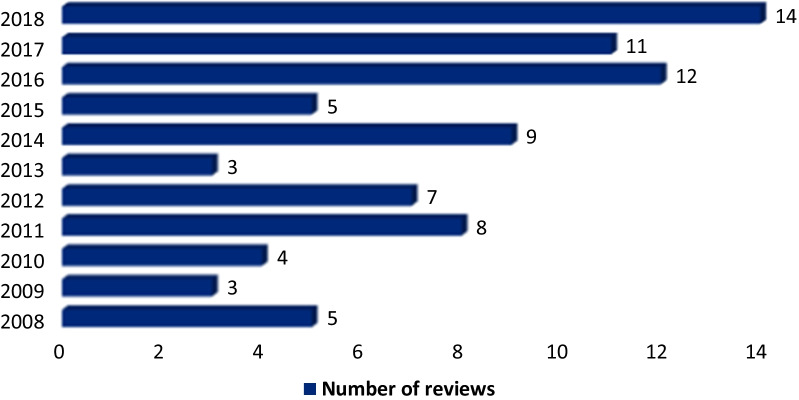
In general, although not having the same quality, currently reviews, systematic reviews and meta-analyses regarding QOL in breast cancer patients are increasing (Fig. 3). However, to summarize evidence, reviews were categorized into the following main topics: reviews on measurements and methodological issue, reviews that dealt with different treatments, and those reviews that touched other topics such as supportive care, physiological distress, age-related reviews, quality of life in different nations/races and qualitative reviews. These are presented in the following sections.
Fig. 3.
Frequency of reviews on quality of life in breast cancer patients during 2008–2018
Quality of life measurement
Instruments used
There were 17 papers that reviewed literature on instruments to quantify quality of life in breast cancer patients [10–26]. In general, there were three types of instruments: generic, specific, and measures assessing psychological issues or breast cancer related symptoms. Among generic measures the Short Form Health survey (SF-36) and the brief version of World Health Organization Quality of Life Questionnaire (WHOQOL-BREF) had a good performance [20]. Also, the European Organization for Research and Treatment of Cancer quality of life core cancer (EORTC QOL-C30) questionnaire and the Functional Assessment of Cancer Therapy/Functional Assessment of Chronic Illness Therapy (FACIT) were the most commonly used questionnaires [12, 13]. Reviews also found that specific measures including the Functional Assessment of Cancer Therapy-Breast quality-of-life (FACT-B) and the European Organization for Research and Treatment of Cancer quality of life core breast cancer (EORTC QLQ-BR23) were the frequently used specific QOL instruments in breast cancer patients [13, 18–20]. The FACT-ES and the Hot Flash Related Daily Interference Scale (HFRDIS) had good applicability for patients who receive hormonal treatment and who have hot flashes [17]. A systematic review of QOL instruments in long-term BCS indicated that the Quality of Life in Adult Cancer Survivors Scale has acceptable reliability, validity, and responsiveness [14]. The findings are summarized in Table 1.
-
(2)
The challenges exist
Table 1.
A list of reviews on measurement issue and quality of life in breast cancer patients (2008–2018)
| Authors [References] | Year | Main focus | Description/analysis | No. of databases | No. of included studies | Performed QA | Risk of bias assessment | Result(s) |
|---|---|---|---|---|---|---|---|---|
| Chen et al. [10] | 2010 | Patient-reported outcome measures for oncologic breast surgery | Systematic review | 8 | NA | No | No | Reliable and valid instruments exist, but even the best instruments do not address all important surgery‐specific and psychometric issues |
| Winters et al. [11] | 2010 | Treatment recommendations in breast reconstruction based on patient-reported outcome measures and HRQOL | Systematic review | 4 | 34 | Yes | No |
Sound scientific methodology in HRQOL is undermined by poorly designed and underpowered studies There is a pressing need for further longitudinal studies in breast reconstruction incorporating sensitive and condition-specific patient-report outcome measures; provide adequate sample sizes, and respect established guidelines for rigorous HRQOL methodology |
| Lemieux et al. [12] | 2011 | QOL measurement in RCTs | An updated systematic review | PubMed | 190 | No | No | Reporting of QOL methodology should improve |
| Reed et al. [13] | 2012 | QOL assessments in advanced breast cancer | Review | PubMed | 51 | No | No | There should be more consensuses on which QOL instruments are used |
| Chopra and Kamal [14] | 2012 | QOL instruments in long-term BCS | Systematic review | 5 | 19 | No | No | The use of validated instruments will not only provide valid data but also help improve the quality of care in long-term BCS |
| Adamowicz et al. [15] | 2012 | Assessment of HRQOL parameters as end points in phase III trials in advanced BC | Review | NA | 34 | No | No | HRQOL evaluation in clinical trials has the potential to predict patient prognosis and serves as a useful tool to assess patients’ experience during cancer therapy |
| Pusic et al. [16] | 2013 | Patient-reported outcome instruments and outcomes in breast cancer patients with lymphedema | Systematic review | NA | 39 | Yes | No | The Upper Limb Lymphedema 27 (ULL-27) was found to have strong psychometric properties. Future studies should strive to use high-quality condition- specific PRO instruments, follow existing guidelines for HRQOL measurement |
| Niu HY et al. [17] | 2014 | Validity, reliability and responsiveness of breast cancer-specific HRQL instruments | Review | 3 | 4 | Yes | No | The EORTC QLQ-BR23, FACT-B, FACT-ES, and HFRDIS had fairly good psychometric properties to assess HRQOL |
| Nguyen et al. [18] | 2015 | Effectiveness of EORTC QLQ-BR23 and FACT-B | Review | 3 | NA | No | No | Both questionnaires were effective in assessing QOL. Decision-making between the questionnaires depends on the study’s purpose and design |
| Oliveira et al. [19] | 2015 | The procedures of translation, cross-cultural adaptation, and measurement properties of breast cancer-specific QOL questionnaires | Systematic review | 4 | 24 | Yes | No | Caution should be exercised when using breast cancer-specific QOL questionnaires that have been translated, adapted, and tested |
| Maratia et al. [20] | 2016 | Evaluation of available specific and generic breast cancer HRQOL instruments | Systematic review | 2 | 32 | Yes | No | The EORTC BR-23, IBCSG, SF-36, and WHO-QOL BREF had good performance, depending on the purpose of the study |
| Ghislain et al. [21] | 2016 | HRQOL in locally advanced and metastatic breast cancer: reporting of methodological and clinical issues in RCTs | Systematic review | PubMed | 49 | Yes | No | The absence of the HRQOL research hypotheses and the overemphasis on statistical rather than clinical significance was the main problem |
| Turner-Bowker et al. [22] | 2016 | Patient-reported outcomes in advanced breast cancer clinical trials | Systematic review | 3 | 25 | No | No | Patient-reported outcomes may be used to provide a more comprehensive perspective of the benefits and risks from treatment |
| Krohe et a l [23] | 2016 | PRO in metastatic breast cancer: a review of industry-sponsored clinical trials | Review | Clinicaltrial.gov | 38 | No | No | Stakeholders turn more attention to the patient perspective; one would expect PROs to increase as complementary measures to traditional endpoints and become an even more critical part of treatment evaluation |
| Pe et al. [24] | 2018 | Patient-reported outcome data in randomized controlled trials of locally advanced and metastatic breast cancer | Review | PubMed | 66 | No | No | A need to improve standards in the analysis, interpretation, and reporting of Patient-reported outcome and quality of life data in cancer RCTs |
| Liu et al. [25] | 2018 | BREAST-Q measurement of the patient perspective in oncoplastic breast surgery | Systematic review | 4 | 54 | Yes | No | BREAST-Q can effectively measure patient's satisfaction and HRQOL in relation to different type of breast oncoplastic surgeries. BREAST-Q captured meaningful and reliable information from the patients' perspective and may be useful for clinical decision-making |
| Tevis et al. [26] | 2018 | Patient-reported outcomes for breast cancer | Review | Not specified | 123 | No | No | The implementation of PROs can be complex and challenging and care must be taken to minimize the potential for survey fatigue by patients and the potential financial burden for implementation, maintenance, and analyses of collected data |
QA quality appraisal, NA not available, QOL quality of life, HRQO health-related quality of life, PRO patient-reported outcomes, RCTs randomized clinical trials, EORTC QLQ-C30 the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core, FACT-B The Functional Assessment of Cancer Therapy-Breast quality-of-life, EORTC QLQ-BR23 the European Organization for Research and Treatment of Cancer quality of life core breast cancer, HFRDIS Hot Flash Related Daily Interference Scale, IBCSG the International Breast Cancer Study Group, SF-36 The 36-Item Short Form Health Survey, WHO-QOL BREF World Health Organization Quality of Life Instruments, FACT-ES Functional Assessment of Cancer Therapy-Endocrine Subscale, BREAST-Q patient-reported outcome measure for breast surgery
Three papers critically reviewed the literature and pointed out that some shortcomings exist among studies reporting quality of life in breast cancer patients. As such a review on quality of life in breast cancer patients who received breast conservation surgery echoed that instruments do not address all important surgery‐specific and psychometric issues of oncologic breast surgery patients [10]. Similarly, a systematic review conducted to guide treatment recommendations in breast reconstruction based on patient-reported outcomes and HRQOL revealed that sound scientific methodology in HRQOL were undermined by poorly designed and underpowered studies. The review recommends that studies on the topic ‘should incorporate sensitive and condition-specific patient-report outcome measures, provide adequate sample sizes, and respect established guidelines for rigorous HRQOL methodology’ [11].
