Abstract
Depression in the postpartum period impacts approximately 13–26% of the general population. This number can be much higher for rural veteran women who face additional barriers to accessing specialized mental health services due to isolation and cultural factors. This study reports on a program evaluation of MomMoodBooster, a coach-supported internet-delivered CBT program for the treatment of maternal depression in veteran women. Repeated measures ANOVA, run with this sample of 326 women, demonstrated an overall positive effect size across outcome measures and engagement with no differences found between rural women and their urban counterparts. Some differences between urban and rural participants were found in total and average time spent with coaches as well as ratings of coach helpfulness, possibly indicating some cultural differences between coaches and rural women that need to be addressed. These results and the results of earlier trials suggest that MomMoodBooster can be a valid and efficacious option for reaching under-served veteran populations with specialized postpartum mental health support and is as effective with rural women as with urban women
Keywords: Postpartum, Depression, Rural, Veteran, Telehealth
Introduction
In the general population, 10–15% of women will develop depression in the perinatal period (Ashford et al., 2016; Thomas et al., 2018). Among active duty and veteran women, the prevalence may be higher. For example, Klaman and Turner (2016) found that 16–32% of veteran women in the antenatal period and 19% in the postpartum period experience depression. Moreover, Appolomio and Fingerhut (2008) reported that 19.5% active duty, exposed to combat, first-time mothers experience postpartum depression. Finally, Schachman and Lindsey (2013) found that 50.7% of mothers (enlisted and civilian sample) with deployed partners experience postpartum depression.
In the general population, risk factors for developing postpartum depression are well known. Military mothers face additional stressors such as the increased isolation of living on base, separation from deployed spouses, comorbid diagnoses of post-traumatic stress disorder (PTSD) (Nguyen et al., 2013), frequent relocations, working longer into pregnancy, less reported support (Klaman & Turner, 2016), and increased incidence of sexual assault and sexual harassment (Kintzle et al., 2015). Although much of the literature addressing women’s exposure to trauma and comorbid diagnoses are active military samples, it is reasonable to assume that the impact of these traumatic experiences does not end when military commitment ends and therefore also impacts the experiences of veteran mothers.
The consequences of postpartum depression (PPD) to both mother and child have prompted both the United Kingdom’s National Institute for Health and Care Excellence (NICE, 2020) and the U.S. National Research Council and Institute of Medicine (NRCIM, 2009) to recommend prompt intervention for perinatal depression (PND). However, women face many barriers to seeking and/or receiving treatment and only a small percentage (33–42%) of women experiencing depression in the perinatal period seek assistance (Flynn et al., 2006; Henshaw et al., 2013; Smith et al., 2008). In addition, healthcare providers have trouble recognizing PND and PPD (O’Mahen & Flynn, 2008), which results in low screening and low diagnosis rates (Ashford et al., 2016). The barriers of greatest relevance to this paper are long wait times for face-to-face services, particularly specialized services, the supermom myth and stigma (Lee et al., 2016), and geographical-based barriers (Andrilla et al., 2018).
Rural veteran mothers face additional barriers. The Veterans Health Administration (VHA) Office of Rural Health (ORH) reports that approximately 25% of veterans live in rural communities (Veterans Administration, 2020). When comparing samples of veterans with diagnosed depression, anxiety or PTSD, rural veterans are less likely than their urban counterparts to receive any mental health treatment (Teich et al., 2017), face longer wait times between diagnosis and first appointments, and are less likely to receive specialty mental health care (Cully et al., 2010). In general, rural areas are underserved by mental health professionals (Riding-Malon & Werth, 2014), rural veterans have less access to care, are more affected by distance barriers, and have lower health-related quality of life (Cully et al., 2010; Weeks et al., 2008). Unfortunately, more specific information about the unique experiences of women veterans in the perinatal period are not delineated in the rural veteran mental health literature.
Cultural factors related to military experience and rural values may impact a veteran’s willingness to access mental health treatment. For example, research on suicide and help-seeking suggests that agrarian values and stigma contribute to lower help-seeking and initiating mental health services in rural samples (Judd et al., 2006; McCarthy et al., 2012). Other investigators argue that rural values of independence and conformity to social norms contribute to lower levels of acceptance of psychotherapy (Fox et al., 1995; Rost et al., 1993). More work is needed to understand the specific cultural barriers experienced by rural veteran women in the postpartum period.
