Abstract
The concept of health system resilience has gained popularity in the global health discourse, featuring in UN policies, academic articles and conferences. While substantial effort has gone into the conceptualization of health system resilience, there has been no review of how the concept has been operationalized in empirical studies. We conducted an empirical review in three databases using systematic methods. Findings were synthesized using descriptive quantitative analysis and by mapping aims, findings, underlying concepts and measurement approaches according to the resilience definition by Blanchet et al. We identified 71 empirical studies on health system resilience from 2008 to 2019, with an increase in literature in recent years (62% of studies published since 2017). Most studies addressed a specific crisis or challenge (82%), most notably infectious disease outbreaks (20%), natural disasters (15%) and climate change (11%). A large proportion of studies focused on service delivery (48%), while other health system building blocks were side-lined. The studies differed in terms of their disciplinary tradition and conceptual background, which was reflected in the variety of concepts and measurement approaches used. Despite extensive theoretical work on the domains which constitute health system resilience, we found that most of the empirical literature only addressed particular aspects related to absorptive and adaptive capacities, with legitimacy of institutions and transformative resilience seldom addressed. Qualitative and mixed methods research captured a broader range of resilience domains than quantitative research. The review shows that the way in which resilience is currently applied in the empirical literature does not match its theoretical foundations. In order to do justice to the complexities of the resilience concept, knowledge from both quantitative and qualitative research traditions should be integrated in a comprehensive assessment framework. Only then will the theoretical ‘resilience idea’ be able to prove its usefulness for the research community.
Keywords: Health system resilience, health system research, resilience, responsiveness
Key Messages
The way in which resilience is currently applied in the empirical literature does not match its theoretical foundations.
In order to do justice to the complexities of the resilience concept, knowledge from both quantitative and qualitative research traditions should be integrated in a comprehensive assessment framework.
Introduction
The word ‘resilience’ origins from the Latin prefix ‘re-’ (back) and the verb ‘salire’ (to jump, leap). In science, it has long been used by engineering and material science to describe the ability of a material to absorb energy without losing its original form or characteristics (Hollnagel 2009). Over time, different disciplines adopted and adapted the term, adding different interpretations and facets to it: In ecology, resilience describes the persistence of ecological systems and measures a system’s ability to absorb changes of variables and maintain relationships between different populations (Holling 1973). In psychology, resilience is understood as the individual human capability to cope with crises, losses or hardships without negative consequences (Tugade and Fredrickson 2004).
In the last decade, the concept of resilience has also gained popularity in global public health. This development is reflected by major UN frameworks adopted in the last decade: The 2005–15 Hyogo Framework for Action (UNISDR, 2005) was subtitled ‘Building the Resilience of Nations and Communities to Disasters’. Its successor, the 2015–30 Sendai Framework for Disaster Risk Reduction (UNISDR, 2015), increases the focus on health in the disaster preparedness discourse and correspondingly calls for health resilience. Various sustainable development goals point to resilience as a target (1.5: ‘resilience of the poor’, 2.4 ‘resilient agricultural practices’, 11b ‘resilience to disasters’; Bahadur et al. 2015; UNISDR 2015) In a 2016 editorial of Bulletin of the World Health Organisation (WHO), health system resilience is named as a critical concept for global health, in the same vein as health system strengthening, universal health coverage and health security (Kutzin and Sparkes 2016).
The shifting conceptualization of health system resilience
While definitions and concepts of health systems resilience differ substantially throughout the literature, all have a common core: they regard resilience as the degree of change a system can undergo while maintaining its functionality. The concept of resilience was introduced to the health systems literature from the ecological sciences through an increased understanding of health systems as complex adaptive systems (Blanchet and James 2013). In this context, the idea of resilience, defined as ‘a measure of the amount of change a system can experience while maintaining the same controls on structure and function’ (Blanchet and James 2013), can act as a useful tool to help us understand health system dynamics. The ecological idea that strategies to enhance resilience can be absorptive, adaptive or transformative depending on the impact and intensity of the crisis has been particularly impactful in the health system resilience discourse.
Popularized further during the Ebola crisis, health system resilience underwent a conceptual shift; from a mere ‘system’ capacity to recognizing the contribution of individuals and their agency within that system and acknowledging the wider social, economic and political context in which responses occur. Critics argued that the application of the resilience concept—as a ‘top-down’ approach—obscured important factors which prevented an adequate response to the Ebola crisis. They emphasized instead the importance of ‘understanding and reducing local power disparities, building the trustworthiness of health actors […] both between and during crisis’ which improves the ‘everyday functioning of the health system’ (Martineau 2016). In response to these criticisms, Barasa et al. (2017) proposed the idea of ‘everyday resilience’, emphasizing in particular the importance of the capacities and resources available to individuals faced with delivering health services every day. Everyday resilience may especially be of relevance, they argued, in low- and middle-income countries where managers may ‘routinely face structural and policy instability, such as changes in governance structures, payment delays, abrupt and imposed policy directives […], unstable authority delegations, unpredictable staff and […] changing patient and community expectations’ (Barasa et al. 2017).
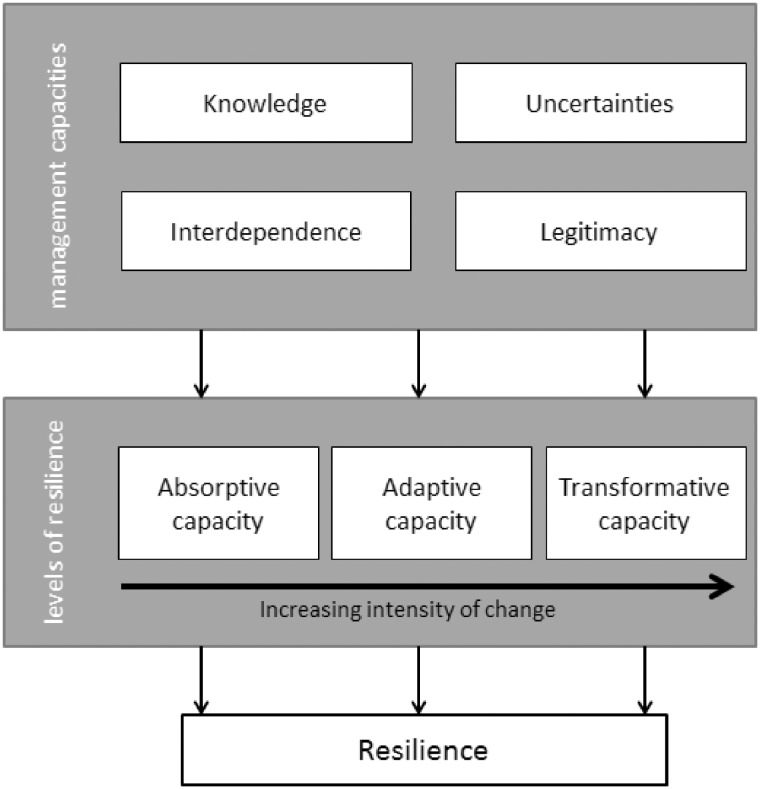
Similarly, Blanchet et al. (2017) proposed a new model of understanding health systems resilience which focuses not just on the outcome of the resilience process (i.e. absorptive, adaptive and transformative capacities), but also on the underlying management capacities of the system and its actors to response to change: knowledge, uncertainties, interdependence and legitimacy (Box 1). These operational dimensions are interlinked with each other and together characterize the management of resilience in health systems (Figure 1). While these two more recent conceptualizations of resilience can be understood as different in terms of taking a ‘top-down’ (Blanchet et al. 2017) and ‘bottom-up’ (Barasa et al. 2017) approach, they both acknowledge the importance of the context in which the resilience process takes place and the agency of actors involved, and thus represent two sides of the same coin.
Box 1 Resilience domains used in conceptual analysis of studies, as defined by Blanchet et al. (2017)
Management capacities:
Knowledge—‘Capacity to collect, integrate and analyse different forms of knowledge and information’
Uncertainties—‘Ability to anticipate and cope with uncertainties and surprises’
Interdependence—‘Capacity to manage interdependence: to engage effectively with and handle multiple- and cross-scale dynamics’
Legitimacy—‘Capacity to build or develop legitimate institutions that are socially accepted and contextually adapted’
Three levels of resilience:
Absorptive capacity—‘capacity of a health system to continue to deliver the same level (quantity, quality and equity) of basic healthcare services and protection to populations despite the shock using the same level of resources and capacities’
Adaptive capacity—‘capacity of the health system actors to deliver the same level of healthcare services with fewer and/ or different resources, which requires making organisational adaptations’
Transformative capacity—‘the ability of health system actors to transform the functions and structure of the health system to respond to a changing environment’
Figure 1.
Conceptual overview of health system resilience, adapted from Blanchet et al. (2017).
Conceptual influences from other fields
In addition to the conceptualization of resilience outlined above, other disciplinary fields have influenced the discourse on health system resilience, most notably the disaster management and healthcare quality literature.
In the disaster management sciences, resilience discussions were initially focused on the maintenance of infrastructure, functionality of health care facilities and continued service delivery (Crowe et al. 2014; Balbus et al. 2016; Cimellaro et al. 2017) operationalizing resilience as ‘capability of a health system to mitigate the impact of major external disruptions on its ability to meet the needs of the population during the disaster’ (Crowe et al. 2014). However, experiences of Hurricane Catrina in the USA shifted the dominant discourse in the disaster management literature to the concept of community resilience (Wulff et al. 2015; Olu 2017). Community resilience proposes that the key to a good disaster response lies in communities, and their ability to ‘prepare, respond, and recover’ from major events through a range of measures including increased social connectedness, adaptive health and social systems and emergency preparedness planning (Wulff et al. 2015).
A further prominent influence on the health system resilience discussions has been the concept of ‘resilience engineering’ or ‘health care resilience’, emerging from the healthcare quality literature. This approach, developed as a critique to traditional views of healthcare safety as an ‘absence of failures’, defines safety as the ‘ability to succeed under varying conditions’ (Hollnagel et al. 2006). It thus focuses on nurturing the everyday functioning of healthcare teams and facilities to strengthen resilience and reduce clinical mistakes. A recent review on the topic has found that this approach has garnered significant attention in both the primary and secondary literature since its emergence around 2012 (Ellis et al. 2019).
The need for a review of the empirical literature
Existing literature reviews have been conducted on the theoretical conceptualization of health system resilience (Turenne et al. 2019) and the factors contributing to resilient health systems (Barasa et al. 2018). The concept of resilience has also been extensively discussed outside the health sector (Tanner et al. 2017). While grasping the theoretical background of the concept is certainly crucial, understanding how theory is translated into evidence is equally important for assessing the usefulness of the ‘resilience idea’ for the research community. However, so far there has been no critical appraisal of how the concept of health system resilience has been operationalized and applied in the empirical literature.
