Abstract
Background:
Two surgical approaches, an anterolateral and a posterolateral approach, have been advocated for lateral condylar fractures (LCFs) of the humerus in children. The purpose of this study was to evaluate the radiographic and clinical outcomes of the 2 surgical approaches.
Methods:
We retrospectively analyzed the data of consecutive patients <15 years of age with an LCF treated via open reduction and internal fixation through 1 of 2 surgical approaches during the period of April 2000 to March 2019. Patients were classified into the anterolateral (AL) and posterolateral (PL) groups, according to the surgical approach used. Postoperative complications and radiographic and clinical findings (including range of motion and findings on the basis of the Flynn criteria) were investigated. To investigate humeral deformity, the Baumann angle and the carrying angle were measured on anteroposterior radiographs.
Results:
Sixty-one of 82 patients met the inclusion criteria. The AL group included 17 patients (13 male, 4 female), and the PL group included 44 patients (28 male, 16 female). In the PL group, 7 patients had cubitus varus deformity, 3 had malunion due to unacceptable reduction of fracture fragments, and 6 had elbow joint contracture. In the AL group, the overall clinical results were excellent for 15 patients and good for 2. In the PL group, the clinical results were excellent for 12 patients, good for 14, fair for 6, and poor for 12.
Conclusions:
An anterolateral approach would be the optimal approach for an LCF in pediatric patients.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
A lateral condylar fracture (LCF) of the distal part of the humerus (OTA/AO classification, 13B1) is the second-most common elbow injury in pediatric patients, accounting for 12% of pediatric fractures around the elbow joint2. LCFs that are minimally displaced or nondisplaced can be treated nonoperatively3-7. However, LCFs with fracture-fragment displacement of >2 mm are typically treated surgically3,4,7-10. Because LCFs are intra-articular fractures, anatomical reduction with open reduction and internal fixation (ORIF) is required to prevent nonunion or malunion and deformity of the humerus4,11. Therefore, the optimal approach to the articular surface of the humeroulnar and humeroradial joints must provide good access to the injured articular surface.
Several surgical approaches to the humeroulnar and humeroradial joints have been reported12-15. In the present study, we retrospectively reviewed the radiographic and clinical results of pediatric LCFs treated with ORIF via an anterolateral or a posterolateral approach and assessed postoperative complications, including infection, malunion, osteonecrosis, cubitus valgus or varus deformity, and restriction of elbow range of motion.
Materials and Methods
This retrospective case series included patients treated at our institution and related hospitals. Patients’ demographic characteristics, medical history, imaging findings, and follow-up data were extracted from their medical records. This study received approval from our institutional review board and was conducted in conformity with the ethical guidelines of the 1975 Declaration of Helsinki. Written informed consent for treatment and publication of data was obtained from all patients and their parents.
Patients
Screened for inclusion were consecutive patients <15 years of age who were treated with ORIF for an LCF during the period of April 2000 to March 2019. Inclusion criteria included complete baseline and demographic data as well as pre- and postoperative radiographs of the bilateral humeri. Exclusion criteria included incomplete data, a follow-up duration of <6 months, bilateral injuries, a previous ipsilateral and/or contralateral upper-extremity fracture, and previous elbow deformity. In addition, patients who underwent ORIF >3 weeks after the fracture were excluded. Patients were classified into 2 groups according to the surgical approach used: an anterolateral approach (the AL group) or a posterolateral approach (the PL group).
Preoperative Evaluation
Preoperative data collected for analysis included age, sex, side of injury, mechanism of injury, concomitant injures, and type of fracture displacement or fracture line. Preoperative radiographic evaluation included classification of LCF displacement in accordance with the Jakob classification11, and classification of LCF lines in accordance with the Milch classification16 (Table I). To verify these classifications, surgical reports were also reviewed.
TABLE I.
