Abstract
Background and Aims.
Heavy drinking is associated with increased risk of incident HIV infection among men who have sex with men (MSM). Past studies suggest that this association may be due to the tendency for intoxication to interfere with condom use. However, research on potential causal mechanisms explaining this relationship has been limited primarily to laboratory studies. In this study, we tested several potential mediators of the relationship between alcohol use level and HIV-risk behavior.
Design.
Ecological momentary assessment (EMA) methods conducted over a 30-day period.
Setting and participants/Cases.
MSM (N = 100) in the Northeastern US.
Measurements.
Participants completed daily diary surveys and up to six experience sampling surveys randomly prompted throughout the day.
Findings.
Very heavy levels of drinking (12+ drinks) increased the odds of engaging in any sex (OR=1.87, p < .001). Coefficient products and 95% confidence intervals indicated that both subjective sexual arousal (OR=1.52, p < .001) and sex intentions (OR=1.74, p < .001) significantly mediated the association between very heavy drinking and the odds of sex. When participants reported sex, the odds of engaging in high-risk condomless anal sex (CAS) increased incrementally after drinking heavily (5–11 drinks; OR = 3.27, p = .006) and very heavily (12+ drinks; OR = 4.42, p < .001). Only subjective sexual arousal significantly mediated the association between alcohol use level and high-risk CAS (OR=1.16, p = .040).
Conclusions.
Increases in subjective sexual arousal after drinking heavily appear to partly account for alcohol-related HIV-risk behaviors in the daily lives of men who have sex with men. Alcohol’s role in strengthening motivationally-consistent emotional states may therefore play a more important role in facilitating alcohol-involved HIV-risk than explicit sexual motivation.
Keywords: HIV-risk behavior, sexual risk behavior, alcohol use, gay and bisexual men, EMA, mechanisms
Introduction
In the United States (US), new HIV infections continue to increase among certain subgroups of men who have sex with men (MSM), particularly young MSM (aged 18–35), despite stability or decline among other at-risk groups (1–3). High-risk sex accounts for nearly all new infections among MSM, specifically insertive and receptive anal sex without using a prevention method (4). Although pre-exposure prophylaxis (PrEP) uptake is increasing (5, 6) condoms remain the most widely accessible and frequently used form of HIV prevention (7, 8).
Heavy drinking is associated with increased risk of incident HIV infection among MSM (9, 10). Research suggests this is mostly due to the tendency for intoxication to reduce condom use (11, 12). Laboratory-based alcohol administration studies have shown that MSM endorse higher intentions to engage in condomless anal sex (CAS) and communicate less effectively with partners in hypothetical sexual situations when intoxicated (13, 14). Men who are intoxicated may experience more subjective sexual arousal when in sexual situations, and that this may lead them to forego condom use (15). Although laboratory-based studies have produced important findings that point to potential mediators of alcohol’s effects on condom use, their use of hypothetical scenarios is a key limitation. Identifying real-world mechanisms of alcohol-involved HIV risk behavior can inform more specific interventions that help MSM increase their awareness of these effects and take steps to plan for them.
In this study, we used ecological momentary assessment (EMA) methods among high-risk MSM in the Northeastern US to test whether alcohol use increases the odds of engaging in (1) any sex and/or (2) high-risk condomless anal sex (CAS), as well as (3) several potential mechanisms of these effects. Participants completed daily diaries (DD) and up to six experience sampling (ES) surveys each day on their smartphones for 30 days. Proposed mediators were drawn both from the literature specific to HIV-risk behavior, as well as more general health behavior theories. For example, several past experimental and longitudinal studies have suggested that emotional processes, like sexual arousal but also general positive and negative affect, may be involved in increasing HIV-risk behavior in MSM (13, 16, 17). The theory of planned behavior also proposes that constructs like intentions, perceived control, attitudes, and norms may be key determinants of HIV-risk behavior (18), and past studies have supported the role of these constructs in predicting condom use, at least at the between-subjects level and in other populations (19, 20). Identifying which of these factors are involved in HIV-risk behavior could inform targets for intervention (21). In parallel multiple mediator models, we tested whether changes in these factors accompanying alcohol use accounted for alcohol’s role in increasing HIV-risk behavior.
Methods
Participants (N = 100) were recruited from social media sites (e.g., Facebook, Instagram), gay-oriented dating apps (e.g., Grindr, Scruff), and in-person outreach (e.g., flyers) from January 2016 to October 2018. Eligible participants were (1) 18+ years old, (2) assigned male sex at birth, (3) currently male gender, (4) HIV-negative or unknown, (5) not currently prescribed or taking PrEP, (6) reported CAS with a non-sexually-exclusive male partner in the past 30 days, and (7) had consumed five or more drinks on a single occasion at least once in the past 30 days. Exclusions were (1) currently receiving counseling/medications for alcohol/drug problems, (2) serious mental illness (e.g., schizophrenia), or (3) injection drug use in the past three months.
Procedures
Participants were screened for eligibility online and met with staff either in-person or via videoconference to enroll. Staff obtained informed consent, reviewed procedures, and provided guidance downloading survey software (MetricWire, Inc.) to participants’ smartphones. Staff thoroughly trained participants in using the app, explained each survey, and walked through a typical study day. For each of 30 days, participants completed (1) a self-initiated DD survey upon waking, and (2) up to six ES surveys, randomly prompted from 9 a.m. to midnight. Participants were coached to achieve response rates of 100% of DD and >80% of ES surveys. Staff sent feedback about participants’ response rates every week and provided coaching when they fell below targets. Participants earned $2 for each DD and $0.50 for each ES, plus a bonus of $10 for every 10 days rates were above targets for both survey types (for a total possible of $185). Procedures were approved by Brown University’s IRB.
Measures
Daily diary surveys.
DDs assessed sexual behavior, alcohol use, and drug use over the past 24 hours. To assess sexual behavior, participants reported the number of partners they had oral, anal, or vaginal sex with (up to 4). For each, they reported various partner characteristics (e.g., HIV status, sexual exclusivity), what time sex occurred, which sex acts they engaged in, and whether they used a condom for each act. Two primary outcomes were: (1) Whether that day (or “day-period,” in the case of multiple sex events at different times in a given day) involved any sex (versus none), and (2) whether participants engaged in condomless anal sex (insertive or receptive) that day with a ‘high risk’ partner. High risk partners were partners who (a) were not on PrEP, (b) were not mutually sexually exclusive with the participant, or (c) were mutually sexually exclusive, but were of unknown HIV status. The reference group for high risk CAS compared these events to sex events that did not meet these conditions (i.e., sex that involved less risk, like oral sex only, condom-protected anal sex, and CAS with a lower risk partner). Alcohol use was assessed by asking participants to report the number of standard drinks they had (12 oz. beer, 5 oz. wine, 1 oz. liquor), the number of hours they drank, and when they started drinking. Drug use was assessed by selecting which types of drugs they used (e.g., marijuana, cocaine, methamphetamine, prescription painkillers, sedatives, or stimulants).
