Abstract
Physical and mental stressors on radiologists can result in burnout. Although current efforts seek to target the issues of burnout and stress for radiologists, the impact of their physical workspace is often overlooked. By combining evidence-based design, human factors, and the architectural concept of the Eudaimonia Machine, we have developed a redesign of the radiology reading room that aims to create an optimal workspace for the radiologist. Informed by classical principles of well-being and contemporary work theory, Eudaimonia integrates concerns for individual wellness and efficiency to create an environment that fosters productivity. This layout arranges a work environment into purposeful spaces, each hosting tasks of varying degrees of intensity. The improved design addresses the radiologist’s work requirements while also alleviating cognitive and physical stress, fatigue, and burnout. This new layout organizes the reading room into separate areas, each with a distinct purpose intended to support the range of radiologists’ work, from consultation with other health care providers to reading images without interruption. The scientific principles that undergird evidence-based design and human factors considerations ensure that the Eudaimonia Radiology Machine is best suited to support the work of the radiologists and the entire radiology department.
Key Words: Burnout, evidence-based design, human factors, reading room
Introduction
Radiologists working in the hospital or outpatient imaging center spend the majority of their time in the reading room. Although multiple factors contribute to the personal and professional satisfaction of radiologists, the physical environment can have a significant impact on their ability to perform key activities. Poor environmental design can hinder performance by affecting physical well-being (eg, eye strain, repetitive stress disorders), cognitive function (eg, distraction, error), and operational efficiency (eg, inefficiency, wasted time).
The physical toll and inefficiency associated with poor ergonomic and workflow design has been documented [1,2], but few publications explore approaches and solutions to the negative effects of poorly designed reading rooms. This lack of discussion is not because of a lack of architectural and engineering theory and practice—disciplines that could be applied to designing an optimal reading room. Evidence-based design and human factors engineering are two such approaches that have informed specific models of environmental design that can optimize human cognitive performance.
The increasing rate of burnout among medical professionals is a source of concern for hospital administrators and professional societies [3,4], which is particularly high within radiology [5,6]. Burnout, like distraction, has been linked to increased medical error [4], clinician job dissatisfaction, and turnover [7]. In addition, radiology trainees and fellows experience significantly higher rates of burnout compared with their peers in other specialties, potentially because of the unique demands of radiology practice [5,8,9]. Because radiologists spend much of their time in the reading room, it follows that the space’s layout should proactively facilitate the work requirements and the well-being of the people working there.
The authors recognized the detractions of a poorly designed reading room and sought to design a reading room that would serve the needs of our institution’s Department of Radiology. This article invites radiology departments to consider the problems of distraction and burnout and suggests that these problems could be addressed by the design of the reading room environment. It then presents an architectural case study of the multi-stakeholder, iterative, and theory- and evidence-informed approach to designing an optimal reading room environment for a large academic pediatric radiology department. Finally, it acknowledges that the coronavirus disease 2019 (COVID-19) pandemic has dramatically changed the landscape and the nature of work and workflow for radiology departments and suggests future adaptations to the reading room environment based on evolving infectious disease control and occupational health and safety guidelines.
Why Good Design of Reading Rooms Matters
Physical Impact of Bad Design: Repetitive Stress Disorders
The architectural features of a workplace will affect both the work and the worker—for radiologists, the work environment is most often the reading room. Reading room design can have a significant impact on the accuracy, productivity, and general health of the radiologists who work there [10]. During a typical shift, a radiologist may spend over 8 hours at a workstation, interacting with a keyboard and mouse to retrieve and manipulate images [2]. This prolonged time performing repeated motions contributes to physical injuries: approximately one-third of radiologists suffer from cubital or carpal tunnel syndrome [10], neck and low back pain [2], and other forms of repeated stress injuries. Some departments have implemented interventions that give the radiologist the ability to adjust the furniture, temperature, and work space lighting to their own personal preferences [2]. Though helpful, these are surface-level fixes. Deliberate and targeted interventions can resolve the greater environmental design issues that affect quality of work in the reading room.
Operational and Safety Impact of Bad Design: Inefficiency and Error
Work space design can influence the risk of distraction and interruption. Interruption of primary work tasks afflicts all workers, no matter the field. In health care, however, interruption can be particularly dangerous, introducing the risk of error and decreasing overall performance [1]. Over time, interruptions cause chronic inefficiency, creating a feedback loop of distraction and poor performance, resulting in burnout. For the radiologist already under pressure to deliver results rapidly, every telephone call and consultation means less time interpreting and reporting studies. Radiologists may also attend administrative meetings while also engaged in clinical duty. The pressures of an increasing work queue and the expectation to deliver rapid results have been linked to increased medical error [4]. In a specialty so heavily dependent on attention to detail when interpreting studies, distractions can lead to serious diagnostic errors, which are recognized as the leading basis for malpractice cases against radiologists [11].
