Abstract
Background
Healthcare workers (HCWs) are at the forefront of fighting against the COVID-19 pandemic. However, they are at high risk of acquiring the pathogen from infected patients and transmitting to other HCWs. We aimed to investigate risk factors for nosocomial COVID-19 infection among HCWs in a non-COVID-19 hospital yard.
Methods
Retrospective data collection on demographics, lifestyles, contact status with infected subjects for 118 HCWs (including 12 COVID-19 HCWs) at Union Hospital of Wuhan, China. Sleep quality and working pressure were evaluated by the Pittsburgh Sleep Quality Index (PSQI) and The Nurse Stress Index (NSI), respectively. The follow-up duration was from Dec 25, 2019, to Feb 15, 2020.
Results
A high proportion of COVID-19 HCWs had engaged in night shift-work (75.0% vs. 40.6%) and felt working under pressure (66.7% vs. 32.1%) than uninfected HCWs. SARS-CoV-2 infected HCWs had significantly higher scores of PSQI and NSI than uninfected HCWs (P < 0.001). Specifically, scores of 5 factors (sleep quality, sleep time, sleep efficiency, sleep disorder, and daytime dysfunction) in PSQI were higher among infected HCWs. For NSI, its 5 subscales (nursing profession and work, workload and time allocation, working environment and resources, patient care, management and interpersonal relations) were all higher in infected than uninfected nurse. Furthermore, total scores of PSQI (HR = 2.97, 95%CI = 1.86−4.76; P <0.001) and NSI (HR = 4.67, 95%CI = 1.42−15.45; P = 0.011) were both positively associated with the risk of SARS-CoV-2 infection.
Conclusion
Our analysis shows that poor sleep quality and higher working pressure may increase the risk of nosocomial SARS-CoV-2 infection among HCWs.
Keywords: SARS-CoV-2, Risk factors, Healthcare workers, Pittsburgh sleep quality index, The nurse stress index
Highlights
-
•
Risk factors of the susceptibility of HCWs to COVID-19 remained largely unknown.
-
•
Infected HCWs had poorer sleep quality and higher working pressure than uninfected.
-
•
Poor sleep quality and high working pressure were associated with COVID-19 risk.
-
•
Improving the night duty system, decreasing psychological pressure is necessary for HCWs.
1. Introduction
In December 2019, pneumonia with previously unknown etiology began to spread in Wuhan, Hubei province in China. The causative virus of this disease was soon identified as a novel coronavirus, and it was preliminarily named as the 2019 novel coronavirus (2019-nCoV). This virus was later renamed as SARS-CoV-2, and pneumonia it causes was named 2019 novel coronavirus diseases (COVID-19) by the World Health Organization (WHO). As with other infectious disease outbreaks, healthcare workers (HCWs) have been at the front line of the fight against COVID-19. However, hospitals are vulnerable to infectious disease spread through rapid patients-HCWs and HCWs–HCWs cross-infection, especially when dealing with a disease of unknown or not well-known etiology as it was the case during the early phase of the COVID-19 outbreak [[1], [2], [3]].
A recent study from the Chinese Center for Disease Control and Prevention showed that a total of 1716 HCWs had been diagnosed with COVID-19, including 5 deaths by Feb 11, 2020, with a crude case fatality rate of 0.3% [4]. This situation resulted in a shortage of HCWs and the collapse of the medical system, even though Wuhan had high-quality medical resources [5]. Thousands of HCWs from various provinces in China were needed to ease the strain on the Wuhan medical system and support the response to the epidemic. Since then, similar scenarios have been observed in various countries. For example, reports from Italy indicated that 20% of responding HCWs were infected with COVID-196, and in Spain, HCWs infected with COVID-19 accounts for around 12% of all confirmed cases [7]. Therefore, the establishment of protection guidelines for HCWs is an important step to fight against COVID-19, and is the most important bridge that prevents the collapse of the medical system and reduces social panic. However, the specific reasons for the infection of HCWs and the failure of protection still need to be fully investigated [8].
Before public health interventions were implemented by the Chinese government on Jan 23, 2020, the COVID-19 had already spread to HCWs unknowingly treating patients infected with the virus. Little is known of risk factors for nosocomial COVID-19 infection among HCWs prior to this date, as there is no existing peer-reviewed literature quantifying the transmissibility of SARS-CoV-2 among HCWs during that period. Besides, the dynamics of COVID-19 spread among HCWs largely remained unknown. In the present study, we conducted a retrospective study of a COVID-19 outbreak among HCWs in the Department of Neurosurgery, which is not a COVID-19 hospitalization yard in Union Hospital in Wuhan. Their information before the phase of the big outbreak of COVID-19, including epidemiological, demographical, and lifestyles were collected. We investigated the risk factors that play roles in the susceptibility of HCWs to COVID-19.
