Abstract
Background:
Metabolic syndrome (MetS) refers to a cluster of risk factors for cardiovascular disease and type 2 diabetes. The aim of this study is to assess the effects of acarbose as an antihyperglycemic agent (drug) on late complications of MetS.
Methods:
This double-blind randomized clinical trial was done on patients with MetS admitted to Isfahan Endocrine and Metabolism Research Center. They were assigned randomly to two groups: A who received acarbose (n = 32) and group B who received a placebo (n = 42) for 6 months. Cardiovascular indexes including flow-mediated dilation (FMD), intima-media thickness (IMT), epicardial fat thickness (EFT), and C-reactive protein (CRP) were measured at baseline and 6 months after the treatment and compared between the two groups.
Results:
Post-intervention mean of weight (mean difference: −2.5 ± 0.89) and abdominal obesity (mean difference: −2.2 ± 0.64) in acarbose group were significantly decreased (P value < 0.001). High-density lipoprotein (HDL) level in acarbose group was significantly higher than control group (44.7 ± 7.6 vs 41.1 ± 6.4; P value = 0.043), while the other metabolic parameters were not significantly different between the two groups (P value > 0.05). In both groups, CRP and EFT decreased significantly after the intervention, and the levels of CRP, EFT, and IMT markers in the acarbose group were significantly lower than control group (P value < 0.05).
Conclusions:
The administration of acarbose in patients with MetS can decrease weight and abdominal obesity as well as the reduction of inflammatory and cardiovascular markers, including CRP, EFT, and IMT and also increases HDL.
Keywords: Acarbose, cardiovascular, C-reactive protein, inflammatory marker, metabolic syndrome, obesity
Introduction
Metabolic syndrome (MetS) refers to a group of metabolic risk factors associated with the increased risk of cardiovascular diseases (CVDs) and type 2 diabetes,[1] these factors include abdominal obesity, hyperlipidemia, hypertension, hyperglycemia, and insulin resistance.[1,2] The prevalence of MetS increases with age from lower than 10% in young adults to nearly 40% in people over 60.[3] It is estimated that 20–25% of the world adult population suffers from MetS disorders. MetS is more prevalent in Asian population. There has been growing evidence suggesting that the inflammatory markers are the main causes of macro- and microvascular, including renal, ophthalmic, and cardiac, complications in patients with MetS who suffer from diabetes.[4] The plasma concentration of C-reactive protein (CRP), a marker of inflammation, is elevated in obese patients, and is correlated with the MetS and decreases with weight loss. CRP is produced by mature adipocytes in adipose tissue and may contribute to the elevated circulating plasma CRP concentrations present in obese patients and people with the MetS. Treatment of the MetS is aimed at improving insulin resistance through lifestyle changes, namely weight loss and regular physical activity. In patients with abnormal glucose concentrations, dyslipidemia, or hypertension, treatment of the individual components of the syndrome may result in greater impact on reducing overall CVD risks. Given the prevalence of the MetS and the exaggerated CVD risks, innovative therapeutic approaches continue to evolve.[5]
Studies have shown that even in patients without diabetes, each of the MetS' risk factors, such as obesity, can increase inflammatory markers' levels and cardiovascular adverse events.[5,6,7] Ceriello and colleagues have shown that postprandial hyperglycemia and/or hypertriglyceridemia are associated with an increase of plasma levels of nitrotyrosine and inflammatory and thrombogenic biomarkers such as IL-6, soluble intercellular adhesion molecule (ICAM-1), soluble vascular cell adhesion molecule-1 (VCAM-1), and prothrombin fragment 1 + 2.[7,8,9] They showed that postprandial dysmetabolism was accompanied by oxidative stress and endothelial dysfunction in diabetic patients as well.
Many antidiabetic medications are only effective in glycemic control and have slight or no effect on inflammatory markers and cardiovascular adverse events.[10,11] Acarbose is an alpha-glucosidases inhibitor; a group of antidiabetic agents which are poorly absorbed. Acarbose is associated with lesser gastrointestinal side effects compared to other alpha-glucosidase inhibitors and was used as a single drug or in combination with other antidiabetic medications to control blood glucose levels in type 2 diabetic patients. Acarbose can lower HbA1C level by 0.5–1% and can reduce the incidence of type 2 diabetes in prediabetic patients by 36%.[12] This medication can reduce serum lipid levels, body weight, and blood pressure, and also decrease inflammatory markers and cardiovascular complications.[12,13,14] This study aims to compare the effect of acarbose and placebo on inflammatory markers and cardiovascular indexes in MetS patients among Iranian population.
