Supplemental digital content is available in the text.
KEY WORDS: Brugada electrocardiogram, elderly, sudden cardiac death, women
Abstract
Background
Brugada syndrome is a disorder associated with sudden cardiac death and characterized by an abnormal electrocardiogram (ECG). Previous studies were predominantly conducted in men, and the data on long-term prognosis are limited. Information about women, especially elderly women, is lacking.
Objective
The aim of this study was to investigate the long-term prognosis of the Brugada ECG pattern in elderly women.
Method
We investigated the 10-year prognosis of the Brugada ECG pattern in elderly women in a nationwide community-based population in Taiwan. Community-dwelling women older than 55 years were prospectively recruited from December 2008 to March 2013 by a stratified random sampling method. All enrolled individuals were followed up annually until April 2019, and the cause of death was documented by citizen death records.
Results
Among 2597 women, 60 (2.31%) had a Brugada-type ECG, and this prevalence was higher than the mean global prevalence of 0.23%. One woman had a type 1 ECG (0.04%), whereas 15 (0.58%) and 44 (1.70%) women had type 2 and type 3 ECG patterns, respectively. Cox survival analysis revealed that all-cause mortality and cardiac mortality were similar in the individuals with and without a Brugada-type ECG during a mean follow-up of 96.1 ± 20.5 months.
Conclusions
Our findings suggest that Brugada ECG patterns are not infrequent in elderly women but are not associated with increased risk of mortality in long-term follow-up; these findings may help reduce unnecessary anxiety for physicians, nurses, allied health caregivers, and patients.
Sudden cardiac death refers to an unexpected death due to a cardiac cause within a short period in a person with or without known heart disease.1 The incidence rate of sudden cardiac death is estimated to be 36 to 128 cases per 100 000 population per year2–4 and represents 6% of all deaths globally.5 Although women have a lower incidence of sudden cardiac death than men,6 women still constitute 30% to 40% of these deaths.7
Brugada syndrome (BrS) has been described as an inheritable cardiac disorder characterized by a distinct electrocardiogram (ECG) pattern consisting of a right bundle-branch block with ST-segment elevation in V1, V2, and V3 with a structurally normal heart and a high susceptibility to sudden cardiac death.8,9 This disorder is estimated to be responsible for at least 20% of sudden deaths in patients with no clearly apparent structural heart disease.10 BrS most commonly affects healthy men younger than 40 years, with a mean age of sudden death of 41 ± 15 years.10,11 Therefore, BrS not only remains an important challenge in cardiology but can also result in a significant psychological impact on patients and their families.12–14
Brugada syndrome occurs more frequently in Southeast Asia than in Western countries, with the prevalence of a Brugada ECG pattern (BrP) of approximately 0.12% versus 0.05%15; however, epidemiological studies regarding this syndrome in Southeast Asia are rather limited. Brugada syndrome is 8 to 10 times more prevalent in men than in women in Europe16 and has a male/female ratio of approximately 15 to 1 in Japan17 and 10 to 1 in Taiwan.18,19 In fact, most of the epidemiological research on BrS to date has focused only on men because most of available study candidates were men.20 As a result, information regarding the clinical course and prognosis of BrS in women is sparse. Previous studies have shown that women with BrS have less frequent symptoms and spontaneous BrPs as compared with men.21,22 Even though women are generally considered to be a clinically low-risk group, this low level of risk does not translate into women having zero risk. Moreover, because men and women are fundamentally different in terms of biology, we should not neglect the clinical differences between men and women or attempt to assimilate women's health into men's.
Although the mean age at onset of arrhythmic event of patients with BrS is in the third or fourth decade,18,22–24 the initial symptoms can appear as early as the age of 1 year25 and late as the age of 87 years.26 In Taiwan, 2 elderly-onset adult BrS cases have been identified previously, and the patients were 71 and 74 years old when initial symptoms occurred.27 In the Survey on Arrhythmic Events in Brugada Syndrome study,28 approximately 20% of women with BrS exhibited their first arrhythmic events at over 60 years of age. Therefore, diagnosis and screening of BrS should still be considered in middle-aged and elderly people. Moreover, the prevalence of BrP in women has not been investigated in community-based studies, and information regarding the long-term prognosis of women with Brugada-type ECG is not available. Therefore, the aim of this study was to investigate the prevalence and 10-year prognosis of a spontaneous BrP in a community-based female population.
Methods
Study Population and Participant Recruitment Process
The study method has previously been described.29 Briefly, our study candidates included 2597 women enrolled in the Healthy Aging Longitudinal Study in Taiwan (HALST), an ongoing population-based longitudinal study of adults recruited from December 2008 to March 2013 and followed up annually until the end of April 2019. The recruitment process was as follows (see Figure, Supplemental Digital Content 1, http://links.lww.com/JCN/A106, and Figure 1): adults living in the townships located within 2 km of the study hospital in 7 regions across Taiwan were stratified by age, gender, and education level, and respondents were selected from each stratum by the systematic random sampling method. These 7 locations cover both urban and rural areas, as well as different ethnic groups speaking different dialects, representing the diverse sociodemographic characteristics of the Taiwanese population. The eligibility criterion was people aged 55 years or older, and exclusion criteria were having a highly contagious infectious disease or severe illness including malignancy undergoing active treatment, inability to ambulate, and institutionalization or hospitalization. Subjects with severe hearing, speech, mental, or cognitive impairments were also excluded because of their inability to answer questions accurately. All of the study participants underwent home-visit assessments that included interviewer-administered questionnaires by the study nurses, and within 2 weeks after the home visit, they received a detailed history taking, a standardized physical examination performed by board-certified physicians, and 3 serial ECG examinations and laboratory examinations in the hospital. All of the data obtained by questionnaire were crossed-checked with patient medical records. This long-term follow-up study was reviewed and approved by the institutional review board of the National Health Research Institutes in Taiwan and their participating hospitals, and all participants provided written informed consent.
