Abstract
Cholecystocutaneous Fistula (CCF) is a type of external biliary fistula, which connects the gallbladder with the skin. Thilesus first described this phenomenon in 1670. There is usually a history of calculi in the gallbladder or neglected gallbladder disease.
The incidence of CCF is rare, most patients are elderly females with the mean age of 72.8 years old. They usually present with chronic calculus cholecystitis or a history of a previous surgical intervention.
US, CT, MRI, MRCP and (CT or X-ray) fistulogram are used to confirm the diagnosis. CT was more significant than US in identifying the track of the fistula and the fluid that runs throw it.
CCF patients presented with systemic symptoms (fever, nausea and vomiting) or local symptoms. RUQ region is the most common site of external opening.
Open cholecystectomy with excision of the fistulous tract is considered an acceptable option for treatment and it is curative in most cases.
However, laparoscopic approach can be another option with experience surgeons.
Keywords: Hepatobiliary disease, Gallstones and cholestasis
Highlights
-
•
Cholecystocutaneous Fistula (CCF) is a type of external biliary fistula, which connects the gallbladder with the skin.
-
•
Most patients present with chronic calculus cholecystitis or with a history of a previous surgical intervention.
-
•
Patients treated with conservative or surgical way.
-
•
We clarified, and in numbers, the possible pathogens that might be the main cause of the CCF.
-
•
A new comprehensive illustration of the CCF.
1. Introduction
Fistula is an abnormal condition, which results from abnormal connection between two epithelialized surfaces. Biliary fistulas are rare complications of gallstone, that connect between the biliary tract and other organs, there are two main groups of biliary fistulas: external and internal [1].
Internal biliary fistula connects the gallbladder with gastrointestinal tract, it is induced by chronic cholecystitis [2].
External biliary fistula connects the gallbladder with abdominal wall, it could be spontaneous, postoperative or post-traumatic or caused by iatrogenic injury of biliary tract [[1], [3]].
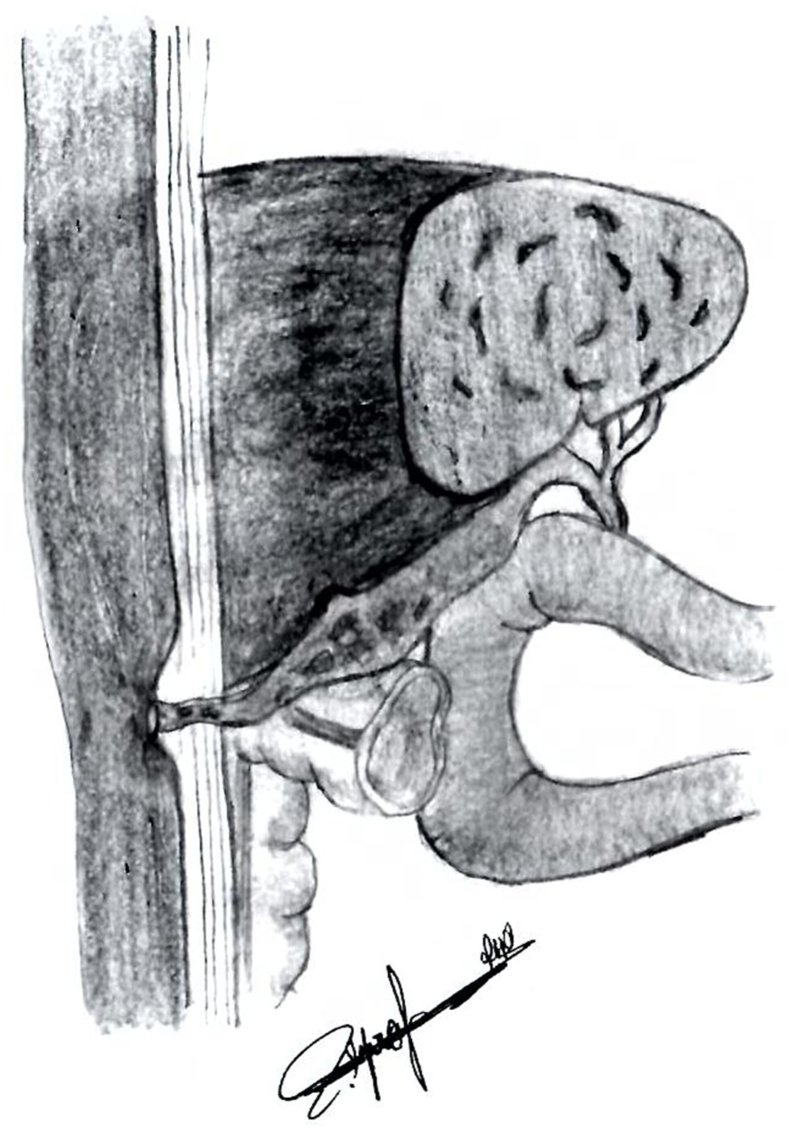
Cholecystocutaneous fistula is a type of external biliary fistula, which connects the gallbladder with skin (Fig. 1).