Experience sampling surveys.
Participants also reported on their alcohol use in ES surveys, recording how many standard drinks they had consumed since the last ES survey. They also rated their current affect using item subsets from the Positive and Negative Affect Scales – Extended Form (PANAS-X; 22), on a 0 (not at all) to 4 (extremely) scale. Positive affect was assessed with three items: happy, enthusiastic, and excited. Negative affect was assessed with four: sad, afraid, hostile, and nervous. Items were chosen given their use in alcohol EMA studies (23–25). Sexual arousal was assessed with the question “How horny are you right now?”, rated similarly. Other potential mediators of alcohol effects on sexual behavior were assessed using single items, each rated on similar 0–4 scales, including intentions for sex and condom use (“how likely are you to…”), perceived behavioral control (“how difficult would it be to use a condom if you wanted to?”), attitudes (“using condoms would be…good/bad”), and norms (“how important do the people you’re around right now think it is to use condoms…”)(20).
Data Analysis Plan
First, we created an ordinal variable that reflected categories of cumulative alcohol use level at the moment-level based on the number of drinks reported on successive ES surveys (0=No drinking, 1=1–4 drinks, 2=5–11 drinks, 3=12+ drinks). These categories align with guidelines from the National Institute on Alcohol Abuse and Alcoholism suggesting that men who consume five or more drinks on a given occasion are at higher risk for alcohol-related problems (26). The “very heavy drinking” category aligns with research showing that, for men with high average levels of consumption (i.e., 2–4 drinks per day), drinking 12+ drinks on a given day confers additional risk for problems compared to drinking 5+ drinks (27). This approach is consistent with similar past studies of alcohol and HIV-risk (28, 29). Since participants reported the number of drinks consumed since the last ES assessment, when participants reported drinking on adjacent ES assessments in a given day, the total number of drinks reported on these adjacent surveys were summed to represent the total drinking amount during that episode. Surveys separated by a report of no drinking were unchanged. Although ES data on alcohol use were missing on 8.1% of days that were likely drinking days (as determined by participants’ DD responses the next day), alcohol data on these days were left as missing to maintain temporality. ES surveys collected after sex events occurred were dropped (6.2% of all ES surveys) to ensure that alcohol use and mediators preceded sex events in time. Only 2.9% of these post-sex-event ES surveys involved new drinking events.
On days when multiple sex events were reported at different times (15.6% of all sex events), we separated the day into ‘day-periods,’ in which all ES assessments collected before each sex event that day, but after any preceding sex events, were nested within each day-period. (see Figure 1). We then estimated three-level multilevel parallel multiple mediator models for logistic outcomes (30) using methods described by Preacher et al. (31, 32). Before estimating the full models, we first tested direct effects between alcohol use level and each outcome. Since some similar past studies have suggested that the effects of alcohol use level on sex and risk among MSM may not be fully linear across similar categories (28), we first tested the effects of each category (versus no drinking) on the outcomes. If their effects appeared to be approximately linear, the ordinal variable reflecting alcohol use level was used in the full model for that outcome. Otherwise, specific alcohol use categories that showed direct effects on the outcome were used in the final model. This approach is the same as that used in previous studies on alcohol use and HIV-risk behavior (28, 29) and can help preserve parameters in final models, when supported.
Figure 1. Timeline of study surveys collected and our approach to nesting experience sampling surveys within days or periods prior to sex.
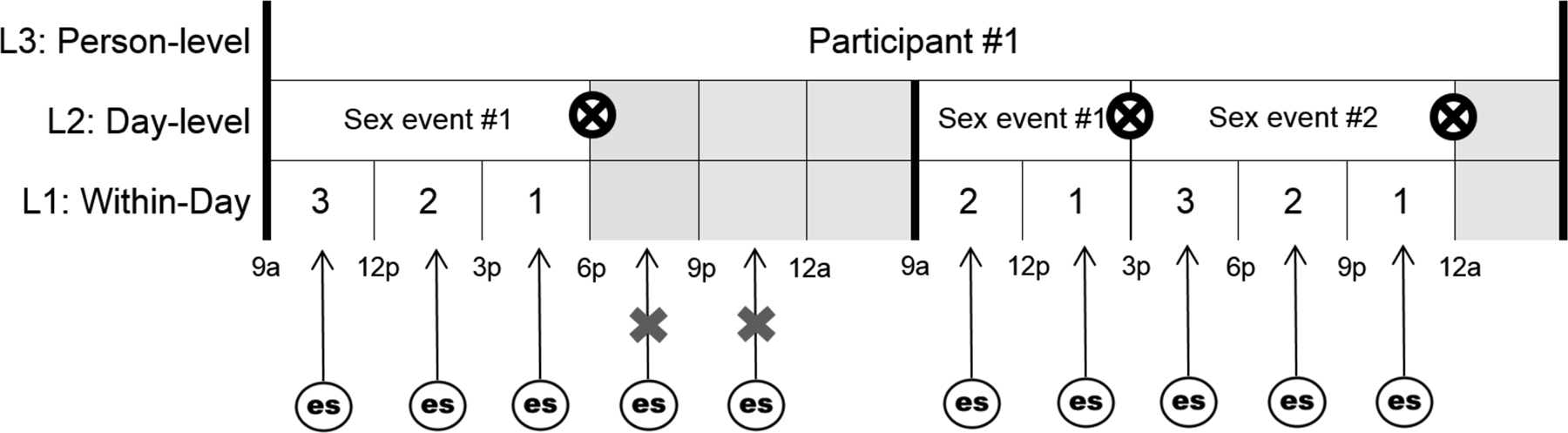
Note. ES = Experience sampling survey. ⊗Represents the time at which a sex event occurred. Numbers on the within-day level represent experience sampling surveys collected containing data about participants’ current alcohol use level. Greyed cells and “x” symbols represent experience samples that would be dropped in our approach, if they were non-missing.
Since both alcohol use level and all mediators were measured at the within-day-level and sex outcomes were measured at the day-level, we used procedures for testing 1-1-2 mediation in full models (i.e., Level 1 = Within-day surveys that assessed both independent and mediating variables [ES], Level 2 = Day/period surveys assessing outcome variables [DD], Level 3 = Participants [Empty]; 32) using a maximum likelihood estimator. Each model specified alcohol as the focal predictor and day-level marijuana and stimulant use as covariates, with relationships between these predictors and sexual behavior outcomes occurring both directly and indirectly through eight possible mediators. We used coefficient products and 95% CIs to test indirect effects, as bootstrapping methods for generating bias-corrected CIs were not yet available for three-level models. Given evidence that ignored interactions between the exposure variable and mediators can result in biased indirect effects (33), we also tested all possible exposure-mediator interactions. However, no interaction terms were statistically significant, so we omitted these terms from final models. Analyses were conducted in Mplus version 8.3 (Muthén & Muthén, 2019), and α < .05. These analyses were not pre-registered in a publicly available trial registry, and should therefore be considered exploratory.
