Abstract
Few studies had been published regarding imaging findings of skin adnexal tumors. We experienced two giant cases of them with a characteristic mushroom-like growth pattern. MRI showed a circumscribed mushroom-like shaped mass extruding from the subcutaneous tissue with microcystic lesions. Although differentiation between benignancy and malignancy may be difficult by radiological examinations, MRI may be helpful to identify its origin and differentiate soft tissue tumors with skin adnexal tumors in having these imaging findings.
Keywords: magnetic resonance imaging, mushroom-like shape, porocarcinoma, sebaceoma, skin adnexal tumor
Introduction
Skin and skin adnexal tumors are usually diagnosed by gross examination or dermoscopy. These tumors are readily noticeable and are easy to access for biopsy. Therefore, the necessity of radiological examination in these tumors is uncertain, and the image examination is often performed to check metastases only in case of malignancy. However, when the main lesion is huge or wide-spread, radiological examination is needed to reveal tumor characteristics and its malignancy/benignancy. Sometimes, soft tissue tumors can be one of differential diagnoses against skin adnexal tumors. Because treatment strategies including the decision of optimal biopsy site and the selection of operative procedures differ greatly between skin adnexal tumors and soft tissue tumors, their differentiation is very important in clinical setting. In addition, the expertise in pathological diagnosis is also quite different between them. In that case, MRI can be useful to identify its origin1 and help to decide treatment and management options.
We experienced two cases of giant skin adnexal tumor with a mushroom-like growth, which may be a characteristic finding of skin adnexal tumors. To the best of our knowledge, there are few reports about imaging findings of skin adnexal tumors. Herein, we report MRI findings of giant skin adnexal tumors with literature review.
Case Reports
Case 1
A 69-year-old man presented with a protruding mass in the occipital region. The tumor had been seen for 10 years, but left untreated. The tumor had gradually increased since half a year ago. From 1 month ago exudates appeared and the size doubled. The local stimulus to the occipital area was only wearing a hat. Macroscopically, a protruding mass was observed in the occipital region, measuring 11.0 × 8.0 cm2 (Fig. 1a). There was a lack of dermis in the right side of tumor, and leakage of hemorrhagic exudate was also seen. There were no symptoms including pain, and there was no malodor from the tumor.
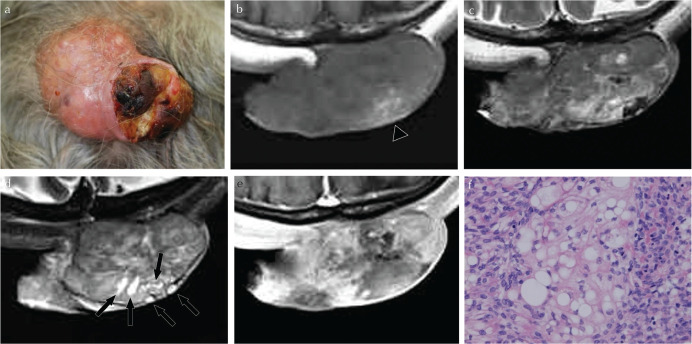
Fig. 1.
A 69-year-old man presented with a giant mushroom-like shaped mass protruding from the scalp. Grossly, a reddish protruding mass with a defect of dermis in the right side was seen (a). The mass showed homogeneous iso signal intensity with a high signal intensity area suggestive of hemorrhage (arrowhead) on T1-weighted image on MRI (b), and heterogeneous signal intensity with a high signal intensity area on T2-weighted image compared with muscle (c). Fat-saturated T2-weighted image of more cranial slice from (b) showed a collection of small cysts with linear lesions like small ducts (arrows) (d). The mass was heterogeneously enhanced after injection of gadolinium (e). Hematoxylin and eosin (H&E) staining of the specimen showed a differentiation toward sebaceous ducts, and the pathological final diagnosis was sebaceoma (f).