Fig. 1.
This figure is an illustration of Cholecystocutaneous fistula. It shows the fistula that connects the gallbladder with the skin.
Untreated or neglected gallbladder disease may lead to CCF are the main risk for CCF cases. Most patient presented with a history of calculi in the gallbladder or neglected gallbladder disease and they treated with conservative or surgical way.
There are less than 100 cases of cholecystocutaneous fistula reported in the medical literature [4]. The first reported case of CCF was in 1670 by Thilesus, who described this phenomenon for the first time.
CCF can be spontaneous after cholethiasis and neglected gallbladder disease (5), or following previous surgery such as percutaneous cholecystostomy drain removal [4].
This study reviews the Incidence, Etiology, Clinical Manifestations, Diagnosis and Management for Cholecystocutaneous Fistula patients, using data of pervious case report in the medical literature.
2. Methods
We conducted a literature search for relevant studies that have been published between 1954 and 2020 in Pubmed database by using the following search term “Cholecystocutaneous Fistula”. There were no restrictions on country, or language. Articles were excluded if they were animal studies or uncompleted data. We reviewed 48 case report articles that were published between 1954 and 2020.
2.1. Incidence and etiology
The incidence of CCF is rare, most patients are elderly females (M/F: 18/29) with the mean age of 72.8 years old (Table .1) (see Table 2).
Table 1.
Age, sex, etiology, presentations, diagnosis and management of Cholecystocutaneous Fistula.
| Authors | Age | Sex | Etiology | Presentations | Confirmed diagnosis | Management |
|---|---|---|---|---|---|---|
| Wang et al. [18] | 86 | M | Calculous cholecystitis | Pain and swelling in the RUQ | MRI | Open cholecystectomy |
| Rinzivillo et al. [5] | 76 | M | Calculous cholecystitis | tumefaction of the right hypochondrium, | MRI | Open cholecystectomy |
| El Tinay et al. [23] | 78 | M | Calculous cholecystitis | Fever, malaise and a right subcostal mass | CT | Open cholecystectomy |
| Ioannidis et al. [8] | 71 | M | Calculous cholecystitis | persistent bilious drainage from an old surgical scare, from surgical drainage, of the right upper abdominal quadrant |
X-Ray fistulogram | Open cholecystectomy |
| Cheng et al. [32] | 21 | F | Calculous cholecystitis | Soft tissue defect at posterior trunk and sacral area after a major trauma | CT fistulogram | PTGBD |
| Chatterjee et al. [11] | 45 | F | Calculous cholecystitis | acute onset of pain and swelling in the right hypochondrium | X-Ray fistulogram | Open cholecystectomy |
| Ijaz et al. [10] | 74 | F | Calculous Cholecystitis | fevers, malaise and a right subcostal mass | CT | Open cholecystectomy |
| Ayoub et al. [26] | 65 | M | Gallstones | Swelling in the right hypochondriac area. | During the surgery | Open cholecystectomy |
| Pol et al. [21] | 70 | F | Gallstones | Discharging sinus in the right hypochondriac region | CT fistulogram | Laparoscopic cholecystectomy |
| Kassi et al. [6] | 46 | _ | Gallstones | Painful, fluctuating, epigastric swelling of 15 days' duration. | CT | Open cholecystectomy |
| Bermúdeza et al. [30] | 30 | F | Gallstones | pain in the right hypochondrium of years evolution | X-Ray Fistulogram | Open cholecystectomy |
| Dixon et al. [28] | 94 | F | Gallstones | wound discharge and non-healing wound |
CT | conservative management |
| Polite et al. [29] | 70 | F | Gallstones | acute on chronic midepigastric abdominal pain, associated with nausea and vomiting |
Hepatobiliary iminodiacetic acid | Open cholecystectomy |
| Ozdemir et al. [24] | 89 | F | Gallstones | right upper abdominal pain and icterus | CT | Open cholecystectomy |
| Gordon et al. [33] | 83 | F | Gallstones | mild, intermittent right upper quadrant pain | CT | Open cholecystectomy |
| Khan et al. [34] | 76 | M | Gallstones | necrotizing fasciitis of anterior abdominal wall and cholecystocutaneous fistula | X-Ray fistulogram | Open cholecystectomy |
| Pezzilli et al. [17] | 90 | F | Gallstones | diarrhea and low-grade fever | CT | conservative management and Ct drainage of the purulent collection was also carried out |
| Aguilar et al. [35] | 83 | M | Gallstones | pain in the right upper quadrant and the appearance of a mass | CT | conservative management |
| Hawari et al. [9] | 84 | M | Gallstones | intermittent right upper quadrant abdominal pain, nausea, darkening of his urine, and increasing jaundice |
X-Ray fistulogram | Open cholecystectomy |
