Abstract
Objective
To evaluate the extent to which pain-related beliefs, appraisals, coping, and catastrophizing differ between countries, language groups, and country economy.
Design
Systematic review.
Methods
Two independent reviewers searched 15 databases without restriction for date or language of publication. Studies comparing pain beliefs/appraisals, coping, or catastrophizing across two or more countries or language groups in adults with chronic pain (pain for longer than three months) were included. Two independent reviewers extracted data and performed the quality appraisal. Study quality was rated as low, moderate, or high using a 10-item modified STROBE checklist. Effect sizes were reported as small (0.20–0.49), medium (0.50–0.79), or large (≥0.80).
Results
We retrieved 1,365 articles, read 42 potential full texts, and included 10 (four moderate-quality, six low-quality) studies. A total of 6,797 adults with chronic pain (33% with chronic low back pain) were included from 16 countries. Meta-analysis was not performed because of heterogeneity in the studies. A total of 103 effect sizes were computed for individual studies, some of which indicated between-country differences in pain beliefs, coping, and catastrophizing. Of these, the majority of effect sizes for pain beliefs/appraisal (60%; eight large, eight medium, and eight small), for coping (60%; seven large, 11 medium, and 16 small), and for catastrophizing (50%; two medium, one small) evidenced statistically significant between-country differences, although study quality was low to moderate.
Conclusions
In 50% or more of the studies, mean scores in the measures of pain beliefs and appraisals, coping responses, and catastrophizing were significantly different between people from different countries.
Keywords: Culture, Chronic Pain, Coping, Pain Beliefs, Musculoskeletal Pain, Catastrophizing, Low Back Pain
Introduction
Chronic pain is a significant problem worldwide, influenced by a complex interaction between biological, psychological, and social factors [1]. The one-year prevalence of chronic pain ranges from 37% to 41% in developed and developing countries [2], with substantial percentages having constant pain and moderate to severe pain [3]. Chronic pain imposes an enormous emotional and financial burden both at individual and societal levels [4], and psychological factors contribute to this.
One such factor is pain beliefs. Pain beliefs can be defined as cognitions or thoughts related to the pain problem [5] (such as beliefs about the cause of pain, its meaning, or appropriate treatments for pain [6–9]). Such beliefs can be personally held, culturally shared, or both [10]. Another factor, coping, is defined as cognitive and behavorial responses intended to manage stressful events such as chronic pain [5,11]. Pain-related beliefs and coping are often classified as adaptive (i.e., beliefs thought to lead to positive outcomes and adjustment) or maladaptive (i.e., beliefs thought to contribute to negative outcomes and poor adjustment) [10,12]. However, it is likely that adaptiveness varies with context—what is maladaptive in one context might be adaptive in another. Moreover, this classification disregards the cultural appropriateness of behavior such as seeking others’ emotional support vs keeping problems to oneself [13,14].
A third psychological factor—catastrophizing—can be defined as an exaggerated negative orientation toward pain [15]. Because catastrophizing is often significantly associated with greater pain intensity, pain interference, depressed mood, and anxiety [15–17], it is generally viewed as a maladaptive (coping) response to pain [18]. However, although catastrophizing is viewed in the West as maladaptive because it contributes to a depressive-thinking bias, in other cultures it could be viewed as maladaptive for different reasons; for example, it may reflect a lack of acceptance of (divinely determined) fate.
Cultural factors may therefore influence pain beliefs/appraisal, coping responses, and catastrophizing [19–22]—all of which are targeted by psychologically based treatments [23–30]. However, “culture” is notoriously difficult to define and operationalize. Variables such as ethnicity, gender, nationality, and language group are commonly used as proxy measures of culture in research studies because these variables are thought to reflect cultural differences [13,31–33]. Consistent with this, previous systematic reviews related to culture have studied racial and ethnic differences [19,34] and religiosity and spirituality [35].
Regardless of how culture is defined, however, it remains important to understand the associations between variables thought to reflect culture—variables such as country of origin and language—because these variables have the potential to influence the acceptability and efficacy of treatments that target pain beliefs, coping, and catastrophizing for change. The findings from research in this area could help us understand the extent to which pain treatments may need to be adapted to make them most appropriate to new populations who may live in different countries or speak different languages than those for whom the interventions were first developed [13].
One recently published review—registered in the PROSPERO registry two months after the current review was registered—sought to provide a summary of the state of knowledge in this area [34]. These investigators reviewed research studies examining differences in pain-related beliefs, cognitions, and behaviors as a function of race, ethnicity, and culture in samples of individuals with chronic musculoskeletal pain. However, this review was limited in that 1) it only included studies whose participants had chronic musculoskeletal pain and not other chronic pain problems and 2) the search was limited to only two databases. The current study sought to address these limitations by including studies whose participants had any chronic pain problem and by searching 15 databases. As a result, we were able to identify five additional studies not included in the previously published review.
The primary aim of this systematic review was to increase our understanding of the role of country of origin and language spoken on pain beliefs/appraisals, pain coping, and pain catastrophizing in individuals with chronic pain. We hypothesized that people living in two different countries or people living within a country but speaking different languages would endorse different levels of pain-related beliefs/appraisals, ways of coping with their chronic pain, and extents of pain catastrophizing [1]. We also aimed to explore differences in pain beliefs/appraisals, coping, and catastrophizing between countries’ income levels.
Methods
Review Protocol and Registration
We followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) checklist and Meta-analysis Of Observational Studies in Epidemiology (MOOSE) guidelines for both the conduct and reporting of this systematic review [36,37]. The review was prospectively registered in the PROSPERO registry (CRD42017082449).
Eligibility Criteria
We included studies if they 1) compared pain-related beliefs/appraisals, coping, and catastrophizing in different countries or groups within one country that speak different languages, or both, in a single study; 2) included quantitative scales of pain beliefs/appraisals, pain coping, and/or pain catastrophizing; 3) were an observational study (cohort, case–control, and cross-sectional studies) or a multicountry clinical trial with information on pain beliefs/appraisal, coping, or catastrophizing separately for the two countries; and 4) included adults (age 18 years or older) with chronic pain (defined as pain lasting for longer than three months), irrespective of etiology (e.g., cancer, trauma, infection, nerve damage, musculoskeletal problems, surgery-related, other systemic illness) or body part (e.g., headache, neck pain, low back pain, upper or lower extremity pain). There were no restrictions in the language and date of publication. We excluded studies if 1) the sample included individuals younger than age 18 years; 2) the study did not report a quantitative scale of pain beliefs/appraisal, coping, or catastrophizing; and 3) the study was a review, editorial, or qualitative research.
Information Sources and Search Strategies
We adapted several search strategies to identify relevant publications. First, we searched 15 databases or search engines for articles to include in the review; namely MEDLINE, Embase, Cochrane Central Register of Controlled Clinical Trials, PsycINFO, CINAHL, Web of Science, Scopus, PubMed, Physiotherapy Evidence Database (PEDro), Google Scholar, Applied Social Sciences Index and Abstracts (ASSIA) via PROQUEST, International Bibliography for Social Sciences (IBSS) via PROQUEST, Literatura Latino Americana em Ciências da Saúde (LILACS), opengrey.eu, and OpenSIGLE. Second, we searched unpublished literature in the largest and most widely used clinical trial registry platform, ClinicalTrials.gov. Finally, we screened the titles in the reference list of included studies in order to identify articles there were not identified by the database search.
We searched databases for articles published before January 15, 2019. We used the search terms 1) chronic pain AND 2) country, language, and socioeconomic status AND 3) belief OR coping OR catastrophizing, as well as their synonyms in various combinations. We repeated the search again on November 21, 2019, with additional search terms to incorporate “language” and “socioeconomic status,” but did not retrieve any additional eligible papers. The detailed search strategy for MEDLINE can be found in the Supplementary Data; we customized search strategies for each database.
Domains of Interest
We were interested in studies reporting pain-related beliefs (or appraisal), coping, or catastrophizing in two or more countries, or in two or more language groups within the same country. The following are commonly used self-report questionnaires for the assessment of pain-related beliefs or appraisal, coping, and catastrophizing and were used in the included studies.
Pain Beliefs and Appraisals
The Survey of Pain Attitudes (SOPA) is commonly used to assess pain beliefs in pain research [6,7]. It assesses seven belief domains, namely 1) belief in one’s control over pain (Pain Control), 2) belief that one is disabled by pain (Disability), 3) belief in a medical cure for pain (Medical Cure), 4) belief that others should be solicitous in response to pain (Solicitude), 5) belief that medications are appropriate for pain management (Medications), 6) belief that emotions influence pain (Emotions), and 7) belief that pain is a signal of harm, and that therefore activity should be avoided (Harm) [7]. Internal consistencies of its subscales have been shown to be acceptable to good, with Cronbach’s alphas ranging from 0.70 to 0.84 for its 57-item and 35-item versions, with an exception for the Harm subscale (alpha = 0.66) [38]. A one-item version of the SOPA was created to increase clinical and research utility based on its strength of association with the parent subscale [7]. The single items have demonstrated their construct validity similar to those of their full version by moderate correlations, with scales assessing depression, pain intensity, and physical disability [7].
Goubert and colleagues developed the Low Back Pain Beliefs Questionnaire (LBPBQ) using items from different scales assessing pain beliefs [21]. It assesses six domains of back pain beliefs related to harm, limited physical activity, belief in a medical cure, caution, lack of self-control, and belief in pain medication. The internal consistencies of the LBPBQ subscales have not been reported.