Given these barriers to diagnosis and treatment, one possibility to increase access is internet delivered therapies (iTx). Internet-based treatments for perinatal depression have been validated as efficacious, resulting in moderate-to-large effect sizes (Andersson & Cuijpers, 2009; Andrews et al., 2010; Ashford et al., 2016; Milgrom et al., 2016; Nair et al., 2018) and are acceptable for the general population (Ashford et al., 2016; Lee et al., 2016). Additionally, women are more likely to report sensitive information over the internet (Le et al., 2009) because this mode of treatment delivery offers anonymity (Lavender et al., 2016) and flexibility to adapt to specific cultural and identity considerations (Lee et al., 2016). The literature in support of internet-based interventions has resulted in the Canadian Network for Mood and Anxiety Treatments (Parikh et al., 2009) and the United Kingdom’s Improving Access to Psychological Treatment program (Clark, 2011) recommending web-based interventions as second-line treatments for perinatal depression. iTx may be a viable option for a stepped-care approach (van Ballegooijen et al., 2014) to the treatment of PND and a promising option for reaching rural veteran women who would otherwise not have access to specialized care.
One problem with internet interventions, however, is that adherence can be poor and early dropout rates can be quite significant. van Ballegooijen et al.’s (2014) meta-analysis of adherence to iCBT interventions concluded that 65.1% of those starting supported iCBT completed 100% of the treatment and that adherence and clinical effect were similar between supported iCBT and face-to-face therapies. Additionally, there appears to be a dose–response effect with iTx such that engaging in more sessions correlates with better outcomes. No studies have compared outcomes, attrition, and uptake between urban and rural cohorts. More information is needed in order to understand what aspects of iTx promote initiation, retention and completion for specific populations (Renton et al., 2014).
This report provides an evaluation of programmatic engagement and mental health outcomes for veteran women participating in the MomMoodBooster program (Danaher et al., 2013; Milgrom et al., 2016), an empirically validated iTx for postpartum depression. More specifically, this paper reports on a program evaluation comparing urban veteran women to their rural counterparts using pre-post measures of depression, behavioral activation, and automatic thoughts. The goal was to determine if MomMoodBooster for veteran women, a six session, coach-supported, CBT-based, iTx delivered to veteran women across the United States is a promising option for treatment of PPD in the rural veteran population.
Methods
Participants
Veteran women with a confirmed live birth in their VA medical record between March 2015 and August 2019 were mailed recruitment letters and then contacted by phone to screen for interest and eligibility. To be eligible for inclusion women had to be between the ages of 18 and 50 and be within 18 months of the birth of their baby with access to phone and internet. Screening consisted of the Patient Health Questionnaire-9 (PHQ-9; Kroenke et al., 2001) using the recommended cut-point of 10 for inclusion (Gilbody et al., 2007). The PHQ-9 has been validated for screening in the perinatal (Sidebottom et al., 2012) and military (Searle et al., 2019) populations. Women scoring 10 or greater on the nine-item PHQ-9 were then screened for major depression, mania, hypomania, and psychosis using the respective subscales from the Mini International Neuropsychiatric Interview (M.I.N.I. 5.0.0; Sheehan et al., 1998). Women with a history of past but not current hypomanic episodes were included. Women could be in concurrent psychotherapy or be using psychotropic medications.
Exclusion criteria
Women reporting current suicidality as indicated by a 2 (“More than half the days”) or 3 (“Nearly every day”) on item 9 of the PHQ-9, “Thoughts that you would be better off dead, or of hurting yourself in some way,” (Kroenke et al., 2001) were excluded after risk assessment and safety planning. Individuals with a history of current or previous manic episodes, current hypomanic episodes, or a presence of psychotic symptoms were excluded and encouraged to reach out to mental health providers at their local VA. Currently pregnant women were excluded.
