Implementation of evidence-based pharmacotherapy for individuals with opioid use disorder (OUD) is cornerstone of the response to the opioid crisis [1]. ED-initiated OUD treatment with buprenorphine has been shown to increase treatment engagement at 30 days [2], but this practice has not been widely adopted [3]. To better develop strategies for implementation, we sought to 1) describe ED physician preparedness to treat OUD and 2) rank physician-perceived barriers and facilitators of ED administration of buprenorphine and obtaining a Drug Addiction Treatment Act of 2000 waiver to prescribe buprenorphine (X-waiver).
To do this, we conducted a cross-sectional survey of physicians in two urban, academic EDs assessing two domains. First, we measured self-rated levels of preparation for various aspects of OUD treatment using a 5-point Likert scale. Second, we assessed barriers and facilitators to buprenorphine administration in the ED and obtaining and X-waiver. Barriers were based on those identified in prior literature from other settings [4–9]. Barriers and facilitators were rated individually on a continuous 10-point scale, with 1 indicating “not at all a barrier” and 10 indicating “the most significant barrier.” We also collected demographic and other physician characteristics. The survey was administered via the REDCap version 8.9.0 secure web platform [10], and participants received a $10 incentive. Data were analyzed using descriptive statistics, and we compared responses by X-waiver status using chi-squared tests for categorical variables and the Mann-Whitney test for continuous variables (Stata, version 15.1; StataCorp, College Station, TX). The Institutional Review Board from the University of Pennsylvania approved this study.
