Abstract
Purpose
It is a challenge to evaluate the maintenance of medial and lateral soft tissue balance in total knee arthroplasty (TKA). This study aimed to determine the “isoheight” points and the “isoheight” axis (IHA) that can measure constant medial/lateral condyle heights during flexion of the knee, and compare the IHA with two major anatomical axes, the transepicondylar axis (TEA) and the geometric center axis (GCA).
Methods
Twenty-two healthy human knees were imaged using a combined MRI and dual fluoroscopic imaging system while performing a single-legged lunge (0°−120°). The isoheight points of the medial and lateral femoral condyles were defined as the locations with the least amount of changes in heights during the knee flexion; an IHA is the line connecting the medial and lateral isoheight points. The measured changes of the condyle heights using the IHA were compared with those measured using the TEA and GCA.
Results
Overall, the IHA was posterior and distal to the TEA, and anterior to the GCA. The isoheight points measured condyle height changes within 1.2±2.3 mm at the medial and 0.7±3.3 mm at the lateral sides during the knee flexion. Between 0° to 45°, the condyle height changes measured using the GCA (medial: 3.0±1.8 mm, lateral: 2.3±2.0 mm) were significantly larger than those of the IHA and the TEA (p<0.05). Between 90° to 120°, the changes of the condyle heights measured using the TEA (medial: 5.3±1.8 mm, lateral: 3.3±1.8 mm) were significantly larger than those of the IHA and GCA (p<0.05).
Conclusion
There are isoheight points in the medial and lateral femoral condyles that can measure constant heights along the full range of knee flexion and could be used to formulate an “isoheight” axis (IHA) of the femur. The condyle height changes measured by the TEA and GCA were greater than the IHA measurements along the flexion path. These data could be used as a valuable reference to evaluate the condyle height changes after TKA surgeries and help achieve soft tissue balance and optimal knee kinematics along the flexion path.
Level of Evidence
Level IV
Keywords: In vivo knee flexion, Femoral condyle heights, isoheight characteristics, Total knee arthroplasty, Soft tissue balance, Gap balance
Introduction
Over 20% of total knee arthroplasty (TKA) patients were reported unsatisfied with the surgery in follow up studies [3, 25]. Imbalance of the soft tissues has been acknowledged as an important factor affecting the clinical outcomes [15, 22]. Precise bony resection and correct implant positioning have been investigated to improve the gap balancing [19, 20]. Recent studies have reported that contemporary TKAs could not maintain gap balance in the full range flexion of the knee [6, 22].
Elongations of the medial and lateral soft tissues change along the knee flexion path [6, 13, 16, 31]. A proximal shift of the femoral condyle could cause excessive tissue stretch and reduced knee flexion [14], while a distal shift of the condyle could result in soft tissue laxity and joint instability [6, 33]. Therefore, maintenance of the physiological heights of the medial and lateral condyles is critical to maintain the soft tissue balance during the knee flexion [30, 32]. Different reference axes to evaluate the changes of the condyle heights during knee flexion have been widely discussed [4, 5, 7, 23, 29], including the transepicondylar axis (TEA) and geometric center axis (GCA) [1, 4, 7, 23, 26]. Both TEA and GCA measured uneven condyle heights along the knee flexion path [23, 27], indicating their limitations as reference axes to guide medial and lateral soft tissue balancing in TKA surgery. No study has reported whether there is a reference axis in the femur that could measure the constant condyle heights along the flexion path of the knee. This information is necessary for establishing biomechanical references to preserve the soft tissue tensions of the knee after TKAs [5].
The purpose of this study was to determine the isoheight points in the medial and lateral femoral condyles that can maintain constant heights along the knee flexion path and to formulate an “isoheight” axis (IHA) of the femur. We specifically compared the femoral condyle heights measured using the IHA with those measured using the conventional TEA and GCA axes during an in vivo weight-bearing flexion of the knee. It was hypothesized that there are isoheight points in the medial and lateral femoral condyles that can maintain constant condyle heights along the full range flexion of the knee.
Materials and Methods
Participants
This study was approved by our institutional review board (protocol number: 2003P000337/PHS). Written consent was obtained from each subject prior to participating in this study. Twenty-two healthy knees in 22 subjects were included (16 men and 6 women; age: 33±13 years; BMI: 25.5±3.5 kg/m2; 9 left and 13 right). Standard examination was performed on each knee, including the Lachman and anterior drawer test. The exclusion criteria included pain, previous injury, and previous surgery of the studied knee. MRI images of the knee was assessed further for exclusion if there were meniscal tears, chondral defects, and ligamentous injuries.
