Abstract
Background
Phantom limb pain (PLP)—pain felt in the amputated limb–is often accompanied by significant suffering. Estimates of the burden of PLP have provided conflicting data. To obtain a robust estimate of the burden of PLP, we gathered and critically appraised the literature on the prevalence and risk factors associated with PLP in people with limb amputations.
Methods
Articles published between 1980 and July 2019 were identified through a systematic search of the following electronic databases: MEDLINE/PubMed, PsycINFO, PsycArticles, Cumulative Index to Nursing and Allied Health Literature, Africa-Wide Information, Health Source: Nursing/Academic Edition, SCOPUS, Web of Science and Academic Search Premier. Grey literature was searched on databases for preprints. Two reviewers independently conducted the screening of articles, data extraction and risk of bias assessment. The meta-analyses were conducted using the random effects model. A statistically significant level for the analyses was set at p<0.05.
Results
The pooling of all studies demonstrated a prevalence estimate of 64% [95% CI: 60.01–68.05] with high heterogeneity [I2 = 95.95% (95% CI: 95.10–96.60)]. The prevalence of PLP was significantly lower in developing countries compared to developed countries [53.98% vs 66.55%; p = 0.03]. Persistent pre-operative pain, proximal site of amputation, stump pain, lower limb amputation and phantom sensations were identified as risk factors for PLP.
Conclusion
This systematic review and meta-analysis estimates that six of every 10 people with an amputation report PLP–a high and important prevalence of PLP. Healthcare professionals ought to be aware of the high rates of PLP and implement strategies to reduce PLP by addressing known risk factors, specifically those identified by the current study.
Introduction
Phantom limb pain (PLP)—pain felt in the amputated limb–is often accompanied by significant suffering [1]. The condition is difficult to manage and can lead to disability and reduced health-related quality of life [2]. Several risk factors, including stump pain, diabetic cause of amputation and depression, have been found to be associated with the onset and continuation of PLP [3–5]. While there are reports of PLP in people with congenital amputations [6], PLP appears to be more prevalent in people with traumatic or surgical limb amputations [7].
There are conflicting reports on the prevalence of PLP in people with limb amputations. Whereas one study reported a high prevalence of 85.6% [8], another reported a substantially lower prevalence of 29% [9]. The inconsistent reports on the prevalence of PLP are perplexing, but may be due to differences in the study samples (upper- vs lower-limb amputees or mixed populations), countries in which the research was undertaken, and methodologies between studies [10].
Higher prevalence rates of PLP have been reported in people with lower limb amputations than in those with upper limb amputations [4, 11]. Lower limb(s) amputations are performed chiefly to treat complications of diabetes, and may be associated with risk factors for PLP such as pre-amputation pain and depression [12]. The high PLP prevalence could be explained by these risk factors, which are typically absent in people with upper limb amputations, who are typically healthy and undergo amputation due to trauma [13]. Studies that report PLP prevalence in people receiving continuing medical care have a selection bias [3, 4, 14], in that they fail to account for patients not receiving continuing medical care, who may have different prevalence rates [15]. In addition, previous studies suggest that PLP prevalence rates may be lower in developing countries [16]. However, no clear hypothesis for these lower prevalence rates has been proposed. Further, it is not clear if the prevalence rates in developing countries are significantly lower to those seen in developed countries.
Epidemiological studies are essential to inform health care professionals and health system planners about the burden of diseases in a population [17]. Estimates of the burden of PLP have provided conflicting data. To our knowledge, no systematic review has been conducted on the prevalence and risk factors for PLP. Therefore, to obtain an accurate estimate of the burden of PLP, we gathered and critically appraised the literature on the prevalence and risk factors associated with PLP in people with limb amputations.
The primary aim of this systematic review was to estimate the prevalence of PLP in people with limb amputations. The secondary aim was to determine whether there is a difference in the prevalence of PLP in developed and developing countries, as per the World Economic Situation and Prospects classification system [18]. The exploratory aim was to identify risk factors associated with PLP in people with limb amputations.
Materials and methods
This systematic review was designed according to the Preferred Reporting Items of Systematic Reviews and Meta-Analysis (PRISMA) guidelines [19]. The review protocol was registered on PROSPERO [ID: CRD42018094821], and published in Systematic Reviews [15]. The PRISMA criteria fulfilled by this systematic review are presented in S1 File.
Data sources and search procedure
The lead investigator (KL) and a senior librarian (MS) developed a comprehensive search strategy (S2 File) using five Medical Subject Headings (MeSH): prevalence, risk factors, amputation, phantom limb and epidemiology. Articles published between 1980 and July 2019 were identified through a systematic search of the following electronic databases: MEDLINE/PubMed (via EBSCOhost), PsycINFO (via EBSCOhost), PsycArticles, Cumulative Index to Nursing and Allied Health Literature (CINAHL) (via EBSCOhost), Africa-Wide Information (via EBSCOhost), Health Source: Nursing/Academic Edition (via EBSCOhost), SCOPUS, Web of Science and Academic Search Premier (via EBSCOhost). We deviated from protocol and searched for grey literature on bioRxiv (www.biorxiv.org), Preprints (www.preprints.org), Open Science Framework (www.osf.io) and medRxiv (www.medrxiv.org). The reference lists of eligible studies were searched manually to identify more studies that may have been eligible for inclusion in this review. Studies identified from the literature search were saved using the citation manager software programme (EndNote x8), which was also used to remove duplicates [20].
Study selection
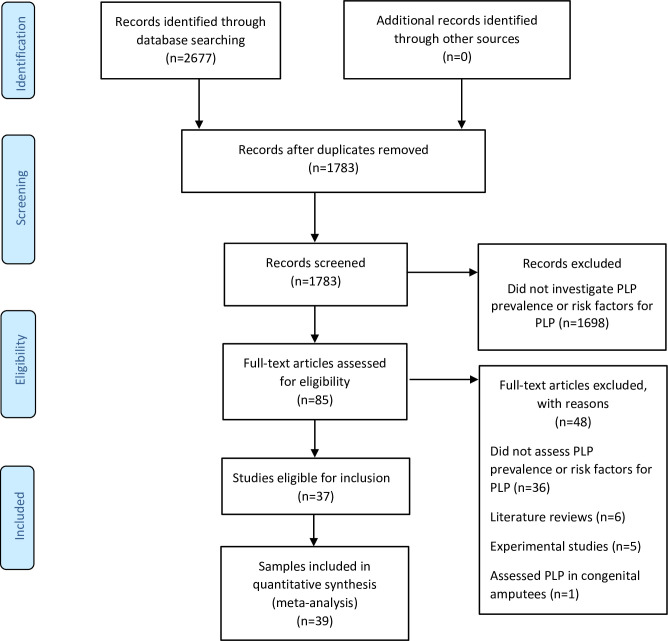
We included cross-sectional, cohort and case-control studies that investigated the prevalence of PLP in adults (18 years or older) with surgical and traumatic upper or lower limb amputations. Only studies written in English, with full text published between 1980 and 2019, were eligible for inclusion in this review. The risk factors for PLP were identified from the included studies. We excluded literature reviews and experimental studies. Two reviewers (KL and GJB) independently screened study titles and abstracts for eligibility. Studies identified in the initial screening as potentially eligible were assessed for eligibility in full-text form by the same reviewers, using the inclusion/exclusion criteria. The study selection procedure was performed using a Microsoft Excel spreadsheet (2016) on which the studies were listed and marked as either eligible or ineligible. In this, we deviated from the registered protocol, which specified the use of Covidence, because Covidence has limited usability offline. A PRISMA flow diagram (Fig 1) represents the entire screening process detailing the numbers of included and excluded studies, with reasons for exclusion. After each stage, results were compared, and disagreements resolved through discussion.
Fig 1. The PRISMA flow diagram illustrating the screening process.
Risk of bias assessment
Two reviewers (KL and GJB) independently assessed the included articles for risk of bias using a risk of bias assessment tool for prevalence studies that had been developed by Hoy et al (S3 File) [21]. This tool assesses the risk of bias based on 10 categories which evaluate the study’s external and internal validity. Each category of the risk of bias tool was set as “high risk” if the study scored “high risk” for any single item within that category, and “low risk” if it scored “low risk” for all items in that category. Categories with “low risk” and “high risk” were given a rating of zero and one respectively. The summary risk of bias rating for each study was presented as “low risk” (score: 0–3), “moderate risk” (score: 4–6), or “high risk” (score: 7–10).