Cognitive Impact of Bad Design: Distraction, Error, Burnout
For the radiologist, the work most vulnerable to distraction and error is the task of reading images. Viewing and interpreting images from a study and then generating a report places a high cognitive demand on the radiologist. Distraction is recognized to be a potential cause of errors [12], and designing distraction-free spaces has been shown to protect against distraction [13]. Disruptions or distractions delay completion of a task; after each interruption, the radiologist must refocus on interpreting the images and dictating, and if fully disengaged, find where he or she left off. A recent study of radiologists and their workflow and efficiency found that most interruptions forced the radiologist to completely disengage from the current task [1].
Physician Well-Being Impact of Bad Design: The Burnout Factor
Clinician burnout is gaining significant attention in the medical community. Radiologists experience higher rates of burnout than clinicians in other specialties, resulting in talent loss as skilled radiologists exit clinical practice [3,6,8]. Factors like burnout are often exacerbated by increasing pressure for radiologists to report results quickly; however, expectations of faster turnaround times can overburden the cognitive and physical limitations of the radiologist [14]. Furthermore, a typical radiology workflow includes consultations with nonradiology clinicians, technologists, and other clinical support staff [10]. These consultations take the radiologist away from the core image interpretation tasks but are often conducted next to other radiologists continuing to read studies. An optimally designed reading room separates the consultation activities from the image interpretation tasks so that radiologists can choose the environment best suited to the task.
Theory and Practice Can Inform Good Reading Room Design
Evidence-Based Design
The principles of environmental design reach beyond the reading room. A well-designed health care environment can contribute to a positive patient and clinician experiences. Among scientists, “design” is often relegated to the realm of the subjective, dismissed as a matter of opinion and considered not essential to well-being. But evidence-based design applies empirical methods to establish a framework and financial justification for designing better health care environments [15]. More and more, hospitals are motivated to enhance the quality of patient care by investing in a holistic patient experience [15]. This drive to redesign physical environments also attempts to address the increasing epidemic of clinician burnout [3,8]. Unfortunately, without consideration of all of the necessary activities and interactions that a health care environment must support, many redesign efforts fail to deliver the desired outcomes. Evidence-based design applies a disciplined approach to environmental changes, supporting both the patient and the provider.
Human Factors Engineering
Human factors engineering improves health care environments by employing evidence-based design. This discipline is focused on understanding how complex systems function while being run by imperfect human operators [16]. Human factors practitioners have found that radiologists are experiencing stress from workplace factors that drastically impact their wellness [3,10]. The interplay between human elements, technology, and environment can inform the design of a balanced work system that supports the human worker and establishes “guardrails” that make mistakes less likely to occur [17,18]. These redesigned work systems are custom-made, uniquely suited to the needs of its workers. A subset of human factors engineering, participatory ergonomics, invites the people for whom the system is being designed to be stakeholders in the planning of the workplace [19]. Using this approach, the radiologists themselves are actively engaged in the design process of their own work space, circumventing several initial iterations of design and inviting buy-in from stakeholders.
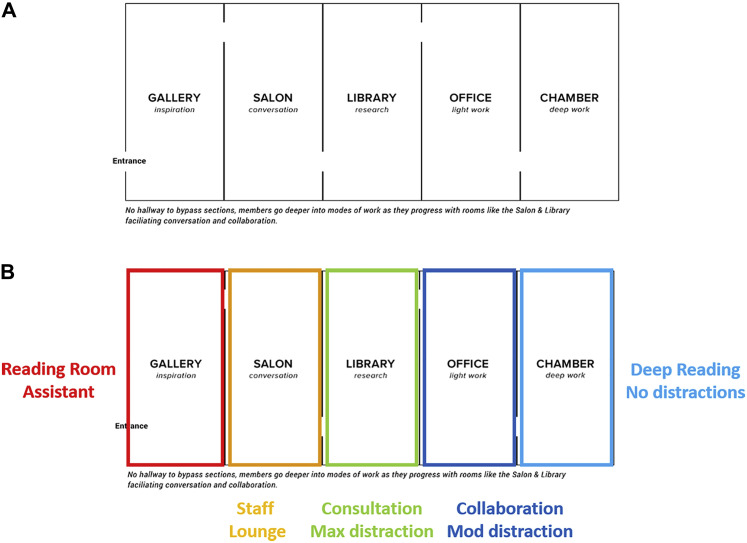
The Eudaimonia Machine
Evidence-based design and human factors engineering are two routes to the same destination: a work environment that promotes productivity and wellness. One approach originates from architect David Dewane, who designed a construct he named the Eudaimonia Machine [20]. We invited Mr Dewane as a visiting architect to consult on our department’s initiative to redesign our reading room. The intent of the Eudaimonia Machine is to facilitate focused, or “deep,” work. Coined by computer scientist and author Cal Newport, the term “deep work” describes a state of maximal focus, creativity, and productivity [21], which is increasingly difficult to achieve in our distraction-filled world. Newport posits that in our work environments fragmented by social media, e-mail, and meetings, the ability to perform deep work has become a measure of success—a new IQ. Instead of a scattered and incidental approach to the work space, the Eudaimonia Machine is linear and purposeful, each of its five sequential rooms meeting the needs of specific work tasks. The gallery is meant for inspiration; the salon for socialization, inspiration, and fostering creativity; the library for research; the office for light work; and finally, the chamber for deep work (Fig. 1 A). Each room follows the other in a sequential progression with one entrance and one exit.