Procedure
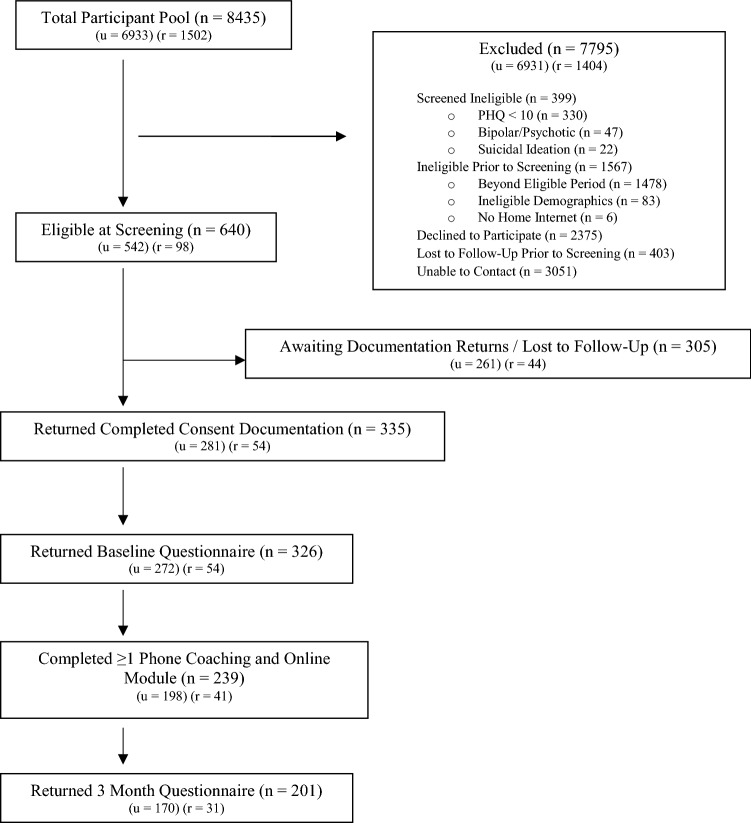
Following recruitment letters, women were contacted by phone to discuss interest and enrollment procedures. Those eligible after screening were mailed a consent and baseline packet. Participants with returned baseline questionnaires were added to a waitlist for the first available coach. See Fig. 1 for participant flow through the program. Coaches contacted participants for a welcome call and then six scheduled coaching calls. Participants were reminded of their scheduled times with coaches via text reminders, which most participants consented to receive. Participants completed questionnaires at baseline and 3 months post-baseline. For each time point participants received $25 for returned questionnaires. Ethics approval was obtained from the University of Iowa Institutional Review Board, and all participants provided informed consent.
Fig. 1.
Flowchart of participants. Note u = urban, r = rural
Measures
Participant demographics
Baseline questions included age, date of delivery, baby gender, parity, marital status, ethnicity, education, family income, occupation, amount of previous counseling, and length of time on anti-depressant medication.
Primary outcomes
Behavioral activation for depression
The Behavioral Activation for Depression Scale (BADS; Kanter et al., 2007) is a 25-item self-report measure that consists of a total score, as well as four subscales: Activation, Avoidance/Rumination, Work/School Impairment, and Social Impairment. Behavioral activation is considered an essential component of treatment of depression (Fuhr et al., 2016). Standalone behavioral activation is a validated treatment for depression with two meta-analyses demonstrating large and significant effect sizes (Cuijpers et al., 2007; Mazzucchelli et al., 2009). The reliability of the BADS-Total for this sample at baseline and follow-up were α = 0.850 and α = 0.918, respectively.
Inventory of depression and anxiety symptoms II
The Inventory of Depression and Anxiety Symptoms II (IDAS-II; Watson et al., 2008, 2012) is a multi-scale measure of the core symptoms of depression and anxiety. The General Depression scale, a 20-item scale meant to capture the full range of diagnostic criteria for depression, has been validated for use with postpartum women (Watson et al., 2007). In this sample, the reliability of IDAS General Depression was α = 0.860 and α = 0.923 at baseline and follow-up, respectively.
Automatic Thoughts Questionnaire
The Automatic Thoughts Questionnaire (ATQ; Hollon & Kendall, 1980) is a 15-item self-report measure developed to capture the severity of automatic thoughts in depressed individuals (Netemeyer et al., 2002). The 15-item short version of the ATQ has been validated as a predictor of negative affect, such as self-esteem and maladjusted thinking patterns (Netemeyer et al., 2002). The reliability of the ATQ for this sample was α = 0.920 at baseline and α = 0.945 at follow-up.