Results
Response Rates and Descriptive Statistics
Participants (N = 100, see Table 1) provided an average of 28.6 days of data (2,793 total days) and completed an average of 97.3% of all DD surveys (SD = .06) and 77.3% of all prompted ES surveys (SD = .13). Participants reported a total of 1,113 drinking events, 18.9% of which involved heavy drinking (5–11 drinks) and 3.5% of which involved very heavy drinking (VHD; 12+ drinks). They reported 622 total sex events, 61.9% of which involved anal sex. Of these, 70.3% occurred without a condom. Seventy-four percent of all anal sex events, and 69.6% of all CAS events, occurred with partners characterized as “high-risk.” See Table 2 for correlation matrix of key covariates.
TABLE 1.
Demographic Characteristics and Key Variables (N = 100)
| Characteristics | Mean (SD) or N (%) |
|---|---|
| Age (Range: 18 – 54) | 27.1 (7.7) |
| Race | |
| White | 76 (76.0) |
| Black or African American | 4 (4.0) |
| Asian | 8 (8.0) |
| American Indian/Alaska Native | 1 (1.0) |
| Multiracial | 6 (6.0) |
| Chose not to respond | 5 (5.0) |
| Ethnicity (Hispanic or Latino) | 16 (16.0) |
| HIV-status (self-reported) | |
| Negative | 83 (83.0) |
| Don’t know | 17 (17.0) |
| Currently in sexually-exclusive relationship | 5 (5.0) |
| Avg. length of relationship (in months) | 1.4 (0.9) |
| College degree | 54 (54.0) |
| Low income1 | 29 (29.0) |
| Unemployed | 13 (13.0) |
| Identify as gay or bisexual | 94 (94.0) |
| Avg. # total EMA days completed | 29.3 (1.6) |
Note.
Represents those with a household annual income <$30,000/year.
TABLE 2.
Bivariate correlation matrix
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Alcohol use level1 | -- | |||||||||
| 2. Stimulant drug use | 0.07* | -- | ||||||||
| 3. Marijuana use | 0.07* | 0.10* | -- | |||||||
| 4. Subjective sexual arousal | 0.08* | 0.04* | 0.01 | -- | ||||||
| 5. Positive affect | 0.16* | 0.02* | 0.05* | 0.28* | -- | |||||
| 6. Negative affect | −0.01 | −0.01 | 0.09* | 0.07* | −0.17* | -- | ||||
| 7. Anal sex intentions2 | 0.04* | 0.05* | 0.15* | 0.39* | 0.30* | −0.03* | -- | |||
| 8. Condom use intentions2 | −0.02 | −0.02 | 0.02* | −0.09* | −0.03* | 0.05* | −0.09* | -- | ||
| 9. Perceived control of condom use3 | 0.01 | 0.07* | 0.05* | −0.01 | 0.01 | 0.18* | 0.03* | −0.05* | -- | |
| 10. Condom attitudes4 | 0.03* | −0.07* | 0.07* | −0.08* | −0.01 | 0.02 | −0.05* | 0.75* | −0.13* | -- |
| 11. Condom use norms5 | 0.03* | 0.02 | 0.02* | −0.02* | 0.01 | −0.01 | −0.03* | 0.50* | 0.01 | 0.63* |
Note.
Alcohol use level was coded 1 = consumed 1–4 drinks at a given point in an episode, 2 = 5–11 drinks, and 3 = 12+ drinks.
Intentions were assessed by asking “how likely” participants were to engage in the behavior in the near future.
Percieved behavioral control was assessed by asking “how difficult it would be” for participants to use condoms if they were to have sex in the near future.
Condom attitudes were assessed by asking whether “using a condom during anal sex would be…[0] very bad to [4] very good.”
Condom use norms were assessed by asking “how important” they thought “those [they were] around right now think it is to use condoms if [they] were to have anal sex.”
Mechanisms of Alcohol-Involved Sex
In initial models testing the direct effects alcohol/drug use, only VHD increased the odds of engaging in sex (OR=1.87, p<.001). However, the odds of sex were not significantly different after participants either drank moderately (1–4 drinks; OR=0.94, p=.420) or heavily (5–11 drinks; OR=1.07, p=.360) versus periods in which participants did not drink. As such, only the effects of VHD, compared to all other levels of drinking (including none), were included in the final model for this outcome. Odds of any sex occurring were 40% higher on days/periods during which marijuana had been used (OR= 1.40, p<.001) and 162% higher when stimulants had been used (OR=2.62, p<.001). Figure 2 and Table 3 show results of the full model that explored mediators of VHD’s effects on engaging in any sex. Results showed participants reported significantly higher levels of subjective sexual arousal (OR=1.90, p<.001) and positive affect (OR= 2.31, p<.001) when drinking very heavily, as well as greater sex intentions (OR= 1.96, p<.001). Both subjective sexual arousal (OR= 1.93, p<.001) and sex intentions (OR=2.23, p<.001) were also significantly positively associated with ultimately engaging in sex. Surprisingly, negative affect was also positively associated with engaging in sex (OR= 1.34, p=.040). There was no evidence that condom use intentions, perceived control of condom use, condom attitudes, or condom use norms were significantly different when VHD occurred versus when it did not (condom attitudes and norms were both omitted from Figures 2 and 3, as a result). However, the effects of very VHD on engaging in any sex were substantially mediated by subjective sexual arousal (OR= 1.52, p<.001) and anal sex intentions (OR= 1.74, p<.001). These results show that the predicted increase in sexual arousal associated with VHD, compared to less drinking or non-drinking, resulted in a 52% increase in the odds of engaging in any sex beyond the direct effect of VHD. Similarly, the predicted increase in sex intentions associated with VHD resulted in a 74% increase in the odds of engaging in any sex beyond the direct effect of VHD.
Figure 2. Three-level logistic regression model of any sex event.