Recently a review including 49 RCTs in locally advanced and metastatic setting concluded that the absence of QOL research hypotheses and overemphasis on statistical than clinical significance is still problematic in measuring quality of life in breast cancer patients. The authors pointed out that ‘although most of the experts’ recommendations have been broadly followed by the research community during the past decade, the specification of the HRQOL research hypothesis is still under-reported’ [21].
Treatment
A summary of reviews that focused on different treatment modalities and quality of life are presented in Table 2 [27–54].
Systemic therapy
Table 2.
A list of reviews covering local, systemic treatments and side-effects and quality of life in breast cancer patients (2008–2018)
| Authors [References] | Year | Main focus | Description/analysis | No. of databases | No. of included studies | Performed QA | Risk of bias assessment | Result(s) |
|---|---|---|---|---|---|---|---|---|
| Lemieux et al. [27] | 2008 | Effects of Chemotherapy-induced alopecia on QOL | Review | 5 | 38 | No | No | Hair loss consistently ranked amongst the most troublesome side effects, was described as distressing, and may affect the body image |
| Cella and Fallowfiel [28] | 2008 | Side-effects of endocrine therapy and QOL | Review | NA | 6 | No | No | Starting with better QOL, which should lead to better adherence, will result in better patient outcomes |
| Buijs et al. [29] | 2008 | Endocrine treatments for breast cancer and HRQOL | Review | NA | NA | No | No | HRQOL mostly is severely influenced by chemotherapy and part of these symptoms may be lasting, especially when associated with the induction of premature menopause. The varying side effect profiles of tamoxifen and aromatase inhibitors did not lead to significant difference in overall HRQOL |
| Pockaj et al. [30] | 2009 | QOL after breast surgery | Review | NA | NA | No | No | Better preoperative counseling, informed decision-making, and appropriate interventions will lead to improved QOL |
| Reimer and Gerber [31] | 2010 | Impact of local or systemic treatments on QOL in the elderly early-breast cancer patients | Review | PubMed | 18 | No | No | Overall QOL was maintained or improved |
| Devi et al. [32] | 2011 | QOL of women during and up to ten years after treatment for breast cancer | Systematic review | 9 | 11 qualitative studies | Yes | No | Breast cancer diagnosis and its treatment can have a significant effect on several domains of women’s QOL |
| Pinto and de Azambuja [33] | 2011 | Symptoms in BCS | Review | NA | NA | No | No | The most common symptoms affecting BCS were fatigue, insomnia, depression, cognitive dysfunction, reproductive and menopausal symptoms and lymphedema |
| Howard-Anderson et al. [34] | 2012 | QOL, menopausal symptoms and fertility concerns, and behavioral health outcomes in younger patients | Systematic review | PubMed | 28 | No | No | Younger women experienced concerns on premature menopause, menopausal symptoms and infertility that had a role in the level of distress after treatment. Health outcomes in younger ones include weight gain and physical inactivity |
| Kaviani et al. [35] | 2013 | Type of surgery and QOL | Narrative review | NA | NA | No | No | QOL had a better score for oncoplastic breast surgery in comparison with mastectomy or BCT |
| Orsaria et al. [36] | 2014 | Nodal status assessment and QOL | Review | NA | NA | No | No | Quality results in breast cancer surgery need to generate oncological safety devoid of complications through renewed clinical experience |
| Tsoi et al. [37] | 2014 | Tissue-expander/implant vs. autologous abdominal tissue breast reconstruction | Systematic review | 5 | 15 | Yes | Yes | There is some weak evidence that tissue-expander/implant reconstruction becomes a less favorable approach in terms of patient satisfaction after mastectomy |
| Taghian et al. [38] | 2014 | Impact of lymphedema on QOL | Review | PubMed | NA | No | No | Lymphedema remains a significant QOL issue which affected woman’s physical, psychological, and emotional well-being |
| Sodergren et al. [39] | 2015 | The side effects associated with targeted therapies used in the adjuvant and metastatic settings for HER2+ | Systematic review | 5 | 18 | No | No | Compared with conventional cytotoxics, targeted therapies are delivered over longer periods of time and present unique and often extensive side-effect profiles. Diarrhoea and skin rash as particularly prevalent anti-HER2 inhibitor side effects |
| Kameo and Sawada [40] | 2016 | QOL and adverse reactions of chemotherapy | Integrative review | 5 | 50 | NA | NA | Multidisciplinary and thinking on the individual vulnerabilities should be considered when evaluating adverse reaction and QOL |
| Mioranza et al. [41] | 2016 | The impact of adjuvant endocrine therapy in early breast cancer on QOL | Review | NA | NA | No | No | Impact of adjuvant endocrine therapies on HRQOL was not comparable since they used different QOL instruments |
| Razdan et al. [42] | 2016 | Quality of life among patients after bilateral prophylactic mastectomy | Systematic review | 6 | 22 | Yes | No | Post-BPM, patients are satisfied with the outcomes and report high psychosocial well-being and positive body image. Sexual well-being and somatosensory function are most negatively affected. Vulnerability, psychological distress and preoperative cancer distress are significant negative predictors of quality of life and body image post-BPM |
| Chalasani [43] | 2017 | Optimizing QOL in patients with hormone receptor-positive metastatic breast cancer | Review | NA | NA | No | No | Patients with HR-positive disease may receive maximum clinical benefit from endocrine therapy while optimizing QOL |
| Garrido-Oyarzun and Castelo-Branco [44] | 2017 | Use of hormone therapy for menopausal symptoms and QOL in survivors | Review | NA | NA | No | No | The management of menopausal symptoms and QOL of patients treated for breast cancer remains an important problem without an optimal solution |
| Marta et al. [45] | 2017 | QOL in patients treated with radiation therapy | Systematic review | PubMed | 353 | No | No | Significant benefit in HRQOL was often reported when a positive primary outcome was reported |
| Zhou et al. [46] | 2017 | Impact of endocrine monotherapy and in combination with targeted therapy on QOL | Systematic review | 3 databases and key conferences | 11 | No | No | Users of both treatments experienced similar QOL in the first-line and ET-failure setting relative to patients on ET mono. Moreover, these users experienced better QOL outcomes in some domains in the ET-failure setting relative to ET mono users |
| Mileski et al. [47] | 2017 | QOL considerations during cancer treatment in invasive ductal carcinoma patients | Systematic review | PubMed | 9 | No | No | The most prevalent positive QOL factors included patient expectations, decreased side effects, and increased survival rate. The most prevalent negative QOL factors included treatment, specific side effects and decreased quality of life |
| Platt and Zhong [48] | 2017 | Patient-centered breast reconstruction based on health-related QOL evidence | Review | NA | NA | No | No | Both immediate and delayed breast reconstruction increased satisfaction and QOL after reconstruction, and both groups have reported similar satisfaction and QOL scores at long-term follow-up |
| Rivera et al. [49] | 2018 | Chemotherapy-associated peripheral neuropathy | Systematic review | 4 | 60 | Yes | No | Neuropathic symptoms persisted in 11.0% to more than 80% of participants at one to three years following treatment. There is a paucity of data describing persistent PN in ESBC patients |
| Xiao et al. [50] | 2018 | Effects of adjuvant endocrine therapy on the QOL of post-menopausal women with non-metastatic ER+ | Systematic review | 3 | 13 | Yes | No | Most studies found no differences between tamoxifen and aromatase inhibitor groups in terms of global QOL. The QOL of post-menopausal women is unlikely to be adversely affected by long-term use of adjuvant endocrine therapy |
| Yee et al. [51] | 2018 | Radiation-induced skin toxicity in breast cancer patients | Systematic review | NA | 96 | Yes | No | Methods including simultaneous integrated boost, accelerated partial breast irradiation, and prone positioning may cause less radiation dermatitis than conventional treatments |
| Cheng et al. [52] | 2018 | QOL of elderly patients with solid tumors undergoing adjuvant cancer therapy | Systematic review | 5 | 4 | Yes | Yes | Adjuvant chemotherapy and radiotherapy may not have detrimental effects on QOL in most elderly patients with solid tumors |
| Muller et al. [53] | 2018 | Impact of manual lymphatic drainage on the HRQOL | Systematic review | 6 | 8 | Yes | Yes | No studies reported reductions in HRQOL, or severe adverse events after MLD |
| Jeffs et al. [54] | 2018 | Effectiveness of decongestive treatments on excess arm volume and patient-centered outcomes in women with early breast cancer-related arm lymphedema | Systematic review | 3 | 7 | Yes | Yes | Weak evidence for the impact of decongestive lymphedema treatment did not allow any conclusions to be drawn about the most effective treatment to be offered when patients with early breast cancer first present for treatment |
QA quality appraisal, NA not available, QOL quality of life, HRQO health-related quality of life, BPM body image post, ET endocrine therapy, BCT breast conserving therapy, HER_2 human epidermal growth factor receptor 2, RCTs randomized clinical trials, BCS breast cancer survivors, MLD impact of manual lymphatic drainage
Seventeen reviews were focused on HRQOL in patients undergoing systemic therapy including chemotherapy, hormonal therapy, and targeted therapy. Of these, the effect of endocrine therapy alone or combined with adjuvant treatments was the center of focus. Hot flashes were the most common side effect of adjuvant endocrine therapies. Side effects of tamoxifen and aromatase inhibitors including vaginal dryness, vaginal discharge, dyspareunia, and arthralgia were often reported in reviews [28]. A review assessing the impact of adjuvant endocrine therapy in early breast cancer on QOL found that in most trials, treatment-related symptoms led to the small drop in different domains of QOL [41].
Despite the current guidelines considering that hormonal therapy is contraindicated in breast cancer survivors, recently a review suggested that in some women, menopausal symptom relief might be more important than the potential risks of hormonal therapy. The review concluded that on the use of hormonal therapy and tibolone in newly diagnosed patients, survivors or suspected to breast cancer will remain contraindicated [44].
