Abstract
Background:
One of the critical components in pain management is the assessment of pain. Multidimensional measurement tools capture multiple aspects of a patient’s pain experience, yet can be cumbersome to administer in busy clinical settings. We conducted a systematic review to identify brief multidimensional pain assessment tools that nurses can use in both ambulatory and acute care settings.
Methods:
We searched PUBMED/MEDLINE, PsychInfo, and CINAHL databases from January 1977 through December 2019. Eligible English-language articles were systematically screened and data were extracted independently by two raters. Main outcomes included the number and types of domains captured by each instrument (e.g., sensory, impact on function, temporal components) and tool characteristics (e.g., administration time, validity) that may impact instrument uptake in practice.
Results:
Our search identified eight multi-dimensional assessment tools. All eight measured sensory and/or affective qualities of pain and its impact on functioning. Most tools measured impact of pain on affective functioning, mood, or enjoyment of life. One tool used ecological momentary assessment via a web-based app to assess pain symptoms. Time to administer the varying tools ranged from less than two minutes to ten minutes and evidence of validity was reported for seven of the eight tools.
Conclusions:
Our review identified eight multidimensional pain measurement tools that nurses can use in ambulatory or acute care settings to capture patients’ experience of pain. The most important element in selecting a multidimensional pain measure, though, is that one tool is selected that best fits the practice and is used consistently over time.
Keywords: chronic pain, multidimensional pain assessment tools, ambulatory care
Background
It is estimated that greater than 100 million Americans suffer from chronic non-cancer pain, which is far more than the total number affected by diabetes, heart disease, and cancer combined (Institute of Medicine, 2011). Pain is associated with substantial suffering, morbidity (Dahlhamer et al., 2018; Institute of Medicine, 2011), and healthcare costs (Centers for Disease Control and Prevention, 2014.). Its negative effects often extend beyond the patient to disrupt both family and social relationships (Reid, Eccleston, & Pillemer, 2015). Given its public health impact, healthcare providers, irrespective of discipline, should develop competencies in assessing and managing pain.
Given widespread recognition that pain was underassessed and undertreated, various societies and organizations began in the 1990’s to promote the adoption of systematic pain assessment practices (Scher, Meador, Van Cleave, & Reid, 2018). To accommodate busy clinical settings, these assessments usually consisted of brief questions that addressed only one dimension of pain, i.e., its sensory component. This movement included the Pain as the Fifth Vital Sign (P5VS) initiative. Launched in the early 2000’s, P5VS called for healthcare providers to assess for pain and when present determine its intensity and/or severity. Despite widespread adoption of P5VS, a growing body of literature demonstrates that this initiative has not improved the quality of pain care, and may have contributed, in part, to the current opioid crisis (Ballantyne & Sullivan, 2015; Kolodny et al., 2015; Petti, Scher, Meador, Van Cleave, & Reid, 2018; Scher et al., 2018).
Given the established limitations of using unidimensional pain measures, clinicians and researchers’ focus has now turned toward the use of multidimensional pain assessment tools (Giannitrapani et al., 2019; Radnovich et al., 2014; Twining & Padula, 2019). Multidimensional pain assessment tools by definition consist of multiple domains - including sensory and affective qualities of pain, temporal dimensions of pain, and the location and bodily distribution of pain (Fillingim, Loeser, Baron, & Edwards, 2016). Use of multidimensional tools to assess pain could increase the likelihood of identifying a specific diagnosis, help to select the most appropriate pharmacological and non-pharmacological interventions for pain relief, and guide selection of treatments that align with patients’ needs and desires (Dansie & Turk, 2013; van Boekel et al., 2017).
Despite the apparent benefits of multidimensional pain assessment, a critical barrier to implementation is the length of time needed to administer multi-item tools. Busy inpatient and outpatient settings necessitate the need for tools that are user–friendly for both patients and clinicians, easy to administer, and capture the impact of pain on patients’ lives (Giannitrapani et al., 2019). But what multidimensional pain assessment tools are currently available? What domains do they assess and have the tools been validated for use in practice? As importantly, how feasible are they to implement in busy practice settings? To address these questions, we undertook the following systematic review to identify multidimensional pain assessment tools for use in adult patients with chronic pain. Some of the tools identified in this review may also be appropriate for individuals suffering from acute pain (Radnovich et al., 2014). Finally, because nurses care for adult patients with chronic pain in various clinical settings, we focused our search on tools appropriate for use in both ambulatory and acute care environments.
Methods
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Liberati et al., 2009; Moher, Liberati, Tetzlaff, & Altman, 2009). To identify existing multidimensional pain assessment tools, we searched the PUBMED/MEDLINE, PsychInfo, and CINAHL databases for English-language articles published from January 1977 through December 2019. MEsH search terms used included, “chronic pain,” “surveys and questionnaires,” “outpatient clinics,” “hospital,” and “ambulatory care.” Reference lists of the retained articles were also searched to identify additional eligible articles. Articles were retained for review if the tool was developed for use in clinical practice to assess adults with pain. Articles were excluded if the tool 1) included only one dimension of pain (e.g., a severity measure), 2) was designed for use as a research measure, 3) took more than an average of ten minutes to complete, or 4) was designed to measure pain in a specific part of the body (e.g., back) or pain related to a specific disease (e.g., diabetes). Finally, articles were also excluded if published in a language other than English.