FIGURE 1.
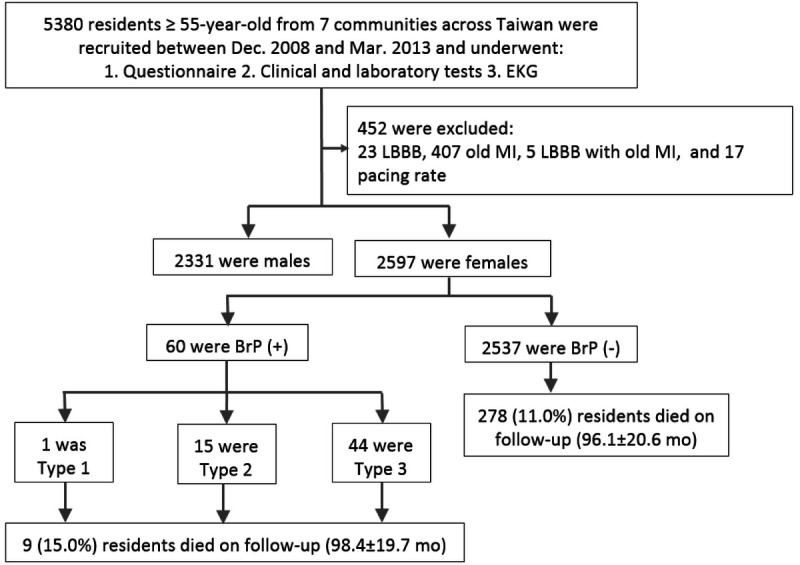
Flowchart of study subject selection.
The demographic variables explored include age, educational level, marital status, smoking status, alcohol intake, physical activity, and medications including antiarrhythmic drugs. Body height, body weight, and blood pressure were recorded. Blood tests included a lipid profile (total cholesterol, triglycerides, and high-density lipoprotein cholesterol), fasting glucose, and hemoglobin A1c. Hypertension was defined by self-report, current use of antihypertensive medication, systolic blood pressure 130 mm Hg or higher, or diastolic blood pressure 85 mm Hg or higher at home. Dyslipidemia was defined by self-report, medication use, high total cholesterol (≥240 mg/dL) or triglyceride (≥150 mg/dL) levels, or reduced high-density lipoprotein cholesterol level (men, <40 mg/dL; women, <50 mg/dL). Diabetes mellitus was defined by self-report, medication use, or high fasting plasma glucose (≥126 mg/dl) or hemoglobin A1c (≥6.5%) level.
Electrocardiogram Analysis and Diagnostic Criteria
All study participants received 3 serial ECG examinations at enrollment. These 12-lead ECGs were recorded at 1-minute intervals using the standard settings of 10 mm/mV and 25 mm/s; PR, QRS, and corrected QT intervals were automatically computed by the Bazett formula. All ECGs were analyzed and interpreted by 2 independent cardiologists who were blinded to the participants' clinical data. Those with old myocardial infarction, left bundle branch block, complete atrioventricular block, or pacing rhythm on ECG were excluded from the study. Because most previous epidemiologic studies defined BrPs according to the criteria formalized by the second consensus conference of the Heart Rhythm Society and the European Heart Rhythm Association, we also applied the same criteria for BrPs in this study for comparison between studies.10 Right precordial leads (ie, leads V1–V3) of the resting 12-lead ECG were analyzed and the criteria for classifying BrPs into types 1 to 3 were as follows (see Figure, Supplemental Digital Content 2,http://links.lww.com/JCN/A107):
Type 1 ECG has a coved-type ST-segment elevation with J point elevation more than 0.2 mV, followed by a negative T wave.
Type 2 ECG has a saddle-back type ST-segment elevation with J point elevation more than 0.2 mV, followed by a gradually descending ST-segment elevation more than 0.1 mV and a positive or biphasic T wave.
Type 3 ECG has either a saddle-back or coved appearance, but with ST-segment elevation less than 0.1 mV.
10-Year Follow-Up and Outcomes
An annual follow-up telephone interview for any new cardiovascular or frailty-related events was carried out by the study nurses for all study participants since the initial enrollment in December 2008. Information on the cause of death was confirmed by linking the database of death records from the Taiwan Ministry of Health and Welfare. We used International Classification of Diseases, 10th revision, codes to identify the cause of death and defined cardiovascular death if the International Classification of Diseases code was I01-I02, I05-I09, I20-I25, I27, or I30-I52 (see Supplemental Digital Content 3, http://links.lww.com/JCN/A108).
