Abstract
Introduction
The literature remains unclear on the development, consequences, and interventions for burnout in resident populations. We aim to identify the prevalence and nuances of reported burnout in general surgery resident physicians to better understand which factors contribute the greatest risk.
Methods
A 42-question anonymous online survey was distributed by the Association of Program Directors in Surgery (APDS) to general surgery resident physicians. ANOVA, chi-square and multinomial regression analyses were performed with significance defined as p < 0.05. This survey was reported in line with the STOCSS criteria.
Results
81 survey responses were received. Burnout was reported by 89.5% of university-hospital affiliated respondents and 95.2% of community teaching hospital affiliated respondents. After adjustment, community respondents showed a nearly fifteen times greater likelihood of burnout (aOR = 14.735, 95% CI: 0.791,274.482). Females were 2.7 times as likely as males to report burnout (aOR = 2.749, 95% CI: 0.189,39.960) and nearly twice as likely to report contemplating suicide (aOR = 1.819, 95% CI: 0.380,8.715). Burnout rates by hours worked/week revealed that 100% of those working ≥80 h/week report experiencing burnout.
Conclusion
Overall burnout rates reported by surgical residents respondents were high. Community teaching hospital setting, female gender, and increased number of hours worked per week may be associated with higher rates of burnout. Both female and community-affiliated residents were at increased risk of reporting suicidal ideation. Targeted interventions are needed to adequately address program-specific causes for resident burnout and reduce its prevalence in high-risk cohorts.
Keywords: Residents burnout, Resident training, General surgery residency, Resident wellbeing, Burnout prevention
Highlights
-
•
Burnout as self-reported by general surgery residents is exceptionally high.
-
•
Risk factors associated with increased reporting of burnout include female gender, community affiliated teaching hospitals, and increased work hours.
-
•
Residents reporting burnout are more likely to consider leaving the medical field altogether, report their burnout affects their ABSITE performance and aspects of daily life.
1. Introduction
Surveys report impressively high burnout rates amongst nearly all medical specialties [1]. Studies have shown that resident physicians in particular are at an increased risk for development of burnout symptoms [2,3]. Physician residents are at the beginning stages of acquiring the necessary skills to succeed as independent physicians. Burnout at this stage may impair resident functioning and their ability to refine their clinical acumen [4].
Clinical burnout was originally defined by three pillars of symptomatology: emotional exhaustion, depersonalization, and low sense of personal accomplishment [5]. Standardized evaluation tools such as the Maslach Burnout Inventory (MBI), Physician Worklife Survey, and the Mini Z Burnout survey are frequently utilized. Despite these measures, the influences of non-work related dissatisfactions on the development of clinical burnout remain complex. The question remains of whether depression is due to burnout, or whether burnout is attributed to underlying depression, threatening the validity of considering clinical burnout to be its own “clinical syndrome.” [6,7] Regardless of its distinction, burnout has often been attributed to multiple systemic issues including bureaucratic tasks, electronic health records, work hour demands, lack of autonomy in practice, and administrative disrespect [1]. According to Dimou et al. younger age, poor work-life balance, and increased number of nights on call are associated with surgeon burnout [5]. Resident physicians also experience higher levels of depression, fatigue, and stress, as well as lower levels of mindfulness and coping strategies [8].
The existing literature remains unclear on the development of clinical burnout in resident physicians. It is for this reason that our team sought to identify the prevalence, contributing factors, and nuances of reported burnout in general surgery resident physicians. In addition, we aim to advocate for the implementation of targeted interventions to reduce burnout. We hope that such information will be of value to residency programs in addressing this issue within their own resident workforce.