Methods
This double-blind randomized clinical trial registered in the Iranian Registry of Clinical Trials with the code IRCT20130924014752N5. The research population included all the patients with MetS referred to Isfahan Endocrine and Metabolism Research Center between August 2016 and August 2017. Among them, 84 patients with MetS based on American Heart Association criteria[14] and endocrinologist's opinions were selected using nonrandom convenience sampling method. The patients were evaluated regarding the height and weight and after calculating BMI (BMI = weight/height2, weight [kg] and height [cm]) and the cases with BMI greater than or equal to 30 kg/m2 were included. Patients with the history of underlying diseases such as respiratory diseases and rheumatoid arthritis, those taking antidiabetic or lipid-lowering medication over the past year, using low-calorie diet to reduce weight over the past year, and patients with a history of drug abuse or cases of unwillingness to continue the study of intolerance of high drug dosage and complications were excluded from the study. After obtaining written consent from qualified patients, they were divided into two groups of 42 patients receiving acarbose and placebo using random allocation software.
At baseline, demographic information such as age, sex, and BMI as well as metabolic parameters including body weight and waist circumference (WC), fasting blood sugar (FBS), triglyceride (TG), total cholesterol (TC), high-density lipoprotein (HDL), low-density lipoprotein (LDL), CRP marker, and cardiovascular markers including flow-mediated dilation (FMD), intima-media thickness (IMT), and epicardial fat thickness (EFT) were measured and recorded. FMD; IM and pericardial fat thickness were measured via two-dimensional M-mode echocardiography. Endothelial function was assessed as FMD at the brachial artery. It should be noted that cardiovascular markers were measured by a cardiologist using Doppler ultrasonography (AtCor Medical, Solingen, Germany).
For patients in the acarbose group, treatment was initiated with 25 mg/day acarbose in the first week; and if the dosage was safe and well-tolerated, it was increased by 25 mg/day every week to a maximum dose of 100 mg/day within a month. The dosage was increased up to the maximum dose of 300 mg/day for 3 months and maintained for the second 3 months (a total of 6 months). Patients in the control group also received placebo in the same manner and they took these medications with their main meal to reduce gastrointestinal complications.
Response to treatment was considered if at least 5% of weight loss was achieved during the 6-month follow-up period, but if the patients had serious complications, they were excluded from the study. There were no severe drug side effects such as dehydration or elevated creatinine level. Only 10 patients were excluded from the acarbose group due to mild complications such as abdominal bloating, diarrhea and stool softening, and intolerance to increased drug dosage or unwillingness to continue the participation [Figure 1].
Figure 1.
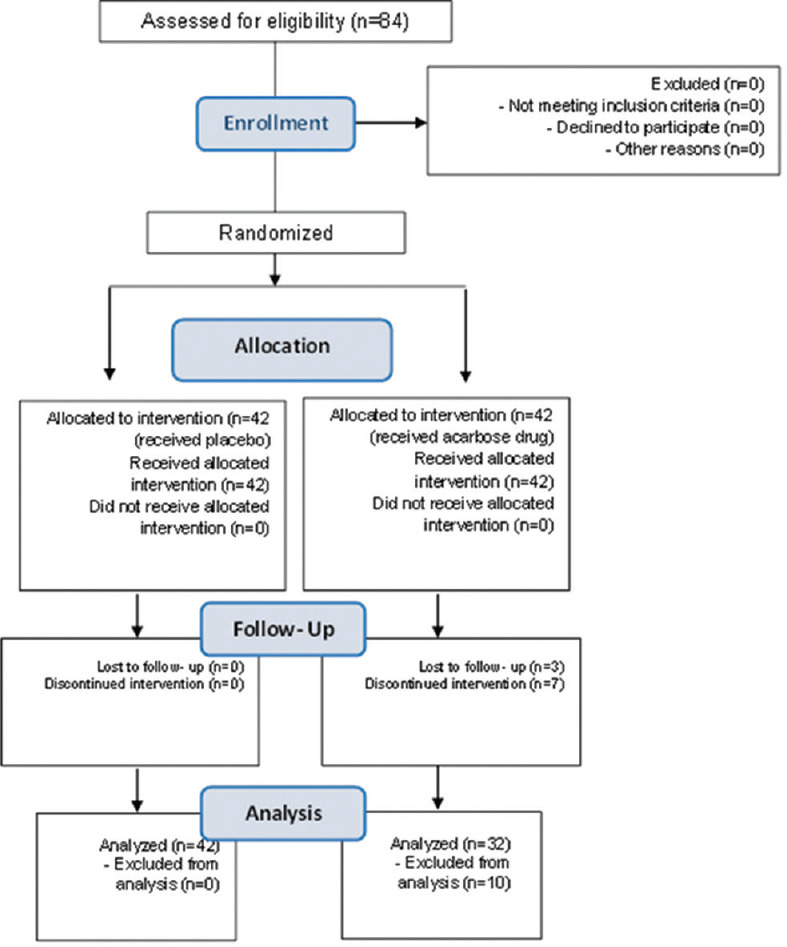
Flowchart consort
Acarbose drug was prepared by Amin Pharmaceuticals in the form of tablets and placebo was also used as the tablets similar to acarbose (in terms of color, appearance, and odor) and without any medicinal effect. Due to the double blindness of the present study, the patient and the researcher were not aware of the contents of the packages.