Two authors reviewed the titles and abstracts of all articles identified from the initial search. If a paper evaluated a multidimensional pain assessment tool, the authors reviewed the full paper independently to determine if it met inclusion criteria. Once the sample was finalized, two authors extracted data independently from the articles into customized tables and compared the results for accuracy.
The study team used directed content analysis (Hsieh & Shannon, 2005) to identify key elements of the selected multidimensional pain assessment tools. These elements were mapped to the domains (e.g. sensory and/or affective qualities, temporal characteristics) identified from prior literature (Fillingim et al., 2016; McGuire, 1992). The study team also identified salient tool characteristics (e.g., time to administer, evidence of validity) that could help clinicians to decide whether to use a given tool in practice. The reviewers and senior author settled any discrepancies through discussion using audit trails.
To appraise the quality of evidence of the identified tools, two members of the study team evaluated the quality of evidence presented in the articles using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) (von Elm et al., 2014) criteria for observational studies. The STROBE checklist consists of 22 criteria.
Additional literature searches were conducted to determine whether published evidence existed regarding key tool characteristics (i.e., recall period, copyright status). Lastly, the study team contacted the authors of the identified tools to confirm that the information presented below was accurately categorized.
Results
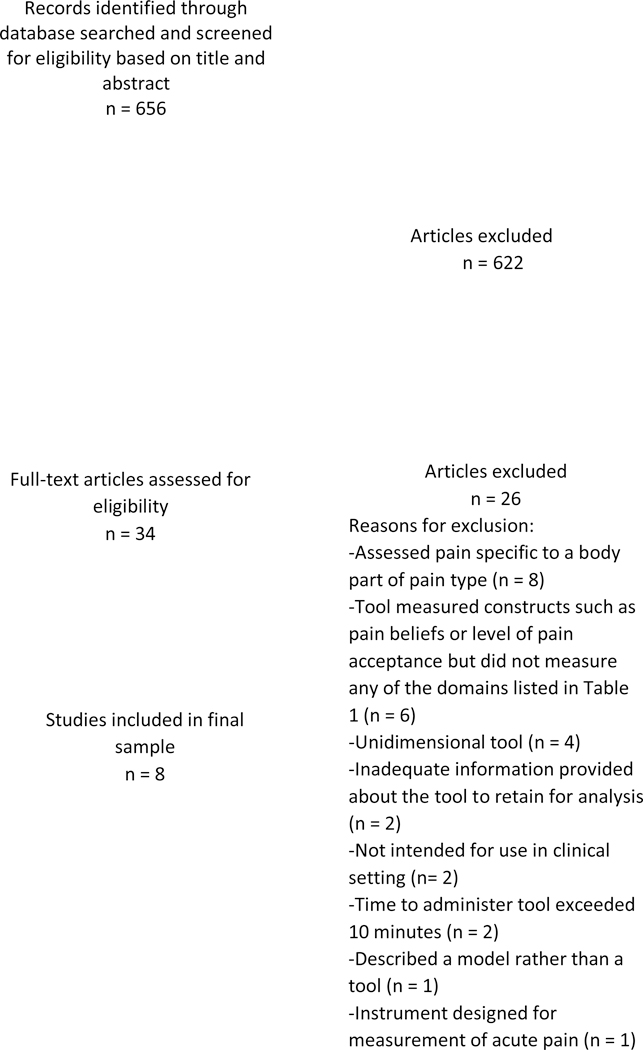
Our search strategy generated 656 citations; 622 were excluded after screening titles and abstracts. Thirty-four articles were selected for further review. Twenty-six articles described pain measurement tools that were excluded for various reasons (Figure 1), leaving a total of eight articles in the final sample. Each article provided information on a different multidimensional pain assessment tool.
Figure 1. Flow diagram of the study selection process.
All individual questions included in the eight tools were assigned to the domains shown in Table 3. These categories included: sensory and affective qualities, temporal characteristics (e.g., duration of pain), location, interference with function/sleep, associated symptoms (e.g., fatigue), impact on quality of life, interference with relationships/social, impact on affective functioning/mood/enjoyment of life, treatments (e.g., efficacy of past treatments), and comorbidities.
Table 3.
STROBE quality appraisal scores.
| Quality Assessment Criteria | Number and % of Articles Meeting Each Criterion |
|---|---|
| Title/Abstract | 8 (100%) |
| Introduction/Background/Rationale | 8 (100%) |
| Objectives | 8 (100%) |
| Methods/Study Design | 5 (63%) |
| Setting | 8 (100%) |
| Participants | 6 (75%) |
| Variables | 5 (63%) |
| Data Source/Measurement | 8 (100%) |
| Bias | 2 (25%) |
| Study Size | 5 (63%) |
| Quantitative Variables | 6 (75%) |
| Statistical Methods | 6 (75%) |
| Results/Participants | 6 (75%) |
| Descriptive Data | 5 (63%) |
| Outcome Data | 6 (75%) |
| Main Results | 8 (100%) |
| Other Analyses | 3 (38%) |
| Discussion/Key Results | 7 (88%) |
| Limitations | 7 (88%) |
| Interpretation | 8 (100%) |
| Generalizability | 6 (75%) |
| Funding/Conflict of Interest | 6 (75%) |
The mean number of domains assessed by the various instruments was 4.75 (range 2–10). All eight tools included at least one item in the sensory and/or affective category and in the impact of pain on functioning and/or sleep category. Six tools included items to gauge the level of pain’s impact on patients’ affect/mood/enjoyment of life. Three tools included items designed to gauge the extent to which pain impacts social relationships, while two tools included questions about the effect of pain on quality of life. Three tools included questions to evaluate the treatment for pain. Two tools prompted patients to indicate the location of their pain.