Imaging and 3D modeling of knees
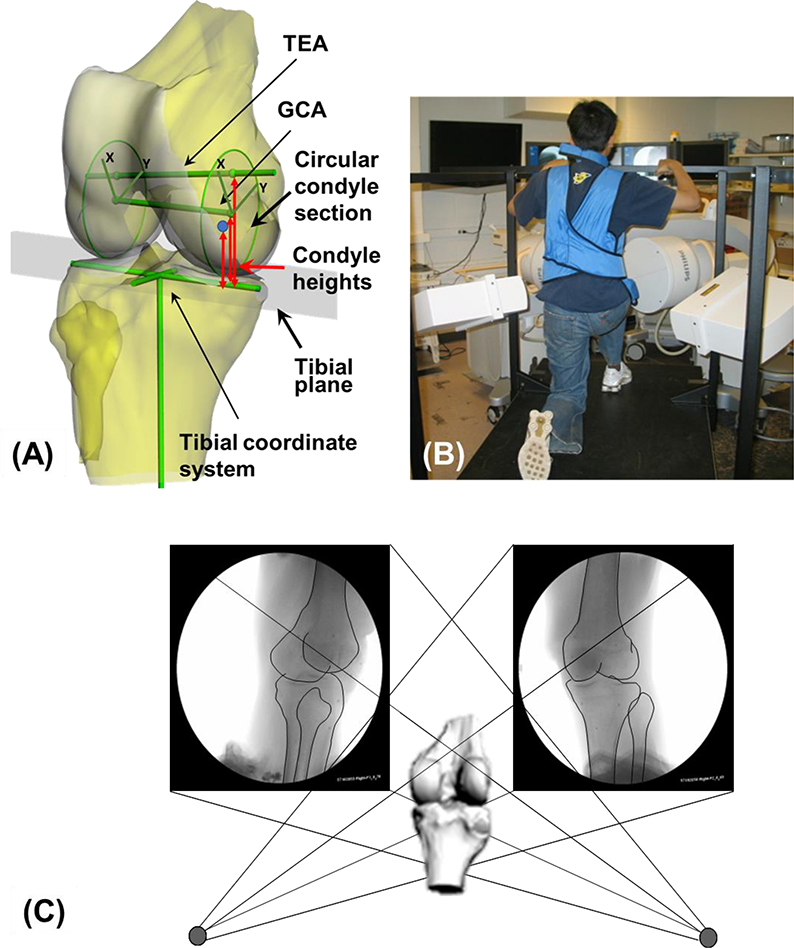
Each knee was imaged using a 3.0-Tesla MRI scanner (Siemens, Erlangen, Germany) [6, 17]. The images were used to construct three-dimensional (3D) surface models of the femur and tibia in a solid modeling software (Rhinoceros; Robert McNeel and Associates, Seattle, WA) (Fig. 1A). The subject then performed a quasi-static single-legged lunge at approximately 0°, 30°, 60°, 75°, 90°, 105°, and 120° of flexion and imaged using two fluoroscopes (BV Pulsera; Philips, Bothell, WA) (Fig. 1B). The fluoroscopic images and the 3D bony models of the femur and tibia were imported into a virtual environment (Fig. 1C) in the solid modeling software that replicated the actual dual fluoroscopic image system [6, 16, 17]. The bony outlines were extracted from the fluoroscopic images. The projections of the 3D femoral and tibial models were matched to their corresponding outlines on the fluoroscopic images to reproduce the in vivo knee positions (Fig. 1C). The relative positions/orientations of the femoral and tibial models were used to represent the tibiofemoral joint at each flexion angle. This technique has been rigorously validated with an error less than 0.1mm and 0.3° in measurements of the tibiofemoral joint translations and rotations, respectively [17].
Fig. 1.
(A) The 3D knee joint model with tibial Cartesian coordinate system, the transepicondylar axis (TEA) and the geometrical center axis (GCA), the sagittal plane circular sections of the medial and lateral femoral condyles (including local coordinate systems on the circular sections). Measurements of femoral condyle heights with respect to the tibial cutting plane were also shown. (B) A subject performing a quasi-static single-legged lunge, which was captured the dual fluoroscopic system. (C) A virtual dual fluoroscopic system used for reproduction of the in vivo knee positions along the flexion path.
