Aim
to compare anulom vilom pranayama (AVP), kapal bhati pranayama (KBP), diaphragmatic breathing exercises (DBE), and pursed-lip breathing (PLB) for breath holding time (BHT) and rating of perceived exertion (RPE). Methods- Participants were assessed for BHT and RPE, before training on any one intervention using online platforms, for one week during lockdown from COVID-19.15 participants in each group total N = 60 at- (α – 0.05), (1- β – 0.90) & (effect size - 0.55); were analysed. Results - AVP & DBE decreased RPE (p < 0.000). KBP & PLB did not decrease RPE as compared to AVP & DBE (p. > 0.05). DBE increased BHT more than KBP & PLB interventions (p < 0.05), but not more than AVP (p > 0.05). One-way ANOVA of four interventions revealed significant variation for RPE change (p < 0.05), for AVP. Conclusions - AVP reduces RPE maximally during breath-holding, whereas DPE increases BHT more.
Keywords: Diaphragmatic breathing, Pranayama, Kapal bhati, Anulom vilom, Pursed-lip breathing
Highlights
-
•
Breathing interventions effectively decrease anxiety & increase breath holding time.
-
•
Anulom vilom pranayama lowers anxiety efficiently.
-
•
Diaphragmatic breathing exercise increases breath holding time efficiently.
1. Introduction
Human breathing is a synergistic process that is under autonomic nervous control continuously, and can also be controlled voluntarily at will, and thus reflects in various breathing patterns [1]. Pranayama is a term that is associated with astanga yoga and deals with formal and traditional practice of control of breath and is intended for regulation of prana – the life-force [2]. Pranayama is controlling the breathing process in a therapeutic way, leading to improvement of the pulmonary reserve function, and efficient neurological control at a basic and obvious level [2]. Anulom vilom pranayama (AVP) is alternate nostril breathing which regulates higher autonomic tone, Kapal bhati pranayama (KBP) is a cerebral detox with bellows of breath in and out with inward contraction of abdominal wall [2]. Breathing exercise as Diaphragmatic breathing exercises (DBE) and Pursed Lip Breathing (PLB) are popular forms [3] that help to improve the process of breathing. During lockdown of COVID-19 online interventions were given to increase breath holding time at lower level of perceived exertion. Anulom Vilom Pranayama (AVP), Kapal Bhati Pranayama (KBP) are investigated in this study along with certain breathing exercises that are also popular like Diaphragmatic Breathing Exercises (DBE) and Pursed Lip Breathing Exercises (PLBE) for supporting the pulmonary volumes and capacities checked using breath holding time (BHT) [4], and rating of perceived exertion (RPE) [5], values (see Table 1, Table 2, Table 3, Table 4 , Fig. 1, Fig. 2 ).
Hypotheses
H0- There is no significant relative superiority of various breathing interventions (pranayamas & breathing exercises) over each other for breath holding time (BHT) and rating of perceived exertion (RPE).
Table 1.
Descriptive and Demographic data of all four groups, (N = 60) Anulom Vilom Pranayama (AVP), Kapal Bhati Pranayama (KBP), Diaphragmatic Breathing exercise (DBE) and Pursed Lip Breathing exercise (PLB).
| SN | Variable | AVP n-15 | KBP n-15 | DBE n-15 | PLB n-15 |
|---|---|---|---|---|---|
| 1 | Age (years) | 22.13 ± 1.06 | 21.9 ± 0.90 | 21.47 ± 0.64 | 23.06 ± 2.79 |
| 2 | BMI (kg/m2) | 22.1 ± 3.79 | 20.92 ± 2.87 | 20.97 ± 1.67 | 22.33 ± 3.24 |
| 3 | M:F | 7:8 | 11:4 | 8:7 | 9:6 |
Table 2.