Table 2 provides information related to characteristics (e.g., number of items, time to administer) that could impact uptake of a given tool in practice. The time to administer the varying tools ranged from less than two minutes to ten minutes, while the number of individual items in each tool varied from 2 to 44. The eight tools differed in terms of recall period, which ranged from right now to the past four weeks. Evidence of validity was reported for seven of the eight tools (Table 2). Four tools are copyrighted while one is trademarked. Three tools may be used without permission from the authors who created the assessment tools.
Table 2.
Specific characteristics of multidimensional pain tools.
| Tool Name | Time to administer | Number of Items | Score range | Recall Period | Validity | Responsiveness to Change | Copyright* |
|---|---|---|---|---|---|---|---|
| Brief Pain Inventory (BPI)a | 10 min. | 11 | 0–10 for each subscale | Past 24 hours | -Concurrent-Predictive | Yes | Copyrighted† |
| Clinically Aligned Pain Assessment (CAPA) Toolb,c | ~ 5 min.‡ | n/a | n/a | Right now | Not yet established | NR§ | Copyrighted|| |
| Defense and Veterans Pain Rating Scaled | < 5 min. | 5 | 0–10 | Past 24 hours | -Concurrent | NR§ | Free of copyright¶ |
| Geriatric Pain Measuree | < 5 min. | 24 | 0–42 | Last 7 days (including today) | -Concurrent | NR§ | Free of copyright# |
| Pain Impact Questionnaire™ (PIQ-6)f | < 5 min. | 6 | 36–81 | Past 4 weeks | -Convergent-Construct | NR§ | Trademarked |
| PEGg | < 5 min. | 3 | 0–10 | Past week | -Construct | Yes | Free of copyright# |
| Pain Monitorh | < 5 min. | 44** | 0–11 or 1–5 | Right now, today, last night | -Construct | NR§ | Copyrighted |
| Short Form-36 Bodily Pain Scale (SF-36 BPS)i,j | < 2 min. | 2 | 0–100 | Past 4 weeks or 1 week | -Face-Content | Yes | Copyrighted†† |
* Copyright typically requires permission and/or license agreement in order to use the tool.
† The BPI may not be used or reproduced without permission from Charles S. Cleeland, PhD or designee; the tool can be ordered at https://www.mdanderson.org/research/departmentslabs-institutes/departments-divisions/symptom-research/symptom-assessment-tools/brief-pain-inventory.html.
‡ Tool requires a conversation that could last a couple minutes to longer, but on average lasts 5 minutes.k
§ NR = not reported.
|| Copyright held by Donaldson & Chapman at University of Utah Health/Department of Anesthesiology.
¶ Permission is granted for clinicians and researchers to freely use the Defense and Veterans Pain Rating Scale as is, without alteration. If used in revised or altered form, it should not be referred to as the Defense and Veterans Pain Rating Scale.
# Can be accessed online through various sources.
** May vary based on time of assessment. 7 items in the morning only, 14 in the evening only, and 6 both in the morning and the evening and on demand; plus 7 items on the first day of app use, 3 on the last day of app use, and 7 both on the first and last day of app use.
†† SF-36 survey instruments, scoring manuals, and licenses for use are available at www.qualitymetric.com.
Quality Appraisal
Table 3 shows that manuscript quality scores ranged between 10 – 22 with a mean of 17.1 +/− 4.6. All articles contained adequate description of the measures and main results. However, only 25% (2 of 8) articles addressed assessment of bias of study findings.
Multidimensional Pain Assessment Tool Descriptions
The following section provides a brief review of each multidimensional tool.
The Brief Pain Inventory (short-form) is an 11-item tool assessing pain intensity and interference over the past 24 hours and at its worst, least, and average (Cleeland, 1989). Widely used to assess pain in patients with cancer and validated in many languages, the Brief Pain Inventory has also been validated for use in patients with chronic non-cancer pain (Tan, Jensen, Thornby, & Shanti, 2004). This tool is also used to capture physical and socio-emotional dimensions of pain that may inform appropriate treatment decisions (Tan et al., 2004).
The Clinically Aligned Pain Assessment Measure (CAPA) is a discussion-based tool without a fixed number of items that assesses comfort, change in pain, pain control, functioning, and sleep through structured dialogue between the patient and provider (Twining & Padula, 2019). The tool was implemented at a Midwest hospital to replace a unidimensional numeric rating scale. After adopting the tool, nurses found that CAPA did not take that much longer than the numeric rating scale to complete. After further pilot testing, physicians and nurses also found that CAPA effectively informed their clinical decision making, and provided comprehensive information about their patients’ pain (Topham & Drew, 2017; Twining & Padula, 2019).
The Defense and Veterans Pain Rating Scale is a 5-item assessment tool that measures the level of pain intensity and interference of pain on an individual’s activity, as well as its impact on sleep, mood, and stress over the last 24 hours (Nassif, Hull, Holliday, Sullivan, & Sandbrink, 2015). Studies have shown strong concurrent validity with other validated pain assessment measures, and acceptable psychometric properties in a military population (Buckenmaier et al., 2013; Nassif et al., 2015). Studies suggest that the tool may be an effective method for ascertaining the presence and degree of pain-related disability (Nassif et al., 2015).