Statistical and Survival Analysis
We used either a χ2 or a Fisher exact test to compare categorical variables and 1-way analysis of variance for continuous variables. Interobserver agreement was determined by the overall proportion of agreement and by using the κ statistic using all ECGs. Survival curves were plotted by the Kaplan-Meier method, and Cox regression modeling and log-rank test were used for the comparison of the difference in all-cause mortality and cardiovascular mortality between study participants with and without BrP. A 2-tailed P value less than 0.05 was considered significant.
Results
Prevalence and Clinical Characteristics of Women With a Brugada Electrocardiogram
Among 2597 healthy elderly women enrolled in the HALST cohort, the prevalence of BrP was 2.310% (n = 60) (Table 1). The overall proportion of agreement in the diagnosis of Brugada-type ECG between the 2 interpreters was 99.1%, with a κ score of 0.95 (95% confidence interval, 0.93–0.97). There were no significant differences in age, height, hypertension, diabetes, dyslipidemia, previous events of stroke, and atrial fibrillation between those with a BrP and those without. However, women with a BrP tended to have lower body weight and lower body mass index. Baseline ECGs showed no significant differences in terms of PR interval, QRS duration, and QTc between the 2 groups.
TABLE 1.
Clinical Characteristics and Prognosis of Women With and Without a Brugada Electrocardiogram Pattern in the Healthy Aging Longitudinal Study in Taiwan Cohort
| BrP (−) (n = 2,537) |
BrP (+) (n = 60) |
P | |
|---|---|---|---|
| Age, years | 69.0 ± 8.0 | 68.3 ± 6.6 | .560 |
| Height, cm | 153.0 ± 5.8 | 153.5 ± 6.0 | .544 |
| Weight, kg | 57.6 ± 9.4 | 51.5 ± 7.8 | <.001 |
| Body mass index, kg/m2 | 24.6 ± 3.6 | 21.8 ± 3.0 | <.001 |
| Systolic blood pressure, mm Hg | 129.0 ± 19.4 | 125.8 ± 20.8 | .221 |
| Diastolic blood pressure, mm Hg | 69.7 ± 10.4 | 68.0 ± 11.2 | .198 |
| Hypertensive | 930 (36.7) | 21 (35.0) | .792 |
| Diabetes mellitus | 434 (17.1) | 5 (8.3) | .073 |
| Dyslipidemia | 923 (36.4) | 23 (38.3) | .756 |
| Stroke | 93 (3.7) | 1 (1.7) | .413 |
| Atrial fibrillation | 24 (0.9) | 0 (0) | .449 |
| ECG parameters | |||
| PR, ms | 167.1 ± 29.8 | 161.6 ± 22.2 | .067 |
| QRS, ms | 90.7 ± 11.8 | 91.0 ± 10.1 | .839 |
| QTc, ms | 443.0 ± 21.1 | 438.8 ± 20.7 | .120 |
| Number of deaths | |||
| Cardiovascular death | 42 (1.7) | 0 (0) | .315 |
| Noncardiovascular death | 236 (9.3) | 9 (15.0) | .136 |
| All-cause death | 278 (11.0) | 9 (15.0) | .324 |
Data are presented as mean ± SD or n (%).
Abbreviations: BrP, Brugada ECG pattern; BrP (−), Brugada ECG pattern negative; BrP (+), Brugada ECG pattern positive; ECG, electrocardiogram.
Long-Term Prognosis of Women With a Brugada Electrocardiogram
During a mean follow-up of 96.1 ± 20.5 months, a total of 278 women without a BrP died, and 42 of these deaths (1.7%) could be attributed to cardiac causes. On the other hand, a total of 9 women with a BrP died, but none could be attributed to cardiac causes. Both all-cause mortality and cardiac mortality were not significantly different between the 2 groups (log-rank test, P = .42, Figure 2A, and log-rank test, P = .30, Figure 2B, respectively).
FIGURE 2.
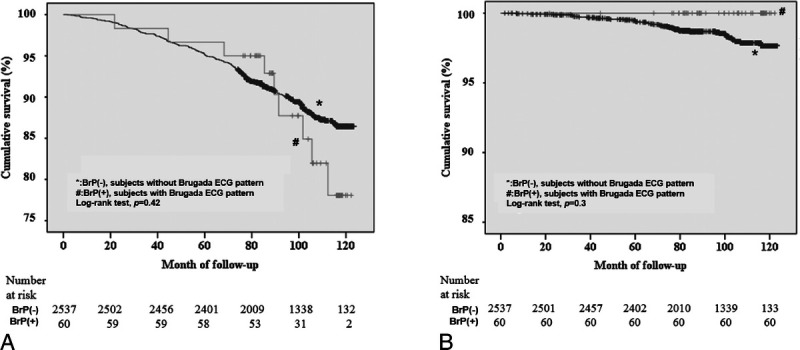
Kaplan-Meier survival analysis. (A) All-cause mortality in subjects with (n = 60) or without (n = 2,537) a Brugada electrocardiogram (ECG) pattern. (B) Cardiovascular mortality in subjects with (n = 60) or without (n = 2,537) a Brugada ECG pattern.
