Abstract
Hereditary factors have a strong influence on prostate cancer (PC) risk and poorer outcomes, thus stratification by genetic factors addresses a critical need for targeted PC screening and risk-adapted follow-up. In this Finnish population-based retrospective study 2283 clinically diagnosed and 455 screen-detected patients from the Finnish Randomised Study of Screening for Prostate Cancer (FinRSPC), 2400 healthy individuals have been involved. Individual genetic risk through establishment of a polygenic risk score based on 55 PC risk SNPs identified through the Finnish subset of the Collaborative Oncological Gene-Environment Study was assessed. Men with PC had significantly higher median polygenic risk score compared to the controls (6.59 vs. 3.83, P < 0.0001). The polygenic risk score above the control median was a significant predictor of PC (OR 2.13, 95% CI 1.90–2.39). The polygenic risk score predicted the risk of PC with an AUC of 0.618 (95% CI 0.60–0.63). Men in the highest polygenic risk score quartile were 2.8—fold (95% CI 2.4–3.30) more likely to develop PC compared with men in the lowest quartile. In the FinRSPC cohort, a significantly higher percentage of men had a PSA level of ≥ 4 ng/mL in polygenic risk score quartile four compared to quartile one (18.7% vs 8.3%, P < 0.00001). Adding the PRS to a PSA-only model contributed additional information in predicting PC in the FinRSPC model. Results strongly suggest that use of the polygenic risk score would facilitate the identification of men at increased risk for PC.
Subject terms: Biomarkers, Oncology, Risk factors, Urology
Introduction
Although prostate cancer (PC) remains the second most common cancer in men, biomarkers for accurate early diagnosis are missing1,2. Owing to the well-known and inherent limitations of using prostate-specific antigen (PSA), novel biomarkers to complement PSA for the prediction of PC and particularly PC with unfavourable outcomes are needed3.
Prostate cancer has a very high heritability, with an estimate of 57% (95% CI 0.51–0.63) based on the Nordic Twin Study of Cancer4, with only a few identified high-risk genes. High penetrance genes, like BRCA1/2, HOXB13, CHEK2 and MMR are important, but explain only a fraction of inherited PC risk5. In addition, the nearly 170 single nucleotide polymorphisms (SNPs) associated with PC risk in large genome-wide studies explain a quarter of the familial risk, and offer an opportunity to create a polygenic risk score (PRS) to identify the subgroups of the population at highest risk of the disease6,7. Combining a broad array of genetic data into a PRS offers an opportunity for accurate prediction of PC risk8 and allows to highlight the sharp contrast in probability of developing the disease between the highest and lowest risk groups9.
There is evidence of population stratification, i.e. differences between populations in the genetic factors contributing to familial PC risk. Previous studies have estimated PRSs mainly based on pooled data from multinational cohorts. Instead of using results from mixed European populations, we utilized population-specific PC risk loci identified from the Finnish subset from Collaborative Oncological Gene-Environment Study (iCOGS)8.
The aim of our study was to evaluate the potential of PRS to predict PC risk in advance and its application in personalized PC diagnosis. Specifically, we evaluated the accuracy of genetic risk stratification to predict overall PC, and separately for clinically diagnosed patients and screening trial cases. Moreover, the aim was to assess the ability of PRS to predict PC subgroups defined by clinical parameters such as high PSA at diagnosis, aggressive disease and advanced stage. In the Finnish Randomised Study of Screening for Prostate Cancer (FinRSPC) cohort, we evaluated the additional contribution of PRS to PSA and age.
Results
Prostate cancer risk
The median PRS in men with PC was 6.59 (interquartile range (IQR) 8.29) versus 3.83 (IQR 8.02) among cancer-free controls (p < 0.0001) (Table 1). There was no statistically significant difference in the median PRS of men with clinically detected (PRS 6.74, IQR 8.41) vs screen-detected (PRS 6.31, IQR 7.14) cancer.
Table 1.
Polygenic risk score of men predicting prostate cancer in Finland*.
| SAMPLE GROUPS | N | Mean (95% CI) | St error of mean | Median | Variance | Standard deviation |
|---|---|---|---|---|---|---|
| Study population | 5138 | 5.99 (5.83–6.16) | 0.085 | 5.01 | 37.05 | 6.09 |
| Men without prostate cancer (controls) (FinRSPC) | 2400 | 4.71 (4.47–4.94) | 0.119 | 3.83 | 33.68 | 5.80 |
| Men with prostate cancer (cases) | 2738 | 7.12 (6.89–7.35) | 0.117 | 6.59 | 37.28 | 6.11 |
| Screening trial cases (FinRSPC) | 455 | 6.65 (6.09–7.20) | 0.282 | 6.31 | 36.22 | 6.02 |
| Clinical cases (Pirkanmaa Hospital) | 2283 | 7.22 (6.97–7.47) | 0.128 | 6.74 | 37.45 | 6.12 |
*Polygenic risk score is based on 55 prostate cancer susceptibility loci.