Program and coach ratings
A four-point scale on the follow-up questionnaire asked participants to rate the program and the coach using the following anchors: (1) not at all helpful, (2) somewhat helpful, (3) moderately helpful, and (4) very helpful. Open-ended responses included helpfulness of program and coach, and improvements that could be made to the program and coaching.
Intervention
MomMoodBooster is a secure, web-based, six-module, coach-supported, interactive intervention tailored for women experiencing postpartum depression (Danaher et al., 2012, 2013). Six sequential modules guide women through Cognitive Behavioral Therapy (CBT) content tailored to address the unique experiences of the postpartum period. Session titles include: (1) Getting Started, (2) Tracking Mood, (3) Pleasant Activities, (4) Managing Your Negative Thoughts, (5) Increasing Your Positive Thoughts, and (6) Planning for the Future. Participants engage in self-paced sessions with each successive module opening on a weekly basis.
Personal coaches support participants as they moved through sessions. With one exception, coaches were advanced graduate students in clinical and counseling psychology programs who received supervision on a regular basis. The remaining coach was a post-doctoral Ph.D. with 2 years’ experience working with the MomMoodBooster program. Length of experience working with MomMoodBooster participants ranged from several months to 4 years. The number of participants per coach ranged from 3 to 144 (median = 22).
The coach is designed to be a non-therapeutic point of personal contact, supporting the participants, encouraging program engagement, and clarifying content and use of the program. Coaching was approached first using an accountability model and then later using an alliance-based model where coaches engaged in an unstructured conversation focused on creating a positive supportive relationship with the participant. Coaching calls occurred weekly and lasted approximately 10–15 min in length. At sessions three and five, coaches assessed current mood using the PHQ-9 (Kroenke et al., 2001). In this context, the PHQ-9 was used for safety purposes to detect suicidal ideation and significant deterioration. It was not obtained at follow-up and was not an outcome measure.
Statistical analysis
SPSS, version 25, was used for all analyses and tests of significance between urban and rural participants. All tests of significance were two-tailed, with significance set to 0.05. Item-level missing data were imputed using mean imputation for scales with fewer than 20% of items missing. For the IDAS-GD, ATQ, and BADS, maximum imputations for missing items were four, three, and four items on these measures, respectively.
Analyses were conducted using both intention-to-treat (ITT) and completer data. For ITT analyses, penalized imputation was used in the absence of follow-up data, following the conservative assumption that depressive symptoms remained the same. Results are reported for both ITT and completers analyses.
Primary outcomes included depressive symptoms, behavioral activation, and automatic thoughts. Given observed strong correlations among the subscales of the BADS measure, the total score was used in primary outcome analyses. Repeated-measures ANOVA examined changes over time (baseline, follow-up) and compared rural/urban residing groups. The results were interpreted with sphericity assumed given that for each measure, there were only two factors. Box’s test of equality of covariance matrices and Levene’s test of equality of error variances were examined to ensure assumptions were not violated. Effect sizes were estimated using partial eta squared with the following considerations of magnitude: small = 0.01, moderate = 0.06, and large = 0.14 (Cohen, 1988).
Results
Baseline characteristics
Descriptive statistics were calculated to characterize the sample (n = 326, see Table 1). Participants ranged in age from 21 to 45 years. There were significant differences between rural and urban veteran women with respect to race/ethnicity. Rural veteran women were largely White (77%); over 25% of urban veteran women were Black, compared to about 4% of rural veteran women. At time of entry into the program, urban veteran women had significantly higher PHQ-9 scores (see Table 1).
Table 1.