The Tampa Scale for Kinesiophobia (TSK) and the Fear-Avoidance Beliefs Questionnaire (FABQ) are the most common questionnaires to assess fear of movement, which is considered an important pain-related belief. The factor structure of the TSK is inconsistent, with reports of support for both a four- and a two-factor structure; therefore, we recorded and reported on the findings for the total score only [39]. There are two versions of the TSK, a 17-item and an 11-item version. The FABQ assesses fear-based avoidance of physical activities and fear-based avoidance of work [40]. The internal consistencies of the TSK scales (both versions) have been reported to range from 0.79 and 0.89 for the total scores [41–43]. The internal consistencies of the FABQ subscales have been shown to range from 0.77 to 0.88 [40].
The Revised Illness Perception Questionnaire (IPQ-R) assesses individuals’ perceptions about their illness using a self-report in a variety of clinical conditions including chronic pain [44]. The first section asks questions related to 14 symptoms (if present) that are related to the illness (chronic pain in this study). The IPQ-R assesses seven illness perception domains labeled identity, consequences, timeline acute/chronic, timeline cyclical, coherence, and emotional dimension. Internal consistencies of the subscales range from 0.77 to 0.88 [44].
Finally, the Pain Self-Efficacy Questionnaire (PSEQ) is a questionnaire related to pain appraisal that assesses pain-related self-efficacy beliefs by asking how confident the person is about engaging in a variety of activities despite pain [45,46]. The internal consistency of the original English version of the scale was reported to be 0.92 [46]. Pain appraisal was assessed using the PSEQ under the broad category of pain beliefs for the purpose of the review.
Pain Coping
Pain-related coping is most commonly assessed using the Coping Strategies Questionnaire (CSQ) [47] or one of the versions of the Chronic Pain Coping Inventory (CPCI) [7,48,49]. The CSQ and CPCI items assess a variety of pain coping responses such as guarding, resting, asking for assistance, relaxing, task persistence, exercising/stretching, seeking support, coping self-statements, diverting attention, reinterpreting pain sensations, ignoring pain, praying and hoping, increasing behavioral activities, and catastrophizing [7,47–49]. Although these questionnaires assess multiple domains, the scales from these questionnaires that are most consistently associated with patient function and/or treatment outcome are those that assess catastrophizing [50,51], guarding and resting [48,50,51], task persistence [48], and asking for assistance [50,51]. Other domains that are sometimes associated (but less consistently or strongly) with function include exercising/stretching, seeking support, and praying and hoping [48,50,51]. The internal consistencies of the subscales of the CSQ are generally acceptable (alpha range = 0.71–0.85), except for increasing pain behaviors (alpha = 0.28) [47]. Similarly, the internal consistencies of the CPCI subscales range from 0.70 to 0.93 [48].
Pain Catastrophizing
Pain catastrophizing is another domain sometimes considered a pain belief and sometimes considered a pain coping mechanism. For the purpose of this review, we are classifying pain catastrophizing as an independent domain from pain beliefs and coping. As described previously, it is commonly assessed by the Catastrophizing subscale of the Coping Strategies Questionnaire (internal consistency = 0.78) [47]. It is also assessed using the Pain Catastrophizing Scale (PCS; internal consistency = 0.87) [15] and the Catastrophizing subscale of the Pain-Related Self-Statements Scale (PRSS; internal consistency = 0.88) [52].
Study Selection and Data Management
We transferred references from the search into EndNote X8 (Clarivate Analytics) and deduplicated. Two study authors (SS and JHA/AFV) independently screened each of the titles and abstracts for eligibility on an Excel spreadsheet. We obtained copies of those that appeared to possibly satisfy inclusion criteria as full papers. Two study authors (SS and AFV) then independently read the full text of these articles and decided on the final list of eligible studies. Any discrepancies were resolved by discussion and consensus with a third reviewer (MPJ) when necessary. Exclusion of the studies was recorded with reasons. Two authors (SS and AFV) then independently extracted data from the included studies. Any differences were resolved by discussion and consensus, and in the event that a consensus was not achieved, a third senior author (MPJ) was consulted, who made the final decision. The reviewers were not blind to the authorship of the study. In case the screeners or data extractors were the authors of the included study, screening and data extraction were completed by an author who is not an author of the included studies.
Data Extraction
We extracted the following data from each article into an Excel spreadsheet: authors, year of publication, countries of study, chronic pain diagnosis, language of data collection, and sample sizes from the countries or language groups. Demographic characteristics of the samples (mean and SD of participants’ age and percentage of female participants) were also extracted when reported. Data (mean and SD) on pain-related beliefs/appraisals, coping, and catastrophizing were extracted for the total scores or subscales (see below for details), as appropriate and available; if not available, authors were contacted to obtain the data.
For pain beliefs, we extracted data related to beliefs about 1) control over pain, 2) being disabled by pain, 3) medical cure for pain, 4) solicitude from others, 5) medications being appropriate for pain management, 6) emotional influence on pain, and 7) pain as a sign of harm from the SOPA scales. We extracted fear and avoidance beliefs about physical activity and work from the FABQ. We extracted beliefs about fear of movement/re-injury and low back pain beliefs from the total scores on the TSK and the LBPBQ, respectively. Data related to pain-related self-efficacy or appraisals were extracted from the total scores of the PSEQ. For pain coping, we extracted the means and SDs for scales assessing guarding, resting, asking for assistance, relaxing, task persistence, exercising/stretching, seeking support, coping self-statements, diverting attention, reinterpreting pain sensations, ignoring pain, praying and hoping, and increasing behavioral activities from the CPCI and CSQ. Finally, we extracted the means and SDs of pain catastrophizing (i.e., CSQ Catastrophizing scale, PRSS Catastrophizing scale, and PCS).
Quality Assessment
We adapted the risk of bias tool based on the STROBE checklist [53] and the Cochrane Collaboration risk of bias tool [54] used by Catley and colleagues [55] to assess the quality of the studies. The a priori items we planned to use as reported in the PROSPERO registry consisted of nine-item scale. Each item was scored as “yes” = 1, “no” = 0, and “unclear” = ?. However, we subsequently revised this to add one question (item #8 assessing the validity and reliability of the original scale), because after pretesting data extraction from the first few papers, we found studies using modified scales without reports of their reliability or validity, and we determined that this potential source of bias should be assessed and incorporated in the quality ratings. Thus, the final risk of bias tool we used was a 10-item checklist with one question on detection bias (diagnosis of chronic pain); two questions each on selection bias (if the cases were consecutive or randomly selected and if the demographic characteristics of the participants were similar between groups), statistical methods (sample size calculation and assessment of confounders), and reporting bias (flow of participants reported and dealing with missing items); and three items on validity and reliability of the scales used (validity and reliability of the original scales or in the language in which they were developed, appropriate cross-cultural validity methods used if translated into a new language, and reliability of the scales in the population and language of interest). Total scores on quality assessment were computed for each study, where higher scores indicated better study quality. We then classified the quality scores into low (<50%), medium (50–80%), and high (>80%) [56,57]. Two study authors (SS and AFV) independently assessed the methodological quality for each study, resolving any discrepancies by consensus and consulting a third author (MPJ) if consensus could not be reached. We did not exclude any articles based on methodological quality.
Data Analysis Plan
To test for possible between-country and -language group differences in pain-related beliefs, appraisal, coping, and catastrophizing, we compared the mean scores of the scales assessing these domains across languages and countries. Additionally, we also compared the mean scores based on the income levels of the countries based on the World Bank country classifications indicating the socioeconomic aspects of the country. We planned to conduct meta-analyses if two or more studies reported the same variable (pain beliefs, appraisals, coping, or catastrophizing) in two of the same languages, countries, or economic regions based on the World Bank country classifications, and if the studies were deemed sufficiently homogenous (I2 < 50%) [54].
For the language-group within-country differences (Comparison 1) and between-country differences (Comparison 2) in pain beliefs, coping responses, and catastrophizing, we computed effect sizes using standardized mean differences (SMDs) for any differences between participants between pairs of countries (or who spoke two different languages within the same country) for each study for each domain separately using means and SDs. We pooled the results of two or more samples (languages or chronic pain conditions) from the same country to perform pairwise comparison between countries for Comparison 2. If the individual studies included more than one language or country, then the SMDs for all possible pairwise comparisons were computed. We used Hedge’s g to compute SMDs, a recommended method when group sizes are dissimilar [58]. It uses pooling of “weighted” standard deviations. Effect sizes (Hedge’s g) of 0.20 were considered small, 0.50 as medium, and 0.80 as large [59]. All data are presented as effect estimates with 95% confidence intervals (CIs). A result is deeemed statistically significant when the upper and lower bounds of the CI do not cross 0 [58]. The results of the Comparison 1 and Comparison 2 analyses were collated, interpreted, and presented as per the recommendations of the Cochrane Collaboration [54]. For the reporting of the results for between-country and -language differences in pain beliefs, coping, and catastrophizing, we summarized the direction of effect, size of the effect (ES), consistency of the effect across the studies, and quality of evidence.
We further compared pain beliefs/appraisals, pain coping, and pain catastrophizing scores by economic region (World Bank classification; Comparison 3) if individual studies included data from two or more economic regions. We pooled the results from two or more countries that represented the same economic region in a single study. We reported results as SMDs (using Hedge’s g) as in the primary analysis.
Addressing Missing Data
If a particular study did not report complete data (e.g., SD), we e-mailed the authors with a request to provide data. A second e-mail was sent to the study authors after about three weeks if they did not respond to the first. A third and final reminder e-mail was sent to the authors two weeks after the second e-mail.