Among those with BrP, 1 woman had a type 1 ECG pattern (0.039%), 15 women had a type 2 ECG pattern (0.578%), and 44 women had a type 3 ECG pattern (1.694%) (Table 2). There were no significant differences in age, height, hypertension, diabetes, dyslipidemia, previous events of stroke, and atrial fibrillation between those without a BrP and those with different types of BrPs, except for body weight [BrP type 1 < BrP type 2 < BrP type 3 < BrP (−); P < .001] and body mass index [BrP type 2 < BrP type 3 < BrP type 1 < BrP (−); P < .001]. The baseline ECG showed no significant differences in terms of PR interval, QRS duration, and QTc among these 4 groups. Two women with a type 2 ECG pattern and 7 women with a type 3 ECG pattern died on follow-up, but all-cause mortality was not significantly different.
TABLE 2.
Clinical Characteristics and Prognosis of Women in 4 Different Brugada Electrocardiogram Pattern Groups in the Healthy Aging Longitudinal Study in Taiwan Cohort
| BrP (−) (n = 2,537) |
Brugada-Type ECG | P | |||
|---|---|---|---|---|---|
| Type 1 (n = 1) |
Type 2 (n = 15) |
Type 3 (n = 44) |
|||
| Age, y | 69.0 ± 8.0 | 76.3 | 65.9 ± 6.5 | 68.9 ± 6.5 | .379 |
| Height, cm | 153.0 ± 5.8 | 147.0 | 153.9 ± 5.0 | 153.5 ± 6.3 | .638 |
| Weight, kg | 57.6 ± 9.4 | 49.3 | 50.4 ± 6.2 | 51.9 ± 8.4 | <.001 |
| Body mass index, kg/m2 | 24.6 ± 3.6 | 22.8 | 21.2 ± 2.0 | 22.0 ± 3.3 | <.001 |
| Systolic blood pressure, mm Hg | 129.0 ± 19.4 | 123.0 | 124.2 ± 25.3 | 126.4 ± 19.6 | .644 |
| Diastolic blood pressure, mm Hg | 69.7 ± 10.4 | 66.5 | 66.8 ± 13.7 | 68.4 ± 10.6 | .586 |
| Hypertensive | 930 (36.7) | 0 (0) | 6 (40.0) | 15 (34.1) | .856 |
| Diabetes mellitus | 434 (17.1) | 0 (0) | 0 (0) | 5 (11.4) | .232 |
| Dyslipidemia | 923 (36.4) | 0 (0) | 2 (13.3) | 21 (47.7) | .091 |
| Stroke | 93 (3.7) | 0 (0) | 0 (0) | 1 (2.3) | .839 |
| Atrial fibrillation | 24 (0.9) | 0 (0) | 0 (0) | 0 (0) | .903 |
| ECG parameters | |||||
| PR, ms | 167.1 ± 29.8 | 170.0 | 171.2 ± 19.8 | 158.1 ± 22.5 | .237 |
| QRS, ms | 90.7 ± 11.8 | 106.0 | 93.6 ± 11.7 | 89.8 ± 9.3 | .409 |
| QTc, ms | 443.0 ± 21.1 | 433.0 | 434.3 ± 21.5 | 440.4 ± 20.7 | .332 |
| Prognosis | |||||
| Cardiovascular death | 42 (1.7) | 0 (0) | 0 (0) | 0 (0) | .799 |
| Noncardiovascular death | 236 (9.3) | 0 (0) | 2 (13.3) | 7 (15.9) | .461 |
| All-cause death | 278 (11.0) | 0 (0) | 2 (13.3) | 7 (15.9) | .733 |
Data are presented as mean ± SD or n (%).
Abbreviations: BrP, Brugada ECG pattern; BrP(−), Brugada ECG pattern negative; ECG, electrocardiogram.
Summaries of Female Brugada Electrocardiogram Patterns in Community-Based Studies Worldwide
We summarized the prevalence of female BrPs in community-based studies30–40 worldwide in the supplementary file (see Table, Supplemental Digital Content 4, http://links.lww.com/JCN/A109). The prevalence of female type 1 ECG ranged from 0% to 0.258% in community-based studies, and our investigation showed that the prevalence was 0.039%, which is very close to the average worldwide prevalence (0.036%). The prevalence of type 2 and type 3 ECG in our study was the highest among all the studies, 0.578% and 1.694%, respectively. Overall, the total prevalence of female BrPs in our study was the highest (2.310%), whereas that of other community-based studies ranged from 0% to 0.954%, and the mean worldwide prevalence was 0.226%.
Discussion
Twenty-eight years have gone by since BrS was reported by Brugada et al8 in 1992, and more than 4000 studies related to BrS have been published. However, the data on prognoses longer than 10 years are scarce and the number of specific studies focusing on women is few, resulting in limited evidence in this field. Extrapolation of BrS outcomes in men to women is based on the false assumption that men and women are identical. The health and risks of women need to be recognized in order to improve healthcare quality and treatment effectiveness. To the best of our knowledge, this is the first study to examine the prevalence and long-term prognosis of BrPs in females worldwide.