Fig 1.
(A) The Eudaimonia Machine, as described by architect David Dewane, is a sequential progression through multiple spaces, each designed for different activities and levels of socialization and interaction. The intent is ultimately to prepare individuals to enter the “chamber” for deep work. (B) The Eudaimonia Machine adapted for the purposes of designing an activity-based reading room. The reading room assistants are positioned at the front of the space (gallery) to both welcome and triage visitors to the reading room; the staff lounge (salon) is for conversation and socialization; the consultation space (library) is for a body and neuroradiology attending radiologist and trainee team to consult with teams visiting the reading room in person; the collaboration space is where most of the day to day reading is performed and where attending radiologist-trainee interaction is facilitated; the deep reading space (chamber) is meant for highly complex studies that require sustained periods of uninterrupted focus.
Case Study and Lessons Learned
Eudaimonia Machine Informs Basic Design
In the redesign of our reading room, we adapted the Eudaimonia Machine concept for the specific activities and needs of those who work there (Fig. 1B). We envisioned a series of spaces within the reading room: The gallery, or front-facing room, serves as the space for reading room assistants, allowing them to welcome and direct consulting physicians to the correct workstation, and to perform other administrative tasks. The salon serves as a staff lounge for conversation and socialization among radiologists; here they can recharge with the support of coffee or tea and be inspired by historical photos of the department’s history. The library is designated as the consultation space in which neuroradiology and body attending radiologist-trainee teams help consulting physicians with patient care. The office is the space for only moderate distraction, where the attending radiologists and trainees spend most of their time. The open floor plan facilitates line of sight and collaborative interaction and teaching. Finally, the chamber serves as a distraction-free “deep reading” space, its quiet and isolation enabling radiologists to interpret the images of patients with highly complex conditions.
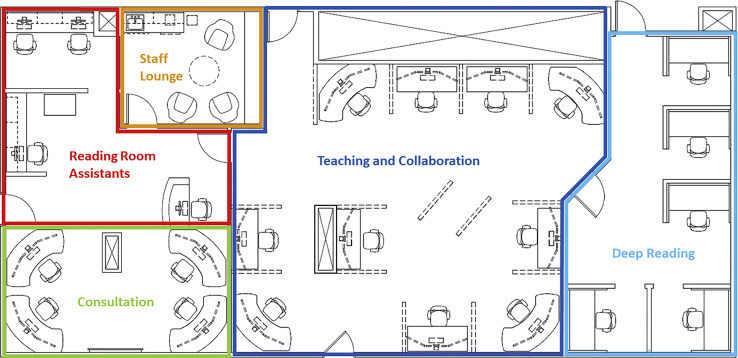
Translating the Eudaimonia reading room from an architectural concept to a final floor plan was an iterative process. Multiple floor plans were developed and reviewed by the combined architectural and radiology department design teams (Fig. 2 ). The floor plan was translated into a full-scale mock-up constructed of a steel framework and foam core walls and outfitted with representative furniture.
Fig 2.
(A) Iterative floor plan. The first version of the reading room was critiqued for not having enough space in the consult area to accommodate body and neuroradiology attending radiologist and trainee pairs. The space did not require both a staff lounge and a conference room; removing the conference room provided more space for an expanded consult and reading room assistant space. The placement of walls and position of workstations within the collaboration space impeded line of sight and situational awareness, both of which were deemed necessary to encourage attending radiologist and trainee interaction and awareness of impromptu discussions with other radiologists about interesting patients and imaging findings. (B) Revised floor plan featured increased space for two reading room assistants upon entry to the reading room, expanded consult space to accommodate four radiologists (body and neuroradiology attending radiologist and trainee pairs), and a staff lounge with sink and casual seating. Deep reading room was expanded to enable seating for nine radiologists.
Human Factors Informs Ergonomics
Participatory ergonomics were employed as a total of eight escorted “field trips” with a total of 51 participants were arranged to ensure that a full complement of stakeholders had a chance to walk through the space and provide feedback (Fig. 3 ). Radiology stakeholders visited the site of the full-scale mock-up housed within the hospital property. Architects and project managers provided tours and took notes based on stakeholder comments. Although constructing a full-scale mock-up is a costly and time-intensive endeavor, the long-term value of this exercise cannot be overestimated. Each stakeholder visit resulted in a new iteration of the design: Walls were shifted, room sizes were adjusted, and the practical ability of the space to meet the designated functions was tested and improved. Specific changes included adjusting the location of the reading room assistants to be in direct line of sight upon entering, shifting furniture orientation and decreasing the size of the chamber, and arranging modality-focused services closer to the technologist access doors.
Fig 3.