Of all PC cases, 68.2% had a PRS above the population control’s median (3.83) (Table 2), corresponding to a sensitivity of 0.68 (95% CI 0.66–0.70) and specificity of 0.50 (0.48–0.52). The positive predictive value was 0.61 (95% CI 0.59–0.63) and positive likelihood ratio 1.36 (95% CI 1.30–1.43). Out of men with a clinically diagnosed PC, the proportion was 68.7%, while for the screening trial cases 65.9%. The odds ratio for overall PC with a PRS above the control median was 2.13 (95% CI 1.90–2.39), the corresponding OR for clinical PC was 2.18 (95% CI 1.93–2.45) and for screening trial cases was 1.92 (95% CI 1.56–2.37).
Table 2.
Evaluation of polygenic risk score to predict prostate cancer risk and associated clinical measures.
| Logistic regression | Receiver Operator Characteristics | ||||
|---|---|---|---|---|---|
| High PRS N (%) | OR (95% CI) | P value | AUC (95% CI) | P value | |
| Risk of prostate cancer: | |||||
| All prostate cancers (n = 2738) | 1868 (68.2) | 2.13 (1.90–2.39) | 5.92E-39 | 0.618 (0.60.0.63) | 4.79E-48 |
| Clinical prostate cancer cases (n = 2283) | 1568 (68.7) | 2.18 (1.93–2.45) | 1.49E-37 | 0.622 (0.61–0.64) | 4.57E-47 |
| Screening trial prostate cancer cases (n = 455) | 300 (65.9) | 1.92 (1.56–2.37) | 1.11E-9 | 0.597 (0.57–0.63) | 4.42E-11 |
| 1Risk of prostate cancer with: | |||||
| High PSA at diagnosis (> 20 ng/mL) (n = 484) | 339 (70.0) | 1.12 (0.90–0.39) | 0.300 | 0.517 (0.49–0.54) | 0.232 |
| 2Aggressive (Gleason score ≥ 8) (n = 368) | 235 (63.9) | 0.83 (0.65–1.06) | 0.140 | 0.478 (0.44–0.51) | 0.206 |
| 3Advanced stage (n = 602) | 418 (69.4) | 1.08 (0.89–1.32) | 0.425 | 0.517 (0.48–0.55) | 0.346 |
| Death by prostate cancer (n = 304) | 204 (67.1) | 0.94 (0.73–1.22) | 0.657 | 0.497 (0.46–0.53) | 0.865 |
| Tumour stage (T3-T4) (n = 540) | 369 (68.3) | 1.01 (0.81–1.25) | 0.936 | 0.512 (0.48–0.54) | 0.435 |
| Cancer in nodus (N1 stage) (n = 14) | 9 (64.3) | 0.84 (0.28–2.51) | 0.752 | 0.443 (0.30–0.58) | 0.462 |
| Metastasis (M1 stage) (n = 191) | 144 (75.4) | 1.47 (1.04–2.06) | 0.028 | 0.549 (0.51–0.59) | 0.023 |
1case only investigation; 2versus Gleason score ≤ 6; 3advanced disease stage is defined as T3-4, or N1 or M1; OR, odds ratio (polygenic risk score above median was applied as binary variable); AUC, area under the curve (polygenic risk score was used as continuous variable); statistically significant results are indicated with bold.
When divided into PRS quartiles, PC cases were distributed 18%, 25%, 27% and 30% from the lowest to the highest quartile. For the controls, the proportions showed an opposite pattern (33%, 26%, 22%, 19%, respectively). Showing that nearly a third of the PC cases belong to the highest PRS quartile, while one-third of the controls belong to the lowest PRS quartile. Men in the highest PRS quartile were of 2.8—fold (95% CI 2.40–3.30) higher risk of PC compared with men in the lowest quartile.
