Abstract
Hemorrhagic cholecystitis is a rare cause of abdominal pain that can have dire consequences. We report a case of hemorrhagic cholecystitis in a 51-year-old female presenting as shock and abdominal pain. The patient was transported to the emergency room. Ultrasound scan revealed hemoperitoneum and cholecystitis features. On computed tomography, mild gallbladder wall thickening and high density materials in the gallbladder suggested acute calculous cholecystitis, bleeding tumor, or hemorrhagic cholecystitis. An urgent cystic arterial embolization and percutaneous transhepatic drainage were done. After initial stablization, laparoscopic cholecystectomy was performed that revealed a necrotic gallbladder filled with large blood clots. It was important for timely management by having an early recognition of this potentially fatal condition.
Keywords: Hemorrhagic, Cholecystitis, Embolization, Angiography, Laparoscopic cholecystectomy
Introduction
Hemorrhagic cholecystitis is a rare condition. The presenting features may mimic nonhemorrhagic acute cholecystitis, ie, right upper abdominal quadrant pain. Hematemesis or lower GI bleeding may also occur if blood clots enter the gut.
During acute inflammation, gallbladder mucosal necrosis can result in bleeding from small vessels in the wall. Cystic artery pseudoaneurysms may also occur, resulting in hemobilia.
Ultrasound is usually the preferred diagnostic modality in the initial investigation of right upper abdominal quadrant pain. Computed tomography (CT) can help diagnose and demonstrate the characteristic findings of cholecystitis and the heterogeneous intraluminal contents.
Now, we report the case of a patient presenting with shock and hemorrhagic cholecystitis.
Case
A 51-year-old Chinese woman, who had a past medical history of end stage renal failure, parathyroidectomy, hemithyroidectomy, was admitted in June 2015 for acute abdomen and shock. Upon initial assessment, she was found to have tachycardia, borderline blood pressure, confusion and abdominal peritoneal signs.
Her white cell count was 16.1 × 103/uL (neutrophils 85.1%) and erythrocyte sedimentation rate 16 mm/h. The results of chemistry studies included a total bilirubin of 1.67 mg/dL with direct bilirubin 0.62 mg/dL, aspartate aminotransferase of 610 IU/L, alanine aminotransferase of 193 IU/L, gamma-glutamyltransferase of 275 IU/L. At presentation, her clotting profile was normal.
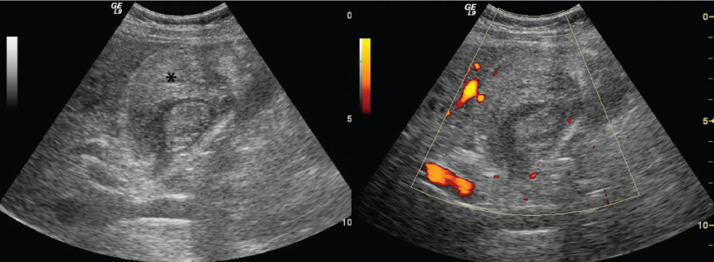
Emergency ultrasound revealed a gallbladder filled with hyperechoic substances. Gallbladder wall was thickened with hypervascularity. Sonographic Murphy's sign was positive. Low-level internal echoes were present within the ascitic fluid in the pelvis and the Morrison's pouch (Fig. 1).
Fig. 1.
Grayscale ultrasound (left) and power doppler ultrasound (right). Echogenic substances represent hemobilia (asterisk).
Immediate contrast-enhanced CT scan was performed. It confirmed hemoperitoneum and distended gallbladder filled with blood and perforation at its fundus. Active contrast extravasation was noted at its wall. Hypodense filling defects inside the gallbladder may represent polypoid growth. Overall finding could be due to acalculous cholecystitis or underlying gallbladder tumor with hemorrhage.
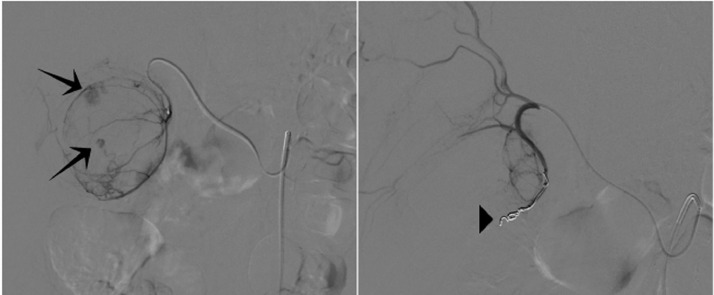
Patient was arranged for emergency embolization. With retrograde right femoral approach, SMA angiogram showed a replaced right hepatic artery from superior mesenteric artery, with active contrast extravasation from the cystic artery of the gallbladder. Celiac angiogram showed no supply to bleeders. Superselective catheterization of the cystic artery was achieved, followed by embolization using particles and coils to the main supplying branch and main cystic artery (Fig. 3).
Fig. 3.
(a) (left). Digital subtraction angiography at the origin of the proper hepatic artery demonstrates active contrast extravasation (arrows) from the cystic artery. Delayed images are not available for reference. (b) (right). Post procedural digital subtraction angiography demonstrates multiple microcoils (arrowhead) within the proximal cystic artery, with complete occlusion of the artery and nonopacification of the distal part.
In order to tide over the acute episode, our interventional radiologist offered percutaneous transhepatic cholecystostomy to the patient, using a 7Fr single-step drainage catheter with ultrasound guidance. Blood clot was removed by manual aspiration. Subsequently, the patient underwent laparotomy and cholecystostomy on the following day. Pathology report of the specimen confirmed acute on chronic inflammation with hemorrhagic necrosis and incidental note of gallbladder polyps.