Data extraction
Two reviewers (KL and GJB) used a pre-piloted customised data extraction sheet to independently extract relevant data from included studies. Data extracted included: the names of authors, year of study publication, study design and setting, country of study, sample size, participants’ age and sex, site of amputation, method of data collection, PLP prevalence (%), as well as risk factors and their measures of association with PLP. The developmental status of each country was identified using the World Economic Situation and Prospects classification system [18].
Data analysis
Data extracted from individual studies were entered into an Excel spreadsheet for analysis. All meta-analyses were conducted using Open Meta Analyst software available on (http://www.cebm.brown.edu/openmeta). In this, we deviated from the registered protocol, which specified the use of Review Manager 5, because Review Manager 5 is not suitable for conducting meta-analyses of single arm studies. Cohen's Kappa was used to report inter-rater agreement during screening, data extraction and risk of bias assessment, and can be interpreted as minimal (0–0.39), weak (0.40–0.59), moderate (0.60–0.79) or strong (0.80–0.90) [22]. Clinical heterogeneity was evaluated qualitatively, based on similarities or differences in participant and outcome characteristics, recruitment and assessment procedures, and study setting [23]. Statistical heterogeneity was assessed using the I2 statistic, and the results were presented as low (<25%), moderate (25–50%) and high (>50%) [24]. Subject to consideration of heterogeneity and risk of bias, studies were pooled for meta-analysis using a random effects model to determine a sample-weighted summary estimate of PLP prevalence. A funnel plot was generated to assess for possible publication bias. Furthermore, the Egger’s test was conducted to assess the funnel plot for asymmetry [25]. To address high statistical heterogeneity, we deviated from protocol to sub-group studies into those with low risk of bias and those with moderate and high risk of bias, and conducted separate meta-analyses, and compared the two pooled estimates using a two-tailed Mann-Whitney U test. We also sub-grouped studies by the developmental status of the country in which each study had been conducted [18], as planned in the protocol and, again, compared the estimates using a two-tailed Mann-Whitney U test. Potential risk factors for PLP were identified from the included studies and analysed descriptively. When an association was confirmed, the strength of association between PLP and each risk factor was classified as either “weak”, “moderate”, “strong” or “very strong”, according to the guidelines for interpreting the strength of association in epidemiology studies [26–29]. We calculated Phi (Ø) to determine the strength of association in studies that used the chi-square test as a measure of association. This sample-size-adjusted chi-square statistic has been shown to provide a more accurate reflection of the strength of association between two variables than the interpretation of chi-square and probability (P) values, where high chi-square and p values are thought to represent a strong association between variables [30]. Alpha was set at 0.05 for all analyses.
Results
The initial literature search returned 2677 records, of which 1783 remained after the removal of duplicates. Initial screening of titles and abstracts identified 85 studies that were eligible for full-text review. Full-text review identified 37 studies that were eligible for inclusion in this systematic review. Two of these studies reported two studies each [31, 32]. Therefore, a total of 39 data sets were included in our analysis. The entire screening process reflected moderate agreement (Kappa = 0.70) between reviewers.
Study characteristics
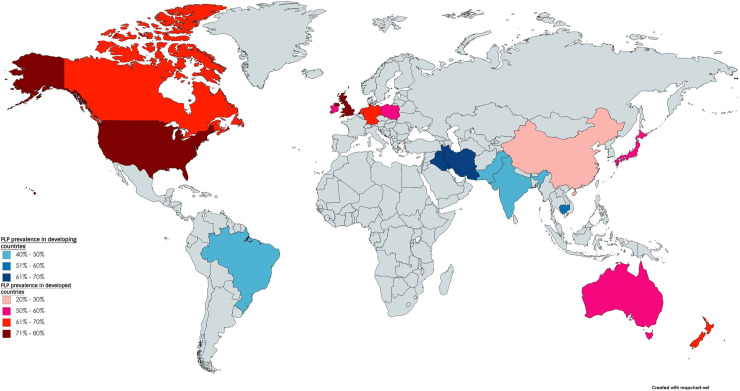
The study characteristics are summarised in Table 1. The included studies had used cross-sectional (n = 35) and cohort (n = 4) study designs. Thirty-two of 39 studies had been conducted in developed countries [18]. Of these, the majority were conducted in North America [USA (n = 7); Canada (n = 2)] and Europe [United Kingdom (n = 8); Germany (n = 5); Netherlands (n = 3); Ireland (n = 2); Poland (n = 1)] (Fig 2). Only seven studies were conducted in developing countries [Iran (n = 2); Iraq (n = 1); India (n = 1); Brazil (n = 1); Pakistan (n = 1); Cambodia (n = 1)]. Table 1 reflects the wide range of data collection approaches used in the studies. The included studies were published between 1986 and 2019. The data extraction process had moderate agreement (Kappa = 0.71) between reviewers prior to discussion.
Table 1. Summary of study and participant characteristics by study.
| Authors | Study type | Country of study | Development status | Method of data collection | Sample size | Age Mean (SD) | Sex M/F | Level of amputation (UL/LL) | PLP prevalence (%) |
|---|---|---|---|---|---|---|---|---|---|
| Ahmed et al., 2017 | Cross-sectional | India | Developing | Self-reported questionnaire | 139 | 38.23 (1.54) | 102/37 | 36/103 | 41 |
| Aldington et al., 2014 | Cross-sectional | UK | Developed | Self-reported questionnaire | 48 | 28.8 (6.7) | - | 11/54 | 49 |
| Bekrater et al., 2015 | Cross-sectional | Germany | Developed | Postal and telephone questionnaire | 3234 | 64.37 (15.89) | 2637/597 | 824/2410 | 62.55 |
| Bin Ayaz et al., 2015 | Cross-sectional | Pakistan | Developing | Face-to-face interview | 268 | 28 (6) | 266/2 | 35/233 | 42.5 |
| Bosmans et al., 2007 | Cross-sectional | Netherlands | Developed | Face-to-face interview | 16 | 66.5 (39–86)* | 11/5 | 0/16 | 81.25 |
| Buchanan et al., 1986 | Cross-sectional | Canada | Developed | Face-to-face interview | 716 | - | 616/100 | 43/647 | 62.4 |
| Byrne et al., 2011a | Cross-sectional | New Zealand | Developed | Face-to-face interview | 29 | 41.7 (4.8) | 25/4 | 7/24 | 69 |
| Byrne et al., 2011b | Cross-sectional | Cambodia | Developing | Face-to-face interview | 29 | 40.3 (10.5) | 25/4 | 1/28 | 51.7 |
| Clark et al., 2013 | Cross-sectional | UK | Developed | Postal and telephone questionnaire | 102 | 70.9 (1.27) | - | 0/97 | 85.6 |