The overall receiver operator curve AUC of the PRS to predict PC was 0.618 (95% CI 0.60–0.63, p 4.79E-48), for clinically diagnosed PC was 0.622 (95% CI 0.61–0.64, p 4.57E-47), and for screening trial PC cases was 0.597 (95% CI 0.57–0.63, p 4.42E-11) (Table 2).
Prostate cancer clinical parameters
Of the patients with metastatic PC, 75.4% had a PRS above the control median, corresponding to an OR of 1.47 (95% CI 1.04–2.06, p 0.028, Table 2) with an AUC of 0.549 (95% CI 0.51–0.59). Although, 70.0% of the men with high PSA at diagnosis (PSA > 20 ng/mL) had a PRS above the median, no association between the PRS and high PSA at diagnosis could be identified. Similarly, there was no significant association between PRS and high Gleason score, advanced stage, tumour and nodal stage or lethal PC, possibly due to the nature of the SNPs included and low amount of cases (Table 2).
Further, there was no statistically significant association between the quartiles of the PRS and age at onset of PC (χ2 = 3.15; p = 0.369), PSA at diagnosis (χ2 = 3.58; p = 0.311), Gleason score (χ2 = 5.37; p = 0.147) or disease stage (χ2 = 1.41; P = 0.703; Supplementary Table 1).
Association with PSA in the subset of FinRSPC cohort: the FinRSPC model
When the FinRSPC cohort was divided into negative and positive PSA (PSA < 4 ng/mL vs PSA ≥ 4 ng/mL), the number of men with elevated PSA increased in each PRS quartile (Table 3, A). The association between PSA and PRS is illustrated by the fact that 8.3% of men in the lowest PRS quartile had PSA ≥ 4 ng/mL compared to 18.7% in the highest quartile (χ2 = 32.95; P < 0.00001).
Table 3.
Evaluation of polygenic risk score in prostate cancer screening in the subset of FinRSPC cohort.
| PRS | PSA < 4 ng/mL | PSA ≥ 4 ng/mL | % of men with PSA ≥ 4 ng/mL in different quartiles (p < 0.00001) | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| A) Association between quartile of polygenic risk score and PSA | |||||
| Q1 (n = 713) | 654 | 27 | 59 | 15 | 8.3% |
| Q2 (n = 711) | 623 | 25 | 88 | 22 | 12.4% |
| Q3 (n = 717) | 592 | 24 | 125 | 31 | 17.4% |
| Q4 (n = 707) | 575 | 24 | 132 | 33 | 18.7% |
| Risk factor | SIMPLE MODEL | MULTIPLE MODEL | |||
|---|---|---|---|---|---|
| OR (95% CI, p) | AUC (95% CI, p) | OR (95% CI) | AUC cumulative (95% CI, p) | ||
| B) Simple and multiple logistic regression models including PSA, age, polygenic risk score and their predictive performance to predict prostate cancer | |||||
| PSA | 6.50 (5.43–7.80, 2.61E-90) | 0.981 (0.97–0.99, 3.17E-232) | 6.60 (5.48–7.95, 8.29E-28) | 0.982 (0.97–0.99, 2.70E-232) | |
| Age | 1.04 (1.01–1.07, 0.016) | 0.557 (0.53–0.59, 0.000116) | 1.02 (0.94–1.11, 0.683) | 0.557 (0.53–0.59,0.000116) | |
| PRS | 1.06 (1.04–1.07, 1.59E-10) | 0.597 (0.57–0.63, 4.42E-11) | 1.05 (1.00–1.11, 0.038) | 0.600 (0.57–0.63, 1.80E-11) | |
P value based on χ2 test; PRS, polygenic risk score; PSA, prostate-specific antigen; Q, quartile.
OR = odds ratio; CI = confidence interval; AUC = area under the receiver operating characteristics curve; PRS, polygenic risk score; Predictive performance was assessed using the AUC for individual risk factors and for the genetic model including all risk factors. AUC cumulative denotes AUC values obtained when one risk factor at the time was added to the model from PSA only to a model including all risk factors. PSA, Age, PRS were used as continuous variables. Men aged 55–67 years at the enrollment to the FinRSPC trial.
In unadjusted logistic regression within the FinRSPC cohort, both PSA (OR 6.50, 95% CI 5.43–7.80), PRS (OR 1.06, 95% CI 1.04–1.07) and age (OR 1.04, 95% CI 1.01–1.07) predicted the risk of PC (Table 3, B). After mutual adjustment, PRS (OR 1.05, 95% CI 1.00–1.11) was still associated with PC risk, indicating that it contributed additional information beyond that provided by PSA.