-
(2)
Local therapy including surgery and radiotherapy
Six reviews addressed the impact of local therapies on quality of life [30, 35–37, 42, 48]. For example, one review found that there was worse body image, disturbances in sexual life as well as great impairment in advanced breast cancer patients after mastectomy [42]. Patients receiving immediate and delayed breast reconstruction experienced increased satisfaction and QOL after reconstruction, and in long-term follow-up, both groups have reported similar satisfaction and QOL scores [48]. Marta et al. found that HRQOL has been infrequently investigated in RCTs in patients who received radiotherapy. QOL can be an important predictor of better treatment outcomes, as significant benefit in HRQOL was often reported once a positive primary outcome was reported [45].
-
(3)
Side effects of treatments
Five reviews focused on side effects of treatment modalities including topics related to fatigue, insomnia, cognitive dysfunction, reproductive and menopausal symptoms and lymphedema [33, 34, 38, 53, 54]. A review of randomized clinical trials found that these symptoms were the most common symptoms affecting survivors’ quality of life [33]. Lymphedema in early-stage breast cancer patients who undergo axillary lymph-node dissection is an important concern. The results derived from a total of 8 studies have shown that impact of manual lymphatic drainage had a significant impact on HRQOL, but a recent published review failed to find that the impact of decongestive lymphedema treatment, the most effective treatment to be offered, on patients with early lymphedema due to the weak evidence [53, 54].
Supportive care
In the following sections we highlighted a number of topics relevant to supportive care in breast cancer patients [55–72]. The findings are summarized in Table 3.
Physical activity (supportive exercise intervention)
Table 3.
A list of reviews on supportive care including physical activity, complementary and alternative medicine and quality of life (2008–2018)
| Authors [References] | Year | Main focus | Description/analysis | No. of databases | No. of included studies | Performed QA | Risk of bias assessment | Result(s) |
|---|---|---|---|---|---|---|---|---|
| Bicego et al. [55] | 2009 | The effect of exercise on QOL | Systematic review | 4 | 9 | Yes | No | Exercise as an effective strategy can improve QOL in patients |
| Bleakley and Stinson [56] | 2011 | CAM and QOL | Narrative review | 6 | 8 | Yes | No | There is great potential for complementary and alternative therapies to be increasingly integrated into clinical practice within breast cancer services |
| Levine and Balk [57] | 2012 | Yoga and QOL improvement | Literature review | 7 | 71 | NA | NA | Participation in yoga programs appeared to benefit breast cancer patients |
| Zhang, et al. [58] | 2012 | Effects of yoga on psychological function and QOL | Systematic review and meta-analysis | 5 | 6 | Yes | Yes | There is insufficient evidence to advocate that yoga should be offered routinely to women diagnosed with breast cancer. However, it may be an acceptable intervention to improve QOL for these women |
| Boehm et al. [59] | 2014 | Arts therapies for anxiety, depression, and QOL | Systematic review and meta-analysis | 3 | 13 | Yes | Yes | Overall, the option of participation in arts therapies can be recommended and has shown to be significantly effective for the reduction of anxiety in patients |
| Sawyer [60] | 2014 | Complementary exercise and QOL | Systematic review | 4 | 9 | No | No | Although complementary exercise improved QOL statistically in two-thirds of the research findings, further research is recommended |
| Zeng Y et al. [61] | 2014 | Effects of exercise intervention on QOL in BCS | Systematic review and meta-analysis | 5 | 19 | Yes | Yes | Exercise interventions have statistically significant effects on overall QOL, as well as positive trends for breast and arm symptoms |
| Yan et al. [62] | 2014 | Lack of Efficacy of Tai Chi in Improving QOL in BCS | Systematic review and meta-analysis | 4 | 9 | Yes | Yes | There is a lack of sufficient evidence to support Tai Chi benefiting the management of BCS in improving QOL and other important clinical outcomes |
| Leggett et al. [63] | 2015 | Effects of CAM on cancer symptoms, treatment side effects, QOL, and survival | Systematic review | 5 | 22 | Yes | Yes | Guarana and Ganoderma lucidum may improve fatigue, whereas glutamine may also be effective in improving oral mucositis symptoms |
| Van Dijck et al. [64] | 2016 | The effects of different physical self-management techniques on QOL | Systematic review | 4 | 13 | Yes | Yes | Physical self-management interventions during breast cancer treatment as well as after the primary treatment seem to generate beneficial effects on QOL |
| Zhang et al. [65] | 2016 | Effects of mindfulness-based therapy on QOL | Systematic review and meta-analysis | 6 | 7 | Yes | Yes | There was limited that mindfulness-based therapy can improve QOL |
| Cramer et al. [66] | 2017 | Yoga for improving HRQOL, mental health and cancer-related symptoms | Systematic review and meta-analysis | 6 | 23 | Yes | Yes | Moderate-quality evidence supported the recommendation of yoga for improving HRQOL and reducing fatigue and sleep disturbances when compared with no therapy, as well as for reducing depression, anxiety and fatigue, when compared with psychosocial/educational interventions |
| D'Egidio et al. [67] | 2017 | Effect of counseling interventions on HRQOL | Systematic review | 2 | 35 | Yes | No | Exercise counseling as well as physical therapy are effective to improve shoulder mobility, healing wounds, and limb strength |
| Husebo et al. [68] | 2017 | Mind–body exercise therapies and QOL | Review | 4 | 11 | Yes | Yes | Yoga was found to benefit patients’ psychological QOL, while less support was established concerning physical QOL elements |
| Lipsett et al. [69] | 2017 | Exercise during adjuvant radiotherapy on fatigue and QOL | Systematic review and meta-analysis | 6 | 9 | Yes | No | Statistically significant benefits of supervised, combined aerobic resistance exercise on fatigue were achieved |
| Pan et al. [70] | 2017 | Yoga practice improve treatment-related side effects and QOL | Systematic review and meta-analysis | 3 | 16 | Yes | No | Yoga was associated with enhanced overall HRQOL and relief of anxiety, depression and gastrointestinal adverse reactions in breast cancer patients and survivors |
| Zaidi et al. [71] | 2018 | Effect of complementary therapies on survivors’ QOL | Review | NA | NA | No | No | There is a need for personalized physical activity plans to be developed to suit the individual and their circumstances |
| Zhang et al. [72] | 2018 | Effectiveness of telephone- based interventions on HRQOL and prognostic outcomes | Systematic review and meta-analysis | 6 | 14 | Yes | Yes | Based on the insufficient evidence, the effects on depression, fatigue and physiological function were not statistically significant |
QA quality appraisal, NA not available, CAM complementary and alternative medicine, QOL patient-reported outcomes, BCS breast cancer survivors, HRQOL health-related quality of life
There were 6 systematic reviews on physical activity and quality of life in breast cancer patients. Overall, evidence suggests that physical activity could enhance quality of life and reduce symptoms [55, 58, 60, 61, 64, 69]. For instance, a meta-analysis consisting of 5544 patients found that exercise interventions such as aerobic, Tai Chi, yoga, stretch training, and resistance training in survivors had statistically significant effects on overall QOL and breast and arm symptoms [61].
-
(2)
Complementary and alternative medicine (CAM)
A variety of reviews assessed the effect of complementary and alternative medicine including diet and dietary supplements, energy therapies, manipulative and body-based practices, and mind–body techniques on the QOL aspects. Reviews on the effect of CAM on symptoms showed a significant improvement in symptoms [63]. One study of reviewing publications targeted mind–body exercise including yoga, Tai Chi chuan, and qigong found that breast cancer patients’ psychological quality of life benefited from yoga, while physical elements of quality of life were not supported [68]. Yoga is the most studied mind–body therapy. Reviews focusing on the effect of yoga on quality of life among survivors showed that although the literature provided evidence of health related quality of life benefits or significant effects of yoga on reducing fatigue and sleep disturbances, for example, [58, 66, 70], any specific aspect of yoga was not recognized as being most advantageous [57]. The results of a meta-analysis including 951 patients on mindfulness-based therapy on QOL aspects indicated an improvement of this therapy on reducing anxiety, depression, fear of recurrence, and fatigue associated with breast cancer [65]. However, a systematic review of the effect of art therapies on anxiety and depression indicated that such interventions could have a significant effect on patients’ reduced anxiety [57].
Psychological distress
Reviews concerning psychological issues and quality of life are presented in Table 4 [73–79]. Psychoeducational support found to be effective in improving breast cancer symptoms and emotional well-being among breast cancer patients [76]. In addition, a review found that reported psychological distress including anxiety and depression were common among breast cancer patients [75] and the treatment of depression could have an important role on improving QOL and increasing longevity [74].
Table 4.
