Abstract
We estimate the potential impact of COVID-19 on the United Kingdom economy, including direct disease effects, preventive public actions and associated policies. A sectoral, whole-economy macroeconomic model was linked to a population-wide epidemiological demographic model to assess the potential macroeconomic impact of COVID-19, together with policies to mitigate or suppress the pandemic by means of home quarantine, school closures, social distancing and accompanying business closures.
Our simulations indicate that, assuming a clinical attack rate of 48% and a case fatality ratio of 1.5%, COVID-19 alone would impose a direct health-related economic burden of £39.6bn (1.73% of GDP) on the UK economy. Mitigation strategies imposed for 12 weeks reduce case fatalities by 29%, but the total cost to the economy is £308bn (13.5% of GDP); £66bn (2.9% of GDP) of which is attributable to labour lost from working parents during school closures, and £201bn (8.8% of GDP) of which is attributable to business closures. Suppressing the pandemic over a longer period of time may reduce deaths by 95%, but the total cost to the UK economy also increases to £668bn (29.2% of GDP), where £166bn (7.3% of GDP) is attributable to school closures and 502bn (21.9% of GDP) to business closures.
Our analyses suggest Covid-19 has the potential to impose unprecedented economic costs on the UK economy, and whilst public actions are necessary to minimise mortality, the duration of school and business closures are key to determining the economic cost. The initial economic support package promised by the UK government may be proportionate to the costs of mitigating Covid-19, but without alternative measures to reduce the scale and duration of school and business closures, the economic support may be insufficient to compensate for longer term suppression of the pandemic which could generate an even greater health impact through major recession.
Keywords: Coronavirus, Macroeconomic, Computable general equilibrium, UK, Covid-19
Highlights
-
•
Health-related economic impacts from Covid-19 may cost the UK economy £40bn in 2020.
-
•
Preventative mitigation/suppression actions will impose unprecedented economic losses.
-
•
Minimising the duration of business closures is key to preventing catastrophic costs.
1. Introduction
1.1. The current outbreak
Since the outbreak of Covid-19 in Wuhan City, Hubei Province, China in December 2019 (WHO, 2020), its rapid spread has transformed lives and behaviour globally. Covid-19 is the third major outbreak of a novel coronavirus in the 21st century, following SARS in 2003 and MERS in 2012. However, whilst these previous outbreaks demonstrated the potential seriousness of an infectious disease outbreak to bring tragic impacts on population health, along with serious repercussions for the economies affected (Keogh-Brown & Smith, 2008; Noy & Shields, 2019), Covid-19 has transformed the approach of policymakers and invoked unprecedented advice, legislation and influence on the lives of individuals, businesses and organisations. For example, previous outbreaks highlighted the need for policymakers to minimise individual avoidance actions, since they may impose substantial economic costs whilst not necessarily reducing transmission (Smith, 2006). However, the high mortality from Covid-19 has taken the responsibility for avoidance behaviour away from individuals by imposing extreme national packages of social distancing and business closures which prioritise reductions in transmission and mortality from the disease, rather than the potentially substantial economic impacts that may result.
Whilst the future path of the pandemic cannot be precisely known, epidemiological models have been constructed to predict both the spread of Covid-19 and the expected efficacy of non-pharmaceutical behavioural interventions to mitigate or suppress that spread (Ferguson, Laydon et al., 2020) and the UK government's actions, in particular, have followed the evidence presented in the mathematical modelling studies closely (Hamzelou, 2020). However, there have been no equivalent economic models to assess the economic impact of the policies imposed by governments to reduce transmission and mortality from Covid-19. Due to the high level of reliance, of the UK government, on well-documented scientific advice, the UK epidemic presents an ideal context for an estimation of both the macroeconomic impact of Covid-19 and the impact of non-pharmaceutical behavioural interventions to combat it.
1.2. The economics of previous pandemics
Previous evidence indicates that there are multiple direct and indirect channels whereby Covid-19 could affect the UK economy. Infectious disease outbreaks have impacts on labour supply and productivity across sectors through the reduction in work time of workers who are infected or time losses by carers. However, the SARS outbreak in 2003 demonstrated that the indirect costs of an infectious disease outbreak can easily exceed the direct productivity costs, as a result of behavioural changes motivated either by advice from national and international bodies or by the public's fear-driven response to the outbreak (APEC, 2004). In Beijing, the estimated $1.4billion indirect costs of SARS to the tourism sector were shown to be 300 times that of the direct medical costs to the city (Beutels, Jia et al., 2009), and, in Hong Kong, the decline in domestic consumption combined with a decrease in tourist spending due to SARS contributed to high levels of unemployment which reached 8.7% in July 2003 (Siu & Wong, 2004). SARS was also blamed for declines in the Hong Kong hospitality industry where 1600 restaurant staff became unemployed and a further 16,000 staff were forced to take leave or pay cuts (Lee & Warner, 2005). Other studies have highlighted the economic impact of the spillover effects of SARS within China and with other countries including Malaysia, Canada, Australia and Singapore (Keogh-Brown & Smith, 2008), mainly related to the tourism sector.
In view of the multi-faceted multi-sectoral impact of infectious disease outbreaks on national economies, the standard “cost of illness” approach to measuring the economic impacts of disease are ill-equipped to perform economic assessments of the full impact of infectious disease outbreaks (Beutels, Edmunds et al., 2008; Brahmbhatt & Dutta, 2008). Furthermore, previous research has highlighted more generally that, since the scale and range of public health emergencies of international concern are sufficient to perturb the general economy, general equilibrium methods, rather than traditional (partial equilibrium) forms of health economic evaluation should be used for analysing their effects (Beutels, Edmunds et al., 2008). In line with this recommendation, this study applies a macroeconomic Computable General Equilibrium (CGE) model to assess the macroeconomic burden of the current Covid-19 pandemic on the UK economy.
1.3. The macro-economics of potential pandemics
Whilst the previous SARS and MERS coronavirus outbreaks did not have a significant economic impact on the UK, macroeconomic simulations of the impact of infectious disease outbreaks were produced around 10 years ago, in the context of a UK flu pandemic, to estimate the potential impact of avoidance behaviour and government policies to reduce disease transmission (Keogh-Brown, Wren-Lewis, et al., 2010; Smith, Keogh-Brown et al., 2009; Smith, Keogh-Brown et al., 2011). These macroeconomic simulations captured the direct and indirect economic impact of a potential pandemic together with school closures and short-term prophylactic absence from work to avoid infection. The results indicated that, depending on the severity of the pandemic, if 30% of the workforce were to absent themselves from work to avoid infection and if schools closed for 13 weeks, these indirect economic impacts could exceed direct health-related economic impacts by a factor of 10. However, although the disease and policy scenarios were considered somewhat extreme when they were first published, they are likely to fall far short of the impact of the national instructions and regulations concerning social distancing which are currently being applied in the UK for Covid-19. It is the purpose of this study, therefore, to produce current estimates of the potential direct and indirect economic impact of the Covid-19 outbreak on the UK economy which capture both the direct health economic impacts and the potential impacts of current measures to either mitigate or suppress epidemic growth.
2. Materials and methods: A whole-economy approach
This study uses a Computable General Equilibrium (CGE) model in order to provide a full analysis of the potential macroeconomic impact of the Covid-19 outbreak and associated policies to the UK. CGE models are multi-sectoral models of the whole economy which have been used extensively in macroeconomic health policy analysis including previous applications to pandemic influenza (Keogh-Brown, Smith, et al., 2010; Smith, Keogh-Brown et al., 2009; Smith, Keogh-Brown et al., 2011) and SARS (Lee & McKibbin, 2012). CGE models are flexible and can be used to simultaneously estimate direct and indirect impacts of health on labour supply, health costs on government budgets and consumption impacts on specific sectors (WHO, 2009). In addition, multi-sectoral CGE models have the capacity to undertake broader macroeconomic policy analyses, and capture behaviour changes for firms and consumers, beyond the health sector, and therefore our UK model is ideally suited to analysing the combined UK economic impact of the UK Covid-19 pandemic burden and related UK mitigation and suppression policy-initiatives.