Discussion
We constructed a population-specific PRS for PC and evaluated its application in genetic risk stratification. The Prs was higher among men with PC than the controls, as indicated by the median and proportion above the control median, with an odds ratio of 2.13. The AUC was 0.62, with sensitivity of 0.68. The PC risk also increased with PRS when it was divided into quartiles. The PRS was associated with metastatic disease, however, it was not associated with other indicators of poor prognosis such as high Gleason score or advanced disease. Furthermore, within the screening trial, PRS was associated with the proportion of men with positive PSA10 and contributed to detect PC.
Our finding (ROC 0.62) was comparable with previous studies, despite our use of a relatively small number of SNPs (n = 55). Previous studies using risk allele based polygenic scores have shown ROC values of 0.54–0.68 for PC11–13. However, they have provided only limited evidence that the PRS using common variants improves risk prediction8,12,13.
Genome-wide association studies (GWASs) for metastatic PC are lacking14 and few studies have investigated the association between known germline PC risk variants and metastatic disease diagnosis or development of metastasis after initial treatment14,15. All of the metastatic patients in this cohort had already been found at diagnosis due to the retrospective nature of this study. The identified association of PRS with metastatic disease at diagnosis is likely due to the inclusion of PC risk SNPs, which have earlier been found to be associated with metastatic PC risk14–16. The lack of association with other clinical variables is in line with earlier findings. Since the performance of our PRS was poorer for metastatic disease than PC overall, it offers only limited use for individual prediction of the risk of metastasis.
PSA has long been used as the primary biomarker for PC diagnosis, however, PSA screening results are frequent in false-positive results and overdiagnosis17,18. Therefore, population-based screening is not recommended19,20. In this study, we show that in the FinRSPC screening cohort the PRS quartiles are associated with elevated PSA of ≥ 4 ng/mL at diagnosis and that the PRS contributed additional information beyond PSA and age in predicting PC in the screening trial men. Performance of the PRS in screening needs an additional prospective cohort in order to test its applicability for population-based screening to supplement PSA-based stewardship in screening for PC.
The main strength of the study is that it is population-based, therefore the selection bias is minimized and the generalizability is increased. Previous studies have included mainly risk variants (OR > 1) for the construction of the PRS13. We used both risk (per allele OR > 1) and protective (per allele OR < 1) SNPs to capture genetic variation in risk more widely. Furthermore, we designed a population-specific risk score, as PC risk variants and their frequencies differ between populations21.
Naturally, the study has some limitations. In the study population there are only few PC deaths and aggressive cases. Since it is based on retrospective data, validation in a prospective setting will elevate the power and would potentially improve the study. In particular, application of the PRS in population screening needs to be conclusively evaluated in a prospective trial in order to test the PRS for clinical implications and potential benefit. Since this a Finnish population based PRS study, application in other, less homogeneous population is needed.
Our findings show that a subgroup of men at an increased risk of PC (OR > 2) can be identified based on a PRS. However, the accuracy in predicting was limited (AUC 0.62). The fact that PRS contributed additional information above PSA and age suggests that its usefulness in screening is worthwhile.
Materials and methods
All methods were carried out in accordance with relevant guidelines and regulations.
The flow diagram shown in Fig. 1 presents the steps of participant enrolment to the study (A) and selection of SNPs for PRS calculation (B).
Figure 1.