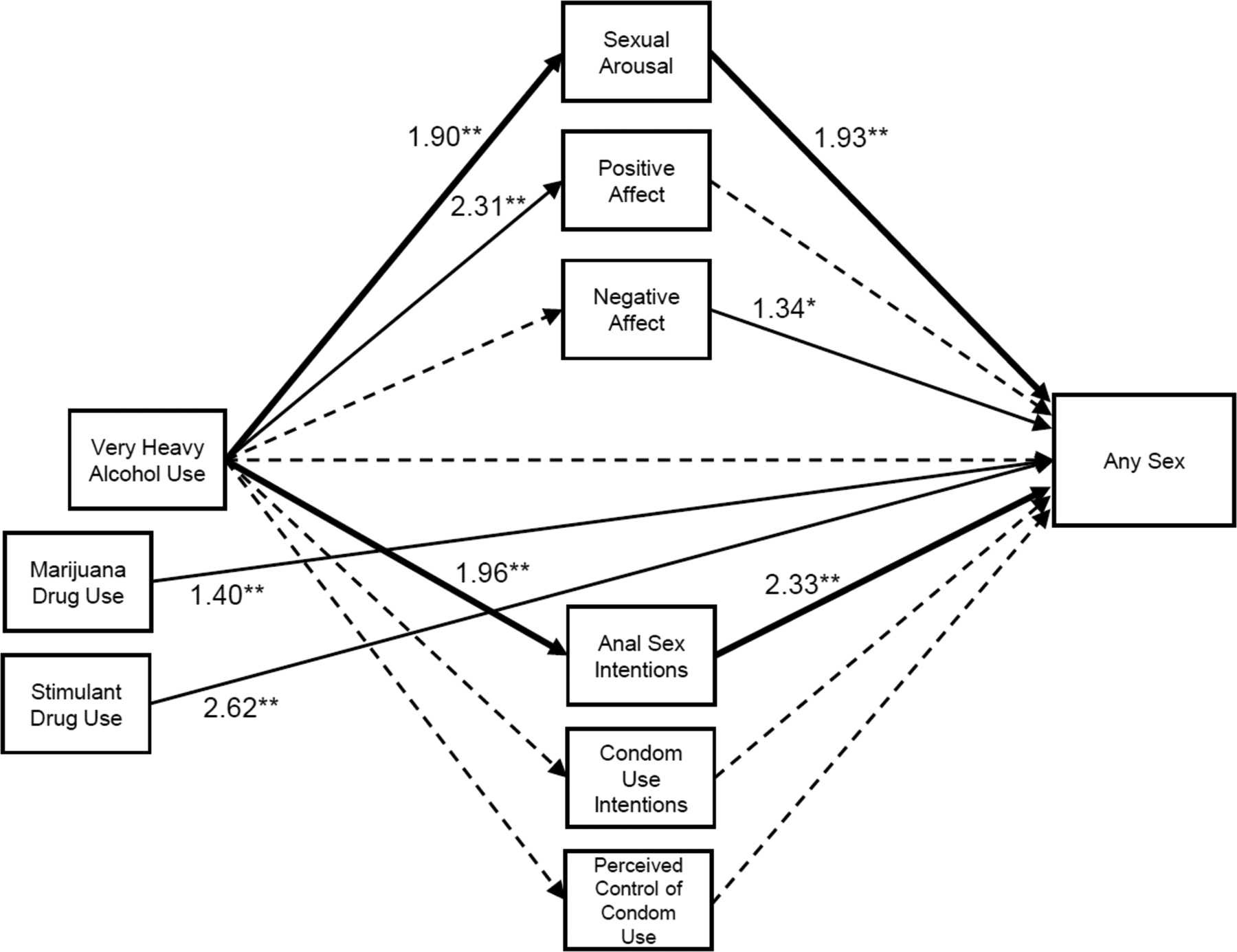
Note. *p < .05, **p < .001. Path coefficients are shown in odds ratios. Very heavy alcohol use refers to episodes involving ≥ 12 drinks. Condom use attitudes and norms are omitted as they were not significantly associated with either alcohol use level or the outcomes.
TABLE 3.
Model results
| Variable | High-Risk CAS1 | |||||||
|---|---|---|---|---|---|---|---|---|
| SE | p | 95% CI | OR | SE | p | 95% CI | ||
| Direct effects only models2 | ||||||||
| Moderate alcohol use (1–4 drinks)3 | 0.94 | 0.21 | .420 | 0.53–1.27 | 0.87 | 0.09 | .407 | 0.43–3.04 |
| Heavy alcohol use (5–11 drinks)3 | 1.07 | 0.18 | .360 | 0.65–1.34 | 3.27 | 0.72 | .006 | 1.53–6.61 |
| Very heavy alcohol use (12+ drinks)3 | 1.87 | 0.72 | <.001 | 1.02–3.27 | 4.42 | 1.07 | <.001 | 1.87–16.21 |
| Alcohol use level (linear)3 | -- | -- | -- | -- | 2.35 | 0.76 | <.001 | 1.30–2.45 |
| Marijuana use | 1.40 | 0.16 | <.001 | 1.18–1.67 | 1.18 | 0.37 | .292 | 0.73–1.89 |
| Stimulant drug use | 2.62 | 0.60 | <.001 | 1.82–3.67 | 0.46 | 0.25 | .047 | 0.22–0.98 |
| Alcohol use level → mediators4 | ||||||||
| Subjective sexual arousal | 1.90 | 0.26 | <.001 | 1.52–2.35 | 1.49 | 0.09 | <.001 | 1.35–1.65 |
| Positive affect | 2.31 | 0.29 | <.001 | 1.84–2.85 | 1.83 | 0.09 | <.001 | 1.67–1.98 |
| Negative affect | 0.94 | 0.08 | .210 | 0.82–1.08 | 0.86 | 0.03 | <.001 | 0.82–0.91 |
| Sex intentions | 1.96 | 0.32 | <.001 | 1.56–2.52 | 1.55 | 0.11 | <.001 | 1.38–1.73 |
| Condom use intentions | 0.95 | 0.13 | .355 | 0.77–1.20 | 0.98 | 0.05 | .349 | 0.89–1.07 |
| Perceived control of condom use | 0.99 | 0.09 | .460 | 0.85–1.13 | 1.04 | 0.04 | .149 | 0.98–1.10 |
| Condom attitudes | 1.02 | 0.12 | .480 | 0.83–1.20 | 0.99 | 0.04 | .398 | 0.92–1.06 |
| Condom use norms | 0.90 | 0.08 | .125 | 0.76–1.06 | 0.95 | 0.03 | .070 | 0.90–1.01 |
| Mediators → outcome5 | ||||||||
| Subjective sexual arousal | 1.93 | 0.04 | <.001 | 1.61–2.54 | 1.46 | 0.34 | .040 | 1.02–2.13 |
| Positive affect | 1.08 | 0.04 | .180 | 0.95–1.35 | 0.99 | 0.30 | .483 | 0.65–1.63 |
| Negative affect | 1.34 | 0.04 | .040 | 1.02–1.87 | 1.46 | 0.84 | .190 | 0.77–3.23 |
| Sex intentions | 2.33 | 0.04 | <.001 | 1.97–2.65 | 0.93 | 0.14 | .309 | 0.71–1.17 |
| Condom use intentions | 1.15 | 0.05 | .122 | 0.98–1.22 | 0.76 | 0.23 | .165 | 0.49–1.22 |
| Perceived control of condom use | 0.59 | 0.05 | .055 | 0.36–1.01 | 0.56 | 0.37 | .162 | 0.25–1.39 |
| Condom attitudes | 1.04 | 0.05 | .370 | 0.82–1.48 | 1.03 | 0.35 | .457 | 0.62–1.76 |
| Condom use norms | 1.23 | 0.04 | .185 | 0.81–1.67 | 0.80 | 0.47 | .322 | 0.35–1.83 |
| Indirect effects6 | ||||||||
| Alcohol use → Sexual arousal | 1.52 | 0.20 | <.001 | 1.28–1.90 | 1.16 | 0.11 | .040 | 1.02–1.37 |
| Alcohol use → Positive affect | 1.07 | 0.11 | .180 | 0.96–1.29 | 0.99 | 0.17 | .483 | 0.77–1.34 |
| Alcohol use → Negative affect | 0.99 | 0.03 | .250 | 0.92–1.02 | 0.95 | 0.06 | .190 | 0.83–1.04 |
| Alcohol use → Sex intentions | 1.74 | 0.26 | <.001 | 1.41–2.30 | 0.97 | 0.06 | .309 | 0.86–1.07 |
| Alcohol use → Condom intentions | 1.03 | 0.07 | .355 | 0.91–1.15 | 1.00 | 0.02 | .399 | 0.97–1.04 |
| Alcohol use → Perceived control | 1.00 | 0.05 | .475 | 0.92–1.08 | 0.99 | 0.03 | .270 | 0.93–1.02 |
| Alcohol use → Condom attitudes | 1.00 | 0.02 | .480 | 0.97–1.03 | 1.00 | 0.01 | .490 | 0.98–1.02 |
| Alcohol use → Condom norms | 0.99 | 0.04 | .300 | 0.92–1.03 | 1.00 | 0.03 | .353 | 0.96–1.07 |
Reference group = condom-protected anal sex / oral sex alone with any partner, or condomless anal sex with a non-exclusive or unknown HIV status partner.