We thus conducted an empirical review of health system literature in order to better understand how the resilience concept has been operationalized in empirical studies. Within this research aim, we address three specific sub-questions: (1) What are the key aspects (methodological approach, geographic focus, health system building block addressed and crisis/challenge discussed) of research on health system resilience and how have these changed over time? (2) What concepts and frameworks on health system resilience have been used to operationalize resilience in the health systems literature? (3) What is the scope of empirical research on health system resilience within current definitions of the concept? We thus provide an overview of the existing empirical literature on health systems research which can be used to further develop the concept and inform its operationalization in future studies.
Methodology
We conducted a review of empirical literature, following systematic review methodology in line with the understanding brought forward by Moher et al. (2015). This included a systematic literature search, and a rigorous and systematic data screening and extraction process (Peters et al. 2015).
Searches were conducted in Medline, Social Science Citation Index and CINAHL (Cumulative Index to Nursing and Allied Health Literature) using Resilien* AND a health system related terms (see Box 2).
Box 2 Search terms
Search terms:
((((((((secondary health care [mh]) OR primary health care [mh]) OR health services [mh]) OR delivery of health care [mh]) OR health services research [mh])) OR ((((((((((((““health system””) OR ““health systems””) OR ““health care system””) OR ““health care systems””) OR ““health care””) OR ““health care sector””) OR ““health care sectors””) OR ““health service””) OR ““health services””) OR ““service delivery””) OR ““health care service””) OR ““health care services””))) AND Resilien*
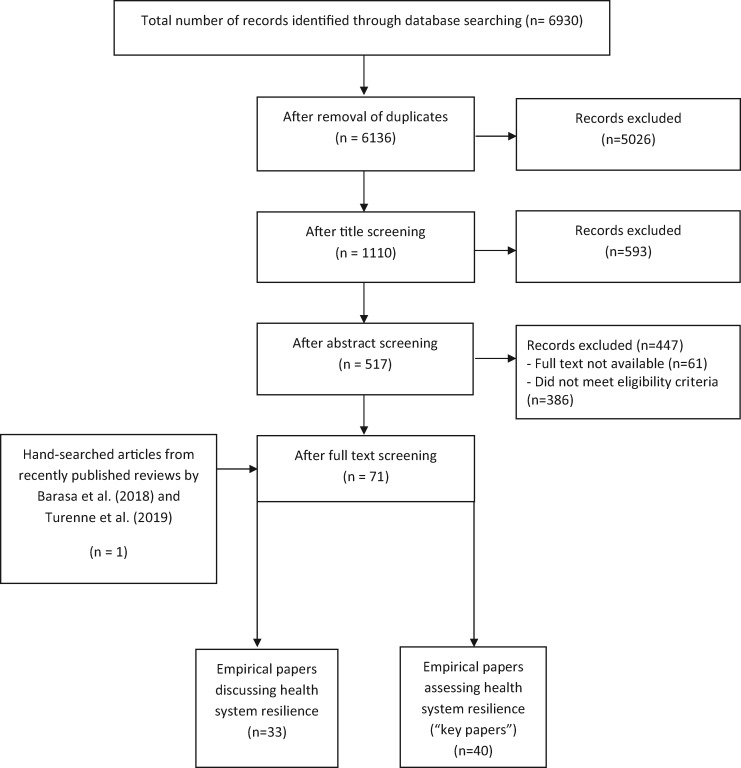
The searches were conducted on 18 October 2019 and were limited to articles published since 2008 in English or German language to keep the extent of the review feasible. The search produced 6136 publications for screening after the removal of 794 duplicates [see Figure 2 for the PRISMA flow diagram in line with Moher et al. (2009)].
Figure 2.
Prisma flow diagram.
Due to the high number of items, we used a three-stage screening process, eliminating non-relevant articles at the stage of title-, abstract- and full text-screening. Items were excluded if they did not report primary data, or were concerned with individual/psychological resilience including resilience of healthcare providers (e.g. nurses, physicians), resilience in the non-health space (e.g. social resilience, resilience of urban environments and resilience of biological systems), community resilience without link to health systems or articles that were concerned neither with health systems nor resilience. We also excluded articles which were concerned with health system resilience, but only used the term as a ‘buzzword’, without further definition, discussion or operationalization of the concept. As the research objective was to understand the application and use of resilience in health system research, items with any research design, geographic scope and health system focus were included.
After the abstract-screening stage, 517 references remained, with another 444 references excluded after screening full texts (see Figure 2). Both abstract- and full text-screening were carried out by the first and second author with joint synthesis until consensus was reached. Two further articles were from the reference lists of the literature reviews by Barasa et al. (2018) and Turenne et al. (2019) met the inclusion criteria for the present study and were included in the review. The remaining articles were divided into two categories: (1) those papers which specifically assessed health system resilience by including this as a specific research objective or applying a framework allowing for the operationalization of health system resilience (‘key papers’) and (2) articles reporting research which led to a discussion of health system resilience or how to achieve health system resilience.
Data extraction was carried out by the first and second author using Microsoft Excel. To answer the first research question on key aspects of the empirical health systems literature, data on type of research (primary/secondary research), discipline of the first author, the health system building block studied [according to World Health Organization (2010)], the type of crisis or conflict studied, study location (country, continent, low-/middle-/high-income country), the organizational level being studied (e.g. global, national or regional) and type of data used were extracted from all identified studies.
To answer the second and third research objectives, only those studies directly measuring or assessing health system resilience (‘key papers’) were analysed. In order to evaluate the use of existing empirical frameworks in the empirical literature (second objective), information on frameworks used was extracted if these guided either the data collection or analysis process, or both. To further extract the scope of empirical research in terms of aspects or elements of the concept being addressed (third objective), we were guided by the conceptual framework of Blanchet et al. (2017). We used this framework because it captures the various ways in which resilience is used in the empirical literature: it describes both the management capacities essential for a resilient system (management capacities: knowledge, uncertainties, interdependence, legitimacy) as well as those describing the outcome (three levels of resilience: absorptive, adaptive and transformative capacities). It thus is able to capture a broad range of research on post ex ante and ex post (Béné et al. 2015) aspects of the resilience process. Research articles were classified within this framework using the definitions listed in Box 2.
We synthesized the findings by combining a narrative synthesis with descriptive quantitative analysis of key aspects addressed. We further tabulated and mapped aims, findings, underlying concepts and measurement approaches according to the resilience definition by Blanchet et al. (2017). Indicators used to measure aspects of resilience in quantitative and mixed methods studies were also extracted and mapped according to their respective resilience domain and the level of data collection (national, organizational, staff or population/patient level).
Results
A total of 71 articles met our inclusion criteria, comprising 40 research papers specifically measuring or addressing health system resilience and 31 discussing health system resilience using empirical research (Figure 2, see Supplementary file for full list of studies).
Quantitative synthesis and mapping of empirical literature in health system resilience
The literature was found to be fairly evenly distributed across continents: Africa (n = 18; 25%), Europe (n = 18; 25%), Asia (n = 15; 21%), North America (n = 15; 21%) and Australia (n = 2; 3%), with four studies reporting data across continents. The exception was South America, where no empirical papers were found. The majority of research was conducted in high-income countries (n = 37; 52%), with 18 studies (25%) in middle-income countries and 13 studies (18%) in low-income countries. We found an increase in literature in recent years (62% of studies published since 2017).
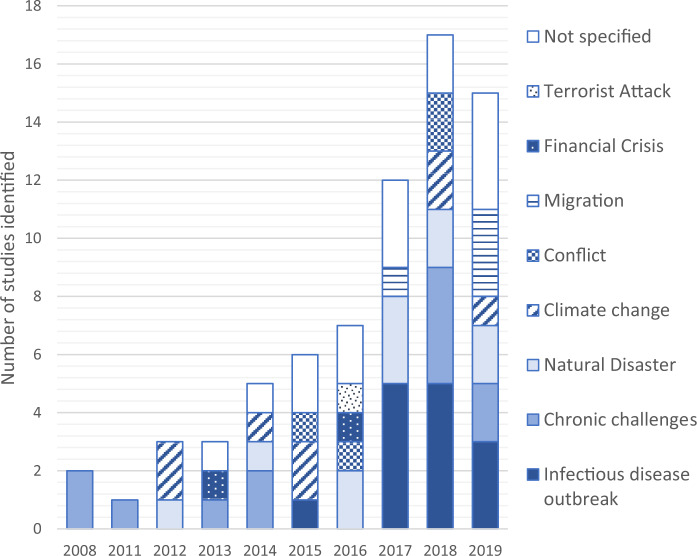
The majority of research (n = 58; 82%) addressed a specific crisis or challenge. Overall, infectious disease outbreaks was the most frequently addressed challenge (n = 14; 20%), followed by natural disasters (n = 11; 15%) and climate change (n = 8; 11%). Other challenges were conflicts (n = 4; 6%), migration (n = 4; 6%), financial crises (n = 2; 3%) and terrorist attacks (n = 1; 1%). Several articles addressed chronic, non-crisis-related challenges (n = 12; 17%): changes in team composition (n = 1; 1%), human error (n = 5; 7%), everyday resilience (n = 3; 4%) and structural change (n = 2; 3%). While non-crisis-related challenges and climate-related studies dominated the early records from 2008 to 2014, over time, the diversity of addressed challenges has grown embracing financial crises from 2013, infectious disease outbreaks from 2015 triggered by the Ebola epidemic and migration from 2017 (see Figure 3).
Figure 3.
Identified literature on health system resilience (N = 71) organized by type of challenge and year (2008–19).
In terms of health system building blocks addressed, a large proportion of studies (n = 34; 48%) focused on service delivery, while 14 (20%) did not focus on a particular health system building block but took a general perspective. Other building blocks addressed frequently include leadership and governance (n = 9; 13%) and health workforce (n = 8; 11%), while health information systems (n = 4; 6%), medicines and access to medicines (n = 2; 3%) and health system financing (n = 1; 1%) are addressed less frequently.
Overall, the empirical studies identified differed in terms of their disciplinary tradition or conceptual background. Studies from the public health sciences tended to converge in three groups: (1) quantitative studies focusing on service delivery, making use of service utilization indicators provide an easily accessible measure to assess resilience before, during and after a crisis (Paterson et al. 2014; Gizelis et al. 2017; Sochas et al. 2017; Kozuki et al. 2018; Ray-Bennett et al. 2019), (2) qualitative studies focusing on the health workforce, influenced by ideas of ‘everyday resilience’ and addressing the contributions of social connectedness and leadership on health system resilience (Mash et al. 2008; Witter et al. 2017; Raven et al. 2018; Brooke-Sumner et al. 2019; Thude et al. 2019), and (3) studies taking a broad perspective of health system resilience, looking at multiple health system building blocks or aspects of a health system to assess resiliency (Ager et al. 2015; Ammar et al. 2016; Fukuma et al. 2017; Ling et al. 2017; Meyer et al. 2018; Watts et al. 2018).