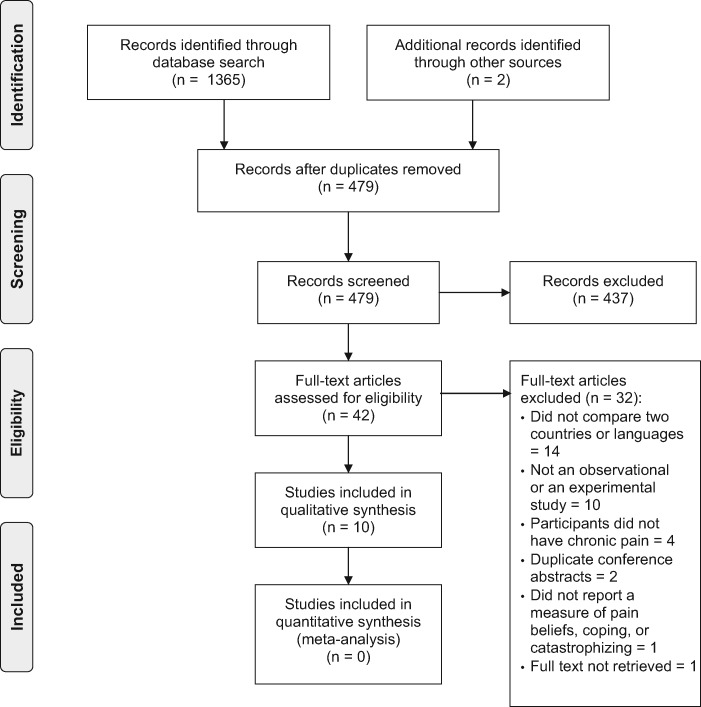
Results
We identified and screened 1,365 potential articles through the database search. We read the full texts of 42 of these, and nine met the criteria for inclusion. One additional article was identified as a citation in a key study. Figure 1 presents the PRISMA flow diagram and describes the number of studies excluded (with reasons), number of duplicates, and the total number of studies included. We contacted the authors of four studies and received data for our analysis from the authors of three studies [21,22,60].
Figure 1.
PRISMA flow diagram.
Description of the Included Studies
All 10 studies included in the review were observational. Six scales were used to assess pain beliefs or appraisals (the LBPBQ, FABQ, TSK, SOPA-brief, IPQ-R, and PSEQ), two were used to assess pain-related coping (the CSQ and CPCI), and three were used to assess pain-related catastrophizing (the CSQ Catastrophizing subscale, PCS, and PRSS Catastrophizing scale).
The 10 studies used data from participants in 16 different countries. One used data from individuals with chronic pain from Asia (Singapore), two each from Australia (Australia), Africa (Ivory Coast, Morocco, South Africa, or Tunisia), and South America (Brazil). Similarly, four studies included data from individuals living in North America (either the United States or Canada), and seven of the studies used data collected from participants from Europe (Belgium, Denmark, France, the Netherlands, Portugal, Spain, or Sweden).
The majority of countries represented were high-income countries (N = 11; Australia, Belgium, Canada, Denmark, France, the Netherlands, Portugal, Singapore, Spain, Sweden, and the United States), followed by lower middle-income countries (N = 3; Tunisia, Ivory Coast, and Morocco) and upper middle-income countries (N = 2; Brazil and South Africa). No countries were represented by the low-income country category. The characteristics of the individual included studies, with year of publication, countries, and languages studied, scales used, diagnosis of chronic pain, study participants’ mean age, SD, and percentage of female participants, are presented in Table 1. We identified two studies by Roelofs et al. [64,65] presenting data from samples that were largely (but not completely) overlapping, which had the aims of evaluating the psychometric properties of two versions of the TSK scale (TSK-11 and TSK-17). We decided to include both of these studies in the review for the qualitative synthesis of the results, which allowed us to determine if different versions of the same scale resulted in similar or different conclusions regarding fear of movement/re-injury beliefs between countries. All the studies and samples used the questionnaires in their first language or official language of the country (e.g., English is the official language of Singapore).
Table 1.
Characteristics of included studies
| Study | Chronic Pain Diagnosis (Setting) | Measures of Pain Beliefs, Coping, and Catastrophizing Used (Score Range) | No. of Countries and Languages | Country (Language) [No.; mean age (SD); % Female] | Comparisons |
|---|---|---|---|---|---|
| Ferreira-Valente, 2011 [61] | Chronic MSK pain (clinical samples) | Coping:
|
|
|
2 (Country: Portugal vs USA) |
| Genet, 2009 [62] | Chronic LBP (clinical samples) |
|
|
|
|
| Goubert, 2004 [21] | Chronic LBP (community samples) |
|
Two languages |
|
1 (2 language-speaking samples in Belgium) |
| Kent, 2014 [60] | Chronic LBP (clinical samples) |
|
|
|
|
| Morris, 2012 [63] | Fibromyalgia (clinical samples) | Beliefs:
|
3 languages |
|
1 (3 languages within same country—South Africa) |
| Roelofs, 2007 [64] | Chronic MSK pain (3 samples) & chronic pain conditions for Dutch sample (clinical samples) | Beliefs:
|
|
|
|
| Roelofs, 2011 [65] | Chronic MSK pain (3 samples) & chronic pain conditions for Dutch sample (clinical samples) | Beliefs:
|
|
|
|
| Ruiz-Montero, 2015 [66] | Fibromyalgia (clinical samples) | Beliefs:
|
|
|
2 (Countries: Spain vs Netherlands) |
| Sarda, 2009 [67] | Chronic pain (clinical samples) | Beliefs:
|
|
|
|
| Thong, 2017 [22] | Chronic pain (clinical samples) | Beliefs:
|
|
|
|
? = unavailable values; CPCI = Chronic Pain Coping Inventory; CSQ = Coping Strategies Questionnaire; FABQ = Fear-Avoidance Beliefs Questionnaire; HICs = high-income countries; IPQ-R = Revised Illness Perception Questionnaire; LBPBQ = Low Back Pain Beliefs Questionnaire; LBP = low back pain; LMIC = low middle-income country; MSK = musculoskeletal; PCS = Pain Catastrophizing Scale; PRSS = Pain-Related Self-Statements Scale; PSEQ = Pain Self-Efficacy Questionnaire; SOPA = Survey of Pain Attitudes; TSK = Tampa Scale for Kinesiophobia; UMIC = upper middle-income country.
Response option was changed from a 0–6 to 0–10 format by the study authors.
Participants
The reviewed studies included 6,797 individuals with chronic pain (excluding the study by Roelofs 2007 [64], which included the same participants plus a few additional participants in a subsequent 2011 study [65]). The most commonly studied diagnoses were chronic low back pain (N = 4 studies: 2,224 participants [21,60,62,65]); followed by chronic musculoskeletal pain (N = 2 studies: 1,526 participants [20,65]); chronic pain in general (N = 2 studies: 823 participants [22,67]); and fibromyalgia (N = 3 studies: 809 participants [63,65,66]). Nine of 10 included studies recruited clinical samples. The exception was a study by Goubert and colleagues that used a postal survey design to assess a sample representative of the population in Belgium [21].
The reports that were identified and included in this review were not sufficiently homogeneous to allow data pooling for a meta-analysis, because no two studies that met the criteria used comparable scales in the same two countries or languages. Therefore, we performed a narrative synthesis of the results without a meta-analysis.
Methodological Quality of Studies
We rated four studies as being of moderate quality and the remaining six as being of low quality (Table 2). No studies were classified as being of high quality. Only three of 10 studies (30%) included a representative sample of consecutive participants, and in only one study (10%) were the demographic characteristics of the study participants similar between the comparison groups. Seven studies (70%) defined chronic pain as pain lasting for at least three months, consistent with the International Association for the Study of Pain definition of chronic pain, and nine studies (90%) either estimated a priori the sample size for the study or included at least 30 participants in each group. Only one study (10%) controlled for confounders (age, sex, socioeconomic status of the study participants). Two studies (20%) reported the flow of participants and how the missing data were handled. Seven studies (70%) used reliable and valid scales (i.e., in the original language they were developed in), and eight studies (80%) met the criteria for cross-cultural adaptation of scales used. Half of the studies (50%) reported the internal consistency of the (multi-item) scales as being at least marginally adequate (i.e., internal consistency of at least 0.60 in the current sample or clear evidence of its reliability in the population of interest in a previous study).
Table 2.
Methodological quality of included studies
| Author and Year | 1. Representativeness: Are the cases consecutive, or was the sample truly randomly selected from the population of interest? | 2. Similar Demographic Characteristics: Are the demographic characteristics of the groups (diagnosis, age, and sex) similar? | 3. Diagnosis of Chronic Pain: Were participants with pain for 3 months or longer included? | 4. Power: Was there an a priori method for sample size estimation, or was the sample size for each group 30 or more? | 5. Confounding Variables: Were the confounding variables controlled for? (matched controls e.g., age, and sex; or use of statistical analysis to control for the confounders) | 6. Reporting Flow of Participants: Was the flow of participants reported? | 7. Dealing with Missing Data: Were methods for dealing with missing data described and appropriate? | 8. Validity and Reliability: Are the scales in the original language reliable and valid measures to assess pain beliefs, coping, or catastrophizing? | 9. Cross-Cultural Adaptation: Did the scales undergo accepted cross-cultural adaptation processes? | 10. Evidence of Reliability: Was evidence presented supporting the reliability of the scales (i.e., internal consistency of >0.60 in the current sample or clear evidence of its reliability in the population of interest in a previous study)? | Total Score | Overall Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ferreira-Valente, 2011 [20] | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 5/10 | Moderate |
| Genet, 2009 [62] | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | N/A* | 3/9 | Low |
| Goubert, 2004 [21] | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 4/10 | Low |
| Kent, 2014 [60] | 1 | 0 | ? | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 3/10 | Low |
| Morris, 2012 [63] | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 7/10 | Moderate |
| Roelofs, 2011 [65] | 0 | 0 | ? | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 4/10 | Low |
| Roelofs, 2007 [64] | 0 | 0 | ? | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 4/10 | Low |
| Ruiz-Montero, 2015 [66] | ? | 0 | 1 | 1 | 0 | 0 | ? | 1 | 1 | 1 | 5/10 | Moderate |
| Sarda, 2009 [67] | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 6/10 | Moderate |
| Thong, 2017 [22] | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | N/A* | 4/9 | Low |
1 = yes, 0 = no, ? = unclear.