The Geriatric Pain Measure is a 24-item questionnaire that assesses pain intensity, physical and social function, mood, quality of life, and health services utilization over the last seven days (Ferrell, Stein, & Beck, 2000). This valid and reliable tool may be particularly helpful when assessing the impact of pain on functioning among older adults with multiple comorbidities. A short version of the Geriatric Pain Measure was successively used to assess pain in a sample of nursing home residents with and without dementia (Monroe et al., 2014), providing support for the tool’s use in older adults with and without cognitive impairment.
The Pain Impact Questionnaire is a 6-item tool that measures pain severity and the extent to which pain interferes with normal work, enjoyment of life, ability to perform simple tasks, pursuit of leisure activities, as well as its impact on mood in the past four weeks (Becker, Schwartz, Saris-Baglama, Kosinski, & Bjorner, 2007). It can be used in homes, clinics, and other clinical settings and is available in both a paper and pencil version as well as a computerized version (Becker et al., 2007). Because it is a short measure that can be adapted to a tablet or other computerized device, the Pain Impact Questionnaire can be readily implemented in a variety of clinical settings to help providers make pain treatment decisions.
The PEG is a three-item tool that measures average pain, pain interference with enjoyment of life, and pain interference with general activity over the past week (Krebs et al., 2009). The PEG has demonstrated reliability and validity when employed in the care of primary care patients with chronic musculoskeletal pain (Krebs et al., 2009). The PEG has also demonstrated responsiveness to change in pain over time (Krebs et al., 2009). The brevity and multidimensionality of the PEG suggests that it may be particularly useful across diverse care settings.
Pain Monitor is a 44-item web-based app that evaluates pain-related variables, including key psychological constructs, twice per day at customizable times (Suso-Ribera et al., 2018). In line with the shift towards using Ecological Momentary Assessment (EMA) in health and pain clinic settings, Pain Monitor evaluates chronic pain in real-time and also allows for the tracking of acute pain episodes. The app was originally developed in Spanish, but has since been translated into English. Participants in one study found the app “extremely easy to use” (Suso-Ribera et al., 2018). The app has demonstrated construct validity, and has the potential to inform the selection of specific pain treatments. Recent iterations of Pain Monitor have added features that involve clinician alarms, where clinicians can be alerted to the “presence of preestablished undesired events” which clinicians and patients work together to identify (Suso-Ribera et al., 2018).
The Short Form 36 Bodily Pain Scale is a two-item questionnaire that measures pain intensity and interference with activities (Hawker, Mian, Kendzerska, & French, 2011). This valid and reliable measure takes less than two minutes to complete. The tool has been shown to detect change in pain over time (Hawker et al., 2011). In addition, the entire SF-36 Health Survey may also be used in addition to the SF-36 Bodily Pain Scale (BPS) to measure additional domains such as mental health and physical function (Ware & Sherbourne, 1992).
Discussion
Nurses are on the frontline of providing healthcare for millions of adults who experience chronic pain (Dahlhamer et al., 2018). Thus, assessment of patients in pain is a critical component of nursing practice (Fishman et al., 2013; Herr et al., 2015). Our review identified eight multidimensional tools that can be used for such a purpose. The tools identified in this systematic review appear to meet the important criterion that they can be used in busy clinical practices, are easily administered, and capture the impact of pain on patients’ lives (Giannitrapani et al., 2019).
The identified tools reflect variations in approach to pain measurement, including availability, length, and measurement of differing domains. Beyond the domain of “Sensory and/or Affective Qualities,” the only other domain present in all eight tools is assessment of pain’s interference with function and/or sleep. In addition, the tools identified in our study are available for use by clinicians to varying degrees. Four are copyrighted (clinicians are required to request author permission), one is trademarked (clinicians are required to buy the rights to use the tool in their practice), while three are free of copyright. The pain tools also vary considerably by length. For example, the PEG consists of three questions using numerical ratings of pain that rate pain intensity and interference in life enjoyment and general activity. In contrast, the Geriatric Pain Measure consists of 24 questions that include a mixture of binomial questions and numerical ratings of pain intensity.
Despite the documented variations, many of the tools share similar characteristics. Seven out of the eight tools have established some form of validity, demonstrating that questions accurately measure the domains they are trying to capture. Further, all of the identified tools focus on the negative consequences of pain, i.e., they attempt to quantify the extent of interference or impact on various aspects of functioning. In addition, three of the tools have been examined for their ability to detect treatment-related change over time and supporting evidence was found for all three. It is possible that the remaining five measures have the ability to detect clinically relevant changes with treatment, but have not reported the data. Finally, this review documents that none of the tools measure adaptive behavioral responses (e.g., use of distraction, exercise) as a means of managing pain.