84 participants completed the survey (response rate 78%). Participant characteristics are shown in Table 1. Participants were primarily male (62%), white (74%), and attending physicians (55%). Characteristics were similar for the 21% who had completed X-waiver training and those who had not. 39% of physicians reported they had ordered naloxone upon discharge from the ED in the past 3 months, and 33% had ordered buprenorphine in the past 3 months, either in the ED or at discharge. Figure 1 shows physician self-rated preparation for OUD care. While physicians felt prepared for some aspects of care, a minority felt prepared to determine the level of care for patients with OUD (39%), connect patients to outpatient treatment (29%) or initiate buprenorphine (27%). Levels of preparation did not differ significantly by X-waiver status, with the exception of initiating buprenorphine treatment (56% of waiver trained physicians vs 20% of non-waiver trained, p=0.002). Preparation also did not differ by level of training.
Table 1:
Participant Characteristics
| Number | X-waiver | No X-waiver | p-value | |
|---|---|---|---|---|
| PHYSICIAN CHARACTERSTICS | ||||
| Age | ||||
| Less than 30 | 24 (29%) | 2 | 22 | |
| 30–39 | 35 (42%) | 9 | 26 | |
| 40–49 | 15 (18%) | 6 | 9 | |
| 50–59 | 7 (8%) | 1 | 6 | |
| Over 60 | 3 (4%) | 0 | 3 | p=0.149 |
| Sex | ||||
| Female | 32 (38%) | 5 | 27 | |
| Male | 52 (62%) | 13 | 39 | p=0.309 |
| Ethnicity | ||||
| Hispanic/Latino | 4 (5%) | 0 | 4 | |
| Non-Hispanic/Latino | 80 (95%) | 18 | 62 | p=0.573 |
| Race | ||||
| White | 62 (74%) | 13 | 49 | |
| Black/African American | 0 (0%) | 0 | 0 | |
| Asian | 13 (15%) | 4 | 9 | |
| Other | 9 (11%) | 1 | 8 | p= 0.561 |
| Level of Training | ||||
| Intern | 8 (10%) | 0 | 8 | |