A single-item scale was used, for which internal consistency cannot be computed.
Deviation from the Original Study Protocol
Our original goal for this review was to evaluate the role of culture in pain beliefs, coping, and catastrophizing, operationalizing culture (as previous researchers have) as indicated by differences in country, differences in language spoken, or differences in the socioeconomic status of the included countries. However, after we registered the study, we changed our views regarding the appropriateness of these variables as proxy measures of culture [68]. Thus, and although this did not affect the analyses performed, it did change how we discussed the findings; that is, we now discuss them as directly relating to differences as a function of country, the country's economy, or language, as opposed to as differences relating to culture. The second deviation from our original protocol was that we omitted the planned analysis to examine between-continent differences in pain beliefs, coping, and catastrophizing, because of changes in conceptualization of the review during its execution that made these contrasts uninterpretable (Supplementary Data). The third deviation was related to a quality assessment tool, as described earlier.
Differences in Pain-Related Beliefs
Nine of the 10 included studies (90%) used at least one questionnaire to assess pain beliefs or pain appraisal. The results were collated from three studies [21,64,65] for Comparison 1, eight studies [21,22,60,62,64–67] for Comparison 2, and two studies [62,67] for Comparison 3. Overall, we found that 24 of 40 (60%) between-group comparisons were statistically significant (eight large, medium, and small SMDs each). The results indicate that between-country, between–economic region differences in pain beliefs exist (Table 3). However, we found no statistically significant differences in pain beliefs in people living in the same country but speaking different languages based on three low-quality reports [21,64,65].
Table 3.
Standardized mean differences in pain beliefs across countries and languages
| Study | Comparisons (Groups) | Domain/Subdomain | Hedge’s g (Size) | 95% CI | Effect Direction* |
|---|---|---|---|---|---|
| Genet, 2009 [62] | 2 (FRA vs CIV) | Fear avoidance (PA) | –1.14 (L) | –1.48 to –0.80 | CIV > FRA |
| Fear avoidance (work) | –1.25 (L) | –1.59 to –0.91 | CIV > FRA | ||
| 2 (FRA vs TUN) | Fear avoidance (PA) | –0.30 | –0.60 to 0.01 | FRA = TUN | |
| Fear avoidance (work) | –0.02 | –0.32 to 0.29 | FRA = TUN | ||
| 2 (FRA vs MAR) | Fear avoidance (PA) | –0.27 | –0.66 to 0.12 | FRA = MAR | |
| Fear avoidance (work) | 0.28 | –0.11 to 0.67 | FRA = MAR | ||
| 2 (CIV vs TUN) | Fear avoidance (PA) | –0.02 | –0.33 to 0.29 | CIV = TUN | |
| Fear avoidance (work) | 1.17 (L) | 0.84 to 1.51 | CIV > TUN | ||
| 2 (CIV vs MAR) | Fear avoidance (PA) | 0.83 (L) | 0.42 to 1.24 | CIV > MAR | |
| Fear avoidance (work) | 1.40 (L) | 0.96 to 1.83 | CIV > MAR | ||
| 2 (TUN vs MAR) | Fear avoidance (PA) | 0.21 | –0.18 to 0.60 | TUN = MAR | |
| Fear avoidance (work) | 0.28 | –0.11 to 0.67 | TUN = MAR | ||
| 3(HIC vs LMIC) | Fear avoidance (PA) | –0.26 (S) | –0.52 to –0.00 | LMIC > HIC | |
| Fear avoidance (work) | –0.34 (S) | –0.60 to –0.08 | LMIC > HIC | ||
| Goubert, 2004 [21] | 1 (Dutch vs French - BEL) | LBP beliefs | –0.10 | –0.25 to 0.05 | French = Dutch (BEL) |
| Kent, 2014 [60] | (AUS vs DNK) | Fear avoidance (PA) | –0.19 | –0.42 to 0.04 | AUS = DNK |
| Roelofs, 2007 [64]† | 1 (English vs French-CAN) | Fear of movement (TSK-11) | –0.19 | –0.37 to 0.01 | French = English (CAN) |
| 2 (CAN vs SWE) | Fear of movement (TSK-11) | 0.62 (M) | 0.48 to 0.76 | CAN > SWE | |
| 2 (CAN vs NLD) | Fear of movement (TSK-11) | 0.30 (S) | 0.20 to 0.39 | CAN > NLD | |
| 2 (SWE vs NLD) | Fear of movement (TSK-11) | –0.13 | –0.25 to –0.02 | NLD > SWE | |
| Roelofs, 2011 [65]† | 1 (English vs French-CAN) | Fear of movement (TSK-17) | 0.04 | –0.14 to 0.22 | French = English (CAN) |
| 2 (CAN vs SWE) | Fear of movement (TSK-17) | 0.38 (S) | 0.23 to 0.53 | CAN > SWE | |
| 2 (CAN vs NLD) | Fear of movement (TSK-17) | 0.44 (S) | 0.33 to 0.56 | CAN > NLD | |
| 2 (SWE vs NLD) | Fear of movement (TSK-17) | 0.23 (S) | 0.12 to 0.35 | SWE > NLD | |
| Ruiz-Montero, 2015 [66] | 2 (ESP vs NLD) | IP Identity | 1.10 (L) | 0.85 to 1.35 | ESP > NLD |
| IP Timeline | –0.04 | –0.27 to 0.19 | ESP = NLD | ||
| IP Consequences | 0.66 (M) | 0.43 to 0.90 | ESP > NLD | ||
| IP Cyclic Timeline | –0.21 | –0.44 to 0.02 | ESP = NLD | ||
| IP Personal Control | –0.46 (S) | –0.70 to –0.23 | NLD > ESP | ||
| IP Treatment Control | –0.80 (L) | –1.04 to –0.56 | NLD > ESP | ||
| IP Illness Coherence | –0.58 (M) | –0.81 to –0.34 | NLD > ESP | ||
| IP Emotional Representation | 0.92 (L) | 0.68 to 1.16 | ESP > NLD | ||
| Sarda, 2009 [67] | 2, 3 (AUS/HIC vs BRA/UMIC) | ||||
| Pain self-efficacy beliefs (PSEQ) | –0.52 (M) | –0.68 to –0.36 | BRA/UMIC > AUS/HIC | ||
| Thong, 2017 [22] | 2 (USA vs SGP) | SOPA Control | 0.10 | –0.18 to 0.38 | USA = SGP |
| SOPA Medical Cure | –0.57 (M) | –0.85 to –0.29 | SGP > USA | ||
| SOPA Disability | 0.66 (M) | 0.37 to 0.94 | USA > SGP | ||
| SOPA Solicitude | –0.36 (S) | –0.64 to –0.08 | SGP > USA | ||
| SOPA Medication | –0.62 (M) | –0.90 to –0.37 | SGP > USA | ||
| SOPA Emotions | 0.17 | –0.10 to 0.45 | USA = SGP | ||
| SOPA Harm | –0.57 (M) | –0.85 to –0.29 | SGP > USA |
Size of effect: L = large; M = medium; S = small. Large effect sizes are bolded.
AUS = Australia; BEL = Belgium; BRA = Brazil; CAN = Canada; CI = confidence interval; CIV; Ivory Coast; d = effect size; DNK = Denmark; ESP = Spain; FRA = France; HIC = high-income country; IP = illness perception; LBP = low back pain; MAR = Morocco; NLD = the Netherlands; PA = physical activity; SGP = Singapore; SOPA = Survey of Pain Attitudes; SWE = Sweden; TUN = Tunisia; UMIC = upper middle-income country; USA = United States of America; ZAF = South Africa.
Use of “>” indicates significant differences, when the effect does not cross 0.
Results of mean and SD from two samples within Canada and four samples within the Netherlands were combined.
Overall, fear avoidance beliefs (or fear of movement beliefs) were the most commonly studied pain beliefs, with 52% statistically significant between-group effects (12 of 23 ESs; five large, one medium, and six small) indicating the presence of between-country and between-economic region differences in fear avoidance beliefs. Similarly, six of eight illness perception beliefs related to fibromyalgia (75%) were statistically different between patients with fibromyalgia in Spain and the Netherlands, based on one moderate-quality study [66]. Patients from Spain endorsed more illness belief domains related to negative outcomes (e.g., identity, consequences, and cyclic timeline), whereas patients from the Netherlands endorsed statistically significantly more domains associated with positive outcomes (e.g., personal and treatment control and illness coherence). See Table 3 for detailed results.
Differences in Pain-Related Coping
Only three (30%) studies included at least one questionnaire assessing pain coping [20,22,62]. Samples were recruited from seven countries that met the criteria for analysis for Comparisons 2 and 3. Only one study was included for Comparison 3 [62], and no studies met the criteria for Comparison 1. Thirty-four of 57 SMDs (60%) computed for differences in pain coping indicated that pain coping endorsement is significantly different between countries (Table 4). We found that seven, 11, and 16 of these statistically significant ES were large, medium, and small, respectively.
Table 4.