Definition of TEA and GCA
The TEA was defined as the line that connects the most prominent points of the medial and lateral epicondyles (Fig. 1A) [1, 4, 24]. The midpoint of the axis was identified as the knee joint center. The femoral long axis was defined along the femoral shaft and passed through the center point. The femoral anterior-posterior axis was perpendicular to the two axes. To construct the GCA, two co-axial cylinders were constructed using the posterior geometries of the medial and lateral femoral condyles (Fig. 1A) [7, 24]. Two sagittal vertical cross-sections of the cylinders were determined at the largest radii of the two posterior femoral condyles of the knee. The centers of the two circular sections were defined as the geometric centers of the medial and lateral femoral condyles [16, 24]; the line connecting both the geometric centers was defined as the GCA axis. A Cartesian coordinate system was established on each circular section with its origin located at the geometric center. The proximal-distal axis was selected parallel to the longitudinal axis of the femur. The anterior-posterior axis was perpendicular to the proximal-distal axis in the circular section. The intersection points of the TEA axis on the two circular sections were used to measure the TEA motion when compared to those measured using the GCA.
Definition of isoheight points and IHA
As presented in Fig. 1A, a tibial coordinate system was created. The tibial long axis (z-axis) was parallel to the posterior wall of the tibial shaft [16, 24]. The medial-lateral axis (x-axis) was defined as a line connecting the centroids of the two circles fitting the medial and lateral tibial plateau surfaces [16, 24]. The anterior-posterior axis (y-axis) was perpendicular to the other two axes. For measurements of the condyle heights, a plane was created to fit the tibial plateau surface of each knee to represent a tibial cutting plane during TKA (Fig. 1A).
To determine the isoheight points, both the medial and lateral circular sections were evenly discretized using 8000 points. The position of each point was measured using the corresponding Cartesian coordinate system on the circular section (Fig. 1A). The heights of each point in the full range of knee flexion were calculated as the vertical distances between the reference points and the tibial plane [6]. It should be noted that the measured heights depended on the positions and orientations of the femur at each moment during knee flexion. The change of the condyle height measured at each reference point was defined as the difference between the maximal and minimal heights in the full range of flexion. A heat map was generated on each circular section to provide a visual representation of the changes of the condyle height of each reference point on the femoral condyle. The isoheight point corresponded to the reference point which had the least vertical condyle height change along the flexion path. The IHA was defined as the line connecting the medial and lateral isoheight points. For comparison, the condyle heights were also measured at each selected knee flexion angle using the TEA and GCA [6].
Statistical analysis
A repeated measure analysis of Variance (ANOVA) was used to analyze the condyle heights of the same reference point and differences between different points along the flexion path. Independent variables were the flexion angles (0°, 45°, 90° and 120°) and flexion ranges (0°−45°, 45°−90°, 90°−120°). The dependent variables were femoral condyle heights and height variations. A statistically significant difference was determined when p<0.05. A post-test power analysis indicated that 15 subjects could provide over 95% power to detect the condyle height changes along the flexion path.