| Datta et al., 2004 | Cohort | UK | Developed | Postal questionnaire | 60 | 58.1 (-) | 48/12 | 60/0 | 60 |
| Desmond et al., 2010 | Cross-sectional | Ireland | Developed | Self-reported questionnaire | 141 | 74.8 (-) | 138/3 | 141/0 | 42.6 |
| Dijkstra et al., 2002 | Cross-sectional | Netherlands | Developed | Postal questionnaire | 536 | - | 367/150 | 99/433 | 72 |
| Ehde et al., 2000 | Cross-sectional | USA | Developed | Postal questionnaire | 255 | 55.1 (14.3) | 207/48 | 0/255 | 72 |
| Ephraim et al., 2005 | Cross-sectional | USA | Developed | telephone interview | 914 | 50.3 (13.3) | 552/362 | 100/812 | 79.9 |
| Gallagher et al., 2001 | Cross-sectional | Ireland | Developed | Postal questionnaire | 104 | 45.3 (18.9) | 78/26 | 0/104 | 69.2 |
| Hanley et al., 2006 | Cross-sectional | USA | Developed | Postal and telephone questionnaire | 255 | 55 (14.3) | 207/48 | 0/255 | 72 |
| Hanley et al., 2009 | Cross-sectional | USA | Developed | Postal questionnaire | 104 | 46.9 (14.1) | 75/29 | 104/0 | 79 |
| Hnoosh et al., 2014 | Cross-sectional | Iraq | Developing | Self-reported questionnaire | 118 | 32 (12.9) | 97/21 | 0/181 | 61 |
| Houghton et al., 1994 | Cross-sectional | UK | Developed | Postal questionnaire | 176 | 71 (-) | - | 0/176 | 78 |
| Kern et al., 2012 | Cross-sectional | Germany | Developed | Postal questionnaire | 537 | 59 (-) | 382/155 | 24/513 | 74.5 |
| Ketz et al., 2008 | Cross-sectional | Germany | Developed | Self-reported questionnaire | 30 | - | 30/0 | 7/27 | 77 |
| Kooijman et al., 2000 | Cross-sectional | Netherlands | Developed | Unclear | 72 | 44.2 (35–65)* | 57/15 | 72/0 | 51 |
| Larbig et al., 2019 | Cohort | Germany | Developed | Face-to-face interview and self-reported questionnaire | 52 | - | 41/11 | 2/50 | 75 |
| Morgan et al., 2017 | Cross-sectional | USA | Developed | Self-reported and internet questionnaire | 1296 | 54.4 (13.7) | 909/387 | 0/1296 | 48.1 |
| Noguchi et al., 2019 | Cross-sectional | Japan | Developed | Medical records | 44 | - | 33/11 | 22/22 | 50 |
| Penna et al., 2018 | Cohort | Australia | Developed | Medical records | 96 | - | 74/22 | 0/96 | 52.2 |
| Probstner et al., 2010 | Cross-sectional | Brazil | Developing | Self-reported questionnaire | 75 | 54.4 (18.5) | 50/25 | 6/69 | 46.7 |
| Rafferty et al., 2015 | Cross-sectional | UK | Developed | Self-reported questionnaire | 75 | 26.3 (18–42)* | 74/1 | 0/84 | 85 |
| Rahimi et al., 2012 | Cross-sectional | Iran | Developing | Face-to-face interview | 335 | 42.1 (6.32) | 324/11 | 0/670 | 66.7 |
| Rayegani et al., 2010 | Cross-sectional | Iran | Developing | Face-to-face interview and self-reported questionnaire | 335 | - | 327/8 | 0/670 | 64 |
| Razmus et al., 2017 | Cross-sectional | Poland | Developed | Face-to-face interview and self-reported questionnaire | 22 | 61 (11.3) | 15/7 | 3/22 | 59 |
| Reiber et al., 2010a | Cross-sectional | USA | Developed | Postal, internet and telephone questionnaire | 298 | 60.7 (3.0) | 298/0 | 78/300 | 72.2 |
| Reiber et al., 2010b | Cross-sectional | USA | Developed | Postal, internet and telephone questionnaire | 283 | 29.3 (5.8) | 274/9 | 78/273 | 76 |
| Resnik et al., 2019 | Cross-sectional | Canada | Developed | Telephone interview | 808 | 63.2 (14.2) | 787/21 | 840/0 | 76.1 |
| Richardson et al., 2007 | Cohort | UK | Developed | Face-to-Face interview | 59 | 63.8 (10.4) | 37/22 | 0/59 | 78.8 |
| Richardson et al., 2015 | Cross-sectional | UK | Developed | Face-to-face interview | 89 | 65.5 (11.4) | 64/25 | 0/89 | 63 |
| Schley et al., 2008 | Cross-sectional | Germany | Developed | Postal and telephone questionnaire | 65 | 45 (18–80)* | 60/5 | 65/0 | 44.6 |
| Wartan et al., 1997 | Cross-sectional | UK | Developed | unclear | 526 | 73 (-)* | 526/0 | 99/471 | 62 |
| Yin et al., 2017 | Cross-sectional | China | Developed | Telephone interview | 391 | - | - | - | 29 |
* Indicates the median age and range.
The number of amputations and males versus females do not add up to the total sample size because some participants had more than one amputation and these data were not provided.
Fig 2. World map showing the countries in which the studies were conducted.
Participant characteristics
The included studies provided data from a total of 12738 participants (9814 male; 2183 female) who had undergone upper limb (n = 2757) and lower limb (n = 10539) amputations. Participant characteristics are provided in Table 1.
Risk of bias assessment
The risk of bias assessment revealed moderate agreement (Kappa = 0.69) between reviewers prior to discussion. The results of the risk of bias assessment are reported in S4 File. Four studies had an overall rating of “low risk” [33–36]. Six studies scored “low risk” for selection bias, for using a sample that was a close representation of the national population [2, 34, 35, 37–39]. Eight studies scored “low risk” for study participation bias, because their response rates for participation were ≥75% [2, 13, 34, 36, 40–43]. Twelve studies scored “low risk” for measurement bias, for using a clear definition of PLP [1, 4, 5, 12, 16, 33, 35–38, 44, 45]. Other studies scored “high risk” for measurement bias, for not providing a clear definition of PLP (e.g. pain felt in the limb after amputation). All the studies scored “high risk” for measurement bias, for using an instrument that has not been shown to be valid and reliable for measuring the outcome of interest. However, all studies scored “low risk” for reporting bias, for appropriately reporting the numerators and denominators for the outcome of interest.
Prevalence of phantom limb pain
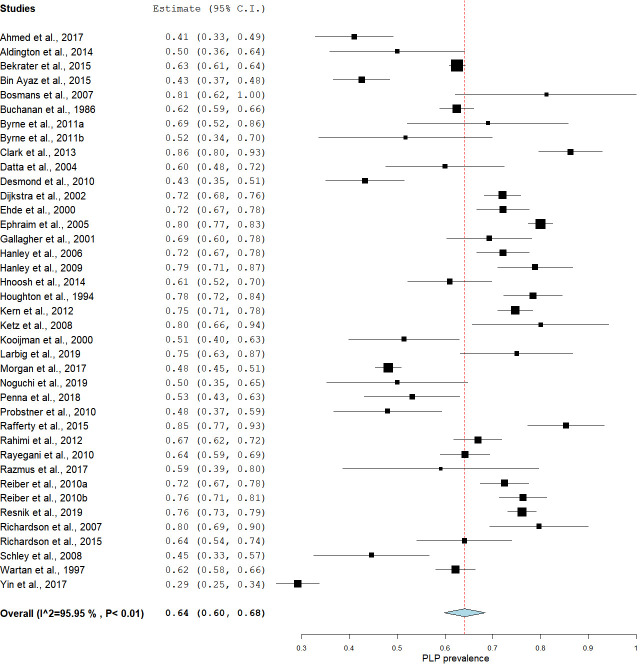
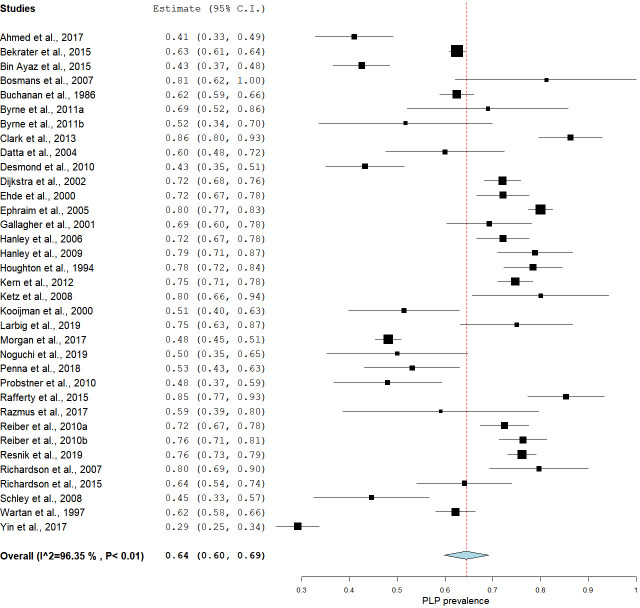
The estimates of PLP prevalence in people with limb amputations ranged between 27% and 85.6% [8, 13], with most studies (31 out of 39) reporting a prevalence between 50% and 85.6% [8, 31]. The pooling of all studies using a random effects model yielded an estimated prevalence of 64% [95% CI: 60.01–68.05], but with high statistical heterogeneity [I2 = 95.95% (95% CI: 95.10–96.60)] (Fig 3). The Egger’s regression analysis of all the included studies revealed no publication bias [-0.80 (95%CI: -4.32–2.01); p = 0.64].
Fig 3. A forest plot showing the overall pooled estimated prevalence of PLP in people with amputations.