| Sayed et al. [31] | 85 | F | Gallstones | soft and non-tender mass in her right flank. | MRCP | ERCP and sphincterotomy |
| Yüceyar et al. [36] | 70 | F | Gallstones | abscess formation in the right upper quadrant | _ | Open cholecystectomy |
| Carragher et al. [37] | 67 | F | Gallstones | Right hypochondrial pain | CT | Conservative management |
| Hoffman et al. [38] | 70 | F | Gallstones | chronic epigastric pain. | During the surgery | Open cholecystectomy and choledocholithotomy |
| 73 | F | Gallstones | ten-day history of dull epigastric pain and anorexia | During the surgery | Laparotomy | |
| Jeffery et al. [39] | _ | M | Gallstones | enlarging mass on the right upper abdomen | During the surgery | Open cholecystostomy |
| Schippers et al. [40] | 75 | M | Cholecystitis | _ | _ | _ |
| Gerrard et al. [22] | 80 | F | Cholecystitis | acute cholecystitis | CT | Percutaneous cholecystectomy |
| Mughal et al. [19] | 74 | F | Cholecystitis | unremitting pain in the right shoulder that had progressed to the right side of the abdomen | During the surgery | Open cholecystectomy |
| pain and swelling in the RUQ, and development of a discharging sinus within it | US + CT | Open cholecystectomy | ||||
| Maynard et al. [7] | 68 | F | Cholecystitis | painful swelling in the right upper anterior abdominal wall. |
CT | Open cholecystectomy |
| Jayasinghe et al. [41] | 87 | F | Cholecystitis | sepsis following a fall | CT | Open abscess drainage |
| Mughal et al. [19] | 74 | F | Cholecystitis | sepsis following a fall | CT | Open abscess drainage |
| Kapoor et al. [15] | 45 | M | Cholecystitis | right hypochondrial tenderness and bilious discharge from the scar |
X-Ray fistulogram | Open Cholecystectomy |
| 65 | M | Cholecystitis | discharging sinus from the anterior abdominal wall |
CT | cholecystocutaneous fistula excision | |
| Kim et al. [42] | 72 | F | Cholecystitis | persistent small volume discharge from the drain site |
sinogram | cholecystocutaneous fistula excision |
| Flora et al. [27] | 67 | M | Cholecystitis | persisting discharge from what was thought to be an ‘abscess’ in the right hypochondrium |
CT | Open cholecystectomy |
| Malik et al. [43] | 76 | F | Cholecystitis | acute cholecystitis | CT | laparoscopic cholecystectomy |
| Cruz et al. [25] | 81 | M | Cholecystitis | right upper abdominal pain | During the surgery | Open cholecystectomy |
| Khan et al. [44] | 90 | F | Cholecystitis | RUQ swelling | CT | Open cholecystectomy |
| Dutriaux et al. [45] | 65 | M | Cholecystitis | inflammatory and ulcerated lesion located on his right flank | Systemic Pathology Exam | Open cholecystectomy |
| Vasanth et al. [46] | _ | _ | Cholecystitis | _ | _ | _ |
| Mathonnet et al. [47] | 87 | F | Cholecystitis | right hypochondrial pain. |
X-Ray fistulogram | Open cholecystectomy |
| Sedgwick et al. [48] | 76 | M | Cholecystitis | acute cholecystitis | upper abdominal pain | ERCP |
| Pripotnev et al. [16] | 85 | F | Cholecystocutaneous fistula developing after the removal of a percutaneous drain for the treatment of acute cholecystitis | sharp intermittent epigastric and right upper quadrant pain radiating to the central back. | During the surgery | laparoscopic cholecystectomy |
| Sodhi et al. [13] | 66 | F | Adenocarcinoma of gallbladder | Pain in the right hypochondrium. | X-Ray fistulogram | Conservative management (chemotherapy) |
| Serrano et al. [49] | 83 | M | Papillary adenocarcinoma | abdominal pain in the right upper quadrant associated with the oozing of hematic purulent content through an orifice in the abdominal wall located in the right hypochondrium |
CT | radical cholecystectomy |
| Andersen et al. [50] | 89 | F | – | abscess in the right breast | ERCP | Open cholecystectomy |
| Lofgren et al. [4] | 60 | F | Severe cholecystitis the year prior that was managed by a percutaneous cholecystostomy drain | Shortness of breath, RUQ pain, nausea, emesis, and a fever. | CT with oral contrast | Robotic cholecystectomy |
| Seoane et al. [51] | 83 | F | Spontaneous external biliary fistula and a history of ERCP three months before | abdominal pain and fever and mass in the RUQ | During the surgery | Open cholecystectomy |
| Murphy et al. [52] | 80 | M | Cholecystitis | swelling on the anterior abdominal wall in the right upper quadrant extending over the right costal margin |
During the surgery | subtotal cholecystectomy |
| Grimes et al. [14] | 70 | F | traumatic rupture of the gallbladder | pain in the upper abdomen | X-Ray | cholecystocutaneous fistula excision |
| Mean age | 72.8 | |||||
| Standard Deviation | 15 |
Table 2.