Given the established limitations of unidimensional pain assessment tools (Ballantyne & Sullivan, 2015; Kolodny et al., 2015; Scher et al., 2018), federal agencies and pain societies now support clinicians use and researchers study of multidimensional pain assessment tools. These federal agencies and pain societies have promulgated recommendations that urge clinicians to employ multidimensional pain assessment tools (Chou et al., 2016). For example, the US Surgeon General’s Turning the Tide campaign recommends use of the PEG as a brief screening tool to reduce opioid use (Kroenke, 2018). In addition, the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and American Society of Anesthesiologists have all published practice guidelines for the management of postoperative pain that recommend the use of multidimensional pain measurement tools (Chou et al., 2016). The Department of Veterans Affairs and the Department of Defense have also issued guidelines that call for thorough multidimensional assessment prior to starting opioid therapy. Additional calls for the use of multidimensional screening tools appear in a recently published evidence-based guideline for pain assessment in nursing home residents (Sirsch et al., 2020) and come from researchers documenting gender differences in the way men and women report pain intensity and pain unpleasantness (Cowan et al., 2017). Finally, other recent research (Monroe et al.,2016; Romano et al., 2019) provides strong support for the use of multidimensional pain assessment in patients with Alzheimer’s Disease.
Among the guidelines and references cited above, there is a notable lack of consensus regarding the type and nature of the multidimensional pain assessment that should be used. Given this lack of consensus, nurses are encouraged to select a tool for use that best matches the practice’s resources, time allowed per patient, and patient population. For example, if nurses are caring for a population composed primarily of older adults, then the Geriatric Pain Measure may be most appropriate.
Clinical Implications
This study has several implications for nursing practice. First, the tools identified in this review can serve as a starting point to screen patients who may be experiencing complex pain patterns. These patients could then undergo more comprehensive assessments as needed. For example, the U. S. Department of Veterans Affairs recommends that patients with chronic pain undergo a full biopsychosocial pain assessment to determine patients’ treatment goals, and to identify significant psychological or behavioral factors that may moderate treatment outcomes (U.S. Department of Veterans Affairs, 2017). In-depth assessments can be found on The University of Iowa Csomay Center for Gerontological Excellence website. This website also houses pain tools and resources that can be useful in the care of nonverbal patients, an important challenge for nurses who care for patients with dementia (University of Iowa Csomay Center for Gerontological Excellence).
Second, our review highlights the promise of online pain assessment, especially with the growth of electronic records in health care. One of the measures identified in this review, i.e., the Pain Monitor, may reflect the future of pain management. The Pain Monitor is a web-based app, designed to be accessible any time, allowing patients to record their acute pain episodes. This tool may be particularly useful in the outpatient setting where it can be employed to monitor temporal patterns of patients’ pain through the collection of longitudinal data. As an online pain measure, this tool has the potential to facilitate patient-provider communication that enhances clinical decision making about appropriate pain treatment for the patient. Further, the tool’s platform may have potential to house clinical decision support tools to deliver behavioral interventions (Meadows et al., 2018). Although excluded from this review because the length of time to administer exceeded the established ten-minute threshold, Pain Tracker (Langford et al., 2018) is an online pain assessment tool that measures diverse domains of the pain experience and is completed prior to clinic visits. The use of mobile-based tools like Pain Monitor and Pain Tracker may allow clinicians to obtain comprehensive evaluations of pain in shorter amounts of time.
The variation in recall periods employed in the assessment tools also deserves comment. Evidence supports that recall periods of one week are similar to daily recall period, whereas recall periods of 2, 3, 4 weeks may result in less reliable symptom reporting (Mendoza et al., 2017). Thus, the value of the loss of information from longer recall periods should be considered when selecting a pain assessment tool for use in outpatient practices. Nevertheless, the most important element in selecting a multidimensional pain measure is that one tool is selected and used consistently over time.
Research Implications
In terms of research gaps, more work is needed to assess whether and to what degree patient outcomes improve when multidimensional (vs. unidimensional) pain assessment tools are routinely employed. Other potential research studies could evaluate whether implementation of multidimensional tools in practice results in an increased use of non-pharmacological therapies such as behavioral interventions like psychotherapy. In addition, future research could also evaluate the feasibility and acceptability of multidimensional pain screening tools in diverse patient samples receiving care in outpatient as well as inpatient settings. More research is also needed to document that all of the identified tools are responsive to change in salient patientreported outcomes over time. Lastly, future work should investigate the utility of mobile-based multidimensional pain tools, such as the Pain Monitor, in clinical practice. A recent consensus conference on the topic of mHealth use and pain in older adults called for more research on the use of these tools in practice, how to enhance their use by patients with chronic pain, and whether the tools can improve patient-provider communication (Wethington et al., 2018).
Strengths and Limitations
The strength of this systematic review is the thorough evaluation of the characteristics and domains of the multidimensional pain tools described above. However, we recognize that there may be other existing multidimensional pain measurement tools that we did not capture using our search strategy. Accordingly, we view the eight tools highlighted in this article as prototypes of multidimensional pain tools that can be used to assess pain in clinical practice. The nature of our search excluded pain assessment tools such as the National Institutes of Health (NIH) Patient Reported Outcomes Measurement Information System (PROMIS) because it is comprised of five unidimensional item banks that when combined can become a comprehensive multidimensional measure of chronic pain (Cella et al., 2010). These item banks were excluded because they are designed for clinical research. In addition, we acknowledge that in a busy outpatient clinical practice, even a 10-minute assessment may be too time intensive. Having patients complete the assessment prior to the actual visit (where results are then reviewed together) could help to address this particular barrier. Finally, our search did not focus on multidimensional pain assessment tools designed for a specific clinical setting or population, so we cannot recommend a specific tool for clinicians to use. Providers should choose a tool based on what is most suitable to their practice.