A list of reviews on psychological distress and quality of life (2008–2018)
| Authors [References] | Year | Main focus | Description/analysis | No. of databases | No. of included studies | Performed QA | Risk of bias assessment | Result(s) |
|---|---|---|---|---|---|---|---|---|
| Reich et al. [73] | 2008 | Impact of depression on QOL | Review | NA | NA | No | No | Treatment of depression improves QOL and may increase longevity |
| Duijts et al. [74] | 2011 | Effect of behavioral techniques and physical exercise on psychosocial functioning and HRQOL outcomes | Systematic review and meta-analysis | 6 | 56 | No | No | Behavioral techniques and physical exercise improve psychosocial functioning and HRQOL in breast cancer patients and survivors |
| Paraskevi [75] | 2012 | QOL outcomes | Review | 4 | NA | No | No | Psychological distress-anxiety and depression were common among BC patients. Pain, fatigue, and insomnia were the most common symptoms reported |
| Matsuda et al. [76] | 2014 | Effectiveness of psychoeducational support on quality of life | Systematic review and meta-analysis | CENTRAL | 8 | No | Yes | Psychosocial support in improving BC symptoms and in improving emotional well-being is effective within 6 months post-intervention |
| Chow et al. [77] | 2016 | Body Image and QOL | Review | 5 | 13 | NA | NA | BC survivors were reported a poorer body image and deterioration in their QOL after treatment. There was not enough evidence of the correlation between body image and QOL |
| Ye et al. [78] | 2018 | Efficacy of cognitive behavior therapy on QOL and psychological health of survivors | Meta-analysis | 4 | 10 | Yes | Yes | Due to the effectiveness of therapy for psychological symptoms, cognitive behavior therapy should be used as the intervention |
| Abrahams et al. [79] | 2018 | Relationship of fatigue with QOL and factors that can be addressed in psychological interventions | Systematic review | 5 | 57 | Yes | No | Moderate to strong evidence appeared for a relationship of fatigue with depressive symptoms, anxiety, distress, sleep disturbances, lower physical activity levels, pain, difficulties with coping with cancer, and catastrophizing about symptoms |
QA quality appraisal, NA not available, QOL quality of life, HRQOL health-related quality of life, NA not applicable, CENTRAL Cochrane Central Register of Controlled Trials, BCS breast cancer survivors
Age-related reviews
Descriptive characteristics of reviews concerning quality of life in young and elderly breast cancer patients are summarized in Table 5 [80–83]. A review on long-term survivors indicated that it seems older patients are better prepared mentally to deal with treatments, despite of having co-morbidities [80]. While a study on young survivors reported greater fear of death, unmet supportive care needs, financial constrain, and minor physical well-being. Spiritual well-being aspects seemed favorable among this subpopulation. However, these patients generally experience suboptimal HRQOL after breast cancer diagnosis [83].
Table 5.
A list of age-related reviews on quality of life in breast cancer patients (2008–2018)
| Authors [References] | Year | Main focus | Description/analysis | No. of databases | No. of included studies | Performed QA | Risk of bias assessment | Result(s) |
|---|---|---|---|---|---|---|---|---|
| Ballinger and Fallowfield [80] | 2009 | Assessment of QOL in older patients | Review | NA | 25 | No | No | The long-term survivorship studies indicate that older patients are perhaps better equipped mentally to deal with treatments |
| Munoz [81] | 2010 | Quality of life during treatment in young patients | Review | NA | NA | No | No | Patients who undergone mastectomy have worse body image and disturbances in their sexual life. Patients treated with mastectomy and adjuvant chemotherapy are those with the greatest impairment. Also, sexual activity is negatively affected by chemotherapy |
| Rosenberg and Partridge [82] | 2013 | QOL related to physical and psychosocial functioning in young premature menopause patients | Review | NA | NA | No | No | Effective strategies as an intervention should be applied to relieve symptoms and improve QOL in younger age groups |
| Samuel et al. [83] | 2016 | HRQOL in young black survivors | Systematic review | 5 | 6 | Yes | No | Young black BCS generally experience suboptimal HRQOL after breast cancer diagnosis |
QA quality appraisal, NA not available, HRQO health-related quality of life, QOL quality of life, BCS breast cancer survivors
Assessment of quality of life among nations/races
A number of reviews [84–91] addressed the quality of life among breast cancer patients of different races for instance African American patients [84, 88], or among different nations such as Spanish breast cancer patients [85], Latina and non-Latina breast cancer survivors [86], Indian breast cancer patients [87], Arab women [89], Asian breast cancer patients [90] and Iranian breast cancer patients [91] (Table 6). Good scores of global health were recorded for in both African American and white survivors [84, 88], but it was reported that Latina breast cancer survivors on average experience worse QOL than non-Latina whites [86]. Asian breast cancer patients with comorbidities and those who treated with chemotherapy, having less social support, and with more unmet needs, had poorer HRQOL [90]. Limited information on quality of life in Arab women with breast cancer patients exist [89].
Table 6.
A list of reviews on quality of life in different nations/races (2008–2018)
| Authors [References] | Year | Main focus | Description/analysis | No. of databases | No. of included studies | Performed QA | Risk of bias assessment | Result(s) |
|---|---|---|---|---|---|---|---|---|
| Russell et al. [84] | 2008 | QOL of African American and white survivors | Review | 4 | 26 qualitative and quantitative | No | No | QOL was different in two groups. Overall global quality of life was favorable in both African American and white survivors |
| Delgado-Sanz et al. [85] | 2011 | QOL in Spanish BC patients | Systematic review | 8 | 25 | Yes | No | Research into health-related quality of life of breast-cancer patients is a little developed |
| Yanez et al. [86] | 2011 | QOL among Latina breast cancer patients | Systematic review | 2 | 22 qualitative and quantitative | No | No | Latina BCS on average experience worse QOL than non-Latina Whites |
| Deshpande et al. [87] | 2013 | QOL outcomes in Indian | Review | NA | NA | No | No | Clinical pharmacists may give the major support to Indian healthcare system in future |
| Mollica et al. [88] | 2015 | QOL in African American breast cancer survivors | Integrative literature review | 5 | 19 | Yes | No | Researchers must focus on factors from a multi-domain perspective to truly understand the varied dimensions influencing QOL |
| Haddou Rahou et al. [89] | 2016 | QOL in Arab women | Systematic review | 5 | 13 qualitative and quantitative studies | Yes | No | Good scores of global health were recorded at Arab women compared to other countries. There was a difference in QOL scores and its associated factors among Arab women from different nations |
| Ho et al. [90] | 2018 | QOL in Asian patients | Systematic review | 3 | 57 | Yes | No | Patients with comorbidities and those treated with chemotherapy, with less social support and with more unmet needs, have poorer HRQOL |
| Bouya et al. [91] | 2018 | QOL of Iranian patients | Systematic review and Meta-analysis | 4 | 18 | Yes | No | Moderate level of QOL in patients was indicated |
QA quality appraisal, NA not available, QOL quality of life, BCS breast cancer survivors
Qualitative reviews
Although some reviews included both quantitative and qualitative studies [84, 86, 89], there was only one review that exclusively reviewed qualitative studies [32]. The review included seven qualitative studies focusing on quality of life of breast cancer patients during and up to 10 years after treatment. Studies were from both developed and developing countries. The review generated three synthesized findings: to achieve effective care, clinicians are required to be aware of the impact of the disease and its treatment on physical and psychosocial domains of quality of life, for effective patient-centered care, they need to know about these effects on social relationships; finally, clinicians should be aware that women use religion and spirituality in order to cope with breast cancer treatment and to improve their own quality of life [32].
Achievements so far and a brief synthesis
During 2008 to 2018 the number of reviews increased to 82 compared to 29 reviews during 1974 to 2007. This in fact is a reflection of the increase in the number of studies on quality of life among breast cancer patients worldwide. Of these, reviews emerging from less developed countries were evident. Even though the quality of these reviews was relatively poor, data from such studies surely provided more understanding on quality of life in breast cancer patients with different cultural backgrounds. According to the AMSTAR on average above 85% of publications had moderate to high quality, as we shown in Tables 1, 2, 3, 4, 5 and 6, but a considerable number of published reviews lacked standards for reporting, 56 out of 82 (68%) did not followed the PRISMA, 51% did not performed quality assessment, and 75% did not reported how risk of bias was evaluated. However, it is difficult to synthesis the data, we provided a tabulated summary of factors that might improve or decrease (worsen) quality of life in breast cancer patients. The summary is derived from review papers that included in this overview (Table 7).
Table 7.
Factors related to improved or reduced quality of life in breast cancer patients and survivors
| Factors that might improve quality of life | Factors that might deteriorate quality of life |
|---|---|
| Reduction of radiation-induced skin toxicity using simultaneous integrated boost, accelerated partial breast irradiation, and prone positioning | Adjuvant endocrine therapy-related side effects including vasomotor symptoms such as hot flashes |
| Adjuvant chemotherapy and radiotherapy in the elderly with solid tumors | Targeted therapy-related side effects: diarrhoea and skin rash in the adjuvant and metastatic settings for HER2+ breast cancer |
| Oncoplastic breast surgery | Body image after mastectomy |
| Both immediate and delayed breast reconstruction in long-term | Chemotherapy-induced alopecia |
| Better preoperative counseling and informed decision-making | Disturbances in sexual life |
| Physical activity interventions such as yoga, exercise, physical self-management, complementary exercise, art therapies, and mind–body exercise therapy | Less social support and unmet needs |
| Treatment of lymphedema: manual lymphatic drainage | Lymphedema affecting woman’s physical, psychological, and emotional well-being |
| Psychoeducational support or receiving social support in early stage breast cancer | Premature menopause, menopausal symptoms, and infertility |
| Cognitive behavioral therapy | Comorbid depression which significantly increases the burden of distress and dysfunction |
Discussion
Patient reported outcomes
Instruments introduced to quantify quality of life in breast cancer patients have developed frequently over the last decade. From the health professionals’ and patients’ views among specific measures, the EORTC QLQ-BR23 and the FACIT-B were the most acceptable instruments. However, despite of reporting the good performance for these measures [17–20], others found that current instruments do not address important specific issues such as surgery‐specific conditions [10]. In addition, a recent review suggested that developing well-designed and more specific tools are needed to evaluate the side effects of novel therapies [21]. We believe that there is no need to develop new instruments, and rather if needed could add extra items to the existing questionnaires to fill the gaps as the EORTC quality of life study group did. They currently updated the EORTC QLQ-BR23 and introduced the QLQ-BR45 to cover all existing gaps. Two main reasons for this revision was indicated: the obvious changes in standard therapy and consequently emergence of new therapies that led to new different side effects, and the impacts of new drugs on patient’s quality of life [92, 93]. Above all we think the new direction for setting international standards for the analysis of quality of life and patient-reported outcomes in cancer trials is a step forward to prevent disorganized reporting, and to encourage using appropriate instruments to measure quality of life in cancer patients in general and in breast cancer patients in particular [94–96].