Exploratory subgrouping
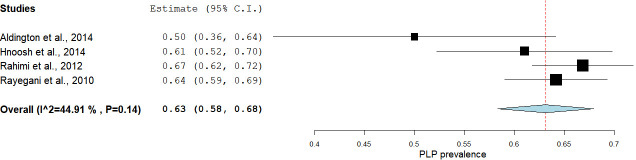
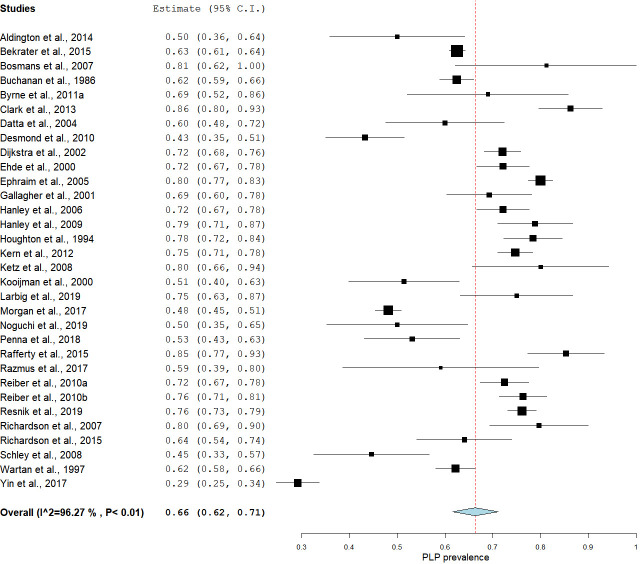
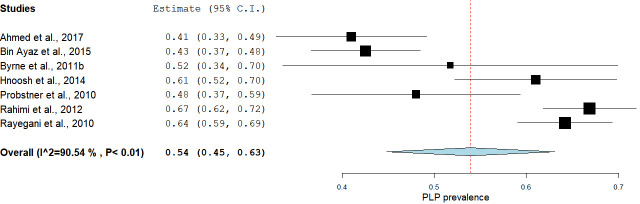
We were concerned by the high statistical heterogeneity in the primary meta-analysis, so we opted to deviate from protocol to conduct two exploratory meta-analyses with studies sub-grouped according to risk of bias score. The first exploratory subgroup analysis, including only the studies that scored low risk of bias overall, estimated prevalence at 63% [95% CI: 58.31–67.90] with moderate statistical heterogeneity [I2 = 44.91 (95% CI: 43.90–45.20)] (Fig 4). The second exploratory subgroup analysis, including only the studies with moderate-high risk of bias, estimated prevalence at 64% [95% CI: 60.23–69.40], but with high statistical heterogeneity [I2 = 96.35% (95% CI: 96.11–98.36)] (Fig 5). The Mann-Whitney U test that served as the sensitivity analysis for the effect of moderate-high risk of bias showed no difference between the estimated prevalence from these two meta-analyses [U = 58.5, p = 0.28].
Fig 4. A subgroup analysis showing the pooled estimated prevalence of PLP in studies with low risk of bias.
Fig 5. A subgroup analysis showing the pooled estimated prevalence of PLP in studies with moderate to high risk of bias.
The subgroup analyses stratified by the developmental status of the countries in which the studies were conducted showed an estimated pooled prevalence of 66.55% [95% CI: 62.02–71.64] in developed countries and 53.98% [95% CI: 44.79–63.05] in developing countries (Figs 6 & 7). The Mann-Whitney U test showed a statistically significant difference between the prevalence estimates of these two meta-analyses [U = 57, p = 0.03].
Fig 6. A subgroup analysis showing the pooled estimated prevalence of PLP in developed countries.
Fig 7. A subgroup analysis showing the pooled estimated prevalence of PLP in developing countries.
Risk factors for phantom limb pain
Twenty-five potential risk factors had been studied in 15 studies representing 4102 participants. Of these, 10 pre-amputation, three peri-operative and eight post-amputation risk factors had data to support their positive association with PLP, and six pre-amputation, four peri-operative and three post-amputation risk factors had not been found to be positively associated with PLP. The risk factors found to be positively associated with PLP and their measures of association are summarised in Table 2. Lower limb amputation was positively associated with PLP (moderate to strong association) in two studies representing a total of 1450 participants [12, 38]. Stump pain was consistently positively associated with PLP (weak to very strong association) in seven studies representing a total of 1254 participants [3, 4, 12, 13, 41, 46, 47]. Phantom sensations were consistently positively associated with PLP (strong to very strong association) in four studies representing a total of 1156 participants [12, 13, 42, 48]. Proximal site of amputation was positively associated with PLP (very strong association) in two studies representing a total of 604 participants [12, 49]. Diabetic cause of amputation was positively associated with PLP (moderate to strong association) in two studies representing a total of 580 participants [5, 12]. Persistent pre-amputation pain was positively associated with PLP in five studies representing a total of 881 participants (weak to very strong association) [3, 5, 9, 46, 50] but was not associated with PLP in two studies representing a total of 625 participants.
Table 2. The summary of the risk factors for PLP and their measures of association with PLP.
| Author | Population | Outcome | Risk factor(s) | Measures of association | Strength of association |
|---|---|---|---|---|---|
| Ahmed et al., 2017 | Cancer patients who had undergone limb amputations | PLP | Post-amputation depression | 3.86 (1.75–8.53)‡ | Strong |
| Pre-amputation pain | 2.83 (1.38–5.76)‡ | Moderate | |||
| Stump pain | 31.2 (8.97–108.50)‡ | Very strong | |||
| Use of prosthesis | 2.83 (1.19–4.76)‡ | Moderate | |||
| Sleep disturbance | 21.43 (8.28–55.43)‡ | Very strong | |||
| Buchanan et al., 1986 | Amputees who were receiving routine prosthetic services | PLP | Age | 0.12 (p<0.01)¥ | Weak |
| Desmond et al., 2010 | Members of the British Limbless Ex-Service Men’s Association | PLP | Stump pain | 11.17 (p<0.01)‡ | Very strong |
| Dijkstra et al., 2002 | Amputees who were receiving routine prosthetic services | PLP | Diabetic cause of amputation | 4 (p<0.001)‡ | Strong |
| Proximal site of amputation | 1.60 (0.038)‡ | Moderate | |||
| Lower limb amputation | 5.60 (p<0.001)‡ | Strong | |||
| Bilateral amputations | 8.20 (p = 0.01)‡ | Strong | |||
| Stump pain | 3.90 (p<0.001)‡ | Strong | |||
| Phantom sensations | 19.50 (p<0.001)‡ | Very strong | |||
| Ephraim et al., 2005 | Amputees who had contacted the Amputee Coalition of America (ACA) between 1998 and 2000 | PLP | Post-amputation depression | 2 (1.3–3.1)‡ | Moderate |
| Lower limb amputation | 2.50 (1.3–4.7)‡ | Moderate | |||
| 2 or more comorbidities | 2.70 (1.3–5.8)‡ | Moderate | |||
| Widow | 2.70 (1.1–6.5)‡ | Moderate | |||
| Gallagher et al., 2001 | Amputees who were attending the Limb Fitting Clinic. | PLP | Proximal site of amputation | 15.65 (p<0.001)‡ | Very strong |
| Traumatic cause of amputation | 14.60 (p<0.002)‡ | Very strong | |||
| Sex (male) | 3.76 (p<0.05)‡ | Strong | |||
| Other medical problems | 5.93 (p<0.02)‡ | Strong | |||
| Lack of pre-amputation counselling | 4.74 (p<0.03)‡ | Strong | |||
| Hanley et al., 2009 | Patients who had undergone upper-limb amputation 6 months or more before recruitment | PLP | Use of prosthesis | 4.23 (p<0.05)¶ | Moderate |
| Hanley et al., 2006 | Patients who had undergone lower limb amputation | PLP | Pre-amputation pain | 0.48 (p<0.01)§ | Weak |
| Stump pain | 0.53 (p<0.0001)§ | Weak | |||
| Kooijman et al., 2000 | Amputees using upper limb prosthesis | PLP | Phantom sensations | 11.30 (p = 0.001)† | Very strong |
| Stump pain | 1.90 (p = 0.015)† | Weak | |||
| Larbig et al., 2019 | Patients who had undergone upper or lower limb amputations | PLP | Pre-amputation depression | 2.05 (p<0.05)§ | Moderate |
| Pre-amputation pain | 4.22 (p<0.01)§ | Moderate | |||
| Stump pain | 3.90 (p<0.01)§ | Moderate | |||
| Noguchi et al., 2019 | Patients who had undergone upper or lower limb amputations | PLP | Diabetic cause of amputation | 2.24 (p = 0.032)‡ | Moderate |
| Pre-amputation pain | 6.36 (p = 0.024)‡ | Strong | |||
| Razmus et al., 2017 | Occupants of the nursing home, and clients of the Public Institute of Orthopaedic Equipment | PLP | Phantom sensations | 4.94 (P<0.05)§ | Strong |
| Richardson et al., 2007 | Patients who had undergone amputation of the lower limb due to peripheral vascular disease. | PLP | Stump pain | 7.03 (1.34–36.82)‡ | Strong |
| Increased ability to move the phantom limb. | 8.31 (1.54–44.79)‡ | Strong | |||
| Praying/hoping | 2.86 (1.68–13.18)‡ | Moderate | |||
| Catastrophizing | 3.28 (1.71–14.91)‡ | Strong | |||
| Passive coping | 4.60 (6.50–25.00)‡ | Strong | |||
| Wartan et al., 1997 | Traumatic amputees | PLP | Phantom sensations | 107.30 (p<0.0001)§ | Strong |
| Yin et al., 2017 | Amputees who underwent limb amputations at a tertiary hospital | PLP | Pre-amputation pain | 10.40 (p = 0.002)‡ | Very strong |
| Post-amputation epidural analgesia | 4.90 (p = 0.008)‡ | Strong |
¥ Point-biserial correlation analysis;
¶ Pearson’s univariate correlation test;
§ Chi-squared;
† Relative risk;
‡ Odds ratio.
