Abstract
Objective.
Persistent post-surgical pain is common among patients undergoing surgery, is detrimental to patients’ quality of life, and can precipitate long-term opioid use. The purpose of this randomized controlled trial is to assess the effects of a behavioral intervention offered prior to surgery for patients at risk for poor post-surgical outcomes, including persistent pain and impaired functioning.
Methods.
Described herein is an ongoing randomized, patient- and assessor-blind, attention-controlled multisite clinical trial. Four hundred and thirty Veterans indicated for total knee arthroplasty (TKA) with distress and/or pain will be recruited for this study. Participants will be randomly assigned to a one-day (~5 hour) Acceptance and Commitment Therapy workshop or one-day education and attention control workshop. Approximately two weeks following their TKA surgery, patients receive an individualized booster session via phone. Following their TKA, patients complete assessments at 1 week, 6 weeks, 3 months, and 6 months.
Results.
The primary outcomes are pain intensity and knee-specific functioning; secondary outcomes are symptoms of distress and coping skills. Mediation analyses will examine whether changes in symptoms of distress and coping skills have an impact on pain and functioning at 6 months in Veterans receiving ACT. This study is conducted mostly with older Veterans; therefore, results may not generalize to women and younger adults who are underrepresented in this veteran population.
Conclusions.
The results of this study will provide the first evidence from a large-scale, patient- and assessor-blind controlled trial on the effectiveness of a brief behavioral intervention for the prevention of persistent post-surgical pain and dysfunction.
Keywords: ACT, mechanisms of change, moderators, efficacy, chronic post-surgical pain, function
Introduction
Persistent post-surgical pain (PPSP) is a common and debilitating problem that impacts a significant number of patients following surgery (1–3). Pain severity up to 12 months following surgery is highly correlated with adverse effects on physical functioning, recovery, and quality of life (3–10). Disabling pain and reduced function also have a dramatic negative impact on mood, daily activities, sleep, cognitive functions, and social life (11, 12). Individuals may become depressed and even consider suicide (13). For patients undergoing total knee arthroplasty (TKA), the prevalence of persistent pain and opioid use is substantial (i.e. 36% of 433 patients reported daily disturbing pain four months or more after TKA (14) and similar rates have been reported up to 7 years following TKA (15)) and PPSP following this surgery impacts both functioning and quality of life (16, 17). Beyond the individual personal costs of persistent pain are the estimated billions of dollars of costs to healthcare systems, as well as costs associated with lost work productivity, including unemployment and disability benefits (18).
Opioid Epidemic and Risk for PPSP
Most notably, PPSP is highly correlated with prolonged opioid use. Opioids are potent acute pain treatments that are readily prescribed following surgery, which serves as an entry point to opioid use for many individuals (19). Between 2008 and 2011, the Total Joint Replacement Registry found 41% of patients who underwent TKA were still using opioids for their knee pain after 90 days (20). Long-term opioid use (≥ 90 days) is not recommended and is, unfortunately, related to increased pain sensitivity over extended periods (21). Recent meta analyses suggest that opioids are ineffective for long-term chronic pain (22). As a result, opioid prescriptions are decreasing nationally (23) due in part to guidelines to reduce their use (24, 25). Indeed, more recent data among veterans shows 26% are using opioids 90 days following TKA (26). In the context of the changes to prescribing patterns and the current opioid epidemic, health care providers are challenged with optimizing postoperative pain management while limiting opioid use after surgery. It is thus imperative that targeted, alternative coping strategies are provided, particularly for those patients at elevated risk for PPSP (27). It is also important to understand how the changes in opioid prescribing patterns are influencing pain management strategies.
Preoperative Pain and Psychological Distress
In recent years, attention has increasingly focused on identifying predictors of PPSP to facilitate early intervention and better pain management. Preoperative pain consistently emerges as an important predictor for the development of PPSP (28). Patients with significant psychological distress (anxiety and/or depression) prior to surgery are also at high risk of having their pain persist after surgery (4, 29–31). Those who screen positive for depression before TKA have significantly higher levels of pain intensity and pain-related distress compared to those who screened negative, and pre-surgery anxiety is the strongest predictor of perceived function at 6 months post-TKA (32). This is not surprising as studies show an important relationship between pain reporting and psychological factors, including anxiety, depression, and catastrophizing (33). Of note, psychological distress is a consistent predictor of prolonged postoperative opioid use (14).
In pilot work, significant correlations were found preoperatively between psychological symptoms (anxiety and depression) and both pain intensity and pain-related distress following TKA (32). Thus, strategies focused on targeting these modifiable risk factors prior to surgery may improve outcomes for surgical patients and are necessary in populations with high levels of pain and distress such as Veterans (34, 35).
Shifting from Treatment to Prevention of PPSP
Current practice does not include psychological interventions specifically aimed at addressing significant pain and/or symptoms of depression and anxiety (distress) prior to surgery. Some institutions have implemented preoperative pain consult services to assist with pain management after surgery in patients expected to have pain control challenges (36). However, most services focus on use of analgesics for improved pain control and do not address the psychological factors influencing persistent pain and impaired functioning (37). There is a need for preoperative interventions to address psychological factors that place individuals at risk for PPSP and impaired functioning after surgery (38).
Acceptance and Commitment Therapy
Acceptance and Commitment Therapy (ACT) is a trans-diagnostic treatment that provides a unified approach for treatment of varied concerns. The goal of ACT is to enhance psychological flexibility by cultivating the six inter-rated skills of acceptance, cognitive defusion, present-moment awareness, values clarification, committed action, and perspective taking. ACT is listed by the American Psychological Association as an evidence-based treatment for depression, chronic pain, mixed anxiety, obsessive-compulsive disorder, and psychosis, and research has consistently shown that ACT-based treatments result in improved functioning and quality of life (39–47).
Beyond its ability to impact several key targets of interest (e.g., depression, pain) within a surgical population, ACT has been successfully delivered in a number of treatment settings, such as primary care clinics (48), and in unique modalities, including 1-day workshops (49, 50). A 1-day workshop is likely more accessible and feasible than weekly treatments for individuals who experience barriers to attending weekly care, including surgical patients who have limited availability between time of the surgery indication and the procedure. A 1-day workshop also ensures treatment adherence and completion, often a significant obstacle to effective mental health care. Finally, this more concentrated and time-limited approach may be more cost-effective.