Methodological issues
A number of reviews indicated that although methodological issues improved greatly, still reviews suffer from poor transparency in reporting on quality appraisal and risk of bias assessment. A review indicated that the sound scientific methodology in HRQOL was undermined by poorly designed and underpowered studies [11]. The current overview indicated that although all reviews have considered the principle components of AMSTAR checklist, the vast majority of reviews not included publication bias. However, the quality of reviews published during the last decade seems did not changed so much and thus that there is a need to further increase their quality. One way to achieve this might be registration of reviews in PROSPERO (International prospective register of systematic reviews).
Treatment modalities
Quality of life can be an important predictor of better treatment outcomes [45]. A review, as an example, indicated that most studies reported increase in long-term satisfaction among patients who underwent surgery [48]. However, as a recent review suggests quality of life in breast cancer patients who receive surgery even might depend on decision-making process and communication style of care physicians. As such the review found that patients who received physician-dominated communication had lower physical function compared with those who took a more active role in their treatment choices processing [97]. This therefore sustains the need to increase the patients' information in order to prevent decisional regret, a common phenomenon after breast reconstruction [98]. In fact, this reflects a previous recommendation to clinicians that: there is a long life after breast cancer and clinicians should consider this while discussing treatment options with patients [33].
Physical activity
Studies and reviews on physical activities have received much attention over the last decade. Reviews showed that interventions based on physical activities have not only improved breast cancer patients’ quality of life, but also could reduce symptoms including breast, arm and early menopausal symptoms [55, 75]. Moreover, positive effects and significant benefits of supervised combined aerobic resistance exercise on fatigue and QOL were reported in patients during their adjuvant radiotherapy [63]. Overall, one might argue that simple and inexpensive interventions or scheduling social events or even providing the green environments and neighborhoods might help to improve quality of life in breast cancer patients.
Alternative therapies
Studies suggest that complementary and alternative therapies have achieved the potential of integrating into clinical practice [56]. However, according to the existing evidence with regard to CAM, yet, further high quality randomized clinical trials or longitudinal studies are required to evaluate net benefits of such treatments on quality of life of breast cancer patients [56, 63]. Yoga as a complementary therapy was frequently recommended in reviews. It seems that since practicing yoga as mind–body exercise could enhance psychological and social well-being, thus it could improve quality of life among breast cancer survivors [68]. Based on the quality of the evidence, for instance, an evidence (with moderate quality) supported the recommendation of yoga as a supportive intervention for improving HRQOL and reducing fatigue and sleep disturbances when compared with no therapy, as well as for reducing depression, anxiety and fatigue, when compared with psychosocial/educational interventions [62]. In spite of suggesting yoga in most studies, a review found that the most advantageous aspect of yoga is still not clear [57].
Symptoms
Symptoms including anxiety, pain, fatigue and menopausal symptoms can significantly impact patients' daily live activities and subsequently their quality of life. It appears that the more affecting symptoms in breast cancer patients are still neglected topics in reviews. Studies are required to be carried out on symptoms’ burden and functional decline in breast cancer patients and survivors. The most frequently reported bothersome symptoms in breast cancer survivors were fatigue, insomnia, depression, cognitive dysfunction, reproductive and menopausal symptoms, and lymphedema [33]. Physical, psychological and emotional well-being of breast cancer patients are affected by lymphedema [53]. Reviews referenced to the treatment of lymphedema indicated that depending on the type of therapy such as manually lymphatic drainage or combined decongestive therapy, a significant positive impact on patient’s quality of life is observed [16, 53], although recently it has been suggested that still there is a need for high-quality evidence to talk about the effectiveness of combined decongestive therapy [54].
Psychological interventions
‘The day you lose your hope is the day you start to die’ is a key sentence that implies the key role for psychological interventions in improving breast cancer symptoms and enhancing patients’ quality of life [99]. Psycho-educational support, for example, in improving breast cancer symptoms and in improving emotional well-being is an effective intervention [76]. Moderate to strong evidence reported a relationship between fatigue and depression, anxiety, pain, sleep disturbances, insufficient physical activity, and difficulties with coping with cancer, all of which can be addressed in psychological interventions [79]. Cognitive behavior therapy as an effective therapy in reducing symptoms and in improving QOL and psychological health of survivors has been reported [78]. Interestingly, it can be seen that joint effect of behavioral techniques and physical exercise can improve psychosocial functioning and HRQOL in breast cancer patients and survivors further [74]. In addition, as recently suggested, specific mindfulness activities also might help patients of all ages to cope with their diagnosis [99].
The elderly and quality of life
Overall, we found that elderly patients reported moderate to good quality of life. Older patients are perhaps better equipped mentally to deal with treatments compared to younger patients [80]. According to the findings of a review, the impact of local or systemic treatments on QOL in the elderly early-breast cancer patients was maintained or improved [31] or adjuvant chemotherapy and radiotherapy did not have detrimental effects on QOL in most elderly patients with solid tumors [52].
Limitations and the future directions
One should note that this review of reviews has some limitations. The main critic is the fact that it is difficult to evaluate in what way the results add to existing knowledge since 82 reviews with different objectives were evaluated. While a more focused and in-depth reviews are recommended, it is useful to bear in mind that this review of reviews in fact is a bibliometric analysis of review papers and provides a representation of what achieved during the last decade studying quality of life in breast cancer patients. We believe this even could highlight repetitions, discrepancies, and indicate areas that require more investments. For instance, we noticed that although reviews included both breast cancer patients and survivors, no specific reviews on quality of life in breast cancer survivors could be identified. Perhaps this is an area that could be addressed independently since there are differences in quality of life between newly diagnosed breast cancer patients, patients who are receiving different treatments, and the long-term survivors who successfully completed their treatments and now they have back to normal life. Survivorship in breast cancer patients is a very important and relevant topic and deserves more attention. Finally, it is important to notice that this review of reviews did not separate the interventional studies from other types of studies (usually descriptive or correlational). Perhaps a better organization might be to reporting reviews based on separate objectives. However, we have tried to provide a summary table (Table 7) which could help to identify factors that might improve or deteriorate quality of life in breast cancer patients.
Conclusion
Quality of life in breast cancer patients improved greatly during recent years as several simple but effective interventions such as physical activity and psychosocial interventions proved to be effective. However, symptoms caused by different treatment modalities are still under estimation and need more serious attention. Pain, lymphedema, worry, sexual function especially for young patients, and the future outlooks all are among issues that deserve further consideration in order to improve quality of life in breast cancer patients.
Supplementary information
Additional file 1. List of reviews from 1974–2007.
Acknowledgements
Not applicable.
Abbreviations
- CDSR
Cochrane Database of Systematic Reviews
- PRISMA
Preferred reporting items for systematic reviews and meta-analyses
- AMSTAR
A Measurement Tool to Assess systematic Reviews
- PROSPERO
International prospective register of systematic reviews
- QOL
Quality of life
- HRQOL
Health related quality of life
- CAM
Complementary and alternative medicine
Authors’ contributions
PMH performed the search, provided initial tables, and helped in writing and responding to reviewers’ comments. AM initiated and designed the study, supervised the literature search, did the manual search, critically evaluated the manuscript and tables, interpreted the findings, responded to reviewers’ comments and provided the final draft. Both authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
2/25/2022
A Correction to this paper has been published: 10.1186/s12955-022-01942-w
Contributor Information
Parisa Mokhtari-Hessari, Email: p.mokhtari@acecr.ac.ir.
Ali Montazeri, Email: montazeri@acecr.ac.ir.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12955-020-01591-x.
