Clinical Implications.
-
•
Nationwide preventive measures for COVID-19 in Japan were associated with a sharp drop in hospitalizations for asthma as a secondary effect. Health professionals may reappraise the importance of patients' behavior and physical environment to improve the regulation of their asthma.
The COVID-19 pandemic has drastically changed patients' behavior and environment worldwide. Although there were concerns that the spread of COVID-19 would increase asthma attacks, recent reports from the United States1 , 2 and Slovenia3 suggest a drop in emergency department visits or hospitalizations for pediatric patients with asthma during urban lockdowns. Nevertheless, these studies are limited to a single children's hospital or a single city, and whether or not this phenomenon is widespread across countries and age groups is unknown. We evaluated the nationwide changes in the number of hospitalizations for asthma during the COVID-19 outbreak in Japan.
We used the Diagnosis Procedure Combination inpatient database, built by Medical Data Vision Co, Ltd (Tokyo, Japan).4 Briefly, this database included deidentified demographic/clinical information collected from Japanese acute-care hospitals for per-diem reimbursement. The details of the database are described elsewhere.5 We aggregated the total number of hospitalizations per week across 272 continuously observed hospitals during the calendar weeks 1 to 22 of 2020 (December 30, 2019, to May 31, 2020) and the same periods in 2017 to 2019. Our internal investigation found that this dataset included 165,360 new admissions in January 2019, which accounted for 12.4% of all acute-care admissions in this month across Japan (n = 1,338,945), according to the Hospital Report (a government-designated monthly survey that covers all hospitals nationwide).
We described weekly trends in the number of hospitalizations with a primary diagnosis of asthma (International Classification of Diseases 10 [ICD-10] code: J45 or J46),6 based on the date of admissions. We also examined the hospitalizations with a primary diagnosis of COVID-19 (ICD-10 code: U07) to illustrate the COVID-19 epidemic in Japan. We estimated changes in the number of asthma hospitalizations during the COVID-19 outbreak using a “difference-in-differences” model that included variables for each week, the year indicator, and the outbreak status (an interaction variable between an indicator of week 9 or later and an indicator of the year 2020). Adjusted incidence rate ratios (aIRRs) were estimated using Poisson regressions with Huber-White heteroscedasticity robust standard errors. We repeated analyses separately for children (aged <18 years) and adults (aged ≥18 years) to account for the difference in factors triggering asthma exacerbation.7 P < .05 was interpreted as statistically significant (Stata 15.1; StataCorp, College Station, TX). The University of Tokyo Ethics Board approved this study (2020105NI).
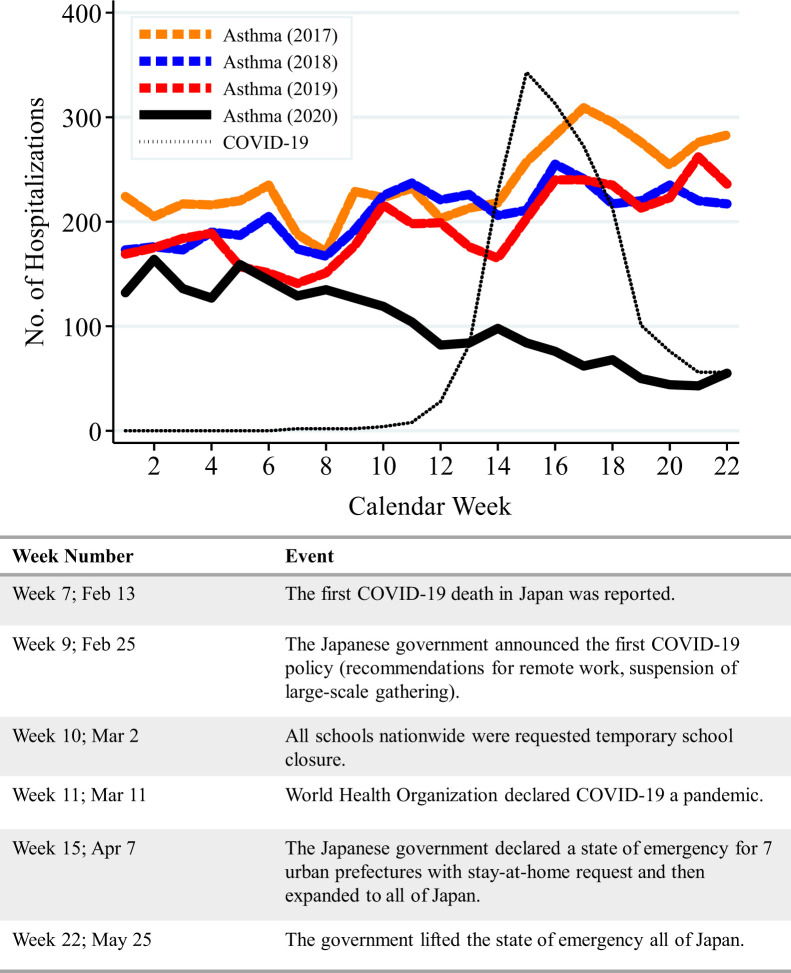
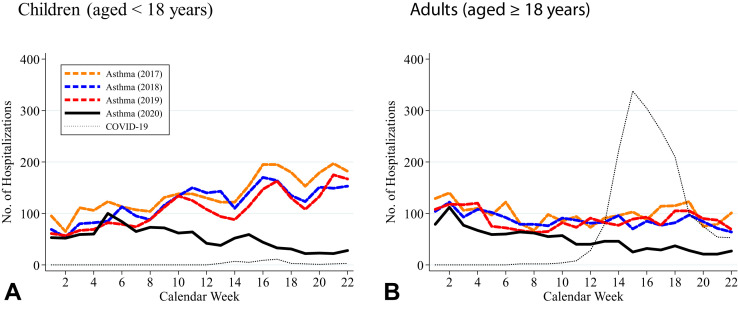
During the weeks 1 to 22 of 2017, 2018, 2019, and 2020, we observed 16,317 hospitalizations for asthma. We compared asthma hospitalizations during weeks 1 to 22 of 2017 to 2019 with those of 2020. Although asthma hospitalizations in 2017 to 2019 and 2020 showed parallel trends until week 8, there was a relative decline from week 9 onward in 2020 compared with the previous 3 years (Figure 1 ). The first hospitalizations for COVID-19 for the analytic hospitals were observed in week 7, followed by a peak in week 15. In the difference-in-differences analyses, the average number of asthma hospitalizations per week during weeks 9 to 22 significantly decreased in 2020 compared with 2017 to 2019 (78.3 vs 229.9; crude reduction rate, 66.0%; aIRR, 0.45; 95% confidence interval [CI], 0.37-0.55; P < .001) (Table E1, available in this article's Online Repository at www.jaci-inpractice.org). When stratified by age group, the average number of asthma hospitalizations per week during weeks 9 to 22 showed relative decreases in 2020 compared with 2017 to 2019 for children (42.3 vs 142.6; aIRR, 0.37; 95% CI, 0.29-0.48; P < .001) and for adults (36.0 vs 87.2; aIRR, 0.56; 95% CI, 0.47-0.68; P < .001) (Figure 2 and Table E1, available in this article's Online Repository at www.jaci-inpractice.org).
Figure 1.
Trends in hospitalizations for asthma and COVID-19 for Japanese acute-care hospitals, 2017 through 2020.
Figure 2.
Trends in hospitalizations for asthma and COVID-19 for Japanese acute-care hospitals among children and adults, 2017 through 2020. Children aged < 18 years (A) and adults aged ≧ 18 years (B).
These reductions in the number of asthma hospitalizations during the COVID-19 outbreak were consistent with previous findings for children.1, 2, 3 Furthermore, our study found a decline in asthma hospitalizations for adults. As hospitalizations for asthma are considered a consequence of poor asthma control,7 our findings suggest that asthma was better controlled during this outbreak.