One-day ACT workshops have produced positive long-term outcomes. In one randomized controlled pilot trial, “at-risk” (i.e. those with high levels of pain or distress) Veterans undergoing TKA who received a 1-day ACT workshop prior to surgery reported greater reduction in average pain from pre-surgery to 3 months post-TKA than the treatment-as-usual (TAU) group. Additionally, fewer Veterans in the ACT group (23%) were taking opioids at 7 weeks post-op than the TAU group (45%) (51). Results were moderated such that Veterans without surgical complications reported greater benefit than Veterans with complications. These results support the feasibility, acceptability and potential efficacy of ACT for pain and opioid outcomes post-TKA in at-risk Veterans.
Current Study
The purpose of this study is to evaluate the efficacy of a brief behavior intervention using Acceptance and Commitment Therapy (ACT), compared to an education plus attention control (AC), to prevent the development of PPSP and dysfunction in Veterans identified to be “at-risk” for poor outcomes following total knee arthroplasty (TKA) and to examine mediators of effects. The specific aims are as follows:
Primary aim: To examine the superior efficacy of ACT versus AC on postoperative pain intensity and functioning.
- Secondary aims:
- To examine the superior efficacy of ACT versus AC on symptoms of distress (anxiety, depression, and stress) and coping skills (pain acceptance, engagement in values-based behavior, and pain catastrophizing).
- Evaluate whether decreases in distress-based symptoms and improvements in coping skills mediate changes in pain and functioning at 6 months in Veterans receiving ACT.
Exploratory aim: Describe the pharmacological and non-pharmacological strategies Veterans are using to manage pain (and their perceived helpfulness) to provide insights into the effects of the current opioid restriction recommendations on pain management strategies.
Method
Study Design
This study is a multi-site, patient- and assessor-blind, two-arm, parallel randomized controlled trial. At-risk Veterans will be randomly assigned to one of two groups: 1) ACT or 2) education plus attention control (AC). Primary and secondary outcomes are measured at 6 weeks, 3 and 6 months following surgery, but 6 months will be the primary outcome endpoint. Pharmacological and non-pharmacological pain management strategies (exploratory outcome) will be collected starting the first week postoperatively. Study procedures have been designed to be consistent with CONSORT guidelines for reporting randomized controlled trials (52).
Setting and Sample
This study is being conducted in two Veterans Affairs Medical Centers (VAMC). The first is in a mid-sized, Midwestern city and projected to enroll 108 Veterans. The second VAMC is in a large, Southern city and projected to enroll 322 Veterans. Target enrollment across the two sites was determined by power analyses described in the Statistical Analyses section below.
Inclusion/Exclusion Criteria
At-risk Veterans scheduled for unilateral total knee arthroplasty (TKA) are being recruited for this study. If veterans do not meet all inclusion and exclusion criteria they are not included in workshops.
Inclusion criteria include: 1) ≥ 18 years old; 2) identified to be “at-risk” at the enrollment visit. At-risk criteria based on one of the following conditions. These cut-offs are based on literature identifying these to be clinically significant levels.
worst pain ≥7/10 (severe pain) on Brief Pain Inventory (BPI) (53)
worst pain 3–6 (moderate to severe pain) on BPI and anxiety symptoms (> 6 on the Anxiety subscale or ≥ 10 on the Stress subscale of the Depression, Anxiety, and Stress Scale (DASS-21)(54).
worst pain 3–6 on BPI and depressive symptoms (≥7 on the Depression subscale of the DASS-21).
worst pain 3–6 on BPI and pain catastrophizing scale score ≥20 (55)
Exclusion criteria include: 1) inability to complete study forms/procedures because of a language/literacy barrier; 2) bipolar or psychotic disorder; 3) history of brain injury; 4) cognitive impairment (determined by score of <4 on MIS-T)(56); 5) ACT therapy within the past year; 6) imminent risk of suicide; 7) surgery is revision of TKA; and 8) inability to attend workshop prior to surgery (as receiving the intervention prior to surgery is needed for it to be a preventive therapy). Receiving ACT within the past year could confound the study results, and therefore those with ACT treatment history withing the past year are excluded. Veterans who have experienced brain injury, have a bipolar or psychotic disorder, or have cognitive impairment are excluded due to perceived inability to concentrate and attend to the ACT intervention. Of note, Veterans with Substance Use Disorder (SUD) and/or Post-Traumatic Stress Disorder (PTSD) are not be excluded due to the high prevalence rates of these psychiatric conditions in this patient population (57). Rather, these factors will be operationalized to determine their potential influences on the efficacy of ACT for the prevention of PPSP and impaired function.
Randomization and Blinding
This study uses cluster randomization where the unit of randomization is the workshops. Randomization occurs at the start of each workshop so that all participants attending that workshop are randomized to the assigned intervention (i.e. ACT vs. AC). This ensures that both assessors and participants are blind to their condition. If a veteran fails to attend the assigned workshop, s/he can attend the next scheduled workshop, assuming it is prior to surgery, without compromising the randomization or blinding. Facilitators are unblinded to condition and protocols are in place to communicate with the team to avoid un-blinding other team members. Additionally, participant and assessor blinding is assessed at the end of data collection. A randomization sequence was generated using PLAN procedure (SAS v9.2) and was stratified by the two VAMCs.
Description of Interventions
Veterans attend either a 1-day group ACT workshop or a 1-day group AC workshop prior to surgery. An AC comparison was selected because it allows for subject blinding, cluster randomization, and exploration of the independent additive effects of ACT components. Each workshop lasts approximately 5 hours, is led by two psychotherapists (see training procedures in Facilitator Preparation, below), and includes 3–12 Veterans, depending on number of veterans indicated for surgery per month at each site.
Two patient workbooks were developed for this study: an ACT workbook and a Pain Education workbook. Patients in the ACT condition receive both workbooks whereas patients in the attention condition receive the Pain Education workbook only. A homework assignment is given at the end of each workshop. ACT homework focuses on implementing a key coping skill whereas the AC homework focuses on information related to pain control. Homework is reviewed two weeks after surgery during an individualized telephone “booster” session with one of the workshop facilitators. A second “booster” call is completed if a participant reports and/or a facilitator determines within 6 weeks of surgery that there are surgical complications, new health problems and/or emotional issues that are affecting recovery or causing significant distress.
Acceptance and Commitment Therapy Workshop.
The goal of the ACT intervention is to cultivate psychological flexibility. This is done by teaching new ways to respond to thoughts and feelings related to pain, depression, and anxiety and encouraging behavioral engagement in meaningful life activities. As such, the ACT intervention includes acceptance and mindfulness training to emphasize new ways of interacting with thoughts, feelings, and physical sensations (e.g., learning how to notice, and disentangle from, unhelpful thoughts). Additionally, Veterans learn how to willingly come into contact with experiences that cannot be altered. Finally, Veterans learn behavioral change training involving a) teaching patients to recognize ineffective patterns of behavior and habits, b) identifying and setting goals related to mental and physical health, and c) promoting committed action to achieve these goals (despite the natural urges to do otherwise and avoid unwanted or troubling sensations and experiences). The workshop also includes a brief review of the TKA surgery and pain control post-TKA consistent with the AC condition (see content below). Both the ACT and Pain Education workbooks are used during the workshop to organize the presentation of content and direct participants to key information and exercises.