The risk factors which were not found to be positively associated with PLP are summarised in Table 3. Sex, age and traumatic cause of amputation were the most commonly assessed of these proposed risk factors. Sex was consistently not associated with PLP in six studies representing a total of 1836 participants [3, 5, 13, 38, 51, 52]. Age was not associated with PLP in three studies representing a total of 1062 adult participants [5, 38, 52] but higher age was positively associated with PLP (weak association) in one study representing a total of 716 adult participants [53]. A traumatic cause of amputation was not associated with PLP in two studies representing a total of 958 participants [5, 38] but was positively associated with PLP (very strong association) in one study representing a total of 104 participants [54]. The meta-analysis of risk factors for PLP could not be conducted because of variations in methods of data collection and analysis across the included studies.
Table 3. The summary of factors not associated with increased risk for PLP and their measures of association with PLP.
| Author | Population | Outcome | Risk factor(s) | Measures of association |
|---|---|---|---|---|
| Ahmed et al., 2017 | Cancer patients who had undergone limb amputations | PLP | Sex | 0.65 (0.31–1.40)‡ |
| smoking | 1.40 (0.71–2.78)‡ | |||
| Regional Anaesthesia | 0.99 (0.68–1.54)‡ | |||
| Post-amputation analgesia | 1.41 (0.94–2.10)‡ | |||
| Perioperative gabapentin | 0.75 (0.76–1.51)‡ | |||
| Radiotherapy | 1.33 (0.66–2.66)‡ | |||
| Dijkstra et al., 2002 | Amputees who were receiving routine prosthetic services | PLP | Sex | — (p = 0.73)‡ |
| Prosthesis use (>8 hours per day) | — (p<0.13)‡ | |||
| Ephraim et al., 2005 | Amputees who had contacted the Amputee Coalition of America (ACA) between 1998 and 2000 | PLP | Sex | 1.4 (0.90–2.20)‡ |
| Age | 1.1 (0.60–1.80)‡ | |||
| Traumatic cause of amputation | 0.9 (0.50–1.70)‡ | |||
| Years since amputation | 1.0 (0.60–1.90)‡ | |||
| Gallagher et al., 2001 | Amputees who were attending the Limb Fitting Clinic. | PLP | Post-amputation support | — (—) |
| Hanley et al., 2009 | Patients who had undergone upper-limb amputation 6 months or more before recruitment | PLP | Age | 3.78 (p = 0.83)¶ |
| Sex | 0.78 (p = 0.99)¶ | |||
| Kooijman et al., 2000 | Amputees using upper limb prosthesis | PLP | Sex | — (p = 0.21)† |
| Amputation of the dominant limb | — (p = 0.59)† | |||
| Pre-amputation pain | — (p = 0.59)† | |||
| Upper limb amputation | — (p = 0.08)† | |||
| Prosthesis use (>8 hours per day) | — (p = 0.06)† | |||
| Noguchi et al., 2019 | Patients who had undergone upper or lower limb amputations | PLP | Sex | 0.78 (p = 0.73)‡ |
| Age | — (p = 0.65)‡ | |||
| Traumatic cause of amputation | 2.941 (p = 0.22)‡ | |||
| Increased hospital-stay | — (p = 0.26)‡ | |||
| Wartan et al., 1997 | Traumatic amputees | PLP | Pre-amputation pain | 10.6 (p<0.30)§ |
¥ Point-biserial correlation analysis;
¶ Pearson’s univariate correlation test;
§ Chi-squared;
† Relative risk;
‡ Odds ratio;—missing figure.
Discussion
According to our knowledge, this is the first systematic review to pool the literature on the prevalence and risk factors for PLP in people with limb amputations. The results of this study estimate that PLP affects 64% of people with amputations. Furthermore, this study identified that lower limb amputation, stump pain, phantom sensations, persistent pre-amputation pain, proximal site of amputation and diabetic cause of amputation are risk factors for PLP.
Phantom limb pain prevalence
The current meta-analysis estimated that 64% of people with amputations report PLP. This estimate suggests that approximately 8169 of 12765 participants in this study reported PLP. Interestingly, dividing studies by risk of bias revealed no difference in estimated prevalence, despite the ‘low risk of bias’ subgroup’s meta-analysis having lower statistical heterogeneity. In addition, the results of the Egger’s regression test indicated that the asymmetry of the funnel plot (S5 File) was not significant (p = 0.64), thus failing to suggest the presence of publication bias. Altogether, these findings suggest that the included studies provide a reasonably stable estimate of the prevalence of PLP in the population of people with amputations. The prevalence of PLP appears to be high, supporting that health professionals should be aware of the risk of this complication and that pragmatic interventions for preventing or alleviating PLP are needed.
The meta-analysis that stratified the studies by country developmental status suggested that the prevalence of PLP was significantly lower in developing countries compared to developed countries [53.98% vs 66.55%; p = 0.03]. This discrepancy is surprising and might be an artefact of selection bias linked either to the lower recruitment success rates (57.9% - 68.4%) seen in most of the included studies conducted in developing countries [3, 34]. The strategy of recruiting participants from amongst patients receiving follow-up medical care may have contributed to underestimation of PLP prevalence if amputees with PLP without continuing medical care were excluded from samples (in developing countries), or overestimation if having PLP made amputees more likely to remain in medical care (in developed countries). This lack of clarity regarding recruitment strategies highlights the need to adapt recruitment strategies specifically to people with amputations in developing countries so that they can be accounted for in future studies.
The current literature suggests the standard of surgical care in developed countries differs significantly from that in developing countries. A study investigating the global burden and distribution of surgery revealed that approximately 80% more surgery-related complications and deaths occur in developing than in developed countries, despite accounting for only 26% of surgical procedures conducted globally [55]. These data may reflect the disparity in the standard of surgical care between developed and developing countries. Many healthcare facilities in developing countries, particularly in rural areas, have poor infrastructure and lack essential surgical equipment and skilled surgeons [56]. Urban areas may have a few skilled surgeons, yet the need for surgical care is typically greater in the rural parts of developing countries. As a result, surgical procedures are often conducted by less trained healthcare professionals under sub-standard conditions. Surgical care in developing countries therefore tends to be substandard than that in developed countries [56].
Another important consideration is that the prevalence estimates could have been influenced by the under-representation of only seven studies conducted in developing countries compared to 32 studies conducted in developed countries. Trauma or combat-related amputations are common in some regions in South America, Middle East, and West and Central Africa [57–59]. However, these regions are underrepresented in the body of studies identified by this review. In fact, we could not find any relevant study conducted in the continent of Africa. This highlights a concerning dearth of scientific research on PLP in these developing regions. Therefore, we recommend that further studies be focused in the burden of PLP in developing countries, specifically.
The included studies had varying risk of bias. However, the lack of statistically significant difference between the prevalence estimates from pooling of the studies with low risk of bias and pooling of the studies with moderate-high risk of bias suggests that the overall risk of bias in included studies had little impact on the prevalence of PLP. Nonetheless, the high risk of bias attributed to most studies for using an ambiguous definition of PLP (e.g pain felt in the limb after amputation) leaves the possibility that participants might have confused residual limb pain and PLP. We suspect that this might have resulted in an overestimation of the prevalence of PLP.
