To the Editor: Worldwide reports describe cutaneous findings, including maculopapules, pseudo-chilblain, vesicles, urticaria, livedo, and multisystem inflammatory syndrome, as manifestations of coronavirus disease 2019 (COVID-19).1, 2, 3, 4, 5 Here, we report on the cutaneous findings observed in hospitalized COVID-19–positive patients at Columbia University Irving Medical Center by the adult dermatology consultation service between March 25, 2020, and May 1, 2020. Cases were included if COVID-19 was most likely associated with or contributed to skin findings observed after other potential causes were excluded. Although previous studies on the cutaneous manifestations of COVID-19 have focused primarily on outpatients and those with mild disease,2 , 3 this study provides insights into the cutaneous manifestations of severe disease. This study was approved by the institutional review board at Columbia University Irving Medical Center.
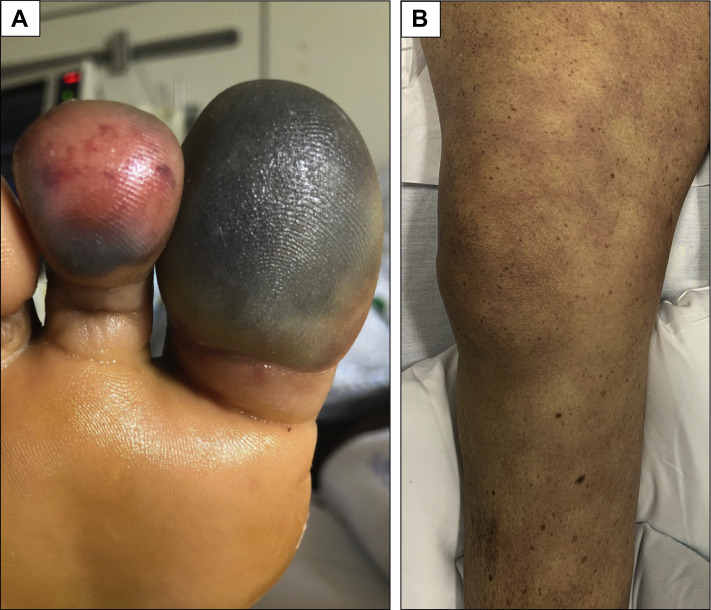
Nine patients developed signs of acral ischemia, including duskiness, necrosis, and bulla (Fig 1, A ). Eight of these patients with acral ischemia required admission to the intensive care unit, and the location of ischemia included fingers, toes, ears, and genital skin (Supplemental Table I available via Mendeley at https://data.mendeley.com/datasets/nywrhw3d8y/1). Two patients with severe lesions had a confirmed deep vein thrombosis, highlighting the potential for thrombotic events (cases 7 and 9).
Fig 1.
Acral ischemia in case 1 (A) and livedo reticularis in case 12 (B).
Three patients developed livedo racemosa, 1 of whom had livedo as a presenting sign of COVID-19 and 2 of whom developed livedo during their hospitalization. One patient developed vesicles in association with his livedoid eruption (case 10). All 3 patients required intensive care unit admission and had evidence of coagulopathy (cases 10 to 12) (Fig 1, B).
Two patients developed evidence of bleeding diatheses. One, a critically ill man in his 60s (case 14), developed petechiae, with perivascular lymphocytic infiltrate with prominent red blood cell extravasation on biopsy. He was mildly thrombocytopenic (114,000 per μL) and had mild coagulopathy (prothrombin time/international normalized ratio 14.7 seconds/1.2, activated partial thromboplastin time 36.2 seconds, and D-dimer 3.95 μg/mL). The other patient, a man in his 70s, developed purpura fulminans with areas of necrosis and superficial desquamation on the chest and axilla (case 13). Laboratory data were consistent with disseminated intravascular coagulation, and ultimately, the patient died.
Erythema multiforme–like lesions were observed in a woman in her 80s 1 week following discharge after treatment for COVID-19–associated pneumonia (case 15). She had no other risk factors for development of erythema multiforme–like lesions, including active herpes simplex virus infection, and received no new medications in the last 3 days of her hospitalization or on discharge.
No pseudo-chilblain (COVID toes) was observed in the hospitalized patients evaluated. Pseudo-chilblain may be more strongly associated with mild disease or present after acute illness has resolved.
In summary, cutaneous manifestations in hospitalized COVID-19 patients are varied and are an important part of this potentially life-threatening illness. Findings in critically ill patients may differ from those in outpatients with mild disease. Limitations of our study include that cases were limited to a single institution, there was a lack of histology on the majority of cases, and there was inability to establish the pathophysiologic role of severe acute respiratory syndrome coronavirus 2 in the reported skin diseases. Additionally, less severe skin findings may not have required dermatology consultation. Further large-scale cohort studies with classification of histology are necessary to better describe both the frequency and etiology of these findings.
Footnotes
Dr Strom and Author Trager contributed equally to this article.
Drs Samie and Geskin are co-senior authors.
Funding sources: None.
Conflicts of interest: None disclosed.
IRB approval status: Approved by Columbia University Irving Medical Center IRB AAAT2471.
Reprints not available from the authors.
References
- 1.Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34(5):e212–e213. doi: 10.1111/jdv.16387. [DOI] [PubMed] [Google Scholar]
- 2.Galván Casas C., Català A., Carretero Hernández G. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol. 2020;183(1):71–77. doi: 10.1111/bjd.19163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Masson A., Bouaziz J.D., Sulimovic L. Chilblains are a common cutaneous finding during the COVID-19 pandemic: a retrospective nationwide study from France. J Am Acad Dermatol. 2020;83(2):667–670. doi: 10.1016/j.jaad.2020.04.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jia J.L., Kamceva M., Rao S.A. Cutaneous manifestations of COVID-19: a preliminary review. J Am Acad Dermatol. 2020;83(2):687–690. doi: 10.1016/j.jaad.2020.05.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shulman S.T. Pediatric coronavirus disease-2019–associated multisystem inflammatory syndrome. J Pediatr Infect Dis Soc. 2020;9(3):285–286. doi: 10.1093/jpids/piaa062. [DOI] [PMC free article] [PubMed] [Google Scholar]