Participant demographics and baseline characteristics
| Overall (n = 326) |
Urban (n = 272) |
Rural (n = 54) |
Χ2/t-value | |
|---|---|---|---|---|
| Age at screening [mean (SD)] | 32.31 (4.55) | 32.30 (4.53) | 32.4 (4.73) | − .145 |
| Days: birth to baseline [mean (SD)] | 237.09 (117.9) | 239.39 (120.70) | 225.42 (104.12) | − .787 |
| No. of children | ||||
| 1 Child | 38.9% | 40.4% | 31.5% | 1.403 |
| 2 Children | 35.2% | 34.8% | 37.0% | |
| ≥ 3 Children | 25.9% | 24.8% | 31.5% | |
| Partnered | 68.2% | 67.4% | 72.2% | .582 |
| Race/ethnicity | ||||
| White | 48.8% | 43.7% | 77.4%* | 19.098** |
| Black | 21.7% | 25.2% | 3.8% | |
| Latino/a | 15.8% | 16.7% | 11.3% | |
| A/PI, AI/AN | 2.4% | 2.7% | 1.9% | |
| Other | 10.7% | 11.8% | 5.7% | |
| Education | ||||
| High school/GED | 17.6% | 16.6% | 22.2% | .200 |
| Bachelors/associates | 56.1% | 55.2% | 61.1% | |
| Master’s/doctoral | 16.7% | 18.2% | 9.3% | |
| Other | 9.6% | 10.0% | 7.4% | |
| Family income | ||||
| < $40,000 | 30.2% | 28.5% | 39.9% | 2.707 |
| $40–60,000 | 22.7% | 23.6% | 18.5% | |
| $60–80,000 | 17.4% | 18.7% | 11.1% | |
| ≥ 80,000 | 20.6% | 20.2% | 22.2% | |
| Prefer not to say | 8.7% | 8.6% | 9.3% | |
| Occupation | ||||
| Student | 12.9% | 13.5% | 9.8% | 2.732 |
| Work outside home | 64.4% | 65.5% | 58.8% | |
| At-home parent | 22.8% | 21.0% | 31.4% | |
| Rurality | ||||
| Urban | 83.7% | |||
| Large rural | 9.2% | |||
| Small rural | 3.1% | |||
| Isolated | 4.0% | |||
| Previous or current therapy | 89.8% | 90.7% | 85.2% | 1.494 |
| Current psychotropic medication | 74.8% | 73.4% | 81.5% | 1.662 |
| Major depression at screening | 68.2% | 70.1% | 59.3% | 2.420 |
| PHQ-9 at screening [mean (SD)] | 15.28 (3.51) | 15.45 (3.54) | 14.38 (3.24) | 2.048* |
Chi2 tests were used to compare rural versus urban
*Denotes p < .05 and **denotes p < .01 using 1 child versus > 1 child, partnered versus not partnered, white versus non-white, associate’s degree and beyond versus high school/GED, income < $40,000 versus $40,000 or greater, student versus work outside the home versus stay at home parent, prior counseling yes/no, medication yes/no, major depression at screening yes/no. Independent samples t-tests were used to compare rural versus urban for age at screening, days birth to baseline, and PHQ-9 at screening; A/PI, AI/NA = Asian, Pacific Islander, American Indian, Native American
Treatment adherence and utilization
Participants who accepted a welcome call logged on to the MomMoodBooster website an average of 7.61 times (SD = 7.54) over an average engagement of approximately 2 months. Women completed about 61% of the six available modules. Overall, participants completed an average of 3.35 coaching sessions with no difference between urban and rural participants (see Table 2). However, urban women did spend significantly more time on each call with their coaches, t = 2.359, p = 0.019 (see Table 2).
Table 2.
Program use and engagement
| Overall | Urban | Rural | Χ2/t-value | |||
|---|---|---|---|---|---|---|
| Days in program | ||||||
| Baseline to follow-up (days) | 121.44 (33.0) | 122.18 (35.3) | 117.52 (16.12) | .720 | ||
| Welcome call to last log-in (days) | 60.67 (43.78) | 60.54 (37.58) | 61.22 (65.49) | − .099 | ||
| Engagement | ||||||
| Welcome to last coaching (days) | 61.33 (36.76) | 61.63 (36.00) | 59.64 (41.26) | .299 | ||
| Coaching sessions completed | 3.35 (2.55) | 3.46 (2.56) | 2.83 (2.49) | 1.646 | ||
| Total minutes with coach | 47.19 (50.18) | 50.14 (51.94) | 33.16 (38.14) | 2.748** | ||
| Average minutes per call | 10.13 (7.93) | 10.62 (8.13) | 7.81 (6.49) | 2.359* | ||
| Modules opened | 3.85 (2.39) | 3.86 (2.39) | 3.81 (2.44) | .131 | ||
| Mean completion (%) | 60.63 (40.05) | 60.29 (41.55) | 62.35 (41.23) | − .332 | ||
| 80% completion: modules | 50.0% | 49.6% | 51.9% | 1.051 | ||