We found it interesting that the pooled prevalence estimate of PLP in this study was relatively high compared to that reported in the literature on people with congenitally absent limbs. The three studies available on people with congenitally absent limbs (not eligible for this review) reported a markedly low PLP prevalence of 0% (out of 27 participants), 5.7% (out of 88 participants) and 7% (out of 57 participants) [6, 13, 60]. Although a robust conclusion cannot be drawn from three small studies, these findings suggest that people with congenitally absent limbs may be less likely to experience PLP than those whose amputations were due to trauma or surgery [54]. Perhaps the peripheral nerves severed during amputation play an important role in the initiation of PLP after amputation [61]. In addition, the absence of pre-operative and peri-operative risk factors for PLP in this group might contribute to the low prevalence.
Risk factors for phantom limb pain
Five studies showed that PLP was more likely to occur in people who reported a history of persistent pre-operative pain than in those who did not report having had persistent limb pain prior to their amputation. One physiological mechanism that has been proposed to explain the link between pre-amputation pain and PLP is central sensitisation—where persistent pre-operative pain contributes to the hyperexcitability of the nervous system and functional changes in the cortical areas involved in the generation of pain [62]. These changes may continue to upregulate peripheral input after limb amputation, thus promoting PLP that shares the characteristics with pre-amputation pain [63]. In fact, over 60% of the patients who experienced persistent pre-amputation pain reported similar characteristics of their PLP [64, 65]. This apparent relationship highlights the importance of addressing limb pain very early in patients who are at high risk of having their limbs amputated. The early management of pre-amputation pain using effective treatments such as pre-operative epidural analgesia (e.g. ketamine) and mirror therapy may reduce risk of developing PLP and improve physical and psychological outcomes often related to delayed or ineffective management of PLP [46, 66].
Two studies showed that PLP was more likely to occur after lower limb amputation than after upper limb amputation [38, 51]. The authors proposed that the use of a cosmetic prosthetic leg, rather than a prosthesis that provided sensory input was a likely contributor to pain in people with lower limb amputations since 70%-78.8% of cosmetic prosthetic leg users had PLP. Lack of proprioceptive feedback during the use of a prosthetic leg has been linked to poor motor control, possibly leading to stump irritation that may trigger PLP [2, 67]. This proposed link is partially supported by seven studies in this review which suggested that PLP was more likely to occur in people with stump pain than in those without stump pain [3, 4, 12, 13, 41, 44, 47]. Interestingly, Dietrich and colleagues investigated the effects of a leg prosthesis with somatosensory feedback on pain and lower limb function [68]. In that study, participants used prosthetic legs with pressure sensors that provided comfortable electrical feedback to the patient’s thigh whenever the prosthetic foot touched the ground. At the end of two weeks of training, the participants had improved function of the lower limb and reduced severity and frequency of PLP. Further, the patients reported greater satisfaction, longer walking distances and improved dynamic stability than prior to the training. These results suggest that people with lower limb amputations might benefit more from using a prosthetic leg with somatosensory feedback than from using a cosmetic prosthesis. However, the mechanisms by which prosthetic legs with somatosensory feedback reduce PLP are not clear. Therefore, it would be interesting to investigate the mechanisms by which somatosensory feedback from a prosthetic leg might influence PLP.
Four studies showed that PLP was more likely to occur in amputees with non-painful phantom sensations than in those without non-painful phantom sensations [13, 42, 48]. In these studies, 70%-100% of amputees with phantom sensations also had PLP. The co-occurrence of these post-amputation sensations suggest that they may share neural mechanisms with PLP [48]. An fMRI study by Andoh et al showed that inducing non-painful phantom sensations in people with amputations activated the somatosensory and premotor cortices contralateral to the amputated limb [69]. The activation of similar cortical areas has been recorded in patients with PLP upon induction of their PLP [70–74]. The similarities in cortical activation patterns might explain a link between PLP and non-painful phantom sensations.
Two studies showed that PLP was more likely to occur in people with proximal amputations than in those with distal amputations [12, 54]. These findings line up with a narrative review that reported an increase in the incidence of PLP with more proximal amputations [75]. Proximal amputations are associated with an increased risk of failure of wound healing, which may result in infection or stump pain [76]. However, the reasons why proximal amputations should be more likely to lead to PLP than distal amputations are not clear [77].
Another interesting finding was that not having pre-amputation counselling was positively associated with PLP (strong association) in a study representing a total of 104 participants [54]. This suggests that patients who receive counselling prior to their amputation maybe less likely to report PLP compared to those who do not receive counselling. We could not find any relevant study to explain this strong association. However, Gallagher et al [54] suggest that pre-amputation counselling may reduce the risk of developing PLP by addressing depression and anxiety prior to limb amputation [78]. Another consideration is that pre-amputation counselling aimed at managing patients’ expectations about pain post-operatively (e.g. prognosis) and equipping them with adaptive coping strategies may reduce the risk of PLP by preventing the onset of post-amputation depression that is sometimes triggered by the feeling of helplessness from the overwhelming new reality of life after limb amputation [38]. No other study has specifically identified not having pre-operative counselling as a predictor for PLP after limb amputation. Therefore, further studies are required to build on the existing literature.
Limitations
The sample in this systematic review was skewed towards males, in that 9814 (77.04%) of the 12738 participants were male. Therefore, the results might not hold for females. We could not perform a subgroup analysis by sex because we did not have individual patient data, nor was analysis by sex an objective identified in the protocol. However, the data on risk factors provide no support for sex influencing the likelihood of PLP after amputation. It was not possible to conduct a meta-analysis on the risk factors for PLP because the included studies used varying methodological approaches and measures of association. None of the included studies used an outcome measure that has been validated for assessing PLP. In fact, we are not aware of any instrument that has been validated for assessing PLP. Such a standardised tool for assessing PLP would be useful to provide us with reliable data. Most studies in this review had moderate-high risk of bias. There is a clear need for high-quality studies to raise the credibility of future meta-analyses. Finally, the search strategy for this study was designed specifically to identify prevalence studies. Therefore, although we did conduct an exploratory search for additional studies of risk factors for PLP, there is a possibility that we could have missed some studies that investigated risk factors for PLP if they did not also estimate PLP prevalence. In consideration of this possibility, the review of risk factors was classified as an exploratory analysis. Thirteen out of 15 included studies determined association between identified risk factors and PLP using a retrospective cross-sectional study design. This study design (compared to a cohort design) is prone to recall bias, resulting from the patient’s inability to clearly recall their exposure to a risk factor prior to developing PLP. Further studies using a cohort design are necessary to provide robust data on risk factors for PLP. It is important to note that studies conducted in developing countries are underrepresented in our meta-analyses. Therefore, the results on PLP prevalence in developing countries should be interpreted with caution. The results of this systematic review were derived from studies conducted mostly in Europe, North America and Asia. To the best of our knowledge, no study has been conducted in Africa, and research in this area is necessary to inform us about the prevalence and risk factors for PLP in the African population.
Conclusions
This systematic review and meta-analysis estimates that six of every 10 people with an amputation report PLP–a high and important prevalence of PLP. Health care professionals ought to be aware of the high rates of PLP and implement strategies to reduce PLP by addressing known risk factors, specifically those identified by the current study. Stump pain and post-amputation depression are all known and modifiable risk factors that are consistently positively associated with PLP. Awareness of these risk factors may motivate health care professionals to address them early in treatment to prevent the onset of PLP in people with amputations.