Prevalence of Brugada-Type Electrocardiogram
A type 1 ECG is the diagnostic cornerstone of BrS.41 Similar to the mean global prevalence of 0.036% (ranging from 0% to 0.258% in community-based studies worldwide), our investigation showed that the prevalence of spontaneous Brugada-type ECG in Taiwanese women was 0.039%. Because symptoms of BrS often occur in young and middle-aged populations, and the participants in our study were elderly, this finding suggests that the prevalence of younger women with type 1 ECG might be higher in Taiwan. Moreover, we reported the highest prevalence of type 2 and type 3 ECG (0.578% and 1.694%, respectively) among all community-based studies. Our study also had the highest total prevalence of female BrPs (2.310%), whereas the worldwide average was 0.226%. The prevalence of a non–type 1 ECG pattern in women in Taiwan was even higher than that in men in other community studies,42–44 implying that most elderly women with BrS in the Han Chinese population may carry a concealed form of BrS. Although a definitive diagnosis of BrS does not include type 2 and type 3 ECGs, these ECG patterns are considered suspicious for BrS, and these participants should be referred to cardiologists for further assessment to confirm the possibility of having BrS and prevent sudden cardiac death.
Clinical Characteristics of Women With a Brugada-Type Electrocardiogram
In concordance with previous results reported for mixed populations of men and women35,36 and those focused on men only,42 our study adds further evidence that women with BrP tended to have significantly lower body mass index than those without (24.6 ± 3.6 vs 21.8 ± 3.0; P < .001). This relationship between low body mass index and a BrP was also reported in the Japanese population,45 the Thai population,40 and a Portuguese family with BrS.46 The possible explanation is the elevated serum thyroxin level in BrS, which decreases body weight, leading to low body mass index, and up-regulates the transient outward current of cardiac ion channels (Ito), which is at the heart of BrS, causing the development of BrP.47–53 Our study did not detect any difference in ECG parameters, including PR interval and QRS duration, between women with BrP and those without. In contrast, Gallagher et al38 reported that PR interval and QRS duration were significantly longer in Brugada participants. This discrepancy may be explained by the significant differences in age and gender in the 2 studies. In Gallagher et al's cohort, 90.8% of participants were men, and none of the 31 participants with BrPs were women. Also, the mean age of healthy participants was 29.9 ± 9 years and that of participants with BrPs was 20.8 ± 2.8 years. In our study, 100% of participants were elderly women, with a mean age of 69.0 ± 8.0 in the no-BrP group and 68.3 ± 6.6 in the BrP group.
10-Year Prognosis of Women With a Brugada-type ECG
To the best of our knowledge, this is the first study to test the association between a Brugada-type ECG and its prognosis in women on the basis of a long-term large-scale study.
Although BrS is one of the sudden cardiac death diseases, epidemiological studies investigating the prognosis of women with a BrP are not available. Most previous studies focused only on men or reported the results for the sexes combined. In 2 exceptions, women made up most of Tsuji et al's35 and Tsuneoka's36 studies (n = 10 662 [73%] and n = 6114 [59.8%], respectively], and some of them were positive for a BrP, but the follow-up results did not clarify the sex ratio for events, such as sudden death or other kinds of mortality. None of the community studies looked into the outcomes that specifically happened to women. Our research is the first community-based study that targeted women only. We found that participants with BrP had no cardiovascular deaths, indicating BrPs found in elderly women were not associated with increased cardiovascular mortality during the long-term follow-up period. Similar outcomes were reported in the studies that enrolled 100% men.42,43 Our results provide important findings for epidemiological research and clinical practice, and further larger-scale studies involving female cases should be conducted.
Summary of Clinical Implications
The ECG is a globally used, essential, inexpensive, and noninvasive technique to detect electric abnormalities of the heart. It is widely used in many clinical practices during health check-ups, preoperation evaluations, and assessment of patients with suspected or documented heart disease. The world's population is aging; virtually every country in the world is experiencing growth in the number and proportion of older persons in its population. Women generally live longer than men, so we expect that the overall number of female patients will increase in the near future. In this study, our findings suggested that accidental BrPs were not infrequent in elderly women but were not associated with increased risk of mortality in long-term follow-up; these findings may help reduce unnecessary anxiety for physicians, nurses, allied health caregivers, and patients.
Limitations of the Study
There are some limitations in this study. First, all of our study participants were older than 55 years old, and the average age was higher than the mean age of patients with BrS. This could underestimate the true prevalence and outcomes of women with BrPs because some higher risk women might have already died of sudden cardiac death before enrollment. Second, spontaneous fluctuations between diagnostic ECGs and nondiagnostic ECGs occur frequently in patients with BrS.54 Our report was based on the analysis of 3 serial 12-lead ECGs collected for each woman at the beginning of the survey; thus, our results might also underestimate the true prevalence of Brugada-type ECGs in women. Third, the family history of sudden cardiac death and personal history of syncope were not accessible in our study; therefore, whether our study participants were truly asymptomatic was unknown. Obviously, a longer follow-up study with more ECG recordings and a thorough history taking for each individual is warranted to validate and extend our data.
Conclusion
The prevalence of BrPs is not rare in the women of Taiwan, but middle-aged and elderly women with Brugada ECG did not have an increased risk of mortality in long-term follow-up. The benign natural phenomenon in this and other studies indicates that prophylactic implantable cardioverter-defibrillators are not recommended in this patient group; however, studies with longer-term follow-up should be conducted to validate and extend our findings.