| Resident | 29 (35%) | 4 | 25 | |
| Attending | 47 (56%) | 14 | 33 | p=0.077 |
| PGY5–9 | 18 (21%) | |||
| PGY10–14 | 9 (11%) | |||
| PGY15+ | 20 (24%) | |||
| Percent Time in Clinical Care | ||||
| Less than 20% | 2 (2%) | 1 | 2 | |
| 20–50% | 10 (12%_ | 1 | 9 | |
| 51–75% | 10 (12%_ | 3 | 7 | |
| Greater than 75% | 61 (73%) | 13 | 48 | p=0.690 |
| Close friend/family with SUD | ||||
| Yes | 24 (29%) | 6 | 18 | p= 0.668 |
| PRACTICE CHARACTERISTICS | ||||
| X-waiver training completed | ||||
| Yes | 18 (21%) | n/a | n/a | n/a |
| Ordered Naloxone in past 3 months | ||||
| Yes | 39 (46%) | 12 | 27 | p=0.052 |
| Ordered Buprenorphine for a patient in past 3 months | ||||
| Yes | 28 (33%) | 8 | 20 | p=0.259 |
Includes physicians who had an X-waiver (X-waiver) and those who had recently completed training but had not yet obtained an X-waiver (No X-waiver)
p-value for comparison of X-waivered vs non X-waivered physicians done using chi2 tests (p<0.05)
Figure 1: Level of preparation for treatment of OUD in the emergency department.
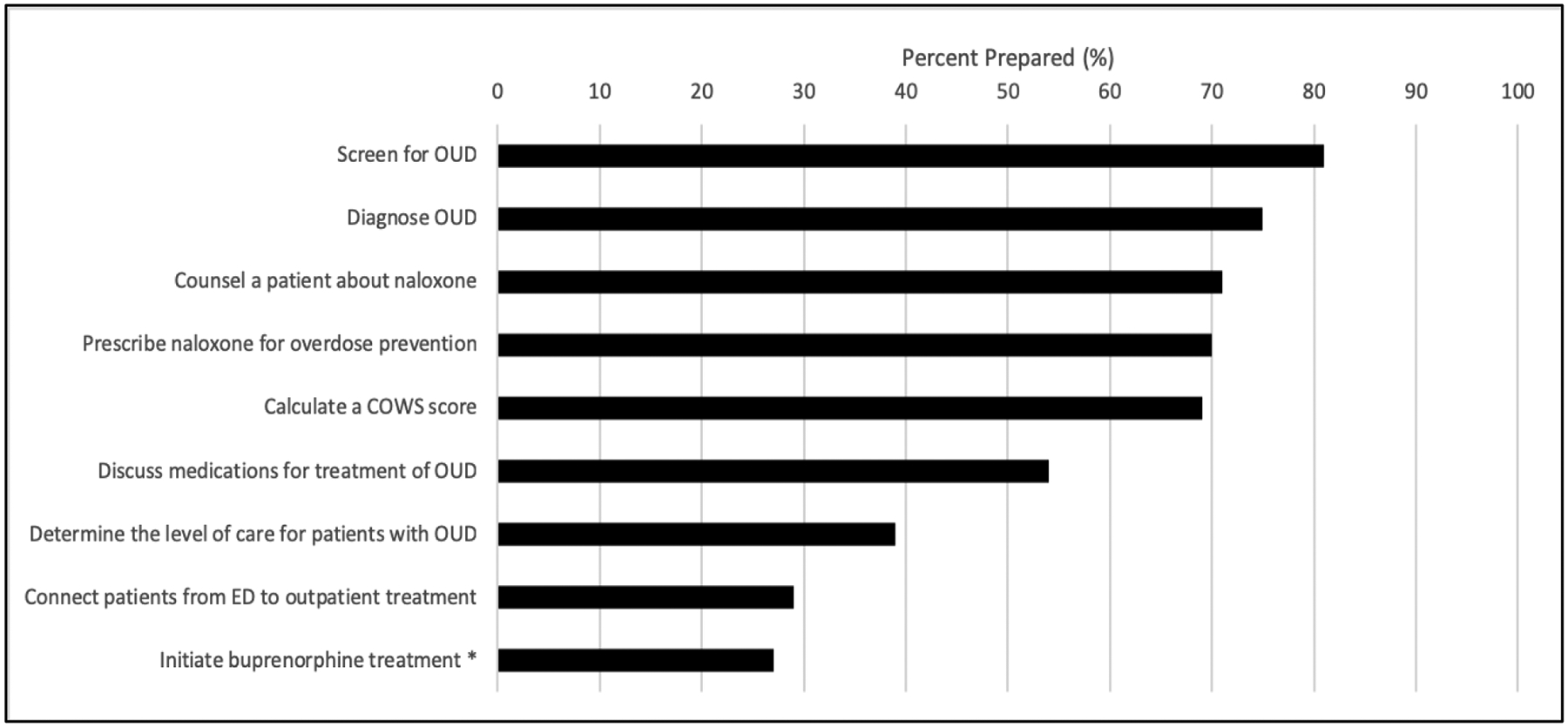
Displayed are the percentage of physicians who rated that they were either “somewhat prepared” or “very prepared” to address each of the aspects of OUD care in the emergency department. The asterisk indicate those responses that significantly differed by X-waiver status. OUD: opioid use disorder; COWS: Clinical Opioid Withdrawal Scale.
Figure 2 shows physician-rated barriers and facilitators to prescribing buprenorphine. Many of the highest-rated concerns related to perceived patient factors, including patient social barriers, lack of patient interest in treatment, availability of referrals for substance use treatment, and patient preference for alternative