Tests the direct effects of alcohol and drug use categories on any sex and high-risk CAS.
Reference group = no drinking. In the Any Sex model, alcohol use level reflected very heavy levels of drinking (12+) versus all other levels of drinking or no drinking, while in the high-risk CAS model, alcohol use level reflected a three-category ordinal variable reflecting heavy (5–11 drinks) and very heavy drinking (12+ drinks) compared to more moderate drinking (1–4 drinks) or no drinking.
Shows the direct effects of alcohol and drug use categories on each of the proposed mediators (e.g., sexual arousal, positive affect, etc.).
Shows the direct effects of each of the proposed mediators (e.g., sexual arousal, positive affect, etc.) on any sex and high-risk CAS.
Shows the indirect effects of alcohol use categories on any sex and high-risk CAS through each of the proposed mediators (e.g., sexual arousal, positive affect, etc.).
Figure 3. Three-level logistic regression model of sex events that involved high-risk CAS.
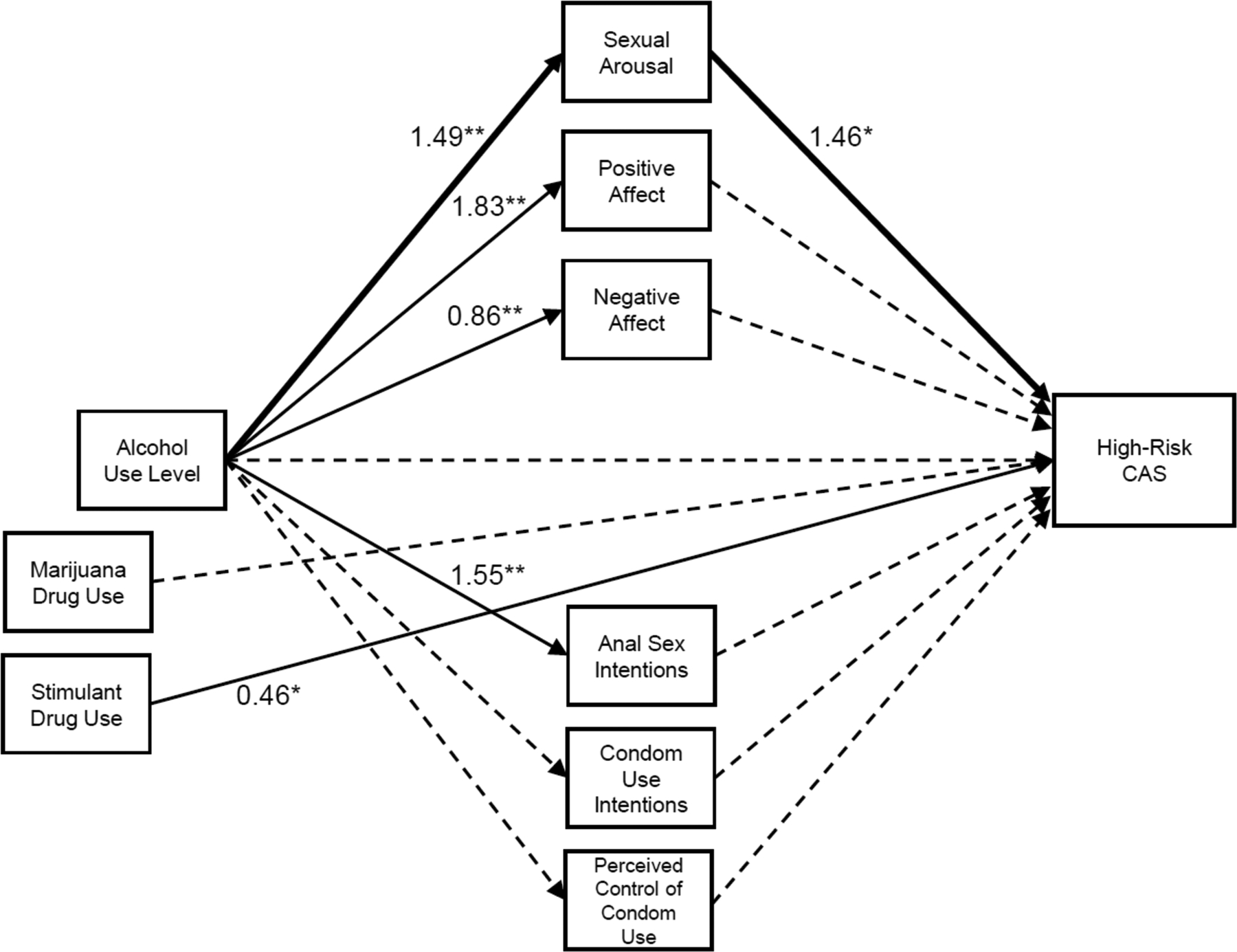
Note. *p < .05, **p < .001. Path coefficients are shown in odds ratios. Alcohol use level is an ordinal variable reflecting heavy drinking (1; 5–11 drinks), and very heavy drinking (2; 12+ drinks), versus moderate drinking (0; 1–4 drinks) and no drinking (0). Condom use attitudes and norms are omitted as they were not significantly associated with either alcohol use level or the outcomes.