However, influences from outside the public health sciences could also be identified in the empirical health system resilience literature. As a relatively distinct influence, the disciplines of engineering and architecture have contributed empirical research assessing the infrastructure and thermal resilience of healthcare facilities and structures (Lomas et al. 2012; Iddon et al. 2015; Short et al. 2015; Dippenaar and Bezuidenhout 2019). A further relatively distinct influence has been the contribution of specific checklists to assess facility and organizational resilience from the fields of disaster management and emergency preparedness (Paterson et al. 2014; Zhong et al. 2014a, 2015; Dobalian et al. 2016; Khan et al. 2018; Meyer et al. 2018). Also from the field of disaster management, but perhaps more intertwined with resilience in the way it has been conceptualized in the health systems literature, are studies assessing community resilience and its relationship with service delivery during a crisis (O’Sullivan et al. 2013; Andrew et al. 2016; Toner et al. 2017; Alonge et al. 2019; Cohen et al. 2019). Finally, hailing from the tradition of medical sciences concerned with patient safety and quality of care, concepts of ‘health care resilience’ or ‘resilience engineering’ have also influenced the empirical literature on health system resilience (Brattheim et al., 2011; Franklin et al., 2014; Falegnami et al. 2018; Merandi et al., 2018; Patriarca et al., 2018). While study object of these studies is also the health workforce, the focus is placed on the analysis of work processes and the avoidance of medical errors to maintain functionality of services.
Methodological analysis of key empirical papers
We identified 40 high-relevance empirical studies specifically assessing health system resilience. Fifteen articles used a quantitative methodology (Table 1), nine articles applied mixed methods (Table 2) and a further 16 used qualitative methods (Table 3). Given the distinction between articles in terms of their thematic focus described above, we present articles in six thematic areas: assessing national-level health system resilience in the context of a specific crisis (n = 8; 20%), assessing health service delivery (n = 10; 25%), addressing health workforce issues (n = 7; 18%), taking a community resilience perspective (n = 3; 7%), looking at infrastructure and thermal resilience (n = 3; 7%) and developing emergency preparedness checklists and assessment tools (n = 9; 23%).
Table 1.
Overview of aims, methods, concepts used and dimensions of resilience addressed by quantitative research papers (n = 15)
| Author | Year | Country | Research objective | Key findings | Study design and data source | Operationalization of resilience | Conceptual framework used | Management capacity dimensions | Resilience outcome dimensions |
|---|---|---|---|---|---|---|---|---|---|
| Assessing national-level health system resilience in context of a specific crisis | |||||||||
| Fukuma et al. | 2017 | Japan | To assess population-level health indicator changes following the Great East Japan Earthquake and discuss redesign to enhance health systems' responsiveness and resilience | Age-adjusted all-cause mortality and some disease specific mortality rates rose more in affected prefectures than the average national rates. Disaster revealed strengths and deficiencies in responsiveness and resilience of health system | Case study using routine data sources | Population indicators, Health system indicators, Health outcome indicators | N/A | N/A | Absorptive |
| Watts et al. | 2018 | Global | To track a series of indicators of progress, publishing an annual ‘health check’, from now until 2030, on the state of the climate, progress made in meeting global commitments under the Paris Agreement, and adapting and mitigating to climate change | The public, and the health systems they depend upon, are ill-prepared to manage the health impacts of climate change | National survey completed by 101 national ministries of health | Six Indicators developed as part of the Lancet Countdown initiative | Several UN frameworks used |
|
Adaptive |
| Assessing health service delivery in context of a specific crisis | |||||||||
| Radcliff et al. | 2018 | USA | To present ‘measures of ambulatory care recovery and resilience that rely on routine appointment records’ | ‘Most clinics in affected areas achieved appointment completion percentages that matched or exceeded prestorm levels within 2 weeks of the storm’. | Administative data from Veterans Affairs clinics | Percentage of completed appointments before and after a disaster | N/A | N/A | Absorptive |
| Simonetti et al. | 2018 | USA | ‘To understand the impacts of emergency situations on blood availability and the resiliency of the US blood supply system’. | ‘The absence of blood shortage in both emergency scenarios highlighted the resilience of the inter-regional system to meet the potential associated blood demand’. | Modelling study using administrative data on blood collections and utilization | Blood stocks available at regional and national level | N/A | N/A | Absorptive |
| Sochas et al. | 2017 | Sierra Leone | To quantify the extent of the drop in utilization of essential reproductive, maternal and neonatal health services in Sierra Leone during the Ebola outbreak and to model the implication of the decrease in utilization in terms of excess maternal and neonatal deaths | Use of essential reproductive health services decreased as a result of Ebola. This decrease translates to 3600 additional maternal, neonatal and stillbirth deaths in 2014–15 meaning the indirect mortality effects of the crisis may be as important as direct mortality. | Modelling study using routine utilization data to compare projected utilization without crisis to real utilization | Antenatal health services utilization data | N/A | N/A | Absorptive |
| Taking a community resilience perspective | |||||||||
| Andrew et al. | 2016 | Thailand | To test the impact of two competing hypotheses - bonding and bridging- on enhancing organisational resiliency during the Thailand floods of 2011 | Resilience was found to be associated with bridging effect, rural location and private and NGO status rather than public sector organizations | Structured interviews with key informants | Four items on the robustness, resourcefulness, redundancy and rapidity of the organization during the crisis | Framework to assess seismic resilience of communities (Bruneau et al. 2003) | Interdependence | Absorptive |
| Cohen et al. | 2019 | Israel | To explore the relationship between the public’s confidence in the availability of healthcare services during and following emergencies, and community resilience | ‘Confidence in continuity of health services during a state of emergency was found to be positively correlated with community resilience’ | Household survey | Conjoint Community Resilience Assessment Measurement (CCRAM) tool | CCRAM model (Leykin et al. 2013) |
|
N/A |
| Health workforce issues | |||||||||
| Falegnami et al. | 2018 | Italy | ‘To assess the anaesthesia professionals' organizational resilient performance with respect to different daily work conditions’. | The questionnaire shows the potential to assess proxy measures of resilience, despite being complex and time‐consuming. | Survey of anaesthesiologists | Resilience Assessment Grid, adapted using analytic hierarchy process method | Four cornerstones of resilience (Hollnagel et al. 2006) |
|
N/A |
| Infrastructure and Thermal Resilience | |||||||||
| Iddon et al. | 2015 | UK | To assess the influence of hospital ward design on resilience to health waves and develop model for predicting inside temperatures | Nightingale wards showed remarkable resilience to hot weather. Distributed lag models are a promising method for forecasting inside temperatures | Distributed lag models developed from measured temperatures | Temperature maintenance | N/A | N/A | Absorption |
| Lomas et al. | 2012 | United Kingdom | To estimate the resilience of a representative building type, the ‘Nightingale wards’ | Nightingale wards demonstrate relative resilience. Modest refurbishment such as insulation, shading, improved natural ventilation and removal of suspended ceilings increase resilience. | Descriptive statistics and calibrated dynamic thermal model developed from measured temperatures | Temperature maintenance | N/A | N/A |
|
| Short et al. | 2015 | UK | To model temperature for Rosie Maternity Hospital in Cambridge and develop and compare adaptive interventions | The existing building is unable to shed heat so that recommended maximum internal temperatures are reached in relatively mild external conditions. Adaptations to the building will be required to maintain resilience to increasing temperatures. | Multizone thermal dynamic model developed from measured temperatures | Temperature maintenance | N/A | N/A |
|
| Development of preparedness checklists and assessment tools | |||||||||
| Dobalian et al. | 2016 | USA | To develop a hospital preparedness tool for six domains or ‘mission areas’ | Tool serves as comprehensive assessment for hospital preparedness | Structured assessment of 140 Veteran Affair Hospitals, two-stage confirmatory factor analysis | Six critical mission areas: programme management, incident management, safety and security, resiliency and continuity, medical surge, support to external requirements | N/A |
|
N/A |
| Goncalves et al. | 2019 | Spain | To adapt and validate the short-form version of the Benchmark Resilience Tool into Spanish language and to explore its relationship with safety climate | The instrument fulfils the psychometric criteria to evaluate resilience in healthcare and nuclear organizations in Spain | Survey of workers in the healthcare and nuclear energy sectors | Short-form version of the Benchmark Resilience Tool (BRT-13B) | Four Cornerstones of Resilience (Hollnagel et al. 2006) |
|
Absorption |
| Zhong et al. | 2014a | China | To validate a framework of key indicators of hospital resilience | Identification of a four-factor structure of hospital resilience: Emergency medical response capability, disaster management mechanisms, hospital infrastructural safety and disaster resources with good internal consistency | Survey among 41 tertiary hospitals in China; factor analysis | Eight key domains: hospital safety standard and procedures, emergency command, communication and cooperation system, disaster plan, disaster resource stockpile and logistics management, emergency staff capability, emergency services and surge capability, training and drills, and recovery and adaptation strategies | Four criteria of disaster resilience (robustness, resourcefulness, redundancy and rapidness) (Zhong et al. 2014b) | Uncertainties | N/A |
| Zhong et al. | 2015 | China | To develop a framework of key indicators of hospital resilience | Framework identified a comprehensive set of indicators for hospital resilience, 60 of 75 proposed measures reached consensus. | Modified Delphi consultation of experts; Likert scale evaluation of proposed measures | ||||
Table 2.