| Classification | Type of Fracture Displacement (Jakob) or Line (Milch) |
| Jakob | |
| Type I | Little or no displacement |
| Type II | Moderate lateral translation with or without fragment tilt |
| Type III | Major fragment tilt or rotation on the axis of the humerus |
| Milch | |
| Type I | Fracture line lateral to the trochlear groove |
| Type II | Fracture line extending into the trochleargroove |
Surgical Procedures
Anterolateral Approach
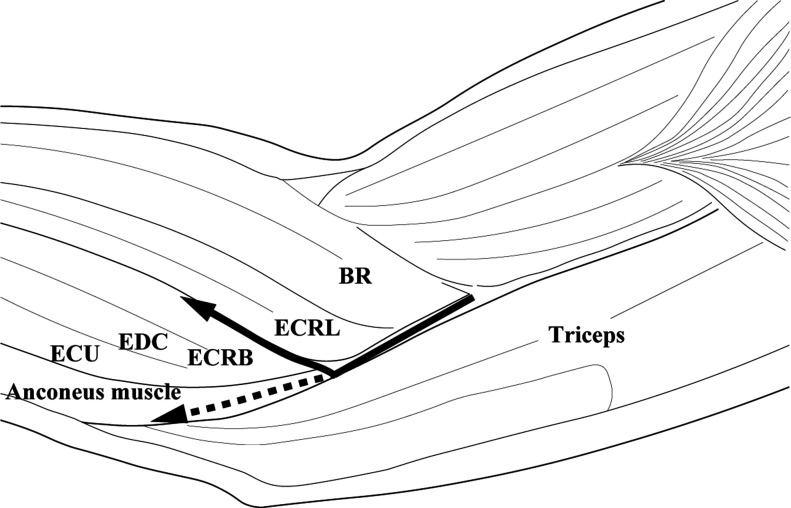
For the anterolateral approach, open reduction was performed with or without use of a pneumatic tourniquet and with the patient under general anesthesia and in the supine position. An approximately 5-cm-long incision was made on the lateral side of the distal part of the humerus. An anterolateral approach to the distal part of the humerus was made through the space between the extensor carpi radialis longus (ECRL) and the extensor carpi radialis brevis (ECRB) anteriorly, and between the ECRL-brachioradialis and the triceps posteriorly (Fig. 1, solid line)14. After the subcutaneous tissue was dissected with blunt scissors, the attachments between the ECRB and ECRL and the distal part of the humerus were identified and released, which exposed the anterior articular aspect of the lateral condyle.
Fig. 1.
Illustration showing the anterolateral and the posterolateral approach. The anterolateral approach to the distal part of the humerus (solid line) is made through the space between the extensor carpi radialis longus (ECRL) and the extensor carpi radialis brevis (ECRB) anteriorly, and between the ECRL-brachioradialis (BR) and the triceps posteriorly. The posterolateral approach to the distal part of the humerus (dashed line) is made through the space between the anconeus muscle and the ECRB anteriorly, and between these same structures and the triceps posteriorly. ECU = extensor carpi ulnaris, and EDC = extensor digitorum communis.
Posterolateral Approach
For the posterolateral approach, open reduction was performed with or without use of a pneumatic tourniquet and with the patient under general anesthesia and in the prone or lateral position. The initial incision was either an approximately 4-cm-long, lazy S incision on the posterolateral aspect of the humerus or an approximately 7-cm-long, longitudinal incision on the posterior aspect of the humerus. The posterolateral approach to the distal part of the humerus was made through the space between the anconeus muscle and the ECRB anteriorly, and between these same structures and the triceps posteriorly (Fig. 1, dashed line)13. After the subcutaneous tissue was dissected with blunt scissors, the attachments between the anconeus muscle and the ECRB and the distal part of the humerus were identified and released, which exposed the posterior aspect of the humerus.
Fixation Procedures for LCFs
After open reduction, internal fixation was carried out under fluoroscopic guidance using 2 or 3 smooth, 1.4 to 1.6-mm-diameter Kirschner wires, or 2 smooth Kirschner wires augmented by tension-band wiring using 0.7 to 0.8-mm-diameter smooth suture wire. All of the wires were buried subcutaneously.
Postoperative Treatment
Postoperatively, a long arm cast was applied in all cases. Following cast removal, patients were encouraged to perform gentle active range-of-motion exercises at home. Pins and wires were removed after the attainment of osseous union.
Postoperative Evaluation
The collected data included the duration between injury and surgery, follow-up duration, duration of immobilization, time from surgery to osseous union, and duration between ORIF and wire removal. The occurrences of clinical and radiographic complications from the time of surgery until the final follow-up evaluation were also recorded, including superficial or deep infection, postoperative displacement, malunion, osteonecrosis of the lateral humeral condyle, elbow deformity, and contracture of the elbow joint.
Osseous union was confirmed by the presence of bone-bridging on anteroposterior, lateral, and oblique radiographs. In the radiographic evaluation, the Baumann angle (BA) and the carrying angle (CA) were measured on anteroposterior radiographs according to the criteria defined by Goldfarb et al.17. The BA and CA of the injured side at the time of final follow-up were compared with those of the uninjured side, and the absolute values of these calculations were used as the outcomes. BA gain and CA loss were calculated by subtracting the value of the BA and CA of the injured side from the BA and CA of the contralateral side, respectively. The incidence of cubitus varus and of cubitus valgus were recorded. Cubitus varus and cubitus valgus were defined as a CA of <0° and a CA of >20°, respectively.
Clinical evaluation included assessments of range of motion and findings on the basis of the Flynn criteria18, whereby functional and cosmetic factors were assessed. All radiographic measurements were performed by the same clinician (Table II).
TABLE II.
Flynn Criteria (Cosmetic and Functional Factors)*
| Result | Rating | Cosmetic Factor, CA loss (°) | Functional Factor, ROM loss (°) |
| Satisfactory | Excellent | 0-5 | 0-5 |
| Good | 6-10 | 6-10 | |
| Unsatisfactory | Fair | 11-15 | 11-15 |
| Poor | >15 | >15 |
CA = carrying angle, and ROM = range of motion. All cases with cubitus varus deformity were rated as “poor.”