Conclusions
Nurses are on the frontline of providing care for millions of adults who experience chronic pain (Dahlhamer et al., 2018; Fishman et al., 2013; Herr et al., 2015). Thus, assessment of patients in pain is a critical component of nursing practice. This systematic review identified eight multidimensional pain assessment tools that may be used in ambulatory and acute care settings. When considering whether to use one of the identified tools, the most important feature is to select a tool that best fits with the nature of the clinical practice and to use the tool consistently over time. The future of pain management may indeed be mobile-based apps that include interactive features that enhance patient–provider communication and shared decision-making. Accordingly, future research should include evaluations of the efficacy of mobile-based multidimensional pain assessment tools to optimize pain management in both ambulatory and acute care settings.
Table 1.
Domains of multidimensional pain tools.
| Domains | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Tools | Sensory and/or Affective Qualities* | Temporal Characteristics† | Location | Interference with Function‡/ Sleep | Associated Symptoms | Impact on Quality of Life | Interference with Relationships/ Social | Impact on Affective Functioning/ Mood/ Enjoyment of Life | Treatments§ | Comorbidities |
| Brief Pain Inventory (BPI)a | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Clinically Aligned Pain Assessment (CAPA) Toolb,c | ✓ | ✓ | ✓ | ✓ | ||||||
| Defense and Veterans Pain Rating Scaled | ✓ | ✓ | ✓ | |||||||
| Geriatric Pain Measuree | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Pain Impact Questionnaire (PIQ-6)f | ✓ | ✓ | ✓ | |||||||
| PEGg | ✓ | ✓ | ✓ | |||||||
| Pain Monitorh | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Short Form-36 Bodily Pain Scale (SF-36 BPS)i,j | ✓ | ✓ | ||||||||
* This includes items such as pain intensity, pain severity, and how unpleasant the pain feels.k
† This includes items such as duration of pain, change in pain, and onset of pain.
‡ This includes items that capture the impact of pain on activities of daily living that range from instrumental to advanced (e.g., leisure) activities.
§ This includes items such as current and past treatments for pain (e.g., opioid use), and questions about any unwanted treatment effects.
Key practice points:
Assessment of patients in pain is a critical component of nursing practice.
Given the established limitations of using unidimensional pain measures, clinicians and researchers’ focus has now turned toward the use of multidimensional pain assessment tools.
Our review identified eight multidimensional pain measurement tools that nurses can use in ambulatory or acute care settings to capture patients’ experience of pain.
The most important element in selecting a multidimensional pain measure, though, is that one tool is selected that best fits the practice and is used consistently over time.
Acknowledgements:
We would like to gratefully acknowledge the assistance of Ms. Jacquie Howard, whose managerial and editing skills greatly facilitated the preparation of the manuscript. Dr. Reid is supported by grants (K24AGO53462, P30AG022845) from the National Institute on Aging.
Footnotes
Conflicts of Interest: The authors declare no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ballantyne JC, & Sullivan MD (2015). Intensity of chronic pain--the wrong metric? New England Journal of Medicine, 373(22), 2098–2099. doi: 10.1056/NEJMp1507136. [DOI] [PubMed] [Google Scholar]
- Becker J, Schwartz C, Saris-Baglama RN, Kosinski M, & Bjorner JB (2007). Using Item Response Theory (IRT) for developing and evaluating the pain impact questionnaire (piq-6tm). Pain Medicine, 8(S3), S129–S144. doi: 10.1111/j.1526-4637.2007.00377.x. [DOI] [Google Scholar]
- Buckenmaier CC, Galloway KT, Polomano RC, McDuffie M, Kwon N, & Gallagher RM (2013). Preliminary validation of the Defense and Veterans Pain Rating Scale (DVPRS) in a military population. Pain Medicine, 14(1), 110–123. doi: 10.1111/j.15264637.2012.01516.x. [DOI] [PubMed] [Google Scholar]
- Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, Amtmann D, Bode R, Buysse D, Choi S, Cook K, Devellis R, DeWalt D, Fries JF, Gershon R, Hahn EA, Lai JS, Pilkonis P, Revicki D, Rose M, Weinfurt K, Hays R, & Group PC (2010). The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of Clinical Epidemiology, 63(11), 1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2014). The cost of arthritis in us adults. Retrieved from https://www.cdc.gov/arthritis/data_statistics/cost.htm (Accessed 11 December 2019). [Google Scholar]
- Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, Carter T, Cassidy CL, Chittenden EH, Degenhardt E, Griffith S, Manworren R, McCarberg B, Montgomery R, Murphy J, Perkal MF, Suresh S, Sluka K, Strassels S, Thirlby R, Viscusi E, Walco GA, Warner L, Weisman SJ, & Wu CL (2016). Management of postoperative pain: A clinical practice guideline from theAmerican Pain Society, The American Society of Regional Anesthesia and Pain Medicine, and The American Society Of Anesthesiologists’ committee on regional anesthesia, executive committee, and administrative council. Journal of Pain, 17(2), 131–157. doi: 10.1016/j.jpain.2015.12.008. [DOI] [PubMed] [Google Scholar]