References
- 1.DeSantis C, Siegel R, Bandi P, Jemal A. Breast cancer statistics, 2011. CA Cancer J Clin. 2011;61(6):408–418. doi: 10.3322/caac.20134. [DOI] [PubMed] [Google Scholar]
- 2.Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 3.Cardoso F, Kyriakides S, Ohno S, Penault-Llorca P, Poortmans I, Rubio T, Zackrisson S, Senkus E. Early breast cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2019;30:1194–1220. doi: 10.1093/annonc/mdz173. [DOI] [PubMed] [Google Scholar]
- 4.Van Leeuwen M, Husson O, Alberti P, et al. Understanding the quality of life (QOL) issues in survivors of cancer: towards the development of an EORTC QOL cancer survivorship questionnaire. Health Qual Life Outcomes. 2018;16(1):114. doi: 10.1186/s12955-018-0920-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bottomley A, Reijneveld JC, Koller M, Flechtner H, Tomaszewski KA, Greimel E. Current state of quality of life and patient-reported outcomes research. Eur J Cancer. 2019;121:55–63. doi: 10.1016/j.ejca.2019.08.016. [DOI] [PubMed] [Google Scholar]
- 6.Montazeri A. Health-related quality of life in breast cancer patients: a bibliographic review of the literature from 1974 to 2007. J Exp Clin Cancer Res. 2008;27:32. doi: 10.1186/1756-9966-27-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith V, Devane D, Begley CM, Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol. 2011;11(1):15. doi: 10.1186/1471-2288-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lunny C, Brennan SE, McDonald S, McKenzie JE. Toward a comprehensive evidence map of overview of systematic review methods: paper 1-purpose, eligibility, search and data extraction. Syst Rev. 2017;6(1):231. doi: 10.1186/s13643-017-0617-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10. doi: 10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen CM, Cano SJ, Klassen AF, King T, McCarthy C, Cordeiro PG, et al. Measuring quality of life in oncologic breast surgery: a systematic review of patient-reported outcome measures. Breast J. 2010;16(6):587–597. doi: 10.1111/j.1524-4741.2010.00983.x. [DOI] [PubMed] [Google Scholar]
- 11.Winters ZE, Benson JR, Pusic AL. A systematic review of the clinical evidence to guide treatment recommendations in breast reconstruction based on patient-reported outcome measures and health-related quality of life. Ann Surg. 2010;252(6):929–942. doi: 10.1097/SLA.0b013e3181e623db. [DOI] [PubMed] [Google Scholar]
- 12.Lemieux J, Goodwin PJ, Bordeleau LJ, Lauzier S, Theberge V. Quality-of-life measurement in randomized clinical trials in breast cancer: an updated systematic review (2001–2009) J Natl Cancer Inst. 2011;103(3):178–231. doi: 10.1093/jnci/djq508. [DOI] [PubMed] [Google Scholar]
- 13.Reed E, Kossler I, Hawthorn J. Quality of life assessments in advanced breast cancer: should there be more consistency? Eur J Cancer Care (Engl) 2012;21(5):565–580. doi: 10.1111/j.1365-2354.2012.01370.x. [DOI] [PubMed] [Google Scholar]
- 14.Chopra I, Kamal KM. A systematic review of quality of life instruments in long-term breast cancer survivors. Health Qual Life Outcomes. 2012;10:14. doi: 10.1186/1477-7525-10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adamowicz K, Jassem J, Katz A, Saad ED. Assessment of quality of life in advanced breast cancer. An overview of randomized phase III trials. Cancer Treat Rev. 2012;38(5):554–558. doi: 10.1016/j.ctrv.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 16.Pusic AL, Cemal Y, Albornoz C, Klassen A, Cano S, Sulimanoff I, et al. Quality of life among breast cancer patients with lymphedema: a systematic review of patient-reported outcome instruments and outcomes. J Cancer Surviv. 2013;7(1):83–92. doi: 10.1007/s11764-012-0247-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Niu HY, Niu CY, Wang JH, Zhang Y, He P. Health-related quality of life in women with breast cancer: a literature-based review of psychometric properties of breast cancer-specific measures. Asian Pac J Cancer Prev. 2014;15(8):3533–3536. doi: 10.7314/apjcp.2014.15.8.3533. [DOI] [PubMed] [Google Scholar]
- 18.Nguyen J, Popovic M, Chow E, Cella D, Beaumont JL, Chu D, et al. EORTC QLQ-BR23 and FACT-B for the assessment of quality of life in patients with breast cancer: a literature review. J Comp Eff Res. 2015;4(2):157–166. doi: 10.2217/cer.14.76. [DOI] [PubMed] [Google Scholar]
- 19.Oliveira IS, da Cunha Menezes Costa L, Fagundes FR, Cabral CM. Evaluation of cross-cultural adaptation and measurement properties of breast cancer-specific quality-of-life questionnaires: a systematic review. Qual Life Res. 2015;24(5):1179–1195. doi: 10.1007/s11136-014-0840-3. [DOI] [PubMed] [Google Scholar]
- 20.Maratia S, Cedillo S, Rejas J. Assessing health-related quality of life in patients with breast cancer: a systematic and standardized comparison of available instruments using the EMPRO tool. Qual Life Res. 2016;25(10):2467–2480. doi: 10.1007/s11136-016-1284-8. [DOI] [PubMed] [Google Scholar]
- 21.Ghislain I, Zikos E, Coens C, Quinten C, Balta V, Tryfonidis K, et al. Health-related quality of life in locally advanced and metastatic breast cancer: methodological and clinical issues in randomised controlled trials. Lancet Oncol. 2016;17(7):e294–e304. doi: 10.1016/S1470-2045(16)30099-7. [DOI] [PubMed] [Google Scholar]
- 22.Turner-Bowker DM, Hao Y, Foley C, Galipeau N, Mazar I, Krohe M, Globe D, Shields AL. The use of patient-reported outcomes in advanced breast cancer clinical trials: a review of the published literature. Curr Med Res Opin. 2016;32(10):1709–1717. doi: 10.1080/03007995.2016.1205005. [DOI] [PubMed] [Google Scholar]
- 23.Krohe M, Hao Y, Lamoureux RE, Galipeau N, Globe D, Foley C, Mazar I, Solomon J, Shields AL. Patient-reported outcomes in metastatic breast cancer: a review of industry sponsored clinical trials. Breast Cancer (Auckl) 2016;14(10):93–102. doi: 10.4137/BCBCR.S39385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pe M, Dorme L, Coens C, Basch E, Calvert M, Campbell A, et al. Statistical analysis of patient-reported outcome data in randomised controlled trials of locally advanced and metastatic breast cancer: a systematic review. Lancet Oncol. 2018;19(9):e459–e469. doi: 10.1016/S1470-2045(18)30418-2. [DOI] [PubMed] [Google Scholar]
- 25.Liu LQ, Branford OA, Mehigan S. BREAST-Q measurement of the patient perspective in oncoplastic breast surgery: a systematic review. Plast Reconstr Surg Glob Open. 2018;6(8):e1904. doi: 10.1097/GOX.0000000000001904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tevis SE, James TA, Kuerer HM, Pusic AL, Yao KA, Merlino J, Dietz J. Patient-reported outcomes for breast cancer. Ann Surg Oncol. 2018;25(10):2839–2845. doi: 10.1245/s10434-018-6616-1. [DOI] [PubMed] [Google Scholar]
- 27.Lemieux J, Maunsell E, Provencher L. Chemotherapy-induced alopecia and effects on quality of life among women with breast cancer: a literature review. Psychooncology. 2008;17(4):317–328. doi: 10.1002/pon.1245. [DOI] [PubMed] [Google Scholar]
- 28.Cella D, Fallowfield LJ. Recognition and management of treatment-related side effects for breast cancer patients receiving adjuvant endocrine therapy. Breast Cancer Res Treat. 2008;107(2):167–180. doi: 10.1007/s10549-007-9548-1. [DOI] [PubMed] [Google Scholar]
- 29.Buijs C, de Vries EG, Mourits MJ, Willemse PH. The influence of endocrine treatments for breast cancer on health-related quality of life. Cancer Treat Rev. 2008;34(7):640–655. doi: 10.1016/j.ctrv.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 30.Pockaj BA, Degnim AC, Boughey JC, Gray RJ, McLaughlin SA, Dueck AC, et al. Quality of life after breast cancer surgery: what have we learned and where should we go next? J Surg Oncol. 2009;99(7):447–455. doi: 10.1002/jso.21151. [DOI] [PubMed] [Google Scholar]
- 31.Reimer T, Gerber B. Quality-of-life considerations in the treatment of early-stage breast cancer in the elderly. Drugs Aging. 2010;27(10):791–800. doi: 10.2165/11584700-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 32.Devi KM, Hegney DG. Quality of life in women during and after treatment for breast cancer: a systematic review of qualitative evidence. JBI Libr Syst Rev. 2011;9(58):2533–2571. doi: 10.11124/01938924-201109580-00001. [DOI] [PubMed] [Google Scholar]
- 33.Pinto AC, de Azambuja E. Improving quality of life after breast cancer: dealing with symptoms. Maturitas. 2011;70(4):343–348. doi: 10.1016/j.maturitas.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 34.Howard-Anderson J, Ganz PA, Bower JE, Stanton AL. Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: a systematic review. J Natl Cancer Inst. 2012;104(5):386–405. doi: 10.1093/jnci/djr541. [DOI] [PubMed] [Google Scholar]