Attention Control Workshop.
The primary purpose of the attention control is to provide attention and education to participants to a similar degree as the ACT intervention so the independent additive effects of psychotherapy can be determined in this superiority trial. The group facilitators present one topic at a time for participants to discuss and reflect on issues and experiences related to each topic. Topics of discussion include: a) the pathophysiology of postoperative pain and how it differs from preoperative pain, b) the role of contextual factors (e.g., depressive or anxiety symptoms, expectation) on the experience of pain, d) the role of inflammation in pain and healing, e) types of pain medications and other pain relief strategies following surgery, and f) goals of pain medications. Additionally, deep (diaphragmatic) breathing and passive muscle relaxation exercises are performed at strategic times in the workshop to maintain Veteran engagement. In general, information on coping practices are purposefully omitted with the exception of a brief problem-solving exercise.
Facilitator Preparation.
Prior to facilitating an ACT workshop, facilitators with experience delivering evidence-based psychotherapies are required to read a description of the one-day ACT workshop (58) as well as portions a book describing the ACT Matrix, which is presented during the workshop (59). Next, new facilitators review the ACT facilitator manual and attend an ACT workshop to observe and independently rate fidelity. An established rater and the new facilitator determine level of agreement and discuss disagreements. This process is repeated at subsequent ACT workshops until 90% agreement is achieved between the new facilitator and established rater. Prior to facilitating an AC workshop, facilitators are required to review the AC facilitator manual and attend training with one of the study PIs.
Workshop Fidelity.
A fidelity checklist is completed at the end of 20% of ACT workshops indicating the exercises/content covered. This checklist is reviewed following each workshop to ensure that all basic exercises/content are included. Adjustments are made, if needed, prior to the next workshop.
Measures
We collect demographic information including age, sex, race, ethnicity, marital status, education, and household income. Medical information on smoking, BMI, co-morbidities (including SUD, PTSD, and other chronic pain conditions) and medications for pain and mood are also collected. All measures for primary, secondary, and exploratory aims are described in Table 1.
Table 1:
Outcome Instruments
| Construct | Instrument | General Information | Responses | Scores | Psychometric Properties |
|---|---|---|---|---|---|
| Primary Outcomes | |||||
| Pain Intensity | Pain Severity Subscale of the Brief Pain Inventory Short Form (BPI-SF) (53) | Subjects rate their average pain, worst pain, and least pain in the past 24 hours as well as their current pain; higher score indicates more severe pain | no pain (0) to pain as bad as you can imagine (10) | Total sum score ranges 0 to 40 | High internal consistency among patients undergoing joint replacement surgery (α = 0.91) (66); adequate convergent validity with the Western Ontario and McMaster Universities Osteoarthritis Index pain subscale among patients after joint replacement surgery (r=0.66) (66) |
| Functioning | Activity in Daily Living (ADL) and Quality of Life (QoL) Subscales of the Knee Injury and Osteoarthritis Outcome Score (KOOS) (60) | 17-items assess ADL function and 4-items assess knee-related QOL in the last week in individuals with knee injury and osteoarthritis | no difficulty (0) to extreme difficulty (4); scores are transformed to 0–100 scale | 0 = extreme knee problems to 100 = no knee problems | Good test-retest reliability (ICCADL = 0.89; ICCQOL = 0.84) and internal consistency (αADL = 0.92; αQoL = 0.80) in patients with knee OA; adequate convergent validity with the short form 36 health survey questionnaire physical function subscale in patients with knee OA (rADL = 0.65; rQOL = 0.51) (67) |
| Secondary Outcomes | |||||
| Depressive Symptoms | Depression, Anxiety, and Stress Subscales of the DASS-21 (54) | 7-item self-report subscale measuring the negative emotional state of depression; higher scores indicating more severe symptoms | Did not apply to me at all (0) to applied to me very much (3) | Scores are summed and multiplied by 2 for possible scores on each subscale from 0 to 42 | Internal consistency high in nonpsychiatric sample (αDEP = 0.88, αANX = 0.83, αSTR = 0.85) (68); adequate convergent validity with Affective Distress subscale of the Multidimensional Pain Inventory (rDEP = 0.55, rANX = 0.44, rSTR = 0.61); adequate discriminant validity with Mental Health subscale of the SF-36 in elderly patients with persistent pain (rDEP = −0.67, rANX = −0.50, rSTR = −0.63) (69) |
| Anxious Symptoms | 7-item self-report subscale measuring the negative emotional state of anxiety; higher scores indicating more severe symptoms | ||||
| Pain Acceptance | Chronic Pain Acceptance Questionnaire Revised (CPAQ-R) (70) | 20-items assessing pain acceptance including two subscales: pain willingness (PW; 9 items) and activity engagement (AE; 11 items); higher scores indicate higher level of pain acceptance | Never true (0) to always true (6) | Subscale scores range from 0 to 54 for PW, and 0 to 66 for AE | Good internal consistency among patients with history of chronic pain (αPW = 0.78, αAE = 0.82); adequate discriminant validity with the pain- related anxiety subscale of the Pain Anxiety Symptoms Scale (rPW = −0.63, rAE = −0.51) (70) |
| Engagement in Values-Based Behavior | Chronic Pain Values Inventory (CPVI) (71) | 12-item measure on the importance of value domains and patient’s level of success at living according to each value in the past two weeks; higher Mean Success (MS) and lower Mean Discrepancy (MD) scores indicate greater engagement in value-based behavior | Not at all important (0) to extremely important (5) and not at all successful (0) to extremely successful (5) (72) | Subscales range from 0–5; MS is an average of success ratings. MD is the average difference between importance and success ratings | Good internal consistencies (α = 0.82) for MS and MD subscales among patients with chronic pain; acceptable convergent validities with the activity engagement subscale of the CPAQ for MS and MD subscales in patients with chronic pain (rMS = 0.62, rMD = 0.54) (71) |
| Exploratory Outcomes | |||||
| Pain Management Strategies | Pain Management Strategies Survey (PMSS) (75) | 42-item PMSS assesses the use and perceived helpfulness of medical, complementary, and self-care strategies used to manage pain; it was adapted for this study to include 10 additional items. Participants indicate whether they have used each strategy in the past year (baseline) or since surgery (postop) and whether they are using the strategy currently. | If endorsed, rate strategy’s helpfulness from not at all helpful (0) to extremely helpful (4). Participants are also provided space to add any therapies received for pain beyond what is listed. | Number and type of strategies used, helpfulness scores for each ranging from 0–4. | Established content validity (76); has been found to provide helpful insights regarding pain management strategies in older adults with persistent pain (77) |
Data Collection Procedures
Following approval by the appropriate Institutional Review Boards (IRBs) to ensure compliance with Human Subject Protections, Veterans undergoing unilateral TKA provide written informed consent to participate and complete self-report surveys using an online data entry system (REDCap) in order to identify those who are “at-risk” (using previously described criteria for pain, anxiety, depression, stress, and pain catastrophizing scale). Veterans are also screened for exclusion criteria. Eligible Veterans are then scheduled for a workshop (see Figure 1).