CGE models arrive at their outputs by capturing the behaviour of different economic agents in the economy. There are four main economic agents: firms, consumers, government, and foreign agents. Firms seek to combine resource inputs to maximise profits, consumers allocate their disposable income between consumption and savings so as to maximise welfare, the government levies taxes, distributes benefits, and purchases goods directly, while foreign agents interact with domestic agents through goods trade (imports/exports), international factor income flows, foreign unrequited transfers and foreign borrowing and lending. The behaviour of the different agents is based on economic theory and is specified mathematically as a system of equations which is solved simultaneously. The model includes multiple production sectors and goods markets, and it also has a government budget which allows for capturing of publicly funded health costs. The model used is the IFPRI standard CGE model (Löfgren, Lee Harris et al., 2001). The equations for this comparative static model are calibrated using economic data, a social accounting matrix (SAM), which, for the purposes of this analysis, is based on the 2015 Supply-Use tables produced by the Office for National Statistics (ONS, 2017) and the model is run forward from the base year, 2015, by targeting key macroeconomic aggregates (WB, 2019) (nominal and real GDP) over the period 2015–2020 such that the model reflects the UK economy for the year of the Covid-19 outbreak.
Linked to the standard CGE model is a simple epidemiological demographic model of the UK population based on UN population projections (UN DESA 2019), and with the capacity to calculate clinical outcomes via application of epidemiological parameters including clinical attack rates (CARs), case fatality rates (CFRs), hospitalisation rates, and intensive care unit (ICU) rates. Since the majority of our scenario estimates relating to Covid-19 transmission and its health effects are expressed as percentages, the demographic model is used to translate those percentages to numbers of symptomatic cases, hospitalisations and deaths. These are used, together with unit costs, to estimate health sector costs which will be borne by the government budget in the model. In addition to the health costs, absenteeism time losses are estimated for patients and caregivers. These are adjusted by age-specific labour force participation rates to calculate labour supply reductions in the model. For each modelling scenario, the model calculates the health- and care-related productivity impacts, health sector costs and also health and care effects on population demographics. More detailed specifications of our direct health impact simulations are provided below.
The detailed specification of production and consumption sectors and inclusion of imports and exports also allows the model to capture the effects of indirect responses to the pandemic and these are also outlined in our specification of modelling scenarios.
The static CGE model used in this study is solved for two equilibrium solutions. The ‘initial baseline’ equilibrium solution reflects a scenario which is the state of the world in 2020 if Covid-19 had not occurred. The model is then shocked to reflect a new state of the world, including the Covid-19 event, and a new ‘C19 baseline’ equilibrium solution is found. Comparison of the two gives the impact of the scenario of Covid-19. More scenarios can then be added with various levels of mitigation and suppression effects and including individual behaviour changes and/or policy initiatives such as social distancing and school closures.
The policy shocks can take various forms in order to reflect the direct and indirect effects of Covid-19 on the UK economy. For example, direct health-related time losses of employed Covid-patients are imposed on the model as economy-wide reductions in labour supply and the accompanying health sector costs are imposed on the government budget. Indirect policy responses such as business closures can be mirrored by reductions in labour and capital supply in specific sectors (which reduces production by those sectors and limits their output). School closures can be simulated as economy-wide reductions in labour supply by those who care for dependent children. Policy shocks can be applied together, in order to estimate the combined impact of direct and indirect impacts, or they can be imposed in isolation to decompose the impacts of specific elements of the policy shocks. The modelling scenarios are outlined in the following subsections.
2.1. Modelling scenarios
As with any emerging infectious disease outbreak there is considerable uncertainty surrounding the current Covid-19 outbreak. However, predictive modelling of the Covid-19 epidemic in the UK has been conducted by the Imperial College COVID-19 Response Team (Ferguson, Laydon et al., 2020) and this model has also predicted the efficacy of non-pharmaceutical interventions to mitigate or suppress epidemic spread. Furthermore, the UK government response to Covid-19 appears to be closely following the type and timing of the policies recommended by the Imperial modelers. The modelling document therefore provides an ideal base from which to produce realistic UK economic simulations in an otherwise very unpredictable situation. Based on the Imperial paper, we model three main scenarios: direct health impacts, pandemic mitigation to slow the spread of the epidemic and suppression to reduce and maintain lower levels of transmission and reduce fatalities. Parameter estimates for all of our modelling scenarios are given in Tables A1.1-A1.3 in appendix A and discussed in sections 1, 2, but the key epidemiological and health-related assumptions are outlined in section 2.1.1 below.Where parameters cannot be supplied by the Imperial modelling study, alternative sources relating to Covid-19, previous knowledge of the SARS and influenza outbreaks, and predictions from pandemic planning documents, are used. In addition, we also employ sensitivity scenarios which vary key parameters in order to capture the potential uncertainty of our estimates.
2.1.1. Scenario 1: Direct health costs and effects only
In order to estimate the direct economic impacts of Covid-19 on the UK economy we parameterise the health-related reductions in labour supply due to the disease and the associated health costs. Various parameters are required in order to distinguish between morbidity effects of differing severity and duration, including, for example, hospitalisations and admissions to intensive care units, and also mortality impacts.
The following parameters are based on the Imperial model of the UK Covid-19 epidemic (Ferguson, Laydon et al., 2020). The CAR is a key parameter and expresses the proportion of people who suffer symptomatic illness. We assume a basic reproductive rate (R0) of 2.4 and that 40% of cases are asymptomatic which yields a CAR of 49%. Recent evidence indicates that the number of clinically confirmed cases of Covid-19 in China varies by age (Zhonghua et al., 2020) and distinguishing clinical effects by age is important in our economic model since health-related labour supply effects only apply to those of working age and costs of ICU treatment differ between children and adults. Since the Imperial study does not provide age specific CARs for the UK population we used the Chinese population based estimates (Verity, Okell et al., 2020) to distribute infections by age. In a similar way, we used the Imperial model's age-specific conversions of Chinese hospitalisations, ICU admissions and deaths (Verity, Okell et al., 2020). which have been scaled to apply to the UK population (Ferguson, Laydon et al., 2020). The CFR is the case fatality rate for symptomatic cases. Specifically, we adopted the Imperial model's aggregate population-weighted infection fatality ratio (IFR) of 0.9%, which implies an aggregate CFR of 1.5%. In a similar way, we calculated age-specific CFRs, based on the Imperial model's age-specific IFRs, and we interpret the difference between implied case fatalities, based on the aggregate and age-specific rates, as a measure of case fatalities outside hospitals. Furthermore, we adopted age-specific hospitalisation rates and age-specific ICU rates from the imperial study (this amounts to assuming that a population-weighted average of 4.4% of symptomatic cases require hospitalisation and 30% of hospitalised cases are admitted to intensive care). For sensitivity analysis a ±50% change in the CAR, CFR, hospitalisation and ICU admission rates are assumed. Finally, our economic modelling scenarios assume that ICU costs for children apply to those aged 0 to 14, and adult costs apply from age 15, working age is assumed to be 15 to 64, those aged 65 and above are assumed to be retired and so do not contribute labour to the economy.