- Cleeland C. (1989). Measurement of pain by subjective report In Chapman C & Loeser J (Eds.), Advances In Pain Research and Therapy (Vol. 12, pp. 391–403). New York: Raven Press. [Google Scholar]
- Cowan RL, Beach PA, Atalla SW, Dietrich MS, Bruehl SP, Deng J, Wang J, Newhouse PA, Gore JC, & Monroe TB (2017). Sex differences in the psychophysical response to contact heat in moderate cognitive impairment Alzheimer’s Disease: A cross-sectional brief report. Journal of Alzheimers Disease, 60(4), 1633–1640. doi: 10.3233/JAD-170532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlhamer J, Lucas J, Zelaya C, Nahin R, Mackey S, DeBar L, Kerns R, Von Korff M, Porter L, & Helmick C. (2018). Prevalence of chronic pain and high-impact chronic pain among adults — united states, 2016. MMWR Morbidity and Mortality Weekly Report, 67(36), 1001–1006. doi: 10.15585/mmwr.mm6736a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dansie EJ, & Turk DC (2013). Assessment of patients with chronic pain. British Journal of Anaesthesia, 111(1), 19–25. doi: 10.1093/bja/aet124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrell BA, Stein WM, & Beck JC (2000). The geriatric pain measure: Validity, reliability and factor analysis. Journal of the American Geriatrics Society, 48(12), 1669–1673. doi:DOI: 10.1111/j.1532-5415.2000.tb03881.x. [DOI] [PubMed] [Google Scholar]
- Fillingim RB, Loeser JD, Baron R, & Edwards RR (2016). Assessment of chronic pain: Domains, methods, and mechanisms. Journal of Pain, 17(9 Suppl), T10–20. doi: 10.1016/j.jpain.2015.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishman SM, Young HM, Lucas Arwood E, Chou R, Herr K, Murinson BB, Watt-Watson J, Carr DB, Gordon DB, Stevens BJ, Bakerjian D, Ballantyne JC, Courtenay M, Djukic M, Koebner IJ, Mongoven JM, Paice JA, Prasad R, Singh N, Sluka KA, St Marie B, & Strassels SA (2013). Core competencies for pain management: Results of an interprofessional consensus summit. Pain Medicine, 14(7), 971–981. doi: 10.1111/pme.12107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giannitrapani KF, Day RT, Azarfar A, Ahluwalia SC, Dobscha S, & Lorenz KA (2019). What do providers want from a pain screening measure used in daily practice? Pain Medicine, 20(1), 68–76. doi: 10.1093/pm/pny135. [DOI] [PubMed] [Google Scholar]
- Hawker GA, Mian S, Kendzerska T, & French M. (2011). Measures of adult pain: Visual Analog Scale for Pain (VAS PAIN), Numeric Rating Scale for Pain (NRS PAIN), Mcgill Pain Questionnaire (MPQ), Short-Form Mcgill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (sf-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care and Research (Hoboken), 63 Suppl 11, S240–252. doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- Herr K, Marie BS, Gordon DB, Paice JA, Watt-Watson J, Stevens BJ, Bakerjian D, & Young HM (2015). An interprofessional consensus of core competencies for prelicensure education in pain management: Curriculum application for nursing. Journal of Nursing Education, 54(6), 317–327. doi: 10.3928/01484834-20150515-02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh HF, & Shannon SE (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2011). Relieving pain in America: A blueprint for transforming prevention, care, education, and research. Washington, D.C.: The National Academies Press. [PubMed] [Google Scholar]
- Kolodny A, Courtwright DT, Hwang CS, Kreiner P, Eadie JL, Clark TW, & Alexander GC (2015). The prescription opioid and heroin crisis: A public health approach to an epidemic of addiction. Annual Review of Public Health, 36, 559–574. [DOI] [PubMed] [Google Scholar]
- Krebs EE, Lorenz KA, Bair MJ, Damush TM, Wu J, Sutherland JM, Asch SM, & Kroenke K. (2009). Development and initial validation of the PEG, a three-item scale assessing pain intensity and interference. J Gen Intern Med, 24(6), 733–738. doi: 10.1007/s11606-009-0981-1. PMC2686775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K. (2018). Pain measurement in research and practice. J Gen Intern Med, 33(Suppl 1), 7–8. doi: 10.1007/s11606-018-4363-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langford DJ, Tauben DJ, Sturgeon JA, Godfrey DS, Sullivan MD, & Doorenbos AZ (2018). Treat the patient, not the pain: Using a multidimensional assessment tool to facilitate patient-centered chronic pain care. Journal of General Internal Medicine, 33(8), 1235–1238. doi: 10.1007/s11606-018-4456-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, & Moher D. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLOS Medicine, 6(7), e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire DB (1992). Comprehensive and multidimensional assessment and measurement of pain. Journal of Pain Symptom Management, 7(5), 312–319. [DOI] [PubMed] [Google Scholar]
- Meadows G, Moesel C, Nichols J, Pacchiana S, Sebastian S, Winters D, Corporation TM, van Leeuwen D, & Hats H. (2018). Factors to consider in managing chronic pain: A pain management summary Implementation guide. Prepared under contract no. Hhsm500–2012- 00008i. Ahrq publication no.18–0058-2-ef. Rockville, MD: Agency for Healthcare Research and Quality. [Google Scholar]