Statistical Analysis
All statistical analyses were conducted using SPSS software (version 25; IBM). Patient characteristics are summarized using descriptive statistics; continuous variables are reported as the mean and standard deviation, while categorical variables are reported as the number of cases and percentage. Continuous normally distributed variables were compared using a Welch t test, while continuous non-normally distributed variables were compared using the Mann-Whitney U test. A Fisher exact test was used to compare 2 independent groups. Differences among categorical variables were analyzed using the chi-square test. P values of <0.05 were considered significant. To interpret the various effect sizes, independent of the unit of measure of the outcome variable, the effect size of the Pearson correlation (r) was calculated; the effect size is low if the value of r is around 0.1; medium, if r is around 0.3; and large, if r is >0.5. Moreover, to estimate the statistical power to detect differences between 2 groups, post-hoc estimates of our statistical power were carried out in G*Power software (version 3.1.9.4)19. An a priori power analysis was not performed, as this study was a retrospective review study.
Results
A total of 82 children <15 years of age were screened for inclusion. Twenty patients with a follow-up duration of <6 months or with incomplete radiographic and medical records were excluded. A patient who underwent ORIF at 50 days after initial injury was also excluded. Thus, 61 of 82 patients met the inclusion criteria. Cohort demographic and injury data are shown in Table III. All of the surgical procedures were performed by 3 experienced hand surgeons who used magnifying surgical glasses. Regarding the procedure used for LCF fixation, all 17 patients in the AL group and 17 of the 44 patients in the PL group underwent Kirschner wire fixation augmented by tension-band wiring; the other 27 patients in the PL group underwent fixation with 2 or 3 Kirschner wires only.
TABLE III.
Cohort Demographic and Injury Data for Lateral Condylar Fractures of the Humerus in Children
| Parameter | AL Group (N = 17) | PL Group (N = 44) | P Value | R Value* |
| Age† (yr) | 6.0 ± 2.1 (3-10) | 6.1 ± 2.3 (1-10) | 0.853 | 0.03 |
| Sex (no. [%]) | ||||
| Male | 13 (76.5) | 28 (63.6) | 0.382 | 0.12 |
| Female | 4 (23.5) | 16 (36.4) | ||
| Side of injury (no. [%]) | ||||
| Left | 10 (58.8) | 22 (50) | 0.580 | 0.08 |
| Right | 7 (41.2) | 22 (50) | ||
| Mechanism of injury (no. [%]) | ||||
| Fall from a height of >1 m | 6 (35.3) | 23 (52.3) | 0.266 | 0.12 |
| Fell down | 11 (64.7) | 21 (47.7) | ||
| Concomitant injures (no.) | ||||
| Olecranon fracture | 0 | 2 | 0.524 | 0.02 |
| Posteromedial elbow dislocation | 1 | 3 | 0.700 | 0.11 |
| Jakob classification (no. [%]) | ||||
| Type II | 13 (76.5) | 30 (68.2) | 0.755 | 0.01 |
| Type III | 4 (23.5) | 14 (31.8) | ||
| Milch classification (no. [%]) | 1.000 | 0.08 | ||
| Type I | 2 (11.8) | 5 (11.4) | ||
| Type II | 15 (88.2) | 39 (88.6) |
The r value represents the effect size of Pearson correlation.
The values are given as the mean and standard deviation, with the range in parentheses.
Cohort follow-up data and postoperative complications are shown in Table IV. Additional surgical procedures for wire removal were needed for all patients in the AL group and for 41 patients in the PL group; 3 patients in the PL group underwent Kirschner wire removal under local anesthesia at an outpatient clinic.
TABLE IV.
Cohort Follow-up Data and Complications
| Parameter | AL Group (N = 17) | PL Group (N = 44) | P Value | R Value* |
| Duration between injury and surgery† (days) | 5.2 ± 4.8 (1-16) | 4.7 ± 4.6 (0-21) | 0.718 | 0.05 |
| Follow-up duration† (mo) | 20.0 ± 18.8 (6-70) | 14.6 ± 13.4 (6-61) | 0.354 | 0.16 |
| Duration of immobilization† (wk) | 4.2 ± 0.5 (3-5.5) | 4.8 ± 1.4 (3-8) | 0.117 | 0.22 |
| Time from surgery to osseous union† (wk) | 6.6 ± 0.9 (6-8) | 6.5 ± 1.1 (5-10) | 0.785 | 0.03 |
| Duration between ORIF and wire removal (3 cases excluded)† (mo) | 3.6 ± 0.9 (2.5-6) | 4.0 ± 2.0 (1.5-10) | 0.428 | 0.10 |
| Complications‡ | ||||
| Pin-track infection | 0 | 3 | 0.368 | 0.14 |
| Secondary displacement | 0 | 1 | 0.721 | 0.08 |
| Cubitus varus deformity | 0 | 7 | 0.092 | 0.22 |
| Malunion | 0 | 3 | 0.368 | 014 |
| Elbow joint contracture | 0 | 6 | 0.127 | 0.20 |
| Restriction of flexion (>10°) | 0 | 5 | ||
| 11° to 15° | 0 | 2 | ||
| 16° to 20° | 0 | 2 | ||
| >20° | 0 | 1 (capsulolysis was performed) | ||
| Restriction of extension (>15°) | 0 | 1 |
The r value represents the effect size of the Pearson correlation.