Figure 1:
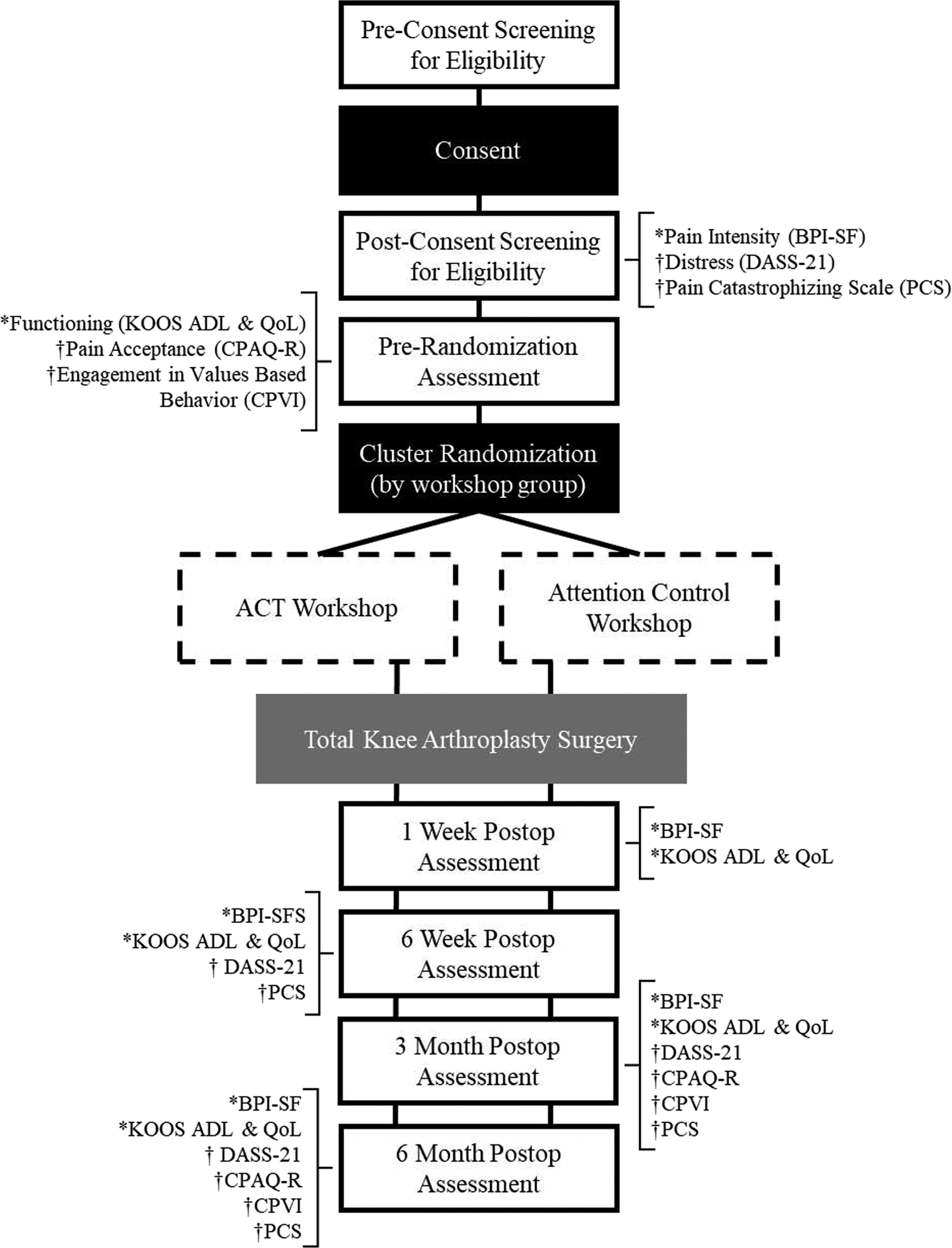
Note: Flowchart for the study showing order and timing of assessments, consent, workshops, and surgery. *Indicates primary outcome measure. †Indicates secondary outcome measure.
At 1 week following surgery, Veterans are sent the BPI and Knee Injury and Osteoarthritis Outcome Score (KOOS) via mail or online using a personalized REDCap link. At 2 weeks following surgery, Veterans receive an individual phone booster session based on their intervention group. At subsequent follow-ups (i.e., 6 weeks, 3 and 6 months), Veterans complete self-report measures on primary, secondary, and exploratory outcomes (see Figure 1). If Veterans do not complete self-report measures, research assistants call and remind them to do so. Veterans who do not have surgery within one year of the workshop complete the same self-report measures and are then discontinued from the study. All Veterans who complete the study are reimbursed for their time.
Data Analyses
Sample Size Justification
Sample size was estimated using the primary outcome requiring the largest sample size to detect a clinically significant difference (KOOS; change of ≥8 points represents a clinically significant improvement) (60). Assuming an average of 6 participants per workshop (cluster), with an intraclass correlation of 0.06 and SD of 18, a sample size of 300 Veterans (n=150 per treatment group) is needed to detect a clinically significant difference at a 0.0167 significance level (adjusted for testing at 3 time points) with 0.80 power. For the other primary outcome of mean change in BPI pain severity (intraclass correlation of 0.01 and SD of 2.0), the detectable difference with sample size of n=150 per treatment group is at least 0.8. Clinically significant reduction in pain for a 0–10 scale is at least 2.0 (61).
Assuming 20% will have surgery cancelled/postponed due to health issues and 10% will drop out after randomization (based off pilot data; (62), we plan to enroll 430 Veterans to ensure that we will have n=150 per treatment group for the primary aim analyses.