What’s New and Important
The prevalence of middle-aged and elderly women with Brugada-type ECGs in Taiwan was 2.31%, which was higher than the mean global prevalence of 0.23%.
There was no difference in all-cause mortality and cardiac mortality in the women with or without Brugada-type ECG during a mean follow-up of 96.1 ± 20.5 months.
Supplementary Material
Acknowledgments
We are grateful to the HALST study's advisory committee (Drs Luigi Ferrucci, Jack M. Guralnik, Dilip V. Jeste, and Kung-Yee Liang) for the precious suggestions. We wish to thank the men and women who participated in the study and all the members of the HALST study group. The members of the HALST study group are as follows: Drs Chao-Agnes Hsiung, Chih-Cheng Hsu, I-Chien Wu, Hsing-Yi Chang, Chu-Chih Chen, Yen-Feng Chiu, Hui-Ju Tsai, and Ken N. Kuo, of National Heath Research Institutes; Dr Ching-Yu Chen of National Taiwan University; Dr Kiang Liu of Northwestern University Medical School; Dr Marion Lee of University of California at San Francisco; Dr Ida Chen of Cedars-Sinai Medical Center; Dr Shu-Han Yu of Chung Shan Medical University; Dr Kai-Ting Ko of Mackay Memorial Hospital; Dr Tzuo-Yun Lan of National Yang-Ming University; Dr Hou-Chang Chiu of Shin Kong Wu Ho-Su Memorial Hospital; Dr Wen-Jin Liaw of Yee Zen General Hospital; Dr Yo-Hann Liu of Hope Doctors Hospital; Dr I-Ching Lin of Changhua Christian Hospital; Dr Ping-An Wu of Potz General Hospital; Dr Chon-Chou Juan of Yuan's General Hospital; and Dr Shi-Chen Shen of Mennonite Christian Hospital. We are also grateful to the staff of the Sixth Core Lab, Department of Medical Research, National Taiwan University Hospital, and Taiwan Healthy foundation for technical support.
Footnotes
The authors have no conflicts of interest to disclose.
This work was supported by National Health Research Institutes of Taiwan under grant PH-101-SP-01, PH-102-SP-01, and PH-103-SP-01; Ministry of Science and Technology, Taiwan (grant numbers MOST-104-2314-B-002-193-MY3, MOST 106-2314-B-002-047-MY3, MOST 106-2314-B-002-134-MY2, MOST 106-2314-B-002-206, MOST 107-2314-B-002-009, MOST 108-2635-B-002-002, MOST 107-2314-B-002-261-MY3, and MOST 108-2635-B-002-002), the Taiwan Health Foundation, and National Taiwan University Hospital (grant numbers NTUH 105-S3077 and NTUH 106-018)
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.jcnjournal.com).
REFERENCES
- 1.Zipes DP, Wellens HJ. Sudden cardiac death. Circulation. 1998;98:2334–2351. [DOI] [PubMed] [Google Scholar]
- 2.Priori SG Aliot E Blomstrom-Lundqvist C, et al. Task Force on Sudden Cardiac Death of the European Society of Cardiology. Eur Heart J. 2001;22:1374–1450. [DOI] [PubMed] [Google Scholar]
- 3.Chugh SS Jui J Gunson K, et al. Current burden of sudden cardiac death: multiple source surveillance versus retrospective death certificate–based review in a large U.S. community. J Am Coll Cardiol. 2004;44:1268–1275. [DOI] [PubMed] [Google Scholar]
- 4.Maruyama M Ohira T Imano H, et al. Trends in sudden cardiac death and its risk factors in Japan from 1981 to 2005: the Circulatory Risk in Communities Study (CIRCS). BMJ Open. 2012;2:e000573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehra R. Global public health problem of sudden cardiac death. J Electrocardiol. 2007;40:S118–S122. [DOI] [PubMed] [Google Scholar]
- 6.Hayashi M, Shimizu W, Albert CM. The spectrum of epidemiology underlying sudden cardiac death. Circ Res. 2015;116:1887–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simmons A, Pimentel R, Lakkireddy D. Sudden cardiac death in women. Rev Cardiovasc Med. 2012;13:e37–e42. [DOI] [PubMed] [Google Scholar]
- 8.Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome: a multicenter report. J Am Coll Cardiol. 1992;20:1391–1396. [DOI] [PubMed] [Google Scholar]
- 9.Juang JJ, Horie M. Genetics of Brugada syndrome. J Arrhythm. 2016;32:418–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Antzelevitch C Brugada P Borggrefe M, et al. Brugada syndrome: report of the second consensus conference. Heart Rhythm. 2005;2:429–440. [DOI] [PubMed] [Google Scholar]
- 11.Juang JM Lu TP Lai LC, et al. Utilizing multiple in silico analyses to identify putative causal SCN5A variants in Brugada syndrome. Sci Rep. 2014;4:3850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Conte G Dewals W Sieira J, et al. Drug-induced Brugada syndrome in children: clinical features, device-based management, and long-term follow-up. J Am Coll Cardiol. 2014;63:2272–2279. [DOI] [PubMed] [Google Scholar]