The values are given as the mean and standard deviation, with the range in parentheses.
The values are given as the number of cases.
Although no deep infection occurred in either group, pin-track infection occurred in 3 patients in the PL group. Postoperative displacement of the fracture fragment was observed in 1 patient in the PL group, and a reoperation was required to fix the displaced fracture fragment.
Radiographic Evaluation
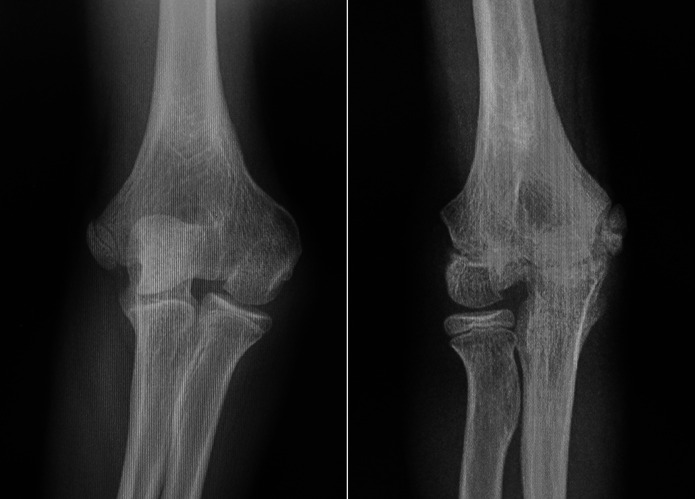
Radiographic findings are shown in Table V. In the PL group, 7 patients had cubitus varus deformity and 3 had malunion due to unacceptable reduction of fracture fragments (Table IV). The malunion comprised articular step-off of the capitellum and cubitus varus deformity (Fig. 2). Moreover, in the PL group, malunion and cubitus varus deformity occurred in 3 and 4 of the 5 patients with a Milch Type-I LCF, respectively. Significant differences were observed in the BA (p = 0.035) and CA (p = 0.025) of the injured elbow. Furthermore, there was a significant difference in the incidence of “excellent” or “good” ratings for cosmetic factor (p = 0.028) based on the Flynn criteria (Table V).
Fig. 2.
Final follow-up radiographs from 2 case examples. Left: Posteroanterior view of the right elbow of a 6-year-old boy with a Milch Type-I lateral condylar fracture (LCF), showing malunion with residual articular step-off of the LCF and notable cubitus varus deformity. Right: Posteroanterior view of the right elbow of a 9-year-old boy with a Milch Type-I LCF, showing the residual articular step-off of the capitellum.
TABLE V.
Radiographic and Clinical Outcomes
| AL Group (N = 17) | PL Group (N = 44) | P Value | R Value* | |
| Baumann angle† (°) | ||||
| Injured elbow | 69.3 ± 8.4 (57 to 84) | 74.6 ± 8.2 (61 to 98) | 0.035‡ | 0.30 |
| Contralateral elbow | 69.5 ± 7.4 (60 to 83) | 71.0 ± 4.3 (61 to 80) | 0.438 | 0.14 |
| Gain | −0.1 ± 6.3 (−11 to 17) | 3.6 ± 8.5 (−11 to 32) | 0.067 | 0.23 |
| Carrying angle† (°) | ||||
| Injured elbow | 11.3 ± 5.2 (4 to 22) | 7.2 ± 8.0 (−17 to 20) | 0.025‡ | 0.26 |
| Contralateral elbow | 12.7 ± 4.8 (5 to 25) | 12.3 ± 5.7 (3 to 31) | 0.645 | 0.06 |
| Loss | 1.4 ± 3.2 (-3 to 8) | 5.1 ± 8.5 (−9 to 32) | 0.238 | 0.17 |
| Cosmetic factor, Flynn criteria (no. of cases) | ||||
| Excellent | 15 | 19 | ||
| Good | 2 | 15 | ||
| Fair | 0 | 2 | ||
| Poor | 0 | 8 | ||
| Incidence of “excellent” or “good” ratings (% [no. of cases]) | 100% (17/17) | 77.3% (34/44) | 0.028‡ | 0.29 |
| Elbow joint range of motion† (°) | ||||
| Extension | ||||
| Injured elbow | 5.0 ± 4.3 (0 to 15) | 2.1 ± 5.0 (−15 to 15) | 0.035‡ | 0.28 |
| Contralateral elbow | 5.6 ± 4.3 (0 to 15) | 4.7 ± 5.6 (0 to 20) | 0.394 | 0.11 |
| Loss of extension | 0.6 ± 1.7 (0 to 5) | 2.6 ± 5.6 (−5 to 29) | 0.017‡ | 0.33 |
| Flexion | ||||
| Injured elbow | 140.6 ± 2.4 (135 to 145) | 134.7 ± 7.6 (110 to 150) | 0.006‡ | 0.39 |
| Contralateral elbow | 140.6 ± 2.4 (135 to 145) | 138.6 ± 4.4 (130 to 150) | 0.136 | 0.21 |
| Loss of flexion | 0.0 ± 0.0 (0) | 3.9 ± 5.6 (0 to 20) | 0.005‡ | 0.38 |
| Arc | ||||
| Injured elbow | 145.6 ± 5.8 (135 to 155) | 136.9 ± 4.4 (110 to 155) | <0.001‡ | 0.44 |
| Contralateral elbow | 146.2 ± 5.7 (135 to 155) | 143.3 ± 7.4 (130 to 160) | 0.114 | 0.20 |
| Loss of arc | 0.6 ± 1.7 (0 to 5) | 6.8 ± 8.1 (−5 to 31) | <0.001‡ | 0.47 |
| Functional factor, Flynn criteria (no. of cases) | ||||
| Excellent | 17 | 27 | ||
| Good | 0 | 8 | ||
| Fair | 0 | 4 | ||
| Poor | 0 | 5 | ||
| Incidence of “excellent” or “good” ratings (% [no. of cases]) | 100% (17/17) | 79.5% (35/44) | 0.041‡ | 0.26 |