Illness duration is used to estimate the duration of absence from work and consequent loss of labour from Covid-19. For symptomatic non-hospitalised cases we assume individuals will take 7 days of absence from work in accordance with assumptions for illness duration without complications from pandemic flu (Cabinet Office, 2013). Our assumptions for work absence for hospitalised patients are based on illness duration estimates from the Imperial model and assume an additional week of absence following hospitalisation before those who recover can return to work. For standard hospitalisations we assume 5 days of onset and 8 days of hospitalisation which, including the week for recovery implies 15 days of work absenteeism, while for ICU admissions we assume 5 days of onset, 6 days of standard hospitalisation and 10 days in ICU which, after recovery, implies a conservative 20 days of work absenteeism (the durations of hospitalisation and ICU care are also used for health cost estimation of both ICU and non-ICU cases). Costs per case for hospital and ICU treatment are taken from the literature (Baguelin, Hoek et al., 2010; OpenDataNI (2018)) and are provided in the appendices. For fatal cases of Covid-19 in working age individuals we assume a conservative loss, in 2020, of 6 months of labour in accordance with previously published replacement costs for employee departures but excluding the loss of future lifetime earnings.
In order to calculate Covid-19 related losses of productive labour supply from employed individuals, rates for symptomatic, hospitalised, ICU and fatal cases are multiplied by absenteeism duration to form work time loss estimates for working age individuals. These are multiplied by gender-specific labour force participation rates in order to calculate the reductions in labour supply due to Covid-19. This enables the simulation of reductions in productive labour supply to be calculated and presented as part of a holistic set of outputs. Estimates of hospitalisation and ICU admission costs are applied across age groups for the durations specified above. In addition, we make the conservative assumption that no employed caregivers will take time from their work in order to care for infected relatives/friends. Tables showing all the health-related shocks, which are used as inputs to the CGE model, including symptomatic cases, hospitalisations, deaths, time loss estimates and health system costs are included in appendices 2–4.
2.1.2. Scenario 2: Direct health effects with pandemic mitigation
In addition to the direct health effects of an infectious disease outbreak, indirect effects from preventive actions in order to avoid infection are also an important consideration (Sadique, Edmunds et al., 2007; Smith, 2006). These may be provoked either by the responses of individuals or individual organisations to the outbreak or by nationally orchestrated policy advice. In the case of the current covid-19 pandemic in the UK individual preventive actions have been superseded in favour of stringent national policies of social distancing. These policies broadly follow the specifications outlined by the Imperial College COVID-19 Response Team's modelling and our second modelling scenario combines the direct health impacts described above with a policy of mitigation which “focuses on slowing but not necessarily stopping epidemic spread reducing peak healthcare demand while protecting those most at risk of severe disease from infection” (Ferguson, Laydon et al., 2020).
The mitigation policy package described in the Imperial modelling paper is similar to the package of advice from the UK government which is being applied to the current pandemic. This consists of household quarantine for 14 days when an individual within a household is affected, shielding of those over 70 years of age, social distancing of the entire population, and closure of schools and universities. Case isolation for seven days is also mentioned but we assume this will not increase labour supply losses on top of those included within the 14 day home quarantine.
In terms of the economic modelling, this mitigation policy package is captured as follows. Home quarantine for 14 days is reflected in a change in the assumption of work absence for infected cases from seven working days to 10 working days (two weeks). Shielding for those aged over 70 does not affect labour supply since workers are assumed to be aged 15 to 64, but the impact of this policy to reduce deaths, in combination with the other elements, is incorporated in our assumptions for changes in the CFR. When modelling social distancing of the working population, we assume that, as outlined in the current UK government advice, workers will be encouraged only to engage in essential work and to work from home where possible. While central to the assessment of mitigation and suppression interventions, the impact of this advice is difficult to quantify. We assume that it will invoke substantial business closures in non-essential sectors and that, as exhibited in the current UK situation (Cabinet Office, 2020), the supply of tourism related sectors such as hotels and restaurants and recreation and entertainment sectors will be drastically reduced. We model this supply-side shock as a 90% reduction in labour and capital factor employment in hotels and restaurant and entertainment/recreation sectors, and a 50% reduction in labour and capital factor employment in remaining non-essential sectors (where non-essential are defined in the appendix). Whilst estimates are not available for compliance with government advice on business closures, the latter assumption is consistent with the assumption of 50% reduction in workplace contacts assumed in the Imperial model (Ferguson, Laydon et al., 2020).
School closures would normally require working parents who are responsible for dependent children to find care arrangements for their children or take time off work if they are unable to make alternative care arrangements. However, in the case of Covid-19, the social distancing measures will prevent grandparents, relatives or friends outside a household from providing care to children causing working parents to take time off work to care for (and, possibly, educate) their children. Precise estimates for the effect of school closure on working parents in the UK, or estimates of the impact on working parents who try to educate their children at home whilst working, is not available. One Australian study found that 53.4% of parents had to take time off work to care for children with flu (Willis, Preen et al., 2019). According to national statistics, the number of employed women with dependent children was 74% in 2017 (ONS, 2020). We assume 68% of these working mothers will take time off work for the duration of school closures, and thereby that 50% of all UK mothers take time off work.
Preventive actions in response to infectious disease outbreaks are highly unpredictable. Whilst they may be driven by the severity of a pandemic and the fear associated with the number of infections and deaths that result, they may also be influenced by the media (Pickles & Goodwin, 2006; Washer, 2004). However, for the mitigation scenario, the business closures and school-closure related absences described above are assumed to be applied for 12 weeks, as prescribed by the Imperial mitigation scenario.
The impact of the mitigation scenario, as estimated by the Imperial model, is assumed to be a flattening of the epidemic curve reducing overall deaths by 29%. This is captured in the economic model by adjusting the overall and age-adjusted CFR rates.
2.1.3. Scenario 3: Direct health effects with pandemic suppression
In contrast to the mitigation scenario which applies a package of interventions for 12 weeks to slow but not stop epidemic spread, the suppression scenario specified by the imperial model aims to reverse epidemic growth by applying and releasing the package of interventions indefinitely, to ensure the recurring peaks of the disease continue to remain at manageable levels. The policy interventions for suppression remain the same as the mitigation interventions: 14 days of household quarantine for symptomatic individuals, social distancing across the population and closure of schools and universities. However, based on the Imperial model, the business and school closure measures, which were applied on 23rd March, are assumed to continue for 74% of the time from implementation until end-of-2020 (and beyond, but we only simulate until end-of-2020). This implies that closures will continue for 207 days or slightly less than seven months during 2020. The impact of the suppression interventions is, in line with the Imperial model, assumed to reduce the overall and age-adjusted CFR rates by 95% and this will again be captured in the economic model adjusting health-related shocks to the changes in fatality rates.
3. Results
A complete set of our computed health- and mitigation/suppression scenario-related shocks to the UK economy, derived from our Covid-19 assumptions outlined under scenarios 1–3, are presented in appendices 2–4, but our central scenario inputs of the main health effects for the three scenarios are summarised in Table 11 The summarised numbers indicate that, if no action is taken to mitigate the virus spread (‘C19 baseline’ scenario), the direct health effects of Covid-19 outbreak in the UK could result in over 30 million symptomatic cases, 3.3 million hospitalisations, 900,000 ICU admissions and almost half a million hospitalised and non-hospitalised case fatalities (which is within 5% of the value presented in the underlying epidemiological study (Ferguson, Laydon et al., 2020). The vast majority (25.3 million, see appendix 2) of non-hospitalised cases are assumed to be amongst prime age adults, but our assumptions indicate that around 70% of deaths (358,000, see appendix 2) will occur in elderly age groups.
Table 1.