Standardized mean differences in pain coping across countries
| Study | Comparisons(Groups) | Scales/Subdomain | Hedge’s g (Size) | 95% CI | Effect Direction |
|---|---|---|---|---|---|
| Ferreira-Valente, 2011 [20] | 2 (USA vs PRT) | CPCI Guarding | 0.74 (M) | 0.54 to 0.94 | USA > PRT |
| CPCI Resting | 0.96 (L) | 0.76 to 1.17 | USA > PRT | ||
| CPCI Asking for Assistance | –0.07 | –0.27 to 0.13 | USA = PRT | ||
| CPCI Relaxation | –0.15 | –0.35 to 0.05 | USA = PRT | ||
| CPCI Task Persistence | –0.50 (M) | –0.70 to –0.30 | PRT > USA | ||
| CPCI Self-Statements | –0.05 | –0.25 to 0.14 | USA = PRT | ||
| CPCI Exercise/Stretch | –0.34 (S) | –0.54 to –0.14 | PRT > USA | ||
| CPCI Seeking Social Support | –0.20 (S) | –0.40 to –0.00 | PRT > USA | ||
| CSQ Diverting Attention | 0.35 (S) | 0.15 to 0.55 | USA > PRT | ||
| CSQ Ignoring Pain | 0.35 (S) | 0.15 to 0.55 | USA > PRT | ||
| CSQ Reinterpreting Pain Sensations | –0.12 | –0.32 to 0.08 | USA = PRT | ||
| CSQ Praying and Hoping | 0.44 (S) | 0.24 to 0.64 | USA > PRT | ||
| CSQ Increase Behavioral Activities | –0.25 (S) | –0.45 to –0.05 | PRT > USA | ||
| Genet, 2009 [62] | 2 (FRA vs CIV) | CSQ Seeking Social Support | –0.94 (L) | –1.27 to –0.61 | CIV > FRA |
| CSQ Diverting Attention | –0.95 (L) | –1.28 to –0.62 | CIV > FRA | ||
| CSQ Ignoring Pain | –0.10 | –0.41 to 0.21 | FRA = CIV | ||
| CSQ Reinterpreting Pain Sensations | –0.32 (S) | –0.63 to –0.00 | CIV > FRA | ||
| CSQ Praying and Hoping | –2.20 (L) | –2.59 to –1.80 | CIV > FRA | ||
| CSQ Increase Behavioral Activities | –0.56 (M) | –0.88 to –0.24 | CIV > FRA | ||
| 2 (FRA vs TUN) | CSQ Seeking Social Support | –0.32 (S) | –0.63 to –0.02 | TUN > FRA | |
| CSQ Diverting Attention | –0.50 (M) | –0.81 to –0.19 | TUN > FRA | ||
| CSQ Ignoring Pain | –0.27 | –0.57 to 0.03 | FRA = TUN | ||
| CSQ Reinterpreting Pain Sensations | –0.49 (S) | –0.80 to –0.18 | TUN > FRA | ||
| CSQ Praying and Hoping | –1.45 (L) | –1.79 to –1.11 | TUN > FRA | ||
| CSQ Increase Behavioral Activities | 0.05 | –0.25 to 0.35 | FRA = TUN | ||
| 2 (FRA vs MAR) | CSQ Seeking Social Support | –0.39 (S) | –0.78 to –0.00 | MAR > FRA | |
| CSQ Diverting Attention | –0.46 (S) | –0.85 to –0.06 | MAR > FRA | ||
| CSQ Ignoring Pain | –0.14 | –0.53 to 0.25 | FRA = MAR | ||
| CSQ Reinterpreting Pain Sensations | –0.53 (M) | –0.93 to –0.13 | MAR > FRA | ||
| CSQ Praying and Hoping | –1.27 (L) | –1.70 to –0.85 | MAR > FRA | ||
| CSQ Increase Behavioral Activities | 0.38 | –0.01 to 0.77 | FRA = MAR | ||
| 2 (CIV vs TUN) | CSQ Seeking Social Support | 0.59 (M) | 0.27 to 0.91 | CIV > TUN | |
| CSQ Diverting Attention | 0.38 (S) | 0.07 to 0.70 | CIV > TUN | ||
| CSQ Ignoring Pain | –0.17 | –0.49 to 0.14 | CIV = TUN | ||
| CSQ Reinterpreting Pain Sensations | –0.20 | –0.51 to 0.11 | CIV = TUN | ||
| CSQ Praying and Hoping | 0.55 (M) | 0.23 to 0.86 | CIV > TUN | ||
| CSQ Increase Behavioral Activities | 0.60 (M) | 0.28 to 0.92 | CIV > TUN | ||
| 2 (CIV vs MAR) | CSQ Seeking Social Support | 0.49 (S) | 0.09 to 0.89 | CIV > MAR | |
| CSQ Diverting Attention | 0.49 (S) | 0.09 to 0.90 | CIV > MAR | ||
| CSQ Ignoring Pain | –0.04 | –0.43 to 0.36 | CIV = MAR | ||
| CSQ Reinterpreting Pain Sensations | –0.23 | –0.63 to 0.17 | CIV = MAR | ||
| CSQ Praying and Hoping | 0.68 (M) | 0.28 to 1.09 | CIV > MAR | ||
| CSQ Increase Behavioral Activities | 1.02 (L) | 0.60 to 1.44 | CIV > MAR | ||
| 2 (TUN vs MAR) | CSQ Seeking Social Support | –0.08 | –0.47 to 0.31 | TUN = MAR | |
| CSQ Diverting Attention | 0.05 | –0.34 to 0.44 | TUN = MAR | ||
| CSQ Ignoring Pain | 0.14 | –0.25 to 0.53 | TUN = MAR | ||
| CSQ Reinterpreting Pain Sensations | –0.03 | –0.42 to 0.36 | TUN = MAR | ||
| CSQ Praying and Hoping | 0.10 | –0.29 to 0.49 | TUN = MAR | ||
| CSQ Increase Behavioral Activities | 0.32 | –0.07 to 0.71 | TUN = MAR | ||
| 3 (HIC vs LMIC) | CSQ Seeking Social Support | –0.55 (M) | –0.81 to –0.29 | LMIC > HIC | |
| CSQ Diverting Attention | –0.65 (M) | –0.92 to –0.39 | LMIC > HIC | ||
| CSQ Ignoring Pain | –0.17 | –0.43 to 0.08 | LMIC = HIC | ||
| CSQ Reinterpreting Pain Sensations | –0.43 (S) | –0.69 to –0.17 | LMIC > HIC | ||
| CSQ Praying and Hoping | –1.75 (L) | –2.04 to –1.45 | LMIC > HIC | ||
| CSQ Increase Behavioral Activities | –0.03 | –0.29 to 0.22 | LMIC = HIC | ||
| Thong, 2017 [22] | 2 (USA vs SGP) | CPCI Guarding | 0.73 (M) | 0.45 to 1.02 | USA > SGP |
| CPCI Resting | 0.42 (S) | 0.14 to 0.70 | USA > SGP | ||
| CPCI Asking for Assistance | 0.49 (S) | 0.21 to 0.77 | USA > SGP | ||
| CPCI Relaxation | 0.16 | –0.12 to 0.44 | USA = SGP | ||
| CPCI Task Persistence | –0.17 | –0.45 to 0.10 | USA = SGP | ||
| CPCI Self-Statements | 0.10 | –0.18 to 0.37 | USA = SGP | ||
| CPCI Exercise/Stretching | –0.04 | –0.31 to 0.24 | USA = SGP | ||
| CPCI Seeking Social Support | 0.50 (M) | 0.22 to 0.78 | USA > SGP |
Size of effect: L = large; M = medium; S = small. Large effect sizes are bolded.
CI = confidence interval; CIV; Ivory Coast; CPCI = Chronic Pain Coping Inventory; CSQ = Coping Strategies Questionnaire; d = effect size; FRA = France; HIC = high-income country; LMIC = lower middle-income country; MAR = Morocco; PRT = Portugal; SGP = Singapore; TUN = Tunisia; USA = United States of America.
The most commonly observed between-country statistically significant difference in coping was for seeking social support (87%; seven of eight ESs; one large, two medium, and four small), followed by 86% each (six of seven ESs) for praying and hoping (three large, two medium, and one small ESs), and diverting attention (one large, one medium, and four small ESs). These coping strategies were endorsed more often by patients with chronic pain from lower middle-income African countries (Tunisia, Ivory Coast, and Morocco) than a high-income European country: France. Similarly, guarding and resting was statistically significant in two of two comparisons, with samples from the United States endorsing more guarding and resting than samples from Portugal or Singapore.
On the other hand, there was no statistically significant difference in ignoring pain between the same three African countries and France (six of six SMDs), whereas we found a small ES in ignoring pain between samples from the United States and Portugal. The results of the pooled estimates of coping strategies listed in the CSQ from the three lower-middle income African countries compared with a high-income European country (France) showed that the former group endorsed statistically significantly more praying and hoping (large ES), seeking social support (medium ES), diverting attention (medium ES), and reinterpreting pain sensations (small ES) compared with the latter.
Differences in Pain Catastrophizing
Four of the 10 included studies (40%) assessed pain catastrophizing in six countries [20,60,63,67]. Findings from three studies were used for Comparison 2, whereas findings from one study were used to perform Comparisons 1 and 3. Three of six SMDs (two medium and one small ES) indicated that pain catastrophizing reporting is different across countries/economic regions. Of the medium ES, patients with chronic musculoskeletal pain from the United States endorsed more pain catastrophizing (SMD = 0.79) than patients with chronic musculoskeletal pain from Portugal [20]. Similarly, patients with chronic LBP from Australia endorsed more pain catastrophizing (SMD = 0.70) than those from Denmark [60]. Three nonsignificant differences concerned pain catastrophizing between samples of individuals who spoke different languages within South Africa (Table 5) [63].
Table 5.