After 6 months, metabolic parameters including body weight, WC, FBS, TG, TC, HDL, and LDL, an inflammatory marker of CRP, and cardiovascular markers including FMD, IMT, EFT were assessed and recorded through blood tests.
Finally, the collected data were entered into SPSS software (Version 20) and considering the results of the Kolmogorov-Smirnov test for normal distribution, parametric tests such as independent t-test were used to compare the mean of quantitative variables between the two groups. A paired t-test was used to compare the mean of quantitative variables before and after intervention in both groups, and Chi-square test was used to compare the frequency distribution of gender between the two groups. In all analyses, the significance level was considered as <0.05.
Results
In the present study, from 32 patients in acarbose group, there were 25 (78.1%) females and 7 (21.9%) males with the mean age of 41.25 ± 7.71 years; and from 42 patients in the control group, 29 (69%) individuals were female and 13 (31.0%) were male with the mean age of 38.92 ± 9.05 years. The two groups were matched in terms of the mean age, sex, and BMI (P value > 0.05) [Table 1]. On the other hand, there was no significant difference between the two groups in the mean levels of metabolic parameters before intervention. However, after treatment, only HDL level in acarbose group with the mean value of 44.7 ± 7.6 was significantly higher than the control group (41.1 ± 6.4; P value = 0.043) and other metabolic parameters were not significantly different between two groups (P value > 0.05) [Table 2].
Table 1.
Demographic characteristic of the two groups
| Characteristics | Acarbose group | Control group | P |
|---|---|---|---|
| Sex | |||
| Female | 25 (78.1%) | 29 (69%) | 0.384† |
| Male | 7 (21.9%) | 13 (31.0%) | |
| Age; year | 41.25±7.71 | 38.92±9.05 | 0.248†† |
| BMI; kg/m2 | 38.11±5.02 | 36.12±4.66 | 0.082†† |
Data shown n (%) or mean±SD. BMI=Body mass index. †Use of Chi-square test for comparison of sex frequency distribution between two groups. ††Use of independent sample t-test for comparison of mean variables between two groups
Table 2.