2. Methods
A 42-question, anonymous, web-based survey tool was distributed to current general surgery resident physician members of the Association of Program Directors in Surgery (APDS). APDS was utilized as the sole distributer of our survey as many associated residents come from multiple practice settings, backgrounds, and/or program designs. Residents were not contacted directly for survey completion. The survey investigated multiple demographic factors such as age, gender, type of program institution (university hospital or community teaching), educational background, and hours worked. The majority of the survey included questions regarding general perceptions of physician burnout, personal feelings of burnout, notable consequences of reported burnout, and methods used to manage burnout. Multiple questions regarding contributing factors to the development of burnout were included. For example, respondents were asked to rate, on a scale of 1–10, the extent to which finances, relationships, health, family, etc. Impacted one's burnout development. We also included multiple questions inquiring about one's satisfaction with their respective program and their access to burnout prevention resources, if applicable, to identify potential causative factors. Respondents were asked to rate their burnout, if any, by level of frequency (daily, weekly, etc.). In order to ensure accurate reporting of attributed causes of burnout, several questions were included to determine if a respondent's burnout was mainly due to their training, personal life, concurrent or previous depressive symptoms, or non-work related factors. Those who did not report burnout were able to document as such and opt-out of answering additional questions. Respondents were allowed to choose multiple answers on most questions and include custom responses when applicable. Survey question content was derived from an aggregate of validated burnout assessment surveys, although an official, complete diagnostic assessment was not utilized in our survey [[9], [10], [11], [12], [13]]. Some included questions were unique in that they directly inquired about contributing factors, or consequences of, burnout not previously described in the current literature. Prior to APDS distribution, the survey underwent a pilot study for internal validation via survey completion and review by 22 residents and 8 faculty members. The review process entailed anonymous completion of the survey by each resident or faculty member along with subsequent detailed review and itemized critique of content. This study was conducted in compliance with all ethical standards and deemed exempt by our institutional review board. The APDS Research Committee conducted a final review of survey content and confirmed design approval prior to distribution. Once distributed by the APDS, no additional alterations were made to survey content. The survey was kept open for completion from May–July 2020. No incentives were provided to respondents for survey completion.
IBM SPSS Statistics Version 26.0 (Armonk, NY) was utilized to complete the data analysis with statistical significance defined as p < 0.05. Chi-square was used to compare categorical variables. Multivariable logistic regression was used to investigate differences in burnout among cohorts after adjusting for age, gender, race, years of practice, practice setting, and hours worked per week. This survey was reported in line with the STOCSS criteria [14]. This work was submitted to the Research registry (UIN #:researchregistry5860) which can be found via the following link: https://www.researchregistry.com/browse-the-registry#home/registrationdetails/5f262ece3e958300185f78e0/
3. Results
Eighty-one survey responses were received. 41 (50.6%) respondents identified as male, 39 (48.1%) as female, and 1 (1.2%) preferred not to answer. 62 (76.5%) reported being a resident in a community teaching hospital whereas 19 (23.5%) reported being a resident in a university hospital (Table 1).
Table 1.
Socio-demographics of Respondents. Shown in each category are the frequency and relative proportion of respondent demographics.