Results
Positions of the isoheight points and the IHA
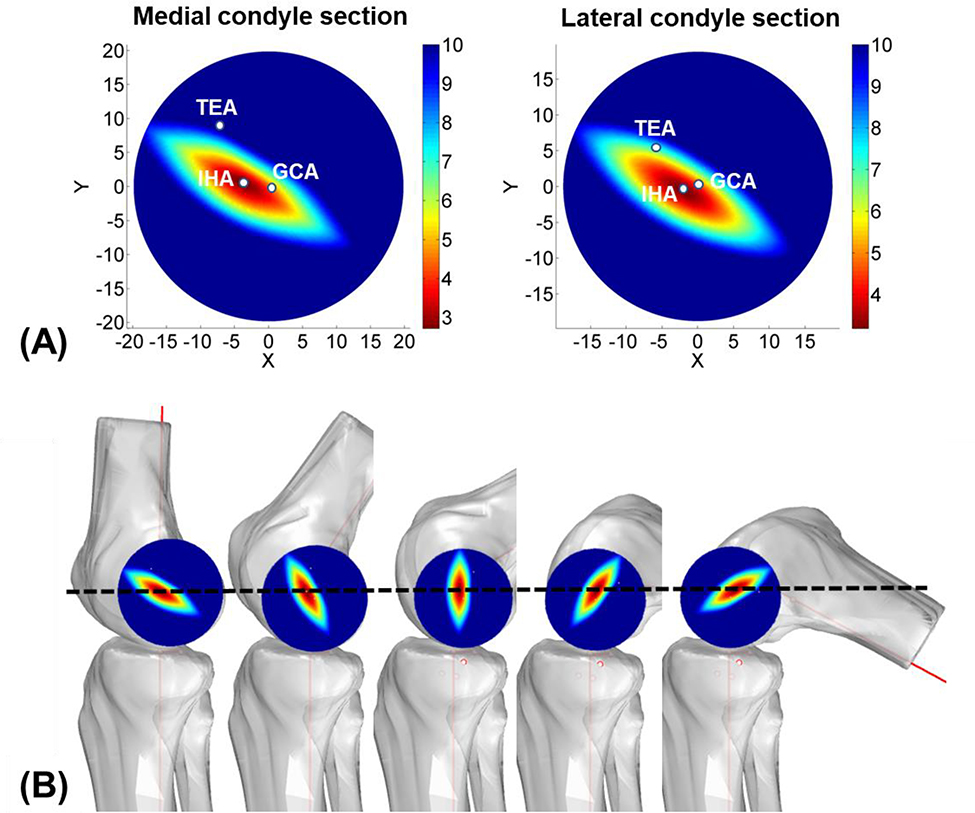
The radii of the medial and lateral circular sections were rM = 19.8±2.0mm and rL = 18.8±2.3mm, respectively. The medial TEA point was 7.2±3.4mm anterior (36.4% of rM) and 8.7±2.9mm proximal (43.9% of rM) to the medial GCA point; the lateral TEA point was 5.8±1.8mm anterior (30.9% of rL) and 4.6±2.0mm proximal (24.5% of rL) to the lateral GCA point. Overall, the IHA was posterior and distal to the TEA, and anterior and distal to the GCA (Fig. 2a). The most isoheight point on the medial condyle was 3.2±2.9 mm posterior (16.2% of rM) and 8.0±2.8 mm distal (40.4% of rM) to the medial TEA point; the most isoheight point on the lateral condyle was 4.8±1.7mm posterior (25.6% of rL) and 5.6±2.2mm distal (29.8% of rL) to the lateral TEA point. The most isoheight point on the medial condyle was 4.0±0.4mm anterior (20.2% of rM) and 0.7±0.1mm proximal (3.5% of rM) to the medial GCA point; the most isoheight point on the lateral condyle was 1.0±0.1mm anterior (5.0% of rL) and 1.0±0.1mm distal (5.0% of rL) to the lateral GCA point (Fig. 2A).
Fig. 2.
(A) Heat maps of the changes (mm) of the medial and lateral femoral condyle heights along the flexion path of the knee to illustrate the uniqueness of the IHA. The positions of the TEA, GCA and IHA on the condyle circular sections in full extension were marked. X and Y axes point to the posterior and proximal directions, respectively. (B) Diagrams showing the condyle height changes along the knee flexion path.