Determination and comparison of the means of metabolic parameters before and after the intervention between the two study groups
| Variables | Time of intervention | Acarbose group | Control group | P† |
|---|---|---|---|---|
| Body weight (kg) | Before | 91.2±10.1 | 89.5±7.6 | 0.411 |
| After | 88.7±10.1 | 89.4±7.3 | 0.730 | |
| P†† | <0.001 | 0.640 | ||
| WC (cm) | Before | 103.7±7.4 | 101.6±6.8 | 0.209 |
| After | 101.5±7.2 | 101.5±6.7 | 1.00 | |
| P†† | <0.001 | 0.610 | ||
| FBS (mg/dl) | Before | 93.2±8.6 | 91.9±13.2 | 0.629 |
| After | 90.2±8.5 | 92.02±12.5 | 0.481 | |
| P†† | 0.090 | 0.960 | ||
| TC (mg/dl) | Before | 194.7±33.7 | 199.8±34.6 | 0.527 |
| After | 195.6±29.6 | 200.1±33.7 | 0.551 | |
| P†† | 0.840 | 0.690 | ||
| HDL (mg/dl) | Before | 42.3±7.8 | 40.7±7.3 | 0.374 |
| After | 44.7±7.6 | 41.1±6.4 | 0.043 | |
| P†† | 0.020 | 0.490 | ||
| LDL (mg/dl) | Before | 99.1±21.4 | 99.1±21.9 | 1.00 |
| After | 97.3±17.1 | 99.3±21.1 | 0.663 | |
| P†† | 0.500 | 0.730 | ||
| TG (mg/dl) | Before | 183.9±14.5 | 179.9±10.7 | 0.891 |
| After | 169.6±16.7 | 179.7±9.3 | 0.747 | |
| P†† | 0.520 | 0.900 |
Data shown mean±SD. WC=Waist circumference, FBS=Fasting blood sugar, TG=Triglyceride, TC=Total cholesterol, HDL=High-density lipoprotein, LDL=Low-density lipoprotein. †Use of independent sample t-test for the comparison of mean variables between two groups. ††Use of paired sample t-test for comparing mean variables after intervention versus before intervention in each group
In addition, the inflammatory marker evaluated in this study (CRP) was not significantly different between the two groups before intervention (P value > 0.05). After the intervention, despite a significant decrease in both groups (P-value < 0.05), CRP level in acarbose group with the mean of 0.43 ± 0.26 was significantly lower than the control group with the mean of 0.93 ± 0.38 (P-value < 0.001). In addition, cardiovascular markers including IMT, FMD, and EFT did not show any significant difference between the two groups before intervention (P-value > 0.05). But, after intervention, the mean CRP, IMT, and EFT levels in the acarbose group were significantly lower than the control group (P-value < 0.05). Additionally, the mean reduction in IMT and EFT levels in the acarbose group was significantly higher than the control group (IMT: −0.24 ± 0.39 vs −0.01 ± 0.06; P value = 0.001 and EFT: −0.89 ± 0.83 vs −0.43 ± 0.64; P value = 0.046). While there was no significant difference in mean reduction FMD between two groups (−0.02 ± 0.05 vs −0.01 ± 0.04; P value = 0.371) [Table 3].
Table 3.
Determination and comparison of the means of inflammatory and cardiovascular markers before and after the intervention between the two study groups
| Variables | Time of intervention | Acarbose group | Control group | P† |
|---|---|---|---|---|
| CRP | Before | 1.03±0.44 | 1.06±0.36 | 0.748 |
| After | 0.43±0.26 | 0.93±0.38 | <0.001 | |
| Change CRP | −0.60±0.47 | −0.14±0.42 | <0.001 | |
| IMT | Before | 0.74±0.14 | 0.68±0.15 | 0.083 |
| After | 0.49±0.40 | 0.67±0.16 | 0.009 | |
| Change IMT | −0.24±0.39 | −0.01±0.06 | 0.001 | |
| FMD | Before | 0.12±0.04 | 0.11±0.04 | 0.290 |
| After | 0.10±0.06 | 0.10±0.05 | 1.00 | |
| Change FMD | −0.02±0.05 | −0.01±0.04 | 0.371 | |
| EFT | Before | 2.72±1.26 | 2.87±0.88 | 0.548 |
| After | 1.83±0.68 | 2.45±0.62 | <0.001 | |
| Change EFT | −0.89±0.83 | −0.43±0.64 | 0.046 |
Data shown mean±SD. CRP=C-reactive protein, FMD=Flow-mediated dilation, IMT=Intima-media thickness, EFT=Epicardial fat thickness. †Use of independent sample t-test for comparison of mean variables between two groups
Discussion
MetS composed of central obesity, hyperglycemia, dyslipidemia, and hypertension is considered as the strongest predictor of CVDs and/or diabetes, and it is important as a medical emergency to control and prevent the side effects.[15]
Acarbose is an alpha-glucosidase inhibitor agent which has little systemic absorption (less than 2%). Gastrointestinal adverse events such as flatulence (78%) and diarrhea (14%) are the most common side effects of this medication.[12] Alpha-glucosidase inhibitors cause competitive, dose-dependent inhibition of alpha-glucosidase enzymes that hydrolyze nonabsorbable oligosaccharides and polysaccharides into absorbable monosaccharides and are located in the brush border of enterocytes. Acarbose lowers the level of postprandial blood glucose without increasing serum insulin levels. This drug can also reduce the HbA1C level by 0.5–1% thereby decreasing the incidence of type 2 diabetes in prediabetes individuals.[13] A study on 94 diabetic patients showed that acarbose alone can remarkably lower postprandial blood glucose. Acarbose also prolongs carbohydrate absorption time suggesting that it will be effective especially in patients with postprandial hyperglycemia who fail to achieve their glycemic goal through diet control.[15] A review article by Dinicolantonia et al. demonstrated that acarbose reduces blood glucose 60 min after meals and keeps it low for 5 hours. In accordance with previous studies, the current study showed that acarbose can lower blood glucose 60 and 120 min after meal.[16]