| Adjustment | Community Hospital vs. University Hospital Respondents |
Female vs. Male Respondents |
||||
|---|---|---|---|---|---|---|
| OR | p-value | 95% CI | OR | p-value | 95% CI | |
| Race | 7.514 | 0.118 | 0.600–94.033 | 3.764 | 0.272 | 0.353–40.125 |
| Age | 2.765 | 0.299 | 0.405–18.882 | 4.834 | 0.172 | 0.505–46.294 |
| Years Since Graduating Medical School | 2.530 | 0.334 | 0.384–16.671 | 4.274 | 0.204 | 0.454–40.203 |
| Hours Worked per Week | 2.421 | 0.367 | 0.354–16.541 | 3.027 | 0.337 | 0.316–29.032 |
| Gender | 2.493 | 0.348 | 0.371–16.765 | – | – | – |
| Institution Type | – | – | – | 4.342 | 0.201 | 0.456–41.317 |
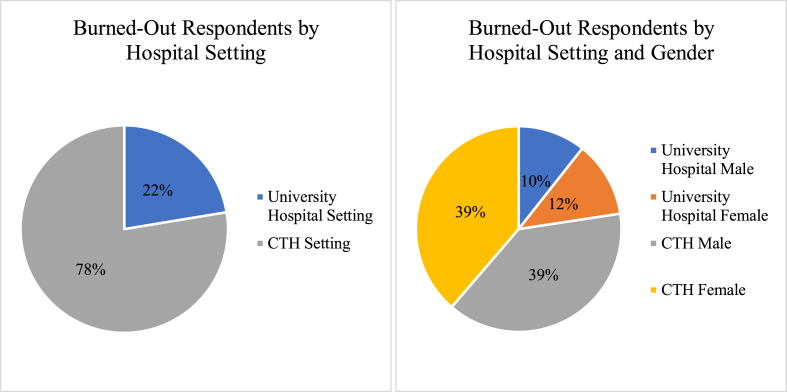
Burnout was reported by 89.5% of university-hospital affiliated respondents and 95.2% of community teaching hospital affiliated respondents (Fig. 1). When adjusting for race, age, gender, years since graduating medical school, and hours worked per week, community hospital affiliated respondents showed a nearly fifteen times greater likelihood of burnout compared to university hospital affiliated respondents (aOR = 14.735, 95% CI: 0.791,274.482). Table 2 shows the odds of experiencing burnout based on institution type for each individual adjustment utilized in their respective multivariable regression. Respondents with a university affiliation who reported burnout were less likely to contemplate committing suicide compared to community teaching hospital affiliated respondents who reported burnout (aOR = 0.817, 95% CI: 0.068,3.078). Compared to university affiliated respondents, community-teaching hospital affiliated respondents were 7.4% less likely to report having adequate administrative support to address burnout (OR = 0.926, 95% CI: 0.085,10.085) and over five times as likely to report their administration needing more resources to address burnout compared to university affiliated respondents (OR = 5.500, 95% CI: 0.644,46.949).
Fig. 1.
(A) Fraction of Burned out Respondents by Hospital Setting. 22.4% of respondents who reported burnout were affiliated with a university hospital, whereas 77.6% reported being affiliated community teaching hospital. (B) Fraction of Burned Out Respondents by Hospital Setting and Gender. It can be observed that male and female residents at a community teaching hospital have equal rates of burnout at 38.20%, followed by university hospital females at 11.8% and university hospital males at 10.5%. Abbreviations: CTH = Community Teaching Hospital.
Table 2.
Adjusted Odds Ratios for Burnout Among Respondents. Shown are the odds ratios describing odds of experiencing burnout, p-values, and 95% confidence intervals after only controlling for each individual adjustment utilized in their respective multivariable regressions. Abbreviations: OR = Odds Ratio, CI = Confidence Interval.
| Category Analyzed | X [2] Value | P-value |
|---|---|---|
| Females – Category A | 14.922 | 0.021 |
| 30–34 Years Old – Category B | 20.740 | 0.014 |
| 40–44 Years Old– Category C | 22.517 | 0.007 |
| 40–44 Years Old – Category D | 21.012 | 0.013 |
| Graduated Medical School <5 Years Ago – Category E | 13.941 | 0.030 |
| Graduated Medical School 5–10 Years Ago – Category D | 18.808 | 0.005 |
| Graduated Medical School 5–10 Years Ago – Category F | 15.039 | 0.020 |
| 70-79 Hours Worked per Week – Category G | 13.749 | 0.033 |
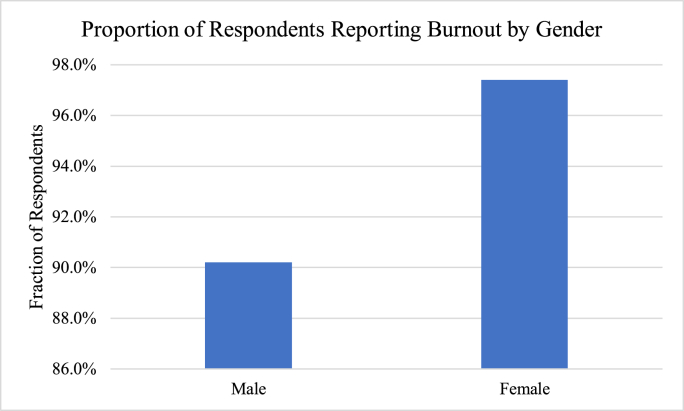
37 (90.2%) male respondents and 38 (97.4%) female respondents reported experiencing burnout (Fig. 2). Females were over four times as likely to report burnout experience compared to males (OR = 4.108, 95% CI: 0.438,38.495). Adjusting for race, age, institution type, hours worked per week, and years since graduating medical school, females were 2.7 times as likely as males to report experiencing burnout (aOR = 2.749, 95% CI: 0.189,39.960). Table 2 shows the odds of experiencing burnout based on respondent gender for each individual adjustment utilized in their respective multivariable regression. Females who reported experiencing burnout were nearly twice as likely to also report contemplating committing suicide (aOR = 1.819, 95% CI: 0.380,8.715).