Mechanisms of Alcohol-Involved HIV-Risk
In the initial model, the odds that participants would engage in high-risk CAS during a sex event were 227% higher when they drank heavily beforehand (5–11 drinks; OR=3.27, p=.006) and 342% higher when they drank very heavily (12+ drinks; OR=4.42, p<001), compared to no drinking. However, the odds of high-risk CAS occurring were not significantly different after participants drank moderately (1–4 drinks; OR=0.87, p=.407). Given that these results are consistent with past studies that suggest HIV-risk behavior among MSM begins to increase primarily above 5–6 drinks (12, 28), we used a linear variable for alcohol use level in the full model that ranged from no or moderate drinking (0) to heavy drinking (1) to VHD (2). There was no evidence that the odds of engaging in high-risk CAS were different on days/periods when participants used marijuana (OR=1.18, p=.292), but surprisingly, the odds of high-risk CAS were 117% lower when participants had used stimulant drugs during that same day-period than when they did not (OR= 0.46, p=.047). Similar to the previous model (see Figure 3), on day-periods when participants reported having sex, greater alcohol use level was associated with increased positive affect (OR= 1.83, p<.001) and subjective sexual arousal (OR= 1.49, p<.001), and decreased negative affect (OR= , p<.001). Alcohol use level prior to sex was also associated with an increase in anal sex intentions (OR= 1.55, p<.001). However, only participants’ level of subjective sexual arousal was associated with having high-risk CAS relative to other types of sex (OR= 1.46, p=.040). The effects of alcohol on high-risk CAS were significantly mediated by subjective sexual arousal (OR= 1.16, p=.040), such that the predicted increase in sexual arousal associated with each increased level of alcohol use, compared to moderate or non-drinking, resulted in a 16% increase in the odds of engaging in high-risk CAS during a sex event, beyond the direct effects of alcohol use. Although this indirect effect accounted for 62% of the total effect of alcohol use level on high-risk CAS, it only partially mediated alcohol’s direct effects (direct effect of alcohol use level with mediation: OR=2.31, SE=1.08, p=.045, 95% CI: 1.02 – 4.50).
Discussion
In this study, we used EMA to collect data about the timing of both drinking and sex events and assessed potential mediators of this relationship in near real-time, allowing us to test causal hypotheses about mechanisms of alcohol’s effects on sexual decision-making in the daily lives of MSM. By focusing on these within-persons associations, we were also able to test whether the same participant engaged in sex and risk more often after drinking than not drinking. Consistent with other studies (12, 28, 34), our initial models showed that alcohol use level was associated with an increased odds of engaging in sex, and when participants had sex, an increased odds that sex would involve high-risk CAS. Specifically, MSM were significantly more likely to engage in sex after VHD (12+ drinks during a single drinking episode) when compared to more moderate levels of drinking and/or no drinking, and when participants had sex, alcohol use levels of 5+ drinks resulted in incrementally increased odds that they would engage in high-risk CAS. These findings go beyond past event-level studies to show that alcohol use preceding sex events increases HIV-risk behavior among MSM in the real world, as opposed to simply showing that these two behaviors co-occur around the same timeframe. In contrast to many past event-level studies (12, 28), our findings suggest that although stimulant use was associated with engaging in sex, it was negatively associated with engaging in high-risk CAS when participants reported sex. Although this may reflect random variation in this effect specific to our sample, participants may have opted for safer sex when engaging in sex specifically with high-risk partners, perhaps reflecting planned episodes of stimulant drug use and sex.
In the model exploring mechanisms of alcohol-involved sex, increases in both subjective sexual arousal and sex intentions when drinking very heavily (12+ drinks) accounted for most of the tendency for VHD to lead to sex. Although it is perhaps unsurprising that emotional states fundamental to motivating sexual behavior, like subjective sexual arousal, ultimately lead to sexual behavior (35), past studies of alcohol’s effects on sexual arousal have produced somewhat inconsistent results (35–37). However, the vast majority of studies have been conducted in lab settings using hypothetical sexual situations and have focused on populations other than MSM (35). Our results advance this literature by showing both that participants report higher subjective arousal while drinking and that this increase partly accounts for alcohol’s impact on sexual behavior. Our finding that MSM often report increased intentions to have sex before doing so also offers some support for specific models of health behavior (e.g., theory of planned behavior; 38).
The second model explored mechanisms of alcohol’s effects on high-risk sexual behavior specifically when MSM reported having sex. The only significant indirect effect—through subjective sexual arousal—suggested that increasing levels of alcohol use beyond 5+ drinks incrementally increased levels of subjective sexual arousal, which in turn increased the odds of MSM engaging in high-risk CAS (relative to safer sex). These results are consistent with at least some previous experimental studies conducted in heterosexual men and women, which have shown that alcohol intoxication uniquely increased subjective sexual arousal, but not physiological sexual arousal, and that these intoxication-related increases in subjective arousal are often associated with reporting greater intentions to engage in condomless sex in hypothetical scenarios (15, 39, 40). Again, our findings extend these previous results by showing that this process also drives alcohol-involved HIV-risk behavior among MSM in the real world (15).
We found no evidence supporting the role of other previously proposed mediators, including condom use intentions or perceived control over condom use, in explaining alcohol’s tendency to reduce condom use and facilitate sex with high-risk partners. This suggests MSM may be more likely to engage in HIV-risk behavior when under the influence of alcohol due to alcohol’s role in strengthening sexual emotional states more so than its role in increasing explicit sexual motivation or intentions. Although it is difficult even for researchers to distinguish between these two constructs (35, 41), these findings suggest that a strong emotional component may play a more important role in MSM’s decisions to engage in unsafe sex than their plans or intentions beforehand. As such, interventions that help recipients develop insight about the role of strong emotions on their sexual choices and provide strategies to temper this influence may be beneficial (35, 42), e.g., helping recipients regulate high-approach emotions or strengthen more deliberative processes when in the “heat of the moment” (e.g., practicing safe sex negotiation in similar situations; 43, 44). However, it is important to note that this indirect path only partially accounted for the effect of alcohol level on high-risk CAS, suggesting that other, unobserved processes may be important. Similarly, it is unlikely that subjective sexual arousal is the sole mediator involved in this indirect effect. Alcohol’s unique effects on subjective arousal, independent of physiological arousal, suggests this effect is not solely due to one’s interpretation or feedback from one’s physiological state. Instead, alcohol may activate beliefs or expectations that drinking facilitates sex and/or decreases inhibitions, which in turn increase sexual arousal (45, 46). Although some studies have shown that individuals with stronger beliefs about alcohol’s effects on sexual decisions endorsed stronger condomless sex intentions when drinking (13), others have not (14).