Presenting microorganism found in cholecystocutaneous fistula cases.
| Authors | Microorganism |
|---|---|
| Lofgren et al. [4], Micu et al. [12], El Tinay et al. [23] Jayasinghe et al. [41] Fabbi et al. [53], Ioannidis et al. [8], Hoffman et al. [38], Orville et al. [14] | Escherichia coli |
| Flora et al.(27), Murphy et al. [52], Ijaz (10) | Coliforms |
| El Tinay et al. [23], Ioannidis et al. [8] | Klebsiella pneumonia |
| Kassi et al. [6] | Helicobacter pylori |
| Ioannidis et al. [8] | Staphylococcus hominis, |
| Cheng et al. [32] | Staphylococcus aureus |
| Hawari (9) | Strepto-coccus milleri |
| Micu et al. [12] | Enterococcus faecalis |
| Lofgren et al. [4] | Bacteroides fragilis |
| Mathonnet et al. [47] | Fragils |
| Hoffman et al. [38] | Proteus mirubilis |
| Orville et al. [14] | Viridans streptococci (enterococci) |
CCF mainly is a result of neglected gallbladder disease.
Most cases presented with chronic calculus cholecystitis or with a history of previous surgical intervention as a case of subtotal cholecystectomy for acute cholecystitis [[6], [7], [8], [9], [10], [11]].
Increasing pressure in the gallbladder after calculus cholecystitis, which leads to fistula formation, is believed to be the pathophysiology mechanism of this condition.
Most common cases of CCF are related to bacterial infection in the gallbladder, but there are few cases of CCF arising from adenocarcinoma of gallbladder [[12], [13]].
Escherichia coli is the most common microorganism found in cholecystocutaneous fistula cases followed by Coliforms and klebsiella pneumonia. (Table. 2).
Also retained stones after laparoscopic cholecystectomy and traumatic rupture of the gallbladder are considered as predisposing factors for cholecystocutaneous fistula [[14], [15]].
2.2. Clinical Manifestations
The general condition of the patient variable is depending on the age and past medical history. There is usually a history of calculi in the gallbladder or neglected gallbladder disease.
CCF patients presented with systemic symptoms or specific symptoms.
The patients showed systemic symptoms such as: fever, nausea and vomiting [[12], [16], [17]].
However, patients may present with pain and swelling in the RUQ or epigastric region [[6], [18]], discharging sinus from the anterior abdominal wall [[15], [19]], erythematous mass [20], subcostal abscess [18] (Table .1). The most common site of external opening is in the right upper quadrant of the abdominal wall. It can also be seen in right flank, right subcostal area, epigastric region, right breast, para-umbilical site (Table .3).
Table 3.
Presenting site of external opening.
| Location | Authors |
|---|---|
| RUQ | Ayoub et al. [26], Lofgren et al. [4], Seoane et al. [51], pol et al. [21], Wang et al. [18], Rinzivillo et al. [5], Gerrard et al. [22], El Tinay et al. [23], Mughal et al. [19], Maynard et al. [7], Bermúdez et al. [30], Pripotneva et al. [16], Kapoor et al. [15], Polite et al. [29], Kim et al. [42], Sodhi et al. [13], Ioannidis et al. [8], Cheng et al. [32], Serrano et al. [49], Gordon et al. [33], Khan et al. [34], Pezzillia et al. [17], Hawari et al. [9], Chatterjee et al. [11], Flora et al. [27], Ijaz et al. [10], Malik et al. [43], Yüceyar et al. [36], Carragher et al. [37], Sedgwick et al. [49], Abril et al. [54], Jeffrey et al. [39], Orville et al. [14], |
| Right flank | Sayed et al. [31], Khan et al. [44], Jayasinghe et al. [41] |
| Right subcostal area | Ozdemir et al. [24], Cruz et al. [25], Hoffman et al. [38] |
| Epigastric region | Micu et al. [12], Kassi et al. [6] |
| Right breast | Andersen et al. [50] |
| para-umbilical | Dixon et al. [28] |
2.3. Diagnosis
CCF is diagnosed usually using imaging studies, or exploratory laparotomy in special cases.
2.4. Imaging studies include
-
•
Ultrasonography (US)
-
•
Computed tomography (CT)
-
•
Fistulogram
-
•
Magnetic resonance imaging (MRI)
US provides good assessment for CCF diagnosis by showing abnormal findings such as abscess, gallbladder stones, edema, thickened in gallbladder wall and dilated biliary ducts [[5], [15], [17], [21]] but often fails to confirm the CCF diagnosis. In a few cases, US was able to demonstrate the track of CCF [[12], [19]].
CT confirmed the diagnosis by identifying the track between the gallbladder and the skin in several cases [[22], [23], [24], [25]]. Furthermore, CT fistulogram can also show the track of CCF which confirm the diagnosis [21]. CT couldn't identify the track of CCF in a few cases where it just showed abnormal findings which point toward the diagnosis [[19], [23], [26], [27]].