Planned Analyses
Descriptive statistics of all variables (including substance use disorder [SUD] and PTSD) will be computed for each intervention group. Any significant differences between the groups will be used as covariates or effect moderators in the comparison of outcome measures between the treatment groups. Intent-to-treat (ITT) analyses will be conducted to assess treatment efficacy on post-operative outcomes using all subjects that are randomized and have surgery performed. The ITT analysis using linear mixed model analysis or applying multiple imputation will include all individuals that have any post-surgical assessments, including those with only immediate post-operative pain but with missing post-surgical follow-up at 6 weeks, 3 months, and 6 months.
For variables in the primary aim (pain severity and functioning), efficacy of ACT compared to AC at 6 weeks, 3 months and 6 months will be tested using linear mixed model analysis for repeated measures. The fixed effect in the model will include intervention group (ACT or AC), time (baseline, 6 weeks, 3 months, 6 months), and intervention*time interaction effect. The model will also include site, workshop (cluster) within intervention, and subject as random effects. Since efficacy of ACT will be assessed at multiple time points, p-values will be adjusted using Bonferroni’s method to account for the multiple tests performed. The same analysis will be used to examine the effect of ACT compared to AC on the secondary outcome measures of anxiety symptoms, depressive symptoms, stress, pain acceptance, engagement in values-based behavior, and pain catastrophizing. Significance level for test of treatment efficacy for each of the primary and secondary outcome measures will be at the 0.05 significance level with Bonferroni correction applied to account for the 3 time points.
For the clinical and demographic variables that are found to differ between the intervention groups, the model will be expanded to include these variables as covariates. In addition, exploratory analysis will be performed to assess for possible moderator effect of each of these variables intervention. This will be done by including an interaction effect of the variable with intervention (i.e. variable*intervention) to the model.
In addition, as a secondary analyses, the same linear mixed model analysis will be performed on the primary and secondary outcome measures that will include all the study participants that attended a workshop regardless of whether they had surgery or not. To differentiate the impact of the intervention between those with and without surgery, the mixed model will include surgery status, and surgery status*treatment interaction as fixed effects.
For the secondary aim, the causal pathway between intervention (ACT or AC) and change in pain intensity (or function) at 6 months as mediated by decreases in anxious and depressive symptoms, stress, and pain catastrophizing as well as increases in acceptance-based coping and engagement in values-based behaviors will be explored. With individuals nested within workshops in this multilevel design, multilevel structural equation modeling, as described by Preacher, Zyphur, and Zhang (63), will be used to estimate and test the direct and indirect effects to assess multilevel mediation. For this analysis, the candidate mediator variables will be defined as change from baseline at 6 weeks and at 3 months in anxious and depressive symptoms, stress, acceptance-based coping, engagement in values-based behaviors, and pain catastrophizing. For the exploratory aim, frequencies for each pharmacologic and non-pharmacologic pain management strategy will be calculated to describe the types of strategies reported at each visit. Patterns (from baseline to 6 months) and trends (i.e. changes over the 4 year data collection period) will be examined. Differences in types and helpfulness of pain management strategies by treatment group will be explored.
Missing Data
In the case of subject drop-out, reasons for subject drop-out will be recorded and compared between treatment groups. Subject characteristics and outcome measures collected prior to drop-out for those that drop-out will be compared to those that complete the study. In the presence of missing data, under the assumption of missing at random (MAR), the proposed analysis of the primary outcome measure using linear mixed model analysis which can handle incompletely observed subjects and uses likelihood estimation method will provide correct likelihoods and lead to valid estimates (64). However, since it is difficult to ascertain if data are MAR or missing not at random (MNAR), sensitivity analysis will also be performed. Missing data patterns will be examined to assess for possible association of dropout with outcome that may suggest data to be MNAR, and how such patterns differ between intervention groups will determine the sensitivity adjustment that will be used. Methods for sensitivity analysis such as marginal delta adjustment, conditional delta adjustment, reference-based controlled imputation, and other pattern mixture models will be considered (65).
Funding source/registration
This study was funded by grant #1R01NR017610–01A1 by the National Institutes of Health. This study was preregistered at clinicaltrials.gov (#201812794).
Discussion
This study seeks to build on the promising results from a pilot study testing the one-day ACT workshop for PPSP in ‘at-risk’ Veterans undergoing TKA. Specifically, this project leverages longitudinal, multi-site, randomized, controlled methodology to provide innovative data that could fundamentally alter the landscape of PPSP. Moreover, this project has the potential to translate what is known about effective treatments for chronic pain into a group-based, cost effective program to prevent poor surgical outcomes. Using behavioral techniques to intervene prior to surgery on psychological distress and pain management is a novel, non-pharmaceutical approach to decreasing PPSP. Further, the interdisciplinary approach partnering with surgeons and nurses in the care of Veterans attends to major risk factors of postoperative sequelae. This study has the potential to significantly impact Veterans’ quality of life and healthcare utilization following TKA.
If proven efficacious, results from this randomized controlled trial may inform future dissemination efforts to include preoperative workshops as a standard of care for “at-risk” Veterans and potentially all individuals undergoing TKA. Depending on the results of the present trial, either the AC and/or the ACT workshop may be disseminated. Should results be indistinguishable between conditions, the AC workshop may be easier to teach to less experienced facilitators than the ACT workshop, which requires facilitators who have extensive training in psychotherapy to deliver. Should effects of the ACT workshop be superior, this may assist organizations to leverage the one-day group format to optimally utilize trained psychotherapists in a cost-effective modality with demonstrated empirical support. Ultimately, an effective, highly accepted, and deployable intervention would be clinically useful for this and other conditions that can lead to long-term opioid use and chronic pain.
Strengths
This study has several strengths. First, this study aims to prevent PPSP which is an innovative approach to the problem of chronic pain. Second, partnering with the orthopedic surgical team and implementing the workshops at large medical centers is a novel setting to deliver preventative psychological interventions. We have developed and refined both training materials for therapists and companion patient materials, which will allow these workshops to be readily disseminated to interested groups. Third, the multisite trial from large Southern and mid-sized Midwestern cities allows for a diverse patient sample in terms of socioeconomic, racial/ethnic, and rural/urban factors. Thus, we believe the results from this trial will be readily generalizable to a large population of post-surgical individuals. Finally, the large sample size powers the study to detect differences between the two active groups being tested as well as tests for mediators and moderators of effects. Identification of mediators and moderators serves to further clarify active components of change and adapt future interventions accordingly.
Limitations
This study is conducted within an older, primarily male Veteran population. Thus, our power to detect effects among younger Veterans and female Veterans may be limited. As a result, findings here may not generalize to all civilians. Finally, all measures are self-report; conclusions would be strengthened by the inclusion of other data sources such as clinical interviews and physiological or performance-based functional data.