The results of our study showed that the level of serum HDL increased significantly after acarbose therapy but TC, TG, and LDL showed no significant changes after treatment. In a clinical trial on 711 diabetic patients, acarbose increased the level of serum HDL but did not affect serum TG levels. Another study performed on 10 healthy participants who received 300 mg/day acarbose for 3 weeks showed that the TG level decreased significantly but no changes were observed in serum HDL, LDL, and cholesterol levels. Dinicolantonio et al. concluded that acarbose can increase the level of serum HDL but cannot significantly change the level of TC. An investigation by Joshi et al. showed that acarbose could lower serum TG but did not change the serum levels of cholesterol, HDL, and LDL. Since the participants in most of these studies did not follow a similar diet, controversial results seem to be related to different fat and carbohydrate contents of participants' diet.
The present study showed that acarbose therapy is effective in reducing body weight and WC. The previous study revealed that acarbose decreases appetite and opposes unwanted fat storage by reducing food intake. A study conducted by Nakhaee et al. demonstrated that diabetic patients who received acarbose for 3 months followed a low-calorie diet and performed consistent physical exercises had greater weight loss compared to control group. Various studies suggested that acarbose induces weight loss in obese subjects.[17] A study by Zhang et al. revealed that acarbose consumption reduces body weight and waist and hip circumferences in diabetic patients. On the contrary, various studies conducted on Asian people have shown that acarbose was not effective in weight loss. In other words, this medication alone, without low-calorie diet and exercise, did not result in weight loss in Asian people. Controversies surrounding the effect of acarbose on weight loss seem to be due to the heterogeneity of calorie intake and physical activity in different study populations.[18]
Patients with MetS have two- to three-fold risk of developing CVDs.[13] Similarly, cardiovascular events are the leading cause of death and disability in patients with obesity, diabetes, and MetS.[14,15,16] It is well established that inflammation plays a major role in the pathogenesis of MetS and has an influence on the development of coronary heart disease.[17] Most antidiabetic drugs only lower blood glucose and have a slight impact on inflammatory markers. Metformin can suppress some of the inflammatory signaling pathways by increasing AMP-activated protein kinase activity besides its metabolic effects.[19,20] Newer sulfonylurea drugs such as gliclazide and glimepiride are more efficient in reducing inflammatory markers compared to other drugs of this group.[21,22,23] Some studies have demonstrated that acarbose can reduce blood pressure, lipid, body weight, inflammatory markers, and cardiovascular adverse events.[12,13,14] A study of these effects concluded that in diabetic patients who received acarbose, insulin resistance index, interleukin 6 (IL-6), and interleukin 1β (IL-1β) showed no significant reduction after 3 months of treatment.[24] Another study also did not find any significant change in IL-6, VCAM-1, ICAM-1, and hcCRP after 7 months of acarbose therapy.[25] The reason for these contradicting results maybe sex or ethnic differences or having other diseases such as diabetes or hypertension. In this study, we evaluated the effects of acarbose on inflammatory markers such as CRP and cardiovascular indexes EFT, IMT, and EFT in obese patients with MetS. CRP is available, inexpensive, well-established tools for the detection of inflammatory conditions. According to previous studies, cardiovascular indexes are also considered as well-known predictors of adverse cardiac events. The results demonstrated a significant decrease in CPR serum level after 6 months of treatment. IMT and EFT levels also decreased significantly after the treatment compared to baseline but we found no significant changes in the mean FMD level after treatment. In some of previous studies,[24,25,26] CPR did not decrease significantly after acarbose therapy. This might be related to patient selection such as selecting participants who suffer from inflammatory conditions other than cardiovascular inflammation. An important strength of current study is that we specifically studied diabetic patients with MetS while most previous studies assessed the effects of this medication on all diabetic patients. Another strength of our study is the use of the control group which allowed us to compare the effects of acarbose with placebo on the patients. A limitation of our study was its small sample size which prevents the results from being extrapolated to the overall population. Further studies with large enough sample sizes and controlling potential confounding variables such as age and sex are needed for a more generalized conclusion. Finally, frequent evaluation of variables throughout the study and assessing more variables can lead to more precise results.