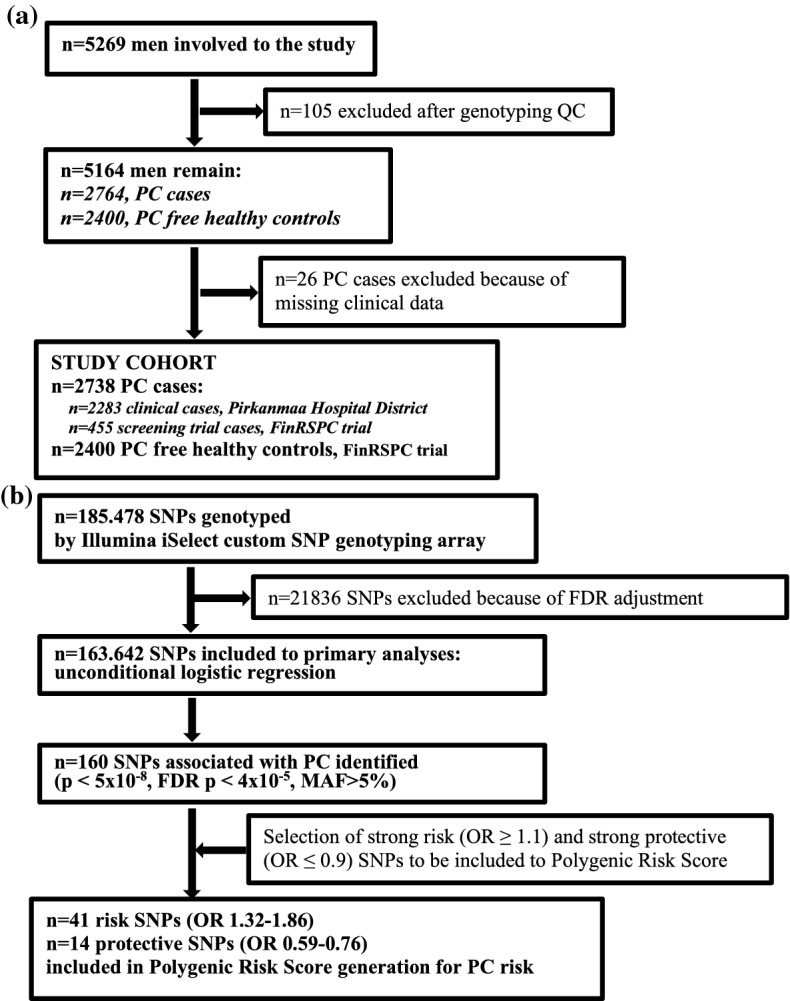
Flow diagram presenting the steps of participant's enrollment to the study (a) and selection of SNPs for polygenic risk score (b) QC, quality control; FDR, false discovery rate, corrected by Benjamini–Hochberg method.
Study participants
All genotyped PC patients and controls without PC were of Finnish origin. The study protocol was reviewed and approved by the research Ethics committee at Pirkanmaa Hospital District (tracking numbers R10167, 90,577, R03203). Permission for the use of samples was given by the National Supervisory Authority for Welfare and Health (VALVIRA). Informed consent was obtained from the participants involved in the study. Altogether, 2738 non-familial PC cases were included in the study. Of them, 2283 were clinical cases from the Pirkanmaa Hospital District, and 455 were from the Finnish Randomized Study of Screening for Prostate Cancer (FinRSPC)22, which is the largest component of the European Randomized Study of Screening for Prostate Cancer (ERSPC)23. Cancer free control subjects (n = 2400) were identified through the FinRSPC trial22. The FinRSPC trial population and the protocol population have been described in detail elsewhere24. Briefly, 80,458 men aged 55–67 years were enrolled during 1996–1999, with 32,000 randomised to the screening arm and invited to PSA-based screenings at four-year intervals.
Clinical characteristics of the genotyped PC patients, separately for clinically detected and for screening trial cases, are summarized in Table 4. PSA at diagnosis was classified as ≤ 20 versus > 20 ng/mL. Gleason score was divided into ≤ 6, 7 and ≥ 8. Stage was divided into organ-confined (T1-2, N0/x, M0/x) versus advanced disease (T3-4, or N1 or M1). PC death was defined based on the underlying cause recorded as the official cause of death by Statistics Finland.
Table 4.
Baseline clinical characteristics of non-familial prostate cancer patients.
| Clinical variables | Clinical cases (n = 2283) | Screening trial cases (n = 455) |
|---|---|---|
| Age at diagnosis | ||
| Early onset (≤ 55 y) | 103 (4.50) | 3 (0.70) |
| Late onset (> 55 y) | 2180 (95.5) | 452 (99.3) |
| Diagnostic PSA level, ng/mL | ||
| Low, ≤ 20 | 1684 (73.8) | 415 (91.2) |
| High, > 20 | 455 (19.9) | 29 (6.40) |
| Missing data | 144 (6.30) | 11 (2.40) |
| Gleason score | ||
| Low, ≤ 6 | 1033 (45.3) | 287 (63.1) |
| High, ≥ 8 | 329 (14.4) | 39 (8.60) |
| Gleason 7 | 564 (24.7) | 121 (26.6) |
| Missing data | 357 (15.6) | 8 (1.80) |
| T stage | ||
| T0/Tx | 0 (0.00) | 13 (2.90) |
| T1 | 746 (32.8) | 359 (78.9) |
| T2 | 922 (40.3) | 50 (11.0) |
| T3 | 418 (18.3) | 25 (5.50) |
| T4 | 96 (4.20) | 1 (0.20) |
| Missing data | 101 (4.40) | 7 (1.50) |
| N stage | ||
| N0/Nx | 2169 (95.0) | 447 (98.2) |
| N1 | 13 (0.60) | 1 (0.20) |
| Missing data | 101 (4.40) | 7 (1.50) |
| M stage | ||
| M0/Mx | 1999 (87.6) | 440 (96.7) |
| M1 | 183 (8.00) | 8 (1.80) |
| Missing data | 101 (4.40) | 7 (1.50) |
| PSA Progression | ||
| Progressed | 804 (35.4) | 156 (34.3) |
| Missing data | 1479 (64.8) | 299 (65.7) |
| Death | ||
| Deceased of PC | 296 (13.0) | 8 (1.76) |
| Deceased of else | 864 (37.9) | 63 (13.9) |
| Alive | 1123 (49.2) | 384 (84.4) |
Genotyping and quality control
The original genotyping was carried out by the PRACTICAL (Prostate Cancer Association group to Investigate Cancer Associated Alterations in the Genome) consortium. The genotyping outcome was obtained from the use of a custom Illumina Infinium array (iCOGS), as described previously8.