| General evaluation, Flynn criteria (no. of cases) | ||||
| Excellent | 15 | 12 | ||
| Good | 2 | 14 | ||
| Fair | 0 | 6 | ||
| Poor | 0 | 12 | ||
| Incidence of “excellent” or “good” ratings (% [no. of cases]) | 100% (17/17) | 59.1% (26/44) | <0.001‡ | 0.40 |
The r value represents the effect size of the Pearson correlation.
The values are given as the mean and standard deviation, with the range in parentheses.
Significant (p < 0.05).
Clinical Results
Clinical evaluation findings are shown in Tables IV and V. In the PL group, 1 patient had an extension loss of >10° in the injured versus the contralateral elbow, and 5 patients had a flexion loss of >10° in the injured versus the contralateral elbow. One of 6 patients underwent elbow joint capsulolysis to treat a flexion restriction of >20°. Data according to the Flynn criteria are shown in Table V. Significant differences were observed in extension (p = 0.035), flexion (p = 0.006), and arc (p <0.001) of the injured elbow. Also, significant differences were noted for loss of extension (p = 0.017), flexion (p = 0.005), and arc (p <0.001). Furthermore, there were significant differences in the incidence of “excellent” or “good” ratings for functional factor (p = 0.041) and general evaluation (p <0.001) based on the Flynn criteria (Table V).
Power Analysis
A post-hoc power analysis revealed that sample sizes of 17 and 44 elbows in the AL and PL groups, respectively, were sufficient to provide 80% power at a 2-sided alpha level of 0.05 to detect differences between the 2 groups in flexion of the injured elbow (r = 0.39), arc of motion of the injured elbow (r = 0.44), and loss of extension (r = 0.33), loss of flexion (r = 0.38), and loss of arc (r = 0.47) compared with the contralateral elbow. Post-hoc power analysis also revealed that the sample sizes for the assessment of the BA and CA of the injured elbow were sufficient to identify a medium effect size (r = 0.30 and 0.26, respectively). Also, for the general evaluation of the Flynn criteria, a post-hoc power analysis revealed that sample sizes of 17 and 44 elbows in the AL and PL groups, respectively, were sufficient to provide 80% power at a 2-sided alpha level of 0.05 to detect differences between the 2 groups in the incidence of “excellent” or “good” ratings (r = 0.40).
Discussion
Since an LCF is an intra-articular fracture, anatomical reduction of the articular surface of the distal part of the humerus is essential for satisfactory outcomes of LCF treatment in children4,11. In the present study, we reviewed pediatric LCFs treated via ORIF performed through an anterolateral or a posterolateral approach in our institution and related hospitals. Satisfactory clinical outcomes were obtained for all 17 patients in the AL group, compared with only 26 (59.1%) of the 44 patients in the PL group. Moreover, the PL group experienced several serious complications, including postoperative displacement, malunion, cubitus varus deformity, and restriction of extension, flexion, and range of motion.
In the PL group, final follow-up radiographs showed an increased BA compared with the contralateral elbow, and 25 patients had a CA loss of >6°, indicating the failure of anatomical reduction of the LCF. Additionally, LCF malunion and cubitus varus deformity frequently occurred in patients with a Milch Type-I LCF in the PL group. In contrast, only 2 patients had a CA loss of >6° in the AL group. Furthermore, LCF malunion and cubitus varus deformity were not observed in the AL group, regardless of the Jakob or Milch classification.