Condyle heights measured using the TEA, GCA and IHA
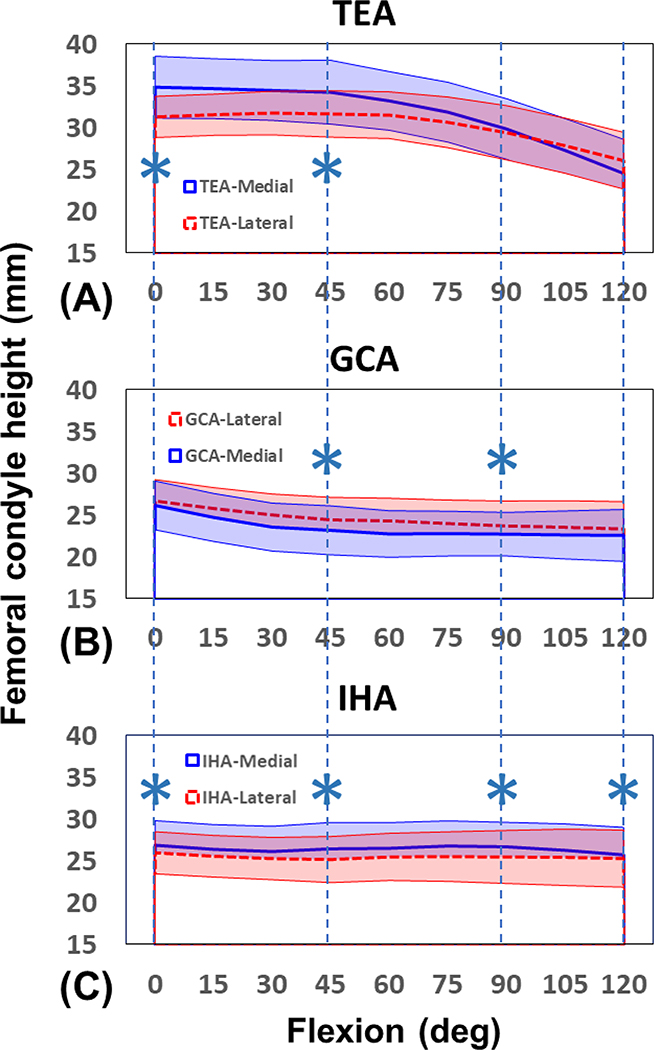
For the TEA axis, the medial and lateral femoral condyle heights slightly changed by −0.6±3.1 mm (p=0.36) and 0.4±2.0 mm (p=0.47), respectively, from full extension to 45° of knee flexion (Fig. 3A and Table 1). Both condyle heights were significantly reduced at 90° (by −4.4±2.5 mm (p=0.000) and −2.2±2.0 mm (p=0.000), respectively) and 120° (by −5.3±1.8 mm (p=0.00) and −3.3±1.8 mm (p=0.00), respectively) of flexion. For the GCA axis, the medial and lateral condyle heights were significantly decreased from full extension to 45° of knee flexion (by −3.0±1.8 mm (p=0.00) and −2.3±2.0 mm (p=0.00), respectively) (Fig. 3B and Table 1). Beyond 45°, the heights of medial and lateral condyles showed no significant changes (p=0.91 and p=0.24, respectively). For the IHA axis, the medial condyle height was 26.8±2.9mm at full extension (Fig. 3C). The condyle height changed within 1.2±2.3mm along the knee flexion path (p=0.60). The lateral condyle height was 25.9±2.5mm at full extension (Fig. 3C). It changed within 0.7±3.3mm along the flexion path (p=0.95). On average, the medial femoral condyle was significantly higher than the lateral side by 1.0±0.3mm along the knee flexion (p=0.01).
Fig. 3.
Medial and lateral femoral condyle heights along the flexion path of the knee measured using (A) TEA, (B) GCA, and (C) IHA. “*” indicates significant differences between the medial and lateral condyle heights (p<0.05). The shaded area represents ± one standard deviation.
Table 1.
Comparison of overall femoral condyle height changes measured using TEA, GCA and IHA methods. Values of mean ± standard deviation are presented.
| 0°–45° | 45°–90° | 90°–120° | ||||
|---|---|---|---|---|---|---|
| Medial | Lateral | Medial | Lateral | Medial | Lateral | |
| TEA | −0.6±3.1#* | 0.4±2.0#* | −4.4±2.5ab& | −2.2±2.0ab& | −5.3±1.8ab | −3.3±1.8ab |
| GCA | −3.0±1.8bc#* | −2.3±2.0bc#* | −0.5±1.6 | −0.7±2.1 | −0.2±1.2 | −0.4±1.4 |
| IHA | −0.4±1.9 | −0.8±2.1 | 0.2±1.6 | 0.3±2.1 | −1.0±1.1 | −0.2±1.4 |
Note:
p<0.05 between TEA and GCA
p<0.05 between TEA and IHA
p<0.05 between GCA and IHA
p<0.05 between 0–45° and 45–90°
p<0.05 between 45–90° and 90–120°
p<0.05 between 0–45° and 90–120°
Comparison between the different axes
The changes of medial femoral condyle heights from 0° to 45° measured using the TEA, GCA, and IHA were −0.6±3.1 mm, −3.0±1.8 mm, −0.4±1.9 mm, respectively (Table 1). The height changes of the GCA were significantly larger than those of the IHA (p=0.00). Similar observations were obtained at the lateral side (p=0.00). Between 45° to 90° and between 90° to 120°, the changes of the condyle heights of the TEA were significantly larger than those of the IHA (p=0.02, p=0.01, respectively) (Table 1).