2. Materials and methods
2.1. Study design and participants
We carried out this single-center respective cohort study in the Department of Neurosurgery, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China. The nucleic acid testing for SARS-CoV-2 by RT-PCR tests showed 14 of 171 HCWs (an infection rate of 8.19%) in this single-center were infected with SARS-CoV-2 by a hospitalized patient who was later diagnosed with COVID-19 and defined as the index case. Out of the 14 COVID-19 HCWs, 12 participants with complete questionnaire data were enrolled in this study. The participants reported they do not have a history of contacting other infected cases and also their family members have not been previously infected. To acquire the information of the history of HCWs’ contact with other infected cases, they were asked about the following question in the questionnaire: (1) Have you ever contacted with other infected cases inside or outside the hospital? (2) Were your close colleagues or family members infected? If “yes”, they were further asked whether they were diagnosed or developed clinical manifestations (e.g., fever, nonproductive cough, dyspnea, fatigue, and radiographic evidence of pneumonia) earlier than their contacts. This study was approved by the institutional ethics board of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology (No. 20200029). All participants provided informed consent using an online form, and they were assured of the only academic use of the collected data.
2.2. Data collection and assessment
An online electronic questionnaire was sent to all 171 HCWs in the Department of Neurosurgery of Union Hospital of Wuhan, and 118 valid questionnaires were finally collected, including the questionnaires from 12 COVID-19 HCWs (including 4 doctors and 8 nurses), and 106 uninfected HCWs. Baseline demographics (age, gender, height, weight, education level), lifestyle factors (physical activity, smoking status, and alcohol drinking status, diet), medical post, and chronic medical diseases were gathered. For all HCWs, their data on sleep quality were assessed by the Pittsburgh Sleep Quality Index (PSQI) [9], and for nurses, their feeling of working under pressure was further evaluated by The Nurse Stress Index (NSI) [10]. The contact status with the identified COVID-19 cases was also collected. A detailed description of these data as described in the Supplementary Materials.
We used several methods to minimized recall bias. First, the online questionnaires were filled out as soon as HCWs completed their nucleic acid testing to minimize the time-interval between memory acquisition and exposure. Second, the data of the exposure to the index cases and infected colleagues, as well as their night duty information were matched to their daily work records in the department. Third, 8 of the 118 valid questionnaires were re-filled out (within a two-week interval) by the same participants, which showed good consistency (Kappa = 0.871). The data on the use of personal protective equipment (PPE) (e.g., surgical masks, non-surgical masks, disposable gloves, safety glasses, and protective clothing) in the early stages before an outbreak were also collected. But this data was not shown in the following analysis due to the low utilization rate of PPE in daily work in a non-infectious ward. The follow-up duration for each HCWs was calculated as the number of days between Dec 25, 2019 (the hospital admission time of the index case), and the date when HCWs developed symptoms of COVID-19 or Feb 15, 2020.
2.3. Statistical analysis
Continuous variables were described as mean ± SD, or median and interquartile range (IQR), and values between COVID-19 HCWs and uninfected groups were compared using independent Student's t-test or Mann–Whitney U test when data were normally or skewed distributed, respectively. Categorical variables were described using counts (%) and were compared using the χ [2] test, or Fisher's exact test. Hazard ratios (HRs) and 95% confidence intervals (CIs) for the risk of COVID-19 that are associated with the sleep quality and working pressure were calculated by Cox proportional hazards regression models, with adjustment for age, gender, and medical post (if necessary) in model 1, while HCWs' exposure status to the COVID-19 index patient or HCWs diagnosed with COVID-19 were additionally adjusted in model 2. All the statistical hypothesis tests were two-sided with p-value < 0.05 as the level to reject the null hypothesis, and these analyses were performed with the SAS program (version 9.4; SAS Institute, Carry, NC). Detailed descriptions for the calculation of basic reproduction number (R0) were shown in Supplementary Materials.