Fig. 2.
Proportion of Respondents Reporting Burnout by Gender. It can be shown that 90.2% of male respondents and 97.4% of female respondents reported burnout.
Burnout rates stratified by age group showed that 100% of those aged 40–44 years, 100% of those aged 35–39 years, 89.7% of those aged 30–34, and 97.0% of those aged <30 reported experiencing burnout. After adjusting for race, gender, institution type, hours working, and years since graduating medical school, the <30 years old group was 21.2% more likely to experience burnout compared to the age 40–44 years group (aOR = 1.212, 95% CI: 0.000,6,257.135) whereas the 35–39 year old group was nearly three times as likely to experience burnout compared to the 40–44 year old group (aOR = 2.997, 95% CI: 0.000,71,354.358). The age 30–34 group was 26.5% less likely to report experiencing burnout compared to the age 40–44 group (aOR = 0.735, 95% CI: 0.000.3262.565). .
Burnout rates stratified by number of hours worked per week revealed that 83.3% of those who work 60–69 h per week, 92.9% of those who work 70–79 h per week, and 100% of those who work 80–89 h per week and ≥90 h per week report experiencing burnout. After adjusting for age, gender, race, number of years since graduating medical school, and institution type, the respondents in the 60–69 h per week group were 99.7% less likely to report burnout than the ≥90 h per week group (aOR = 0.003, 95% CI: 0.000,18.789). The 70–79 h group was 90.2% less likely to report burnout compared to the ≥90 h group (aOR = 0.098, 95% CI: 0.0005,190.166). The 80–89 h worked per week group was 22.3% less likely to report burnout compared to the ≥90 h group (aOR = 0.777, 95% CI: 0.0004,12,610.45). Additionally, statistically significant differences between cohorts based on various survey questions are presented in Table 3. The ways in which respondents reported managing their burnout and the fraction of respondents who felt supported by administration to support burnout can be found in Table 4.
Table 3.
Significant Differences between Cohorts per Question Category. Chi-square analysis was performed to obtain significant associations. Each row represents the relationship between the Years of Practicing groups and the question category listed. Category A: Respondents considered leaving the medical field altogether due to burnout. Category B: Respondents report feeling able to properly manage their burnout. Category C: Respondents feel their burnout affects aspects of daily life. Category D: Respondents feel depressed due to their burnout. Category E: Respondents feel that their burnout negatively impacts their performance on residency examinations. Category F: Respondents feel they cannot address burnout due to fear of repercussions from administration Category G: Respondents feel satisfied with the quality of training at in their residency program.
| Burnout Management Method | N | % of Respondentsa | Felt Supported by Administration | N | % of Respondents |
|---|---|---|---|---|---|
| Talking with Friends/Associates | 55 | 67.9% | Strongly Agree/Agree | 34 | 42.0% |
| Vacation/Time Off | 50 | 61.7% | Neutral | 20 | 24.7% |
| Exercise | 44 | 54.3% | Strongly Disagree/Disagree | 23 | 28.4% |
| Isolation from Others | 24 | 29.6% | Other | 4 | 4.9 |
| Spend Time with Family | 23 | 28.4% | |||
| Alcohol | 21 | 25.9% | |||
| Do Nothing | 16 | 19.8% | |||
| Not Applicable | 9 | 11.1% | |||
| Seeking Professional Help | 7 | 8.6% |
As respondents were able to choose more than one way they try to manage their burnout, these frequencies represent the total counts per burnout management category.
Table 4.