Mock-up tours. A full-scale mock-up was built out of a steel framework and foam core panels. Visits were facilitated by project architects and designers. A total of eight visits including 51 multidisciplinary stakeholders (attending radiologists and trainee radiologists, reading room assistants, technologists, administrative staff, and research staff) were organized to enable staff to experience the spaces and ask questions of the architects and each other. Light furniture served as stand-ins for workstations and ancillary furniture and could be easily shifted to test usability of the spaces.
Surveys and Focus Groups Provide Evidence
To record stakeholder feedback and to support our case for redesigning the reading room with objective evidence, we designed a study using statistical and qualitative methods to assess how a radiology reading room environment could best meet the needs of referring clinicians, trainees, and attending radiologists.
Multistakeholder Surveys
This assessment was conducted at our institution and approved by the institutional review board, which determined that it does not qualify as human subject research. To gather feedback for this project, surveys were distributed to the respective groups regarding their experiences with the current radiology reading room. The survey questions solicited information about each participant’s role, level of interaction with colleagues, and suggestions for improving the reading room.
Participants were recruited from our institution’s referring clinicians and our radiology department, which is comprised of 42 radiologists, 14 clinical fellows, and resident physicians. Several referring clinicians interact with the department’s attending radiologists and trainees on a monthly basis.
Electronic surveys were e-mailed to potential participants in February 2019. Paper surveys for referring clinicians were placed in the reading rooms. Participants who completed the survey were entered into a drawing to receive a $30 gift card. Survey feedback was collected and managed using REDCap electronic data capture tools hosted by our institution [22]. The survey questions were customized to be applicable to each role and utilized a Likert scale.
Survey results were assessed for normality using the Shapiro-Wilk test to determine the descriptive analysis plan. After determining that all responses rejected the null hypothesis of normality (P < .05), it was most appropriate to summarize the data by median and interquartile range [23]. All analyses were conducted in R Studio version 1.2 (Table 1, Table 2, Table 3 ) [24].
Table 1.
Demographic characteristics of the survey sample (n = 98)
| Role (n,%) | Full Sample (n = 98)∗ | Body Reading Room (n = 85) | Neuroradiological Reading Room (n = 6) |
|---|---|---|---|
| Attending radiologist | 31 (32) | 28 (33) | 3 (50) |
| Trainee | 22 (22) | 20 (24) | 2 (33) |
| Referring clinician | 45 (46) | 37 (43) | 1 (17) |
Body and neuroradiological may not sum to the full sample, as referring clinicians were allowed to answer both.
Table 2.
Survey responses from attending radiologists, trainees, and referring clinicians
| Survey Question | Combined Reading Rooms, Median (p25, p75) | Body Reading Room, Median (p25, p75) | Neuroradiological Reading Room, Median (p25, p75) |
|---|---|---|---|
| Attending radiologist | |||
| The reading room meets my interpretation needs. | 4.0 (2.5, 4.0) | 4.0 (2.75, 4.0) | 3.0 (2.5, 4.0) |
| The reading room meets my consultation needs. | 4.0 (2.0, 4.0) | 4.0 (2.0, 4.0) | 4.0 (2.5, 4.5) |
| The reading room meets my teaching needs. | 4.0 (3.0, 4.0) | 4.0 (3.0, 4.0) | 4.0 (2.0, 4.5) |
| The reading room is distracting. | 4.0 (3.0, 5.0) | 4.0 (3.0, 5.0) | 3.0 (2.5, 4.0) |
| The reading room facilitates awareness of trainee’s educational or workload assistance needs. | 3.0 (2.0, 4.0) | 3.0 (2.0, 4.0) | 4.0 (3.0, 4.0) |
| Trainees | |||
| The reading room supports independent reading. | 1.0 (1.0, 1.0) | 1.0 (1.0, 1.0) | 1.0 (1.0, 1.0) |
| The reading room facilitates interaction with and access to my attending radiologist. | 5.0 (4.0, 5.0) | 5.0 (4.0, 5.0) | 5.0 (5.0, 5.0) |
| The reading room is distracting. | 2.0 (2.0, 4.0) | 2.0 (2.0, 3.25) | 2.0 (2.0, 4.0) |
| Do you feel the reading room facilitates your attending radiologist’s awareness of your workload? (Yes or no) | 86.3% (Yes, n = 19) 15.8% (No, n = 3) |
85.0% (Yes, n = 17) 17.6% (No, n = 3) |
100.0% (Yes, n = 2) 0.0% (No, n = 0) |
| Referring clinicians | |||
| The reading room is welcoming. | 5.0 (4.0, 5.0) | 5.0 (4.0, 5.0) | N/A |
| It was easy to find a radiologist to help me. | 5.0 (5.0, 5.0) | 5.0 (5.0, 5.0) | N/A |
| The radiologist seemed to have enough time to help me. | 5.0 (5.0, 5.0) | 5.0 (5.0, 5.0) | N/A |
| The in-person consultation was useful. | 5.0 (5.0, 5.0) | 5.0 (5.0, 5.0) | N/A |
Responses were based on a 5-point Likert scale (5 = strongly agree, 4 = somewhat agree, 3 = neither agree nor disagree, 2 = somewhat disagree, 1 = strongly disagree. N/A = not applicable.