In total, CT was more significant than US in identifying the track of the fistula and the fluid that runs throw it.
MRI was able to detect gallstones, gallbladder perforation, and the fluid, which extruded through the abdominal wall [[5], [18]].
MRI could be more accurate when CT detects no abnormalities.
MRCP increases the confirmed cases [[7], [17], [19], [28]]. The results of MRCP are identical to US and CT.
Hepatobiliary iminodiacetic acid scan was used in two cases; it failed to demonstrate the fistula in one case (4) and showed obstruction in biliary tracks in the second one [29].
In addition, exploratory laparotomy may be the only diagnosis methods especially in old reported cases, in poor countries or with shortage of appropriate equipment and laparoscopic experience.
CT Fistulogram or X-ray Fistulogram have been used to demonstrate track of the fistula accurately [[14], [21], [30]], although in most cases Fistulogram was not used and the diagnose was made by another method.
There are problem and the difficulties facing the diagnosis such as absence of radiological expertise, it is uncommon to consider CCF as deferential diagnosis since it is a rare condition and presence of mucous discharge rather than yellowish discharge if there is an obstruction in the cystic duct makes it hard to diagnose especially in the early stages.
2.5. Management
The management of CCF vary according to disease severity, age, and the patient's preference.
There is no standard base line management for cholecystocutaneous fistula, due to the fewness of the number of cases and the differences in patients’ illness quality.
The medical literature mentioned different ways of CCF management, either conservative or surgical management.
2.6. Conservative management
Conservative management includes antibiotics, fluids or ERCP.
Percutaneous abscess drainage is performed immediately with the guidance of CT, or US, then all patients should receive management by antibiotics to manage infections and cholecystitis [[4], [7], [16], [17], [23], [26]].
Conservative management is performed to elderly patients who are unable to tolerate surgery [17].
Few cases were treated by using endoscopic retrograde cholangiopancreatography (ERCP) for CCF treatment, by removing calculi using ERCP balloon trawl and sphincterotomy [31].
Chemotherapy is applied for CCF patients due to carcinoma of the gallbladder [13].
Percutaneous transhepatic gallbladder drainage (PTGBD) can be applied to treat CCF. Where the fistula heals under secondary intention after removing drainage tube [32].
Conservative management cured few cases, helped relieve symptoms and improved patient's condition.
Surgical management:
Surgical management includes open cholecystectomy and laparoscopic cholecystectomy.
Open cholecystectomy with excision of the fistulous tract is considered as a standard option for management and it is curative in most cases. In the other hand, laparoscopic cholecystectomy with excision of the tract can be another acceptable and preferable option with advance experienced laparoscopic surgeons.
Presence of comorbidity in patients lead to failure of healing, also difficulty in performing surgery for cachectic or elderly patients.
Lack of adequate surgical experience can lead to serious complications and difficulty in treatment.
3. Conclusion
CCF diagnosis and management represent one of the surgical obstacles, which we still encountered from time to time.
We noticed through our review different ways of diagnosis and management. Most of them were dependent on the surgical experience and the advanced medical investigation equipment.
In conclusion, there is no standard ways for diagnosis and management of CCF but according to our review; we think that each surgeon should choose the best way to deal with CCF patients depending on patients ‘quality, available equipment and advanced experienced surgeons.
Ethical approval
Not required.
Sources of funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Author contribution
MZBA, MM, MZ, OA: Writing - Original Draft. MM, MZBA: Writing - Review & Editing. MM: Formal analysis and Resources. MZBA: Validation and Visualization. AG: Supervision and Project administration. MZ: corresponding author.
Guarantor
Mohammad Ziadeh.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Ethics
Not required.
Patient consent for publication
Not required.
Provenance and peer review
Not commissioned, externally peer reviewed.
Declaration of competing interest
None declared.
Acknowledgements
The authors wish to thank Razan Hallak for drawing the figure, Ms. Nour Ajam for proofreading the manuscript and Ruqua Masri, Mohammad Nour Shashaa and Muhammad Diabi for technical support
Contributor Information
Muhamad Zakaria Brimo Alsaman, Email: dr.zakariaBrimo@gmail.com.
Muhammad Mazketly, Email: midomazketly@yahoo.com.
Mohammad Ziadeh, Email: Mohammadziadeh98@gmail.com.
Owais Aleter, Email: owaisaleter33@gmail.com.
Ahmad Ghazal, Email: Ghazal929@yahoo.com.