Supporting information
(DOC)
(DOCX)
(DOCX)
(DOCX)
(JPG)
Acknowledgments
The authors thank Mrs Mary Shelton (Health Sciences reference librarian, University of Cape Town) for assisting with the development of the search strategy.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
KML URC: 101 University of Cape Town www.uct.ac.za The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Ehde D.M., et al. , Chronic phantom sensations, phantom pain, residual limb pain, and other regional pain after lower limb amputation. Archives of physical medicine and rehabilitation, 2000. 81(8): p. 1039–1044. 10.1053/apmr.2000.7583 [DOI] [PubMed] [Google Scholar]
- 2.Morgan S.J., et al. , Cross-Sectional Assessment of Factors Related to Pain Intensity and Pain Interference in Lower Limb Prosthesis Users. Arch Phys Med Rehabil, 2017. 98(1): p. 105–113. 10.1016/j.apmr.2016.09.118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahmed A., et al. , Prevalence of phantom limb pain, stump pain, and phantom limb sensation among the amputated cancer patients in India: A prospective, observational study. Indian journal of palliative care, 2017. 23(1): p. 24 10.4103/0973-1075.197944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Desmond D.M. and MacLachlan M., Prevalence and characteristics of phantom limb pain and residual limb pain in the long term after upper limb amputation. International Journal of Rehabilitation Research, 2010. 33(3): p. 279–282. 10.1097/MRR.0b013e328336388d [DOI] [PubMed] [Google Scholar]
- 5.Noguchi S., et al. , Factors affecting phantom limb pain in patients undergoing amputation: retrospective study. Journal of anesthesia, 2019. 33(2): p. 216–220. 10.1007/s00540-018-2599-0 [DOI] [PubMed] [Google Scholar]
- 6.Garcia D., et al. , Phantom pain in congenital amputees: Myth or reality? Annals of Physical and Rehabilitation Medicine, 2018. 61: p. e118. [Google Scholar]
- 7.Neil M., Pain after amputation. BJA Education, 2015. 16(3): p. 107–112. [Google Scholar]
- 8.Clark R.L., et al. , Phantom limb pain after amputation in diabetic patients does not differ from that after amputation in nondiabetic patients. Pain, 2013. 154(5): p. 729–32. 10.1016/j.pain.2013.01.009 [DOI] [PubMed] [Google Scholar]
- 9.Yin Y., et al. , The pre-amputation pain and the postoperative deafferentation are the risk factors of phantom limb pain: a clinical survey in a sample of Chinese population. BMC anesthesiology, 2017. 17(1): p. 69 10.1186/s12871-017-0359-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maimela E., et al. , The prevalence and determinants of chronic non-communicable disease risk factors amongst adults in the Dikgale health demographic and surveillance system (HDSS) site, Limpopo Province of South Africa. PLoS One, 2016. 11(2): p. e0147926 10.1371/journal.pone.0147926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Montoya P., et al. , The relationship of phantom limb pain to other phantom limb phenomena in upper extremity amputees. Pain, 1997. 72(1–2): p. 87–93. 10.1016/s0304-3959(97)00004-3 [DOI] [PubMed] [Google Scholar]
- 12.Dijkstra P.U., et al. , Phantom Pain and Risk Factors: A Multivariate Analysis. Journal of Pain and Symptom Management, 2002. 24(6): p. 578–585. 10.1016/s0885-3924(02)00538-9 [DOI] [PubMed] [Google Scholar]
- 13.Kooijman C.M., et al. , Phantom pain and phantom sensations in upper limb amputees: an epidemiological study. Pain, 2000. 87(1): p. 33–41. 10.1016/s0304-3959(00)00264-5 [DOI] [PubMed] [Google Scholar]
- 14.Ventham N., Heyburn P., and Huston N., Prevalence of phantom limb pain in diabetic and non-diabetic leg amputees: a cross-sectional observational survey. European Journal of Pain Supplements, 2010. 4(1): p. 106–107. [Google Scholar]
- 15.Limakatso K., et al. , The prevalence of phantom limb pain and associated risk factors in people with amputations: a systematic review protocol. Systematic reviews, 2019. 8(1): p. 17–17. 10.1186/s13643-018-0938-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bin Ayaz S., et al. , Frequency and the related socio-demographic and clinical factors of phantom limb pain in traumatic amputees presenting at a tertiary care rehabilitation setup. Pakistan Armed Forces Medical Journal, 2015(6): p. 782–788. [Google Scholar]
- 17.Murray C.J. and Lopez A.D., Measuring the global burden of disease. New England Journal of Medicine, 2013. 369(5): p. 448–457. 10.1056/NEJMra1201534 [DOI] [PubMed] [Google Scholar]
- 18.WESP. Data sources, country classifications and aggregation methodology. (2014, January 25). 2018. [cited (2014, January 25); Available from: Retrieved from http://www.un.org/en/development/desa/policy/wesp/wesp_current/2014wesp_country_classification.pdf. [Google Scholar]
- 19.Moher D., et al. , Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews, 2015. 4(1): p. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rathvon D., EndNote X8—Citation Manager—What's New? 2017. [Google Scholar]
- 21.Hoy D., et al. , Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. Journal of clinical epidemiology, 2012. 65(9): p. 934–939. 10.1016/j.jclinepi.2011.11.014 [DOI] [PubMed] [Google Scholar]
- 22.Cohen J., A coefficient of agreement for nominal scales. Educational and psychological measurement, 1960. 20(1): p. 37–46. [Google Scholar]
- 23.Gagnier J.J., et al. , Investigating clinical heterogeneity in systematic reviews: a methodologic review of guidance in the literature. BMC medical research methodology, 2012. 12(1): p. 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Higgins J.P., et al. , Measuring inconsistency in meta-analyses. BMJ: British Medical Journal, 2003. 327(7414): p. 557 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Egger M., et al. , Bias in meta-analysis detected by a simple, graphical test. Bmj, 1997. 315(7109): p. 629–634. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rosenthal J.A., Qualitative descriptors of strength of association and effect size. Journal of social service Research, 1996. 21(4): p. 37–59. [Google Scholar]
- 27.Nicolich M.J. and Gamble J.F., What is the minimum risk that can be estimated from an epidemiology Study. Advanced Topics in Environmental Health and Air Pollution Case Studies, 2011: p. 3–26. [Google Scholar]
- 28.Healey J.F., Statistics: A tool for social research. 2014: Cengage Learning. [Google Scholar]
- 29.Allen M., The SAGE encyclopedia of communication research methods. 2017: SAGE Publications. [Google Scholar]
- 30.Frankfort-Nachmias C. and Leon-Guerrero A., Social statistics for a diverse society. 2017: Sage Publications. [Google Scholar]
- 31.Byrne K.P., Survey of phantom limb pain, phantom sensation and stump pain in Cambodian and New Zealand amputees. Pain Med, 2011. 12(5): p. 794–8. 10.1111/j.1526-4637.2011.01105.x [DOI] [PubMed] [Google Scholar]
- 32.Reiber G.E., et al. , Servicemembers and veterans with major traumatic limb loss from Vietnam war and OIF/OEF conflicts: Survey methods, participants, and summary findings. Journal of Rehabilitation Research & Development, 2010. 47(3): p. 275–297. [DOI] [PubMed] [Google Scholar]
- 33.Aldington D., et al. , A survey of post-amputation pains in serving military personnel. J R Army Med Corps, 2014. 160(1): p. 38–41. 10.1136/jramc-2013-000069 [DOI] [PubMed] [Google Scholar]
- 34.Rahimi A., et al. , Pain and health-related quality of life in war veterans with bilateral lower limb amputations. Trauma Monthly, 2012. 17(2): p. 282–286. 10.5812/traumamon.5135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hnoosh A.H., Phantom Limb and pain after traumatic lower extremity amputation. Journal of the Faculty of Medicine, 2014. 56(1): p. 57–61. [Google Scholar]
- 36.Rayegani S.M., et al. , Phantom pain, phantom sensation, and spine pain in bilateral lower limb amputees: Results of a national survey of Iraq-Iran war victims' health status. Journal of Prosthetics and Orthotics, 2010. 22(3): p. 162–165. [Google Scholar]
- 37.Bekrater-Bodmann R., et al. , Post-amputation pain is associated with the recall of an impaired body representation in dreams-results from a nation-wide survey on limb amputees. PLoS One, 2015. 10(3): p. e0119552 10.1371/journal.pone.0119552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ephraim P.L., et al. , Phantom pain, residual limb pain, and back pain in amputees: results of a national survey. Archives of Physical Medicine & Rehabilitation, 2005. 86(10): p. 1910–1919. [DOI] [PubMed] [Google Scholar]