Conclusions
Preventing post-surgical pain and dysfunction by implementing a behavioral intervention focusing on modifiable factors prior to surgery is a novel strategy. This work has the potential to positively impact patient care as well as increase our understanding of how and for whom these interventions are most effective.
Funding:
This work was made possible by grant number 1 R01 NR017610-01 from the National Institutes of Health awarded to Barbara Rakel and Lilian N. Dindo. It is also partially supported by the use and resources of the Houston VA HSR&D Center for Innovations in Quality, Effectiveness and Safety (CIN13-413). The funding agency does not play a role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication. The opinions expressed reflect those of the authors and not necessarily those of the US government, the University of Iowa, the Department of Veterans Affairs, or Baylor College of Medicine.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: None
References
- 1.Macrae WA. Chronic post-surgical pain: 10 years on. Br J Anaesth. 2008;101(1):77–86. [DOI] [PubMed] [Google Scholar]
- 2.Chapman CR, Vierck CJ. The Transition of Acute Postoperative Pain to Chronic Pain: An Integrative Overview of Research on Mechanisms. The journal of pain : official journal of the American Pain Society. 2017;18(4):359 e1–e38. [DOI] [PubMed] [Google Scholar]
- 3.Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res 2017;10:2287–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh JA, Lewallen DG. Predictors of use of pain medications for persistent knee pain after primary Total Knee Arthroplasty: a cohort study using an institutional joint registry. Arthritis Res Ther. 2012;14(6):R248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patton CM, Hung M, Lawrence BD, Patel AA, Woodbury AM, Brodke DS, et al. Psychological distress in a Department of Veterans Affairs spine patient population. Spine J. 2012;12(9):798–803. [DOI] [PubMed] [Google Scholar]
- 6.Otis JD, Keane TM, Kerns RD, Monson C, Scioli E. The development of an integrated treatment for veterans with comorbid chronic pain and posttraumatic stress disorder. Pain Med. 2009;10(7):1300–11. [DOI] [PubMed] [Google Scholar]
- 7.Riddle DL. Prevalence and Predictors of Symptom Resolution and Functional Restoration in the Index Knee Following Knee Arthroplasty: A Longitudinal Study. Archives of physical medicine and rehabilitation. 2018. [DOI] [PubMed] [Google Scholar]
- 8.Biswas A, Perlas A, Ghosh M, Chin K, Niazi A, Pandher B, et al. Relative Contributions of Adductor Canal Block and Intrathecal Morphine to Analgesia and Functional Recovery After Total Knee Arthroplasty: A Randomized Controlled Trial. Regional anesthesia and pain medicine. 2018;43(2):154–60. [DOI] [PubMed] [Google Scholar]
- 9.Veal FC, Bereznicki LR, Thompson AJ, Peterson GM, Orlikowski C. Subacute Pain as a Predictor of Long-Term Pain Following Orthopedic Surgery: An Australian Prospective 12 Month Observational Cohort Study. Medicine (Baltimore). 2015;94(36):e1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoofwijk DM, Fiddelers AA, Emans PJ, Joosten EA, Gramke HF, Marcus MA, et al. Prevalence and Predictive Factors of Chronic Postsurgical Pain and Global Surgical Recovery 1 Year After Outpatient Knee Arthroscopy: A Prospective Cohort Study. Medicine (Baltimore). 2015;94(45):e2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Caffo O, Amichetti M, Ferro A, Lucenti A, Valduga F, Galligioni E. Pain and quality of life after surgery for breast cancer. Breast Cancer Res Treat. 2003;80(1):39–48. [DOI] [PubMed] [Google Scholar]
- 12.von Sperling ML, Hoimyr H, Finnerup K, Jensen TS, Finnerup NB. Persistent pain and sensory changes following cosmetic breast augmentation. European journal of pain. 2011;15(3):328–32. [DOI] [PubMed] [Google Scholar]
- 13.Abyholm AS, Hjortdahl P. [The pain takes hold of life. A qualitative study of how patients with chronic back pain experience and cope with their life situation]. Tidsskr Nor Laegeforen. 1999;119(11):1624–9. [PubMed] [Google Scholar]
- 14.Puolakka PA, Rorarius MG, Roviola M, Puolakka TJ, Nordhausen K, Lindgren L. Persistent pain following knee arthroplasty. Eur J Anaesthesiol. 2010;27(5):455–60. [DOI] [PubMed] [Google Scholar]
- 15.Hawker GA, Badley EM, Croxford R, Coyte PC, Glazier RH, Guan J, et al. A population-based nested case-control study of the costs of hip and knee replacement surgery. Med Care. 2009;47(7):732–41. [DOI] [PubMed] [Google Scholar]
- 16.Rakel BA, Zimmerman MB, Geasland K, Embree J, Clark CR, Noiseux NO, et al. Transcutaneous electrical nerve stimulation for the control of pain during rehabilitation after total knee arthroplasty: A randomized, blinded, placebo-controlled trial. Pain. 2014;155(12):2599–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hadlandsmyth K, Zimmerman MB, Wajid R, Sluka KA, Herr K, Clark CR, et al. Longitudinal Postoperative Course of Pain and Dysfunction Following Total Knee Arthroplasty. The Clinical journal of pain. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kerns RD, Sellinger J, Goodin BR. Psychological treatment of chronic pain. Annu Rev Clin Psychol. 2011;7:411–34. [DOI] [PubMed] [Google Scholar]
- 19.Brummett CM, Waljee JF, Goesling J, Moser S, Lin P, Englesbe MJ, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA surgery. 2017;152(6):e170504–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Namba RS, Inacio MCS, Pratt NL, Graves SE, Roughead EE, Paxton EW. Persistent Opioid Use Following Total Knee Arthroplasty: A Signal for Close Surveillance. J Arthroplasty. 2018;33(2):331–6. [DOI] [PubMed] [Google Scholar]
- 21.Fletcher D, Martinez V. Opioid-induced hyperalgesia in patients after surgery: a systematic review and a meta-analysis. British Journal of Anaesthesia. 2014;112(6):991–1004. [DOI] [PubMed] [Google Scholar]
- 22.Noble M, Tregear SJ, Treadwell JR, Schoelles K. Long-term opioid therapy for chronic noncancer pain: a systematic review and meta-analysis of efficacy and safety. Journal of pain and symptom management. 2008;35(2):214–28. [DOI] [PubMed] [Google Scholar]