Overview of aims, methods, concepts used and dimensions of resilience addressed by mixed methods research papers (n = 9)
| Author | Year | Country | Research objective | Key findings | Study design and data source | Operationalization of resilience | Conceptual framework used | Management capacity dimensions | Resilience outcome dimensions |
|---|---|---|---|---|---|---|---|---|---|
| Assessing national-level health system resilience in context of a specific crisis | |||||||||
| Ammar et al. | 2016 | Lebanon | ‘To assess the resilience of the Lebanese health system in the face of an acute and severe crisis and in the context of political instability’. | Institutions sustained performance and even improved during the crisis | Case study approach with descriptive statistics of routine data | Indicators on human resources, financing, governance, service provision, utilization, expenditure, morbidity/mortality and prevention of outbreaks | input–process–out- put/outcome model of a health system to measure capacities and performance | Knowledge, Uncertainties, Interdependence, Legitimacy |
|
| Orru et al. | 2018 | Estonia | To clarify the factors determining the effectiveness of the Estonian health system in assessing and managing the health risks of climate change | The health effects of climate change have not been mainstreamed into policy. | Document review; expert interviews; population survey | Indicators in five key areas: Policies and programmes; Responses and protective measures; Monitoring and information; Admin. capacity and culture; Issue salience and contextual drivers | WHO Operational Framework for Building Climate Resilient Health Systems (World Health Organization 2015) |
|
N/A |
| Thomas et al. | 2013 | Ireland | To develop a framework for health system resilience in economic crises and to apply to Irish health system | Irish health system performed well for adaptive resilience, with mixed evidence for adaptive and transformatory resilience. | Quantitative indicators calculated from gov. documents; Semi-structured interviews | Indicators in for three elements: Financial, adaptive and transformatory resilience | Own framework | N/A |
|
| Assessing health service delivery in context of a specific crisis | |||||||||
| Gizelis et al. | 2017 | Liberia | To assess impact of Ebola epidemic on maternal delivery services | Decline in the use of public hospital deliveries, increase of deliveries in private facilities and equal levels of home births. Private sector played critical role during outbreak. |
|
Maternity service utilization | N/A |
|
|
| Kozuki et al. | 2018 | South Sudan | To document the operations of an Integrated Community Case Management programme during an acute crisis and to assess the programme’s ability to continue operations. | community health workers continued to provide treatment for childhood illnesses during an acute emergency and service provision recovered faster to pre-crisis levels than the formal health sector. | Interviews and focus groups with key stakeholders; routine programme data | Process evaluation of response to crisis, including quant. indicators: reporting, contact, treatment, supervision & referral rates | N/A | N/A | Absorption |
| Ray-Bennett et al. | 2019 | Bangladesh | To study the reproductive health challenges at the facility and community levels during the 2016 flood in Belkuchi, Bangladesh | Major challenges of a lack of services and a shortage of medicines, as well as inadequate equipment and insufficient trained health workers were found during both the dry and wet season |
|
|
N/A | Uncertainties | Absorption |
| Witter et al. | 2017 | Uganda, Sierra Leone, Zimbabwe, Cambodia | To analyse the impact of different kinds of shocks on health staff (their vulnerabilities)—but also how they coped (their adaptive capacity). | The impact of shocks and coping strategies are similar between conflict/post-conflict and epidemic contexts—particularly in relation to physical threats and psychosocial threats—while all contexts create challenges for working conditions and remuneration |
|
Challenges faced in the job and during crisis as well as coping strategies | N/A | N/A |
|
| Development of preparedness checklists and assessment tools | |||||||||
| Paterson et al. | 2014 | Canada | Development of a toolkit to assess health care facility resiliency to climate change | ‘The toolkit helps health care facility officials identify gaps in climate change preparedness, direct allocation of adaptation resources and inform strategic planning to increase resiliency to climate change’. | Literature review, workshops | Indicators in two areas: (1) Emergency management and strengthening health care services; (2) Climate-proofing and greening operations | N/A |
|
N/A |
Table 3.
Overview of aims, methods, concepts used and dimensions of resilience addressed by qualitative research papers (n = 16)
| Author | Year | Country | Research objective | Key findings | Study design and data source | Conceptual framework used | Management capacity dimensions | Resilience outcome dimensions | |
|---|---|---|---|---|---|---|---|---|---|
| Assessing national-level health system resilience in context of a specific crisis | |||||||||
| Ager et al. | 2015 | Nigeria | To identify key pathways of threat to provision, response and adaption for health service resilience in Nigeria in context of Boko Haram | Transport restrictions, health worker migration and suspension of external programmes identified as threat to provision. Political will, indigenous staff commitment and policy changes supported health system recovery/function. | Structured Interviews, systems dynamics analysis with group model building approach | UK Government Humanitarian Policy (DfID 2011) | N/A |
|
|
| Alameddine et al. | 2019 |
|
To assess the ‘validity and utility of a capacity-oriented resilience framework […] in Lebanon and Jordan in the context of the Syrian crisis’. | ‘We find that UNRWA systems in Lebanon and Jordan were broadly resilient, deploying diverse strategies to address health challenges and friction between host and refugee populations’. | Semi-structured interviews with health professionals in primary care and management functions | ‘capacities’ framework (Blanchet et al. 2017) |
|
|
|
| Ling et al. | 2017 | Liberia | ‘To understand how a health system adapts to crisis and how the priorities of different heath system actors influence this response’. | Although the Ebola epidemic stimulated some positive adaptations in Liberia's health system, building a resilient health system will require longer-term investments and sustained attention | Thematic analysis of semi-structured interviews and focus group discussions | ‘resilience index’ framework (Kruk et al. 2015) |
|
|
|
| Assessing health service delivery in context of a specific crisis | |||||||||
| Landeg et al. | 2019 | United Kingdom | ‘To assess the health care system impacts associated with the December 2013 east coast flooding in Boston, Lincolnshire, in order to gain an insight into the capacity of the health care sector to respond to high-impact weather’. | ‘The health care sector appears to have limited capacity to respond to weather-related impacts and is therefore unprepared for the risks associated with a future changing climate’. | Semi-structured interviews with key decision-makers;Document analysis | N/A |
|
|
|
| Ridde et al. | 2016 | Burkina Faso | To describe the management of the Ouagadougou Terrorist attack in January 2016 from the standpoint of health system resilience. | Identified strengths were an emergency response plan which had been put in place and available blood bank and psychological services. Challenges included the development, application and coordination of framework documents for financial, material and human resources. | Observations and expert interviews structured as anecdotal event report | ‘Resilience index’ framework (Kruk et al. 2015) |
|
|
|
| Back et al. | 2017 | United Kingdom | ‘To examine escalation policy in theory and practice, using resilient health care principles to identify opportunities for improving the way escalation is planned and managed’. | Under pressure it may be difficult to dynamically reconfigure resources, such as staff and equipment and lead to informal management of processes not specified in the policies. |
|
Concepts for Applying Resilience Engineering (CARE) model of resilient healthcare (Anderson et al. 2016) | Uncertainties | Adaptation | |
| Errett et al. | 2018 | Canada | ‘To identify maritime transportation disruption impacts on available health care supplies and workers necessary to deliver hospital-based acute health care in geographically isolated communities post-disaster’ | Critical vulnerabilities to care delivery include ‘lack of information about the existing supply chain, lack of formal plans and agreements, and limited local supply storage and workforce capacity’. | Semi-structured key informant interviews | N/A |
|
N/A | |
| Taking a community resilience perspective | |||||||||
| Alonge et al. | 2019 | Liberia | ‘To understand key factors that constitute community resilience and their role in responding to the EVD outbreak in Liberia’. | ‘Efforts to systematically build responsible leadership and social capital at community level, including those that strengthen bonds in communities and trust across key actors in the health systems, are needed to address health shocks like EVD outbreaks’. | Key informant interviews and a national stakeholder meeting | N/A | Legitimacy |
|
|
| Health workforce issues | |||||||||
| Gilson et al. | 2017 | Kenya; South Africa | To compare experiences from district health systems in Kenya and South Africa order to reveal patterns and insights for everyday resilience | Stable governance structures and adequate resources influence everyday resilience, however empowerment of leaders, mindful staff engagement and social networks also appear important. | Case study methodology: synthesis of document reviews, interviews, group discussions and observations | Vulnerability reduction framework (Béné et al. 2012) Everyday resilience (Barasa et al. 2017) |
|
|
|
| Raven et al. | 2018 | Nepal; Sierra Leone | To assess how health workers cope in times of crisis and how they can best be enabled to continue their work. | ‘In both contexts, health workers demonstrated considerable resilience in continuing to provide services despite limited support’. |
|
N/A |
|
|
|
| Russo et al. | 2016 | Portugal | To ‘explore physicians’ perceptions of the changes brought on by the [economic] crisis and associated austerity measures to the market for medical services, as well as to their working routines, remuneration and intention to leave the sector’. | The economic crisis brought considerable changes for the health system, however insights to existence of resilience merged | Semi-structured interviews with physicians | N/A | N/A |
|
|
| Thude et al. | 2019 | Denmark | ‘To understand how the staff at the two wards with challenged leader teams coped with everyday work and whether the way in which the staff handled the challenges was resilient’. | ‘The staff at both wards were handling the everyday work in a resilient way. […] To increase the resilience in an organisation, leaders should acknowledge the need to establish strong emotional ties among staff and at the same time ensure role structures that make sense in the everyday work’. | Semi-structured interviews with healthcare staff | N/A | N/A | Absorption | |
| Development of preparedness checklists and assessment tools | |||||||||
| Toner et al. | 2017 | USA | To use experiences from communities affected by Hurricane Sandy 2012 for developing a checklist outlining action steps for assessing and strengthening communities' health sector resilience | Description of a conceptual map of health sector resilience, with key findings organized in eight themes. Identification of recommended actions for improvement of health sector resilience at local level |
|
N/A |
|
|
|
| O'Sullivan et al. | 2013 | Canada | To explore the complexity of disasters at the micro level and to determine levers for action to facilitate collaborative action and promote health among high risk population | ‘Promoting population health in disaster context requires shifting from risk management to resilience, […] from command and control models to collaboration’. | Community-based participatory research design with focus groups | Resilient communities framework (Norris et al. 2008)Functional needs framework (Kailes and Enders 2007) |
|
N/A | |
| Khan et al. | 2018 | Canada | ‘To describe the essential elements of a resilient public health system and how the elements interact as a complex adaptive system’. | Eleven essential elements for public health emergency preparedness were identified, and a conceptual framework developed with ethics and values at its core. | Focus groups using Structured Interview Matrix facilitation technique | N/A |
|
N/A | |
| Meyer et al. | 2018 | USA | To identify and integrate lessons from response to the EVB epidemic into an actionable checklist. | ‘Health care facilities shouldered much of the response, and even those facilities with designated treatment units had to adapt in real time’. Experiences can help inform future response. | Semi-structures key informant interviews | N/A |
|
|
|
Assessing national-level health system resilience in context of a specific crisis
Of the eight studies which assessed an entire, national health system in the context of a particular crisis, two studies took a purely quantitative approach: Fukuma et al. (2017) assessed Japan’s health system responsiveness and resilience after the Great East Japan Earthquake and Watts et al. (2018) assessed the resilience of 101 health systems in the context of climate change. Fukuma et al. (2017) operationalized resilience by using composite routine data indicators during the time of crisis, including: service utilization, cause-specific mortality rates incl. suicides, number of hospitals, health expenditures, human resources and immunization coverage. Watts et al. (2018) assessed resilience by surveying for the presence of specific policy efforts and strategies in the context of climate change at a national level.
Three further studies assessed the resilience of a health system at the country level using a mixed methods approach. Ammar et al. (2016) studied the Lebanese health system in the context of the Syrian refugee crisis using a case study approach. Orru et al. (2018) assessed the ways in which the Estonian health system was able to assess and manage the health risks of climate change using a combination of document review, expert interviews and population survey data as applied to the WHO Operational Framework for Building Climate Resilient Health Systems (World Health Organization 2015). Thomas et al. (2013) assessed the performance of the Irish health system in the face of the economic crisis by applying quantitative indicators developed from their own resilience framework to government documents and supplementing these with semi-structured interviews.
Finally, three qualitative studies considered national health system resilience. Ager et al. (2015) assessed key barriers to the provision of responsive service in the context of Boko Haram in Nigeria, Alameddine et al. (2019) assessed the resilience of Lebanon and Jordan’s health systems in the context of the Syrian crisis and Ling et al. (2017) assessed the resilience of Liberia’s health system during the Ebola crisis. All three studies used semi-structured interviews with health professionals and other key health stakeholders for data collection, with Ling et al. (2017) complementing these with focus group discussions.