- 39.Kern U., et al. , [Prevalence and risk factors of phantom limb pain and phantom limb sensations in Germany. A nationwide field survey ] Schmerz, 2009. 23(5): p. 479–88. 10.1007/s00482-009-0786-5 [DOI] [PubMed] [Google Scholar]
- 40.Datta D., Selvarajah K., and Davey N., Functional outcome of patients with proximal upper limb deficiency—acquired and congenital. Clinical Rehabilitation, 2004. 18(2): p. 172–177. 10.1191/0269215504cr716oa [DOI] [PubMed] [Google Scholar]
- 41.Richardson C., et al. , Incidence of phantom phenomena including phantom limb pain 6 months after major lower limb amputation in patients with peripheral vascular disease. The Clinical journal of pain, 2006. 22(4): p. 353–358. 10.1097/01.ajp.0000177793.01415.bd [DOI] [PubMed] [Google Scholar]
- 42.Wartan S.W., et al. , Phantom pain and sensation among British veteran amputees. Br J Anaesth, 1997. 78(6): p. 652–9. 10.1093/bja/78.6.652 [DOI] [PubMed] [Google Scholar]
- 43.Rafferty M., et al. , Cross-sectional study of alteration of phantom limb pain with visceral stimulation in military personnel with amputation. J Rehabil Res Dev, 2015. 52(4): p. 441–8. 10.1682/JRRD.2014.04.0114 [DOI] [PubMed] [Google Scholar]
- 44.Hanley M.A., et al. , Self-reported treatments used for lower-limb phantom pain: descriptive findings. Archives of Physical Medicine & Rehabilitation, 2006. 87(2): p. 270–311. [DOI] [PubMed] [Google Scholar]
- 45.Ketz A.K., The experience of phantom limb pain in patients with combat-related traumatic amputations. Archives of Physical Medicine & Rehabilitation, 2008. 89(6): p. 1127–1132. [DOI] [PubMed] [Google Scholar]
- 46.Hanley M.A., et al. , Preamputation Pain and Acute Pain Predict Chronic Pain After Lower Extremity Amputation. The Journal of Pain, 2007. 8(2): p. 102–109. 10.1016/j.jpain.2006.06.004 [DOI] [PubMed] [Google Scholar]
- 47.Larbig W., et al. , Pre-and postoperative predictors of phantom limb pain. Neuroscience letters, 2019. 702: p. 44–50. 10.1016/j.neulet.2018.11.044 [DOI] [PubMed] [Google Scholar]
- 48.Razmus M., Daniluk B., and Markiewicz P., Phantom limb phenomenon as an example of body image distortion. Current Problems of Psychiatry, 2017. 18(2): p. 153–159. [Google Scholar]
- 49.Gallagher S., et al. , Hand-mouth coordination, congenital absence of limb, and evidence for innate body schemas. Brain Cogn, 1998. 38(1): p. 53–65. 10.1006/brcg.1998.1020 [DOI] [PubMed] [Google Scholar]
- 50.Larbig W., et al. , Evidence for a change in neural processing in phantom limb pain patients. Pain, 1996. 67(2–3): p. 275–283. 10.1016/0304-3959(96)03107-7 [DOI] [PubMed] [Google Scholar]
- 51.Dijkstra P.U., 'Re: Phantom limb pain': Commentary reply. Journal of Pain and Symptom Management, 2006. 32(2): p. 103–103. 10.1016/j.jpainsymman.2006.06.002 [DOI] [PubMed] [Google Scholar]
- 52.Hanley M.A., et al. , Chronic Pain Associated with Upper-Limb Loss. American Journal of Physical Medicine & Rehabilitation, 2009. 88(9): p. 742–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Buchanan D.C. and Mandel A.R., The prevalence of phantom limb experience in amputees. Rehabilitation Psychology, 1986. 31(3): p. 183. [Google Scholar]
- 54.Gallagher P., Allen D., and MacLachlan M., Phantom limb pain and residual limb pain following lower limb amputation: a descriptive analysis. Disability & Rehabilitation, 2001. 23(12): p. 522–530. [DOI] [PubMed] [Google Scholar]
- 55.Weiser T.G., et al. , An estimation of the global volume of surgery: a modelling strategy based on available data. The Lancet, 2008. 372(9633): p. 139–144. [DOI] [PubMed] [Google Scholar]
- 56.Akenroye O.O., Adebona O.T., and Akenroye A.T., Surgical Care in the Developing World-Strategies and Framework for Improvement. Journal of public health in Africa, 2013. 4(2): p. e20–e20. 10.4081/jphia.2013.e20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tintle S.M., et al. , Lower extremity combat-related amputations. Journal of Surgical Orthopaedic Advances, 2010. 19(1): p. 35 [PubMed] [Google Scholar]
- 58.Nwosu C., et al. , Major limb amputations in a tertiary hospital in North Western Nigeria. African Health Sciences, 2017. 17(2): p. 508–512. 10.4314/ahs.v17i2.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Martínez-Rondanelli A., et al. , Initial treatment of combat related limb injuries in Colombia. Revista de la Universidad Industrial de Santander. Salud, 2016. 48(3): p. 295–300. [Google Scholar]
- 60.Boonstra A.M., et al. , Children with congenital deficiencies or acquired amputations of the lower limbs: functional aspects. Prosthet Orthot Int, 2000. 24(1): p. 19–27. 10.1080/03093640008726518 [DOI] [PubMed] [Google Scholar]
- 61.Vaso A., et al. , Peripheral nervous system origin of phantom limb pain. PAIN®, 2014. 155(7): p. 1384–1391. [DOI] [PubMed] [Google Scholar]
- 62.Lee M.C., et al. , Identifying brain activity specifically related to the maintenance and perceptual consequence of central sensitization in humans. J Neurosci, 2008. 28(45): p. 11642–9. 10.1523/JNEUROSCI.2638-08.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rathmell J.P., M.D. and Kehlet H., M.D., Ph.D., Do We Have the Tools to Prevent Phantom Limb Pain? Anesthesiology: The Journal of the American Society of Anesthesiologists, 2011. 114(5): p. 1021–1024. [DOI] [PubMed] [Google Scholar]
- 64.Jensen T.S., et al. , Immediate and long-term phantom limb pain in amputees: incidence, clinical characteristics and relationship to pre-amputation limb pain. Pain, 1985. 21(3): p. 267–278. 10.1016/0304-3959(85)90090-9 [DOI] [PubMed] [Google Scholar]
- 65.Katz J. and Melzack R., Pain 'memories' in phantom limbs: Review and clinical observations. Pain, 1990. 43(3): p. 319–336. 10.1016/0304-3959(90)90029-d [DOI] [PubMed] [Google Scholar]
- 66.Hanley M.A., et al. , Psychosocial predictors of long-term adjustment to lower-limb amputation and phantom limb pain. Disability & Rehabilitation, 2004. 26(14/15): p. 882–893. [DOI] [PubMed] [Google Scholar]
- 67.Page D.M., et al. , Motor Control and Sensory Feedback Enhance Prosthesis Embodiment and Reduce Phantom Pain After Long-Term Hand Amputation. Frontiers in Human Neuroscience, 2018. 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dietrich C., et al. , Leg Prosthesis With Somatosensory Feedback Reduces Phantom Limb Pain and Increases Functionality. Frontiers in Neurology, 2018. 9(270). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Andoh J., et al. , Neural correlates of evoked phantom limb sensations. Biological Psychology, 2017. 126: p. 89–97. 10.1016/j.biopsycho.2017.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lotze M., et al. , Activation of cortical and cerebellar motor areas during executed and imagined hand movements: an fMRI study. Journal of cognitive neuroscience, 1999. 11(5): p. 491–501. 10.1162/089892999563553 [DOI] [PubMed] [Google Scholar]
- 71.Flor H., Nikolajsen L., and Jensen T.S., Phantom limb pain: a case of maladaptive CNS plasticity? Nature Reviews Neuroscience, 2006. 7(11): p. 873 10.1038/nrn1991 [DOI] [PubMed] [Google Scholar]
- 72.Lotze M., et al. , Phantom movements and pain An fMRI study in upper limb amputees. Brain, 2001. 124(11): p. 2268–2277. [DOI] [PubMed] [Google Scholar]
- 73.Flor H. and Elbert T., Phantom-limb pain as a perceptual correlate of cortical reorganization following arm amputation. Nature, 1995. 375(6531): p. 482 10.1038/375482a0 [DOI] [PubMed] [Google Scholar]
- 74.Karl A., et al. , Reorganization of motor and somatosensory cortex in upper extremity amputees with phantom limb pain. Journal of Neuroscience, 2001. 21(10): p. 3609–3618. 10.1523/JNEUROSCI.21-10-03609.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Manchikanti L. and Singh V., Managing phantom pain. Pain Physician, 2004. 7(3): p. 365–375. [PubMed] [Google Scholar]
- 76.Stone P.A., et al. , Factors affecting perioperative mortality and wound-related complications following major lower extremity amputations. Annals of vascular surgery, 2006. 20(2): p. 209–216. 10.1007/s10016-006-9009-z [DOI] [PubMed] [Google Scholar]
- 77.Kelle B., et al. , Association between phantom limb complex and the level of amputation in lower limb amputee. Acta Orthop Traumatol Turc, 2017. 51(2): p. 142–145. 10.1016/j.aott.2017.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Aragão J.A., et al. , Anxiety and depression in patients with peripheral arterial disease admitted to a tertiary hospital. Jornal Vascular Brasileiro, 2019. 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOCX)
(DOCX)
(DOCX)
(JPG)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.