Standardized mean differences in pain catastrophizing across countries and languages
| Study | Comparisons, No. | Scale Used | Hedge’s g (Size) | 95% CI | Effect Direction |
|---|---|---|---|---|---|
| Ferreira-Valente, 2011 [20] | 2 (USA vs PRT) | CSQ Catastrophizing subscale | 0.79 (M) | 0.59 to 0.99 | USA > PRT |
| Kent, 2014 [60] | 2 (AUS vs DNK) | Brief Catastrophizing Scale | 0.70 (M) | 0.47 to 0.94 | (AUS > DNK) |
| Morris, 2012 [63] | 1 (English vs Xhosa - ZAF) | PCS | 0.38 | –0.19 to 0.95 | English = Xhosa |
| 1 (English vs African - ZAF) | PCS | 0.11 | –0.35 to 0.56 | English = African | |
| 1 (Xhosa vs African - ZAF) | PCS | –0.27 | –0.82 to 0.27 | Xhosa = African | |
| Sarda, 2009 [67] | 2, 3 (AUS/HIC vs BRA/UMIC) | PRSS Catastrophizing subscale | 0.20 (S) | 0.05 to 0.36 | AUS/HIC > BRA/UMIC |
Size of effect: M = medium; S = small. Medium effect sizes are bolded.
AUS = Australia; BRA = Brazil; CI = confidence interval; CSQ = Coping Strategies Questionnaire; d = effect size; DNK = Denmark; HIC = high-income country; PCS = Pain Catastrophizing Scale; PRSS = Pain-Related Self-Statement Scale; PRT = Portugal; UMIC = upper middle-income country; USA = United States of America; ZAF = South Africa.
Discussion
The primary aim of this systematic review was to determine if pain beliefs/appraisals, coping, and catastrophizing varied between countries or between language groups within a country. The findings suggest that between-country differences in pain beliefs/appraisals, coping, and catastrophizing may exist for some pain-related domains, but not for all. If between-country differences do exist, the findings suggest that these are more likely to occur for fear of movement and re-injury, some subscales of pain coping (resting and guarding, seeking social support, diverting attention, and praying and hoping), and pain catastrophizing. However, as discussed later, these conclusions should be viewed as tentative at this point; additional studies using higher-quality methods are needed to determine the reliability of the findings from the studies reviewed here.
Differences in Pain-Related Beliefs
The findings from low- to moderate-quality evidence suggest that differences in fear avoidance beliefs between countries appear to exist. Specifically, the mean values for fear avoidance beliefs in the Ivory Coast were greater than in Tunisia, Morocco, and France; and Canadian samples endorsed higher levels of fear avoidance beliefs than samples from Sweden and the Netherlands. Several factors could potentially explain the between-country differences in patients’ observed fear avoidance beliefs, including the pain treatments available in a country (a function of historical, political, and economic influences) and health professionals’ pain beliefs [69]. For example, health professionals in some countries tend to advise patients to rest in response to pain, rather than maintain a steady level of activity. Advice to rest in response to pain runs counter to evidence, and may foster fearful beliefs in patients [70]. The factors that contribute to the between-country differences in fear avoidance beliefs should further be explored using higher-quality research designs (discussed later).
Between-country differences in other types of pain beliefs were fewer and less consistent than in fear avoidance beliefs, in part because of the limited number of studies on pain beliefs using the same questionnaire(s). For example, three studies [22,66,67] compared differences in pain beliefs/appraisals using scales that assessed somewhat different constructs (IPQ, PSEQ, SOPA), which were therefore not pooled. Whether systematic differences exist between pain beliefs other than fear avoidance beliefs as a function of cultural difference will require additional research.
Differences in Pain-Related Coping
We observed that individuals with chronic low back pain from the three lower-middle income African countries (Tunisia, Morocco, and Ivory Coast) endorsed more praying and hoping (large effect size), seeking social support (medium effect size), and diverting attention (medium effect size) as pain coping responses than individuals from France. However, no significant differences were found in ignoring pain and increasing behavioral activities between individuals from lower-middle income African countries and individuals from France, based on a single low-quality study [62]. The differences identified in the studies reviewed here could be related to either differences in ethnicity, religiosity, socioeconomic status, or some combination of these or other factors.
Differences appeared in comparisons of guarding, resting, and task persistence between samples of people with chronic pain in the United States vs the samples from Portugal and Singapore, but not in relaxation. However, data used to compare coping responses in these two studies were not collected concurrently but five to 10 years apart. Additionally, it is possible that the between-country differences found could be in part due to differences in the overall health care systems of the countries, including the availability of more paid sick leave in the United States (especially compared with Singapore), which in turn may promote more passive forms of coping strategies such as resting and guarding. This possibility could be tested by specific comparisons between countries that control for or evaluate the effects of measures of health care sick leave policy variables.
Differences in Pain Catastrophizing
We observed that pain catastrophizing was significantly different across countries based on findings from three studies. Specifically, a sample of people with chronic pain from the United States endorsed higher levels of pain catastrophizing than the sample from Portugal [20], and those from Australia endorsed more pain catastrophizing than samples from Denmark [60] and Brazil [67]. However, there were no significant differences in pain catastrophizing within different language-speaking groups within South Africa [63], although the study was small. The small number of studies limits any conclusions regarding pain catastrophizing; additional studies from different countries (and different language groups within a single study), ideally using larger sample sizes, are needed.
Research Recommendations
The findings from the current review could help to guide future research on group differences between countries or between groups that speak different languages, or cultural differences in general, in pain beliefs, coping responses, and catastrophizing. Culture is a very complex concept, which has not yet been satisfactorily defined or operationalized in the context of pain research. At present, for psychological domains such as pain beliefs/appraisals, coping, and catastrophizing, studies that describe themselves as “cross-cultural” predominantly use scales originally developed in Western countries. It is challenging to determine if between-country differences in scores from (translated) questionnaires that are rooted in Western philosophy and psychology reflect differences between respondents or nonequivalence of culture and/or translation, especially when research participants are recruited from a non-Western country. Bicultural researchers with expertise in both qualitative and quantitative methods could help develop appropriate and culturally sound ways of assessment of pain-related domains [71]. A meta-synthesis of existing qualitative studies in this area may also further our understanding of the role of culture (however defined) in chronic pain.
Ideally, cross-cultural comparison research would collect data from individuals from different cultures concurrently rather than compare groups of patients using preexisting data, use transparent sampling methods, and pay attention to local norms of social desirability [72]. Similarly, researchers should consider conducting longitudinal studies to explore how a coping strategy assessed at one point in time predicts subsequent pain and function. A study comparing the endorsement of certain pain coping strategies between individuals from different countries or who speak different languages using a cross-sectional design provides at best very limited information regarding the relative efficacy of the coping response in the population studied, because a coping strategy that is adaptive for one individual in one situation (or from one country) is not necessarily adaptive in another situation for the same person, or a person from another country.
Given the current findings suggesting some between-country differences in pain beliefs, coping, and catastrophizing, another recommendation is that a treatment developed in and recommended for individuals from one country or who speak one language should not necessarily be assumed to be effective in individuals from another country or who speak another language without evidence of efficacy in the target population. There is a growing trend to apply psychological interventions for chronic pain that were developed in one country to individuals from a different country [73–76]. However, before trying to change beliefs or coping strategies in individuals from a different country, it would be useful to first conduct research to identify the effects of particular pain beliefs and coping responses on pain and function in the target population in that country.
Limitations
Although we adapted high-quality systematic review methods recommended by the Cochrane Collaboration and the PRISMA guidelines (searching 15 databases and gray literature without limiting our search to language or date of publication), it is important to recognize the review’s limitations. First, the cross-country comparison of pain beliefs, coping, and catastrophizing does not adequately consider individual factors such as race/ethnicity, socioeconomic status (occupation, education, and income), religion, lifestyle factors (e.g., generally active vs sedentary), individual access to health care, or country-related factors such as the health care system (e.g., self-funded vs publicly funded), worker compensation policies, and geography. We cannot confirm whether the between-country differences identified are due to racial differences [19], ethnic differences [34], or individuals’ access to health care, or one or more of many other factors that might influence beliefs or whether these could explain, at least in part, the differences found. Further, ethnic groups within a country can be so diverse that grouping people together “simply on the basis of country” obscures important differences. Similarly, immigrant individuals to a host country may not necessarily hold views of other individuals who live in that country and may or may not be partly or fully acculturated in different areas of life, and the level of acculturation could potentially influence their pain beliefs or coping responses, as well as the impact of those beliefs and coping responses on pain and function [77]. Differences under investigation need to be clearly specified. Although some may consider between-country differences to be cultural differences [33,78], others argue that “country” is not a valid proxy for culture [68].
A second limitation is related to the stringent inclusion criteria used for this review. For example, we chose to include studies based on their use of quantitative scales to assess pain beliefs, coping, or catastrophizing. However, the use of quantitative scales to assess psychological functions has limitations that have been noted for decades [79,80]. The widely accepted view is that it is possible to quantify psychological domains using multiple-item questions, such as those used in the studies reviewed here. Either way, an additional way to address the role of culture in cognitive and behavioral responses to pain would be by qualitative studies across two or more countries, and comparison of emergent themes.
The third limitation of this and other systematic reviews on this topic is the limited number and heterogeneity of eligible studies (i.e., they studied different patient populations and used different scales to assess the same domain), many of which were of low to moderate quality for comparison purposes, as most were designed to 1) evaluate measurement properties of patient-reported questionnaires or 2) compare between-country differences using preexisting data sets [20,22]. Findings from adequately powered quantitative and qualitative studies specifically designed to evaluate the effects of countries, and using the same set of measures and procedures concurrently, would be important to be able draw firmer conclusions.
Finally, the between-country similarities and differences in the scale scores (of pain beliefs/appraisal, coping, and catastrophizing) identified in this review could have been influenced by the different language versions of the questionnaires used in eight of the 10 studies included. To address this issue, future researchers should use cross-culturally adapted scales that are valid and reliable in both countries/language being compared whenever possible.
Conclusions
Despite the review’s limitations, the findings indicate that between-country differences appear to exist in a number of pain beliefs/appraisals (specifically, fear avoidance beliefs), pain coping responses (specifically, use of resting, guarding, praying, and hoping), and pain catastrophizing, whereas between-country differences do not appear to exist for other pain beliefs or coping responses.