Independent t-test values (p-value) between all four groups of different interventions (AVP, DBE, KBP & PLB intergroup comparison) at pre post intervention for breath holding time (BHT) and rating of perceived exertion (RPE) at various points of time, level of significance * taken at p < 0.05.
| SN | Variables and groups | Independent t-test values |
|
|---|---|---|---|
| Pre-Intervention t-value (p value) | Post-Intervention t-value (p value) | ||
| 1 | BHT AVP - KBP | 0.23 (0.82) | −0.10 (0.92) |
| 2 | BHT AVP - DBE | −1.26 (0.21) | −2.0 (0.055) |
| 3 | BHT AVP -PLB | −0.17 (0.86) | −0.07 (0.94) |
| 4 | BHT KBP - DBE | 1.85 (0.07) | 2.57 (0.015) * |
| 5 | BHT KBP - PLB | −0.49 (0.62) | 0.02 (.98) |
| 6 | BHT DBE -PLB | 1.23 (.22) | 2.3 (0.02) * |
| 7 | Increment in time AVP - KBP | −0.89 (0.38) | |
| 8 | Increment in time AVP - DBE | −2.7 (0.011) * | |
| 9 | Increment in time AVP - PLB | 0.26 (0.79) | |
| 10 | Increment in time KBP - DBE | 1.21 (0.24) | |
| 11 | Increment in time KBP - PLB | 0.83 (0.41) | |
| 12 | Increment in time DBE -PLB | 2.01 (0.05) * | |
| 13 | RPE AVP - KBP | 1.99 (0.056) | 0.25 (0.80) |
| 14 | RPE AVP - DBE | 1.73 (0.09) | 0.76 (0.45) |
| 15 | RPE AVP - PLB | 1.65 (0.11) | −0.46 (0.64) |
| 16 | RPE KBP - DBE | 1.29 (0.21) | −0.13 (0.89) |
| 17 | RPE KBP - PLB | −0.42 (0.67) | −0.55 (0.58) |
| 18 | RPE DBE -PLB | .85 (0.40) | −0.84 (0.40) |
| 19 | RPE change AVP - KBP | 2.97 (0.006) * | |
| 20 | RPE change AVP - DBE | −1.08 (0.28) | |
| 21 | RPE change AVP - PLB | 3.89 (0.0005) * | |
| 22 | RPE change KBP - DBE | 3.5 (0.0015) * | |
| 23 | RPE change KBP - PLB | 0.15 (0.88) | |
| 24 | RPE change DBE -PLB | 4.53 (.0001) * | |
Table 3.
Paired t-test values (p value) for breath holding time (BHT) and rating of perceived exertion (RPE) for different pranayamas and breathing exercises, pre and post intervention, (within group comparison) level of significance * taken at p < 0.05.
| SN | Variable/Group | Pre-Intervention | Post-Intervention | Paired “t” value (p value) |
|---|---|---|---|---|
| 1 | BHT for AVP | 43.00 ± 20.33 | 51.47 ± 22.32 | −11.71 (0.0000) * |
| 2 | BHT for KBP | 41.60 ± 12.38 | 52.13 ± 12.73 | −4.80 (0.0003) * |
| 3 | BHT for DBE | 51.53 ± 16.61 | 65 .60 ± 15.81 | −7.29 (0.0000) * |
| 4 | BHT for PLB | 44.20 ± 15.92 | 52.00 ± 16.58 | −3.18 (0.0065) * |
| 5 | RPE for AVP | 4.60 ± 0.83 | 3.20 ± 0.86 | 10.69 (0.0000) * |
| 6 | RPE for KBP | 3.33 ± 2.32 | 3.07 ± 1.91 | 0.74 (0.47) |
| 7 | RPE for DBE | 4.13 ± 0.64 | 3.06 ± 0.53 | 12.47 (0.0000) * |
| 8 | RPE for PLB | 3.67 ± 2.02 | 3.47 ± .06 | 0.715 (0.46) |
Table 4.
One Way ANOVA of different variables (BHT, RPE, increment in BHT & change in RPE) for Pranayamas and Breathing exercises (AVP, KBP, DBE & PLB), pre and post intervention with their F values & p – values. Only RPE change is significant at a p-value of <0.05 with maximum decrease (of more than one gradation unit) seen in AVP followed by DBE.