Out of these eight studies, all studies except one (Fukuma et al. 2017) applied a specific conceptual framework to study resilience. However, the frameworks used in the other studies vary, including frameworks developed by international or development agencies, such as the World Health Organization or the United Kingdom’s Department for International Development (Ager et al. 2015; Orru et al. 2018; Watts et al. 2018), general health system frameworks (Ammar et al. 2016) and resilience frameworks developed in the academic literature (Thomas et al. 2013; Ling et al. 2017; Alameddine et al. 2019).
Assessing resilience of health service delivery
Ten studies focused on the resilience of health service delivery. Six studies assessed the delivery of emergency services, three focused on the delivery of maternal health services, while one considered the continuity of a community health worker programme.
Two quantitative studies from the USA take a specific look at the delivery of emergency services: Radcliff et al. (2018) analyse ambulatory care measures during and after a storm, while Simonetti et al. (2018) model the potential of the US blood supply system during an emergency. Both make use of available administrative data, with Radcliff et al. (2018) relying in utilization data from Veterans Affairs clinics and Simonetti et al. (2018) using data on the national availability of blood stocks. The provision of emergency services during a crisis is also explored in four qualitative studies. Two of these assess service provision in the context of a particular crisis: Ridde et al. (2016) describe the emergency response to the Ouagadougou Terrorist attack in Burkina Faso, using a mixture of observations and expert interviews as their data source and structuring insights around Kruk et al.’s (2017) ‘resilience indicators’ framework. Landeg et al. (2019) assess the emergency response to localized flooding in the UK using semi-structured interviews with decision-makers and document analysis. Finally, two qualitative studies explore the functionality of emergency service processes: while Back et al. (2017) use policy analysis and observation to examine escalation policies in UK hospitals, Errett et al. (2019) use semi-structured interviews with key informants to identify the impact of disruption of maritime transportation on the provision of emergency services during a disaster.
Being the only purely quantitative study to do so, Sochas et al. (2017) analysed the utilization of reproductive, maternal and neonatal health services in Sierra Leone in the context of the Ebola crisis using antenatal health service utilisation data. Gizelis et al. (2017) also assessed the impact of the Ebola epidemic on maternity delivery services, using a mixed methods approach by complementing maternity service utilization data from population surveys with semi-structured interviews and focus group discussions. Ray-Bennett et al. (2019) looked at the provision of reproductive health services in the context of flooding in Bangladesh, applying a structured facility assessment tool complemented by structured interviews with patients.
Kozuki et al. (2018) use a process evaluation methodology to document the ability of an integrated community case management programme to continue operation during the active conflict of 2013 and 2014 in South Sudan. The authors use routine programme data, including reporting, supervision, contact, treatment and referral rates, as well as interviews and focus groups with key stakeholders to evaluate the programme’s resiliency.
Only two of these studies (Ridde et al. 2016; Back et al. 2017), both using qualitative methodologies, apply a specific framework of health system resilience. All quantitative studies and one mixed methods study focus on the absorptive capacities of service delivery, while the other studies address a more varied set of resilience dimensions.
Health workforce issues
A total of seven studies were identified which address aspects of health workforce resilience. These include studies both from the tradition of ‘resilience engineering’, as well as research influenced by the concept of ‘everyday resilience’.
One quantitative and one mixed methods study were conducted in the field of resilience engineering and safety research. Falegnami et al. (2018) surveyed the resilience of anaesthesia professionals in different work conditions in Italy using the four cornerstones of resilience framework (Hollnagel 2009). In the same setting, Patriarca et al. (2018) applied the functional resonance analysis method to explore the potential of the tool in enhancing the resilience of anaesthesia practices, drawing on documentary studies, interviews, observations and patient pathway modelling to do so.
Three studies considered health workforce issues on the context of a specific crisis. Applying a mixed methods approach, Witter et al. (2017) explored the impact of shocks on the health workforce across different contexts in Uganda, Sierra Leone, Zimbabwe and Cambodia, with a particular focus on vulnerabilities and coping strategies employed. The authors employed a mixture of methods for analysis, including surveys, human resource data, document review and qualitative interviews. Also taking a cross-national perspective, Raven et al. (2018) conducted observations and in-depth interviews with healthcare workers and management in Sierra Leone during the time of the Ebola crisis and in Nepal during a major earthquake to explore coping strategies of staff in both settings. In Portugal, Russo et al. (2016) explored physician’s perceptions of the changes in their work environment during the economic crisis in semi-structured interviews.
Finally, two qualitative studies take an ‘everyday resilience’ perspective to understand the ability of health workers in dealing with everyday challenges. Comparing experiences in Kenya and South Africa, Gilson et al. (2017) synthesize information from documents, interviews, group discussions and observations to understand factors influencing everyday resilience of staff. In Denmark, Thude et al. (2019) conducted semi-structured interviews with healthcare staff to explore the resilience of the workforce faced with challenges in their work environment, including changing leadership structures.
Only two of these studies (Gilson et al. 2017; Falegnami et al. 2018) make use of an explicit resilience framework in their analysis. The dimensions assessed in individual studies varies: while Gilson et al. (2017) and Raven et al. (2018) explore a broad range of management capacities and resilience outcomes, the other five studies focus on only one of these two aspects, with three studies restricted in their analysis to a single outcome dimension (Witter et al. 2017; Patriarca et al. 2018; Thude et al. 2019).
Taking a community resilience perspective
Three studies approached health system resilience from a community perspective. Cohen et al. (2019) quantitatively analyse the relationship between community resilience and the public’s confidence in the availability of healthcare services during emergency situations in Israel. Data for this study were conducted using the conjoint community resilience assessment measurement tool (Leykin et al. 2013) in a household survey. Alonge et al. (2019) apply a qualitative approach to understand the relationship between community resilience and health system resilience. Combining information from key informant interviews and a national stakeholder meeting, they look at the contribution of responsible leadership and social capital into the resilience of the health system during the Ebola outbreak in Liberia. Finally, Andrew et al. (2016) take a slightly different approach to the issue of community resilience, by focusing on the resilience of community organizations involved with the relief efforts in the aftermath of the Thailand floods in 2011. Applying Bruneau et al. (2003) framework on the seismic resilience of communities, the authors quantitatively assess whether the bonding or the bridging effect made a larger contribution on the ability of organizations to deliver essential services after the crisis.
Both quantitative community resilience studies made use of an explicit framework for their analysis, while the qualitative study did not. While one study (Cohen et al. 2019) focused entirely on dimensions of resilience management capacities, the other two studies explored a mix of management capacities and outcomes.
Infrastructure and thermal resilience
Three studies assessed the infrastructure and thermal resilience of hospitals, taking a purely quantitative approach. Resilience in this context is understood as the capability of buildings to withstand extreme conditions such as heat or earthquakes. Iddon et al. (2015), Lomas et al. (2012) and Short et al. (2015) assessed the thermal resilience for specific building styles of wards in the UK in order to ensure climate change resiliency. None of these studies used specific conceptual frameworks for their analysis. In terms of the dimensions of resilience addressed, they focused entirely on dimensions of outcome, rather than management capacities. All three studies considered ways in which hospital infrastructure was able to absorb temperature changes, with two studies additionally assessing the potential for adaptation in response to these changes.
Development of preparedness checklists and assessment tools
A total of nine articles described the development of checklists to prepare for future catastrophic events or tools with which such preparedness can be measured. These have been developed at different levels: six studies focused on healthcare facilities and hospitals, two studies considered communities, while one study developed a conceptual framework at the national level.
Four articles described the quantitative development of checklists or measurement tools for assessing resilience of healthcare facilities. Dobalian et al. (2016) developed a general hospital preparedness tool, while Zhong et al. (2015) developed a framework for measuring hospital resilience and applied it to 41 tertiary care hospitals in a province in China (Zhong et al. 2014a). Goncalves et al. (2019) adapted and validated the short-form version of the Benchmark resilience tool for assessing the resilience of healthcare organizations. Using a mixed methods approach, Paterson et al. (2014) developed a toolkit for assessing the resiliency of healthcare facilities in the context of climate change. The methods for development differ: while Zhong et al. (2015) and Paterson et al. (2014), respectively, used a Delphi consultation and workshops for an expert evaluation of proposed domains, Dobalian et al. (2016), Goncalves et al. (2019) and Zhong et al. (2014a) used psychometric assessments to assess validity and reliability. One of the instruments was operationalized as a survey of workers (Goncalves et al. 2019), while the other three carried out assessments at the organizational level—either by external evaluation (Dobalian et al. 2016), as a survey completed by managers of the facility (Zhong et al. 2014a, 2015) or as a toolkit for facilities aiming to improve their climate resiliency (Paterson et al. 2014). Finally, Meyer et al. (2018) conduct semi-structured interviews with key informants involved in the Ebola response in the USA to develop an actionable checklist to enable preparedness for future responses.
Two further papers used a qualitative approach to develop checklist for enhancing community resilience in a health system context. O’Sullivan et al. (2013) identify levers to promote community resilience for health during disasters using a community-based participatory research approach. Toner et al. (2017) used experiences from Hurricane Sandy collected through key informant interviews and focus groups to develop a checklist for assessing and strengthening communities’ health sector resilience.
Finally, Khan et al. (2018) conducted focus groups to develop a framework comprising of essential elements of a resilient public health system in during emergencies, using the lens of complex adaptive health systems. They discuss the importance of recognizing the interconnectedness of actors and processes during an emergency response, acknowledging that these dimensions, while crucial, are particularly difficult to measure and quantify.
Many of these studies understandably did not use a specific resilience framework, as part of the research aim was to develop key dimensions of resilience in a particular context. However, three studies did use frameworks to guide the selection of their proposed dimensions (Zhong et al. 2014a, 2015; Goncalves et al. 2019) or the development of topics for discussion in focus groups (O’Sullivan et al. 2013). Checklists tended to focus on measuring the management capacities of facilities, organizations and systems, with a noticeable trend towards a more diverse set of dimensions among the qualitative studies. Only two studies (O’Sullivan et al. 2013; Khan et al. 2018) considered assessment of the system’s ability for absorption and adaptation.
Conceptual analysis of key empirical studies
Conceptual frameworks used
Across the empirical studies, a specific framework for assessing resilience was used by four quantitative studies, two mixed methods studies and seven qualitative studies. The types and disciplinary origins of the frameworks differed widely. Of the concepts developed in the health systems resilience discourse, the ‘resilience index’ framework (Kruk et al. 2017), ‘resilience capacities’ framework (Blanchet et al. 2017) and ‘everyday resilience’ framework (Barasa et al. 2017) were used. From the resilience engineering discourse, the Concepts for Applying Resilience Engineering (CARE) model (Anderson et al. 2016) and the Four Cornerstones of Resilience framework (Hollnagel 2009) were applied. Notably, three frameworks from the area of community resilience were used: CCRAM model (Leykin et al. 2013), framework to assess seismic resilience of communities (Bruneau et al. 2003) and the resilient communities framework (Norris et al. 2008). Other frameworks used included the UK government’s humanitarian policy (DfID 2011) and the WHO Operational Framework for Building Climate Resilient Health Systems (World Health Organization 2015). Only two frameworks (Hollnagel 2009; Kruk et al. 2017) were used twice, all other studies used distinctive frameworks for their analysis.