3. Results
3.1. Overview of the transmission of COVID-19 from the index case to 12 healthcare workers
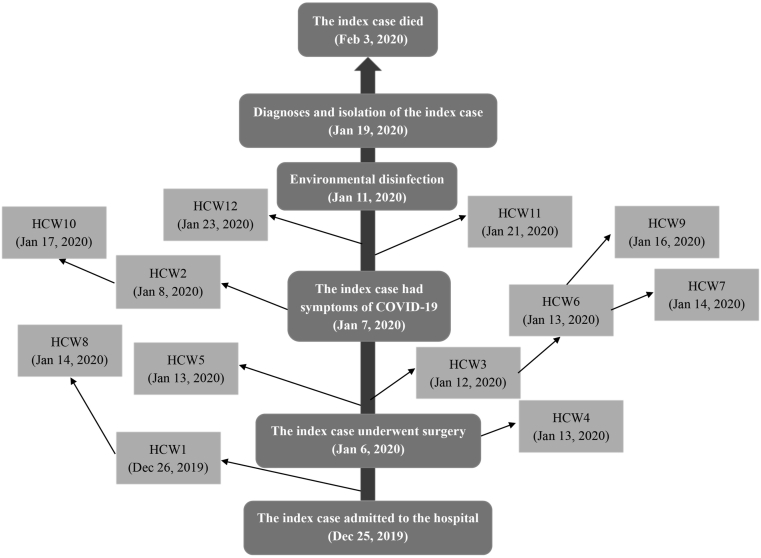
The overview of the transmission of SARS-CoV-2 from the index case to HCWs was shown in Fig. 1. A male patient (the index case) with pituitary adenoma was hospitalized on Dec 25, 2019, and underwent surgery on Jan 6, 2020. However, this patient developed flu-like symptoms, including fever (38.5 °C), cough, and white sputum without obvious inducement on Jan 7, 2020. Meanwhile, antibiotics and antiviral therapy tended to be ineffective during the following 2 days, and this symptom developed into pneumonia of unknown etiology. Then, the environmental disinfection was conducted in the department of the ward area. On Jan 19, 2020, this patient was transferred into the isolation ward and was confirmed SARS-CoV-2 infection by RT-PCR test. However, the patient was dead on Feb 3, 2020.
Fig. 1.
Overview of the transmission of COVID-19 from the index case to 12 healthcare workers. Note: HCWs, healthcare workers. The number (1–12) for each HCWs was sorted according to the onset time (the date in parentheses) of their symptoms of COVID-19. The index case, the patient who was diagnosed with pituitary adenoma at first, and finally diagnosed with COVID-19, and this case was believed to be the source of infection among HCWs. HCW1-8 were nurses, and HCW9-12 were doctors.
During the hospitalization of the index case, a total of 12 HCWs including 4 doctors (HCW9-12) and 8 nurses (HCW1-8) had one or more flu-like and pneumonia symptoms during Dec 26, 2019, and Jan 25, 2020, and they were finally confirmed infection. HCW1 was the first one to contact the index case on Dec 25, 2019, and developed symptoms of COVID-19 on Jan 8, 2019, while her close friend HCW8 also had symptoms on Jan 14, 2020. HCW4 worked in the operating room when contacted the index case on Jan 6, 2020, and developed symptoms on Jan 13, 2020. HCW3 contacted the index case in the process of surgical nursing, and then she had lunch and dinner with HCW6 between Jan 6 and Jan 8, 2020. In the meantime, HCW6 worked together with HCW9 and HCW7. These four HCWs successively developed symptoms from Jan 12 to Jan 16, 2020. HCW2 participated in the symptomatic treatment of the index case on Jan 7, 2020, and she also had a history of contact with HCW10, then both of them showed symptoms onset on Jan 8 and Jan 17, 2020, respectively. HCW11 and HCW12 contacted the index case before the environmental disinfection was conducted on Jan 11, 2020, and they developed symptoms on Jan 21, 2020, and Jan 23, 2020, respectively. Detailed dates of these 12 HCWs with the onset of symptoms, isolation, and diagnosis of COVID-19 were shown in Table S1.
3.2. Presenting characteristics
The mean age of COVID-19 HCWs was 36.6 (SD = 7.4) years old, which was significantly higher than uninfected HCWs (mean = 30.5, SD = 5.3) (P = 0.006) (Table 1). The proportion of COVID-19 HCWs was significantly higher for those who had a master's degree or above (50.0% vs. 18.9%), engaged in night shift-work (75.0% vs. 40.6%), felt working under pressure (66.7% vs. 32.1%), and had ever contacted the infected HCWs (100.0% vs. 28.3%) than the uninfected HCWs. The distributions of other demographical characteristics (sex, BMI), lifestyles (smoking status, alcohol drinking status, physical activity, and diet), contact the index case, and chronic medical disease were not significantly different between COVID-19 HCWs and uninfected HCWs. Though the outbreak data of the studied HCWs (Table S1 and Figure S1), the resulting R0 was estimated to be 1.03.
Table 1.
