Abstract
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is a pandemic and a public health emergency. The overwhelming increase in the number of cases has brought significant challenges to health care systems worldwide. Patients with end-stage kidney disease are highly vulnerable with the multiple comorbid conditions that make them susceptible to adverse outcomes with COVID-19. More than 2 million people worldwide receive maintenance hemodialysis at outpatient centers. Effectively preventing the spread of infection among hemodialysis centers, health care personnel, and patients is essential to ensure the continued delivery of dialysis to patients with end-stage kidney disease. This article discusses dialysis patients’ care during COVID-19, addressing measures for patient and health care personnel protection and care of dialysis patients with suspected or confirmed COVID-19.
Index Words: Hemodialysis, COVID-19, peritoneal dialysis, outpatient dialysis units
Editorial, p. 675
Coronavirus disease 2019 (COVID-19) is a respiratory illness that started in Wuhan, China, and has now spread to more than 150 countries, including the United States.1 As of July 14, the total number of confirmed COVID-19 cases has reached 13,145,302 worldwide.2 Patients with COVID-19 usually present with fever (44%-98%), cough (68%-76%), myalgia (18%), and fatigue (18%).3 The overwhelming increase in the number of cases has challenged health care systems all over the world. The estimated case fatality risk for COVID-19 ranges from 0.25% to 3%,4 with risks higher in those with preexisting comorbid conditions: 10.5% for cardiovascular disease, 7.3% for diabetes, 6.3% for chronic respiratory disease, 6.0% for hypertension, and 5.6% for cancer.5
In 2016, nearly 125,000 people in the United States were initiated on kidney replacement therapy (KRT) for end-stage kidney disease, with more than 726,000 receiving dialysis or living with a kidney transplant.6 Dialysis patients receive KRT through various modalities, including in-center hemodialysis (HD), peritoneal dialysis, and home HD. In the United States, 62.7% of patients with end-stage kidney disease receive HD as their KRT modality, with 98% of them receiving treatments in outpatient centers. Patients on KRT have multiple comorbid conditions, such as diabetes, hypertension, and cardiovascular disease, which are risk factors for adverse outcomes in COVID-19. In addition, patients on KRT who are infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) usually present with atypical symptoms, making it a diagnostic challenge.7 The second patient who died from COVID-19 in the United States was an outpatient HD patient from the Seattle area.8,9 The experiences of frontline nephrologists caring for dialysis patients in Seattle and New York have been described recently.9,10
Scope of the Problem
SARS-CoV-2 spreads from person to person through droplets expelled during coughing and sneezing.1 Transmission through direct contact and fecal contamination can also occur.1 Recent reports show that aerosol transmission is also possible.11 Patients receiving HD are a particularly unique and vulnerable population in the COVID-19 pandemic. HD patients cannot practice social distancing because they receive HD treatments routinely at least 3 times a week at outpatient dialysis units. Each session requires traveling to and from the outpatient group and inevitable exposures to health care personnel and all the patients concurrently receiving treatment in a particular session. At any given shift, more than 20 patients can be treated.
To continue providing usual care for these patients, a framework to protect patients and health care personnel from contracting and spreading COVID-19 needs to be in place. In response to this, the American Society of Nephrology, together with the Centers for Disease Control and Prevention (CDC), established a COVID-19 response team. This response team has laid out guidelines for all HD facilities to follow, especially in caring for patients under investigation and patients infected with COVID-19. In this review, we discuss the best practices on how to care for patients with known or suspected COVID-19 in the outpatient HD setting, how to protect patients and health care personnel from disease exposure using personal protective equipment (PPE), and how to approach a patient receiving HD with confirmed COVID-19.