Table 3.
Qualitative feedback from survey distributed to attending radiologists, trainees, and referring clinicians
| Theme | Comment | Role |
|---|---|---|
| Suggestions for improvement | Space utilization not optimal, consultation setup not effective—need big screen for demo, improved lighted signs with modality and maybe screens with names of attending radiologists on service, availability of water filter, coffee machine, better seats different for those on service and visitors. | Attending radiologist |
| Improve line of sight so that radiologists are aware of each other’s presence and make it easier for attending radiologist and trainee interaction. Make it easier for visiting clinicians to understand who to speak with for consultation. | Attending radiologist | |
| (1) Change public access to one door—eg, off main hallway. (2) Move Reading Room Assistants to site of first access by walk in visitors for triage. (3) Create dedicated consultant role and put them close to where clinicians enter. (4) If possible, rearrange workstations so staff and trainees can see one another rather than having to stand up and walk around to look at nearby workstations or calling to one another over divider walls (I admit I am guilty of the later). | Attending radiologist | |
| I would remove the walls in the center of the reading room to create an open concept. This will create space for additional workstations that can be positioned in a way similar to fluoroscopy or cardiothoracic. However, the amount of discussion that goes on in an open concept reading room may be regarded as distracting to some. But it also allows easy discussion of complex cases with others in the vicinity. | Trainee | |
| I like the idea of multiple zones where people who are trying to focus are insulated from interruptions by technologists and coworkers. I love the current openness of our reading room, and that we can easily chat with colleagues and clinicians. But sometimes it’s difficult to focus without being dismissive of others. | Trainee | |
| Clear signage of whom to talk to, areas to talk without disturbing others. | Referring clinician | |
| The physical space is too small and not conducive for reviewing images, teaching for clinical teams. | Referring clinician | |
| Physical availability of attending radiologists for trainees | Walls block view of attending radiologists. Sometimes attending radiologists sit quite remote to fellow, which creates even more physical distance. Hard to find attending radiologists to have additional opinions on complex cases. | Trainee |
| Workstations are isolated and private enough for concentration and focus without significant distraction or disruption while having colleagues and attending radiologists immediately available for support. | Trainee | |
| The sections where there are four desks (fluoro and chest) limit visibility between the desks and thus easy interaction between two and attending radiologist. | Trainee |
Multistakeholder Focus Groups
As a follow-up to survey results, we gathered more information about trainees’ and attending radiologists’ experience in the reading room through focus groups. A focus group with trainees was conducted in January 2020, and a focus group with attending radiologists was conducted in February 2020. The questions for the focus group discussion were similar to those in the survey; however, the group environment elicited further discussion of their experience. Each focus group was audio-recorded and transcribed. Direct content analysis of the transcripts was conducted to identify emergent themes (Table 4 ). The main themes that were identified include praise for current environment, practical suggestions for improvement, and concerns that potential redesign could impact interaction between attending radiologists and trainees. The authors interpreted the positive feedback on the current reading room as reflecting the lack of a better model. Radiologists were not able to point out the deficiencies in their work environment because they had not experienced anything better.
Table 4.
Qualitative feedback from focus groups with 6 attending radiologists and 17 trainees
| Theme | Comment | Role |
|---|---|---|
| High praise about current environment | The side by side I think is definitely more conducive to teaching. | Trainee |
| Some of the positive things are that there are lots of people around. You can easily confer with others. | Attending radiologist | |
| The nice thing about this reading room that I have not seen at any other place I’ve been where there’s a main reading room is the fact that the doors actually exit into the fluoro, ultrasound, etc. | Trainee | |
| Currently the partitions that we have, especially in the body reading room, are you know, good-sized partitions. | Attending radiologist | |
| Suggestions for improvement | I think the ambient lighting, the newer work stations have, kind of coupled with a dimmer I think would be a nice feature. | Trainee |
| So in a perfect world we’d be doing a much better job of getting all the phone calls triaged to the reading room assistant. | Trainee | |
| You can put sound damping materials in the ceiling, in the cubicles, I mean, there are ways to engineer a room to be quieter. | Trainee | |
| In the main reading room when you walk in you have a very large 3-D work space. It breaks up the whole reading room. I suggest taking this out. | Attending radiologist | |
| So to me the perfect situation is partitioned rooms with doors that open and close. | Trainee | |
| To have a concierge-type person who has enough knowledge that you ask where to go and who you want to see and they have the skills to bring up the images in a quieter area and direct you there. | Attending radiologist | |
| The problem with neuro reading room, which is a subspecialty reading room, are the high dividers such that you won’t see anybody in the reading room at any point, so you don’t know who is physically there. Need dividers but appropriately sized ones. | Trainee | |