References
- 1.Crespi M., Montecamozzo G., Foschi D. Diagnosis and treatment of biliary fistulas in the laparoscopic era. Gastroenterol Res Pract. 2016;2016:6293538. doi: 10.1155/2016/6293538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Puestow C.B. Spontaneous internal biliary fistulae. Ann. Surg. 1942 Jun;115(6):1043–1054. doi: 10.1097/00000658-194206000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dadoukis J., Prousalidis J., Botsios D., Tzartinoglou E., Apostolidis S., Papadopoulos V. External biliary fistula. HPB Surg. 1998;10(6):375–377. doi: 10.1155/1998/42791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lofgren D.H., Vasani S., Singzon V. vol. 11. Cureus; United States: 2019. p. e4444. (Abdominal Wall Abscess Secondary to Cholecystocutaneous Fistula via Percutaneous Cholecystostomy Tract). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rinzivillo N.M.A., Danna R., Leanza V., Lodato M., Marchese S., Basile F. Case Report: spontaneous cholecystocutaneous fistula, a rare cholethiasis complication. F1000Research. 2017;6:1768. doi: 10.12688/f1000research.12235.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kassi A.B.F., Koffi E., Yenon K.S., Bombet-Kouame C. vol. 11. Case reports in gastroenterology; Switzerland: 2017. pp. 225–228. (Cholecystoparietal Fistula Revealed by an Epigastric Abscess). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maynard W., McGlone E.R., Deguara J. Unusual aetiology of abdominal wall abscess: cholecystocutaneous fistula presenting 20 years after open subtotal cholecystectomy. BMJ Case Rep. 2016 doi: 10.1136/bcr-2015-213326. 2016 Mar, bcr2015213326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ioannidis O., Paraskevas G., Kotronis A., Chatzopoulos S., Konstantara A., Papadimitriou N. Spontaneous cholecystocutaneous fistula draining from an abdominal scar from previous surgical drainage. Ann. Ital. Chir. 2012;83(1):67–69. [PubMed] [Google Scholar]
- 9.Hawari M., Wemyss-Holden S., Parry G.W. Recurrent chest wall abscesses overlying a pneumonectomy scar: an unusual presentation of a cholecystocutaneous fistula. Interact. Cardiovasc. Thorac. Surg. 2010 May;10(5):828–829. doi: 10.1510/icvts.2009.221085. [DOI] [PubMed] [Google Scholar]
- 10.Ijaz S., Lidder S., Mohamid W., Thompson H.H. vol. 2. Case reports in gastroenterology; Switzerland: 2008. pp. 71–75. (Cholecystocutaneous Fistula Secondary to Chronic Calculous Cholecystitis). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chatterjee S., Choudhuri T., Ghosh G., Ganguly A. Spontaneous cholecystocutaneous fistula in a case of chronic colculous cholecystitis-a case report. J. Indian Med. Assoc. 2007 Nov;105(11) 644,646,656. [PubMed] [Google Scholar]
- 12.Micu B.V., Andercou O.A., Micu C.M., Militaru V., Jeican, Bungardean C.I. Spontaneous cholecystocutaneous fistula as a primary manifestation of gallbladder adenocarcinoma associated with gallbladder lithiasis - case report. Rom J Morphol Embryol = Rev Roum Morphol Embryol. 2017;58(2):575–583. [PubMed] [Google Scholar]
- 13.Sodhi K., Athar M., Kumar V., Sharma I.D., Husain N. Spontaneous cholecysto-cutaneous fistula complicating carcinoma of the gall bladder: a case report. Indian J. Surg. 2012 Apr;74(2):191–193. doi: 10.1007/s12262-011-0280-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grimes Of, Steinbach Hl Traumatic cholecystocutaneous fistula. AMA Arch Surg. 1955 Jul;71(1):68–70. doi: 10.1001/archsurg.1955.01270130070010. [DOI] [PubMed] [Google Scholar]
- 15.Kapoor Y., Singh G., Khokhar M. Spontaneous cholecystocutaneous fistula-not an old time story. Indian J. Surg. 2013 Jun;75(Suppl 1):188–191. doi: 10.1007/s12262-012-0560-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pripotnev S., Petrakos A. vol. 8. Case reports in gastroenterology; Switzerland: 2014. pp. 119–122. (Cholecystocutaneous Fistula after Percutaneous Gallbladder Drainage). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pezzilli R., Barakat B., Corinaldesi R., Cavazza M. vol. 4. Case reports in gastroenterology; 2010. pp. 356–360. (Spontaneous Cholecystocutaneous Fistula). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Y.-F., Chen H.-Q. Hepatobiliary and pancreatic: spontaneous cholecystocutaneous fistula. J. Gastroenterol. Hepatol. 2019 Jan;34(1):11. doi: 10.1111/jgh.14285. [DOI] [PubMed] [Google Scholar]