Dimensions of resilience addressed
We used the framework formulated by Blanchet et al. (2017) as an analytical lens allows for a more in-depth analysis of the content and dimensions of resilience addressed across the empirical papers using the definitions of management capacities and levels of resilience provided in Box 1. Across the empirical papers, 12 studies focused exclusively on resilience domains in the ex ante ‘management capacities’ side of Blanchet et al.’s resilience definition, while 14 studies focused exclusively on absorptive, adaptive or transformative levels of the resilience process. Fourteen studies considered both management capacities and resilience levels. Qualitative studies more often considered both management capacities and resilience levels, while quantitative studies more often exclusively focused on one of the two (Figure 4a). Among the management capacities, the dimension of ‘uncertainty’ was most frequently assessed by all types of research, followed by dimensions of ‘interdependence’, ‘knowledge’ and ‘legitimacy’, in that order (Figure 4b).
Figure 4.
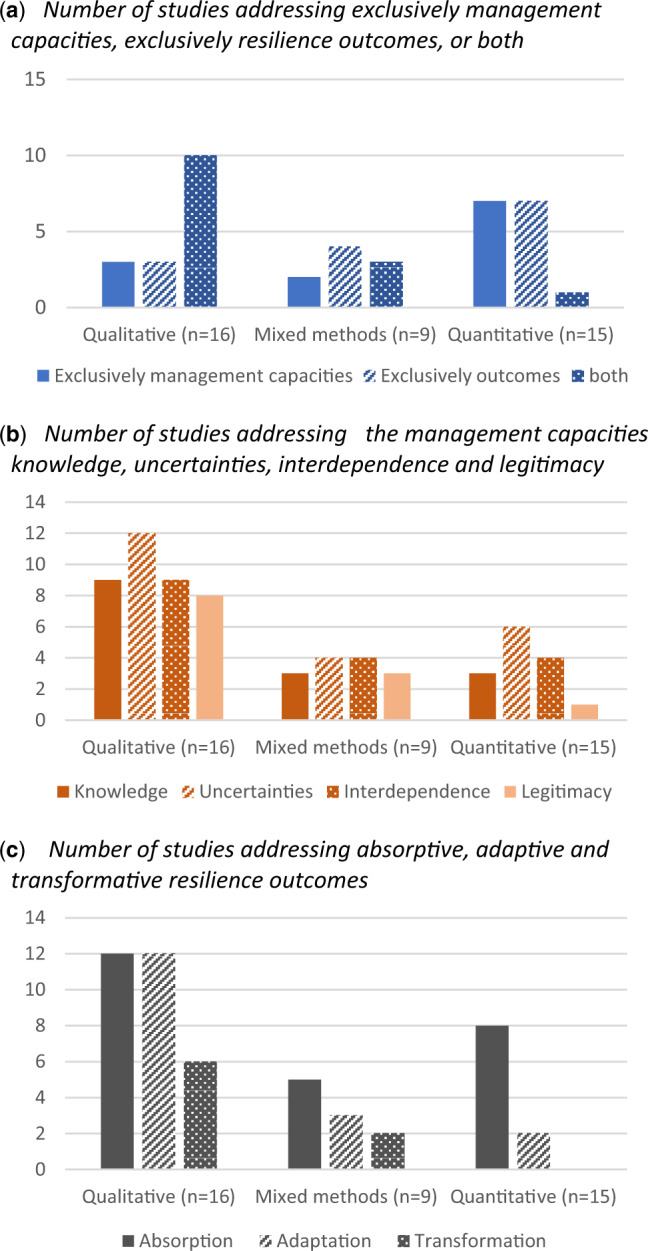
(a–c) Domains of resilience addressed by key papers (n = 40), by research methodology.
Among the ex post resilience levels, ‘absorptive capacities’ was most frequently addressed across research types, although qualitative research explored ‘absorptive capacities’ and ‘adaptive capacities’ to an equal extent (Figure 4c). Only a limited number of quantitative and mixed methods studies considered the ‘adaptive capacities’ and ‘transformative capacities’ dimensions of health system resilience.
Looking across management capacities and resilience levels, qualitative research was able to address a much broader range of dimensions than quantitative research, with individual studies often exploring multiple dimensions of the resilience concept (Figure 4b and 4c).
Quantitative indicators used
A total of 24 studies used quantitative indicators to measure different aspects of the resilience concept, with several studies using multiple indicators across multiple domains of responsiveness (Table 4). The reported indicators were collected using different data collection strategies, including the use of routine data, observational data and primary survey data. The indicators further differed in the level at which data were collected, spanning national, organizational, staff and patient/population levels. Across the ‘management capacities’ domains, several indicators at different levels of data collection addressed the domains of knowledge, uncertainties and interdependence. However, only two indicators, both collected at population level, captured the legitimacy dimension. Across the ‘levels of resilience’ domains, several studies used indicators across different levels of data collection for the ‘absorption’ domain. However, only three indicators were used for the ‘adaptation’ domain, collected at national and organizational level, while no indicators were identified for the ‘transformation’ domain.
Table 4.
Resilience indicators used in quantitative and mixed methods studies (n = 24), by resilience domain and level of data collection
| Level of data collection |
||||||
|---|---|---|---|---|---|---|
| National level | Organizational level | Staff level | Patient/ Population level | |||
| Management Capacities | Knowledge |
|
|
|
||
| Uncertainties |
|
|
|
Conjoint Community Resilience Assessment Measurement (CCRAM) tool Items 3, 8, 17 and 24 (Cohen et al. 2019)b | ||
| Interdependence |
|
|
Short-form version of the Benchmark Resilience Tool Question 4 (Goncalves et al. 2019) b | Conjoint Community Resilience Assessment Measurement (CCRAM) tool (Cohen et al. 2019)b | ||
| Legitimacy | N/A | N/A | N/A |
|
||
| Levels of Resilience | Absorption | [R] Changes in population-level health indicators (Ammar et al. 2016; Fukuma et al. 2017)a:
|
|
Short-form version of the Benchmark Resilience Tool Questions 3 and 7 (Goncalves et al. 2019)b | Health service utilisation during a disaster and reasons for non-utilisation (Ray-Bennett et al. 2019)b | |
| Adaptation | Indicators for assessing adaptive financial resilience (Thomas et al. 2013)a:
|
Modelling studies effect of different adaptive scenarios health facility temperatures (Lomas et al. 2012; Short et al. 2015)a | N/A | N/A | ||
| Transformation | N/A | N/A | N/A | N/A | ||
Routine data, document review or observation;.
Survey data.
Discussion
The concept of health system resilience has soared in popularity in the health system field over the last years, not just in the theoretical or political discourse but also as an object of empirical inquiry. Its application has been incredibly diverse, with research from different disciplines applying the concepts in different healthcare sectors and in various settings. This diversity is not itself problematic. However, this review has demonstrated that empirical studies fundamentally differ in the way that resilience is understood in a health system context.
In terms of the content of the studies, much empirical research focuses on service delivery, health workforce or governance issues, whereas resilience of other health system building blocks is either barely studied, such as health financing, or only studied in high-income countries, as is the case of health information systems. This shows a distinct gap between the concepts and the operationalization of resilience in the context of health system research. If research on health system resilience is to live up to recent comprehensive definitions, the focus has to widen: all building blocks are interlinked and essential for well-functioning health systems, and should therefore not be analysed in singularity, but be considered jointly when assessing health system resilience.
Furthermore, despite much theoretical work on the dimensions which constitute health system resilience, we found that most of the empirical literature only addressed particular aspects. Applying the dimensions outlined by Blanchet et al. (2017), we found that the importance of developing legitimate institutions appears to be neglected in empirical research. This is particularly concerning given that a lack of in healthcare institutions has recently emerged as one of the key barriers to the continued functioning of the health system, e.g. in the context of the Ebola outbreak (Kittelsen and Keating 2019). The ability of health systems to demonstrate transformative capacities has been similarly under-evaluated, especially in quantitative research. Very few empirical studies took an approach to resilience that takes into account the various nuances in the conceptualization of the term which have recently emerged. This trend appeared to be particularly pronounced in those studies with a quantitative or mixed methods approach.
Thus, there is a mismatch between the conceptual models of health system resilience and the way resilience is understood and applied in empirical research both in terms of the breadth of health system factors considered and in terms of the resilience dimensions which are taken into account. Part of the issue may be that the empirical literature assessed in this review comes from a broad range of disciplines, with differing traditions of how ‘resilience’ is understood. While different traditions can offer unique and potentially complementary perspectives on the topic of resilience, this underlines the importance of more clarity in the empirical literature about which concepts and definitions are applied, and how these are then operationalized.
However, only very few empirical studies make use of an explicit conceptual framework for collection or analysis of data, thus not linking research objectives to the rich theoretical body of work on how resilience can be understood in a health system context. Arguably, those studies assessing resilience at a national level were most cognizant of using conceptual frameworks for their analysis. Our review showed that these studies were best able to capture the multiple dimensions of health system resilience. While several other studies aimed to measure health system resilience, they subsequently operationalized this concept in a very narrow way, e.g. by measuring only health service utilization, infrastructure resilience or emergency preparedness. Encouraging the use of an explicit framework for health system resilience could help to strengthen the links between the conceptualization and the operationalization of resilience, thus improving our understanding of health system resilience in different contexts and settings.
Our review further demonstrates that qualitative articles tend to employ a more comprehensive approach to the resilience concept than quantitative studies, which are often limited by availability of data and indicators to few aspects of resilience. The mismatch between concepts and research, therefore, appears to lie not in a lack of appreciation for the complexities of the resilience concept, but rather in a lack of measurable indices which reflect this complexity. While the proposed resilience index (Kruk et al. 2017) specifies a list of potentially measurable indicators, so far these have only been operationalized in qualitative research. Similarly, the ‘resilience capacities’ framework specified by Blanchet et al. (2017), and the ‘everyday resilience’ framework by Barasa et al. (2017) have been operationalized exclusively in qualitative research. All identified quantitative studies have utilized frameworks originating in discourses tangential to the health system resilience discourse.
Yet so far there has been no discussion about which aspects of the health system resilience frameworks are actually measurable. Within the ‘resilience capacities’ framework, the identified studies demonstrate that it is possible to measure ‘absorptive’ aspects by comparing levels of service provision and utilization in different circumstances. However, this is more challenging for ‘adaptive’ and ‘transformative’ aspects. Understanding whether a health system has truly transformed itself in response to a challenge needs to take into account multiple contextual factors and thus lends itself more naturally to be answered by qualitative methods and policy analysis, but also to complexity science. Equally, studies were able to quantitatively assess the presence or absence of preparedness plans to deal with uncertainties and data collection mechanisms for an improved knowledge of potential challenges, but quantifying the ability to handle cross-scale dynamics and develop legitimate institutions proved to be more difficult to capture. Incidentally, the identified studies developing resilience checklists and measurement tools all took a very narrow perspective of resilience by focusing on single healthcare facilities and organizations.