Reported Methods of Managing Burnout and Feelings of Administrative Support to Address Burnout. Shown in the left half of the table is the frequency of methods respondents use to reduce burnout. Shown in the right half of the table is the frequency of answers responders choice when asked if they felt supported by their administration to be able to address burnout.
| Total = 81 |
||||||
|---|---|---|---|---|---|---|
| Practice Setting | University Hospital |
Community Teaching Hospital |
||||
| 19 | 62 | |||||
| 23.5% | 76.5% | |||||
| Gender | Male | Female | Unspecified | |||
| 41 | 39 | 1 | ||||
| 50.6% | 48.1% | 1.2% | ||||
| Years Since Graduating Medical School | <5 | 5–10 | 11–15 | |||
| 67 | 13 | 1 | ||||
| 82.7% | 16.0% | 1.2% | ||||
| Age Groups | <30 | 30–34 | 35–39 | 40–44 | ||
| 33 | 39 | 6 | 3 | |||
| 40.7% | 48.1% | 7.4% | 3.7% | |||
| Hours Worked per Week | 60–69 | 70–79 | 80–89 | ≥90 | ||
| 6 | 56 | 14 | 5 | |||
| 7.4% | 69.1% | 17.3% | 6.2% | |||
| Race/Ethnicity | African American | Asian | Caucasian | Hispanic | Multiracial | |
| 4 | 17 | 36 | 16 | 8 | ||
| 4.9% | 21.0% | 44.4% | 19.8% | 9.9% | ||
| Residency Programa | General Surgery | Trauma and Surgical Critical Care | Pediatric Surgery | Vascular Surgery | Plastic Surgery | |
| 81 | 3 | 1 | 2 | 2 | ||
| 100% | 3.7% | 1.2% | 2.5% | 2.5% | ||
| Year in Residency | PGY-1 | PGY-2 | PGY-3 | PGY-4 | PGY-5 | PGY-6 |
| 16 | 26 | 19 | 11 | 8 | 1 | |
| 19.8% | 32.1% | 23.5% | 13.6% | 9.9% | 1.2% |
As respondents were able to choose more than one field as their specialty, these frequencies represent the total counts per surgical field.
4. Discussion
Our study investigated the prevalence, causes, and consequences of reported burnout in general surgery resident physicians. Overall, reported rates of burnout were high. However, multiple trends in burnout risk, consequences, and causes were observed across various groups.
Our survey showed that respondents training in a community teaching hospital program were more likely to report burnout relative to their university-affiliated counterparts. Community residents were also more likely to report that their respective administration needed more resources to address burnout and were less likely to report having adequate support from their administration. There has been little to no consensus on a clear benefit with any particular burnout intervention [15]. In a retrospective study by Satterfield et al. small group sessions over a two year period were utilized to focus on resident physician identity development, stress coping, building professional confidence, management of anxiety and guilt, and burnout [16]. Introspective, discussion-based trainings such as the “Balint Group” format have been shown to lower the risk of maladaptive feelings/behaviors that could contribute to burnout development and improve communication styles. The development of stronger communication skills have been observed to have impressive effects, especially when the group sessions are implemented in early resident training [17].
Our survey results showed female general surgery residents were nearly three times more likely to report burnout than were male respondents, other have found similar findings [12,13,[18], [19], [20], [21]]. Studies conducted by Elkbuli et al. and Sutherland et al. found a 20x and 5x higher risk of reported burnout in women compared to men [12,13]. Jackson et al. reported that female gender was an independent risk factor for PTSD development in residents training in multiple specialties [18]. Dyrbye et al. showed women were also more likely to report depressive symptoms, work-life imbalance, difficulties with child-care, and spouses prioritizing their own careers over the women physicians [19]. Based on 2018 Centers for Disease Control and Prevention national data, women are at roughly 1.4x the risk of attempting suicide while males are more likely to die from suicide attempts (3.6x) [20]. We also observed that female respondents were significantly more likely to report considering leaving the medical field altogether due to their burnout symptoms. From an economic standpoint, physician burnout causes those affected to have less motivation for their work, greater consideration of early retirement, or dropping the field/training altogether [21]. Preventative measures may be needed at the residency training level to prevent loss of female physicians from the healthcare field.