- 19.Mughal Z., Green J., Whatling P.J., Patel R., Holme T.C. Performation of the gallbladder: “bait” for the unsuspecting laparoscopic surgeon. Ann. R. Coll. Surg. Engl. 2017 Jan;99(1):e15–e18. doi: 10.1308/rcsann.2016.0274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Batty L., Freeman L., Dubrava Z. vol. 81. ANZ journal of surgery; Australia: 2011. p. 847. (A Spontaneous Cholecystocutaneous Fistula). [DOI] [PubMed] [Google Scholar]
- 21.Pol M.M., Vyas S., Singh P., Rathore Y.S. Spontaneous cholecystocutaneous fistula: empirically treated for a missed diagnosis, managed by laparoscopy. BMJ Case Rep. 2019 Feb;12(2) doi: 10.1136/bcr-2018-228138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gerrard A., Date R. vol. 4. ACG case reports journal; United States: 2017. p. e102. (Delayed Spontaneous Passage of Gallstones via Cholecystocutaneous Fistula). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.El Tinay O., Siddiqui Z.U.R., Alhedaithy M., Kharashgah M.N.M. Right hypochondrial abscess: a rare consequence of supportive cholecystitis. Annals of medicine and surgery. 2012;12 doi: 10.1016/j.amsu.2016.11.009. England; 2016. pp. 106–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ozdemir Y., Yucel E., Sucullu I., Filiz I., Gulec B., Akin M.L. Spontaneous cholecystocutaneous fistula as a rare complication of gallstones. Bratisl. Lek. Listy. 2012;113(7):445–447. doi: 10.4149/bll_2012_099. [DOI] [PubMed] [Google Scholar]
- 25.Cruz R.J.J., Nahas J., de Figueiredo L.F.P. Spontaneous cholecystocutaneous fistula: a rare complication of gallbladder disease. Sao Paulo Med. J. 2006 Jul;124(4):234–236. doi: 10.1590/S1516-31802006000400012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ayoub K., Alkarrash M.S., Shashaa M.N., Zazo A., Rhayim R., Mahli N. A rare complication of gallstones ended with spontaneous cholecystocutaneus fistula in an old man: a case report. International journal of surgery case reports. 2020;67:42–44. doi: 10.1016/j.ijscr.2020.01.008. Netherlands. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Flora H.S., Bhattacharya S. Spontaneous cholecystocutaneous fistula. HPB. 2001;3(4):279–280. doi: 10.1080/136518201753335584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dixon S., Sharma M., Holtham S. Cholecystocutaneous fistula: an unusual complication of a para-umbilical hernia repair. BMJ Case Rep. 2014 doi: 10.1136/bcr-2013-202417. May;2014, bcr2013202417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Polite N.M., Brown R., Braveman J. The use of laser lithotripsy status post cholecystostomy tube placement without interval cholecystectomy for calculous cholecystitis in a patient unfit for general anesthesia. Surg. Laparosc. Endosc. Percutaneous Tech. 2013 Dec;23(6):e229–e231. doi: 10.1097/SLE.0b013e31828b8736. [DOI] [PubMed] [Google Scholar]
- 30.Guardado-Bermudez F., Aguilar-Jaimes A., Ardisson-Zamora F.J., Guerrero-Silva L.A., Villanueva-Rodriguez E., Gomez-de Leija N.A. [Spontaneous cholecystocutaneous fistula] Cir. Cir. 2015;83(1):61–64. doi: 10.1016/j.circir.2015.04.026. [DOI] [PubMed] [Google Scholar]
- 31.Sayed L., Sangal S., Finch G. Spontaneous cholecystocutaneous fistula: a rare presentation of gallstones. J Surg case reports. 2010 Jul;2010(5):5. doi: 10.1093/jscr/2010.5.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cheng H.-T., Wu C.-I., Hsu Y.-C. Spontaneous cholecystocutaneous fistula managed with percutaneous transhepatic gallbladder drainage. Am. Surg. 2011 Dec;77(12):E285–E286. [PubMed] [Google Scholar]
- 33.Gordon P.E., Miller D.L., Rattner D.W., Conrad C. Image of the month. Cholecystocutaneous fistula (Jean-Louis Petit phlegmon) Arch. Surg. 2011 Apr;146(4):487–488. doi: 10.1001/archsurg.2011.66-a. [DOI] [PubMed] [Google Scholar]
- 34.Khan A., Rajendran S., Baban C., Murphy M., O'Hanlon D. Spontaneous cholecystocutaneous fistula. BMJ Case Rep. 2011 doi: 10.1136/bcr.05.2011.4176. 2011 Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tallon Aguilar L., Lopez Porras M., Molina Garcia D., Bustos Jimenez M., Tamayo Lopez M.J. vol. 33. Gastroenterologia y hepatologia; Spain: 2010. pp. 553–554. (Cholecystocutaneous Fistula: a Rare Complication of Gallstones). [DOI] [PubMed] [Google Scholar]