| SN | Variable/Group | Anulom Vilom Pranayama Mean ± SD | Kapal Bhati Pranayama Mean ± SD | Diaphragmatic Breathing exercise Mean ± SD | Pursed Lip Breathing exercise Mean ± SD | F Value | p-value |
|---|---|---|---|---|---|---|---|
| 1 | Pre- Breath holding time, sec | 43 ± 20.34 | 41.6 ± 12.38 | 51.53 ± 16.61 | 44.2 ± 15.92 | 1.07 | 0.36 |
| 2 | Post- Breath holding time, sec | 51.46 ± 22.31 | 52.13 ± 12.73 | 65.6 ± 15.81 | 52 ± 16.58 | 2.39 | 0.07 |
| 3 | Increment in time, sec | 8.45 ± 2.8 | 10.53± | 14.06 ± 7.5 | 7.8 ± 9.5 | 2.1 | 0.10 |
| 4 | Pre RPE | 4.6 ± .82 | 3.33 ± 2.32 | 4.13 ± .64 | 3.67 ± 2.02 | 1.73 | 0.17 |
| 5 | Post RPE | 3.2 ± .86 | 3.0 ± 1.9 | 3.06 ± .53 | 3.46 ± 2.07 | .28 | .835 |
| 6 | RPE change | 1.40 ± 0.50 | 0.27 ± 1.39 | 1.06 ± 0.50 | 0.2 ± 1.08 | 9.0 | .000** |
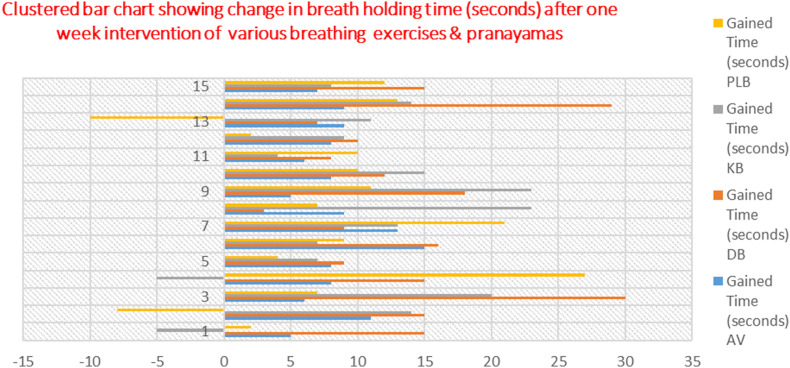
Fig. 1.
Clustered bar chart showing changes in BHT in seconds from pre level seen as increase or decrease in the time for all four interventions AVP, KBP, DBE & PLB. Maximum gain in time is seen for DBE & AVP there are few negative direction bars for PLB and KBP showing decrease or less gain in BHT.
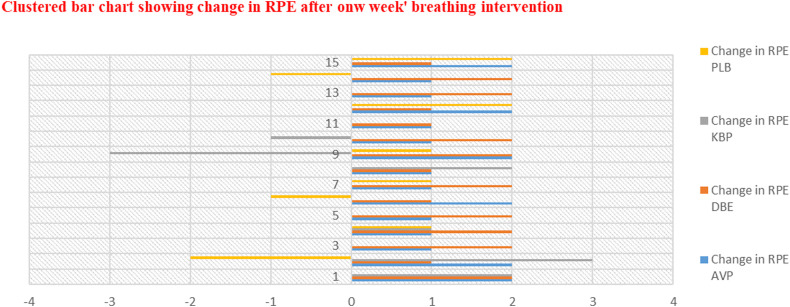
Fig. 2.
Clustered bar chart showing changes in RPE from pre intervention seen as less or more change in RPE level for all four interventions AVP, KBP, DBE & PLB. Maximum increased change in RPE is for AVP & DBE in positive direction signifying reduction in RPE, however changes for PLB and KBP are towards negative direction it means no change or reverse change (increase in RPE).
2. Materials and methods
Ethical approval was given by institutional committee of NTCC AIPT, AUUP. All participants gave written informed consent to participate in the study. Google forms were used for data collection.
Subject selection- As per the inclusion and exclusion criteria a total of 75 participants were included and randomly allocated to each of the four groups using chit method. Data has been described (table −1) and analysed for 60 participants with 15 in each group who completed one-week’ intervention. Out of 15 excluded there are 10 dropouts (2 DBE, 3 KBP, 4 PLB and 1 from ABP group), 5 individuals were not able to complete the online assessment due to technical failure/non-compliance. Interventions were demonstrated using video-based IT platforms like WhatsApp and video calls by two trained physiotherapists who were certified for pranayama training. Data was recorded using the same platforms online.