The findings indicate that additional research on the role of country (both country of origin and country where an individual lives) in pain responses is warranted. Such research should 1) use procedures specifically designed to address this question including the collection of data at the same time using measures that are known to be culturally relevant (e.g., have the same underlying meaning in the samples studied) and 2) use qualitative approaches to evaluate pain-related beliefs/appraisals, coping, and catastrophizing to identify similar and different themes in the different samples.
Supplementary Material
Acknowledgments
The authors would like to acknowledge Mr. Richard German, librarian at the University of Otago, for his help during planning of search strategies for the review. We would also like to thank the authors of the studies included in the review (Prof. Liesbet Goubert and Prof. Peter Kent, Dr. Ivan Thong Shin Kai), who shared their data with us.
Supplementary Data
Supplementary data are available at Pain Medicine online.
Funding sources: SS is supported by the University of Otago Doctoral Scholarship, and AFV has received a research grant from the Portuguese Foundation for Science and Technology (SFRH/BPD/121452/2016).
Conflicts of interest: Two of the studies included in this review were co-authored by MPJ, one of which was co-authored by AFV and JPR. Otherwise, the authors declare no conflicts of interest with respect to the findings reported here.
Authors Saurab Sharma and Alexandra Ferreira-Valente contributed equally to this work.
PROSPERO registration: CRD42017082449.
References
- 1. Sharma S, Abbott JH, Jensen MP.. Why clinicians should consider the role of culture in chronic pain. Braz J Phys Ther 2018;22(5):345–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tsang A, Von Korff M, Lee S, et al. Common chronic pain conditions in developed and developing countries: Gender and age differences and comorbidity with depression-anxiety disorders. J Pain 2008;9(10):883–91. [DOI] [PubMed] [Google Scholar]
- 3. Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D.. Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. Eur J Pain 2006;10(4):287–333. [DOI] [PubMed] [Google Scholar]
- 4.Institute of Medicine Committee on Advancing Pain Research, Care, and Education: The National Academies Collection: Reports funded by National Institutes of Health. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 5. Jensen MP, Turner JA, Romano JM, Karoly P.. Coping with chronic pain: A critical review of the literature. Pain 1991;47(3):249–83. [DOI] [PubMed] [Google Scholar]
- 6. Jensen MP, Karoly P, Huger R.. The development and preliminary validation of an instrument to assess patients' attitudes toward pain. J Psychosom Res 1987;31(3):393–400. [DOI] [PubMed] [Google Scholar]
- 7. Jensen MP, Keefe FJ, Lefebvre JC, Romano JM, Turner JA.. One- and two-item measures of pain beliefs and coping strategies. Pain 2003;104(3):453–69. [DOI] [PubMed] [Google Scholar]
- 8. Edwards LC, Pearce SA, Turner-Stokes L, Jones A.. The Pain Beliefs Questionnaire: An investigation of beliefs in the causes and consequences of pain. Pain 1992;51(3):267–72. [DOI] [PubMed] [Google Scholar]
- 9. Kori SH, Miller RP, Todd DD.. Kinesiophobia: A new view of chronic pain behavior. Pain Manage 1990;3(1):35–43. [Google Scholar]
- 10. DeGood DE, Tait RC.. Assessment of pain beliefs and pain coping. Handbook Pain Assessment 2001;2:320–41. [Google Scholar]
- 11. Lazarus RS, Folkman S.. Stress, Appraisal, and Coping. New York: Springer Publishing Company; 1984. [Google Scholar]
- 12. Brown GK, Nicassio PM.. Development of a questionnaire for the assessment of active and passive coping strategies in chronic pain patients. Pain 1987;31(1):53–64. [DOI] [PubMed] [Google Scholar]
- 13. Brady B, Veljanova I, Chipchase L.. Culturally informed practice and physiotherapy. J Physiother 2016;62(3):121–3. [DOI] [PubMed] [Google Scholar]
- 14. Callister LC, Khalaf I, Semenic S, Kartchner R, Vehvilainen-Julkunen K.. The pain of childbirth: Perceptions of culturally diverse women. Pain Manage Nurs 2003;4(4):145–54. [DOI] [PubMed] [Google Scholar]
- 15. Sullivan MJL, Bishop SR, Pivik J.. The Pain Catastrophizing Scale: Development and validation. Psychol Assessment 1995;7(4):524–32. [Google Scholar]
- 16. Osman A, Barrios FX, Gutierrez PM, Kopper BA, Merrifield T, Grittmann L.. The Pain Catastrophizing Scale: Further psychometric evaluation with adult samples. J Behav Med 2000;23(4):351–65. [DOI] [PubMed] [Google Scholar]
- 17. Hirsh AT, Bockow TB, Jensen MP.. Catastrophizing, pain, and pain interference in individuals with disabilities. Am J Phys Med Rehabil 2011;90(9):713–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Thorn BE, Ward LC, Sullivan MJ, Boothby JL.. Communal coping model of catastrophizing: Conceptual model building. Pain 2003;106(1):1–2. [DOI] [PubMed] [Google Scholar]
- 19. Meints SM, Miller MM, Hirsh AT.. Differences in pain coping between black and white Americans: A meta-analysis. J Pain 2016;17(6):642–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ferreira-Valente MA, Ribeiro JL, Jensen MP, Almeida R.. Coping with chronic musculoskeletal pain in Portugal and in the United States: A cross-cultural study. Pain Med 2011;12(10):1470–80. [DOI] [PubMed] [Google Scholar]
- 21. Goubert L, Crombez G, De Bourdeaudhuij I. Low back pain, disability and back pain myths in a community sample: Prevalence and interrelationships. Eur J Pain 2004;8(4):385–94. [DOI] [PubMed] [Google Scholar]
- 22. Thong ISK, Tan G, Lee TYC, Jensen MP.. A comparison of pain beliefs and coping strategies and their association with chronic pain adjustment between Singapore and United States. Pain Med 2017;18(9):1668–78. [DOI] [PubMed] [Google Scholar]
- 23. Ehde DM, Dillworth TM, Turner JA.. Cognitive-behavioral therapy for individuals with chronic pain: Efficacy, innovations, and directions for research. Am Psychol 2014;69(2):153–66. [DOI] [PubMed] [Google Scholar]
- 24. Wetherell JL, Afari N, Rutledge T, et al. A randomized, controlled trial of acceptance and commitment therapy and cognitive-behavioral therapy for chronic pain. Pain 2011;152(9):2098–107. [DOI] [PubMed] [Google Scholar]
- 25. Palermo TM, Wilson AC, Peters M, Lewandowski A, Somhegyi H.. Randomized controlled trial of an Internet-delivered family cognitive–behavioral therapy intervention for children and adolescents with chronic pain. Pain 2009;146(1):205–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. McCracken LM, MacKichan F, Eccleston C.. Contextual cognitive-behavioral therapy for severely disabled chronic pain sufferers: Effectiveness and clinically significant change. Eur J Pain 2007;11(3):314–22. [DOI] [PubMed] [Google Scholar]
- 27. Koffel E, Amundson E, Wisdom JP.. Exploring the meaning of cognitive behavioral therapy for insomnia for patients with chronic pain. Pain Med 2019;21(1):67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Day MA, Ward LC, Ehde DM, et al. A pilot randomized controlled trial comparing mindfulness meditation, cognitive therapy, and mindfulness-based cognitive therapy for chronic low back pain. Pain Med 2019;20(11):2134–48. [DOI] [PubMed] [Google Scholar]
- 29. Jensen MP, Ehde DM, Gertz KJ, et al. Effects of self-hypnosis training and cognitive restructuring on daily pain intensity and catastrophizing in individuals with multiple sclerosis and chronic pain. Int J Clin Exp Hypn 2010;59(1):45–63. [DOI] [PubMed] [Google Scholar]
- 30. Mendoza ME, Capafons A, Gralow JR, et al. Randomized controlled trial of the Valencia model of waking hypnosis plus CBT for pain, fatigue, and sleep management in patients with cancer and cancer survivors. Psychooncology 2017;26(11):1832–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Henschke N, Lorenz E, Pokora R, Michaleff ZA, Quartey JNA, Oliveira VC.. Understanding cultural influences on back pain and back pain research. Best Pract Res Clin Rheumatol 2016;30(6):1037–49. [DOI] [PubMed] [Google Scholar]
- 32. Lee K, Scandura TA, Sharif MM.. Cultures have consequences: A configural approach to leadership across two cultures. Leadership Quart 2014;25(4):692–710. [Google Scholar]
- 33. Houghton JD, Carnes A, Ellison CN.. A cross-cultural examination of self-leadership: Testing for measurement invariance across four cultures. J Leadersh Org Stud 2014;21(4):414–30. [Google Scholar]
- 34. Orhan C, Van Looveren E, Cagnie B, Mukhtar NB, Lenoir D, Meeus M.. Are pain beliefs, cognitions, and behaviors influenced by race, ethnicity, and culture in patients with chronic musculoskeletal pain: A systematic review. Pain Physician 2018;21(6):541–58. [PubMed] [Google Scholar]
- 35. Ferreira-Valente A, Sharma S, Torres S, et al. Does religiosity/spirituality play a role in function, pain-related beliefs, and coping in patients with chronic pain? A systematic review. J Relig Health. 2019; (doi: 10.1007/s10943-019-00914-7). [DOI] [PubMed] [Google Scholar]
- 36. Moher D, Liberati A, Tetzlaff J, Altman DG; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. PLoS Med 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283(15):2008–12. [DOI] [PubMed] [Google Scholar]