- 36.Yuceyar S., Erturk S., Karabicak I., Onur E., Aydogan F. Spontaneous cholecystocutaneous fistula presenting with an abscess containing multiple gallstones: a case report. Mt. Sinai J. Med. 2005 Nov;72(6):402–404. [PubMed] [Google Scholar]
- 37.Carragher A.M., Jackson P.R., Panesar K.J. Subcutaneous herniation of gall-bladder with spontaneous cholecystocutaneous fistula. Clin. Radiol. 1990 Oct;42(4):283–284. doi: 10.1016/s0009-9260(05)82120-8. [DOI] [PubMed] [Google Scholar]
- 38.Hoffman L., Beaton H., Wantz G. Spontaneous cholecystocutaneous fistula: a complication of neglected biliary tract disease. J. Am. Geriatr. Soc. 1982 Oct;30(10):632–634. doi: 10.1111/j.1532-5415.1982.tb05059.x. [DOI] [PubMed] [Google Scholar]
- 39.Callen J.P. Cholecystocutaneous fistula. Int. J. Dermatol. 1979 Jan 1;18(1) doi: 10.1111/j.1365-4362.1979.tb01915.x. [Internet] 63–4. Available from. [DOI] [PubMed] [Google Scholar]
- 40.Schippers H.J.W., Toorenvliet B.R. [A late complication of cholecystitis] Ned. Tijdschr. Geneeskd. 2018 Jun:162. [PubMed] [Google Scholar]
- 41.Jayasinghe G., Adam J., Abdul-Aal Y. Unusual presentation of gallbladder perforation. Int J Surg Case Rep. 2016;18:42–44. doi: 10.1016/j.ijscr.2015.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kim M., Beenen E., Fergusson J. Spontaneous cholecystocutaneous fistula by gallstone erosion into abdominal wall. ANZ J. Surg. 2014 Nov;84(11):888–889. doi: 10.1111/ans.12359. [DOI] [PubMed] [Google Scholar]
- 43.Malik A.H., Nadeem M., Ockrim J. Complete laparoscopic management of cholecystocutaneous fistula. Ulster Med. J. 2007 Sep;76(3):166–167. [PMC free article] [PubMed] [Google Scholar]
- 44.Khan A.A., Azhar M.Z., Khan A.A., Rasheed A., Khan K.N. Spontaneous cholecystocutaneous fistula. J Coll Physicians Surg Pak. 2005 Nov;15(11):726–727. [PubMed] [Google Scholar]
- 45.Dutriaux C., Maillard H., Prophette B., Catala M., Celerier P. [Spontaneous cholecystocutaneous fistula] Ann. Dermatol. Venereol. 2005 May;132(5):467–469. doi: 10.1016/s0151-9638(05)79310-8. [DOI] [PubMed] [Google Scholar]
- 46.Vasanth A., Siddiqui A., O'Donnell K. Spontaneous cholecystocutaneous fistula. South. Med. J. 2004 Feb;97(2):183–185. doi: 10.1097/01.SMJ.0000051150.63130.E8. [DOI] [PubMed] [Google Scholar]
- 47.Mathonnet M., Maisonnette F., Gainant A., Cubertafond P. [Spontaneous cholecystocutaneous fistula: natural history of biliary cholecystitis] Ann. Chir. 2002 May;127(5):378–380. doi: 10.1016/s0003-3944(02)00775-7. [DOI] [PubMed] [Google Scholar]
- 48.Sedgwick M.L., Denyer M.E. Treatment of a postoperative cholecystocutaneous fistula by an endoscopic stent. Br. J. Surg. 1989 Feb;76(2):159–160. doi: 10.1002/bjs.1800760218. [DOI] [PubMed] [Google Scholar]
- 49.Ugalde Serrano P., Solar Garcia L., Miyar de Leon A., Gonzalez-Pinto Arrillaga I., Gonzalez Gonzalez J. vol. 91. Cirugia espanola; Spain: 2013. pp. 396–397. ([Cholecystocutaneous Fistula as a First Sign of Presentation of a Gallbladder Adenocarcinoma]). [DOI] [PubMed] [Google Scholar]
- 50.Andersen P., Friis-Andersen H. [Spontaneous cholecystocutaneous fistula presenting in the right breast] Ugeskr Laeger. 2012 Apr;174(18):1235–1236. [PubMed] [Google Scholar]
- 51.Santos Seoane S.M., Diaz Fernandez V., Arenas Garcia V. vol. 111. Revista espanola de enfermedades digestivas : organo oficial de la Sociedad Espanola de Patologia Digestiva; Spain: 2019. pp. 407–408. (Cholecystocutaneous Fistula). [DOI] [PubMed] [Google Scholar]
- 52.Murphy J.A., Vimalachandran C.D., Howes N., Ghaneh P. vol. 2. Case reports in gastroenterology; Switzerland: 2008. pp. 219–223. (Anterior Abdominal Wall Abscess Secondary to Subcutaneous Gallstones). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fabbi M., Volta A., Quintavalla F., Zubin E., Manfredi S., Martini F.M. Cholecystocutaneous fistula containing multiple gallstones in a dog. Can Vet J = La Rev Vet Can. 2014 Dec;55(12):1163–1166. [PMC free article] [PubMed] [Google Scholar]
- 54.Abril A., Ulfohn A. Spontaneous cholecystocutaneous fistula. South. Med. J. 1984 Sep;77(9):1192–1193. doi: 10.1097/00007611-198409000-00039. [DOI] [PubMed] [Google Scholar]