Measures for Patient Protection
Patients with COVID-19 can be asymptomatic or symptomatic 2 to 14 days after exposure.1 In the setting of COVID-19, HD facilities need to provide instructions for preventative measures to include proper hygiene and handwashing techniques, coughing and sneezing etiquette, and practice of social distancing to all patients. Each patient should be instructed to inform the HD unit if they had traveled to COVID-19 endemic areas or had contact with persons found to be positive for SARS-CoV-2. On arrival, patients should be screened for signs and symptoms of respiratory infections before entering the outpatient unit. In a recent perspective from Wuhan, China, HD patients were screened for viral pneumonia using computed tomography of the chest to augment the limited sensitivity and relatively slower turnaround time of SARS-CoV-2 polymerase chain reaction testing.12
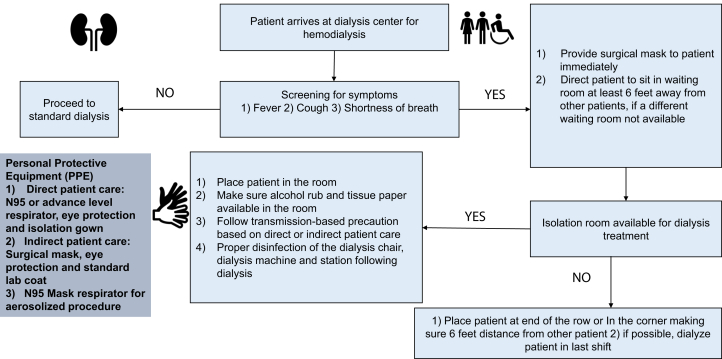
If possible, all patients with suspected or confirmed COVID-19 should travel in private vehicles and not in shared rides. Mandatory signs and directions should be clearly shown in the outpatient dialysis units. Educational pamphlets about CDC dialysis guidelines and COVID-19 should be kept at the front desk for patients and visitors. Patients with symptoms should wear masks while in the dialysis facility and should be seated at least 6 feet away from other patients and health care personnel. If available, a different seating room for patients with suspected or confirmed SARS-CoV-2 infection is preferred. If patients with symptoms are medically stable, they should only present to the dialysis center at the time of their shift to minimize time within the HD facility. All supplies such as alcohol hand rubs, tissue paper, and masks should be available in the triage and waiting areas. Clear communication among the unit health care personnel, medical director, and state health department is vital to stay updated with the evolving guidelines for COVID-19. Figure 1 shows the algorithm for screening patients and delivery of dialysis.
Figure 1.
Algorithm for screening patients and delivery of dialysis.
Measures for Health Care Personnel Protection
Health care personnel are at the front lines caring for HD patients with suspected or confirmed COVID-19. Protecting health care personnel from contracting this infection is of prime importance. Although guidelines for PPE may vary across different institutions, all health care personnel in outpatient HD units should wear a surgical mask for their shifts. All outpatient and inpatient HD facilities should offer nonpunitive and flexible sick leave to their employees, consistent with current public health policies that mandate ill health care personnel to stay home. As with dialysis patients, health care personnel should practice proper hand hygiene techniques.
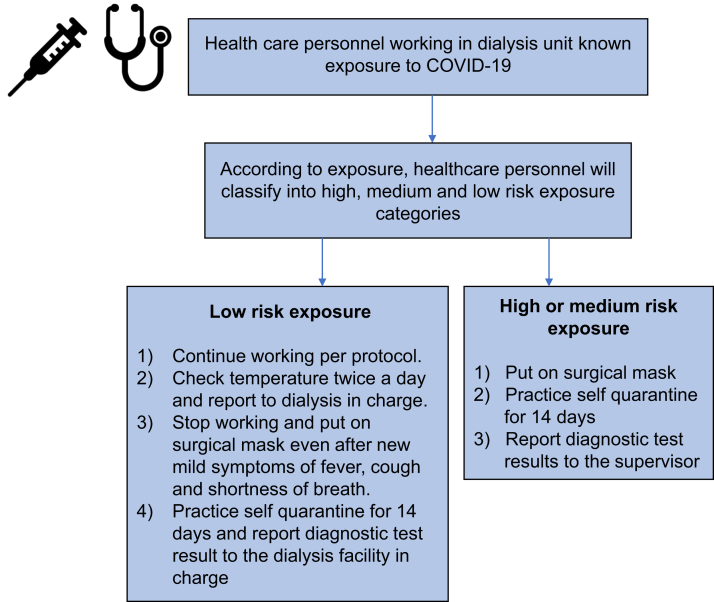
After a known exposure, health care personnel should inform their supervisor and should stop working if symptomatic. If asymptomatic, the next course of action would depend on the type of exposure as determined by CDC or relevant national guidelines.13 High-risk exposure is defined as having prolonged close contact with COVID-19–infected patients with the health care personnel not wearing PPE, with nose and mouth exposed to droplets potentially carrying the virus. Medium-risk exposure is defined as having prolonged close contact with COVID-19–infected patients while wearing a face mask while the nose and mouth were potentially exposed to material that may contain the virus. Low-risk exposure is defined as having brief interactions with patients with COVID-19 or prolonged close contact with patients wearing a face mask for source control while the health care personnel was wearing a face mask or respirator.