- 38. Jensen MP, Turner JA, Romano JM.. Pain belief assessment: A comparison of the short and long versions of the Survey of Pain Attitudes. J Pain 2000;1(2):138–50. [Google Scholar]
- 39. Goubert L, Crombez G, Van Damme S, Vlaeyen JW, Bijttebier P, Roelofs J.. Confirmatory factor analysis of the Tampa Scale for Kinesiophobia: Invariant two-factor model across low back pain patients and fibromyalgia patients. Clin J Pain 2004;20(2):103–10. [DOI] [PubMed] [Google Scholar]
- 40. Waddell G, Newton M, Henderson I, Somerville D, Main CJ.. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 1993;52(2):157–68. [DOI] [PubMed] [Google Scholar]
- 41. Cleland JA, Fritz JM, Childs JD.. Psychometric properties of the Fear-Avoidance Beliefs Questionnaire and Tampa Scale of Kinesiophobia in patients with neck pain. Am J Phys Med Rehabil 2008;87(2):109–17. [DOI] [PubMed] [Google Scholar]
- 42. Roelofs J, Goubert L, Peters ML, Vlaeyen JW, Crombez G.. The Tampa Scale for Kinesiophobia: Further examination of psychometric properties in patients with chronic low back pain and fibromyalgia. Eur J Pain 2004;8(5):495–502. [DOI] [PubMed] [Google Scholar]
- 43. French DJ, France CR, Vigneau F, French JA, Evans RT.. Fear of movement/(re)injury in chronic pain: A psychometric assessment of the original English version of the Tampa Scale for Kinesiophobia (TSK). Pain 2007;127(1):42–51. [DOI] [PubMed] [Google Scholar]
- 44. Moss-Morris R, Weinman J, Petrie KJ, Horne R, Cameron LD, Buick D.. The revised Illness Perception Questionnaire (IPQ-R). Psychol Health 2002;17(1):1–16. [Google Scholar]
- 45. Nicholas MK, Wilson PH, Goyen J.. Comparison of cognitive-behavioral group treatment and an alternative non-psychological treatment for chronic low back pain. Pain 1992;48(3):339–47. [DOI] [PubMed] [Google Scholar]
- 46. Nicholas MK. The Pain Self‐Efficacy Questionnaire: Taking pain into account. Eur J Pain 2007;11(2):153–63. [DOI] [PubMed] [Google Scholar]
- 47. Rosenstiel AK, Keefe FJ.. The use of coping strategies in chronic low-back-pain patients - relationship to patient characteristics and current adjustment. Pain 1983;17(1):33–44. [DOI] [PubMed] [Google Scholar]
- 48. Jensen MP, Turner JA, Romano JM, Strom SE.. The Chronic Pain Coping Inventory - development and preliminary validation. Pain 1995;60(2):203–16. [DOI] [PubMed] [Google Scholar]
- 49. Vowles KE, McCracken LM, Sowden G, Ashworth J.. Psychological flexibility in coping with chronic pain: Further examination of the Brief Pain Coping Inventory-2. Clin J Pain 2014;30(4):324–30. [DOI] [PubMed] [Google Scholar]
- 50. Jensen MP, Turner JA, Romano JM.. Changes in beliefs, catastrophizing, and coping are associated with improvement in multidisciplinary pain treatment. J Consult Clin Psychol 2001;69(4):655–62. [DOI] [PubMed] [Google Scholar]
- 51. Jensen MP, Turner JA, Romano JM.. Changes after multidisciplinary pain treatment in patient pain beliefs and coping are associated with concurrent changes in patient functioning. Pain 2007;131(1):38–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Flor H, Behle DJ, Birbaumer N.. Assessment of pain-related cognitions in chronic pain patients. Behav Res Ther 1993;31(1):63–73. [DOI] [PubMed] [Google Scholar]
- 53. von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP; for the STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. PLoS Med 2007;4(10):e296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Higgins JP, Green S.. Cochrane Handbook for Systematic Reviews of Interventions. Vol. 4 Hoboken, NJ: John Wiley & Sons; 2011. [Google Scholar]
- 55. Catley MJ, O'Connell NE, Berryman C, Ayhan FF, Moseley GL.. Is tactile acuity altered in people with chronic pain? A systematic review and meta-analysis. J Pain 2014;15(10):985–1000. [DOI] [PubMed] [Google Scholar]
- 56. Scott W, Arkuter C, Kioskli K, et al. Psychosocial factors associated with persistent pain in people with HIV: A systematic review with meta-analysis. Pain 2018;159(12):2461–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Harrison AM, McCracken LM, Bogosian A, Moss-Morris R.. Towards a better understanding of MS pain: A systematic review of potentially modifiable psychosocial factors. J Psychosom Res 2015;78(1):12–24. [DOI] [PubMed] [Google Scholar]
- 58. Ellis PD. The Essential Guide to Effect Sizes: Statistical Power, Meta-Analysis, and the Interpretation of Research Results. Cambridge, UK: Cambridge University Press; 2010. [Google Scholar]
- 59. Cohen J. A power primer. Psychol Bull 1992;112(1):155–9. [DOI] [PubMed] [Google Scholar]
- 60. Kent P, Mirkhil S, Keating J, Buchbinder R, Manniche C, Albert HB.. The concurrent validity of brief screening questions for anxiety, depression, social isolation, catastrophization, and fear of movement in people with low back pain. Clin J Pain 2014;30(6):479–89. [DOI] [PubMed] [Google Scholar]
- 61. Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP.. Associations between psychosocial factors and pain intensity, physical functioning, and psychological functioning in patients with chronic pain: A cross-cultural comparison. Clin J Pain 2014;30(8):713–23. [DOI] [PubMed] [Google Scholar]
- 62. Genet F, Autret K, Roche N, et al. Comparison of the repercussions of cLBP in four French-speaking countries. Ann Phys Rehabil Med 2009;52(10):717–28. [DOI] [PubMed] [Google Scholar]
- 63. Morris LD, Grimmer-Somers KA, Louw QA, Sullivan MJ.. Cross-cultural adaptation and validation of the South African Pain Catastrophizing Scale (SA-PCS) among patients with fibromyalgia. Health Qual Life Outcomes 2012;10:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Roelofs J, Sluiter JK, Frings-Dresen MH, et al. Fear of movement and (re)injury in chronic musculoskeletal pain: Evidence for an invariant two-factor model of the Tampa Scale for Kinesiophobia across pain diagnoses and Dutch, Swedish, and Canadian samples. Pain 2007;131(1):181–90. [DOI] [PubMed] [Google Scholar]
- 65. Roelofs J, van Breukelen G, Sluiter J, et al. Norming of the Tampa Scale for Kinesiophobia across pain diagnoses and various countries. Pain 2011;152(5):1090–5. [DOI] [PubMed] [Google Scholar]
- 66. Ruiz-Montero PJ, Van Wilgen CP, Segura-Jimenez V, Carbonell-Baeza A, Delgado-Fernandez M.. Illness perception and fibromyalgia impact on female patients from Spain and the Netherlands: Do cultural differences exist? Rheumatol Int 2015;35(12):1985–93. [DOI] [PubMed] [Google Scholar]
- 67. Sarda J Jr, Nicholas MK, Asghari A, Pimenta CA.. The contribution of self-efficacy and depression to disability and work status in chronic pain patients: A comparison between Australian and Brazilian samples. Eur J Pain 2009;13(2):189–95. [DOI] [PubMed] [Google Scholar]
- 68. Taras V, Steel P, Kirkman BL.. Does country equate with culture? Beyond geography in the search for cultural boundaries. Manage Int Rev 2016;56(4):455–87. [Google Scholar]
- 69. Darlow B, Fullen BM, Dean S, Hurley DA, Baxter GD, Dowell A.. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: A systematic review. Eur J Pain 2012;16(1):3–17. [DOI] [PubMed] [Google Scholar]
- 70. Sharma S, Jensen MP, Pathak A, Sharma S, Pokharel M, Abbott JH.. State of pain research in Nepal: A systematic scoping review. Pain Reports 2019;4(6):e788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Sousa VD, Rojjanasrirat W.. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline. J Eval Clin Pract 2011;17(2):268–74. [DOI] [PubMed] [Google Scholar]
- 72. Edwards AL. The Social Desirability Variable in Personality Assessment and Research. Ft Worth, TX: Dryden Press; 1957. [Google Scholar]
- 73. Sharma S, Jensen MP, Moseley GL, Abbott JH.. Results of a feasibility randomised clinical trial on pain education for low back pain in Nepal: The Pain Education in Nepal-Low Back Pain (PEN-LBP) feasibility trial. BMJ Open 2019;9(3):e026874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Sharma S, Jensen MP, Moseley GL, Abbott JH.. Pain education for patients with non-specific low back pain in Nepal: Protocol of a feasibility randomised clinical trial (PEN-LBP Trial). BMJ Open 2018;8(8):e022423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Orhan C, Cagnie B, Favoreel A, et al. Development of culturally sensitive Pain Neuroscience Education for first-generation Turkish patients with chronic pain: A modified Delphi study. Musculoskelet Sci Pract 2019;39:1–9. [DOI] [PubMed] [Google Scholar]
- 76. Brady B, Veljanova I, Schabrun S, Chipchase L.. Integrating culturally informed approaches into the physiotherapy assessment and treatment of chronic pain: Protocol for a pilot randomised controlled trial. BMJ Open 2018;8(7):e021999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Ho PC, Johnson MH.. Behaviours and beliefs about pain and treatment among Chinese immigrants and New Zealand Europeans. N Z Med J 2013;126(1370):10–22. [PubMed] [Google Scholar]
- 78. Goodwin R, Plaza SH.. Perceived and received social support in two cultures: Collectivism and support among British and Spanish students. J Soc Pers Relat 2000;17(2):282–91. [Google Scholar]
- 79. Michell J. Is psychometrics pathological science? Measur Interdiscipl Res Perspect 2008;6(1–2):7–24. [Google Scholar]
- 80. Michell J. Quantitative science and the definition of measurement in psychology. Brit J Psychol 1997;88(3):355–83. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.