| The temperature is up and down. There are [sic] a certain point of the day that it’s really cold. Need a functional thermostat. | Trainee | |
| Perhaps one thing if we section six spaces in which, maybe not physical walls, but at least good glass walls, so everybody can see what you’re doing, but not necessarily hear you. Also, without doors, just enough that there is a section for everybody so you are not disruptive, just from your tone of voice. | Attending radiologist | |
| Concern about potential redesign | As a trainee, if I had to go speak with an attending radiologist about a difficult case and they were in the deep learning area, I think that would be enough of a deterrent. It would be the awkwardness that would prevent me from seeking out that attending radiologist for support. | Trainee |
| Neuro and body sitting next to each other in a big room I would say, no, I would rather have the same specialty radiologist sit next to me than a different subspecialty radiologist. | Attending radiologist | |
| So my question is deep reading. Given that in neuro, single person deep reading rarely happens, if at all. So I don’t know how many shifts or assignments are deep reading friendly and would utilize the space. | Attending radiologist | |
| My fear of sectioning off the consultation is I think it’s sort of taking away a lot of teaching moments because sometimes when the team comes down those are I think the most educational. | Attending radiologist |
Final Eudaimonia Reading Room Design
Drawing on the Eudaimonia concept, the redesigned room has been organized into the various stages and spaces of focus or distraction and adjusted for the specific functions of the radiology and hospital staff who will make use of it (Fig. 4 ). In this revised design, the reading room assistants now work at the front of the room near the entrance in the gallery. This enables them to greet health care provider teams and provide them with administrative help. For the radiologists, the staff lounge is the salon, providing a place to socialize and relax. For visiting clinicians, the consultation room functions as the library directly to the right of the main entrance. Here, visiting clinicians can consult with a neuroradiology and body attending radiologist-trainee pair. Stationed in the consultation room, the radiologists expect to be interrupted from their nonconsultative responsibilities. The teaching and collaboration space (office) is a large “ballroom” with acoustic insulation to minimize noise, but with unobstructed line of sight allowing attending radiologists and trainees to interact with each other. This moderate distraction space also provides convenient access to fluoroscopy technologists and sonographers, but these doors will not be accessible to nontechnologist staff. Finally, the deep reading room is the chamber, designated for radiologists who need a distraction-free space to focus and perform their most cognitively demanding interpretation.
Fig 4.
Final floor plan. Two major changes were made for the final design. First, the reading room assistant space was expanded to include space for processing CD requests for patients; a greeting desk was positioned as the first thing visitors would see upon entering the reading room. Second, the deep reading space was reduced from nine to five workstations; in both full-scale mock-up tours and during focus group conversations, trainees expressed concerns that attending radiologists could be tempted to spend inordinate amounts of time in this space (“hiding”). Limited seating (and signage describing a deep reading protocol) is meant to encourage attending radiologists to use the space for the intended purpose of deep reading of complex cases and to return to the teaching and collaboration space when finished.
Reading Room Design Considerations in the Age of COVID-19
The needs of our department have shifted in response to the COVID-19 pandemic. The National Institute for Occupational Safety and Health presents a hierarchy of controls for hazard exposure. The model itself (Fig. 5 ) comes from the prevention-through-design program for worker safety led by National Institute for Occupational Safety and Health [25]. Within the hierarchy, personal protective equipment is considered the last line of defense and the least effective [25,26]. Most effective is the elimination of the hazard, followed by substitution, which may mean a change of materials to eliminate the hazard. However, when dealing with COVID-19, elimination and substitution are not feasible. The next two levels in the hierarchy are engineering controls and administrative controls, both of which could inform the design of the radiology reading room.
Fig 5.
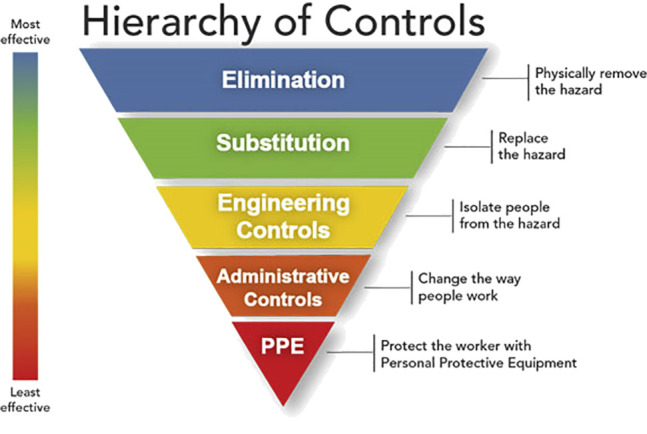
National Institute for Occupational Safety and Health Hierarchy of Controls (from National Institute for Occupational Safety and Health Workplace Safety and Health, 2015 [25]).
Engineering controls can be incorporated as a contingency of the reading room design. During the current COVID-19 pandemic, we have been forced to restructure our work environments to enable social distancing in spaces that were never designed for it. Restricting access and traffic through the reading room provides a layer of engineering control in the environment for those working in the space. Similarly, a design that facilitates and encourages a structured flow of movement through the space may provide additional safety (see systematic layout planning in Benitez et al [27]). Designing consultation spaces near the entrance to the reading room would prevent nonradiology staff from entering the reading room itself, reducing exposure risks, disruptions, and distractions. Modular barriers can section off work areas to help reduce the risk of person-to-person transmission among radiologists.