Single nucleotide polymorphism selection and statistical analyses
The Hardy–Weinberg equilibrium was ensured by checking that the proportion of each genotype obtained was in agreement with the expectation calculated from the allele frequencies. Statistical analyses were performed with IBM SPSS version 25 (SPSS Inc., Chicago, USA) unless otherwise specified. For each SNP, allelic ORs for PC with 95% confidence intervals were computed using logistic regression. A total of 55 variants shown to be associated with PC in the Finnish subset from iCOGS (Supplementary Table 2) were chosen for the calculation of the PRS based on the selection criteria described in Fig. 1. In short, selected SNPs were associated with PC at a genome-wide significance level (p < 5 × 10–8) and had the effect size of OR > 1.1 for risk SNPs and OR < 0.9 for protective SNPs.
We assessed the PRS of men with and without PC, and also separately for clinically diagnosed and screening trial cases. Sensitivity and specificity of the PRS were calculated. The use of the control median as the cut-off-point showed a near-optimal sensitivity and specificity. Therefore, the study participants were divided into those with a polygenic risk below and above the control median, which represents men free of PC. The odds ratio for PC risk prediction relating to the PRS above median was evaluated by logistic regression with PC as the outcome. We evaluated the predictive performance of PRS by calculating the area under the curve (AUC) of the receiver operator characteristic (ROC). Evaluation of the discriminative potential of the PRS for subsets of cases with high PSA at diagnosis, high Gleason score, advanced stage, local and distant progression, and PC death was performed with the same methodology.
In order to evaluate the possible implications of the PRS in the screening trial, we evaluated the additional contribution of PRS quartiles incremental to PSA and age in predicting PC in the FinRSPC cohort. Logistic regression models including PSA, age and the PRS were applied to assess PC prediction and the AUC calculated. All reported p values are two-sided.
Polygenic risk score calculation
A PRS for each individual was calculated by summing the number of risk alleles25 at each of the 55 SNPs multiplied by the logarithm of the SNP’s OR as follows:
where βi is the per-allele log-odds ratio for locus i, xij represents the number of risk alleles (i.e., 0, 1 or 2) carried by an individual j at locus i, and n is the number of loci. The risk conferred by each of the variants is assumed to be allele dose-dependent with a multiplicative (log-additive) effect on a relative risk scale6. Under the multiplicative model, the distribution of polygenic risk in the population follows the normal distribution, when relative risk is plotted on a logarithmic scale, with mean, μ, and variance σ2. We set the mean, μ = −σ2/2, so that the mean relative risk in the population is equal to unity. Log-transformation of non-normally distributed PRS data was applied.