Clinical health impacts - C19 baseline, Mitigation, and Suppression scenarios (number of patient cases).
| C19 baseline | Mitigation | Suppression | |
|---|---|---|---|
| Symptomatic Infections |
32,685,705 |
32,685,705 |
32,685,705 |
| Total Fatalities | 490,286 | 348,103 | 24,272 |
| - hospitalised | 438,789 | 311,540 | 21,723 |
| - non-hospitalised |
51,496 |
36,562 |
2549 |
| Hospitalised | 3,285,781 | 3,285,781 | 3,285,781 |
| - ICU | 907,027 | 907,027 | 907,027 |
| - non-ICU |
2,378,754 |
2,378,754 |
2,378,754 |
| Symptomatic (not hospitalised) | 29,399,924.29 | 29,399,924 | 29,399,924 |
3.1. Direct health-related economic burden
Economic impacts of the C19 baseline scenario simulation (scenario 1) are shown in Table 2. The total direct economic burden from Covid-19 in the UK, measured by changes in real GDP, is just over £39.6bn or 1.73% of GDP. Decomposition of these effects indicates that just £0.7bn (0.03%) of the health-related economic impact on real GDP is attributable to hospital costs which are primarily made up from ICU patient admissions (£0.6bn). The real government consumption figures show that hospital costs imposed by Covid-19 (£8.9bn increase in government consumption) are more substantial than reflected in the GDP figures,2 but since government consumption is funded by taxation, the additional healthcare funding required in the model is primarily drawn from private consumption channels and, whilst it will place a significant burden on households’ welfare via increased taxation and decreased consumption (-£40.5bn or 2.7% as shown in Table 2), the isolated impact of increased health costs on GDP overall is likely to be small.
Table 2.
Macroeconomic impacts - C19 baseline scenario (bn GBP, 2020 prices).
| Real GDP | Real GDP (%) | Real Private Consumption | Real Private Consumption (%) | Real Government Consumption | Real Government Consumption (%) | |
|---|---|---|---|---|---|---|
| Total health-related costs | −39.6 | −1.73% | −40.5 | −2.70% | 8.5 | 1.93% |
| - Hospital Costs, total | −0.7 | −0.03% | −7.6 | −0.50% | 8.9 | 2.02% |
| - hospitalised fatalities | −0.3 | −0.01% | −4.5 | −0.30% | 5.3 | 1.20% |
| - hospitalised recovered ICU | −0.3 | −0.01% | −4.3 | −0.29% | 5.0 | 1.14% |
| - hospitalised recovered non-ICU | −0.1 |
0.00% |
−1.4 |
−0.09% |
1.5 |
0.35% |
| - Labour supply losses, total | −38.9 | −1.70% | −31.7 | −2.11% | −2.1 | −0.48% |
| - hospitalised fatalities | −2.8 | −0.12% | −2.3 | −0.15% | −0.1 | −0.03% |
| - hospitalised recovered | −4.7 | −0.21% | −3.9 | −0.26% | −0.2 | −0.05% |
| - non-hospitalised recovered | −30.8 | −1.35% | −25.3 | −1.68% | −1.6 | −0.37% |
The large health-related impact on GDP is mainly attributable to health-related labour supply losses of £38.9bn. The vast majority of these economic losses (£30.8bn) are due to work absence from non-hospitalised cases, which is not surprising since nearly 70% of symptomatic Covid-19 cases are assumed to occur in working age individuals who will not require hospitalisation. The economic cost of hospitalised but recovered patients on GDP is estimated to be £4.7bn while the economic cost of lost labour from fatalities in the labour force amount to £2.8bn. In practice these health-related costs cannot be isolated from the broader indirect economic impacts and do not capture the substantial loss of life which occurs from the 358,000 deaths (not shown) that are assumed to occur outside the workforce.
3.2. Mitigation scenario economic burden
The total economic impact of the mitigation scenario is presented in Table 3 and, including both direct health-related economic costs and public prevention related costs, it amounts to £308bn or 13.5% of GDP. These impacts represent a potentially unprecedented loss to the UK economy in a single year and includes a private household welfare loss of 15.1% or £261.2bn measured by consumption (equivalent variation = -£261.4bn). Government consumption is also expected to reduce by £14.7bn (3.3%). Under the mitigation strategy, the direct health-related economic burden increases by a third to £53.1bn (2.3% of GDP). The change in the health-related economic burden derives from an increased loss of labour under the mitigation strategy compared with the direct health-related burden simulation. Under mitigation, the number of working age deaths reduce, decreasing the economic losses due to fatalities from £2.8bn at baseline to £2.0bn. The reduction in deaths amongst working age individuals increases the number of hospitalised recovered patients who return to work but this increase in the number of individuals who are hospitalised and recover results in an increase from £4.7bn to £4.9bn in the costs from labour lost amongst hospitalised survivors. The largest contributor to the increased economic burden from direct health effects derives from non-hospitalised recovered patients who, under the mitigation scenario's quarantine rules take a longer absence from work (two weeks) compared with the baseline assumption of seven working days. This increases economic time loss estimates for non-hospitalised recovered individuals from £30.8bn to £44.8bn. The hospital costs under the mitigation scenario are unchanged since, although deaths are reduced, we assume no difference in the duration of hospitalisation and ICU treatment between fatal and non-fatal cases.
Table 3.
Macroeconomic impacts - public Mitigation scenario (bn GBP, 2020 prices).
| Real GDP | Real GDP (%) | Real Private Consumption | Real Private Consumption (%) | Real Government Consumption | Real Government Consumption (%) | |
|---|---|---|---|---|---|---|
|
Total health and prevention-related costs |
−308.0 |
−13.5% |
−226.2 |
−15.1% |
−14.7 |
−3.3% |
|
Total health-related costs |
−53.1 |
−2.3% |
−51.8 |
−3.5% |
8.6 |
1.9% |
| - Hospital Costs, total | −0.7 | 0.0% | −7.6 | −0.5% | 8.9 | 2.0% |
| - hospitalised intensive-care | −0.3 | 0.0% | −4.5 | −0.3% | 5.3 | 1.2% |
| - hospitalised non-intensive-care | −0.3 |
0.0% |
−4.3 |
−0.3% |
5.0 |
1.1% |
| - Labour supply losses, total | −52.4 | −2.3% | −42.2 | −2.8% | −3.0 | −0.7% |
| - hospitalised fatalities | −2.0 | −0.1% | −1.6 | −0.1% | −0.1 | 0.0% |
| - hospitalised recovered | −4.9 | −0.2% | −4.1 | −0.3% | −0.2 | −0.1% |
| - non-hospitalised recovered |
−44.8 |
−2.0% |
−36.3 |
−2.4% |
−2.5 |
−0.6% |
|
Total public prevention-related costs |
−261.4 |
−11.4% |
−172.6 |
−11.5% |
−31.2 |
−7.1% |
| - School closures | −66.1 | −2.9% | −37.5 | −2.5% | −16.4 | −3.7% |
| - labour supply losses, caregivers | −66.1 |
−2.9% |
−37.5 |
−2.5% |
−16.4 |
−3.7% |
| - Business closures | −200.9 | −8.8% | −138.0 | −9.2% | −16.2 | −3.7% |
| - domestic business closures - other non-essential | −154.8 | −6.8% | −101.2 | −6.7% | −11.6 | −2.6% |
| - recreational services sector | −17.3 | −0.8% | −14.5 | −1.0% | −0.9 | −0.2% |
| - hotels & restaurants sector | −38.5 | −1.7% | −32.3 | −2.2% | −2.0 | −0.5% |
However, the economic burden from the mitigation scenario is dominated by the non-health related policy impacts which total £264.1bn or 11.4% of GDP. These costs include labour supply reductions attributable to 12 weeks of school closure (£66.1bn) which, by itself, exceeds the direct health-related burden. Domestic business closures in non-essential sectors is the largest single contributor at £200.9bn (8.8% of GDP), and this includes substantial losses for recreation services (£17.3bn) and hotels and restaurants (£38.5bn). In terms of the population health benefits, the mitigation policies are estimated to reduce the number of Covid-19 UK deaths by almost one third (saving just over 142,000 lives).