Health care personnel deemed to be high or medium risk will be instructed to self-quarantine for 14 days. Health care personnel considered to have had low-risk exposure can continue to work and self-monitor for symptoms, including twice-a-day temperature checks, with instructions to stop working if fever or respiratory symptoms develop. The health care personnel should then self-quarantine and subsequently update the dialysis facility about disease course.
Figure 2 illustrates an algorithm for health care personnel after a positive exposure. The symptoms-based strategy and test-based strategy should be used for directing discontinuation of home isolation for health care personnel. A person with symptoms and positive COVID-19 should discontinue home isolation after the resolution of fever without the use of fever-reducing medications, improvement in respiratory symptoms, and subsequent negative results of a molecular assay for COVID-19 from at least 2 consecutive nasopharyngeal swab specimens collected 24 or more hours apart.14 A person without symptoms and positive COVID-19 should discontinue home isolation when at least 7 days have passed since the date of their first positive COVID-19 diagnostic test and have had no subsequent illness.14
Figure 2.
Algorithm for health care personnel screening. Abbreviation: COVID-19, coronavirus disease 2019.
Strategies for PPE Conservation and Use
PPE conservation and use are integral parts of health care delivery in times of COVID-19. PPE, which includes surgical mask, eye goggles, face shield, N95 respirator mask, and isolation gown, is critical for all health care personnel safety. Guidance for PPE practice varies across countries and specified units within the country. Universally, all guidelines have advised using surgical masks for patients and health care personnel. In the United States, using N95 is advised for care of COVID-19–infected dialysis patients. Variation in PPE practice across units is dependent on the availability of resources and specific guidelines adopted by the units. All dialysis facilities should provide health care personnel required education and training about using PPE and proper technique of donning and doffing of the PPE. All dialysis facilities should keep an updated PPE inventory. The administration should keep track of all PPE use and future needs. The administration should be communicating with local, public, and federal health offices on the need for additional supplies. Standard droplet and contact precautions should be applied when caring for suspected or confirmed COVID-19–infected patients. Isolation gowns, N95 masks or high-level respirator (or facemask, if respirator is not available), and eye protection should be used for direct patient care within 6 feet of COVID-19–positive patients. For procedures mostly on inpatient HD patients, when there is the risk for aerosolization, N95 respirator masks should be used with eye protection and isolation gowns. For nondirect care of patients, only a surgical mask, standard laboratory coat, and eye protection are required. Physician encounters for home dialysis patients should be transitioned to telemedicine if possible to reduce further contact and exposure. Similarly, reducing physical examination during inpatient rounds on COVID-19–infected patients, cohorting patients, and restricting visitors to the patient rooms are essential to minimize exposure and conserve PPE.
Dialyzing Patients with COVID-19
Patients with suspected or confirmed COVID-19 should be dialyzed in a separate isolation room. Hepatitis B isolation rooms should be used first with patients with positive hepatitis B antigen and then can be used for isolation of patients with COVID-19. If the isolation room is not available, patients should dialyze during the last shift and at the end of a row or in a corner at least 6 feet away from other patients. If there is more than 1 suspected or confirmed COVID-19–infected patient at a dialysis center, all such patients should receive dialysis during the last dialysis shift. The same health care personnel staff should dialyze patients with suspected or confirmed COVID-19 to avoid cross-contamination and infection. In dire circumstances of HD nursing staff shortage, a fast credentialing and accreditation for nurses should be in place. All dialysis machines, dialysis stations, and chairs should be disinfected per protocol. Telemedicine should be used for physicians’ visits when applicable.