The key question in the development of a comprehensive resilience index, or a measure that allows for effective combination of quantitative and qualitative aspects, becomes whether the requirements to create a comparable measurement tool can be reconciled with the very broad and comprehensive definition of resilience which has emerged from an understanding of health systems as complex adaptive systems. According to Haldane et al. (2017) the resilience concept ‘should […] not be prescriptive, but have breadth and flexibility, recognize complexity, consider shocks and cumulative stresses, attempt to deal with disruptions and anticipate future failures’. It appears that, so far, the qualitative literature has been more successful in translating such a comprehensive framework into research practice, while quantitative studies have been limited both by theoretical models and a lack of appropriate data with which to measure resilience. Thus a key task for future researchers in the resilience field will be not only how the resilience concept can be operationalized, but—acknowledging that quantitative assessment of resilience in its entirety is illusionary—determine how measureable aspects can be combined with qualitative aspects in a way that allows for an assessment of health system resilience as a dynamic, complex phenomenon. Thus further research is required for the development of an operational framework on health system resilience which seamlessly integrates both qualitative and quantitative evidence; knowledge from existing guidelines on integrating quantitative and qualitative knowledge, e.g. in the realm of assessing the effectiveness of complex interventions, could be utilized for this purpose (Noyes et al. 2019).
Our review adds to the existing conceptual review by Turenne et al. (2019), who argue that the concept of health system resilience is still in infancy. We demonstrate the implications of this conceptual immaturity on existing empirical research: while the qualitative literature has explored the notion of health system resilience in its broad definition, the quantitative literature has been limited by the lack of clearly defined characteristics, preconditions and limits of the concept.
Our review makes a substantial contribution to the health systems research literature by analysing the operationalization of the health system resilience concept in empirical studies. Due to our inclusive search and broad inclusion criteria, we were able to consider a broad range of relevant articles from multiple disciplines and thus demonstrate the influence of other disciplines in the health systems research field. However, as search terms were geared to finding articles which specifically referred to the resilience concept, we may have missed empirical studies which operationalized aspects of resilience, but used different terminology. Further research could specifically identify such studies by using elements of the resilience definition instead of merely using the term itself. This could also help to better gain an understanding of how the concept of resilience overlaps with other health systems concepts such as health system strengthening or health system responsiveness and map potential synergies in assessment. We also did not include secondary research or grey literature in our review, which may provide further useful information on the operationalization of the resilience concept. Further research is needed to combine and integrate knowledge from these diverse sources in a comprehensive assessment framework.
A further limitation of our study is the initial exclusion of items based on titles, which was necessary due to the sheer number of results. This may have excluded several studies in associated disciplines, such as those relating to community resilience, which are of importance to the health systems resilience discourse. Findings of our review should be complemented by reviews of the resilience concept in other disciplines to check for congruence.
Conclusion
The health systems research community has made substantial advances in the conceptualization of health system resilience and its potential for the analysis of health systems in changing environments. However, the empirical literature has not yet caught up with the complexities of the concept: there is a mismatch between the nuances and the breadth of the concept at a theoretical level and the way it has been operationalized in empirical studies. In order to do justice to the complexities of the resilience concept, knowledge from both quantitative and qualitative research traditions should be integrated in a way that resilience as a complex, adaptive phenomenon. Only once a comprehensive assessment framework has been defined and applied across different research contexts will the theoretical ‘resilience idea’ be able to more convincingly prove its usefulness for the research community.
Supplementary Material
Acknowledgements
The authors are supported by a grant from the German Federal Ministry for Education and Research (BMBF) in the scope of the project RESPOND (Grant number: 01GY1611). Further grants are received by the German Science Foundation (DFG) in the scope of the Research Unit PH-LENS and its subproject NEXUS (Grant no: FOR 2928 / BO 5233/1-1). The funders had no influence on study design, analysis or decision to publish.
Conflict of interest statement. None declared.
Ethical approval. No ethical approval was required for this study.
References
- Ager AK, Lembani M, Mohammed A. et al. 2015. Health service resilience in Yobe state, Nigeria in the context of the Boko Haram insurgency: a systems dynamics analysis using group model building. Conflict and Health 9:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alameddine M, Fouad FM, Diaconu K. et al. 2019. Resilience capacities of health systems: accommodating the needs of Palestinian refugees from Syria. Social Science & Medicine 220: 22–30. [DOI] [PubMed] [Google Scholar]
- Alonge O, Sonkarlay S, Gwaikolo W. et al. 2019. Understanding the role of community resilience in addressing the Ebola virus disease epidemic in Liberia: a qualitative study (community resilience in Liberia). Global Health Action 12: 1662682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammar W, Kdouh O, Hammoud R. et al. 2016. Health system resilience: Lebanon and the Syrian refugee crisis. Journal of Global Health 6: 020704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson J, Ross A, Back J. et al. 2016. Implementing resilience engineering for healthcare quality improvement using the CARE model: a feasibility study protocol. Pilot and Feasibility Studies 2: 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrew S, Arlikatti S, Siebeneck L, Pongponrat K, Jaikampan K.. 2016. Sources of organisational resiliency during the Thailand floods of 2011: a test of the bonding and bridging hypotheses. Disasters 40: 65–84. [DOI] [PubMed] [Google Scholar]
- Back J, Ross AJ, Duncan MD. et al. 2017. Emergency department escalation in theory and practice: a mixed-methods study using a model of organizational resilience. Annals of Emergency Medicine 70: 659–71. [DOI] [PubMed] [Google Scholar]
- Bahadur A, Lovell E, Wilkinson E, Tanner T.. 2015. Resilience in the SDGs: Developing an Indicator for Target 1.5 That Is Fit for Purpose. London: Overseas Development Institute Briefing.
- Balbus J, Berry P, Brettle M. et al. 2016. Enhancing the sustainability and climate resiliency of health care facilities: a comparison of initiatives and toolkits. Revista Panamericana de Salud Publica = Pan American Journal of Public Health 40: 174–80. [PubMed] [Google Scholar]
- Barasa E, Mbau R, Gilson L.. 2018. What is resilience and how can it be nurtured? A systematic review of empirical literature on organizational resilience. International Journal of Health Policy and Management 7: 491–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barasa EW, Cloete K, Gilson L.. 2017. From bouncing back, to nurturing emergence: reframing the concept of resilience in health systems strengthening. Health Policy and Planning 32: iii91–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Béné C, Frankenberger T, Nelson S.. 2015. Design, monitoring and evaluation of resilience interventions: conceptual and empirical considerations. IDS working Paper 459. Brighton: Institute of Development Studies.
- Béné C, Godfrey-Wood R, Newsham A, Davies M.. 2012. Resilience: new utopia or new tyranny?—reflection about the potentials and limits of the concept of resilience about vulnerability reduction programmes. IDS working Paper 405. Brighton: Institute of Development Studies.
- Blanchet K, James P.. 2013. The role of social networks in the governance of health systems: the case of eye care systems in Ghana. Health Policy and Planning 28: 143–56. [DOI] [PubMed] [Google Scholar]
- Blanchet K, Nam SL, Ramalingam B, Pozo-Martin F.. 2017. Governance and capacity to manage resilience of health systems: towards a new conceptual framework. International Journal of Health Policy and Management 6: 431–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brattheim B, Faxvaag A, Seim A.. 2011. Process support for risk mitigation: a case study of variability and resilience in vascular surgery. BMJ Quality & Safety 20: 672–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooke-Sumner C, Petersen-Williams P, Kruger J, Mahomed H, Myers B.. 2019. ‘ Doing more with less’: a qualitative investigation of perceptions of South African health service managers on implementation of health innovations. Health Policy and Planning 34: 132–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruneau M, Chang SE, Eguchi RT. et al. 2003. A framework to quantitatively assess and enhance the seismic resilience of communities. Earthquake Spectra 19: 733–52. [Google Scholar]
- Cimellaro GP, Malavisi M, Mahin S.. 2017. Using discrete event simulation models to evaluate resilience of an emergency department. Journal of Earthquake Engineering 21: 203–26. [Google Scholar]
- Cohen O, Shapira S, Aharonson-Daniel L, Shamian J.. 2019. Confidence in health-services availability during disasters and emergency situations-does it matter?—lessons learned from an Israeli population survey. International Journal of Environmental Research and Public Health 16:3519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowe S, Vasilakis C, Skeen A. et al. 2014. Examining the feasibility of using a modelling tool to assess resilience across a health-care system and assist with decisions concerning service reconfiguration. Journal of the Operational Research Society 65: 1522–32. [Google Scholar]
- DFID 2011. Saving Lives, Preventing Suffering and Building Resilience: The UK Government’s Humanitarian Policy. London: DfID. [Google Scholar]
- Dippenaar A, Bezuidenhout T.. 2019. The development of a robust risk management plan for the continuous supply of water to hospitals in the Western Cape Province. South African Journal of Industrial Engineering 30: 190–204. [Google Scholar]
- Dobalian A, Stein JA, Radcliff TA. et al. 2016. Developing valid measures of emergency management capabilities within us department of veterans affairs hospitals. Prehospital and Disaster Medicine 31: 475–84. [DOI] [PubMed] [Google Scholar]
- Ellis LA, Churruca K, Clay-Williams R. et al. 2019. Patterns of resilience: a scoping review and bibliometric analysis of resilient health care. Safety Science 118: 241–57. [Google Scholar]
- Errett NA, Tanner A, Shen X, Chang SE.. 2019. Understanding the impacts of maritime disruption transportation to hospital-based acute health care supplies and personnel in coastal and geographically isolated communities. Disaster Medicine and Public Health Preparedness 13: 440–8. [DOI] [PubMed] [Google Scholar]
- Falegnami A, Bilotta F, Pugliese F. et al. 2018. A multicountry comparative survey about organizational resilience in anaesthesia. Journal of Evaluation in Clinical Practice 24: 1347–57. [DOI] [PubMed] [Google Scholar]