Discussions
In 1979, Shah and Clegg described hemobilia caused by cholecystitis as hemorrhagic cholecystitis [1]. Common presentation was right upper quadrant pain associated with fever and leukocytosis in the majority of the reported cases [2]. The pathogenesis may be related to the transmural inflammation which led to ischemia and the gallbladder mucosal erosion, which can lead to haemobilia. Hemorrhagic cholecystitis could be triggered by multiple risk factors, such as anticoagulation, blunt trauma or gastrointestinal malignancies, such as gallbladder cancer [3,4].
Ultrasonography could help to evaluate the diagnosis as the initial step, but the atypical appearance of the condition may pose a diagnostic challenge for inexperienced ultrasonographers [5]. A CT may demonstrate high density fluid with or without layering [6]. The arterial phase of a contrast-enhanced CT may additionally demonstrate active extravasation of the contrast into the lumen of the gallbladder [7].
As in our case, active contrast extravasation was demonstrated at the gallbladder wall (Fig. 2). CBD obstruction may occur due to a blood clot during hemorrhagic cholecystitis [8]. Severe hemorrhagic cholecystitis could also induce hypovolemic shock, which is associated with high mortality rate and requires emergent resuscitation [9]. Subsequently, successful transcatheter embolization was achieved with particles and coils since the patient was unfit for surgery [10].
Fig. 2.
(a) (left). Noncontrast CT scan of the abdomen shows hemobilia. (b) (right). Contrast-enhanced arterial phase CT scan shows a bright focus (arrowhead) which refers to the site of active contrast extravasation on the lateral gallbladder wall.
After hemodynamic stabilization, for patients who are not surgical candidates, a cholecystostomy is an option. There was a report of hemorrhagic cholecystitis treated with a cholecystostomy and urokinase therapy [11]. Urgent percutaneous transhepatic cholecystostomy was undertaken in our case using a 7 Fr single-step drainage catheter with ultrasound guidance and blood clots were aspirated. It was followed by cholecystectomy on the ensuing day. In summary, hemorrhagic cholecystitis is rare but its fatal complications are not rare. The condition warrants a high index of suspicion.
Patient consent
Patient written consent was obtained before submission of this case report.
Footnotes
Acknowledgments: This paper was supported by the Hong Kong North District Hospital Department of Radiology in 2020.
Contributor Information
Max K.H. Yam, Email: ntecradiology@gmail.com.
Shiu Wah Sim, Email: ssw539@ha.org.hk.
Ka Ying Tam, Email: tky018@ha.org.hk.
Yan Lin Li, Email: lyl506@ha.org.hk.
References
- 1.Shah VR, Clegg JF. Haemorrhagic cholecystitis. Br J Surg. 1979;66:404–405. doi: 10.1002/bjs.1800660608. [DOI] [PubMed] [Google Scholar]
- 2.Morris DS, Porterfield JR, Sawyer MD. Hemorrhagic cholecystitis in an elderly patient taking aspirin and cilostazol. Case Rep Gastroenterol. 2008;2:203–207. doi: 10.1159/000135693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iki K, Inada H, Satoh M, Tsunoda T. Hemorrhagic acalculous cholecystitis associated with hemodialysis. Surgery. 2002;132(5):903. doi: 10.1067/msy.2002.127424. [DOI] [PubMed] [Google Scholar]
- 4.Kubota H, Kageoka M, Iwasaki H, Sugimoto K, Higuchi R, Honda S. A patient with undifferentiated carcinoma of gallbladder presenting with hemobilia. J Gastroenterol. 2000;35(1):63–68. doi: 10.1007/PL00009979. [DOI] [PubMed] [Google Scholar]
- 5.Chinn DH, Miller EI, Piper N. Hemorrhagic cholecystitis. Sonographic appearance and clinical presentation. J Ultrasound Med. 1987;6(6):313–317. doi: 10.7863/jum.1987.6.6.313. [DOI] [PubMed] [Google Scholar]
- 6.Tavernaraki K, Sykara A, Tavernaraki E, Chondros D, Lolis ED. Massive intraperitoneal bleeding due to hemorrhagic cholecystitis and gallbladder rupture: CT findings. Abdom Imaging. 2011;36:565–568. doi: 10.1007/s00261-010-9672-y. [DOI] [PubMed] [Google Scholar]
- 7.Pandya R, O'Malley C. Hemorrhagic cholecystitis as a complication of anticoagulant therapy: role of CT in its diagnosis. Abdom Imaging. 2008;33:652–653. doi: 10.1007/s00261-007-9358-2. [DOI] [PubMed] [Google Scholar]
- 8.Parekh J, Corvera CU. Hemorrhagic cholecystitis. Arch Surg. 2010;145:202–204. doi: 10.1001/archsurg.2009.265. [DOI] [PubMed] [Google Scholar]
- 9.Lopez V, Alconchel F. Hemorrhagic cholecystitis. Radiology. 2018;289(2):316. doi: 10.1148/radiol.2018181161. [DOI] [PubMed] [Google Scholar]
- 10.Komatsu Y., Orita H., Sakurada M., Maekawa H., Hoppo T., Sato K. Report of a case: pseudoaneurysm of the cystic artery with hemobilia treated by arterial embolization. J Med Cases, North Am. 2011;2 [Google Scholar]
- 11.Stempel LR, Vogelzang RL. Hemorrhagic cholecystitis with hemobilia: treatment with percutaneous cholecystostomy and transcatheter urokinase. J Vasc Interv Radiol. 1993;4:377–380. doi: 10.1016/s1051-0443(93)71882-5. [DOI] [PubMed] [Google Scholar]