All dialysis patients, mainly in inpatient sites, should be instructed to have strict potassium and fluid restriction to avoid the need for added treatment sessions.15
If there is a surge of outpatient HD patients with COVID-19, a dedicated unit for them could help minimize exposure to the uninfected HD population and associated health care personnel. All physicians at one particular city should be credentialed at all outpatient dialysis centers. Further, facilitating the sharing of workload during the time of the surge is essential. The dialysis staff should be trained to do diagnostic testing in the outpatient dialysis facilities. Proper technique of taking nasopharyngeal swab specimens should be instructed. The testing of these patients in the outpatient dialysis center, if possible, will prevent added patient load in the emergency department at hospitals. Patients should be told and educated about practicing self-quarantine at home and family members after dialysis. Family members should also monitor them for symptoms.
For patients with COVID-19 and patients under investigation admitted to hospitals getting inpatient HD, similar guidelines should be followed in delivering dialysis. All dialysis catheter placement procedures should be done using eye protection, isolation gowns, and N95 masks. The symptoms-based strategy and test-based strategy should be used for directing discontinuation of transmission-based isolation for the patient. For a patient with symptoms and positive COVID-19, transmission-based isolation should discontinue after the resolution of fever without fever-reducing medications and improvement in respiratory symptoms and negative results of a molecular assay for COVID-19 from at least 2 consecutive nasopharyngeal swab specimens collected 24 or more hours apart as test-based strategy.16 Per non–test-based strategy transmission-based protocol, the isolation should discontinue when at least 3 days have passed since recovery, defined as resolution of respiratory symptoms, and at least 7 days have passed since symptoms first appeared.16 Box 114,16 shows guidance for discontinuing home isolation for health care personnel and transmission-based protocol for patients.
Box 1. Guidance for Discontinuing Home Isolation for Health Care Professionals and Transmission-Based Protocol for Patients.
Test-based strategy a
-
•
Resolution of fever without the use of fever-reducing medications and
-
•
Improvement in respiratory symptoms (eg, cough, shortness of breath) and
-
•
Negative results of a US Food and Drug Administration Emergency Use Authorized molecular assay for coronavirus disease 2019 from at least 2 consecutive nasopharyngeal swab specimens collected ≥24 hours apart.
Symptoms-based strategy
-
•
At least 3 days (72 hours) have passed since recovery, defined as resolution of fever without the use of fever-reducing medications and improvement in respiratory symptoms (eg, cough, shortness of breath), and
-
•
At least 7 days have passed since symptoms first appeared.
aTest-based strategy is only used for health care personnel, when there are adequate resources for test available.
When these patients are ready to discharge from the hospitals, appropriate planning and allocation to the outpatient dialysis unit should be done. Isolation should be maintained at home if the patient gets discharged before the removal of the transmission-based protocol. If a patient is discharged to a long-term care facility or assisted living facility before discontinuing the transmission-based protocol, it should continue at the discharge facility. If a patient is discharged to a long-term care or assisted-care facility following stop of transmission-based protocol and still has symptoms, he or she should be kept in an isolation room wearing a mask all day for a total of 14 days after onset of illness or resolution of symptoms.16
Both primary teams and nephrologists need to be aware of the importance of appropriate discharge planning for this vulnerable patient population. If discharge occurs before removing transmission-based precautions, the patient would be expected to maintain social distancing at home for the remaining time. Arrangements should be made regarding where the patient would continue outpatient dialysis sessions, usually in COVID-19–designated facilities, if available. Excellent communication with outpatient units is essential to ensure the patient’s smooth transition to receiving their regular treatments on discharge. If a patient were to be discharged to a long-term care or assisted living facility, the facility must provide regular dialysis treatments. Contact precautions should be in place in the facility if the patient were to continue the rest of transmission-based precautions. When the precautions are lifted but the patient remains symptomatic, the patient must be kept in an isolation room while wearing a mask for a total duration of 14 days after the onset of illness or on the resolution of symptoms.