Administrative controls minimize the hazards in the workplace by changing the way the work is performed. For example, in our initial response to the COVID-19 pandemic we determined the minimum number of radiologists to be physically present in the department and implemented a rotation schedule alternative work arrangements including reduced staffing and remote teleradiology. Reading room access was limited to only a set number of scheduled staff, and the rooms were deep-cleaned nightly.
Limitations
This study was based on the premise that our reading room was scheduled to be renovated in the near future, and we chose to adopt a multidisciplinary, evidence-based approach to the process. We were fortunate to secure funding for this remodeling project and to have access to shell space in a separate building in which to construct our full-scale model. We recognize that limited resources and funding would constrain the ability of many departments to replicate our approach to iterative design.
In conclusion, the reading room is a critical environment for radiologists and consulting physicians who depend on them. The design of this space can hamper or support the cognitive and physical performance and the emotional well-being of radiologists in their consulting, teaching, and interpreting responsibilities. Although the literature has documented the negative consequences of poorly designed reading room environments, there are few descriptions of how to design a reading room environment that will optimize radiologists’ performance and experience.
Although not all practices or institutions may currently have the budget and freedom of a nearby building to construct a walk-through, full-scale model, or even consider a complete renovation, many of these activities could be conducted in lower cost-digital formats utilizing computer graphics or virtual reality environments. In addition, although we had the freedom to consider a design that could be executed as part of a full renovation, other institutions could rearrange their reading room and redesignate spaces for deep work utilizing existing space and furniture. The ideal Eudaimonia design involves well-defined chambers; however, the ultimate goal is to control which areas of the reading room can accommodate distractions and which areas should be restricted to deep work.
The COVID-19 pandemic requires additional infectious disease control and occupational health considerations for environmental design to ensure the safety of radiologists and visitors to the reading room. At this time, we have not started construction of the redesigned reading room. We have implemented COVID-19 interventions in the existing space. We have placed directional arrows directing previously free-flowing, multidirectional traffic into a linear flow-through, also facilitated by signage and locked exit-only doors. We have placed markers indicating locations to stand for consultation behind all workstations with 6 feet of distance from the radiologist. Finally, we have installed plastic chains on open hooks, providing additional physical barrier to unwanted movement in the space. The plastic chains block normal traffic but are not an impediment to emergency or necessary movement.
A combination of evidence-based design, human factors engineering, and the Eudaimonia Machine can guide the design of a reading room that not only actively supports the work of the radiologists but also fosters their continued well-being.
Take-Home Points
-
▪
Reading rooms are a vital part of the radiology work flow, but their design and layout are often an afterthought.
-
▪
Designing the reading room to facilitate the different types of work that take place in it can help reduce distractions and errors.
-
▪
A combination of evidence-based design, human factors, and Eudaimonia architectural concepts can inform the design of a purposeful, effective reading room.
-
▪
The Eudaimonia Machine is an architectural concept featuring different designated areas that have specific distraction potential thresholds and are intended for specific intensity of work tasks to be completed inside. The concept emphasizes purposeful work support and the wellness of the worker inside.
-
▪
Burnout among radiologists may be mitigated by a physical work environment that promotes wellness.
Footnotes
Mr Dewane reports personal fees from The Children’s Hospital of Philadelphia. The other authors state that they have no conflict of interest related to the material discussed in this article. Dr Larsen, Ms Hailu, Ms Sheldon, Ms Ginader, Ms Bodo, Mr Dewane, Mr Finley, and Dr Sze are nonpartner, non–partnership track employees. Dr Degnan is on a partnership track.
Additional Resources
Additional resources can be found online at: https://doi.org/10.1016/j.jacr.2020.09.041.