treatments (e.g. non-medication based). Other highly rated barriers related to buprenorphine – comfort in counseling, ordering, or navigating regulatory barriers – differed significantly between those who had completed the waiver training and those who had not, with a mean rating 4.9 vs 6.3 (p=0.030); 3.1 vs 6.4 (p=0.001); and 3.4 vs 6.4, (p<0.001), respectively. The highest-rated facilitators for buprenorphine prescribing related to longitudinal treatment, including access to ongoing treatment services after discharge and access to a care coordinator/social worker for patients with OUD. Other highly rated facilitators related to support for ED-based treatment, including electronic medical record order sets, pharmacist consultation and availability of peer counselors.
Figure 2: Barriers and Facilitators to Prescribing Buprenorphine in the Emergency Department.
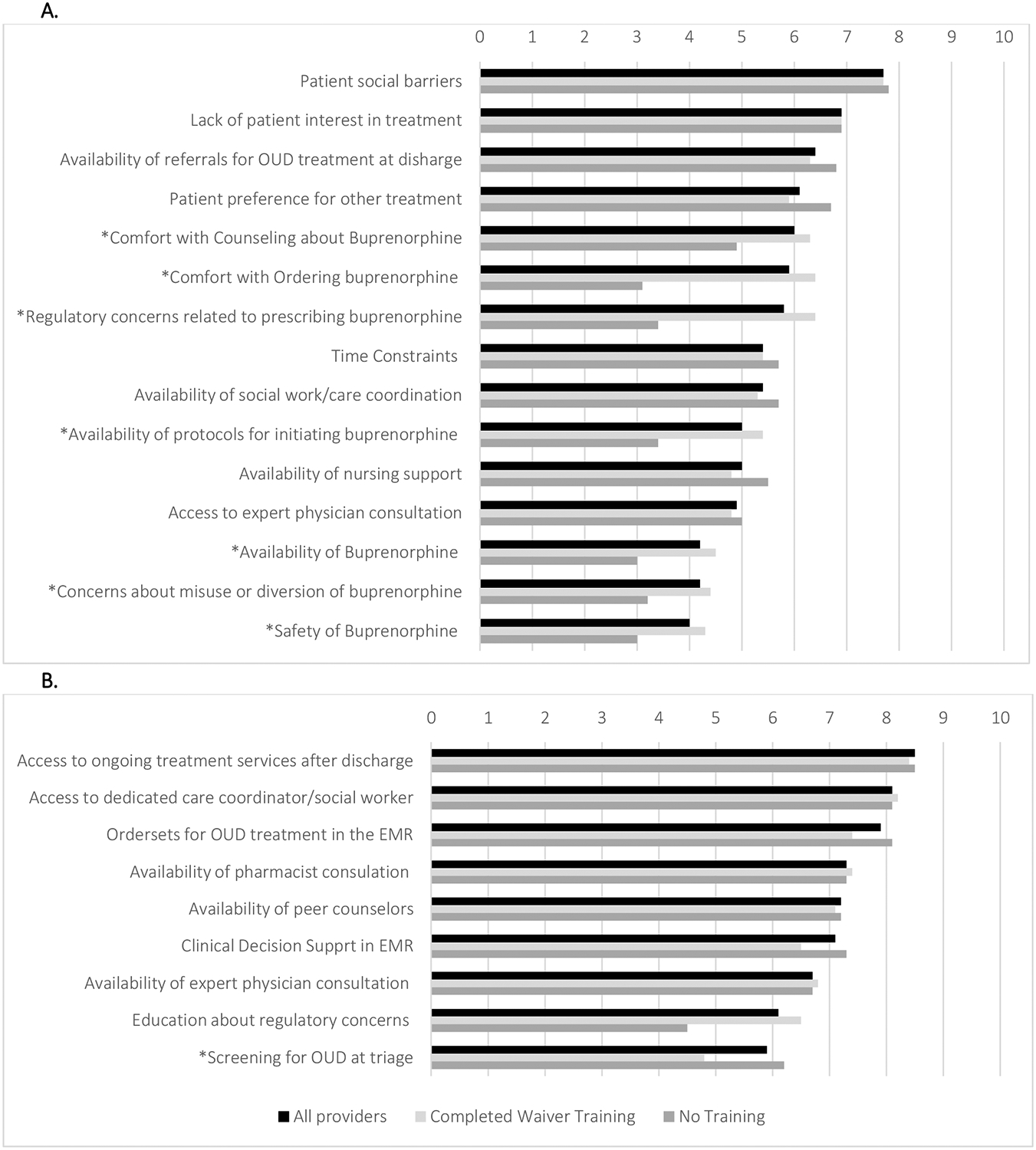
Panel A shows survey results for physician-rated barriers on a scale from 1–10 (10 being the most significant barrier). Panel B shows physician-rated facilitators for prescribing of buprenorphine in the emergency department. The asterisks indicate those responses that significantly differed by X-waiver status (p < 0.05). OUD: opioid use disorder; EMR: electronic medical record.
Finally, we asked the 66 physicians who had not yet completed X-waiver training about barriers and facilitators to obtaining an X-waiver (Figure 3). The highest rated barriers to obtaining an X-waiver were the inconvenience of the process and uncompensated time outside work. Top-rated facilitators included substituting training for a shift and financial incentives.
Figure 3: Barriers and Facilitators to obtaining an X-waiver for emergency department physicians.