Limitations
A number of important limitations should be noted. First, results reflect one sample of 100 MSM mostly from the northeastern US, and so, may not generalize to other populations. Second, our approach to analysis used all ES surveys occurring prior to a sex event on a given day. Although this enabled us to test whether alcohol use preceding sex events resulted in more risk, it raises the possibility that drinking actually occurred much earlier in the day on sex days and had stopped for some time when sex occurred. However, examining the raw data does not support this conclusion. Of the 62% of sex events that were preceded by drinking anytime earlier in the day, participants only reported having consumed no drinks in the ES immediately preceding a sex event 8% of the time. Thus, this scenario was very rare and is unlikely to account for observed results. Even for these events, many reported drinking in the next earlier ES assessment, suggesting they may still have been experiencing alcohol’s effects at the time of sex. Third, we tested indirect effects using the typical product-of-coefficients strategy, because (to our knowledge) resampling methods for estimating the CIs of indirect effects in three-level logistic models have not yet been described. The product-of-coefficients approach yields standard errors based on normal theory (47) and has been shown to produce biased standard errors that may lead to type I error and power problems (48, 49). Since methods for correcting this bias have not yet been identified, however, we believe applying the best available practice was appropriate. Third, we did not intend this model to be all-inclusive, and these analyses focused on a limited set of what we believed were among the most relevant potential mediators of the alcohol-sexual risk relationship. Other mediators are likely to have been omitted. Similarly, it is likely that some variables have relationships with alcohol use and sexual behavior that are more complex than simply as mediators between the two variables. However, our goal in applying these parallel mediation models was primarily to identify key mediators that could serve as a starting point for exploring more complex relationships. Finally, although the majority of included mediators varied considerably at the moment-level (ρ=.31-.55), one was particularly stable within participants (norms [ρ=.82]). Although it is not necessarily improper to include variables like these in models exploring variation across moments, these data suggest that norms may be more appropriately characterized as a person-level attribute.
Conclusions
In summary, we showed that VHD was indirectly associated with engaging in sex through both subjective sexual arousal and anal sex intentions. When MSM reported engaging in sex, the odds of engaging in high-risk CAS increased incrementally after drinking heavily (5–11 drinks) and very heavily (12+ drinks), and this effect was significantly mediated by sexual arousal. Findings suggest that interventions might help MSM plan for using prevention methods when drinking and monitor the effects of sexual arousal on their decision-making. Future research should focus on specifying when and for whom these effects are strongest, as well as identifying other, potentially modifiable mediators of the alcohol-sexual risk relationship (e.g., expectations about alcohol’s effects on sex).
Acknowledgements
This manuscript was supported by P01AA019072 (to PM), L30AA023336 (to TW), and K05AA019681 (to PM) from the National Institute on Alcohol Abuse and Alcoholism, and P30AI042853 (to CK) from the National Institute on Allergy and Infectious Diseases.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to report.
Clinical Trial Registration: None.
References
- 1.Centers for Disease Control and Prevention. Fact Sheet: Today’s HIV Epidemic Atlanta, GA: U.S. Department of Health and Human Services; 2016. [Available from: http://www.webcitation.org/6vAPiBrwN. [Google Scholar]
- 2.Centers for Disease Control and Prevention. HIV Among Youth Atlanta, GA: U.S. Department of Health and Human Services; 2018. [Available from: https://www.cdc.gov/hiv/group/age/youth/index.html. [Google Scholar]
- 3.Centers for Disease Control and Prevention. CDC Fact Sheet: HIV Among Gay and Bisexual Men. Atlanta, GA: U.S. Department of Health and Human Services; 2017. [Google Scholar]
- 4.Centers for Disease Control and Prevention. Diagnoses of HIV infection in the United States and dependent areas, 2016 HIV Surveillance Report. Atlanta, GA: National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention; 2017. [Google Scholar]
- 5.Finlayson T, Cha S, Denson D, Trujillo L, Xia M, Prejean J, et al. Abstract 972: Changes in HIV PrEP awareness and use among men who have sex with men, 2014 vs. 2017. 2019.
- 6.Wu H, Mendoza MC, Huang Y-lA, Hayes T, Smith DK, Hoover KW. Uptake of HIV preexposure prophylaxis among commercially insured persons—United States, 2010–2014. Clinical Infectious Diseases. 2016;64(2):144–9. [DOI] [PubMed] [Google Scholar]
- 7.Paz-Bailey G, Mendoza MC, Finlayson T, Wejnert C, Le B, Rose C, et al. Trends in condom use among MSM in the United States: the role of antiretroviral therapy and seroadaptive strategies. AIDS (London, England). 2016;30(12):1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kirby T, Thornber-Dunwell M. Uptake of PrEP for HIV slow among MSM. The Lancet. 2014;383(9915):399. [DOI] [PubMed] [Google Scholar]
- 9.Sander PM, Cole SR, Stall RD, Jacobson LP, Eron JJ, Napravnik S, et al. Joint effects of alcohol consumption and high-risk sexual behavior on HIV seroconversion among men who have sex with men. AIDS. 2013;27(5):815–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koblin BA, Husnik MJ, Colfax G, Huang Y, Madison M, Mayer K, et al. Risk factors for HIV infection among men who have sex with men. Aids. 2006;20(5):731–9. [DOI] [PubMed] [Google Scholar]
- 11.Rehm J, Shield KD, Joharchi N, Shuper PA. Alcohol consumption and the intention to engage in unprotected sex: Systematic review and meta‐analysis of experimental studies. Addiction. 2012;107(1):51–9. [DOI] [PubMed] [Google Scholar]
- 12.Vosburgh HW, Mansergh G, Sullivan PS, Purcell DW. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS and Behavior. 2012;16(6):1394–410. [DOI] [PubMed] [Google Scholar]
- 13.Maisto SA, Palfai T, Vanable P, Heath J, Woolf-King S. The effects of alcohol and sexual arousal on determinants of sexual risk in men who have sex with men. Archives of Sexual Behavior. 2012;41(4):971–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wray TB, Celio MA, Pérez AE, DiGuiseppi GT, Carr DJ, Woods LA, et al. Causal Effects of Alcohol Intoxication on Sexual Risk Intentions and Condom Negotiation Skills Among High-Risk Men Who Have Sex with Men (MSM). AIDS and behavior. 2019;23(1):161–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.George WH, Davis KC, Norris J, Heiman JR, Stoner SA, Schacht RL, et al. Indirect effects of acute alcohol intoxication on sexual risk-taking: The roles of subjective and physiological sexual arousal. Archives of sexual behavior. 2009;38(4):498–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mustanski B. The influence of state and trait affect on HIV risk behaviors: A daily diary study of MSM. Health Psychology. 2007;26(5):618. [DOI] [PubMed] [Google Scholar]
- 17.Grov C, Golub SA, Mustanski B, Parsons JT. Sexual compulsivity, state affect, and sexual risk behavior in a daily diary study of gay and bisexual men. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors. 2010;24(3):487–97. [DOI] [PubMed] [Google Scholar]
- 18.Ajzen I. The theory of planned behaviour: reactions and reflections. Psychology & health. 2011;26(9):1113–27. [DOI] [PubMed] [Google Scholar]
- 19.Sheeran P, Taylor S. Predicting Intentions to Use Condoms: A Meta‐Analysis and Comparison of the Theories of Reasoned Action and Planned Behavior 1. Journal of Applied Social Psychology. 1999;29(8):1624–75. [Google Scholar]
- 20.Albarracin D, Johnson BT, Fishbein M, Muellerleile PA. Theories of reasoned action and planned behavior as models of condom use: a meta-analysis. Psychological bulletin. 2001;127(1):142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hardeman W, Johnston M, Johnston D, Bonetti D, Wareham N, Kinmonth AL. Application of the theory of planned behaviour in behaviour change interventions: A systematic review. Psychology and health. 2002;17(2):123–58. [Google Scholar]
- 22.Watson D, Clark LA. The PANAS-X: Manual for the positive and negative affect schedule-expanded form. 1994.