Demographic and epidemiological characteristics of the healthcare workers.
| Variables | All HCWs (n = 118) | Uninfected HCWs (n = 106) | COVID-19 HCWs (n = 12) | P |
|---|---|---|---|---|
| Age, years | ||||
| Mean (SD) | 31.1 ± 5.8 | 30.5 ± 5.3 | 36.6 ± 7.4 | 0.006 |
| Range | 23–51 | 23–50 | 27–51 | |
| Sex | ||||
| Men | 43 (36.4) | 38 (35.9) | 5 (41.7) | 0.76 |
| Women | 75 (63.6) | 68 (64.1) | 7 (58.3) | |
| BMI (kg/m2) | 22.1 ± 3.3 | 22.0 ± 3.3 | 22.4 ± 3.7 | 0.85 |
| Education level | ||||
| Bachelor degree | 92 (78.0) | 86 (81.1) | 6 (50.0) | 0.024 |
| Master degree or above | 26 (22.0) | 20 (18.9) | 6 (50.0) | |
| Current smoking | 9 (0.08) | 9 (8.5) | 0 (0) | 0.63 |
| Current alcohol drinking | 10 (0.08) | 10 (9.4) | 0 (0) | 0.57 |
| Regular physical activity | 40 (33.9) | 34 (32.1) | 6 (50.0) | 0.33 |
| Regular diet | 53 (44.9) | 47 (44.3) | 6 (50.0) | 0.77 |
| Number of daily diets | 2.7 ± 0.5 | 2.7 ± 0.5 | 2.8 ± 0.4 | 0.71 |
| Medical post | 0.52 | |||
| Nurse | 88 (74.6) | 80 (75.5) | 8 (66.7) | 0.019 |
| General nurses | 31 (35.2) | 29 (36.3) | 2 (25.0) | |
| Nurse practitioners | 42 (47.7) | 41 (51.2) | 1 (12.5) | |
| Nurse-in-charge | 15 (17.1) | 10 (12.5) | 5 (62.5) | |
| Doctor | 30 (25.4) | 26 (24.5) | 4 (33.3) | |
| Night shift-work | ||||
| No | 66 (55.9) | 63 (59.4) | 3 (25.0) | 0.023 |
| Yes | 52 (44.1) | 43 (40.6) | 9 (75.0) | |
| Working under pressure | ||||
| No | 76 (64.4) | 72 (67.9) | 4 (33.3) | 0.022 |
| Yes | 42 (35.6) | 34 (32.1) | 8 (66.7) | |
| Contact the index case a | ||||
| No | 22 (18.6) | 17 (16.0) | 5 (41.7) | 0.077 |
| Yes | 96 (81.4) | 89 (84.0) | 7 (58.3) | |
| Contact mode | ||||
| Air | 35 (36.5) | 32 (36.0) | 3 (42.9) | 0.90 |
| Direct contact | 49 (51.0) | 46 (51.7) | 3 (42.9) | |
| Both | 12 (12.5) | 11 (12.4) | 1 (14.3) | |
| Contact frequency (No./day) | 5.0 (2.0, 6.0) | 5.0 (2.0, 6.0) | 3.0 (1.0, 6.0) | 0.95 |
| Average contact duration (min/time) | 4.0 (2.0, 6.0) | 4.0 (2.0, 6.0) | 4.0 (2.0, 6.0) | 0.54 |
| Longest contact duration (min) | 10.0 (5.0, 25.0) | 10.0 (5.0, 20.0) | 10.0 (5.0, 30.0) | 0.69 |
| Contact the infected HCWs b | ||||
| No | 76 (68.6) | 76 (71.7) | 0 (0) | <0.001 |
| Yes | 42 (31.4) | 30 (28.3) | 12 (100.0) | |
| Chronic medical disease | ||||
| Pulmonary disease | 9 (7.6) | 8 (7.6) | 1 (8.3) | 0.49 |
| Non-pulmonary disease | 6 (5.1) | 6 (5.7) | 0 (0) | |
Note: Continuous variables were expressed as mean ± SD or median (IQR), and categorical variables were expressed as No (%). Differences in the distribution of variables between COVID-19 HCWs and uninfected HCWs were compared by Student's t-test, the Mann–Whitney U test, Chi-square test or Fisher's exact test.
The patient who was initially hospitalized with pituitary adenoma, and finally diagnosed with COVID-19.
The COVID-19 HCWs in the same department.