Our analysis of burnout reports by hours worked per week showed a positive correlation. Those residents reporting ≥90 h/week were at the highest risk of reporting burnout. Despite not reaching statistical significance, these findings do align with the prevailing concept of targeting resident scheduling as a primary means of alleviating burnout. Recent ACGME updates have attempted to directly mitigate this risk by limiting resident hours [22]. A systematic review conducted by Busireddy et al. on efficacy of interventions for resident physicians found that reduction in work hours was the strongest modifier of emotional exhaustion and depersonalization scores [15]. Residency administrations should be keenly aware of the need for work-life balance and the positive effect that fair schedule design can have on reducing burnout. A prior study of internal medicine residents by Goitein et al. found that in addition to work hour restrictions, addition of a night float, hospitalist services expansion, reduction of call frequency, and reduction in patient census improved resident well-being [23]. Hutter et al. found that in a study of 58 surgical residents, a decrease in average hours per week from 99.5 to 78.9 was associated with decreased MBI burnout scores, significant reduction in emotional exhaustion, better overall quality of life, and higher motivation to work [24].
We discovered that residents in the age 40–44 year group were the least likely to report burnout symptoms compared to all other groups, except for the 30–34 year group (roughly 3x less likely). The 30–34 year group also was significantly more likely to report feeling that they could manage their burnout symptoms, which aligns with their relatively lower overall rates. While the 40–44 year group was one of the relatively lower at-risk groups, they were significantly more likely to report that their burnout affects various aspects of their daily life as well as suffer from depression secondary to their burnout. While we found no clear trend of burnout with increasing age, our findings do suggest that resident age may affect burnout severity and quality of life outside their training. Interventions targeting both program-related and lifestyle-related causes may be helpful.
Our investigation does have limitations, the main being our small sample size of 81 respondents. The timing of our survey distribution and data collection period in relation to the COVID-19 pandemic likely had a profound impact on our sample size. While trends were exhibited in identifying resident groups at highest risk for burnout development, the relatively small number of responses likely influenced our ability to reach statistical significance in multiple categories presented and also limited the number of regression analyses able to be performed. For example, our individual adjustments by each variable of interest presented were feasible for only institution type and gender variables. Age and hours worked per week variables provided too small samples across their respective subgroups to provide comprehensible odds ratios and confidence intervals, and therefore, were not included in Table 2. The findings from our investigation that were able to reach statistical significance were regarding various descriptive questions covered in Table 3, but generalizability of such findings to all general surgery residents remains uncertain. Based on our preliminary findings, future investigations consisting of a higher respondent rate and/or distribution through multiple associations are warranted to produce a clearer picture of the general surgery resident population and need for specific change. Additionally, we assessed the rate of burnout by survey respondents through multiple survey questions based on validated assessments, rather than utilizing validated assessment directly (MBI, Mini Z Burnout Survey). Our objective to identify the prevalence and nuances of perceived burnout spurred the need for a more succinct, evidence-based survey as to maximize the number of responses received and generalizability of results. Incorporation of multiple formal survey review periods by both interdepartmental and APDS research committees were utilized to further validate our survey content and enhance clarity for respondents. Our investigation being survey-based, our results may also be limited by both recall and selection bias. It is possible that those respondents experiencing higher burnout rates were more inclined to complete the survey, as well as more inclined to report contributing factors (i.e. higher work hours, inadequate administrative support, etc.).
In general, our findings suggest that resident physicians who train in a community setting, are female, or have high work-hour demands may be at an increased risk of reporting burnout. When considering interventions to prevent/manage burnout, an assessment of the causative factors is imperative. Response to burnout should focus on burnout prevention strategies and offering clinical, educational, and/or emotional support [25]. While “resiliency traits” have been proposed as a protective factor against burnout development, we believe that programs should not simply attempt to reduce burnout rates by selection of only residents who subjectively exhibit traits believed to be most protective against burnout (low anxiety, adequate social support, less debt) [26]. Such actions will inevitably create further marginalization of at-risk groups and does not address the true issue at hand; the healthcare system structure in which one trains. Burnout is attributed to a compilation of life stressors, work demands, and lack of adequate support from their administrations. Actions such as a simple reduction in hours worked will not be sufficient in alleviating burnout for all. Based on our results, potential avenues of additional need could include targeted efforts toward retention of female residents and addressing gender-specific causes for wanting to leave the medical field for alternative careers. Additionally, residents reporting inadequate support and resources from their respective administrations may induce urgency for administrations to act in any capacity to aid their trainees, as burnout has been shown to have adverse consequences on quality of care provided to patients [27]. Targeted small group sessions, early emphasis on emotional and professional development, and facilitation of rapport building amongst residents may help alleviate the multiple factors that contribute to burnout symptomatology. Ultimately, larger, validated studies are needed to further clarify our presented preliminary trends and the extent to which they effect the general surgery resident population and necessary targets for intervention.