CT showed a circumscribed mushroom-like shaped mass extruding from the subcutaneous tissue to the surface, measuring 8.5 × 6.0 × 3.7 cm3. The tumor had slightly high density compared with the gray-white matter on plain CT. With the injection of contrast media, the tumor was heterogeneously well enhanced, and an enlarged feeding artery was observed in the subcutaneous tissue. On MRI, the tumor showed iso signal intensity on T1-weighted image and heterogeneous signal intensity on T2-weighted image mixed with slightly low signal intensity areas and edema-like high signal intensity areas (Fig. 1b and 1c). In the portion near the surface, a lot of microcystic components were seen (Fig. 1d). Slight hemorrhage was also seen as high signal intensity on T1-weighted image (Fig. 1b). Contrast-enhanced MRI showed heterogeneous and gradual enhancement (Fig. 1e). There was no apparent restricted diffusion. The tumor was adjacent widely to occipital bone, but no obvious invasion was found. Swelling of the left posterior cervical lymph node was observed. Pre-operative diagnosis in imaging was a malignant skin adnexal tumor. Excisional biopsy was performed. Hematoxylin and eosin (H&E) stain demonstrated differentiation toward sebaceous glands, and the final pathological diagnosis was a sebaceoma with no malignancy (Fig. 1f). There was also no malignant cells in the cervical lymph node.
Case 2
A 57-year-old woman presented with a large mass in the left temporal region. About 30 years ago, she noticed a mass which was about 1 cm in diameter, and it had grown slowly. In gross examination, a mushroom-like shaped mass with a reddish rough surface was seen in the left temporal region (Fig. 2a). There was erosion on the surface of the tumor with hemorrhage.
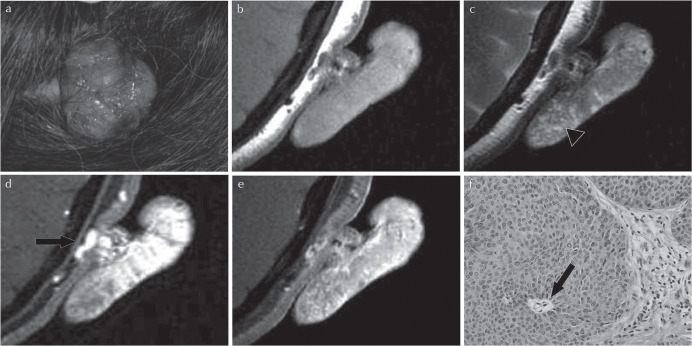
Fig. 2.
A 57-year-old woman presented with a mushroom-like shaped mass protruding from the left temporal region. Grossly, a reddish lobulated mass protruded from the scalp (a). The tumor showed homogeneous and slightly high signal intensity compared with muscle on T1-weighted image on MRI (b). T2-weighted image showed heterogeneous intensity, including multiple small high signal intensity areas on the periphery of the tumor (arrowhead) (c). On dynamic contrast-enhanced imaging, an enlarged vessel in the stalk of the tumor was observed at the early phase (arrow) (d), and the mass was slightly and heterogeneously enhanced at the delayed phase (e). Hematoxylin and eosin (H&E) staining of the specimen showed ductal structures, suggestive of differentiation to eccrine glands (arrow) (f). Because of the existence of invasive lesion with severe dysplasia, the pathological final diagnosis was porocarcinoma in poroma.
MRI showed a pedunculated mass measuring 5.1 × 4.4 × 1.3 mm3 that protruded from the subcutaneous tissue toward left auricle. T1-weighted MR image showed a mass with homogeneous high signal intensity, and T2-weighed image showed a central lesion with low signal intensity and a peripheral lesion with high signal intensity, compared with muscle (Fig. 2b and 2c). In a peripheral area, well circumscribed small cysts were observed (Fig. 2c). Hemorrhage was also seen in some part. On dynamic contrast-enhanced imaging, the tumor showed rapid and persistent enhancement with an enlarged feeding vessel in the part adhered to the scalp (Fig. 2d and 2e). In gallium scintigraphy, uptake was seen in the left temporal tumor, and no metastasis was apparent. Pre-operative diagnosis in imaging was a skin adnexal tumor and resection was performed. H&E stain revealed ductal structures which differentiated toward eccrine sweat glands with severe dysplasia, and the final pathological diagnosis was a porocarcinoma in poroma (Fig. 2f).