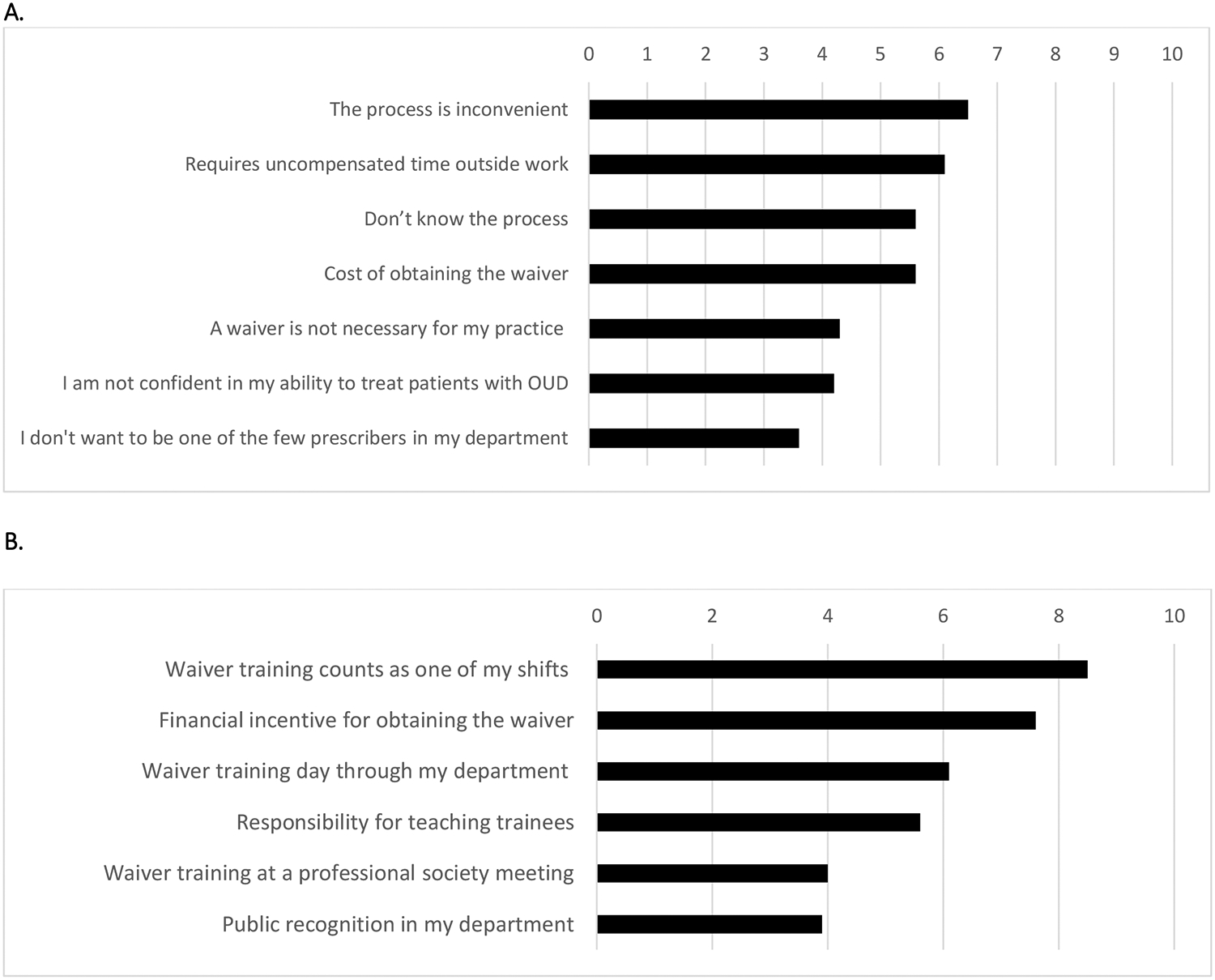
Panel A shows survey results for physician-rated barriers to obtaining an X-waiver among those who had not completed a waiver training on a scale from 1–10 (10 being the most significant barrier). Panel B shows physician-rated facilitators for obtaining an X-wavier. OUD: opioid use disorder.
Our results contribute to translation of evidence into practice for ED-initiated addiction treatment in several key ways. First, while most physicians felt unprepared for referral and treatment with buprenorphine in the ED, X-waiver training was associated with higher self-rated preparation, suggesting that interventions to address knowledge or confidence gaps may increase buprenorphine implementation. However, the most significant physician-reported barriers to prescribing buprenorphine related to perceived patient, logistical or systemic factors. These barriers did not differ by X-waiver status, suggesting that they may not be mitigated by waiver training or other educational interventions alone. Promising strategies to address these barriers and increase treatment include multidisciplinary teams with social workers and peer specialists, development of treatment and referral protocols, and other supports that address patient or system-level barriers [11]. Finally, our findings demonstrate that the burden of X-waiver training poses challenges. Incentives may be one effective strategy for overcoming barriers, but they may need to be further reduced through regulatory changes to ease the burden of the X-waiver training [12]. As ED-initiated treatment expands, it will be critical to develop interventions that address not only provider knowledge but also patient and system-level challenges.