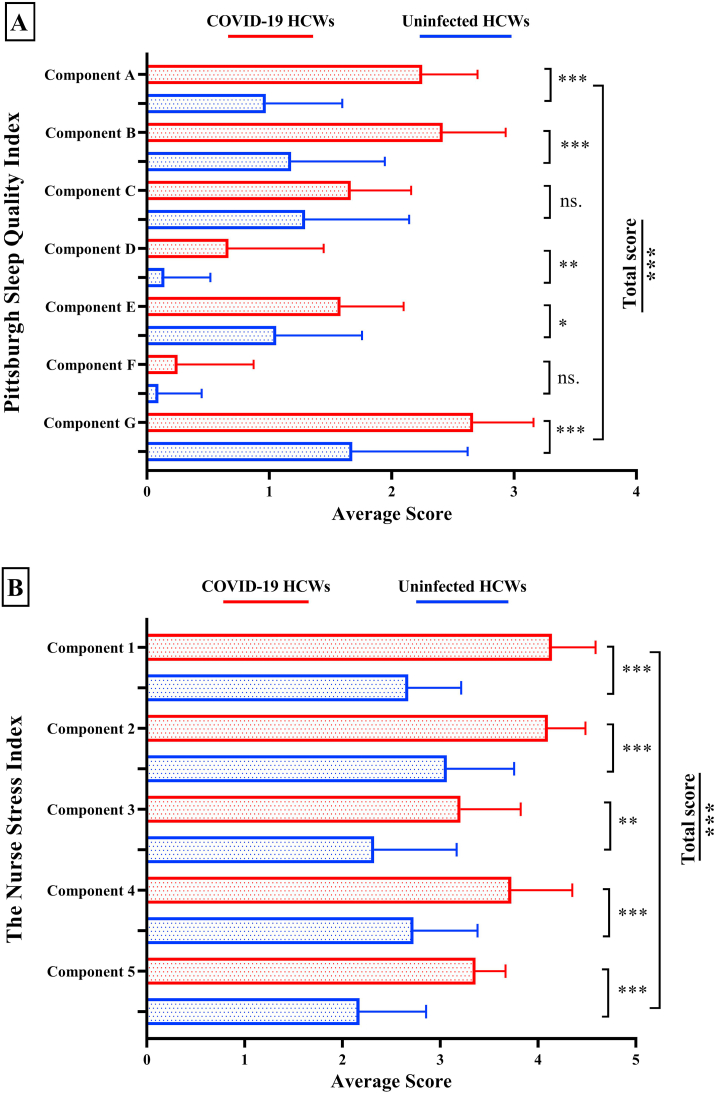
3.3. Distribution of the Pittsburgh Sleep Quality Index and The Nurse Stress Index
Given the findings that a higher proportion of COVID-19 HCWs worked the night shift and felt they were working under pressure than uninfected HCWs, we further evaluated their sleep quality and work-related stress by computing and analyzing their scores of PSQI and NSI. The analyses showed that COVID-19 HCWs had a significantly higher PSQI score than uninfected HCWs (P < 0.001, Fig. 2A). Specifically, for the 7 factors of the PSQI test, COVID-19 HCWs had significantly high scores for 5 factors (sleep quality, sleep time, sleep efficiency, sleep disorder, and daytime dysfunction), while the remaining 2 factors (sleep duration, and use of the hypnotic drug) were not significantly different. For the NSI, the scores of its 5 subscales (nursing profession and work, workload and time allocation, working environment and resources, patient care, management and interpersonal relations) were all significantly higher in infected than uninfected nurses (Fig. 2B).
Fig. 2.
The difference in the distribution of the Pittsburgh Sleep Quality Index and The Nurse Stress Index between COVID-19 cases and uninfected healthcare workers. Note: Figure A: Component A, sleep quality; Component B, sleep time; Component C, sleep duration; Component D, sleep efficiency; Component E, sleep disorder; Component F, hypnotic drug; Component G, daytime dysfunction; Total score, summary values of the 7 factors from component A to G. Figure B: Component 1, the stress of Nursing profession and work; Component 2, the stress of Workload; Component 3, the stress of Working environment and resources; Component 4, the stress of Patient care; Component 5, the stress of Management and interpersonal relations. Total score, summary values of the 5 subscales from component 1 to 5. The straight bar is the mean score of each component in scale and the whisker line is the standard error. HCWs, healthcare workers. Ns., not significant. p-value ∗ <0.05; ∗∗ <0.01; ∗∗∗ <0.001.
3.4. Associations of the Pittsburgh Sleep Quality Index and The Nurse Stress Index with the risk of COVID-19
We further investigated the associations of sleep quality and working pressure with the risk of COVID-19 using two models. In both models, we found that the total scores of PSQI and NSI were positively associated with the risk of COVID-19 (Table 2). For PSQI, high scores on sleep quality (HR = 50.99, 95%CI = 4.13–630.15) and sleep time (HR = 55.42, 95%CI = 2.39–1285.99) were associated with high risks of COVID-19, and for NSI, high scores on the subscales of the nursing profession and work (HR = 136.59, 95%CI = 1.20–15549.73), and management and interpersonal relations (HR = 59.62, 95%CI = 1.62–2192.60) were associated with high COVID-19 risk.
Table 2.