- Franklin BD, Panesar SS, Vincent C, Donaldson LJ.. 2014. Identifying systems failures in the pathway to a catastrophic event: an analysis of national incident report data relating to vinca alkaloids. BMJ Quality & Safety 23: 765–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuma S, Ahmed S, Goto R. et al. 2017. Fukushima after the Great East Japan Earthquake: lessons for developing responsive and resilient health systems. Journal of Global Health 7: 010501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilson L, Barasa E, Nxumalo N. et al. 2017. Everyday resilience in district health systems: emerging insights from the front lines in Kenya and South Africa. BMJ Global Health 2: e000224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gizelis TI, Karim S, Ostby G, Urdal H.. 2017. Maternal health care in the time of ebola: a mixed-method exploration of the impact of the epidemic on. World Development 98: 169–78. [Google Scholar]
- Goncalves L, Navarro JB, Sala R.. 2019. Spanish validation of the Benchmark Resilience Tool (short-form version) to evaluate organisational resilience. Safety Science 111: 94–101. [Google Scholar]
- Haldane V, Ong SE, Chuah FL, Legido-Quigley H.. 2017. Health systems resilience: meaningful construct or catchphrase?. Lancet (London, England) 389: 1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holling CS. 1973. Resilience and stability of ecological systems. Annual Review of Ecology and Systematics 4: 1–23. [Google Scholar]
- Hollnagel E. 2009. The four cornerstones of resilience engineering In: Nemeth CP, Hollnagel E, Dekker SWA (eds). Resilience Engineering Perspectives, Vol. 2: Preparation and Restoration Farnham, UK: Ashgate. [Google Scholar]
- Hollnagel E, Woods DD, Leveson N.. 2006. Resilience Engineering: Concepts and Precepts. Aldershot, UK: Ashgate . [Google Scholar]
- Iddon CR, Mills TC, Giridharan R, Lomas KJ.. 2015. The influence of hospital ward design on resilience to heat waves: an exploration using distributed lag models. Energy and Buildings 86: 573–88. [Google Scholar]
- Kailes JI, Enders A.. 2007. Moving beyond “special needs” A function-based framework for emergency management and planning. Journal of Disability Policy Studies 17: 230–7. [Google Scholar]
- Khan Y, O’Sullivan T, Brown A. et al. 2018. Public health emergency preparedness: a framework to promote resilience. BMC Public Health 18: 1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kittelsen SK, Keating VC.. 2019. Rational trust in resilient health systems. Health Policy and Planning 34: 553–7. [DOI] [PubMed] [Google Scholar]
- Kozuki N, Ericson K, Marron B, Lainez YB, Miller NP.. 2018. The resilience of integrated community case management in acute emergency: a case study from Unity State, South Sudan. Journal of Global Health 8: 020602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruk ME, Ling EJ, Bitton A. et al. 2017. Building resilient health systems: a proposal for a resilience index. BMJ (Clinical Research ed.) 357: j2323. [DOI] [PubMed] [Google Scholar]
- Kruk ME, Myers M, Varpilah ST, Dahn BT.. 2015. What is a resilient health system? The Lancet 385: 1910–2. [DOI] [PubMed] [Google Scholar]
- Kutzin J, Sparkes SP.. 2016. Health systems strengthening, universal health coverage, health security and resilience. Bulletin of the World Health Organization 94: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landeg O, Whitman G, Walker-Springett K. et al. 2019. Coastal flooding and frontline health care services: challenges for flood risk resilience in the English health care system. Journal of Health Services Research & Policy 24: 219–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leykin D, Lahad M, Cohen O, Goldberg A, Aharonson-Daniel L.. 2013. Conjoint community resiliency assessment measure-28/10 items (CCRAM28 and CCRAM10): a self-report tool for assessing community resilience. American Journal of Community Psychology 52: 313–23. [DOI] [PubMed] [Google Scholar]
- Ling EJ, Larson E, Macauley RJ. et al. 2017. Beyond the crisis: did the Ebola epidemic improve resilience of Liberia’s health system? Health Policy and Planning 32: iii40–7. [DOI] [PubMed] [Google Scholar]
- Lomas KJ, Giridharan R, Short CA, Fair AJ.. 2012. Resilience of ‘Nightingale’ hospital wards in a changing climate. Building Services Engineering Research & Technology 33: 81–103. [Google Scholar]
- Martineau FP. 2016. People-centred health systems: building more resilient health systems in the wake of the Ebola crisis. International Health 8: 307–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mash BJ, Mayers P, Conradie H. et al. 2008. How to manage organisational change and create practice teams: experiences of a South African primary care health centre. Educ Health (Abingdon) 21: 132. [PubMed] [Google Scholar]
- Merandi J, Vannatta K, Davis JT. et al. 2018. Safety II behavior in a pediatric intensive care unit. Pediatrics 141: e20180018. [DOI] [PubMed] [Google Scholar]
- Meyer D, Kirk Sell T, Schoch-Spana M. et al. 2018. Lessons from the domestic Ebola response: improving health care system resilience to high consequence infectious diseases. American Journal of Infection Control 46: 533–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Shamseer L, Clarke M et al. 2015. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews, 4: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. 2009. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine, 151: 264–269. [DOI] [PubMed] [Google Scholar]
- Norris FH, Stevens SP, Pfefferbaum B, Wyche KF, Pfefferbaum RL.. 2008. Community resilience as a metaphor, theory, set of capacities, and strategy for disaster readiness. American Journal of Community Psychology 41: 127–50. [DOI] [PubMed] [Google Scholar]
- Noyes J, Booth A, Moore G. et al. 2019. Synthesising quantitative and qualitative evidence to inform guidelines on complex interventions: clarifying the purposes, designs and outlining some methods. BMJ Global Health 4: e000893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Sullivan TL, Kuziemsky CE, Toal-Sullivan D, Corneil W.. 2013. Unraveling the complexities of disaster management: a framework for critical social infrastructure to promote population health and resilience. Social Science & Medicine 93: 238–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olu O. 2017. Resilient health system as conceptual framework for strengthening public health disaster risk management: an African viewpoint. Frontiers in Public Health 5:263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orru K, Tillmann M, Ebi KL, Orru H.. 2018. Making administrative systems adaptive to emerging climate change-related health effects: case of Estonia. Atmosphere 9: 221. [Google Scholar]
- Paterson J, Berry P, Ebi K, Varangu L.. 2014. Health care facilities resilient to climate change impacts. International Journal of Environmental Research and Public Health 11: 13097–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patriarca R, Falegnami A, Costantino F, Bilotta F.. 2018. Resilience engineering for socio-technical risk analysis: application in neuro-surgery. Reliability Engineering & System Safety 180: 321–335. [Google Scholar]
- Peters MD, Godfrey CM, Khalil H. et al. 2015. Guidance for conducting systematic scoping reviews. International Journal of Evidence-Based Healthcare 13: 141–6. [DOI] [PubMed] [Google Scholar]
- Radcliff TA, Chu K, DER-Martirosian C, Dobalian A.. 2018. A model for measuring ambulatory access to care recovery after disasters . The Journal of the American Board of Family Medicine 31: 252–9. [DOI] [PubMed] [Google Scholar]
- Raven J, Wurie H, Witter S.. 2018. Health workers’ experiences of coping with the Ebola epidemic in Sierra Leone’s health system: a qualitative study. BMC Health Services Research 18: 251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray-Bennett NS, Corsel DMJ, Goswami N, Ghosh A.. 2019. Understanding reproductive health challenges during a flood: insights from Belkuchi Upazila. Gates Open Research 3: 788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridde V, Lechat L, Meda IB.. 2016. Terrorist attack of 15 January 2016 in Ouagadougou: how resilient was Burkina Faso’s health system? BMJ Global Health 1: e000056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russo G, Rego I, Perelman J, Barros PP.. 2016. A tale of loss of privilege, resilience and change: the impact of the economic crisis on physicians and medical services in Portugal. Health Policy 120: 1079–86. [DOI] [PubMed] [Google Scholar]
- Short CA, Renganathan G, Lomas KJ.. 2015. A medium-rise 1970s maternity hospital in the east of England: resilience and adaptation to climate change. Building Services Engineering Research and Technology 36: 247–74. [Google Scholar]
- Simonetti A, Ezzeldin H, Walderhaug M, Anderson SA, Forshee RA.. 2018. An inter-regional US blood supply simulation model to evaluate blood availability to support planning for emergency preparedness and medical countermeasures. Disaster Medicine and Public Health Preparedness 12: 201–10. [DOI] [PubMed] [Google Scholar]
- Sochas L, Channon AA, Nam S.. 2017. Counting indirect crisis-related deaths in the context of a low-resilience health system: the case of maternal and neonatal health during the Ebola epidemic in Sierra Leone. Health Policy and Planning 32: iii32–9. [DOI] [PubMed] [Google Scholar]
- Tanner T, Bahadur A, Moench M.. 2017. Challenges for resilience policy and practice. London: Overseas Development Institute.
- Thomas S, Keegan C, Barry S. et al. 2013. A framework for assessing health system resilience in an economic crisis: Ireland as a test case. BMC Health Services Research 13: 450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thude BR, Juhl AG, Stenager E, Plessen CV, Hollnagel E.. 2019. Staff acting resiliently at two hospital wards. Leadership in Health Services (Bradford, England) 32: 445–57. [DOI] [PubMed] [Google Scholar]
- Toner ES, Mcginty M, Schoch-Spana M. et al. 2017. A community checklist for health sector resilience informed by Hurricane Sandy. Health Security 15: 53–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tugade MM, Fredrickson BL.. 2004. Resilient individuals use positive emotions to bounce back from negative emotional experiences. Journal of Personality and Social Psychology 86: 320–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turenne CP, Gautier L, Degroote S. et al. 2019. Conceptual analysis of health systems resilience: a scoping review. Social Science & Medicine 232: 168–80. [DOI] [PubMed] [Google Scholar]
- UNISDR. 2005. Hyogo framework for action 2005–2015: building the resilience of nations and communities to disasters. Extract from the final report of the World Conference on Disaster Reduction (A/CONF. 206/6). The United Nations International Strategy for Disaster Reduction Geneva.
- UNISDR. 2015. Sendai framework for disaster risk reduction 2015–2030. Proceedings of the 3rd United Nations World Conference on DRR, Sendai, Japan, 14–8.
- Watts N, Amann M, Ayeb-Karlsson S. et al. 2018. The Lancet Countdown on health and climate change: from 25 years of inaction to a global transformation for public health. The Lancet 391: 581–630. [DOI] [PubMed] [Google Scholar]
- Witter S, Wurie H, Chandiwana P. et al. 2017. How do health workers experience and cope with shocks? Learning from four fragile and conflict-affected health systems in Uganda, Sierra Leone, Zimbabwe and Cambodia. Health Policy and Planning 32: iii3–13. [DOI] [PubMed] [Google Scholar]
- World Health Organization. 2010. Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies. Geneva: World Health Organization.
- World Health Organization. 2015. Operational Framework for Building Climate Resilient Health Systems. Geneva: World Health Organization.
- Wulff K, Donato D, Lurie N.. 2015. What is health resilience and how can we build it? Annual Review of Public Health 36: 361–74. [DOI] [PubMed] [Google Scholar]
- Zhong S, Clark M, Hou XY, Zang Y, Fitzgerald G.. 2014. a. Validation of a framework for measuring hospital disaster resilience using factor analysis. International Journal of Environmental Research and Public Health 11: 6335–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong S, Clark M, Hou XY, Zang YL, Fitzgerald G.. 2014. b. Development of hospital disaster resilience: conceptual framework and potential measurement. Emergency Medicine Journal 31: 930–8. [DOI] [PubMed] [Google Scholar]
- Zhong S, Clark M, Hou XY, Zang Y, Fitzgerald G.. 2015. Development of key indicators of hospital resilience: a modified Delphi study. Journal of Health Services Research & Policy 20: 74–82. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.