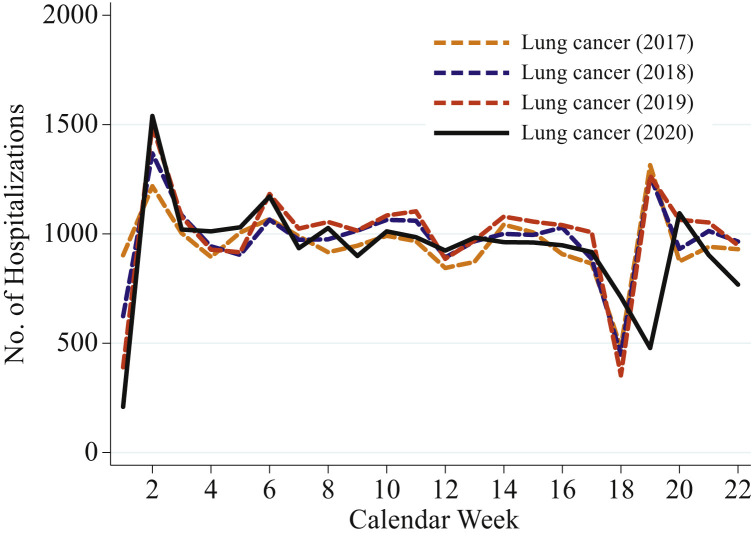
There are several possible mechanisms for this drop in asthma hospitalizations. First, individual-level hygiene measures to prevent COVID-19 infection (refraining from going outside and wearing masks) might reduce exposure to the strong drivers of asthma exacerbations, including respiratory virus infection, allergens such as cedar and cypress pollen, and air pollutants.7 Furthermore, initial concerns that the COVID-19 spread might increase asthma attacks might have encouraged preventive behaviors among people with asthma and their families, including quitting smoking, better adherence to preventive medications,8 or cleaning their rooms more frequently to remove allergens. The decline in asthma hospitalizations during the outbreak appeared to be becoming larger, possibly due to the increased preventive behaviors over this period. Second, community-level prevention measures for COVID-19 (school closure, suspension of large-scale gathering, and promotion of remote work) might result in the suppression of other respiratory infections, which would, in turn, lead to a reduction in hospitalizations for asthma.2 Third, community-level air pollution might have decreased due to lower traffic and plant closures related to the COVID-19 economic shutdown. However, PM2.5 and NO2 showed only a slight decrease even in Tokyo (the most populous district in Japan) under the stay-at-home requests, and this explanation would not markedly explain our findings.2 , 9 Other possibilities included hospitals' incapability of providing inpatient care or patients' postponing hospitalizations. However, our post hoc analyses showed no decrease in lung cancer hospitalizations during the outbreak (Table E1 and Figure E1, available in this article's Online Repository at www.jaci-inpractice.org), suggesting that these possibilities would be minimized.
Figure E1.
Trends in hospitalizations for lung cancer for Japanese acute-care hospitals, 2017 through 2020. We illustrated the trends in the weekly number of hospitalizations with a primary diagnosis of lung cancer (International Classification of Diseases 10: C34) across the 272 analytic acute-care hospitals. The sharp drops in calendar week 18 of 2017 to 2019 and calendar week 19 of 2020 were due to consecutive public holidays called the “Golden Week.”
Several limitations warrant mention. First, as with any observational study, we could not fully account for unmeasured confounders. Other exacerbating factors for asthma that varied by year (eg, infectious disease trends and pollen dispersal conditions unrelated to the COVID-19 outbreak) might partially explain our results. Nevertheless, asthma hospitalizations usually increase during the spring through early summer in Japan, and thus the decreasing trend found in our study indicates that these other factors do not markedly explain our findings. Second, the mechanisms through which the asthma hospitalizations decreased remain unknown, and future studies with individual-level information are warranted. Third, the patient population did not cover all the medical facilities in Japan. Nevertheless, our dataset included as many as 272 hospitals, and the underlying patterns may be similar across Japan.
In summary, we found a sharp drop in asthma hospitalizations during the COVID-19 outbreak in Japan. The current study may encourage health professionals who provide asthma care to reappraise the importance of environmental factors surrounding patients with asthma.
Acknowledgments
A. Miyawaki had full access to the data in the study and takes responsibility for the accuracy and integrity of the data and its analyses. He supervised the study. All authors conceptualized and designed the study; acquired, analyzed, or interpreted the data; drafted the manuscript; critically revised the manuscript for important intellectual content; performed statistical analysis; and provided administrative, technical, or material support.
Footnotes
The Medical Data Vision Co., Ltd. (Tokyo, Japan) supported this study in the form of labor service (non-financial support).
Conflicts of interest: The Medical Data Vision Co, Ltd (Tokyo, Japan) provided the dataset used in this study to A. Miyawaki in the form of labor service. M. Nakamura is one of the board of directors in Medical Data Vision Co, Ltd and received personal salary from it outside this study. H. Ninomiya supported the Medical Data Vision Co, Ltd in algorithm construction and received personal fee outside this study. The rest of the authors declare that they have no relevant conflicts of interest.