3.3. Suppression scenario economic burden
The total macroeconomic cost of the public Suppression scenario is presented in Table 4 and amounts to £668.4bn. This is almost one third (29.2%) of UK GDP for the year of 2020 and it includes a private household welfare loss of 30.0% or £450.0bn measured by consumption (equivalent variation = -£451.2bn). A reduction in government consumption of £73.4bn (16.7%) is also estimated. The direct health-related macroeconomic burden of £51.4bn contributes just 8% of the total economic impact and is slightly smaller than the equivalent £53.1bn impact for the mitigation scenario. The direct health-related macroeconomic impacts relating to suppression are a little smaller than for the mitigation scenario since the suppression scenario assumes there will be a reduction in deaths but no reductions in the number of symptomatic cases, hospitalisations or ICU admissions. Therefore the health-related economic impacts for hospitalised fatalities for suppression (£0.1bn) are smaller than for mitigation (£2.0bn), but economic impacts for recovered hospitalisations increase slightly from £4.9bn for mitigation to £5.2bn for suppression. Since we assume no difference in the duration of hospitalisation and ICU treatment between fatal and non-fatal cases, the hospitalisation costs of suppression are the same as for the mitigation and disease only scenarios.
Table 4.
Macroeconomic impacts - public Suppression scenario (bn GBP, 2020 prices).
| Real GDP | Real GDP | Real Private Consumption | Real Private Consumption | Real Government Consumption | Real Government Consumption | |
|---|---|---|---|---|---|---|
|
Total health and prevention-related costs |
−668.4 |
−29.2% |
−450.0 |
−30.0% |
−73.4 |
−16.7% |
| Total health-related costs | −51.4 | −2.2% | −50.4 | −3.4% | 8.6 | 1.9% |
| - Hospital Costs, total | −0.7 | 0.0% | −7.6 | −0.5% | 8.9 | 2.0% |
| - hospitalised intensive-care | −0.3 | 0.0% | −4.5 | −0.3% | 5.3 | 1.2% |
| - hospitalised non-intensive-care | −0.3 |
0.0% |
−4.3 |
−0.3% |
5.0 |
1.1% |
| - Labour supply losses, total | −50.7 | −2.2% | −40.9 | −2.7% | −2.9 | −0.7% |
| - hospitalised fatalities | −0.1 | 0.0% | −0.1 | 0.0% | 0.0 | 0.0% |
| - hospitalised recovered | −5.2 | −0.2% | −4.3 | −0.3% | −0.2 | −0.1% |
| - non-hospitalised recovered |
−44.8 |
−2.0% |
−36.3 |
−2.4% |
−2.5 |
−0.6% |
| Total public prevention-related costs | −632.9 | −27.7% | −402.5 | −26.8% | −93.6 | −21.2% |
| - School closures | −166.2 | −7.3% | −94.0 | −6.3% | −41.1 | −9.3% |
| - labour supply losses, caregivers | −166.2 |
−7.3% |
−94.0 |
−6.3% |
−41.1 |
−9.3% |
| - Business closures | −501.5 | −21.9% | −325.2 | −21.7% | −62.6 | −14.2% |
| - domestic business closures - other non-essential | −386.6 | −16.9% | −244.4 | −16.3% | −43.9 | −10.0% |
| - recreational services sector | −44.3 | −1.9% | −36.7 | −2.4% | −2.7 | −0.6% |
| - hotels & restaurants sector | −95.5 | −4.2% | −77.1 | −5.1% | −5.8 | −1.3% |
However, the direct health impacts are dwarfed by the £632.9bn of economic losses to GDP from the public prevention interventions. The longer school closures under the suppression scenario impose an impact on UK GDP of £166.2bn, losses from the closures in the recreational sector contribute a further £44.3bn, hotels and restaurant closures contribute £99.5bn and closures of remaining non-essential businesses makes the largest contribution: £386.6bn loss to GDP.
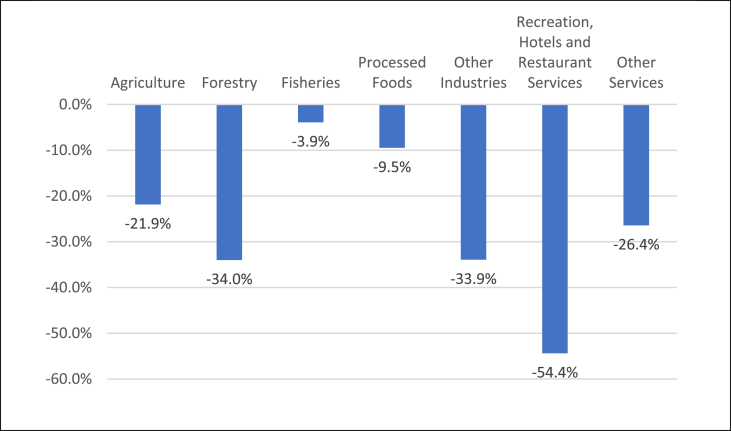
Relative sector-level production changes are illustrated in Fig. 1, and they underline the sharp drop in sector-level activity following from the Suppression scenario. Hotels and restaurant services, and recreational activities, drop by an annualised 54.4%, while processed food sectors are much less affected (−9.5%) and Fisheries are least affected (−3.9%) due to high and persistent exports. While the agricultural production decline (−21.9%) is less than the overall average (−27.9%), it represents a remarkable demand side shock following from a collapse in non-agricultural value added creation.
Fig. 1.
Sector-level output changes – public Suppression scenario (%).
3.4. Sensitivity analysis
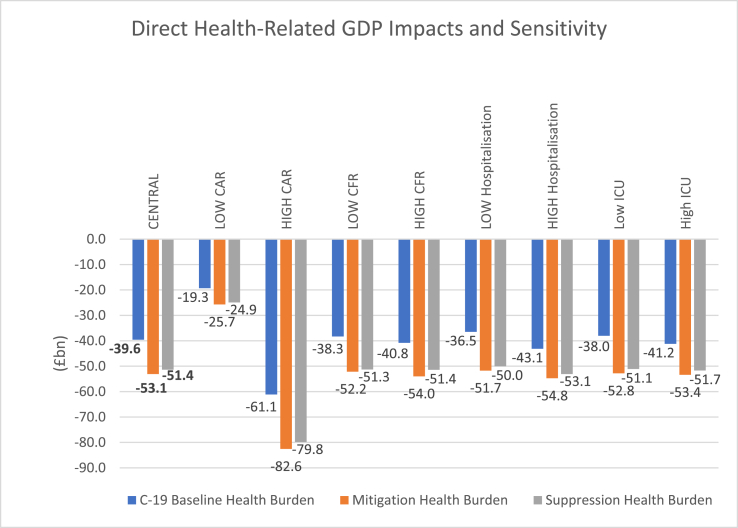
Sensitivity analyses of key disease parameters was employed to illustrate the potential variations in our results due to uncertainty. Tables of sensitivity analysis results are presented for all three scenarios in appendix 5 and direct health impacts are shown in Fig. 2. For each sensitivity analysis, the parameter concerned is decreased or increased by 50% to give an upper or lower limit value. For the C19 baseline scenario, our results indicate that respectively lowering and increasing the clinical attack rate, from our central 48% value, changes the direct health-related economic burden to respectively £19.3bn and £61.1bn (±51–54%), and this is the epidemiological parameter to which the economic impacts are most sensitive. Lowering and increasing the overall and age-specific case fatality rates changes the economic burden to £38.3bn and £40.8bn (±3%), which shows the insensitivity of our economic impacts to the fatality ratio, primarily because most of the deaths occur amongst elderly non-workers and our assumptions of the ICU treatment duration do not alter if a case proves to be fatal. Similarly, variations in our age-specific hospitalisation rates have a relatively small impact changing the economic burden to £36.5bn and £43.1bn (±7–8%). This is because varying the number of hospitalised working age individuals by approximately 900,000 makes a relatively small difference in terms of work time losses compared with the more than 25 million other symptomatic non-hospitalised individuals. Finally, varying age-specific ICU admission rates also has a small effect on our economic burden estimates, changing the economic burden estimates to £38.0bn and £41.2bn (±4%). This variation is small because ICU cases contribute little to the overall health related economic burden. The patterns of variations for the mitigation and suppression scenarios are similar to the C19 baseline scenario sensitivity results. As mentioned in Sections 2, 3, the health-related economic impacts for the mitigation scenario are the largest, followed by the health-related suppression impacts. Nonetheless, the relative sensitivity, of these scenarios, to variation in epidemiological parameters, is very close to the relative sensitivity of the C19 baseline results implying that variation in CAR rates changes the direct health-related economic burden by ±52–56% while other impacts are within ±10%.