- 13.Ingles J, Spinks C, Yeates L, McGeechan K, Kasparian N, Semsarian C. Posttraumatic stress and prolonged grief after the sudden cardiac death of a young relative. JAMA Intern Med. 2016;176:402–405. [DOI] [PubMed] [Google Scholar]
- 14.Probst V Plassard-Kerdoncuf D Mansourati J, et al. The psychological impact of implantable cardioverter defibrillator implantation on Brugada syndrome patients. Europace. 2011;13:1034–1039. [DOI] [PubMed] [Google Scholar]
- 15.Mizusawa Y, Wilde AA. Brugada syndrome. Circ Arrhythm Electrophysiol. 2012;5:606–616. [DOI] [PubMed] [Google Scholar]
- 16.Priori SG Wilde AA Horie M, et al. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm. 2013;10:1932–1963. [DOI] [PubMed] [Google Scholar]
- 17.Hiraoka M. Brugada syndrome in Japan. Circ J. 2007;71(Suppl A):A61–A68. [DOI] [PubMed] [Google Scholar]
- 18.Juang JM Tsai CT Lin LY, et al. Unique clinical characteristics and SCN5A mutations in patients with Brugada syndrome in Taiwan. J Formos Med Assoc. 2015;114:620–626. [DOI] [PubMed] [Google Scholar]
- 19.Juang JM Lu TP Lai LC, et al. Disease-targeted sequencing of ion channel genes identifies de novo mutations in patients with non-familial Brugada syndrome. Sci Rep. 2014;4:6733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eckardt L. Gender differences in Brugada syndrome. J Cardiovasc Electrophysiol. 2007;18:422–424. [DOI] [PubMed] [Google Scholar]
- 21.Sieira J Conte G Ciconte G, et al. Clinical characterisation and long-term prognosis of women with Brugada syndrome. Heart. 2016;102:452–458. [DOI] [PubMed] [Google Scholar]
- 22.Berthome P Tixier R Briand J, et al. Clinical presentation and follow-up of women affected by Brugada syndrome. Heart Rhythm. 2019;16:260–267. [DOI] [PubMed] [Google Scholar]
- 23.Nagayama T Nagase S Kamakura T, et al. Clinical and electrocardiographic differences in Brugada syndrome with spontaneous or drug-induced type 1 electrocardiogram. Circ J. 2019;83:532–539. [DOI] [PubMed] [Google Scholar]
- 24.Kamakura T Wada M Nakajima I, et al. Evaluation of the necessity for cardioverter-defibrillator implantation in elderly patients with Brugada syndrome. Circ Arrhythm Electrophysiol. 2015;8:785–791. [DOI] [PubMed] [Google Scholar]
- 25.Priori SG, Napolitano C, Giordano U, Collisani G, Memmi M. Brugada syndrome and sudden cardiac death in children. Lancet. 2000;355:808–809. [DOI] [PubMed] [Google Scholar]
- 26.Conte G, Levinstein M, Sarkozy A, Brugada P. Brugada syndrome in the elderly. Eur Heart J. 2013;34:319. [DOI] [PubMed] [Google Scholar]
- 27.Juang JM, Lai LP, Lin JL, Chiang FT. Brugada syndrome in the elderly in Taiwan: report of two cases. Acta Cardiol Sin. 2005;21:62–67. [Google Scholar]
- 28.Milman A Andorin A Gourraud JB, et al. Age of first arrhythmic event in Brugada syndrome: data from the SABRUS (Survey on Arrhythmic Events in Brugada Syndrome) in 678 patients. Circ Arrhythm Electrophysiol. 2017;10. [DOI] [PubMed] [Google Scholar]
- 29.Juang JM Chen CY Chen YH, et al. Prevalence and prognosis of Brugada electrocardiogram patterns in an elderly Han Chinese population: a nation-wide community-based study (HALST cohort). Europace. 2015;17(Suppl 2):ii54–ii62. [DOI] [PubMed] [Google Scholar]
- 30.Matsuo K Akahoshi M Nakashima E, et al. The prevalence, incidence and prognostic value of the Brugada-type electrocardiogram: a population-based study of four decades. J Am Coll Cardiol. 2001;38:765–770. [DOI] [PubMed] [Google Scholar]
- 31.Tohyou YNK, Takenobu H, Akagi T, Miyake H, Murayama M. A survey in the incidence of right bundle branch block with ST elevation among normal population. Jpn J Electrocardiol. 1995;15:223–226. [Google Scholar]
- 32.Atarashi H Ogawa S Harumi K, et al. Three-year follow-up of patients with right bundle branch block and ST segment elevation in the right precordial leads: Japanese Registry of Brugada Syndrome. Idiopathic Ventricular Fibrillation Investigators. J Am Coll Cardiol. 2001;37:1916–1920. [DOI] [PubMed] [Google Scholar]
- 33.Furuhashi M Uno K Tsuchihashi K, et al. Prevalence of asymptomatic ST segment elevation in right precordial leads with right bundle branch block (Brugada-type ST shift) among the general Japanese population. Heart. 2001;86:161–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oe H Takagi M Tanaka A, et al. Prevalence and clinical course of the juveniles with Brugada-type ECG in Japanese population. Pacing Clin Electrophysiol. 2005;28:549–554. [DOI] [PubMed] [Google Scholar]