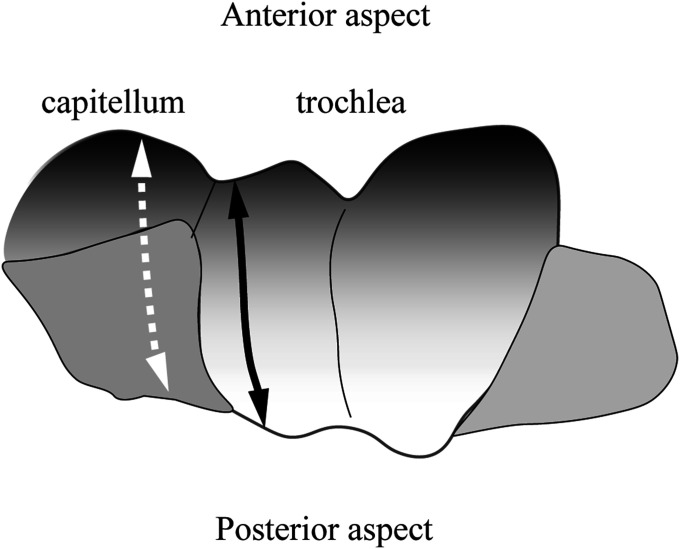
The most widely accepted approach for an LCF in children has traditionally been the posterolateral approach12,13,15. However, the posterolateral approach does not permit visualization of a Milch Type-I LCF: the fracture line for this type is in the humeral capitellum, and the articular cartilage is present only on the anterior side of the distal part of the humerus14. Moreover, the posterolateral approach is inappropriate for some Type-II LCFs with fracture lines on the lateral edge of the trochlea, as the fracture line extends laterally to the humeral capitellum on the posterior side (Fig. 3, solid black line)14. In contrast, an anterolateral approach provides good access to the capitellum and the lateral edge of the trochlea, and is an optimal approach for both Milch Type-I and II LCFs. Since the articular cartilage of the capitellum and the lateral edge of the trochlea are present only on the anterior side, an anterolateral approach provides good visualization of both capitellum and trochlear fractures (Fig. 3, white dashed line). In the PL group, the malreduction of the articular surface was caused by the difficulties in visualizing the articular surface of the lateral edge of the trochlea and the humeral capitellum.
Fig. 3.
Illustration showing the locations of Milch Type-I and II fractures on the anterior and posterior aspects of the humeroulnar and humeroradial joints. The black solid line indicates a Milch Type-II fracture, and the white dashed line indicates a Milch Type-I fracture.
Moreover, a posterolateral approach to LCFs damages the posterior vessels, which provide the blood supply to the lateral humeral condyle. In adults, the vessels penetrating the posterior portion of the lateral epicondyle provide blood supply to the capitellum and trochlea lateral to the trochlear groove, and the interosseous blood supply is distributed anteriorly and medially in the lateral condyle20. In the pediatric population, the blood supply to the capitellum and lateral aspect of the trochlea comes from the posterior condylar perforating vessels on the lateral aspect of the distal part of the humerus21. Thus, damaged vascularization to the lateral condyle might result in growth disturbance or osteonecrosis of the lateral condyle22-26. Conversely, an anterolateral approach with subperiosteal dissection on the anterolateral side of the lateral humeral condyle does not damage the crucial blood supply from the posterior side. Therefore, to prevent damaging the posterior blood supply of the lateral humeral condyle, we recommend that surgeons refrain from a posterior approach for LCF in children20.
The AL and PL groups differed significantly regarding extension, flexion, and arc of motion of the injured elbow. The PL group had restricted extension, flexion, and arc of motion. The reason for this restriction of elbow range of motion is unclear. However, as 5 of 6 of the patients with restriction of elbow flexion underwent ORIF with only 2 Kirschner wires, the fixation procedures might affect the restriction of range of motion. Although several fixation methods have been described11,27-34, fixation with Kirschner wires is common11,28,34. As no comparative study that we are aware of has specifically compared Kirschner wire fixation alone versus tension-band wiring after ORIF for LCF, the optimal fixation procedure for LCF in children is still controversial. However, in the PL group, some patients experienced pain during motion due to irritation from the Kirschner wires, which might have been caused by the loosening of the wires. In contrast, the patients who underwent fixation with Kirschner wires augmented with soft wires did not experience pain during motion. Thus, the method of wire fixation might also affect the restriction of range of motion. Moreover, in the PL group, 1 of the 3 patients with malunion had >15° of restriction of elbow flexion, and 2 of the 3 patients with malunion had approximately 5° of restriction of elbow extension or flexion. Thus, LCF malunion might cause restriction of elbow flexion. Further investigation is needed to determine whether fixation with only Kirschner wires for LCF and/or malunion of an LCF has a negative effect on elbow range of motion.