Discussion
The most important finding of this study was that there are isoheight points and an IHA on the medial and lateral femoral condyles that can measure approximate constant femoral condyle heights along the flexion path of the knee. The condyle height changes measured by the isoheight points were within 1.2±2.3 mm and 0.7±3.3 mm for the medial and lateral condyles, respectively. The condyle height changes measured by the TEA and GCA axes were greater (>3.0 mm) than those of the isoheight points. The data partially confirmed our hypothesis that there are anatomic points in the medial and lateral femoral condyles that can maintain constant condyle heights along the full range flexion of the knee.
The native knee has large coronal and sagittal anatomy variabilities, such as highly variable coronal tibial and femoral alignments [9–11], and interactive sagittal effect of femoral posterior condylar offset and tibial posterior slope [8]. Numerous studies have been reported on the morphometric characters of the femoral condyles [2, 7, 12, 21]. There are also reports on femoral condyle motions measured using the TEA or GCA axes [6, 7, 16, 17, 28]. However, previous studies mainly focused on the anterior-posterior translation and internal-external rotation of the knee [12, 32]. Few data have been reported on the proximal-distal translations of the femoral condyles [6, 23]. Mochizuki et al. [23] reported that the medial condyle had a proximal translation of 7.6mm, and the lateral condyle a distal translation of <3mm from 0° to 90° flexion of the knee using the TEA. Our study showed that the medial and lateral condyles had consistent distal translations beyond 45° using the TEA reference, and both condyles showed decreasing heights from full extension to 45° of flexion using the GCA reference. These data were consistent with the observations of Dimitrious et al., who found that the femoral condyle heights change along the flexion path of the knee when measured using the TEA or GCA references [6].
However, neither TEA nor GCA could represent the constant condyle heights in the full range flexion of the knee. The TEA may oversimplify the intrinsic relationship between the anatomy and kinematics of the knee, without considering the complex knee motion patterns along the flexion path. The GCA is mainly based on the geometry of the posterior femoral condyle without considering the overall distal condyle shape and kinematic features of the knee [18, 23, 27]. It is clinically relevant to determine whether there are locations on the femoral condyles that can represent the constant condyle heights and help achieve soft tissue balance after TKAs [6, 31].
The IHA determined in this study represents the coupling effect of the joint anatomy and kinematics. The IHA is unique for the knee during the flexion as shown by the heat map of Figures 2A and 2B, where the femoral condyle height measurements were sensitive to the locations of the selected reference points. Therefore, the IHA could be used as an alternative physiological reference to evaluate the maintenance of condyle heights along the knee flexion path in preoperative planning, intraoperative positioning, and postoperative evaluation of the TKA surgeries. A balanced TKA may need to maintain the condyle heights with respect to the IHA along the knee flexion path. By maintaining a rather constant condyle height, it is likely to result in a close restoration of medial and lateral soft tissue balances (or minimal changes in ligament lengths caused by surgery). Future clinical evaluations are warranted to explore and validate the application of the IHA in preparation of bony resection and therefore to achieve soft tissue balance in TKA.
There are several limitations to this study. One limitation is the difficulty to technically determine the isoheight points in traditional TKA surgeries as no apparent anatomical landmarks on the femoral condyle surfaces. However, accurate 3D CT and / or MRI images should be used to construct the GCA reference coordinate systems as illustrated in Fig. 1A and then determine the patient-specific IHA locations. Next, the data were measured from normal, healthy knees in this study. Application of these results to arthritic knees may require further development and validation. Future investigation should assess the TKA patients using the IHA to evaluate the gap and soft tissue balances in the mid-range and deep knee flexion. Finally, the condyle heights were measured with respect to the tibial cutting plane that was constructed parallel to the average tibial plateau surface. The tibial cutting slope is generally dependent on the implant design and implantation techniques. Future studies should evaluate the effect of various tibial slopes on the IHA determination. As the knee kinematics could vary with different knee motions, future studies need to examine whether the IHA changes with knee activities. While the IHA could be used to objectively evaluate changes of the femoral condyle heights after knee surgeries, it is possible to use the IHA as an alternative reference to improve the contemporary TKA surgery.