Discussion
Skin is composed of dermis, epidermis, subcutaneous tissue and skin appendages. Skin tumors are divided into melanoma and non-melanoma, and skin adnexal tumors are included in non-melanoma. Skin adnexal tumors are characteristic with differentiation to appendage structures, such as hair follicles, sweat glands and sebaceous glands, and are named according to their differentiated tissues. There is a wide variety of skin adnexal tumors, including tumors presenting differentiation toward two or more appendages, and it makes classification and diagnosis difficult. Many skin adnexal tumors are located within the subcutaneous tissue, and are adjacent focally or widely to the dermis.2 A gross change of the skin may be seen.
In general, the purpose of imaging for tumors is (1) differentiation between benignancy and malignancy, (2) evaluation of disease extent, and (3) evaluation of critical organs. The major purpose of MRI for our cases was both (1) and (2). In addition, an assessment of the optimal biopsy site is also an aim for imaging when biopsy is planned considering malignancy. In the case of tumors that are continuous from subcutaneous tissue, both skin adnexal tumors and soft tissue tumors are included as differential diagnoses.2 The surgical margin differs between soft tissue tumors and skin adnexal tumors.3 Therefore, the selection of operative procedures including reconstruction may also change between them. It is generally known that large soft tissue tumors, especially which are larger than 5 cm in size or have increasing trend, are needed to consider the possibility of soft tissue sarcomas. In the case of soft tissue sarcoma, unplanned excision may worsen the patient’s prognosis.4 In those cases, it is necessary to choose an appropriate approach before performing biopsy (e.g. the incisional or punch site of biopsy) with clarifying tumor characteristics and the extent of tumor using MRI. Therefore, it is thought to be important to perform MRI before biopsy, especially in the case of a huge mass that is continuous with the subcutaneous tissue.
On MRI, both of our cases had a characteristic mushroom-like shape: not sessile, but pedunculated. This shape is speculated to be formed as a subcutaneous lesion growing exophytically and suggests a close relationship between the tumor and the skin appendages. Therefore, we thought that the mushroom-like shape was a characteristic feature suggestive of skin adnexal tumors. The mushroom-like shape is a rare growth pattern in solid tumors, although it had been reported by Albert since 1806 in mycosis fungoides.5,6 Wollina et al.6 reported three cases of mushroom-like shaped masses, melanoma, Merkel cell carcinoma, and basal cell carcinoma, although there were no mentions about imaging findings. Moreover, square cell carcinoma7 and fibroma8 with mushroom-like shape were reported in dermatological and pathological journals.
Few studies had been published referring imaging findings of skin adnexal tumors. This is because radiological examinations are not frequently performed for skin adnexal tumors as mentioned above in introduction, and because there are so many kinds of rare disease that it is difficult to make a comprehensive report. According to a handful of review articles or case reports, skin adnexal tumors have a very wide range of imaging features on MRI.2,9–12 Often, the tumor shows a solid mass containing cystic parts, which shows low signal intensity on T1-weighted image, and intermediate to high signal intensity on T2-weighted image compared with muscle. Cystic change, hemorrhage, fluid-fluid level, and mural nodules are sometimes observed. The solid part is usually hypervascular.
Both of our cases were solid hypervascular tumors and showed homogeneous low to intermediate signal intensity on T1-weighted image, and heterogeneous low signal intensity on T2-weighted image compared with muscle. We paid attention to imaging findings of the distribution of well-defined cysts and collection of microcysts at the periphery of the tumor. These cysts are not ill-defined as seen in cystic degeneration of the tumor in general. We supposed that these small cysts reflected secretions or luminal structures, although strictly it is difficult to prove pathologically. When a tumor is mainly located in the subcutaneous tissue and has the mushroom-like shape with a collection of well-defined small cysts, it is thought to be suggestive of a skin adnexal tumor.
MRI contributed the diagnosis of skin adnexal tumors in our cases, but it was difficult to diagnose whether the tumor was malignant or not. There looked no particular difference between imaging findings of cases 1 and 2, however, case 1 was a benign tumor and case 2 was a malignant tumor. To the best of our knowledge, our case 1 was the largest sebaceoma ever reported. There are a couple of case reports about large skin adnexal tumors which were growing rapidly even though they were benign.13,14 The increasing behavior was thought to be a result of degeneration or hemorrhage, and it was also seen in our cases. Because our cases were large tumors growing exophytically in the occipital or temporal region, it was possible that the tumor surface defected and bled due to mechanical stimulus occurring in the supine position during sleeping. Therefore, it is thought to be hard to distinguish whether the hemorrhage was caused by an external stimulus or intratumoral bleeding. Differentiation between benignancy and malignancy in skin adnexal tumors may be difficult in many cases, except in the cases that have apparent invasion or metastases. Further investigation is required because of its rarity and less frequency for imaging examination.