Funding Sources:
Dr. Lowenstein and Dr. Kilaru are funded by the Department of Veterans Affairs through the National Clinician Scholars Program. Additional funding was provided by NIH K23HD090272001 (Dr. Delgado).
Footnotes
Prior Presentations: None
Disclosures:
ML, AK, JH, DAR, JP, ZFM report no conflicts of interest.
MKD received an honorarium for participating in an Expert Roundtable on opioid prescribing convened by United Health Group.
References
- 1.Understanding the Epidemic. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Division of Unintentional Injury Prevention, 2018. (Accessed December 15, 2018, at https://www.cdc.gov/drugoverdose/index.html.)
- 2.D’Onofrio G, O’Connor PG, Pantalon MV, et al. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. Jama 2015;313:1636–44. doi: 10.1001/jama.2015.3474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martin A, Mitchell A, Wakeman S, White B, Raja A. Emergency Department Treatment of Opioid Addiction: An Opportunity to Lead. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine 2017. doi: 10.1111/acem.13367. [DOI] [PubMed] [Google Scholar]
- 4.Cunningham CO, Sohler NL, McCoy K, Kunins HV. Attending physicians’ and residents’ attitudes and beliefs about prescribing buprenorphine at an urban teaching hospital. Fam Med 2006;38:336–40. [PubMed] [Google Scholar]
- 5.Hutchinson E, Catlin M, Andrilla CH, Baldwin LM, Rosenblatt RA. Barriers to primary care physicians prescribing buprenorphine. Annals of family medicine 2014;12:128–33. doi: 10.1370/afm.1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DeFlavio JR, Rolin SA, Nordstrom BR, Kazal LA Jr. Analysis of barriers to adoption of buprenorphine maintenance therapy by family physicians. Rural Remote Health 2015;15:3019. [PubMed] [Google Scholar]
- 7.Huhn AS, Dunn KE. Why aren’t physicians prescribing more buprenorphine? Journal of substance abuse treatment 2017;78:1–7. doi: 10.1016/j.jsat.2017.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andraka-Christou B, Capone MJ. A qualitative study comparing physician-reported barriers to treating addiction using buprenorphine and extended-release naltrexone in U.S. office-based practices. The International journal on drug policy 2018;54:9–17. doi: 10.1016/j.drugpo.2017.11.021 [DOI] [PubMed] [Google Scholar]
- 9.Haffajee RL, Bohnert ASB, Lagisetty PA. Policy Pathways to Address Provider Workforce Barriers to Buprenorphine Treatment. American journal of preventive medicine 2018;54:S230–s42. doi: 10.1016/j.amepre.2017.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Englander H, Collins D, Perry SP, Rabinowitz M, Phoutrides E, Nicolaidis C. “We’ve Learned It’s a Medical Illness, Not a Moral Choice”: Qualitative Study of the Effects of a Multicomponent Addiction Intervention on Hospital Providers’ Attitudes and Experiences. J Hosp Med 2018;13:752–8. doi: 10.12788/jhm.2993. [DOI] [PubMed] [Google Scholar]
- 12.Fiscella K, Wakeman SE, Beletsky L. Buprenorphine Deregulation and Mainstreaming Treatment for Opioid Use Disorder: X the X Waiver. JAMA psychiatry 2018. doi: 10.1001/jamapsychiatry.2018.3685. [DOI] [PubMed] [Google Scholar]