Conclusions
In summary, this study determined the medial and lateral femoral condyle height changes during the in vivo weight-bearing knee flexion. The TEA and GCA were not found to represent constant femoral condyle heights during the knee motion. However, the IHA, that represents the characteristics of both knee anatomy and kinematics, could measure rather constant condyle heights during the in vivo knee flexion. These data could be used as a valuable reference to evaluate changes of the condyle heights after TKA surgeries and help achieve soft tissue balance and optimal knee kinematics along the flexion path.
Acknowledgments
We are grateful for the financial support of the National Institutes of Health (R01AR055612) and the Department of Orthopaedic Surgery at Newton-Wellesley Hospital.
Footnotes
Conflict of Interest
The authors declare that there is no conflict of interest.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- 1.Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 40–47 [PubMed] [Google Scholar]
- 2.Bonnin MP, Saffarini M, Bossard N, Dantony E, Victor J (2016) Morphometric analysis of the distal femur in total knee arthroplasty and native knees. Bone Joint J 98-B:49–57 [DOI] [PubMed] [Google Scholar]
- 3.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Churchill DL, Incavo SJ, Johnson CC, Beynnon BD (1998) The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res 111–118 [DOI] [PubMed] [Google Scholar]
- 5.Colle F, Bignozzi S, Lopomo N, Zaffagnini S, Sun L, Marcacci M (2012) Knee functional flexion axis in osteoarthritic patients: comparison in vivo with transepicondylar axis using a navigation system. Knee Surg Sports Traumatol Arthrosc 20:552–558 [DOI] [PubMed] [Google Scholar]
- 6.Dimitriou D, Tsai TY, Park KK, Hosseini A, Kwon YM, Rubash HE, et al. (2016) Weight-bearing condyle motion of the knee before and after cruciate-retaining TKA: In-vivo surgical transepicondylar axis and geometric center axis analyses. Journal of biomechanics 49:1891–1898 [DOI] [PubMed] [Google Scholar]
- 7.Eckhoff D, Hogan C, DiMatteo L, Robinson M, Bach J (2007) Difference between the epicondylar and cylindrical axis of the knee. Clin Orthop Relat Res 461:238–244 [DOI] [PubMed] [Google Scholar]
- 8.Han HS, Kang SB (2018) Interactive effect of femoral posterior condylar offset and tibial posterior slope on knee flexion in posterior cruciate ligament-substituting total knee arthroplasty. Knee 25:335–340 [DOI] [PubMed] [Google Scholar]
- 9.Hess S, Moser LB, Amsler F, Behrend H, Hirschmann MT (2019) Highly variable coronal tibial and femoral alignment in osteoarthritic knees: a systematic review. Knee Surgery, Sports Traumatology, Arthroscopy 27:1368–1377 [DOI] [PubMed] [Google Scholar]
- 10.Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclercq V, Hess S (2019) Phenotyping the knee in young non-osteoarthritic knees shows a wide distribution of femoral and tibial coronal alignment. Knee Surgery, Sports Traumatology, Arthroscopy 27:1385–1393 [DOI] [PubMed] [Google Scholar]
- 11.Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S (2019) Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surgery, Sports Traumatology, Arthroscopy 27:1394–1402 [DOI] [PubMed] [Google Scholar]
- 12.Hoshino Y, Wang JH, Lorenz S, Fu FH, Tashman S (2012) The effect of distal femur bony morphology on in vivo knee translational and rotational kinematics. Knee Surg Sports Traumatol Arthrosc 20:1331–1338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hosseini A, Qi W, Tsai TY, Liu Y, Rubash H, Li G (2015) In vivo length change patterns of the medial and lateral collateral ligaments along the flexion path of the knee. Knee Surg Sports Traumatol Arthrosc 23:3055–3061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim JH (2013) Effect of posterior femoral condylar offset and posterior tibial slope on maximal flexion angle of the knee in posterior cruciate ligament sacrificing total knee arthroplasty. Knee Surg Relat Res 25:54–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim TK, Chang CB, Kang YG, Kim SJ, Seong SC (2009) Causes and predictors of patient’s dissatisfaction after uncomplicated total knee arthroplasty. J Arthroplasty 24:263–271 [DOI] [PubMed] [Google Scholar]