Associations of the Pittsburgh Sleep Quality Index and The Nurse Stress Index with the risk of COVID-19.
| Variables | Hazard Ratios (95%CI) | P |
|---|---|---|
| Pittsburgh Sleep Quality Index | ||
| Model 1a | ||
| Total score | 2.99 (1.87, 4.78) | <0.001 |
| The score of the factors on | ||
| Sleep quality | 38.43 (3.68, 401.13) | 0.002 |
| Sleep time | 34.28 (1.72, 683.59) | 0.021 |
| Sleep duration | 4.69 (0.30, 72.18) | 0.27 |
| Sleep efficiency | 0.19 (0.03, 1.46) | 0.11 |
| Sleep disorder | 0.83 (0.11, 6.49) | 0.86 |
| Hypnotic drug | 1.70 (0.41, 6.99) | 0.47 |
| Daytime dysfunction | 3.04 (0.49, 19.11) | 0.24 |
| Model 2a | ||
| Total score | 2.97 (1.86, 4.76) | <0.001 |
| The score of the factors on | ||
| Sleep quality | 50.99 (4.13, 630.15) | 0.002 |
| Sleep time | 55.42 (2.39, 1285.99) | 0.012 |
| Sleep duration | 5.21 (0.31, 88.93) | 0.25 |
| Sleep efficiency | 0.16 (0.02, 1.24) | 0.080 |
| Sleep disorder | 0.74 (0.08, 6.51) | 0.79 |
| Hypnotic drug | 1.59 (0.42, 6.00) | 0.49 |
| Daytime dysfunction | 3.04 (0.52, 17.63) | 0.22 |
| The Nurse Stress Index | ||
| Model 1b | ||
| Total score | 4.27 (1.66, 10.95) | 0.003 |
| The score of the subscales on | ||
| Nursing profession and work | 45.7 (0.88, 2387.94) | 0.058 |
| Workload and time allocation | 0.25 (0.01, 4.86) | 0.36 |
| Inadequate preparation | 0.79 (0.14, 4.55) | 0.80 |
| Patient care | 0.32 (0.02, 4.55) | 0.40 |
| Management and interpersonal relations | 39.73 (1.11, 1421.81) | 0.044 |
| Model 2b | ||
| Total score | 4.67 (1.42, 15.45) | 0.011 |
| The score of the subscales on | ||
| Nursing profession and work | 136.59 (1.20, 15549.73) | 0.042 |
| Workload and time allocation | 0.10 (0.002, 4.48) | 0.24 |
| Working environment and resources | 2.55 (0.15, 43.95) | 0.52 |
| Patient care | 0.21 (0.01, 3.37) | 0.27 |
| Management and interpersonal relations | 59.62 (1.62, 2192.6) | 0.026 |
Data were analyzed by using Cox proportional hazards models, with adjustment for age, gender in model 1, while the contact status to the index case or infected HCWs were additionally adjusted in model 2.
Age and medical post was adjusted in model 1 using Cox proportional hazards models, while the contact status to the index case or infected HCWs were additionally adjusted in model 2.
Given the false-negative rate of the viral nucleic acid test for SARS-CoV-2, we also consider the positive findings from chest computed tomography (CT) scan, which showed bilateral ground-glass opacity among 28 HCWs (including acid test diagnosed 12 infected HCWs). When these 28 HCWs were defined as the infected HCWs, the associations of the total scores PSQI and NSI with the risk of COVID-19 were essentially unchanged (Table S2).
4. Discussion
As the pandemic (COVID-19) accelerates, millions of people are recommended to work from home (social distancing) to minimize the transmission of COVID-19, HCWs have to do the exact opposite -going to hospitals, clinics, and putting themselves at high risk from COVID-2019 [6]. Even as non-COVID-19 related hospital's services and non-essential surgeries are reopening in several countries, the risk of nosocomial COVID-19 transmission to and among HCWs will increase. The present study was conducted in a department of neurosurgery with the incidence COVID-19 rate of 8.19%, which lacks the established practices of infection control, such as early detection and isolation, contact tracing, and the use of PPE when compared with the department of respiratory medicine and infectious disease. Therefore, at this special time, there is an urgent need to pay attention to the nosocomial infection of SARS-CoV-2 in the department of non-communicable diseases.
In this study, 5 of 12 COVID-19 HCWs had no direct contact with the index case (Fig. 1), nor with other infected cases, and their close family members were not previously infected, suggesting the human-to-human transmission between HCWs, which leads to the serious nosocomial infection. Although the main reason for this early infection among HCWs in hospitals was the lack awareness of protective measures in the early stages before an outbreak, the incident HCWs infection continued to occur after they had worn protective equipment [4], due to the contribution of other risk factors on HCWs infection. Until now, no study has evaluated the risk factors that may play roles in the susceptibility of COVID-19 among HCWs before the outbreak of COVID-19. In this study, we collected the potential risk factors before the measures of infection control were widely conducted, which ensured the data was under the natural transmission of COVID-19.