Our study had several limitations. The major limitation is that our study design was retrospective, which is susceptible to bias. Other limitations are the small sample size and short follow-up duration. A post-hoc power analysis revealed that the sample size used to assess the BA and CA of the injured elbow was sufficient to identify a medium effect size (r = 0.30 and 0.26, respectively). However, to provide 80% power at a 2-sided alpha level of 0.05 to detect differences in the BA and CA of the injured elbow between the 2 groups, the total sample size required would have been 96 and 134 cases, respectively. Moreover, although the average follow-up was >12 months in each group, the minimum 6-month follow-up period was not enough to detect late deformity of the injured elbow. As increased BA or decreased CA would affect the alignment of the limb over the long term, longer follow-up periods are needed to estimate late deformity of the injured elbow. Finally, the choice of the surgical approach depended on the preference of the attending surgeons. A prospective study might be required to obtain a precise result regarding the differences in the clinical outcomes between the 2 surgical approaches.
Conclusions
The present study was a review of pediatric cases of ORIF performed through an anterolateral or posterolateral approach for LCFs treated in our institution and related hospitals. Our study showed that a posterolateral approach did not provide good visualization of fracture lines on the capitellum and the lateral aspect of the trochlea. An anterolateral approach would be the optimal approach for LCF.
Acknowledgments
Note: The authors thank Kelly Zammit, BVSc, from Edanz Group (www.edanzediting.com/ac), for editing a draft of this manuscript.
Footnotes
Investigation performed at the Department of Orthopaedic Surgery, Nippon Medical School, Tokyo, Japan
Disclosure: The authors indicated that no external funding was received for any aspect of this work. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A209).
References
- 1.Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Introduction: fracture and dislocation classification compendium-2018. J Orthop Trauma. 2018. Jan;32(Suppl 1):S1-170. [DOI] [PubMed] [Google Scholar]
- 2.Landin LA, Danielsson LG. Elbow fractures in children. An epidemiological analysis of 589 cases. Acta Orthop Scand. 1986. Aug;57(4):309-12. [DOI] [PubMed] [Google Scholar]
- 3.Flynn JC, Richards JF, Jr, Saltzman RI. Prevention and treatment of non-union of slightly displaced fractures of the lateral humeral condyle in children. An end-result study. J Bone Joint Surg Am. 1975. Dec;57(8):1087-92. [PubMed] [Google Scholar]
- 4.Foster DE, Sullivan JA, Gross RH. Lateral humeral condylar fractures in children. J Pediatr Orthop. 1985. Jan-Feb;5(1):16-22. [DOI] [PubMed] [Google Scholar]
- 5.Bast SC, Hoffer MM, Aval S. Nonoperative treatment for minimally and nondisplaced lateral humeral condyle fractures in children. J Pediatr Orthop. 1998. Jul-Aug;18(4):448-50. [PubMed] [Google Scholar]
- 6.Tan SHS, Dartnell J, Lim AKS, Hui JH. Paediatric lateral condyle fractures: a systematic review. Arch Orthop Trauma Surg. 2018. Jun;138(6):809-17. Epub 2018 Mar 24. [DOI] [PubMed] [Google Scholar]
- 7.Tejwani N, Phillips D, Goldstein RY. Management of lateral humeral condylar fracture in children. J Am Acad Orthop Surg. 2011. Jun;19(6):350-8. [DOI] [PubMed] [Google Scholar]
- 8.Tan JW, Mu MZ, Liao GJ, Li JM. Pathology of the annular ligament in paediatric Monteggia fractures. Injury. 2008. Apr;39(4):451-5. Epub 2007 Nov 19. [DOI] [PubMed] [Google Scholar]
- 9.Hasler CC, von Laer L. Prevention of growth disturbances after fractures of the lateral humeral condyle in children. J Pediatr Orthop B. 2001. Apr;10(2):123-30. [PubMed] [Google Scholar]
- 10.Marcheix PS, Vacquerie V, Longis B, Peyrou P, Fourcade L, Moulies D. Distal humerus lateral condyle fracture in children: when is the conservative treatment a valid option? Orthop Traumatol Surg Res. 2011. May;97(3):304-7. Epub 2011 Apr 7. [DOI] [PubMed] [Google Scholar]
- 11.Jakob R, Fowles JV, Rang M, Kassab MT. Observations concerning fractures of the lateral humeral condyle in children. J Bone Joint Surg Br. 1975. Nov;57(4):430-6. [PubMed] [Google Scholar]
- 12.Liu CH, Kao HK, Lee WC, Yang WE, Chang CH. Posterolateral approach for humeral lateral condyle fractures in children. J Pediatr Orthop B. 2016. Mar;25(2):153-8. [DOI] [PubMed] [Google Scholar]
- 13.Mohan N, Hunter JB, Colton CL. The posterolateral approach to the distal humerus for open reduction and internal fixation of fractures of the lateral condyle in children. J Bone Joint Surg Br. 2000. Jul;82(5):643-5. [DOI] [PubMed] [Google Scholar]