Conclusion
We experienced two cases of characteristic mushroom-like shaped skin adnexal tumor. The mushroom-like shape is suggestive of a close relationship between the tumor and skin appendages. Although differentiation between benignancy and malignancy in skin adnexal tumors may be difficult by radiological examinations, the mushroom-like shape and a collection of well-defined microcysts in the tumor reflecting secretions or luminal structures may help to diagnose skin adnexal tumors.
Footnotes
Conflicts of Interest
Dr. Satoru Arai’s activities related to the present article: disclosed no relevant relationships.
Activities not related to the present article: disclosed receipt of payment for lectures by Kyowa Hakko Kirin Company, Janssen Pharmaceutical Company and Celgene Company.
Other authors declare that they have no conflicts of interest.
References
- 1.Zhang J, Li Y, Zhao Y, Qiao J. CT and MRI of superficial solid tumors. Quant Imaging Med Surg 2018; 8:232–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim JH, Kim JY, Chun KA, Jee WH, Sung MS. MR imaging manifestations of skin tumors. Eur Radiol 2008; 18:2652–2661. [DOI] [PubMed] [Google Scholar]
- 3.Green B, Godden D, Brennan PA. Malignant cutaneous adnexal tumours of the head and neck: an update on management. Br J Oral Maxillofac Surg 2015; 53:485–490. [DOI] [PubMed] [Google Scholar]
- 4.Pretell-Mazzini J, Barton MD, Conway SA, Temple HT. Unplanned excision of soft-tissue sarcomas: current concepts for management and prognosis. J Bone Joint Surg Am 2015; 97:597–603. [DOI] [PubMed] [Google Scholar]
- 5.Alibert JL: [Genre I. herpes. In: Monographie des dermatoses ou précis théorique et pratique des maladies de la peau. vol. 2.] chez le Dr Daynac éditeur; Paris, 1832, 23–25. (in French) [Google Scholar]
- 6.Wollina U, Langer D, Tchernev G. Mushroom-like skin tumours: report of three cases. Open Access Maced J Med Sci 2017; 5:515–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang NR, Wang MM, Zhou L, et al. Cutaneous clear cell/signet-ring cell squamous cell carcinoma arising in the right thigh of a patient with type 2 diabetes: combined morphologic, immunohistochemical, and etiologic analysis. Diagn Pathol 2016; 11:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nakamura S, Hashimoto Y, Nishi K, et al. Mushroom-like soft fibromas on chronic leg lymphedema. Eur J Dermatol 2010; 20:228–229. [DOI] [PubMed] [Google Scholar]
- 9.Han YD, Huan Y, Deng JL, Zhang YG, Zhang CH. MRI appearance of multiple eccrine spiradenoma. Br J Radiol 2007; 80:e27–e29. [DOI] [PubMed] [Google Scholar]
- 10.Maldjian C, Adam R, Bonakdarpour A, Robinson TM, Shienbaum AJ. MRI appearance of clear cell hidradenoma. Skeletal Radiol 1999; 28:104–106. [DOI] [PubMed] [Google Scholar]
- 11.Kerimoglu U, Aydingoz U, Ozkaya O, Aksu AE, Ergen FB. MRI of a benign chondroid syringoma. Br J Radiol 2006; 79:e59–e61. [DOI] [PubMed] [Google Scholar]
- 12.Quek ST, Tyrrell PN, Darby AJ. MRI of eccrine cystadenoma. J Comput Assist Tomogr 2000; 24:293–295. [DOI] [PubMed] [Google Scholar]
- 13.Takahashi M, Arima M, Iwata Y, et al. A patient with giant rippled-pattern sebaceoma in the occipital region. Case Rep Dermatol 2016; 8:107–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Knoedler D, Susnik B, Gonyo MB, Osipov V. Giant apocrine hidradenoma of the breast. Breast J 2007; 13:91–93. [DOI] [PubMed] [Google Scholar]