Fig. 2.
Sensitivity analyses of Baseline, Mitigation, and Suppression scenario Economic Health Burdens.
4. Discussion
Our simulations show that the economic impact of Covid-19 is likely to be dominated by the public prevention measures rather than the direct health costs of the disease. With any modelling study, the accuracy and appropriateness of the results hinge upon the accuracy of the parameters used in the model and modelling scenarios regardless of the quality and appropriateness of the model itself. In the case of the current Covid-19 outbreak, uncertainty still exists regarding the future progression of the disease, its clinical effects, the extent and duration of the government-imposed responses to mitigate the disease, and the efficacy of those responses to mitigate the disease. As such, the specific values of economic impact which have been estimated in this modelling study cannot be stated with certainty, but we have designed our simulations to reflect current UK estimates of both the disease burden and measures to mitigate or suppress it. We have also allowed for uncertainty by including upper and lower estimates of key transmission and fatality parameters such that our simulations cover a broad range of outbreak severity which, it is reasonable to assume, will cover the possibilities for a significant Covid-19 pandemic in the UK. However, although our estimates may not simulate the economic impact of Covid-19 with absolute precision, they do illustrate the relative importance of the type and duration of public prevention measures which, though necessary in order to reduce mortality, have significant economic impacts. Furthermore, our three month mitigation scenario results which predict a 13.5% loss to GDP agree with the recent analysis by UKs Office for Budget Responsibility (OBR, 2020) which estimated a 13% loss for the UK for their three month lockdown scenario. Whilst similar models could be produced for other countries, the policy scenarios and health effects used in our model are UK-specific. Since many high income countries have broadly similar economic structures, similar interventions might be expected to yield similar economic impacts in other high income country contexts. However, the current UK scenarios tend to be slightly more restrictive than those currently employed in most other high income country contexts. With regard to other country contexts, research indicates that while many high income countries have strong social protection mechanisms in place, which may allow for similar types of intervention for Covid-19 mitigation, many lower- and middle-income countries have weaker social protection mechanisms (Loayza, N. & Pennings, 2020). Therefore, the selection of and adherence to mitigation policies in other lower- and middle-income country contexts is likely to differ. In addition, there may be country variations in terms of those who are most at risk of infection, those who are most at risk of dying, access to healthcare, and there may be variations in risk of transmission to those who are most economically active. However, the conclusions, particularly regarding the relative importance of health and non-health impacts and the relative impact of different types of intervention are likely to be of broad relevance to many country contexts.
Our simulations show that the direct health-related economic impacts of Covid-19 in the UK are likely to be substantial: around 2% of GDP and approximately equivalent to one quarter of the usual UK spending on health for a given year. Furthermore, our sensitivity analysis shows that halving or doubling key parameters will at most halve or double the health-related economic burden impact and therefore our results are reasonably robust to variations in epidemiological assumptions. In any ‘normal’ year, these health costs alone would be of significant concern, but our simulations suggest that the costs of mitigating or suppressing Covid-19 are likely to be 7 to 16 times larger, respectively, depending on whether a mitigation or suppression strategy is considered. Current epidemiological modelling of non-pharmaceutical behavioural interventions to combat Covid-19 suggests that the package of interventions, that have been applied in the UK, are necessary in order to suppress the pandemic to a level whereby intensive care units will be able to cope with the number of cases. However, our analysis suggests that the different elements of the package have very different cost implications.
Our simulations do not attach a direct cost to the enforcement of social distancing of the over 70s. In practice, social distancing of the elderly will have an economic impact on consumption since the elderly consume goods and services across sectors, some of which they may not be able to access so easily from home. However, since we have captured the closure of many non-essential businesses, the decline in demand from the elderly need not be captured separately. The department for Education conducted a survey in 2018 (DfE, 2018) which suggested that 38% of working parents utilise care by relatives or friends in order to enable them to work. Therefore, if social distancing of the over 70s were not in place, it is likely that this would mitigate the cost of closing schools, but in the case of Covid-19 no care for school children by members outside the immediate household is possible and therefore the impact of school closures on lost labour by working parents cannot be mitigated by alternative care arrangements. Therefore, although the cost of social distancing by the over 70s is not captured separately in our analysis, it does have a bearing on the cost of mitigation or suppression of the disease since it eliminates the option for working parents to use elderly family members or friends to care for their children while they work. In such circumstances, where care for school children and support of their education from home must be managed within the household, the impact on working parents is highly uncertain and the reality may differ from our estimates, which are based on evidence from working mothers.
The current implementation of home quarantine for 14 days when an individual within a household is suspected of Covid-19 infection increases the economic burden of Covid-19 since it increases the duration of work absence by infected individuals. In our simulations, this contributes up to £5.9bn of additional costs to the UK economy.
Lost labour by working parents attributable to school closures is estimated to have a substantial impact on the UK economy whether it be for 12 weeks of pandemic mitigation (approx. £66bn) or for the longer suppression package (£166bn). Whilst the degree to which parents can continue to work under these conditions is difficult to predict and will vary according to the type of work undertaken, it is apparent that the closure of schools combined with the inability of parents to access care arrangements outside the household is likely to prove disruptive and costly.
Our simulations of the closure of recreational businesses, hotels and restaurants indicate that, depending on the duration of the closure, the impact on the UK economy of these closures could range between approximately £55bn and £140bn. We have assumed that approximately 90% of these businesses will close while government policies of mitigation or suppression are in place. Currently UK hotels are accessible to key workers and homeless residents during the pandemic and some food retailers are supplying take-away food, but it is not currently possible to verify how closely this mirrors the 10% of hotel/restaurant activity we have assumed to continue during mitigation/suppression. Recreation sectors have closed almost completely in the UK and our assumption that 90% of such businesses will close may, therefore, be an under-estimate of this closure effect.
The most substantial economic impacts simulated in our model occur due to the closure of the remaining non-essential businesses, i.e. beyond hotels and restaurants and recreational sectors, and these closures are also the most difficult to estimate. Currently UK workers are being encouraged to stay home and also to work from home where possible. There may be variations across sectors in terms of the extent to which businesses either scale-back or continue at close to normal levels through home-working arrangements and this will depend on the nature of the work/businesses affected. However, our illustrative scenarios highlight that if 50% of remaining non-essential businesses were to close, this could provoke unprecedented losses to the UK economy ranging between £155bn for 12 weeks of mitigation to £386bn for suppression. The extent of these costs highlights a key trade-off that will be faced by business owners when deciding how and how long they can adjust their working practices to conform to social distancing requirements.