- Mendoza TR, Dueck AC, Bennett AV, Mitchell SA, Reeve BB, Atkinson TM, Li Y, Castro KM, Denicoff A, Rogak LJ, Piekarz RL, Cleeland CS, Sloan JA, Schrag D, & Basch E. (2017). Evaluation of different recall periods for the us national cancer institute’s pro-ctcae. Clinical Trials, 14(3), 255–263. doi: 10.1177/1740774517698645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, & Altman DG (2009). Preferred Reporting Items For Systematic Reviews And Meta-Analyses: The PRISMA statement. Annals of Internal Medicine, 151, 264–269. [DOI] [PubMed] [Google Scholar]
- Monroe TB, Gibson SJ, Bruehl SP, Gore JC, Dietrich MS, Newhouse P, Atalla S, & Cowan RL (2016). Contact heat sensitivity and reports of unpleasantness in communicative people with mild to moderate cognitive impairment in alzheimer’s disease: A cross-sectional study. BMC Medicine, 14, 74. doi: 10.1186/s12916-016-0619-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe TB, Misra SK, Habermann RC, Dietrich MS, Cowan RL, & Simmons SF (2014). Pain reports and pain medication treatment in nursing home residents with and without dementia. Geriatrics and Gerontology International, 14(3), 541–548. doi: 10.1111/ggi.12130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nassif TH, Hull A, Holliday SB, Sullivan P, & Sandbrink F. (2015). Concurrent validity of the defense and veterans pain rating scale in va outpatients. Pain Medicine, 16(11), 2152–2161. doi: 10.1111/pme.12866. [DOI] [PubMed] [Google Scholar]
- Petti E, Scher C, Meador L, Van Cleave JH, & Reid MC (2018). Can multidimensional pain assessment tools help improve pain outcomes in the perianesthesia setting? Journal of PeriAnesthesia Nursing, 33(5), 767–772. doi: 10.1016/j.jopan.2018.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radnovich R, Chapman CR, Gudin JA, Panchal SJ, Webster LR, & Pergolizzi JV (2014). Acute pain: Effective management requires comprehensive assessment. Postgraduate Medicine, 126(4), 59–72. doi: 10.3810/pgm.2014.07.2784. [DOI] [PubMed] [Google Scholar]
- Reid MC, Eccleston C, & Pillemer K. (2015). Management of chronic pain in older adults. BMJ, 350, h532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scher C, Meador L, Van Cleave JH, & Reid MC (2018). Moving beyond pain as the fifth vital sign and patient satisfaction scores to improve pain care in the 21st century. Pain Management Nursing, 19(2), 125–129. doi: 10.1016/j.pmn.2017.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirsch E, Lukas A, Drebenstedt C, Gnass I, Laekeman M, Kopke K, Fischer T, & Guideline Workgroup (Schmerzassessment bei älteren Menschen in der vollstationären Altenhilfe, A. W. MFR−. (2020). Pain assessment for older persons in nursing home care: An evidence-based practice guideline. Journal of American Medical Directors Association, 21(2), 149–163. doi: 10.1016/j.jamda.2019.08.002. [DOI] [PubMed] [Google Scholar]
- Suso-Ribera C, Castilla D, Zaragozá I, Ribera-Canudas MV, Botella C, & GarcíaPalacios A. (2018). Validity, reliability, feasibility, and usefulness of pain monitor: A multidimensional smartphone app for daily monitoring of adults with heterogenous chronic pain. Clinical Journal of Pain, 34(10), 900–908. doi: 10.1097/AJP.0000000000000618. [DOI] [PubMed] [Google Scholar]
- Tan G, Jensen MP, Thornby JI, & Shanti BF (2004). Validation of the Brief Pain Inventory for chronic nonmalignant pain. J Pain, 5(2), 133–137. doi: 10.1016/j.jpain.2003.12.005. [DOI] [PubMed] [Google Scholar]
- Topham D, & Drew D. (2017). Quality improvement project: Replacing the numeric rating scale with a Clinically Aligned Pain Assessment (CAPA) tool. Pain Management Nursing, 18(6), 363–371. doi: 10.1016/j.pmn.2017.07.001. [DOI] [PubMed] [Google Scholar]
- Twining J, & Padula C. (2019). Pilot testing the Clinically Aligned Pain Assessment (CAPA) measure. Pain Management Nursing. doi: 10.1016/j.pmn.2019.02.005. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Veterans Affairs. (2017). VA/DOD clinical practice guidelines: Management of Opioid Therapy (OT) for chronic pain [Google Scholar]
- University of Iowa Csomay Center for Gerontological Excellence. The geriatric pain website. Retrieved from https://geriatricpain.org/ (Accessed 11 December 2019).
- van Boekel RLM, Vissers KCP, van der Sande R, Bronkhorst E, Lerou JGC, & Steegers MAH (2017). Moving beyond pain scores: Multidimensional pain assessment is essential for adequate pain management after surgery. PLoS One, 12(5), e0177345. doi: 10.1371/journal.pone.0177345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, & Initiative S. (2014). The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. International Journal of Surgery, 12(12), 1495–1499. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- Ware JE, & Sherbourne CD (1992). The MOS 36-Item Short-Form Health Survey (sf-36). I. Conceptual framework and item selection. Medical Care, 30(6), 473–483. [PubMed] [Google Scholar]
- Wethington E, Eccleston C, Gay G, Gooberman-Hill R, Schofield P, Bacon E, Dombrowski W, Jamison R, Rothman M, Meador L, Kenien C, Pillemer K, Löckenhoff C, & Reid MC (2018). Establishing a research agenda on mobile health technologies and later-life pain using an evidence-based consensus workshop approach. Journal of Pain, 19(12), 1416–1423. doi: 10.1016/j.jpain.2018.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]