Conclusions
According to the results of the present study, the administration of acarbose in patients with MetS can lead to weight loss, abdominal obesity reduction, and decreased levels of inflammatory and cardiovascular markers, including CRP, EFT, and IMT, and increased HDL in patients. Therefore, it may be suggested that acarbose can indirectly prevent the occurrence of cardiac problems by controlling metabolic parameters as well as reducing inflammatory markers; but, it seems necessary to do further researches in this area.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We appreciate all staff of Endocrine and Metabolism Research Center of Isfahan University of Medical Sciences and Dr. Fariborz Khorvash, Hasan Shemirani, and Maryam Zare for their contribution.
References
- 1.Limberg JK, Morgan BJ, Schrage WG. Peripheral blood flow regulation in human obesity and metabolic syndrome. Exerc Sport Sci Rev. 2016;44:116–22. doi: 10.1249/JES.0000000000000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jellinger PS, Handelsman Y, Rosenblit PD, Bloomgarden ZT, Fonseca VA, Garber AJ, et al. American association of clinical endocrinologists and American college of endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract. 2017;23(Suppl 2):1–87. doi: 10.4158/EP171764.APPGL. [DOI] [PubMed] [Google Scholar]
- 3.Han TS, Lean ME. A clinical perspective of obesity, metabolic syndrome and cardiovascular disease. JRSM Cardiovasc Dis. 2016;5:2048004016633371. doi: 10.1177/2048004016633371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Verma P, Srivastava RK, Jain D. Association of lifestyle risk factors with metabolic syndrome components: A cross-sectional study in Eastern India. Int J Prev Med. 2018;9:6. doi: 10.4103/ijpvm.IJPVM_236_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lau DC, Yan H, Dhillon B. Metabolic syndrome: A marker of patients at high cardiovascular risk. Can J Cardiol. 2006;22:85B–90B. doi: 10.1016/s0828-282x(06)70992-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Esser N, L'Homme L, De Roover A, Kohnen L, Scheen AJ, Moutschen M, et al. Obesity phenotype is related to NLRP3 inflammasome activity and immunological profile of visceral adipose tissue. Diabetologia. 2013;56:2487–97. doi: 10.1007/s00125-013-3023-9. [DOI] [PubMed] [Google Scholar]
- 7.Yamagishi S. Cardiovascular disease in recent onset diabetes mellitus. J Cardiol. 2011;57:257–62. doi: 10.1016/j.jjcc.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 8.Agrawal NK, Kant S. Targeting inflammation in diabetes: Newer therapeutic options. World J Diabetes. 2014;5:697–710. doi: 10.4239/wjd.v5.i5.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ceriello A, Giacomello R, Stel G, Motz E, Taboga C, Tonutti L, et al. Hyperglycemia-induced thrombin formation in diabetes: The possible role of oxidative stress. Diabetes. 1995;44:924–8. doi: 10.2337/diab.44.8.924. [DOI] [PubMed] [Google Scholar]
- 10.Esser N, Paquot N, Scheen AJ. Anti-inflammatory agents to treat or prevent type 2 diabetes, metabolic syndrome and cardiovascular disease. Expert Opin Investig Drugs. 2015;24:283–307. doi: 10.1517/13543784.2015.974804. [DOI] [PubMed] [Google Scholar]
- 11.Younk LM, Lamos EM, Davis SN. Cardiovascular effects of anti-diabetes drugs. Expert Opinion on Drug Safety. 2016;15:1239–57. doi: 10.1080/14740338.2016.1195368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singla RK, Singh R, Dubey AK. Important aspects of post-prandial antidiabetic drug, acarbose. Curr Top Med Chem. 2016;16:65–70. doi: 10.2174/1568026616666160414123500. [DOI] [PubMed] [Google Scholar]