Clearly the losses estimated under the suppression scenario, where nearly 22% of GDP is lost through combined business closures over a nine month period, are not likely to be sustainable. As mentioned earlier, the SARS outbreak highlighted how struggling businesses failed and many employees lost their jobs under less severe economic circumstances than those predicted by our modelling. Therefore, the UK government will face increasing pressures to lift restrictions, even in periods where increasing transmission may dictate that the restrictions on social and economic activity should be (re-)instated or to enact policy initiatives which may help businesses and employees e.g. via labour re-training and new infrastructure for tele-working, or re-organisation of workplaces to maintain social distancing and, at the same time, to keep new coronavirus reproduction numbers under control. Currently economic support mechanisms have been put in place by the UK government to encourage conformity with business closure instructions and these include measures such as the Coronavirus Job Retention scheme, schemes for claiming back statutory sick pay paid due to Covid-19 and various reliefs and funds from which businesses and self-employed workers may claim for Covid-19 related losses. These measures are essential, but our analysis indicates that the £330bn pledged on 17th March by the UK Chancellor may not be sufficient if the policies imposed to combat Covid-19 in the UK exceed the duration specified under our mitigation scenario.
In terms of the motivation for our scenarios, the mitigation scenario we have implemented was designed to reduce the extent to which demand for ICU beds exceeds supply, but not necessarily to suppress the pandemic to manageable levels. However, since the production of the modelling study underlying this analysis was produced, the capacity for managing critical cases of Covid-19 in the UK has expanded via the construction of the new NHS Nightingale hospital and new ventilators have been produced for use during Covid-19. Nonetheless, the UK government's motivation to pursue future mitigation and suppression seems to remain strong.
Several questions remain which cannot be addressed in our comparative static modelling simulation. Aside from the uncertainties of the disease itself, the most important questions which have not been addressed in our simulations relate to the medium and long-term effects of the outbreak. Our results illustrate the potential direct and indirect economic impacts of Covid-19 and prevention behaviours and those costs appear to be substantial. However, experience shows that a proportion of the costs of previous outbreaks, such as SARS, proved to be temporary and many of the losses during the outbreak were made-up subsequently and this is likely to be the case for Covid-19. However, this optimism should be tempered by the possibility that, as with SARS, economic declines from a pandemic can cause struggling businesses to fail and result in a longer-term increase in unemployment. This was the case for businesses in the Hong Kong Hotel sector during SARS, and business failures may also affect the degree to which the UK economy and livelihoods return to normal levels after Covid-19. That is, there could be longer-term and structural implications that our single-period model has not been able to establish. The unknown dynamic effects may, therefore, have important implications to set our results in context. If, following the pandemic, a subsequent economic bounce-back, in the medium term, is enhanced through additional economic support measures, it may be possible to limit the permanency of some of the economic repercussions predicted in our worst case scenario results. However, it should also be highlighted that, in the absence of an effective vaccine, the economic constraints imposed on the UK economy by Covid-19 and suppression policies could continue beyond 2020 imposing longer-term economic losses and requiring longer-term economic support to sustain businesses and workers. Therefore, it is clearly important from the health and economic perspectives that every effort is made to rapidly develop and obtain an effective vaccine which will alleviate the need for significant population-wide preventive actions. Furthermore, from the economic perspective, further analysis might show that additional government mitigation initiatives, including investment in temporary hospitals and ICU equipment and staff, may also be justified in order to maintain longer periods of ‘normal’ economic activity between periods of suppression in order to alleviate the strain on the UK economy of non-pharmaceutical preventive actions. However, more information on the costs, timescale and feasibility of additional construction of temporary ICU units and provision of ICU equipment would be required in order to evaluate this hypothesis since the facilities produced to date have been under-utilised.
One final aspect of the macroeconomic impacts of Covid-19 which cannot be assessed using our single country model are the consequences of pandemics on global movement and trade. These can be captured using global CGE models. Global CGE studies of Covid-19 to date include an application of the G-Cubed model (McKibbin & Fernando, 2020), the ImpactECON Supply-Chain Model (Walmsley et al., 2020) which is a modified version of the GTAP model, and the ENVISAGE model (Maliszewska et al., 2020). All three model frameworks rely on the global GTAP data base. The McKibbin model application, which is the most sophisticated of these global model applications, explores a range of country-specific shocks involving direct health-related shocks (morbidity and mortality-related labour force impacts), and indirect shocks to equity risk premia, sector-specific (transport) costs of production, consumer preferences (and consumption demand), and government expenditures. However, due to the early publication date (end-of-February 2020), the study relies heavily on data from the 2003 SARS epidemic from China. One global CGE model has been used to assess the direct health related impacts of Covid-19 (Maliszewska et al., 2020). These estimates are broadly in line with our direct health estimates (a 2%–5% fall in GDP for various countries). Whilst future additional Covid-specific analyses of the global trade implications of policy interventions from global models would be complementary to this analysis, they are unlikely to capture the tailored policy specifications used in our single country context.
5. Conclusion
Covid-19 has the potential to impose unprecedented economic impacts on the UK economy and those impacts are likely to be dominated by the indirect costs of mitigation or suppression of the pandemic. Therefore, although priority should be given to policies which delay and flatten the pandemic peak by mitigating the spread of the disease, our estimates indicate that the duration of mitigation or suppression policies are key to determining the economic impact. According to our simulations, the initial economic support mechanisms, promised by the UK government, may require further expansion if the pandemic is to be effectively suppressed without causing the collapse of many businesses and the loss of livelihoods of many workers. The need for additional support will depend critically on whether the government is able to reduce the duration of business and school closures through other initiatives, e.g. via labour re-training and new infrastructure for tele-working, or through re-organisation of workplaces to maintain social distancing and keep new coronavirus reproduction numbers under control, until a vaccine is developed and ready for mass-production.
Disclaimer
The views expressed in the submitted article are those of the authors and not an official position of the institution or funder.
Funding
This project has received funding from the European Union’s Horizon 2020 research and innovation program -project EpiPose (No 101003688).
Ethical approval
Not required for this study.
CRediT authorship contribution statement
Marcus R. Keogh-Brown: Formal analysis, Writing - original draft, was responsible for designing the study and modelling scenarios, for analysis and drafting of the paper. Henning Tarp Jensen: Formal analysis, Writing - original draft, constructed the model, produced analysis and contributed to drafting of the paper. W. John Edmunds: Writing - original draft, advised on the design of the scenarios and disease parameters and contributed to drafting of the paper. Richard D. Smith: Writing - original draft, initiated the work, oversaw and advised on all aspects of the work, completed final drafting of the paper and is guarantor.
Declaration of competing interest
None declared.
Footnotes
The decomposition of results presented in Table 2, Table 3, Table 4 and the appendices are produced from individual simulations of the scenarios described in the first column. Since combining scenarios produces interaction effects in the CGE model, the impacts attributed to the sum of isolated scenarios does not necessarily match the combined impacts exactly.