- 23.Dvorak RD, Pearson MR, Day AM. Ecological momentary assessment of acute alcohol use disorder symptoms: Associations with mood, motives, and use on planned drinking days. Experimental and clinical psychopharmacology. 2014;22(4):285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Simons JS, Dvorak RD, Batien BD, Wray TB. Event-level associations between affect, alcohol intoxication, and acute dependence symptoms: Effects of urgency, self-control, and drinking experience. Addictive behaviors. 2010;35(12):1045–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Trull TJ, Wycoff AM, Lane SP, Carpenter RW, Brown WC. Cannabis and alcohol use, affect and impulsivity in psychiatric out‐patients’ daily lives. Addiction. 2016;111(11):2052–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: A clinician’s guide (NIH Publication No. 07–3769). Rockville, MD: U.S. Department of Health and Human Services; 2005. [Google Scholar]
- 27.Greenfield TK, Ye Y, Bond J, Kerr WC, Nayak MB, Kaskutas LA, et al. Risks of alcohol use disorders related to drinking patterns in the U.S. general population. Journal of studies on alcohol and drugs. 2014;75(2):319–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kahler CW, Wray TB, Pantalone D, Kruis R, Mastroleo N, Monti PM, et al. Daily associations between alcohol use and unprotected anal sex among heavy drinking HIV-positive men who have sex with men. AIDS and Behavior. 2015;19(3):422–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wray TB, Celio M, Mastroleo N, Kahler CW, Monti PM. Daily co-occurence of alcohol use and high-risk sexual behavior among heterosexual, heavy drinking emergency department patients. Drug and alcohol dependence. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach: Guilford Publications; 2017.
- 31.Preacher KJ, Zyphur MJ, Zhang Z. A general multilevel SEM framework for assessing multilevel mediation. Psychological methods. 2010;15(3):209. [DOI] [PubMed] [Google Scholar]
- 32.Preacher KJ. Multilevel SEM strategies for evaluating mediation in three-level data. Multivariate behavioral research. 2011;46(4):691–731. [DOI] [PubMed] [Google Scholar]
- 33.VanderWeele TJ, Vansteelandt S. Odds ratios for mediation analysis for a dichotomous outcome. American journal of epidemiology. 2010;172(12):1339–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Newcomb ME. Moderating effect of age on the association between alcohol use and sexual risk in MSM: evidence for elevated risk among younger MSM. AIDS and Behavior. 2013;17(5):1746–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maisto SA, Simons JS. Research on the effects of alcohol and sexual arousal on sexual risk in men who have sex with men: implications for HIV prevention interventions. AIDS and Behavior. 2016;20(1):158–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.George WH, Davis KC, Norris J, Heiman JR, Schacht RL, Stoner SA, et al. Alcohol and erectile response: the effects of high dosage in the context of demands to maximize sexual arousal. Experimental and clinical psychopharmacology. 2006;14(4):461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.George WH, Cue Davis K, Schraufnagel TJ, Norris J, Heiman JR, Schacht RL, et al. Later that night: Descending alcohol intoxication and men’s sexual arousal. American journal of men’s health. 2008;2(1):76–86. [DOI] [PubMed] [Google Scholar]
- 38.Ajzen I. From intentions to actions: A theory of planned behavior: Springer; 1985. [Google Scholar]
- 39.Prause N, Staley C, Finn P. The effects of acute ethanol consumption on sexual response and sexual risk-taking intent. Archives of Sexual Behavior. 2011;40(2):373–84. [DOI] [PubMed] [Google Scholar]
- 40.Davis KC, George WH, Norris J, Schacht RL, Stoner SA, Hendershot CS, et al. Effects of alcohol and blood alcohol concentration limb on sexual risk-taking intentions. Journal of studies on alcohol and drugs. 2009;70(4):499–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Janssen E. Sexual arousal in men: A review and conceptual analysis. Hormones and behavior. 2011;59(5):708–16. [DOI] [PubMed] [Google Scholar]
- 42.Andrasik MP, Otto JM, Nguyen HV, Burris LD, Gilmore AK, George WH, et al. The potential of alcohol “heat-of-the-moment” scenarios in HIV prevention: A qualitative study exploring intervention implications. Archives of sexual behavior. 2013;42(8):1487–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lorimer K, Kidd L, Lawrence M, McPherson K, Cayless S, Cornish F. Systematic review of reviews of behavioural HIV prevention interventions among men who have sex with men. AIDS care. 2013;25(2):133–50. [DOI] [PubMed] [Google Scholar]
- 44.Read SJ, Miller LC, Appleby PR, Nwosu ME, Reynaldo S, Lauren A, et al. Socially optimized learning in a virtual environment: Reducing risky sexual behavior among men who have sex with men. Human communication research. 2006;32(1):1–34. [Google Scholar]
- 45.Leigh BC. The relationship of sex‐related alcohol expectancies to alcohol consumption and sexual behavior. British journal of addiction. 1990;85(7):919–28. [DOI] [PubMed] [Google Scholar]
- 46.Kahler CW, Wray TB, Pantalone D, Mastroleo N, Kruis R, Mayer K, et al. Assessing sexual motives for drinking alcohol among HIV-positive men who have sex with men. Psychology of Addictive Behaviors. 2015;29(1):247–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sobel ME. Some new results on indirect effects and their standard errors in covariance structure models. Sociological methodology. 1986;16:159–86. [Google Scholar]
- 48.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological methods. 2002;7(1):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate behavioral research. 2004;39(1):99–128. [DOI] [PMC free article] [PubMed] [Google Scholar]