Sleep disturbance was highly prevalent among HCWs [11].The data in the present study suggested that a high proportion of COVID-19 HCWs worked the night shift. Furthermore, the PSQI showed a higher total score, sleep quality score, and sleep time score among infected than uninfected HCWs, and these scores were positively associated with the risk of COVID-19. Although the underlying mechanism for these associations had not been explored, proper sleep is at the first line of defense against infections that had been reported [12], since sleep deprivation may decrease the production of protective cytokines that were released by the immune system. For example, sleep can show effects on plasma levels of cytokine IL-1, TNF, and IL-6 when sleep duration was restricted [13]. Besides, findings in this study showed that a high proportion of COVID-19 nurses felt they were working under pressure, especially the pressure of dealing with pneumonia of unknown etiology, such as COVID-19. Their self-reported working hours were almost 10 h per day for at least 6 days per week before they received the assist from the medical support teams that were dispatched from other provinces in China. We further analyzed the pressure source by NSI, and these scores were positively associated with COVID-19 risk among nurses when the contact status with infected cases was adjusted. Similar results were also shown in a retrospective cohort study in Wuhan, China [14]. One possible reason is the prevalence of oxidative stress among nurses with higher job stress [15], which can weaken the immune function [16] and adverse mental health outcomes [17]. Some studies had revealed that stress could alter the cytokine balance, such as Th1/Th2 with strong deviation toward the Th2 component which could increase susceptibility to certain infections [18]. Therefore, it can be inferred that poor sleep quality and high working pressure among HCWs are likely to lead to their increased susceptibility to COVID-19. However, due to the retrospective design of the present study, and the lack of bio-samples, the individual's immunity parameters were not monitored, and the hypothesis needs to be further validated.
Given the above findings, improving the night duty system of HCWs and decreasing their psychological pressure could be effective measures to reduce their risk of SARS-CoV-2 infection, besides the use of PPE. Adequate provision of PPE is just the basic and the first step [19], however, other practical interventions should be also considered. As indicated in the survey, HCWs suffered both physical and mental exhaustion in this difficult time, the pain of losing patients, the concerns about their safety and passing the infections to their family, the impact of school closure, and shortness of food and other essentials for those who young children and elderly parents [20]. Therefore, reasonable workload assignments, stress relief measures, and psychological assistance should be provided to HCWs engaged with COVID-19 response. The safety of HCWs must be ensured as they are the most valuable resources in the fight against the COVID-19 pandemic.
There are several limitations to this study. These include the possibility of unmeasured residual confounding effects of contact status with infected cases, although we had adjusted for some primary confounders. Besides, our relatively small sample size and the imbalance between the numbers in each group (uninfected and COVID-19 HCWs) may influence the statistical power of our analysis and results. Furthermore, although several methods were used to minimize the recall bias, the influence of recall bias within the retrospective design could not be estimated and excluded. Further large prospective studies are needed to validate our findings.
5. Conclusions
The data before the outbreak of COVID-19 showed poor sleep quality, and high working pressure were positively associated with high risks of COVID-19. These results provide epidemiological evidence on the susceptibility of HCWs to COVID-19, and may be used to inform strategies for mitigating the risk of nosocomial transmission of COVID-19 among HCWs.
Ethics approval and consent to participate
This study was approved by the institutional ethics board of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology (No. 20200029), and all participants provided their informed consent.
Consent for publication
Consent for publication had been obtained from all studied participants.
Credit author statement
Xuan Wang; Conceptualization, Methodology, Software, Data curation, Writing - original draft, Xiaobing Jiang; Supervision, Funding acquisition, Qimin Huang: Conceptualization, Methodology, Software, Data curation, Writing - original draft, Han Wang: Conceptualization, Methodology, Software, Data curation, Writing - original draft, Visualization, David Gurarie: Writing-reviewing and editing, Martial Ndeffo-Mbah: Writing-reviewing and editing, Fei Fan; Data curation, Investigation, Peng Fu; Data curation, Investigation, Mary Ann Horn; Writing-reviewing and editing, Anirban Mondal; Writing-reviewing and editing, Charles King; Writing-reviewing and editing, Shuai Xu; Writing-reviewing and editing, Hongyang Zhao, Supervision, Funding acquisition. Yansen Bai: Conceptualization, Methodology, Software, Data curation, Writing - original draft, Writing-reviewing and editing, Visualization
Funding
This work was supported by the Fundamental Research Funds for the Central Universities [grant number 2020kfyXGYJ010 to X.J.]; the National Science Foundation RAPID Award [grant number DEB-2028631 to Q.H., D.G., and A.M.] and the National Science Foundation RAPID Award [grant number DEB-2028632 to M.N.].
Acknowledgment
The authors would like to appreciate all healthcare workers in this study. W.X., X.J., and Q.H. contributed equally and shared the first authorship. Y.B. and H.Z. contributed equally to this article. Y.B., W.X., Q.H., and H.W. analyzed data and wrote the paper. D.G., M.M., M.H., S.X., A.M., E.L., and C.K. made critical revision of the manuscript. X.J. and H.Z conducted research. Y.B., W.X, Q.H, H.W., and X.J. designed research. R.L., H.S., F.F., and P.F. collected and provided essential materials.