Clinical Data
Table 117, 18, 19, 20, 21 shows clinical outcomes data of clinical studies in HD patients with COVID-19.
Table 1.
Clinical Studies in HD Patients With COVID-19
| Study | No. of HD Patients | COVID-19–Positive Patients | Mortality Rate of COVID-19–Infected Patients |
|---|---|---|---|
| UK Renal Registry17 | 22,431 | 2,414 (10.7%) | 625 (25.8%) |
| Corbett et al18 | 1,530 | 300 (19.6%) | 61 (20.3%) |
| Alberici et al19 | 643 | 94 (14.6%) | 24 (25.5%) |
| Fisher et al20 | 900 | 114 (12.6%) | 32 (28.07%) |
| Xiong et al21 | 7,154 | 154 (2.2%) | 41 (26.6%) |
Abbreviations: COVID-19, coronavirus disease 2019; HD, hemodialysis.
Consideration for Peritoneal Dialysis and Home HD
Peritoneal dialysis and home HD patients can also be affected by COVID-19, though there is limited information related to this. Because both these groups of patients can complete their KRT at home, this minimizes risks of exposure and allows them to practice social distancing. It is vital to prevent any interruptions with the delivery of supplies to those receiving home dialysis treatments.
KRT Initiation
More than 100,000 Americans have been initiated on KRT annually since 2002. In standard practice, preparing patients for KRT initiation requires months of lead time, to include education on KRT modalities, frequent outpatient nephrology visits for medication titration, appointments with respective surgical subspecialties for access evaluation, necessary imaging, surgery for access creation, and ample time to allow for access to mature. Because nonurgent outpatient visits are deferred and elective surgeries and procedures are being cancelled during the pandemic, it is essential to highlight that patients with chronic kidney disease stage 5 nearing KRT are an extremely vulnerable group. On March 26, 2020, the Centers for Medicare & Medicaid Services announced that access creation for patients with end-stage kidney disease remains an essential procedure.22 In reality, these necessary procedures may still experience delays when resources become scarce in the setting of the pandemic. It is necessary to recognize that although resource allocation will be challenging, crash-start dialysis or unprepared dialysis is associated with poorer outcomes, higher mortality, and a significantly negative socioeconomic impact.
Effect of COVID-19 Pandemic on Dialysis Facilities and Patients
The COVID-19 pandemic has resulted in a strain on both dialysis facilities and patients. Dialysis facilities may have to arrange different dialysis shifts for patients under investigation. Dialysis facilities also must ensure staff availability to deliver dialysis to regular patients and COVID-19–infected patients. Transportation for patients can also be a challenge because many patients are dependent on public transit to dialysis facilities. There is substantial psychological stress on patients and dialysis staff during this pandemic. Patients are fearful for their own and others’ well-being, especially because their care makes social distancing difficult. Dialysis staff are also concerned about contracting the infection and being under constant responsibility to deliver dialysis to COVID-19–infected patients safely.
Conclusion
There is a scarcity of real-world data regarding HD patients and COVID-19. The atypical presentation and higher risks for transmission and mortality warrant specific protocols for caring for dialysis patients with COVID-19. In this time of a public health emergency, it is essential to prevent transmission and use evidence-based medicine in caring for dialysis patients to avoid any interruption in their usual care.
Article Information
Authors’ Full Names and Academic Degrees
Ashish Verma, MB, BS, Ankit B. Patel, MD, PhD, Maria Clarissa Tio, MD, and Sushrut S. Waikar, MD, MPH.
Support
None.
Financial Disclosure
The authors declare that they have no relevant financial interests.
Peer Review
Received April 21, 2020. Evaluated by 1 external peer reviewer, with direct editorial input from an Associate Editor, who served as Acting Editor-in-Chief. Accepted in revised form July 21, 2020. The involvement of an Acting Editor-in-Chief was to comply with Kidney Medicine’s procedures for potential conflicts of interest for editors, described in the Information for Authors & Journal Policies.
Footnotes
Complete author and article information provided before references.