- 14.Tomori Y, Nanno M, Takai S. Anterolateral approach for lateral humeral condylar fractures in children: clinical results. Medicine (Baltimore). 2018. Sep;97(39):e12563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sullivan JA. Fractures of the lateral condyle of the humerus. J Am Acad Orthop Surg. 2006. Jan;14(1):58-62. [DOI] [PubMed] [Google Scholar]
- 16.Milch H. Fractures and fracture dislocations of the humeral condyles. J Trauma. 1964. Sep;4:592-607. [DOI] [PubMed] [Google Scholar]
- 17.Goldfarb CA, Patterson JM, Sutter M, Krauss M, Steffen JA, Galatz L. Elbow radiographic anatomy: measurement techniques and normative data. J Shoulder Elbow Surg. 2012. Sep;21(9):1236-46. Epub 2012 Feb 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Flynn JC, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years’ experience with long-term follow-up. J Bone Joint Surg Am. 1974. Mar;56(2):263-72. [PubMed] [Google Scholar]
- 19.Faul F, Erdfelder E, Lang AG, Buchner AG. *Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007. May;39(2):175-91. [DOI] [PubMed] [Google Scholar]
- 20.Yamaguchi K, Sweet FA, Bindra R, Morrey BF, Gelberman RH. The extraosseous and intraosseous arterial anatomy of the adult elbow. J Bone Joint Surg Am. 1997. Nov;79(11):1653-62. [DOI] [PubMed] [Google Scholar]
- 21.Haraldsson S. On osteochondrosis deformas juvenilis capituli humeri including investigation of intra-osseous vasculature in distal humerus. Acta Orthop Scand Suppl. 1959;38:1-232. [PubMed] [Google Scholar]
- 22.Pennock AT, Salgueiro L, Upasani VV, Bastrom TP, Newton PO, Yaszay B. Closed reduction and percutaneous pinning versus open reduction and internal fixation for type II lateral condyle humerus fractures in children displaced >2 mm. J Pediatr Orthop. 2016. Dec;36(8):780-6. [DOI] [PubMed] [Google Scholar]
- 23.Skak SV, Olsen SD, Smaabrekke A. Deformity after fracture of the lateral humeral condyle in children. J Pediatr Orthop B. 2001. Apr;10(2):142-52. [PubMed] [Google Scholar]
- 24.Liu TJ, Wang EB, Dai Q, Zhang LJ, Li QW, Zhao Q. Open reduction and internal fixation for the treatment of fractures of the lateral humeral condyle with an early delayed presentation in children: a radiological and clinical prospective study. Bone Joint J. 2016. Feb;98-B(2):244-8. [DOI] [PubMed] [Google Scholar]
- 25.Koh KH, Seo SW, Kim KM, Shim JS. Clinical and radiographic results of lateral condylar fracture of distal humerus in children. J Pediatr Orthop. 2010. Jul-Aug;30(5):425-9. [DOI] [PubMed] [Google Scholar]
- 26.Loke WP, Shukur MH, Yeap JK. Screw osteosynthesis of displaced lateral humeral condyle fractures in children: a mid-term review. Med J Malaysia. 2006. Feb;61(Suppl A):40-4. [PubMed] [Google Scholar]
- 27.Sharma JC, Arora A, Mathur NC, Gupta SP, Biyani A, Mathur R. Lateral condylar fractures of the humerus in children: fixation with partially threaded 4.0-mm AO cancellous screws. J Trauma. 1995. Dec;39(6):1129-33. [DOI] [PubMed] [Google Scholar]
- 28.Thomas DP, Howard AW, Cole WG, Hedden DM. Three weeks of Kirschner wire fixation for displaced lateral condylar fractures of the humerus in children. J Pediatr Orthop. 2001. Sep-Oct;21(5):565-9. [PubMed] [Google Scholar]
- 29.Mintzer CM, Waters PM, Brown DJ, Kasser JR. Percutaneous pinning in the treatment of displaced lateral condyle fractures. J Pediatr Orthop. 1994. Jul-Aug;14(4):462-5. [DOI] [PubMed] [Google Scholar]
- 30.Song KS, Kang CH, Min BW, Bae KC, Cho CH, Lee JH. Closed reduction and internal fixation of displaced unstable lateral condylar fractures of the humerus in children. J Bone Joint Surg Am. 2008. Dec;90(12):2673-81. [DOI] [PubMed] [Google Scholar]
- 31.Andrey V, Tercier S, Vauclair F, Bregou-Bourgeois A, Lutz N, Zambelli PY. Lateral condyle fracture of the humerus in children treated with bioabsorbable materials. ScientificWorldJournal. 2013. Oct 9;2013:869418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li WC, Xu RJ. Comparison of Kirschner wires and AO cannulated screw internal fixation for displaced lateral humeral condyle fracture in children. Int Orthop. 2012. Jun;36(6):1261-6. Epub 2011 Dec 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Conner AN, Smith MG. Displaced fractures of the lateral humeral condyle in children. J Bone Joint Surg Br. 1970. Aug;52(3):460-4. [PubMed] [Google Scholar]
- 34.Wilson JN. Fractures of the external condyle of the humerus in children. Br J Surg. 1955. Jul;43(177):88-94. [DOI] [PubMed] [Google Scholar]