Online Repository.
Table E1.
Change in the total number of hospitalizations for asthma and lung cancer from weeks 1 through 8 to weeks 9 through 22 for 2017-2019 vs 2020: difference-in-differences analyses for the 272 acute-care hospitals in Japan
| Average number of hospitalizations per week |
Difference-in-differences |
|||||||
|---|---|---|---|---|---|---|---|---|
| 2017-2019 | 2020 | |||||||
| Weeks 1-8 | Weeks 9-22 | Ratio (difference) | Weeks 1-8 | Weeks 9-22 | Ratio (difference) | Adjusted IRR (95% CI)∗ | P value | |
| Asthma, overall | 184.9 | 229.9 | 1.24 (45.0) | 140.8 | 78.3 | 0.56 (−62.5) | 0.45 (0.37, 0.55) | <.001 |
| Asthma, children (aged <18 y) | 86.1 | 142.6 | 1.66 (56.5) | 68.3 | 42.3 | 0.62 (−26.0) | 0.37 (0.29, 0.48) | <.001 |
| Asthma, adults (aged ≥18 y) | 98.8 | 87.2 | 0.88 (−11.6) | 72.5 | 36.0 | 0.50 (−36.5) | 0.56 (0.47, 0.68) | <.001 |
| Lung cancer (post hoc analysis) | 1000.0 | 962.6 | 0.96 (−37.4) | 992.9 | 896.1 | 0.90 (−96.8) | 0.94 (0.81, 1.08) | .38 |
CI, Confidence interval; IRR, incidence rate ratio.
Estimated using a difference-in-differences model that regressed the weekly number of asthma/lung cancer hospitalizations on an interaction variable between outbreak status (weeks 9-22 vs weeks 1-8) and the indicator of the year 2020 with adjustment for variables for each week and the year indicators. Poisson regressions with Huber-White heteroscedasticity robust standard errors were applied.
References
- 1.Kenyon C.C., Hill D.A., Henrickson S.E., Bryant-Stephens T.C., Zorc J.J. Initial effects of the COVID-19 pandemic on pediatric asthma emergency department utilization. J Allergy Clin Immunol Pract. 2020;8:2774–2776.e1. doi: 10.1016/j.jaip.2020.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taquechel K., Diwadkar A.R., Sayed S., Dudley J.W., Grundmeier R.W., Kenyon C.C. Pediatric asthma healthcare utilization, viral testing, and air pollution changes during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2020;8 doi: 10.1016/j.jaip.2020.07.057. 3378-87.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krivec U., Kofol Seliger A., Tursic J. COVID-19 lockdown dropped the rate of paediatric asthma admissions. Arch Dis Child. 2020;105:809–810. doi: 10.1136/archdischild-2020-319522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miyao H., Kotake Y. Renal morbidity of 6% hydroxyethyl starch 130/0.4 in 9000 propensity score matched pairs of surgical patients. Anesth Analg. 2020;130:1618–1627. doi: 10.1213/ANE.0000000000004592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matsuda S., Fujimori K., Kuwabara K., Ishikawa K.B., Fushimi K. Diagnosis procedure combination as an infrastructure for the clinical study. Asian Pac J Dis Manage. 2011;5:81–87. [Google Scholar]
- 6.Okubo Y., Horimukai K., Michihata N., Morita K., Matsui H., Fushimi K. Association between early antibiotic treatment and clinical outcomes in children hospitalized for asthma exacerbation. J Allergy Clin Immunol. 2021;147:114–122. doi: 10.1016/j.jaci.2020.05.030. [DOI] [PubMed] [Google Scholar]
- 7.Castillo J.R., Peters S.P., Busse W.W. Asthma exacerbations: pathogenesis, prevention, and treatment. J Allergy Clin Immunol Pract. 2017;5:918–927. doi: 10.1016/j.jaip.2017.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaye L., Theye B., Smeenk I., Gondalia R., Barrett M.A., Stempel D.A. Changes in medication adherence among patients with asthma and COPD during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2020;8:2384–2385. doi: 10.1016/j.jaip.2020.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ma C.J., Kang G.U. Air quality variation in Wuhan, Daegu, and Tokyo during the explosive outbreak of COVID-19 and its health effects. Int J Environ Res Public Health. 2020;17:4119. doi: 10.3390/ijerph17114119. [DOI] [PMC free article] [PubMed] [Google Scholar]