Additional Resources
References
- 1.Ratwani R.M., Wang E., Fong A., Cooper C.J. A human factors approach to understanding the types and sources of interruptions in radiology reading rooms. J Am Coll Radiol. 2016;13:1102–1105. doi: 10.1016/j.jacr.2016.02.017. [DOI] [PubMed] [Google Scholar]
- 2.Sze G., Bluth E.I., Bender C.E., Parikh J.R. Work-related injuries of radiologists and possible ergonomic solutions: recommendations from the ACR Commission on Human Resources. J Am Coll Radiol. 2017;14:1353–1358. doi: 10.1016/j.jacr.2017.06.021. [DOI] [PubMed] [Google Scholar]
- 3.Parikh J.R., Wolfman D., Bender C.E., Arleo E. Radiologist burnout according to surveyed radiology practice leaders. J Am Coll Radiol. 2020;17(1 Part A):78–81. doi: 10.1016/j.jacr.2019.07.008. [DOI] [PubMed] [Google Scholar]
- 4.Shanafelt T.D., Balch C.M., Bechamps G. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995–1000. doi: 10.1097/SLA.0b013e3181bfdab3. [DOI] [PubMed] [Google Scholar]
- 5.Haber M.A., Gaviola G.C., Mann J.R. Reducing burnout among radiology trainees: a novel residency retreat curriculum to improve camaraderie and personal wellness—3 strategies for success. Curr Probl Diagn Radiol. 2020;49:89–95. doi: 10.1067/j.cpradiol.2019.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Moskowitz P.S. Gathering storm clouds suggest the need for a culture change in radiology: radiologist-centered imaging. Radiology. 2015;276:3–7. doi: 10.1148/radiol.2015142738. [DOI] [PubMed] [Google Scholar]
- 7.Dewa C.S., Jacobs P., Thanh N.X., Loong D. An estimate of the cost of burnout on early retirement and reduction in clinical hours of practicing physicians in Canada. BMC Health Serv Res. 2014;14:254. doi: 10.1186/1472-6963-14-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dyrbye L., Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ. 2016;50:132–149. doi: 10.1111/medu.12927. [DOI] [PubMed] [Google Scholar]
- 9.Mendoza D., Bertino F.J. Why radiology residents experience burnout and how to fix it. Acad Radiol. 2019;26:555–558. doi: 10.1016/j.acra.2018.08.009. [DOI] [PubMed] [Google Scholar]
- 10.Hugine A., Guerlain S., Hedge A. User evaluation of an innovative digital reading room. J Digit Imaging. 2012;25:337–346. doi: 10.1007/s10278-011-9432-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Whang J.S., Baker S.R., Patel R., Luk L., Castro A. The causes of medical malpractice suits against radiologists in the United States. Radiology. 2013;266:548–554. doi: 10.1148/radiol.12111119. [DOI] [PubMed] [Google Scholar]
- 12.Rivera-Rodriguez A.J., Karsh B.-T. Interruptions and distractions in healthcare: review and reappraisal. Qual Saf Health Care. 2010;19:304–312. doi: 10.1136/qshc.2009.033282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anthony K., Wiencek C., Bauer C., Daly B., Anthony M.K. No interruptions please: impact of a no interruption zone on medication safety in intensive care units. Crit Care Nurse. 2010;30:21–29. doi: 10.4037/ccn2010473. [DOI] [PubMed] [Google Scholar]
- 14.Waite S., Kolla S., Jeudy J. Tired in the reading room: the influence of fatigue in radiology. J Am Coll Radiol. 2017;14:191–197. doi: 10.1016/j.jacr.2016.10.009. [DOI] [PubMed] [Google Scholar]
- 15.Sze R.W., Hagerty N.M., Sassano C., Kazmi P. The business case for evidence-based design in radiology departments. J Am Coll Radiol. 2020;17(1 Part B):152–156. doi: 10.1016/j.jacr.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 16.AHRQ Patient safety primer: human factors engineering. Patient safety primer. http://psnet.ahrq.gov/primer/human-factors-engineering Available at: Published September 2019. Accessed April 28, 2020.
- 17.Carayon P. Human factors of complex sociotechnical systems. Appl Ergon. 2006;37:525–535. doi: 10.1016/j.apergo.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 18.Kleiner B. Macroergonomics: analysis and design of work systems. Appl Ergon. 2006;37:81–89. doi: 10.1016/j.apergo.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 19.Henning R., Warren N., Robertson M. Workplace health protection and promotion through participatory ergonomics: an integrated approach. Public Health. 2009;124(Suppl):26–35. doi: 10.1177/00333549091244S104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ruby A. The Eudaimonia Machine—an office space concept for the 21st century? Fentress Incorporated Blog. https://blog.fentress.com/blog/the-eudaimonia-machine-a-space-concept-for-the-21st-century Available at: Published October 25, 2018. Accessed July 10, 2020.
- 21.Newport C. Pitakus-Little, Brown Book Group; London, England: 2016. Deep work—rules for focused success in a distracted world. [Google Scholar]
- 22.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sullivan G.M., Artino A.R., Jr. Analyzing and interpreting data from Likert-type scales. J Grad Med Educ. 2013;5:541–542. doi: 10.4300/JGME-5-4-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.RStudio Team RStudio: integrated development for R. RStudio Team; 2018. https://www.rstudio.com Available at:
- 25.NIOSH Hierarchy of controls—workplace safety and health. Prevention Through Design. https://www.cdc.gov/niosh/topics/hierarchy/default.html Available at: Published January 13, 2015. Accessed April 29, 2020.
- 26.CDC Strategies for optimizing the supply of N95 respirators. Coronavirus Disease 2019 (COVID-19) https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/index.html Available at: Published February 11, 2020. Accessed April 28, 2020. [DOI] [PMC free article] [PubMed]
- 27.Benitez G.B., Fogliatto F.S., Cardoso R.B., Torres F.S., Faccin C.S., Dora J.M. Systematic layout planning of a radiology reporting area to optimize radiologists’ performance. J Digit Imaging. 2018;31:193–200. doi: 10.1007/s10278-017-0036-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.