5. Conclusion
Overall reported burnout rates across surgery resident respondents of our survey were high. Those residents reporting training at community teaching hospital programs, female gender, or increased number of hours worked per week may be at higher risk for reporting burnout. Both female and community-affiliated residents were at increased risk of reporting suicidal ideation, potentially indicating greater severity and need for intervention in these populations. Targeted interventions at the institutional level are needed to adequately address program-specific causes for resident burnout.
Funding
None.
Declaration of competing interest
Authors declare no competing interests.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2020.10.012.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Kane L. Medscape Log in. 2020. Medscape national physician burnout & suicide report 2020: the generational divide.https://www.medscape.com/slideshow/2020-lifestyle-burnout-6012460 Accessed May 31, 2020. [Google Scholar]
- 2.Dyrbye L., Herrin J., West C.P. Association of racial bias with burnout among resident physicians. JAMA Netw Open. 2019;2(7) doi: 10.1001/jamanetworkopen.2019.7457. 2019 Jul 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pulcrano M., Evans S.R., Sosin M. Quality of life and burnout rates across surgical specialties: A systematic review. JAMA Surg. 2016;151(10):970–978. doi: 10.1001/jamasurg.2016.1647. [DOI] [PubMed] [Google Scholar]
- 4.Dewa C.S., Loong D., Bonato S., Trojanowski L., Rea M. The relationship between resident burnout and safety-related and acceptability-related quality of healthcare: a systematic literature review. BMC Med. Educ. 2017;17(1):195. doi: 10.1186/s12909-017-1040-y. Nov 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dimou F.M., Eckelbarger D., Riall T.S. Surgeon burnout: a systematic review. J. Am. Coll. Surg. 2016;222(6):1230–1239. doi: 10.1016/j.jamcollsurg.2016.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moss Jennifer. Burnout is about your workplace, not your people. hbr.org/2019/12/burnout-is-about-your-workplace-not-your-people?utm_source=linkedin&utm_medium=social&utm_campaign=hbr Harv. Bus. Rev., Published.
- 7.International Classification of Diseases. 2019. Burn-out an "occupational phenomenon.https://www.who.int/mental_health/evidence/burn-out/en/ May 28, Retrieved. [Google Scholar]
- 8.Chaukos D., Chad-Friedman E., Mehta D.H. Risk and resilience factors associated with resident burnout. Acad. Psychiatr. 2017;41(2):189–194. doi: 10.1007/s40596-016-0628-6. [DOI] [PubMed] [Google Scholar]
- 9.Maslach C., Jackson S.E., Leiter M.P. Consulting Psychologists Press; Palo Alto, Calif: 1996. Maslach Burnout Inventory Manual. 577 College Ave., Palo Alto 94306. [Google Scholar]
- 10.Maslach, C., & Jackson, S. E. (n.d.). Maslach Burnout Inventory - Human Services Survey for Medical Personnel (MBI-HSS (MP)) - Assessments, Tests: Mind Garden. https://www.mindgarden.com/315-mbi-human-services-survey-medical-personnel. Accessed January 6, 2020.
- 11.Linzer M. Mini Z burnout survey. 2019. https://edhub.ama-assn.org/steps-forward/module/2702509 STEPSfoward. American Medical Association.