Footnotes
The authors declare that they have no competing interests.
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleepx.2020.100028.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sleepx.2020.100028.
Contributor Information
Hongyang Zhao, Email: hyzhao750@sina.com.
Yansen Bai, Email: baiyansen6@hust.edu.cn.
Conflict of interest
The following is the Supplementary data to this article:
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Salgado C.D., Farr B.M., Hall K.K. Influenza in the acute hospital setting. Lancet Infect Dis. 2002;2:145–155. doi: 10.1016/s1473-3099(02)00221-9. [DOI] [PubMed] [Google Scholar]
- 2.Skowronski D.M., Astell C., Brunham R.C. Severe acute respiratory syndrome (SARS): a year in review. Annu Rev Med. 2005;56:357–381. doi: 10.1146/annurev.med.56.091103.134135. [DOI] [PubMed] [Google Scholar]
- 3.Huang Q., Huo X., Ruan S. Optimal control of environmental cleaning and antibiotic prescription in an epidemiological model of methicillin-resistant Staphylococcus aureus infections in hospitals. Math Biosci. 2019;311:13–30. doi: 10.1016/j.mbs.2019.01.013. [DOI] [PubMed] [Google Scholar]
- 4.The COVID-19 Epidemiology Group of Emergency Response Mechanism of Chinese Center for Disease Control and Prevention The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liuxingbingxue Zazhi. 2020;41:145–151. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003. [DOI] [PubMed] [Google Scholar]
- 5.Wang X., Zhou Q., He Y. Nosocomial outbreak of 2019 novel coronavirus pneumonia in Wuhan, China. Eur Respir J. 2020 doi: 10.1183/13993003.00544-2020. [DOI] [Google Scholar]
- 6.The Lancet COVID-19: protecting health-care workers. Lancet. 2020;395:922. doi: 10.1016/s0140-6736(20)30644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.COVID-19 . Anadolu Agency; 2020. Spain reports 462 more deaths in one day.https://wwwaacomtr/en/europe/covid-19-spain-reports-462-more-deaths-in-one-day/1775994 Available at: [Google Scholar]
- 8.Chen Q., Liang M., Li Y. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e15–e16. doi: 10.1016/s2215-0366(20)30078-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buysse D.J., Reynolds C.F., 3rd, Monk T.H. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatr Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 10.Pamela G.T., James G.A. The nursing stress scale: development of an instrument. J Behav Assess. 1981;3:11–23. doi: 10.1007/BF01321348. [DOI] [Google Scholar]
- 11.Wang S., Xie L., Xu Y. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occup Med (Lond) 2020 doi: 10.1093/occmed/kqaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prather A.A., Leung C.W. Association of insufficient sleep with respiratory infection among adults in the United States. JAMA Intern Med. 2016;176:850–852. doi: 10.1001/jamainternmed.2016.0787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Besedovsky L., Lange T., Haack M. The sleep-immune crosstalk in health and disease. Physiol Rev. 2019;99:1325–1380. doi: 10.1152/physrev.00010.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ran L., Chen X., Wang Y. Risk factors of healthcare workers with corona virus disease 2019: a retrospective cohort study in a designated hospital of Wuhan in China. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bardhan R., Heaton K., Davis M. A cross sectional study evaluating psychosocial job stress and health risk in emergency department nurses. Int J Environ Res Publ Health. 2019;16 doi: 10.3390/ijerph16183243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mullen L., Mengozzi M., Hanschmann E.M. How the redox state regulates immunity. Free Radic Biol Med. 2019 doi: 10.1016/j.freeradbiomed.2019.12.022. [DOI] [PubMed] [Google Scholar]
- 17.Gold J.A. Covid-19: adverse mental health outcomes for healthcare workers. BMJ. 2020;369:m1815. doi: 10.1136/bmj.m1815. [DOI] [PubMed] [Google Scholar]
- 18.Marshall G.D., Jr. The adverse effects of psychological stress on immunoregulatory balance: applications to human inflammatory diseases. Immunol Allergy Clin. 2011;31:133–140. doi: 10.1016/j.iac.2010.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bartoszko J.J., Farooqi M.A.M., Alhazzani W. Medical masks vs N95 respirators for preventing COVID-19 in healthcare workers: a systematic review and meta-analysis of randomized trials. Influenza Other Respir Viruses. 2020 doi: 10.1111/irv.12745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shen X., Zou X., Zhong X. Psychological stress of ICU nurses in the time of COVID-19. Crit Care. 2020;24:200. doi: 10.1186/s13054-020-02926-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.