- 35.Tsuji H, Sato T, Morisaki K, Iwasaka T. Prognosis of subjects with Brugada-type electrocardiogram in a population of middle-aged Japanese diagnosed during a health examination. Am J Cardiol. 2008;102:584–587. [DOI] [PubMed] [Google Scholar]
- 36.Tsuneoka H Takagi M Murakoshi N, et al. Long-term prognosis of Brugada-type ECG and ECG with atypical ST-segment elevation in the right precordial leads over 20 years: results from the Circulatory Risk in Communities Study (CIRCS). J Am Heart Assoc. 2016;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wajed A Aslam Z Abbas SF, et al. Frequency of Brugada-type ECG pattern (Brugada sign) in an apparently healthy young population. J Ayub Med Coll Abbottabad. 2008;20:121–124. [PubMed] [Google Scholar]
- 38.Gallagher MM Forleo GB Behr ER, et al. Prevalence and significance of Brugada-type ECG in 12,012 apparently healthy European subjects. Int J Cardiol. 2008;130:44–48. [DOI] [PubMed] [Google Scholar]
- 39.Sinner MF Pfeufer A Perz S, et al. Spontaneous Brugada electrocardiogram patterns are rare in the German general population: results from the KORA study. Europace. 2009;11:1338–1344. [DOI] [PubMed] [Google Scholar]
- 40.Rattanawong P Ngarmukos T Chung EH, et al. Prevalence of Brugada ECG pattern in Thailand from a population-based cohort study. J Am Coll Cardiol. 2017;69:1355–1356. [DOI] [PubMed] [Google Scholar]
- 41.Probst V Veltmann C Eckardt L, et al. Long-term prognosis of patients diagnosed with Brugada syndrome: results from the FINGER Brugada Syndrome Registry. Circulation. 2010;121:635–643. [DOI] [PubMed] [Google Scholar]
- 42.Ito H, Yano K, Chen R, He Q, Curb JD. The prevalence and prognosis of a Brugada-type electrocardiogram in a population of middle-aged Japanese-American men with follow-up of three decades. Am J Med Sci. 2006;331:25–29. [DOI] [PubMed] [Google Scholar]
- 43.Junttila MJ, Raatikainen MJ, Karjalainen J, Kauma H, Kesaniemi YA, Huikuri HV. Prevalence and prognosis of subjects with Brugada-type ECG pattern in a young and middle-aged Finnish population. Eur Heart J. 2004;25:874–878. [DOI] [PubMed] [Google Scholar]
- 44.Uhm JS Hwang IU Oh YS, et al. Prevalence of electrocardiographic findings suggestive of sudden cardiac death risk in 10,867 apparently healthy young Korean men. Pacing Clin Electrophysiol. 2011;34:717–723. [DOI] [PubMed] [Google Scholar]
- 45.Matsuo K, Akahoshi M, Nakashima E, Seto S, Yano K. Clinical characteristics of subjects with the Brugada-type electrocardiogram. J Cardiovasc Electrophysiol. 2004;15:653–657. [DOI] [PubMed] [Google Scholar]
- 46.Santos LF Correia E Rodrigues B, et al. Spontaneous fluctuations between diagnostic and nondiagnostic ECGs in Brugada syndrome screening: Portuguese family with Brugada syndrome. Ann Noninvasive Electrocardiol. 2010;15:337–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gloss B Trost S Bluhm W, et al. Cardiac ion channel expression and contractile function in mice with deletion of thyroid hormone receptor alpha or beta. Endocrinology. 2001;142:544–550. [DOI] [PubMed] [Google Scholar]
- 48.Wickenden AD, Kaprielian R, You XM, Backx PH. The thyroid hormone analog DITPA restores I(to) in rats after myocardial infarction. Am J Physiol Heart Circ Physiol. 2000;278:H1105–H1116. [DOI] [PubMed] [Google Scholar]
- 49.Le Bouter S Demolombe S Chambellan A, et al. Microarray analysis reveals complex remodeling of cardiac ion channel expression with altered thyroid status: relation to cellular and integrated electrophysiology. Circ Res. 2003;92:234–242. [DOI] [PubMed] [Google Scholar]
- 50.Antzelevitch C, Brugada P, Brugada J, Brugada R. The Brugada Syndrome: From Bench to Bedside. Blackwell Futura; 2008. [Google Scholar]
- 51.Gussak I, Antzelevitch C, Bjerregaard P, Towbin JA, Chaitman BR. The Brugada syndrome: clinical, electrophysiologic and genetic aspects. J Am Coll Cardiol. 1999;33:5–15. [DOI] [PubMed] [Google Scholar]
- 52.Tsai CF, Wu DJ, Lin MC, Ueng KC, Lin CS. A Brugada-pattern electrocardiogram and thyrotoxic periodic paralysis. Ann Intern Med. 2010;153:848–849. [DOI] [PubMed] [Google Scholar]
- 53.Korte AK, Derde L, van Wijk J, Tjan DH. Sudden cardiac arrest as a presentation of Brugada syndrome unmasked by thyroid storm. BMJ Case Rep. 2015;2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Veltmann C Schimpf R Echternach C, et al. A prospective study on spontaneous fluctuations between diagnostic and non-diagnostic ECGs in Brugada syndrome: implications for correct phenotyping and risk stratification. Eur Heart J. 2006;27:2544–2552. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