- 12.Elkbuli A., Kinslow K., Boneva D., Liu H., Ang D., McKenney M. The American Surgeon; 2020. Addressing burnout among trauma surgeons. [DOI] [PubMed] [Google Scholar]
- 13.Sutherland M., Kinslow K., Boneva D., McKenney M., Elkbuli A. Perceived burnout among burn surgeons: Results from a survey of American burn association members. https://doi-org.ezproxy.fiu.edu/10.1093/jbcr/iraa146 J. Burn Care Res., official publication of the American Burn Association, iraa146. Advance online publication. [DOI] [PubMed]
- 14.Agha R., Abdall-Razak A., Crossley E., Dowlut N., Iosifidis C., Mathew G., for the STROCSS Group The STROCSS 2019 guideline: strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2019;72:156–165. doi: 10.1016/j.ijsu.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 15.Busireddy K.R., Miller J.A., Ellison K., Ren V., Qayyum R., Panda M. Efficacy of interventions to reduce resident physician burnout: a systematic review. J Grad Med Educ. 2017;9(3):294–301. doi: 10.4300/JGME-D-16-00372.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Satterfield J.M., Becerra C. Developmental challenges, stressors and coping strategies in medical residents: A qualitative analysis of support groups. Med. Educ. 2010;44(9):908–916. doi: 10.1111/j.1365-2923.2010.03736.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bar-Sela G., Lulav-Grinwald D., Mitnik I. Balint group" meetings for oncology residents as a tool to improve therapeutic communication skills and reduce burnout level. J. Canc. Educ. 2012;27(4):786–789. doi: 10.1007/s13187-012-0407-3. [DOI] [PubMed] [Google Scholar]
- 18.Jackson T., Zhou C., Khorgami Z. Traumatized residents - it's not surgery. It's medicine. J. Surg. Educ. 2019;76(6):e30–e40. doi: 10.1016/j.jsurg.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 19.Dyrbye L.N., Shanafelt T.D., Balch C.M., Satele D., Sloan J., Freischlag J. Relationship between work-home conflicts and burnout among American surgeons: A comparison by sex. Arch. Surg. 2011;146(2):211–217. doi: 10.1001/archsurg.2010.310. [DOI] [PubMed] [Google Scholar]
- 20.WISQARS Data Visualization. (n.d.) https://wisqars-viz.cdc.gov:8006/explore-data/home Accessed.
- 21.Imran A., Calopedos R., Habashy D., Rashid P. Acknowledging and addressing surgeon burnout. ANZ J. Surg. 2018;88(11):1100–1101. doi: 10.1111/ans.14817. [DOI] [PubMed] [Google Scholar]
- 22.Summary of Changes to ACGME Common Program Requirements Section VI. (n.d.). https://www.acgme.org/What-We-Do/Accreditation/Common-Program-Requirements/Summary-of-Proposed-Changes-to-ACGME-Common-Program-Requirements-Section-VI. Accessed July 18, 2020.
- 23.Goitein L., Shanafelt T.D., Wipf J.E., Slatore C.G., Back A.L. The effects of work-hour limitations on resident well-being, patient care, and education in an internal medicine residency program. Arch. Intern. Med. 2005;165(22):2601–2606. doi: 10.1001/archinte.165.22.2601. [DOI] [PubMed] [Google Scholar]
- 24.Hutter M.M., Kellogg K.C., Ferguson C.M., Abbott W.M., Warshaw A.L. The impact of the 80-hour resident workweek on surgical residents and attending surgeons. Ann. Surg. 2006;243(6):864–875. doi: 10.1097/01.sla.0000220042.48310.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bilimoria K.Y. Association for academic surgery presidential address—fanning the burnout fire: how our misconceptions and good intentions could fail tomorrow’s surgeons. J. Surg. Res. 2020;S0022-4804(20) doi: 10.1016/j.jss.2020.06.005. 30388–7. [DOI] [PubMed] [Google Scholar]
- 26.Smeds M.R., Janko M.R., Allen S. Burnout and its relationship with perceived stress, self-efficacy, depression, social support, and programmatic factors in general surgery residents. Am. J. Surg. 2020;219(6):907–912. doi: 10.1016/j.amjsurg.2019.07.004. [DOI] [PubMed] [Google Scholar]
- 27.Jacob Moalem M. (n.d. Burnout in Surgery. 2020 https://www.facs.org/education/division-of-education/publications/rise/articles/burnout Retrieved August 09, from. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.