- 13.Yamagishi S, Nakamura K, Takeuchi M. Inhibition of postprandial hyperglycemia by acarbose is a promising therapeutic strategy for the treatment of patients with the metabolic syndrome. Med Hypotheses. 2005;65:152–4. doi: 10.1016/j.mehy.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 14.Tsai SS, Chu YY, Chen ST, Chu PH. A comparison of different definitions of metabolic syndrome for the risks of atherosclerosis and diabetes. Diabetol Metab Syndr. 2018;10:5613. doi: 10.1186/s13098-018-0358-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ghobadi S, Rostami ZH, Marzijarani MS, Faghih S. Association of vitamin D status and metabolic syndrome components in Iranian children. Int J Prev Med. 2019;10:77. doi: 10.4103/ijpvm.IJPVM_242_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Di Nicolantonio JJ, Bhutani J, O'Keefe JH. Acarbose: Safe and effective for lowering postprandial hyperglycaemia and improving cardiovascular outcomes. Open Heart. 2015;2:e000327. doi: 10.1136/openhrt-2015-000327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nakhaee A, Sanjari M. Evaluation of effect of acarbose consumption on weight losing in non-diabetic overweight or obese patients in Kerman. J Res Med Sci. 2013;18:391. [PMC free article] [PubMed] [Google Scholar]
- 18.Schnell O, Weng J, Sheu WH, Watada H, Kalra S, Soegondo S, et al. Acarbose reduces body weight irrespective of glycemic control in patients with diabetes: Results of a worldwide, non-interventional, observational study data pool. J Diabetes Complications. 2016;30:628–37. doi: 10.1016/j.jdiacomp.2016.01.023. [DOI] [PubMed] [Google Scholar]
- 19.Foretz M, Guigas B, Bertrand L, Pollak M, Viollet M. Metformin: From mechanisms of action to therapies. Cell Metab. 2014:953–66. doi: 10.1016/j.cmet.2014.09.018. [DOI] [PubMed] [Google Scholar]
- 20.Grahame Hardie D. AMP-activated protein kinase: A key regulator of energy balance with many roles in human disease. J Intern Med. 2014;276:543–59. doi: 10.1111/joim.12268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rakel A, Renier G, Roussin A, Buithieu J, Mamputu JC, Serri O. Beneficial effects of gliclazide modified release compared with glibenclamide on endothelial activation and low grade inflammation in patients with type 2 diabetes. Diabetes Obes Metab. 2007;9:127–9. doi: 10.1111/j.1463-1326.2006.00571.x. [DOI] [PubMed] [Google Scholar]
- 22.Nicholls SJ, Tuzcu EM, Wolski K, Bayturan O, Lavoie A, Uno K, et al. Lowering the triglyceride/high-density lipoprotein cholesterol ratio is associated with the beneficial impact of pioglitazone on progression of coronary atherosclerosis in diabetic patients: Insights from the PERISCOPE (Pioglitazone Effect on Regression of Intravascular Sonographic Coronary Obstruction Prospective Evaluation) Study. J Am Coll Cardiol. 2011;57:153–9. doi: 10.1016/j.jacc.2010.06.055. [DOI] [PubMed] [Google Scholar]
- 23.Tung D, Cheung PH, Ciallella J, Saha S. Novel anti inflammatory effects of repaglinide in rodent models of inflammation. Pharmacology. 2011;88:295–301. doi: 10.1159/000333793. [DOI] [PubMed] [Google Scholar]
- 24.Scheen AJ, Esser N, Paquot N. Antidiabetic agents: Potential anti inflammatory activity beyond glucose control. Diabetes Metab. 2015;41:183–94. doi: 10.1016/j.diabet.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 25.Rudovich N, Weickert MO, Pivovarova O, Bernigau W, Pfeiffer AF. Effects of acarbose treatment on markers of insulin sensitivity and systemic inflammation. Diabetes Technol Ther. 2011;13:615–23. doi: 10.1089/dia.2010.0235. [DOI] [PubMed] [Google Scholar]
- 26.Derosa G, Maffioli P, Ferrari I, Fogari E, D'Angelo A, Palumbo I, et al. Acarbose actions on insulin resistance and inflammatory parameters during an oral fat load. Eur J Pharmacol. 2011;651:240–50. doi: 10.1016/j.ejphar.2010.11.015. [DOI] [PubMed] [Google Scholar]