The health system treatment costs for Covid-19 are even higher at £43.0bn (see appendix 2), but reduced activity in other parts of the health system, and a general decline in government revenues, limits the expansion of health and general government spending.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2020.100651.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- APEC Commentaries & analyses — the economic impact of SARS on the APEC region. Asia-Pacific Biotech News. 2004;8(1):33–38. [Google Scholar]
- Baguelin M., Hoek A.J., Jit M., Flasche S., White P.J., Edmunds W.J. Vaccination against pandemic influenza A/H1N1v in England: A real-time economic evaluation. Vaccine. 2010;28(12):2370–2384. doi: 10.1016/j.vaccine.2010.01.002. [DOI] [PubMed] [Google Scholar]
- Beutels P., Edmunds W.J., Smith R.D. Partially wrong? Partial equilibrium and the economic analysis of public health emergencies of international concern. Health Economics. 2008;17(11):1317–1322. doi: 10.1002/hec.1339. [DOI] [PubMed] [Google Scholar]
- Beutels P., Jia N., Zhou Q.-Y., Smith R., Cao W.-C., De Vlas S.J. The economic impact of SARS in Beijing, China. Tropical Medicine and International Health. 2009;14(s1):85–91. doi: 10.1111/j.1365-3156.2008.02210.x. [DOI] [PubMed] [Google Scholar]
- Brahmbhatt M., Dutta A. 2008. On SARS type economic effects during infectious disease outbreaks. [Google Scholar]
- Cabinet Office . Cabinet Office; Whitehall, London: 2013. Preparing for pandemic influenza guidance for local planners. [Google Scholar]
- Cabinet Office . C. O. a. M. o. H. C. a. L. Government; 2020. Guidance closing certain businesses and venues.https://www.gov.uk/government/publications/further-businesses-and-premises-to-close/further-businesses-and-premises-to-close-guidance Online. Cabinet Office. [Google Scholar]
- DFE . Department for Education; London, UK: 2018. Childcare and early years survey of parents: 2018. [Google Scholar]
- Ferguson N., Laydon D., Nedjati Gilani G., Imai N., Ainslie K., Baguelin M. Imperial College COVID-19 Response Team; 2020. Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand. [Google Scholar]
- Hamzelou J. UK’s scientific advice on coronavirus is a cause for concern. New Scientist. 2020;245(3275):9. doi: 10.1016/S0262-4079(20)30613-8. Online. 3275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keogh-Brown M.R., Smith R.D. The economic impact of SARS: How does the reality match the predictions? Health Policy. 2008;88(1):110–120. doi: 10.1016/j.healthpol.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keogh-Brown M., Smith R., Edmunds J., Beutels P. The macroeconomic impact of pandemic influenza: Estimates from models of the United Kingdom, France, Belgium and The Netherlands. The European Journal of Health Economics. 2010;11(6):543–554. doi: 10.1007/s10198-009-0210-1. [DOI] [PubMed] [Google Scholar]
- Keogh-Brown M., Wren-Lewis S., Edmunds W., Beutels P., Smith R. The possible macroeconomic impact on the UK of an influenza pandemic. Health Economics. 2010;19:1345–1360. doi: 10.1002/hec.1554. [DOI] [PubMed] [Google Scholar]
- Lee J.-W., McKibbin W.J. ANU Press; 2012. The impact of SARS. China: New engine of world growth. R. Garnaut and L. Song; pp. 19–33. [Google Scholar]
- Lee G.O.M., Warner M. Epidemics, labour markets and unemployment: The impact of SARS on human resource management in the Hong Kong service sector. International Journal of Human Resource Management. 2005;16(5):752–771. [Google Scholar]
- Loayza N., Pennings S. World Bank Malaysia hub; 2020. Macroeconomic policy in the time of COVID-19: A primer for developing countries. [Google Scholar]
- Löfgren H., Lee Harris R., Robinson S. International Food Policy Research Institute (IFPRI); 2001. A standard computable general equilibrium (CGE) model in GAMS. [Google Scholar]
- Maliszewska M., M A., van der Mensbrugghe D. World Bank; Washington DC: 2020. The potential impact of COVID-19 on GDP and trade. World bank policy research working paper No. 9211. [Google Scholar]
- McKibbin W., Fernando R. CAMA working paper No. 19/2020. Centre for Applied Macroeconomic Analysis, Australian National University; 2020. The global macroeconomic impacts of COVID-19: Seven scenarios. [Google Scholar]
- Noy I., Shields S. Asian Development Bank; 2019. The 2003 severe acute respiratory syndrome epidemic: A retroactive examination of economic costs. [Google Scholar]
- OBR . Office for Budget Responsibility; 2020. The OBR's coronavirus analysis. [Google Scholar]
- ONS . Office of National Accounts; London, UK: 2017. Input–output supply and use tables 2017 edition 1997-2015. UK Statistics Authority. [Google Scholar]
- ONS . Office for National Statistics; London, UK: 2020. Labour market statistics time series: Employment rates of men and women with and without dependent children (aged 16 to 64), April to June 1996 to April to June 2017, England. [Google Scholar]
- Pickles H., Goodwin R. Pandemic flu: Encouraging a positive population response. Eurohealth. 2006;12:10–12. [Google Scholar]
- Sadique M.Z., Edmunds W.J., Smith R.D., Meerding W.J., de Zwart O., Brug J. Precautionary behavior in response to perceived threat of pandemic influenza. Emerging Infectious Diseases. 2007;13(9):1307–1313. doi: 10.3201/eid1309.070372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siu A., Wong R. Economic impact of SARS: The case of Hong Kong. Asian Economic Papers. 2004;3:62–83. [Google Scholar]
- Smith R.D. Responding to global infectious disease outbreaks: Lessons from SARS on the role of risk perception, communication and management. Social Science & Medicine. 2006;63(12):3113–3123. doi: 10.1016/j.socscimed.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith R.D., Keogh-Brown M.R., Barnett T. Estimating the economic impact of pandemic influenza: An application of the computable general equilibrium model to the UK. Social Science & Medicine. 2011;73(2):235–244. doi: 10.1016/j.socscimed.2011.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith R.D., Keogh-Brown M.R., Barnett T., Tait J. The economy-wide impact of pandemic influenza on the UK: A computable general equilibrium modelling experiment. BMJ. 2009;339:b4571. doi: 10.1136/bmj.b4571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UN DESA . UN Department of Economic and Social Affairs; New York: 2019. World population prospects: The 2017 revision. [Google Scholar]
- Verity R., Okell L.C., Dorigatti I., Winskill P., Whittaker C., Imai N. Estimates of the severity of coronavirus disease 2019: A model-based analysis. The Lancet Infectious Diseases. 2020;20(6):669–677. doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walmsley T., Rose A., Wei D. University of Southern California; 2020. Impacts on the U.S. Macroeconomy of mandatory business closures in response to the COVID-19 pandemic. CREATE working paper. [Google Scholar]
- Washer P. Representations of SARS in the British newspapers. Social Science & Medicine. 2004;59(12):2561–2571. doi: 10.1016/j.socscimed.2004.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WB . The World Bank; Washington, DC: 2019. World development indicators. The World Bank. [Google Scholar]
- WHO . World Health Organisation; 2009. WHO guide to identifying the economic consequences of disease and injury Geneva. [Google Scholar]
- WHO . World Health Organisation; Geneva: 2020. Novel coronavirus (2019-nCoV) SITUATION REPORT - 1, 21 january 2020. [Google Scholar]
- Willis G.A., Preen D.B., Richmond P.C., Jacoby P., Effler P.V., Smith D.W. The impact of influenza infection on young children, their family and the health care system. Influenza Other Respir Viruses. 2019;13(1):18–27. doi: 10.1111/irv.12604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhonghua Liu, Xing Bing, Xue Za Zhi. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) — China, 2020. China CDC Weekly. 2020;2(8):113–122. [PMC free article] [PubMed] [Google Scholar]
- OpenDataNI (2018). Health Trust Specialist Services Reference Costs 2016-17. https://data.gov.uk/dataset/03209d9b-fe35-4f85-acc9-590c26c0b4d3/health-trust-specialist-services-reference-costs-2016-17. (Accessed 28/08/2020).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.