Contributor Information
Ashish Verma, Email: averma8@bwh.harvard.edu.
Sushrut S. Waikar, Email: swaikar@bu.edu.
References
- 1.US Centers for Disease Control and Prevention Coronavirus disease 2019 (COVID-19): situation summary. Vol 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/index.html
- 2.Johns Hopkins Coronavirus Resource Center. Vol 20202020. https://coronavirus.jhu.edu/map.html
- 3.Guan W.J., Ni Z.Y., Hu Y., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nick W., Amanda K., Lucy Telfar B., Michael G.B. Case-fatality risk estimates for COVID-19 calculated by using a lag time for fatality. Emerg Infect Dis J. 2020;26(6):1339–1441. doi: 10.3201/eid2606.200320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention Chronic Kidney Disease Surveillance System website. Vol 20202019. https://www.cdc.gov/kidneydisease/index.html
- 7.Tang B., Li S., Xiong Y., et al. COVID-19 pneumonia in a hemodialysis patient. Kidney Med. 2020;2(3):354–358. doi: 10.1016/j.xkme.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dialysis should continue despite COVID-19; CDC gives guidance. Vol 20202020. https://www.medscape.com/viewarticle/926720
- 9.Watnick S., McNamara E. On the frontline of the COVID-19 outbreak. CJASN. 2020;15(5):710–713. doi: 10.2215/CJN.03540320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mokrzycki M.H., Coco M. Management of hemodialysis patients with suspected or confirmed COVID-19 infection: perspective of two nephrologists in the United States. Kidney360. 2020;1(4):273–278. doi: 10.34067/KID.0001452020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Doremalen N., Bushmaker T., Morris D.H., et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li J., Xu G. Lessons from the experience in Wuhan to reduce risk of COVID-19 infection in patients undergoing long-term hemodialysis. Clin J Am Soc Nephrol. 2020;15(5):717–719. doi: 10.2215/CJN.03420320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Interim U.S. Guidance for Risk Assessment and Public Health Management of Healthcare Personnel with Potential Exposure in a Healthcare Setting to Patients with Coronavirus Disease (COVID-19). Vol 20202020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html
- 14.Discontinuation of Home Isolation for Persons with COVID-19 (Interim Guidance). Vol 20202020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-in-home-patients.html
- 15.Meyer T.W., Hostetter T.H., Watnick S. Twice-weekly hemodialysis is an option for many patients in times of dialysis unit stress. J Am Soc Nephrol. 2020;31(6):1141–1142. doi: 10.1681/ASN.2020030361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Discontinuation of Transmission-Based Precautions and Disposition of Patients with COVID-19 in Healthcare Settings (Interim Guidance). Vol 20202020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-hospitalized-patients.html
- 17.COVID-19 surveillance report for renal centres in the UK. Vol 20202020. https://renal.org/covid-19/data/
- 18.Corbett R.W., Blakey S., Nitsch D., et al. Epidemiology of COVID-19 in an urban dialysis center. J Am Soc Nephrol. 2020;31(8):1815–1823. doi: 10.1681/ASN.2020040534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alberici F., Delbarba E., Manenti C., et al. A report from the Brescia Renal COVID Task Force on the clinical characteristics and short-term outcome of hemodialysis patients with SARS-CoV-2 infection. Kidney Int. 2020;98(1):20–26. doi: 10.1016/j.kint.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fisher M., Yunes M., Mokrzycki M.H., Golestaneh L., Alahiri E., Coco M. Chronic hemodialysis patients hospitalized with COVID-19: short-term outcomes in the Bronx, New York. Kidney360. 2020;1(8):755–762. doi: 10.34067/KID.0003672020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xiong F., Tang H., Liu L., et al. Clinical characteristics of and medical interventions for COVID-19 in hemodialysis patients in Wuhan, China. J Am Soc Nephrol. 2020;31(7):1387–1397. doi: 10.1681/ASN.2020030354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.End Stage Renal Disease (ESRD) Facilities: CMS Flexibilities to Fight COVID-19. Vol 20202020. https://www.cms.gov/files/document/covid-19-esrd-facilities.pdf