- 23.Guy GP Jr, Zhang K, Bohm MK, Losby J, Lewis B, Young R, et al. Vital signs: changes in opioid prescribing in the United States, 2006–2015. MMWR Morbidity and mortality weekly report. 2017;66(26):697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Howard R, Waljee J, Brummett C, Englesbe M, Lee J. Reduction in opioid prescribing through evidence-based prescribing guidelines. JAMA surgery. 2018;153(3):285–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Workgroup TOTfCP. VA/DoD Clinical Practice Guildelines for Opioid Therapy for Chronic Pain. In: Affairs DoV, Defense Do, editors. Washington, DC: 2017. [Google Scholar]
- 26.Hadlandsmyth K, Vander Weg MW, McCoy KD, Mosher HJ, Vaughan-Sarrazin MS, Lund BC. Risk for prolonged opioid use following total knee arthroplasty in veterans. The Journal of arthroplasty. 2018;33(1):119–23. [DOI] [PubMed] [Google Scholar]
- 27.Hah JM, Bateman BT, Ratliff J, Curtin C, Sun E. Chronic Opioid Use After Surgery: Implications for Perioperative Management in the Face of the Opioid Epidemic. Anesth Analg. 2017;125(5):1733–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pinto PR, McIntyre T, Ferrero R, Almeida A, Araújo-Soares V. Risk factors for moderate and severe persistent pain in patients undergoing total knee and hip arthroplasty: a prospective predictive study. PloS one. 2013;8(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McCracken LM, Gutierrez-Martinez O. Processes of change in psychological flexibility in an interdisciplinary group-based treatment for chronic pain based on Acceptance and Commitment Therapy. Behav Res Ther. 2011;49(4):267–74. [DOI] [PubMed] [Google Scholar]
- 30.Edwards RR, Haythornthwaite JA, Smith MT, Klick B, Katz JN. Catastrophizing and depressive symptoms as prospective predictors of outcomes following total knee replacement. Pain Res Manag. 2009;14(4):307–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Masselin-Dubois A, Attal N, Fletcher D, Jayr C, Albi A, Fermanian J, et al. Are psychological predictors of chronic postsurgical pain dependent on the surgical model? A comparison of total knee arthroplasty and breast surgery for cancer. The journal of pain : official journal of the American Pain Society. 2013;14(8):854–64. [DOI] [PubMed] [Google Scholar]
- 32.Hadlandsmyth K, Sabic E, Zimmerman MB, Sluka KA, Herr KA, Clark CR, et al. Relationships among pain intensity, pain-related distress, and psychological distress in pre-surgical total knee arthroplasty patients: a secondary analysis. Psychol Health Med. 2017;22(5):552–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sullivan M, Tanzer M, Stanish W, Fallaha M, Keefe FJ, Simmonds M, et al. Psychological determinants of problematic outcomes following Total Knee Arthroplasty. Pain. 2009;143(1–2):123–9. [DOI] [PubMed] [Google Scholar]
- 34.Sareen J, Cox BJ, Afifi TO, Stein MB, Belik SL, Meadows G, et al. Combat and peacekeeping operations in relation to prevalence of mental disorders and perceived need for mental health care: findings from a large representative sample of military personnel. Arch Gen Psychiatry. 2007;64(7):843–52. [DOI] [PubMed] [Google Scholar]
- 35.Substance Abuse and Mental Health Services Administration:Results from the 2007 National Survey of Drug Use and Health. Major Depressive Episode and Treatment fpr Depression among Veterans Aged 21 t0 39. 2013. [Available from: http://oas.samhsa.gov/2k8/veteransDepressed/veteransDepressed.htm. [Google Scholar]
- 36.Katz J, Weinrib A, Fashler SR, Katznelzon R, Shah BR, Ladak SS, et al. The Toronto General Hospital Transitional Pain Service: development and implementation of a multidisciplinary program to prevent chronic postsurgical pain. J Pain Res. 2015;8:695–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weinrib AZ, Azam MA, Birnie KA, Burns LC, Clarke H, Katz J. The psychology of chronic post-surgical pain: new frontiers in risk factor identification, prevention and management. Br J Pain 2017;11(4):169–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cooper NA, Rakel BA, Zimmerman B, Tonelli SM, Herr KA, Clark CR, et al. Predictors of multidimensional functional outcomes after total knee arthroplasty. J Orthop Res. 2017;35(12):2790–8. [DOI] [PubMed] [Google Scholar]
- 39.Dimidjian S, Arch JJ, Schneider RL, Desormeau P, Felder JN, Segal ZV. Considering Meta-Analysis, Meaning, and Metaphor: A Systematic Review and Critical Examination of “Third Wave” Cognitive and Behavioral Therapies. Behav Ther. 2016;47(6):886–905. [DOI] [PubMed] [Google Scholar]
- 40.Ruiz F A Review of Acceptance and Commitment Therapy (ACT) Empirical Evidence: Correlational, Experimental Psychopathology, Component and Outcome Studies. International Journal of Psychology and Psychological Therapy. 2010;10(1):125–62. [Google Scholar]
- 41.Hayes SC, Levin ME, Plumb-Vilardaga J, Villatte JL, Pistorello J. Acceptance and commitment therapy and contextual behavioral science: examining the progress of a distinctive model of behavioral and cognitive therapy. Behav Ther. 2013;44(2):180–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gregg JA, Callaghan GM, Hayes SC, Glenn-Lawson JL. Improving diabetes self-management through acceptance, mindfulness, and values: a randomized controlled trial. J Consult Clin Psychol. 2007;75(2):336–43. [DOI] [PubMed] [Google Scholar]
- 43.Dahl J, Wilson KG, Nilsson A. Acceptance and commitment therapy and the treatment of persons at risk for long-term disability resulting from stress and pain symptoms: A preliminary randomized trial. Behavior therapy. 2004;35(4):785–801. [Google Scholar]
- 44.Lillis J, Hayes SC, Bunting K, Masuda A. Teaching acceptance and mindfulness to improve the lives of the obese: a preliminary test of a theoretical model. Ann Behav Med. 2009;37(1):58–69. [DOI] [PubMed] [Google Scholar]
- 45.Lundgren T, Dahl J, Melin L, Kies B. Evaluation of acceptance and commitment therapy for drug refractory epilepsy: a randomized controlled trial in South Africa--a pilot study. Epilepsia. 2006;47(12):2173–9. [DOI] [PubMed] [Google Scholar]
- 46.Bach P, Hayes SC. The use of acceptance and commitment therapy to prevent the rehospitalization of psychotic patients: a randomized controlled trial. J Consult Clin Psychol. 2002;70(5):1129–39. [DOI] [PubMed] [Google Scholar]