- 35.Kaviani A, Sodagari N, Sheikhbahaei S, Eslami V, Hafezi-Nejad N, Safavi A, et al. From radical mastectomy to breast-conserving therapy and oncoplastic breast surgery: a narrative review comparing oncological result, cosmetic outcome, quality of life, and health economy. ISRN Oncol. 2013;2013:742462. doi: 10.1155/2013/742462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Orsaria P, Varvaras D. Nodal status assessment in breast cancer: strategies of clinical grounds and quality of life implications. Int J Breast Cancer. 2014;2014:469803. doi: 10.1155/2014/469803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tsoi B, Ziolkowski NI, Thoma A, Campbell K, O'Reilly D, Goeree R. Systematic review on the patient-reported outcomes of tissue-expander/implant vs autologous abdominal tissue breast reconstruction in postmastectomy breast cancer patients. J Am Coll Surg. 2014;218(5):1038–1048. doi: 10.1016/j.jamcollsurg.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 38.Taghian NR, Miller CL, Jammallo LS, O'Toole J, Skolny MN. Lymphedema following breast cancer treatment and impact on quality of life: a review. Crit Rev Oncol Hematol. 2014;92(3):227–234. doi: 10.1016/j.critrevonc.2014.06.004. [DOI] [PubMed] [Google Scholar]
- 39.Sodergren SC, Copson E, White A, Efficace F, Sprangers M, Fitzsimmons D, et al. Systematic review of the side effects associated with anti-her2-targeted therapies used in the treatment of breast cancer, on behalf of the EORTC quality of life group. Target Oncol. 2016;11(3):277–292. doi: 10.1007/s11523-015-0409-2. [DOI] [PubMed] [Google Scholar]
- 40.Kameo SY, Sawada NO. Quality of life and adverse reactions caused by chemotherapy in breast cancer: an integrative review. Ont Health Technol Assess Ser. 2016;6(4):51–61. [Google Scholar]
- 41.Mioranza E, Falci C, Dieci MV, Guarneri V, Conte P. The impact of adjuvant endocrine therapy in early breast cancer on quality-of-life: an overview of prospective trials. Expert Rev Qual Life Cancer Care. 2016;1(2):111–120. [Google Scholar]
- 42.Razdan SN, Patel V, Jewell S, McCarthy CM. Quality of life among patients after bilateral prophylactic mastectomy: a systematic review of patient-reported outcomes. Qual Life Res. 2016;25(6):1409–1421. doi: 10.1007/s11136-015-1181-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chalasani P. Optimizing quality of life in patients with hormone receptor-positive metastatic breast cancer: treatment options and considerations. Oncology. 2017;93(3):143–156. doi: 10.1159/000477404. [DOI] [PubMed] [Google Scholar]
- 44.Garrido Oyarzun MF, Castelo-Branco C. Use of hormone therapy for menopausal symptoms and quality of life in breast cancer survivors. Safe and ethical? Gynecol Endocrinol. 2017;33(1):10–15. doi: 10.1080/09513590.2016.1247798. [DOI] [PubMed] [Google Scholar]
- 45.Marta GN, Moraes FY, Leite ET, Chow E, Cella D, Bottomley A. A critical evaluation of quality of life in clinical trials of breast cancer patients treated with radiation therapy. Ann Palliat Med. 2017;6(2):S223–S232. doi: 10.21037/apm.2017.09.06. [DOI] [PubMed] [Google Scholar]
- 46.Zhou Z, Tang DH, Xie J, Ayyagari R, Wu E, Niravath PA. Systematic literature review of the impact of endocrine monotherapy and in combination with targeted therapy on quality of life of postmenopausal women with HR+/HER-2 advanced breast cancer. Adv Ther. 2017;34(12):2566–2584. doi: 10.1007/s12325-017-0644-2. [DOI] [PubMed] [Google Scholar]
- 47.Mileski M, Ayala L, Campuzano E, Joy A, Ornelas S, Ortiz M, et al. Quality of life considerations during cancer treatment in invasive ductal carcinoma patients: a systemic review. ABNF J. 2017;28:9–13. [PubMed] [Google Scholar]
- 48.Platt J, Zhong T. Patient-centered breast reconstruction based on health-related quality-of-life evidence. Clin Plast Surg. 2018;45(1):137–143. doi: 10.1016/j.cps.2017.08.011. [DOI] [PubMed] [Google Scholar]
- 49.Rivera DR, Ganz PA, Weyrich MS, Bandos H, Melnikow J. Chemotherapy-associated peripheral neuropathy in patients with early-stage breast cancer: a systematic review. J Natl Cancer Inst. 2018;110(2):djx140. doi: 10.1093/jnci/djx140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xiao H, Jiang X, Chen C, et al. Longitudinal effects of adjuvant endocrine therapy on the quality of life of post-menopausal women with non-metastatic ER+ breast cancer: a systematic review. PharmacoEcon Open. 2018;2:359–369. doi: 10.1007/s41669-018-0070-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yee C, Wang K, Asthana R, Drost L, Lam H, Lee J, et al. Radiation-induced skin toxicity in breast cancer patients: a systematic review of randomized trials. Clin Breast Cancer. 2018;18(5):e825–e840. doi: 10.1016/j.clbc.2018.06.015. [DOI] [PubMed] [Google Scholar]
- 52.Cheng KK, Lim EY, Kanesvaran R. Quality of life of elderly patients with solid tumours undergoing adjuvant cancer therapy: a systematic review. BMJ Open. 2018;8:e018101. doi: 10.1136/bmjopen-2017-018101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Müller M, Klingberg K, Wertli MM, Carreira H. Manual lymphatic drainage and quality of life in patients with lymphoedema and mixed oedema: a systematic review of randomised controlled trials. Qual Life Res. 2018;27(6):1403–1414. doi: 10.1007/s11136-018-1796-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jeffs E, Ream E, Taylor C, Bick D. Clinical effectiveness of decongestive treatments on excess arm volume and patient-centered outcomes in women with early breast cancer-related arm lymphedema: a systematic review. JBI Database Syst Rev Implement Rep. 2018;16(2):453–506. doi: 10.11124/JBISRIR-2016-003185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bicego D, Brown K, Ruddick M, Storey D, Wong C, Harris SR. Effects of exercise on quality of life in women living with breast cancer: a systematic review. Breast J. 2009;15(1):45–51. doi: 10.1111/j.1524-4741.2008.00670.x. [DOI] [PubMed] [Google Scholar]
- 56.Bleakley K, Stinson M. Complementary and alternative therapies: do they improve quality of life for women with breast cancer? Phys Ther Rev. 2011;16(2):96–105. [Google Scholar]
- 57.Levine AS, Balk JL. Yoga and quality-of-life improvement in patients with breast cancer: a literature review. Int J Yoga Ther. 2012;22:95–99. [PubMed] [Google Scholar]
- 58.Zhang J, Yang KH, Tian JH, Wang CM. Effects of yoga on psychologic function and quality of life in women with breast cancer: a meta-analysis of randomized controlled trials. J Altern Complement Med. 2012;18(11):994–1002. doi: 10.1089/acm.2011.0514. [DOI] [PubMed] [Google Scholar]
- 59.Boehm K, Cramer H. Arts therapies for anxiety, depression, and quality of life in breast cancer patients: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2014;2014:103297. doi: 10.1155/2014/103297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sawyer A. Complementary exercise and quality of life in patients with breast cancer. Br J Nurs. 2014;23(Suppl. 16):S18–S23. doi: 10.12968/bjon.2014.23.Sup16.S18. [DOI] [PubMed] [Google Scholar]
- 61.Zeng Y, Huang M, Cheng AS, Zhou Y, So WK. Meta-analysis of the effects of exercise intervention on quality of life in breast cancer survivors. Evid Based Complement Altern Med. 2014;21(3):262–274. doi: 10.1007/s12282-014-0521-7. [DOI] [PubMed] [Google Scholar]
- 62.Yan JH, Pan L, Zhang XM, Sun CX, Cui GH. Lack of efficacy of Tai Chi in improving quality of life in breast cancer survivors: a systematic review and meta-analysis. Asian Pac J Cancer Prev. 2014;15(8):3715–3720. doi: 10.7314/apjcp.2014.15.8.3715. [DOI] [PubMed] [Google Scholar]
- 63.Leggett S, Koczwara B, Miller M. The impact of complementary and alternative medicines on cancer symptoms, treatment side effects, quality of life, and survival in women with breast cancer—a systematic review. Nutr Cancer. 2015;67(3):373–391. doi: 10.1080/01635581.2015.1004731. [DOI] [PubMed] [Google Scholar]
- 64.Van Dijck S, Nelissen P, Verbelen H, Tjalma W, Gebruers N. The effects of physical self-management on quality of life in breast cancer patients: a systematic review. Breast. 2016;28:20–28. doi: 10.1016/j.breast.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 65.Zhang J, Xu R, Wang B, Wang J. Effects of mindfulness-based therapy for patients with breast cancer: a systematic review and meta-analysis. Complement Ther Med. 2016;26:1–10. doi: 10.1016/j.ctim.2016.02.012. [DOI] [PubMed] [Google Scholar]
- 66.Cramer H, Lauche R, Klose P, Lange S, Langhorst J, Dobos GJ. Yoga for improving health-related quality of life, mental health and cancer-related symptoms in women diagnosed with breast cancer. Cochrane Database Syst Rev. 2017;1(1):CD010802. doi: 10.1002/14651858.CD010802.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.D'Egidio V, Sestili C, Mancino M, Sciarra I, Cocchiara R, Backhaus I, et al. Counseling interventions delivered in women with breast cancer to improve health-related quality of life: a systematic review. Qual Life Res. 2017;26(10):2573–2592. doi: 10.1007/s11136-017-1613-6. [DOI] [PubMed] [Google Scholar]
- 68.Husebo AML, Husebo TL. Quality of life and breast cancer: how can mind-body exercise therapies help? An overview study. Sports (Basel) 2017;5(4):79. doi: 10.3390/sports5040079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lipsett A, Barrett S, Haruna F, Mustian K, O'Donovan A. The impact of exercise during adjuvant radiotherapy for breast cancer on fatigue and quality of life: a systematic review and meta-analysis. Breast. 2017;32:144–155. doi: 10.1016/j.breast.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 70.Pan Y, Yang K, Wang Y, Zhang L, Liang H. Could yoga practice improve treatment-related side effects and quality of life for women with breast cancer? A systematic review and meta-analysis. Asia Pac J Clin Oncol. 2017;13(2):e79–e95. doi: 10.1111/ajco.12329. [DOI] [PubMed] [Google Scholar]