Supplementary information
Acknowledgements
The authors thank the patients who participated in this study. Liisa Määttänen is thanked for assistance related to FinRSPC screening trial samples. Tero Vahlberg’s help is acknowledged for his advice in biostatistics. FinRSPC Study Group members are acknowledged for the FinRSPC cohort: Ulf-Håkan Stenman, Faculty of Medicine, University of Helsinki, Finland and Department of Clinical Chemistry, Helsinki University Hospital, Helsinki, Finland; Paula Kujala, Department of Pathology, Fimlab Laboratories, Tampere, Finland. We thank Dr. Samuel Heron for language check. This work was financially supported by the Academy of Finland (#310105 to JS, #123054 and #260931 to AA), the Sigrid Juselius Foundation (to JS), Cancer Foundation Finland sr (to JS), Cancer Foundation Finland sr (Movember grant for prostate cancer research to AA) and State Research Funding (VTR) Tampere University Hospital (grants # 9E089, 9F100, 9G096, 9H099, 9L085, 9N064 and 9R002 TLJT). We thank the members from the Prostate Cancer Association Group to Investigate Cancer Associated Alterations in the Genome (PRACTICAL) consortium who are provided in the Supplement/footnotes. Information of the consortium can be found at https://practical.icr.ac.uk/. This study would not have been possible without the contributions of the following: Per Hall (COGS); Douglas F. Easton, Paul Pharoah, Kyriaki Michailidou, Manjeet K. Bolla, Qin Wang (BCAC), Andrew Berchuck (OCAC), Rosalind A. Eeles, Douglas F. Easton, Ali Amin Al Olama, Zsofia Kote-Jarai, Sara Benlloch (PRACTICAL), Georgia Chenevix-Trench, Antonis Antoniou, Lesley McGuffog, Fergus Couch and Ken Offit (CIMBA), Joe Dennis, Alison M. Dunning, Andrew Lee, and Ed Dicks, Craig Luccarini and the staff of the Centre for Genetic Epidemiology Laboratory, Javier Benitez, Anna Gonzalez-Neira and the staff of the CNIO genotyping unit, Jacques Simard and Daniel C. Tessier, Francois Bacot, Daniel Vincent, Sylvie LaBoissière and Frederic Robidoux and the staff of the McGill University and Génome Québec Innovation Centre, Stig E. Bojesen, Sune F. Nielsen, Borge G. Nordestgaard, and the staff of the Copenhagen DNA laboratory, and Julie M. Cunningham, Sharon A. Windebank, Christopher A. Hilker, Jeffrey Meyer and the staff of Mayo Clinic Genotyping Core Facility. Funding for the iCOGS infrastructure came from: the European Community’s Seventh Framework Programme under grant agreement n° 223175 (HEALTH-F2-2009-223175) (COGS), Cancer Research UK (C1287/A10118, C1287/A 10710, C12292/A11174, C1281/A12014, C5047/A8384, C5047/A15007, C5047/A10692, C8197/A16565), the National Institutes of Health (CA128978) and Post-Cancer GWAS initiative (1U19 CA148537, 1U19 CA148065 and 1U19 CA148112—the GAME-ON initiative), the Department of Defence (W81XWH-10-1-0341), the Canadian Institutes of Health Research (CIHR) for the CIHR Team in Familial Risks of Breast Cancer, Komen Foundation for the Cure, the Breast Cancer Research Foundation, and the Ovarian Cancer Research Fund.
Author contributions
CS: study plan adjustment, data acquisition, statistical analyses, tables, figure and explanation text preparation, literature assembly, manuscript writing, final approval of the manuscript. KT: data acquisition, final approval of the manuscript. TLJT: study plan, final approval of manuscript. KT: study plan, final approval of manuscript. AA: statistical input, approval of the analyses, interpretation of results, manuscript writing, final approval of the manuscript. JS: concept, study plan preparation, interpretation of results, manuscript writing and correcting, final approval of manuscript, correspondence.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Anssi Auvinen and Johanna Schleutker.