- 47.Graham CD, Gouick J, Krahe C, Gillanders D. A systematic review of the use of Acceptance and Commitment Therapy (ACT) in chronic disease and long-term conditions. Clin Psychol Rev. 2016;46:46–58. [DOI] [PubMed] [Google Scholar]
- 48.Robinson PJ, Strosahl KD. Behavioral health consultation and primary care: Lessons learned. Journal of Clinical Psychology in Medical Settings. 2009;16(1):58–71. [DOI] [PubMed] [Google Scholar]
- 49.Huddleston C, Martin L, Woods K, Dindo L. One-Day Behavioral Intervention for Distressed Veterans with Migraine: Results of a Multimethod Pilot Study. Mil Med. 2018. [DOI] [PubMed] [Google Scholar]
- 50.Hou JK, Vanga RR, Thakur E, Gonzalez I, Willis D, Dindo L. One-Day Behavioral Intervention for Patients With Inflammatory Bowel Disease and Co-Occurring Psychological Distress. Clinical Gastroenterology and Hepatology. 2017;15(10):1633–4. [DOI] [PubMed] [Google Scholar]
- 51.Dindo L, Zimmerman M, Hadlandsmyth K, Marie B St., Embree J, Marchman J, et al. Acceptance and Committment Therapy for Prevention of Persistent Post-surgical Pain and Opioid Use in At-Risk Veterans: A Pilot Randomized Controlled Study. Submitted to Journal of Pain. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Moher D, Schulz KF, Altman D, Group C. The CONSORT Statement: revised recommendations for improving the quality of reports of parallel-group randomized trials 2001. Explore. 2005;1(1):40–5. [DOI] [PubMed] [Google Scholar]
- 53.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23(2):129–38. [PubMed] [Google Scholar]
- 54.Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33(3):335–43. [DOI] [PubMed] [Google Scholar]
- 55.Sullivan MJ. The pain catastrophizing scale: user manual. Montreal: McGill University. 2009:1–36. [Google Scholar]
- 56.Lipton RB, Katz MJ, Kuslansky G, Sliwinski MJ, Stewart WF, Verghese J, et al. Screening for dementia by telephone using the memory impairment screen. Journal of the American Geriatrics Society. 2003;51(10):1382–90. [DOI] [PubMed] [Google Scholar]
- 57.Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, Ren L. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug Alcohol Depend. 2011;116(1–3):93–101. [DOI] [PubMed] [Google Scholar]
- 58.Dindo L, Weinrib AZ, Marchman JN. One-Day ACT Workshops for Patients with Chronic Health Problems and Associated Emotional Disorders. Recent Innovations in ACTIn press. [Google Scholar]
- 59.Polk KL, Schoendorff B, Webster M, Olaz FO. The essential guide to the ACT Matrix: A step-by-step approach to using the ACT Matrix model in clinical practice: New Harbinger Publications; 2016. [Google Scholar]
- 60.Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Suzuki H, Aono S, Inoue S, Imajo Y, Nishida N, Funaba M, et al. Clinically significant changes in pain along the Pain Intensity Numerical Rating Scale in patients with chronic low back pain. PLoS One. 2020;15(3):e0229228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dindo L, Zimmerman MB, Hadlandsmyth K, StMarie B, Embree J, Marchman J, et al. Acceptance and Commitment Therapy for Prevention of Chronic Postsurgical Pain and Opioid Use in At-Risk Veterans: A Pilot Randomized Controlled Study. J Pain. 2018;19(10):1211–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Preacher KJ, Zyphur MJ, Zhang Z. A general multilevel SEM framework for assessing multilevel mediation. Psychol Methods. 2010;15(3):209–33. [DOI] [PubMed] [Google Scholar]
- 64.Molenberghs HaK MG. Missing Data in Clinical Studies. West Sussex, England: John Wiley & Sons, Ltd; 2007. [Google Scholar]
- 65.Carpenter JaK MG. Multiple Imputation and its Application. West Sussex, England: John Wiley & Sons, Ltd; 2013. [Google Scholar]
- 66.Kapstad H, Rokne B, Stavem K. Psychometric properties of the Brief Pain Inventory among patients with osteoarthritis undergoing total hip replacement surgery. Health Qual Life Outcomes. 2010;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Collins NJ, Prinsen CA, Christensen R, Bartels EM, Terwee CB, Roos EM. Knee Injury and Osteoarthritis Outcome Score (KOOS): systematic review and meta-analysis of measurement properties. Osteoarthritis Cartilage. 2016;24(8):1317–29. [DOI] [PubMed] [Google Scholar]
- 68.Osman A, Wong JL, Bagge CL, Freedenthal S, Gutierrez PM, Lozano G. The Depression Anxiety Stress Scales-21 (DASS-21): further examination of dimensions, scale reliability, and correlates. J Clin Psychol. 2012;68(12):1322–38. [DOI] [PubMed] [Google Scholar]
- 69.Wood BM, Nicholas MK, Blyth F, Asghari A, Gibson S. The utility of the short version of the Depression Anxiety Stress Scales (DASS-21) in elderly patients with persistent pain: does age make a difference? Pain Medicine. 2010;11(12):1780–90. [DOI] [PubMed] [Google Scholar]
- 70.McCracken LM, Vowles KE, Eccleston C. Acceptance of chronic pain: component analysis and a revised assessment method. Pain. 2004;107(1–2):159–66. [DOI] [PubMed] [Google Scholar]
- 71.McCracken LM, Yang SY. The role of values in a contextual cognitive-behavioral approach to chronic pain. Pain. 2006;123(1–2):137–45. [DOI] [PubMed] [Google Scholar]
- 72.McCracken LM, Vowles KE. A prospective analysis of acceptance of pain and values-based action in patients with chronic pain. Health Psychol. 2008;27(2):215–20. [DOI] [PubMed] [Google Scholar]
- 73.Sullivan MJ, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychological assessment. 1995;7(4):524. [Google Scholar]
- 74.Sullivan M, Tanzer M, Stanish W, Fallaha M, Keefe FJ, Simmonds M, et al. Psychological determinants of problematic outcomes following total knee arthroplasty. Pain. 2009;143(1–2):123–9. [DOI] [PubMed] [Google Scholar]
- 75.Kemp CA, Ersek M, Turner JA. A descriptive study of older adults with persistent pain: use and perceived effectiveness of pain management strategies [ISRCTN11899548]. BMC Geriatr. 2005;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kung F, Gibson SJ, Helme RD. Development of a pain management strategies survey questionnaire-preliminary findings. The Pain Clinic. 2000;12(4):299–315. [Google Scholar]
- 77.Kemp CA, Ersek M, Turner JA. A descriptive study of older adults with persistent pain: Use and perceived effectiveness of pain management strategies [ISRCTN11899548]. BMC geriatrics. 2005;5(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]