2.1. Selection criteria
Inclusion criteria- both male and female individuals, age >18 years, ability to use online platform
Exclusion criteria- any coexisting pulmonary condition like Asthma, Smoking, Chest wall deformities, Obesity.
Microsoft office Professional plus 2016′ excel software was used for data analysis. Student's paired and independent t-test comparison for significant difference of means was done for all four groups. One-way ANOVA was also used to check significant difference among all four groups for BHT and RPE.
2.2. Online platform – WhatsApp and skype video calls
Sample Size & power calculation – Sample size was calculated using G*Power software for one-way ANOVA using 4 groups with – (α – 0.05), (1- β – 0.90) & and (effect size - 0.55). Thus, a total of 52 sample size was derived, however for symmetrical distribution a minimum of 15 per sample of total 60 sample size was used by us for analyses from a total enrolled 75 participants.
Pranayama/Breathing exercise protocol- It comprised of 1-week duration of intervention with two sessions/day: each session of three repetitions initially. Every repetition consisted of one round of intervention i.e. - 10–15 times followed by a brief rest (normal breathing) of <1 min (one repetition). Such 3 repetitions were given initially & advanced till 10 repetitions (one session) by last day of the week. In this manner participants practised 3 sessions twice a day, for a total duration of about 10–20 min every day.
AVP and KBP were described and demonstrated in the video as per the Patanjali Yoga Petha description. Breathing exercises were also demonstrated using video - demonstration.
Instructions for interventions - Standard instructions were provided to the participants for all interventions using videos-based IT platforms. They were advised to be relaxed and follow the steps gradually. Detailed explanations were given to them, for correct performance of the intervention using video demonstration. Instructions were also given using local language. The exact instructional syntax is provided in Appendix A.
Assessment of outcome: Pre intervention and post intervention breath holding time [4] and rating of perceived exertion on a Borg's scale of 6–20 [5] were done for finding out the effects of the intervention.
Recording of Breath holding time- The participants were required to make a maximum expiration followed by a maximum inspiration and to hold the breath as long as possible at maximum inspiratory level. This procedure was repeated three times. The best value was used for further analysis.
Recording of rating of perceived exertion (RPE) - Borg's 15 grade category rating scale for perceived exertion (RPE). There is a possible relation between physiological and psychological variables for favourable outcome. The assessment of psychological perception of physiological stress to breath holding task can be very valuable in this regard. Standard form of RPE 6–10 scale was used [5].
3. Results & discussion
Average age of (N = 60) participants (21–26 years) for all groups is shown in the Table. 1. All groups had comparable age mean ± SD values. All groups had normal BMI (>18 & < 23 kg/m2) as seen in Mean ± SD value. Both males and females participated in the study as per the ratio seen in table −1.
It is seen in independent t-test that KBP & PLB did not decrease RPE as compared to AVP & DBE (p.0.05). DBE increased BHT more than KBP & PLB interventions (p < 0.05), but not more than AVP (p > 0.05). (Table. 2). DBE and KBP both are working on the respiratory diaphragmatic mechanics which is the main muscle of inspiration, but in DBE the work is on the piston movement of diaphragm, on the lower ribs and abdominal compliance [6], which is the prime bio-mechanical movement for inspiration. In KBP the abdominals move inward and outward supplementing the diaphragm in a stimulating manner, however it increases ventilator mechanics it does not specifically changes the diaphragmatic excursion. AVP increase the duration of inspiration similar to DBE, which does not happen in KBP and PLB. PLB rather decreases the inspiration time and increases the expiration time, which is useful for clinical populations [7].
All the four interventions were effective in increasing the breath holding time significantly p < 0.000 from pre intervention values as seen in paired t-test analysis as seen in table - 3. Only AVP & DBE decreased RPE simultaneously (p < 0.000). Highest t value is seen for BHT of AVP amongst all four groups. Highest t value is seen for RPE of DBE amongst all four groups. AVP works on the autonomic nervous system and is known to be a slow pranayama practice as compared to KBP, AVP has been shown [8] to improve the parasympathetic activity as compared to KBP. However, DBE are also known to be sympatholytic and improve the parasympathetic activity [9]. Therefore, as seen in figure −2 both AVP & DBE are producing changes in RPE post training.