- 71.Zaidi S, Hussain S, Verma S, Veqar Z, Khan A, Nazir SU, et al. Efficacy of complementary therapies in the quality of life of breast cancer survivors. Biomed Res Int. 2017;7:326. doi: 10.3389/fonc.2017.00326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhang Q, Zhang L, Yin R, Fu T, Chen H, Shen B. Effectiveness of telephone-based interventions on health-related quality of life and prognostic outcomes in breast cancer patients and survivors-a meta-analysis. Eur J Cancer Care. 2018;27(1):e12632. doi: 10.1111/ecc.12632. [DOI] [PubMed] [Google Scholar]
- 73.Reich M, Lesur A, Perdrizet-Chevallier C. Depression, quality of life and breast cancer: a review of the literature. Breast Cancer Res Treat. 2008;110(1):9–17. doi: 10.1007/s10549-007-9706-5. [DOI] [PubMed] [Google Scholar]
- 74.Duijts SF, Faber MM, Oldenburg HS, van Beurden M, Aaronson NK. Effectiveness of behavioral techniques and physical exercise on psychosocial functioning and health-related quality of life in breast cancer patients and survivors—a meta-analysis. Psychooncology. 2011;20(2):115–126. doi: 10.1002/pon.1728. [DOI] [PubMed] [Google Scholar]
- 75.Paraskevi T. Quality of life outcomes in patients with breast cancer. Oncol Rev. 2012;6(1):e2. doi: 10.4081/oncol.2012.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Matsuda A, Yamaoka K, Tango T, Matsuda T, Nishimoto H. Effectiveness of psychoeducational support on quality of life in early-stage breast cancer patients: a systematic review and meta-analysis of randomized controlled trials. Qual Life Res. 2014;23(1):21–30. doi: 10.1007/s11136-013-0460-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chow K, Hung K, Yeung S. Body image and quality of life among breast cancer survivors: a literature review. World J Oncol Res. 2016;3:12–20. [Google Scholar]
- 78.Ye M, Du K, Zhou J, Zhou Q, Shou M, Hu B, et al. A meta-analysis of the efficacy of cognitive behavior therapy on quality of life and psychological health of breast cancer survivors and patients. Psyco-Oncology. 2018;27(7):1695–1703. doi: 10.1002/pon.4687. [DOI] [PubMed] [Google Scholar]
- 79.Abrahams HJG, Gielissen MFM, Verhagen C, Knoop H. The relationship of fatigue in breast cancer survivors with quality of life and factors to address in psychological interventions: a systematic review. Clin Psychol Rev. 2018;63:1–11. doi: 10.1016/j.cpr.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 80.Ballinger RS, Fallowfield LJ. Quality of life and patient-reported outcomes in the older breast cancer patient. Clin Oncol (R Coll Radiol) 2009;21(2):140–155. doi: 10.1016/j.clon.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 81.Muñoz M. Quality of life during treatment in young women with breast cancer. Breast Cancer Res Treat. 2016;1(2):111–120. doi: 10.1007/s10549-010-1061-2. [DOI] [PubMed] [Google Scholar]
- 82.Rosenberg SM, Partridge AH. Premature menopause in young breast cancer: effects on quality of life and treatment interventions. J Thorac Dis. 2013;5(S1):S55–S61. doi: 10.3978/j.issn.2072-1439.2013.06.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Samuel CA, Pinheiro LC, Reeder-Hayes KE, Walker JS, Corbie-Smith G, Fashaw SA, et al. To be young, Black, and living with breast cancer: a systematic review of health-related quality of life in young Black breast cancer survivors. Breast Cancer Res Treat. 2016;160(1):1–15. doi: 10.1007/s10549-016-3963-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Russell KM, Von Ah DM, Giesler RB, Storniolo AM, Haase JE. Quality of life of African American breast cancer survivors: how much do we know? Cancer Nurs. 2008;31(6):E36–45. doi: 10.1097/01.NCC.0000339254.68324.d7. [DOI] [PubMed] [Google Scholar]
- 85.Delgado-Sanz MC, Garcia-Mendizabal MJ, Pollan M, Forjaz MJ, Lopez-Abente G, Aragones N, et al. Heath-related quality of life in Spanish breast cancer patients: a systematic review. Health Qual Life Outcomes. 2011;9(1):3. doi: 10.1186/1477-7525-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yanez B, Thompson EH, Stanton AL. Quality of life among Latina breast cancer patients: a systematic review of the literature. J Cancer Surviv. 2011;5(2):191–207. doi: 10.1007/s11764-011-0171-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Deshpande PR, Sheriff MK, Nazir A, Bommareddy S, Tumkur A, Naik AN. Patient-reported quality of life outcomes in Indian breast cancer patients: importance, review of the researches, determinants and future directions. J Cancer Res Ther. 2013;9(1):11–16. doi: 10.4103/0973-1482.110341. [DOI] [PubMed] [Google Scholar]
- 88.Mollica M, Nemeth L, Newman SD, Mueller M. Quality of life in African American breast cancer survivors: an integrative literature review. Cancer Nurs. 2015;38(3):194–204. doi: 10.1097/NCC.0000000000000160. [DOI] [PubMed] [Google Scholar]
- 89.Haddou Rahou B, El Rhazi K, Ouasmani F, Nejjari C, Bekkali R, Montazeri A, et al. Quality of life in Arab women with breast cancer: a review of the literature. Health Qual Life Outcomes. 2016;14:64. doi: 10.1186/s12955-016-0468-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ho PJ, Gernaat SAM, Hartman M, Verkooijen HM. Health-related quality of life in Asian patients with breast cancer: a systematic review. BMJ Open. 2018;8:e020512. doi: 10.1136/bmjopen-2017-020512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bouya S, Koochakzai M, Rafiemanesh H, Balouchi A, Taheri S, Badakhsh M. Health-related quality of life of Iranian breast cancer patients: a meta-analysis and systematic review. Breast Cancer Res Treat. 2018;170(2):205–212. doi: 10.1007/s10549-018-4750-x. [DOI] [PubMed] [Google Scholar]
- 92.EORTC Quality of Life Study Group. Breast Cancer (Update of QLQ-BR23). https://qol.eortc.org/questionnaire/update-qlq-br23/. Accessed at 11 April 2020
- 93.Bjelic-Radisic V, Cardoso F, Cameron D, Brain E, Kuljanic K, da Costa RA, Conroy T, Inwald EC, Serpentini S, Pinto M, Weis J, Morag O, Lindviksmoen Astrup G, Tomaszweksi KA, Pogoda K, Sinai P, Sprangers M, Aaronson N, Velikova G, Greimel E, Arraras J, Bottomley A, EORTC Quality of Life Group and Breast Cancer Group An international update of the EORTC questionnaire for assessing quality of life in breast cancer patients: EORTC QLQ-BR45. Ann Oncol. 2020;31(2):283–288. doi: 10.1016/j.annonc.2019.10.027. [DOI] [PubMed] [Google Scholar]
- 94.Bottomley A, Pe M, Sloan J, Basch E, Bonnetain F, Calvert M, Campbell A, Cleeland C, Cocks K, Collette L, Dueck AC, Devlin N, Flechtner HH, Gotay C, Greimel E, Griebsch I, Groenvold M, Hamel JF, King M, Kluetz PG, Koller M, Malone DC, Martinelli F, Mitchell SA, Moinpour CM, Musoro J, O'Connor D, Oliver K, Piault-Louis E, Piccart M, Pimentel FL, Quinten C, Reijneveld JC, Schürmann C, Smith AW, Soltys KM, Taphoorn MJB, Velikova G, Coens C, Setting International Standards in Analyzing Patient-Reported Outcomes and Quality of Life Endpoints Data (SISAQOL) consortium Analyzing data from patient-reported outcome and quality of life endpoints for cancer clinical trials: a start in setting international standards. Lancet Oncol. 2016;17(11):e510–e514. doi: 10.1016/S1470-2045(16)30510-1. [DOI] [PubMed] [Google Scholar]
- 95.Bottomley A, Pe M, Sloan J, Basch E, Bonnetain F, Calvert M, Campbell A, Cleeland C, Cocks K, Collette L, Dueck AC, Devlin N, Flechtner HH, Gotay C, Greimel E, Griebsch I, Groenvold M, Hamel JF, King M, Kluetz PG, Koller M, Malone DC, Martinelli F, Mitchell SA, Moinpour CM, Musoro JZ, O'Connor D, Oliver K, Piault-Louis E, Piccart M, Pimentel FL, Quinten C, Reijneveld JC, Schürmann C, Smith AW, Soltys KM, Sridhara R, Taphoorn MJB, Velikova G, Coens C. Moving forward toward standardizing analysis of quality of life data in randomized cancer clinical trials. Clin Trials. 2018;15(6):624–630. doi: 10.1177/1740774518795637. [DOI] [PubMed] [Google Scholar]
- 96.Coens C, Pe M, Dueck AC, Sloan J, Basch E, Calvert M, Campbell A, Cleeland C, Cocks K, Collette L, Devlin N, Dorme L, Flechtner HH, Gotay C, Griebsch I, Groenvold M, King M, Kluetz PG, Koller M, Malone DC, Martinelli F, Mitchell SA, Musoro JZ, O'Connor D, Oliver K, Piault-Louis E, Piccart M, Quinten C, Reijneveld JC, Schürmann C, Smith AW, Soltys KM, Taphoorn MJB, Velikova G, Bottomley A. International standards for the analysis of quality-of-life and patient-reported outcome endpoints in cancer randomized controlled trials: recommendations of the SISAQOL Consortium. Lancet Oncol. 2020;21(2):e83–e96. doi: 10.1016/S1470-2045(19)30790-9. [DOI] [PubMed] [Google Scholar]
- 97.Sousa H, Castro S, Abreu J, Pereira MG. A systematic review of factors affecting quality of life after postmastectomy breast reconstruction in women with breast cancer. Psycho-Oncology. 2019;28(11):2107–2118. doi: 10.1002/pon.5206. [DOI] [PubMed] [Google Scholar]
- 98.Flitcroft K, Brennan M, Spillane A. Decisional regret and choice of breast reconstruction following mastectomy for breast cancer: a systematic review. Psycho-Oncology. 2018;27(4):1110–1120. doi: 10.1002/pon.4585. [DOI] [PubMed] [Google Scholar]
- 99.Ginter AC. "The day you lose your hope is the day you start to die": quality of life measured by young women with metastatic breast cancer. J Psychosoc Oncol. 2020;18:1–17. doi: 10.1080/07347332.2020.1715523. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. List of reviews from 1974–2007.
Data Availability Statement
Not applicable.