- 16.Kozanek M, Hosseini A, Liu F, Van de Velde SK, Gill TJ, Rubash HE, et al. (2009) Tibiofemoral kinematics and condylar motion during the stance phase of gait. J Biomech 42:1877–1884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li G, Van de Velde SK, Bingham JT (2008) Validation of a non-invasive fluoroscopic imaging technique for the measurement of dynamic knee joint motion. J Biomech 41:1616–1622 [DOI] [PubMed] [Google Scholar]
- 18.Lustig S, Lavoie F, Selmi TA, Servien E, Neyret P (2008) Relationship between the surgical epicondylar axis and the articular surface of the distal femur: an anatomic study. Knee Surg Sports Traumatol Arthrosc 16:674–682 [DOI] [PubMed] [Google Scholar]
- 19.Luyckx T, Vandenneucker H, Ing LS, Vereecke E, Ing AV, Victor J (2018) Raising the Joint Line in TKA is Associated With Mid-flexion Laxity: A Study in Cadaver Knees. Clin Orthop Relat Res 476:601–611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marra MA, Strzelczak M, Heesterbeek PJC, van de Groes SAW, Janssen DW, Koopman B, et al. (2018) Anterior referencing of tibial slope in total knee arthroplasty considerably influences knee kinematics: a musculoskeletal simulation study. Knee Surg Sports Traumatol Arthrosc 26:1540–1548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matsuda S, Miura H, Nagamine R, Mawatari T, Tokunaga M, Nabeyama R, et al. (2004) Anatomical analysis of the femoral condyle in normal and osteoarthritic knees. J Orthop Res 22:104–109 [DOI] [PubMed] [Google Scholar]
- 22.Minoda Y, Nakagawa S, Sugama R, Ikawa T, Noguchi T, Hirakawa M (2015) Midflexion Laxity After Implantation Was Influenced by the Joint Gap Balance Before Implantation in TKA. J Arthroplasty 30:762–765 [DOI] [PubMed] [Google Scholar]
- 23.Mochizuki T, Sato T, Blaha JD, Tanifuji O, Kobayashi K, Yamagiwa H, et al. (2014) The clinical epicondylar axis is not the functional flexion axis of the human knee. J Orthop Sci 19:451–456 [DOI] [PubMed] [Google Scholar]
- 24.Most E, Axe J, Rubash H, Li G (2004) Sensitivity of the knee joint kinematics calculation to selection of flexion axes. J Biomech 37:1743–1748 [DOI] [PubMed] [Google Scholar]
- 25.Nam D, Nunley RM, Barrack RL (2014) Patient dissatisfaction following total knee replacement: a growing concern? Bone Joint J 96-B:96–100 [DOI] [PubMed] [Google Scholar]
- 26.Niki Y, Nagai K, Sassa T, Harato K, Suda Y (2017) Comparison between cylindrical axis-reference and articular surface-reference femoral bone cut for total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:3741–3746 [DOI] [PubMed] [Google Scholar]
- 27.Park IS, Ong A, Nam CH, Ahn NK, Ahn HS, Lee SC, et al. (2014) Transepicondylar axes for femoral component rotation might produce flexion asymmetry during total knee arthroplasty in knees with proximal tibia vara. Knee 21:369–373 [DOI] [PubMed] [Google Scholar]
- 28.Sharma A, Dennis DA, Zingde SM, Mahfouz MR, Komistek RD (2014) Femoral condylar contact points start and remain posterior in high flexing patients. J Arthroplasty 29:945–949 [DOI] [PubMed] [Google Scholar]
- 29.Stiehl JB, Abbott BD (1995) Morphology of the transepicondylar axis and its application in primary and revision total knee arthroplasty. J Arthroplasty 10:785–789 [DOI] [PubMed] [Google Scholar]
- 30.Stoddard JE, Deehan DJ, Bull AM, McCaskie AW, Amis AA (2013) The kinematics and stability of single-radius versus multi-radius femoral components related to mid-range instability after TKA. J Orthop Res 31:53–58 [DOI] [PubMed] [Google Scholar]
- 31.Watanabe T, Muneta T, Sekiya I, Banks SA (2013) Intraoperative joint gaps affect postoperative range of motion in TKAs with posterior-stabilized prostheses. Clin Orthop Relat Res 471:1326–1333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Watanabe T, Muneta T, Sekiya I, Banks SA (2015) Intraoperative joint gaps and mediolateral balance affect postoperative knee kinematics in posterior-stabilized total knee arthroplasty. Knee 22:527–534 [DOI] [PubMed] [Google Scholar]
- 33.Whiteside LA (2004) Ligament balancing in revision total knee arthroplasty. Clin Orthop Relat Res 178–185 [DOI] [PubMed] [Google Scholar]