One-way ANOVA among all four interventions could show significant variation for RPE change only (p < 0.05), with maximum reduction by AVP. No difference is seen for any other variable among the four groups. This is suggestive of overall superiority of AVP to decrease the affective aspect of breath holding. The nature of AVP pranayama is of cooling the exaggerated sympathetic response [2,8].
Out of the two pranayamas and two breathing exercises compared in this study, AVP and DBE have shown significant change in RPE levels during maximum voluntary breath holding after one week’ training. Pranayamas are known to improve sympathovagal balance [11]. There is no difference if we compare both of them in an independent t-test. Breath holding time increased significantly for DBE as compared to PLB and KBP but there was no difference with AVP (table-2).
Certain negative deflections of RPE are seen for KBP and PLB as seen in figure −2. Thus, KBP and PLB may be stimulating the sympathetic wing of autonomic nervous system [2].
It has been reported that pranayama can improve the pulmonary functions [12], thus these findings are important as preventive measures during the COVID-19 related lockdown to overcome the health risk of lockdown [13]. Various pranayamas [14] are known to improve the physiological parameters and same results are seen in this study. There is an association between anxiety and respiratory pathologies [15]. The scaling of COVID-19, by communication channels worldwide, has produced a psychiatric component associated with this pandemic [16]. It leads to “coranophobia” a newly found panic psychosis [17]. Healthcare workers suffer from it [18], AVP pranayama and DBE are two interventions which may become prescriptive for this.
Null hypothesis H0 was rejected based on these findings.
3.1. Limitations
In the present study video based instructions were given for breathing interventions, such interventions are found in previous studies [10], however a face to face teaching is better method.
4. Conclusions and implications
AVP is best among studied interventions for increasing relaxation during breath holding, and DBE increases breath holding time maximally. Thus, a combination of AVP and DBE may be best during lockdown to increase the pulmonary reserve and decrease anxiety of normal individuals. It is useful as promotive health practices during COVID-19.
Financial Support
Nil.
Copyright/patent/royalty
Nil.
CRediT authorship contribution statement
Mayank Shukla: Conceptualization, Methodology, Formal analysis, Writing - review & editing. Diksha Chauhan: Investigation, Writing - original draft. Ritu Raj: Investigation, Writing - original draft.
Declaration of competing interest
Authors declare no conflict of Interest.
Acknowledgments
We would like to acknowledge all participants of the study for their valuable time and cooperation.
Appendix A.
Important points which were emphasized are underlined in the paragraph below
KBP-“Please sit on the floor on a mat with back straight and legs crossed. Take slow breaths and relax. Make a forceful exhalation by contracting abdominal muscles followed by a usual inhalation, relaxing the abdominal muscles. There must be no effort in inhalation.” AVP-“Please sit on the floor on a mat with back straight and legs crossed. Relax neck and shoulder muscles. Inhale slowly through right nostril closing the left nostril, exhale fully through the left one closing the other one, repeat this in cyclic manner. The mouth shall remain closed.” PLB-“Please sit erect on a chair with feet supported. Relax neck and shoulder. Inhale slowly through nose like you were going to, smell the roses. Purse lips like you were going to, whistle. Exhale slowly through pursed lips like, blowing out a candle. Try to blow out twice as long, as it took to inhale.” DBE-“Please sit erect on a chair with feet supported. Relax neck and shoulder. Keep hands on abdomen. Inhale slowly and deeply through nose as if to, inflate the abdomen. Feel the rise of abdomen with hands. Exhale through the mouth completely.”
References
- 1.Jaworski J., Bates J.H. Sources of breathing pattern variability in the respiratory feedback control loop. J. Theor. Biol. 2019;469:148–162. doi: 10.1016/j.jtbi.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 2.Sengupta P. Health impacts of yoga and pranayama: a state-of-the-art review. Int. J. Prev. Med. 2012;3(7):444. [PMC free article] [PubMed] [Google Scholar]
- 3.Kisner, Carolyn. Therapeutic exercise: foundations and techniques/carolyn kisner, lynn allen colby; illustrations by jerry L. Kisner.—fourth ed. p. Cm. Includes Bibliographical References and Index. ISBN 0-8036-0968-X.