Supplementary information
is available for this paper at 10.1038/s41598-020-74172-z.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J. Clin. 2019;69:7–34. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 2.Bray F, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 3.Fantus RJ, Helfand BT. Germline genetics of prostate cancer: Time to incorporate genetics into early detection tools. Clin. Chem. 2019;65:74–79. doi: 10.1373/clinchem.2018.286658. [DOI] [PubMed] [Google Scholar]
- 4.Mucci LA, et al. familial risk and heritability of cancer among twins in Nordic countries. JAMA. 2016;315:68–76. doi: 10.1001/jama.2015.17703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stadler ZK, Schrader KA, Vijai J, Robson ME, Offit K. Cancer genomics and inherited risk. J. Clin. Oncol. 2014;32:687–698. doi: 10.1200/JCO.2013.49.7271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pharoah PD, et al. Polygenic susceptibility to breast cancer and implications for prevention. Nat. Genet. 2002;31:33–36. doi: 10.1038/ng853. [DOI] [PubMed] [Google Scholar]
- 7.Schumacher FR, et al. Association analyses of more than 140,000 men identify 63 new prostate cancer susceptibility loci. Nat. Genet. 2018;50:928–936. doi: 10.1038/s41588-018-0142-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eeles RA, et al. Identification of 23 new prostate cancer susceptibility loci using the iCOGS custom genotyping array. Nat. Genet. 2013;45:385–391, 91e381-382. doi: 10.1038/ng.2560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burton H, et al. Public health implications from COGS and potential for risk stratification and screening. Nat. Genet. 2013;45:349–351. doi: 10.1038/ng.2582. [DOI] [PubMed] [Google Scholar]
- 10.Helfand BT, et al. Associations of prostate cancer risk variants with disease aggressiveness: Results of the NCI-SPORE Genetics Working Group analysis of 18,343 cases. Hum. Genet. 2015;134:439–450. doi: 10.1007/s00439-015-1534-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grönberg H, et al. Prostate cancer screening in men aged 50–69 years (STHLM3): A prospective population-based diagnostic study. Lancet Oncol. 2015 doi: 10.1016/S1470-2045(15)00361-7. [DOI] [PubMed] [Google Scholar]
- 12.Machiela MJ, et al. Evaluation of polygenic risk scores for predicting breast and prostate cancer risk. Genet. Epidemiol. 2011;35:506–514. doi: 10.1002/gepi.20600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aly M, et al. Polygenic risk score improves prostate cancer risk prediction: results from the Stockholm-1 cohort study. Eur. Urol. 2011;60:21–28. doi: 10.1016/j.eururo.2011.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahn J, et al. Prostate cancer predisposition loci and risk of metastatic disease and prostate cancer recurrence. Clin. Cancer Res. 2011;17:1075–1081. doi: 10.1158/1078-0432.CCR-10-0881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gallagher DJ, et al. Susceptibility loci associated with prostate cancer progression and mortality. Clin. Cancer Res. 2010;16:2819–2832. doi: 10.1158/1078-0432.CCR-10-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thomas G, et al. Multiple loci identified in a genome-wide association study of prostate cancer. Nat. Genet. 2008;40:310–315. doi: 10.1038/ng.91. [DOI] [PubMed] [Google Scholar]
- 17.Fenton JJ, et al. Prostate-specific antigen-based screening for prostate cancer: Evidence report and systematic review for the US preventive services task force. JAMA. 2018;319:1914–1931. doi: 10.1001/jama.2018.3712. [DOI] [PubMed] [Google Scholar]
- 18.Ilic D, et al. Prostate cancer screening with prostate-specific antigen (PSA) test: A systematic review and meta-analysis. BMJ. 2018;362:k3519. doi: 10.1136/bmj.k3519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martin RM, et al. Effect of a Low-Intensity PSA-Based Screening Intervention on Prostate Cancer Mortality: The CAP Randomized Clinical Trial. JAMA. 2018;319:883–895. doi: 10.1001/jama.2018.0154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hayes JH, Barry MJ. Screening for prostate cancer with the prostate-specific antigen test: A review of current evidence. JAMA. 2014;311:1143–1149. doi: 10.1001/jama.2014.2085. [DOI] [PubMed] [Google Scholar]
- 21.Virlogeux V, Graff RE, Hoffmann TJ, Witte JS. Replication and heritability of prostate cancer risk variants: Impact of population-specific factors. Cancer Epidemiol. Biomark. Prev. 2015;24:938–943. doi: 10.1158/1055-9965.EPI-14-1372. [DOI] [PubMed] [Google Scholar]
- 22.Schröder FH, et al. Screening and prostate-cancer mortality in a randomized European study. N. Engl. J. Med. 2009;360:1320–1328. doi: 10.1056/NEJMoa0810084. [DOI] [PubMed] [Google Scholar]
- 23.Schröder FH, et al. Screening and prostate cancer mortality: Results of the European Randomised Study of Screening for Prostate Cancer (ERSPC) at 13 years of follow-up. Lancet. 2014;384:2027–2035. doi: 10.1016/S0140-6736(14)60525-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Finne P, et al. The Finnish trial of prostate cancer screening: Where are we now? BJU Int. 2003;92(Suppl 2):22–26. doi: 10.1111/j.1465-5101.2003.04397.x. [DOI] [PubMed] [Google Scholar]
- 25.Kiyotani K, et al. Association of genetic polymorphisms in SLCO1B3 and ABCC2 with docetaxel-induced leukopenia. Cancer Sci. 2008;99:967–972. doi: 10.1111/j.1349-7006.2008.00765.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