- 4.Parkes M.J. Breath‐holding and its breakpoint. Exp. Physiol. 2006;91(1):1–5. doi: 10.1113/expphysiol.2005.031625. [DOI] [PubMed] [Google Scholar]
- 5.Scherr J., Wolfarth B., Christle J.W., Pressler A., Wagenpfeil S., Halle M. Associations between Borg's rating of perceived exertion and physiological measures of exercise intensity. Eur. J. Appl. Physiol. 2013;113(1):147–155. doi: 10.1007/s00421-012-2421-x. [DOI] [PubMed] [Google Scholar]
- 6.Troyer A.D., Wilson T.A. Action of the diaphragm on the rib cage. J. Appl. Physiol. 2016;121(2):391–400. doi: 10.1152/japplphysiol.00268.2016. [DOI] [PubMed] [Google Scholar]
- 7.Bianchi R., Gigliotti F., Romagnoli I., Lanini B., Castellani C., Grazzini M., Scano G. Chest wall kinematics and breathlessness during pursed-lip breathing in patients with COPD. Chest. 2004;125(2):459–465. doi: 10.1378/chest.125.2.459. [DOI] [PubMed] [Google Scholar]
- 8.Sharma V.K., Dinesh T., Rajajeyakumar M., Grrishma B., Bhavanani A.B. Impact of fast and slow pranayam on cardio vascular autonomic function among healthy young volunteers: randomized controlled study. Altern Integr Med. 2018;7(1000265):2. [Google Scholar]
- 9.Kulur A.B., Haleagrahara N., Adhikary P., Jeganathan P.S. Effect of diaphragmatic breathing on heart rate variability in ischemic heart disease with diabetes. Arq. Bras. Cardiol. 2009;92(6):423–463. doi: 10.1590/s0066-782x2009000600008. [DOI] [PubMed] [Google Scholar]
- 10.Slader C.A., Reddel H.K., Spencer L.M., Belousova E.G., Armour C.L., Bosnic-Anticevich S.Z., Thien F.C., Jenkins C.R. Double blind randomised controlled trial of two different breathing techniques in the management of asthma. Thorax. 2006;61(8):651–656. doi: 10.1136/thx.2005.054767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Santaella D.F., Devesa C.R., Rojo M.R., Amato M.B., Drager L.F., Casali K.R., Montano N., Lorenzi-Filho G. Yoga respiratory training improves respiratory function and cardiac sympathovagal balance in elderly subjects: a randomised controlled trial. BMJ open. 2011;1(1) doi: 10.1136/bmjopen-2011-000085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mooventhan A., Khode V. Effect of Bhramari pranayama and OM chanting on pulmonary function in healthy individuals: a prospective randomized control trial. Int. J. Yoga. 2014;7(2):104. doi: 10.4103/0973-6131.133875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lippi G., Henry B.M., Bovo C., Sanchis-Gomar F. Health risks and potential remedies during prolonged lockdowns for coronavirus disease 2019 (COVID-19) Diagnosis. 2020;7(2):85–90. doi: 10.1515/dx-2020-0041. [DOI] [PubMed] [Google Scholar]
- 14.Waghmare P., Baji P.S. Effect of pranayama on cardio-respiratory efficiency. Indian J. Basic Appl. Med. Res. 2013;8(2):918–922. [Google Scholar]
- 15.Smoller J.W., Pollack M.H., Otto M.W., Rosenbaum J.F., Kradin R.L. Panic anxiety, dyspnea, and respiratory disease. Theoretical and clinical considerations. Am. J. Respir. Crit. Care Med. 1996;154(1):6–17. doi: 10.1164/ajrccm.154.1.8680700. [DOI] [PubMed] [Google Scholar]
- 16.Zarghami M. Psychiatric aspects of Coronavirus (2019-nCoV) infection. Iran J Psychiatry Behav Sci. 2020;14(1) [Google Scholar]
- 17.Asmundson G.J., Taylor S. Coronaphobia: fear and the 2019-nCoV outbreak. J. Anxiety Disord. 2020;70:102196. doi: 10.1016/j.janxdis.2020.102196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Amin S. The psychology of coronavirus fear: are healthcare professionals suffering from corona-phobia? Int. J. Healthc. Manag. 2020:1–8. [Google Scholar]