| 100% completion: modules | 44.5% | 43.8% | 48.1% | 2.287 | ||
| N–C mean completion (%) | 23.1 (24.17) | 23.11 (24.61) | 23.08 (22.15) | .007 | ||
| Program rating | ||||||
| Program helpful | 3.21 (.876) | 3.25 (.844) | 2.97 (1.017) | 1.632 | ||
| Coach helpful | 3.20 (.991) | 3.28 (.932) | 2.79 (1.197) | 2.063* | ||
| Follow-up questionnaire completed | 60.4% | 60.7% | 59.3% | .037 | ||
Numbers are reported as mean (SD) unless otherwise indicated. There were a total six coaching sessions available. Mean completion is reported as the overall percentage of six available modules completed. Completion at 80% and 100% indicates the percentage of the sample completing available modules to these respective levels with six modules available. N–C mean completion refers to the average completion of non-completers, those who did not reach the 80% level. Independent samples t-tests and chi2 tests were used to compare rural versus urban
*Denotes p < .05. **denotes p < .01, two-tailed
Adherence was defined in terms of several metrics, including modules opened, mean completion percentage, and percentage who completed 80% and 100% of the six modules (van Ballegooijen et al., 2014) (see Table 2). Mean completion of lessons was 60.63%. Overall, 50.0% of veteran women were exposed to at least 80% of modules and 44.5% of veteran women were exposed at the 100% level of modules. There were no differences between urban and rural users for any of these metrics. These completion rates are not adjusted to account for those participants who dropped out after recovery as indicated by a PHQ-9 score below the clinical cut-off of 10 (a total of 21 women) following completion of modules three or five.
Program and coach ratings
Participants provided favorable ratings for the program and the coach. The average program rating was 3.21 (SD = 0.876) on the 4-point scale with no difference between urban and rural users. With respect to coach ratings, however, there was a significant difference between rural and urban users, with coaches rated more favorably by urban users; average urban rating of coach was 3.28 (SD = 0.932) and for rural users it was 2.79 (SD = 1.197), p = 0.047 (see Table 2).
Intention-to-treat analyses
Depressive symptoms
Reductions in depressive symptoms were observed over time, F(1,315) = 61.69, p < 0.001, ηp2 = 0.16. There was no main effect of rural/urban residence, F(1,315) = 0.18, p = 0.67, ηp2 = 0.00. There was no interaction between time and rural/urban residence, F(1, 315) = 0.24, p = 0.63, ηp2 = 0.00 (see Table 3 for all primary outcome means and SD).
Table 3.
Primary outcomes for completers and intention to treat
| n | Overall | n | Urban | n | Rural | |
|---|---|---|---|---|---|---|
| Baseline | ||||||
| IDAS GD | 325 | 66.26 (11.73) | 271 | 66.40 (11.78) | 54 | 65.56 (11.53) |
| BADS total | 322 | 66.25 (21.78) | 268 | 65.65 (21.89) | 54 | 69.24 (21.19) |
| ATQ | 325 | 35.07 (9.94) | 271 | 35.09 (9.94) | 54 | 34.98 (10.03) |
| Completers follow-up | ||||||
| IDAS GD | 190 | 52.88 (14.85) | 160 | 53.03 (14.67) | 30 | 52.07 (15.97) |
| BADS total | 191 | 89.21 (26.34) | 162 | 89.57 (26.01) | 29 | 87.21 (28.49) |
| ATQ | 193 | 28.61 (10.12) | 163 | 28.48 (9.94) | 30 | 29.30 (11.22) |
| Intention to treat follow-up | ||||||
| IDAS GD | 317 | 58.63 (15.36) | 265 | 58.68 (15.19) | 51 | 58.35 (16.37) |
| BADS total | 316 | 79.27 (27.46) | 265 | 79.07 (27.66) | 52 | 80.27 (26.62) |
| ATQ | 321 | 31.59 (10.61) | 269 | 31.53 (10.59) | 52 | 31.90 (10.83) |
All results are noted as mean (SD)
IDAS GD inventory for depression and anxiety symptoms general depression scale, BADS total behavioral activation for depression scale total score, ATQ Automatic Thoughts Questionnaire
Behavioral activation
Increased behavioral activation was reported over time, F(1, 313) = 55.05, p < 0.001, ηp2 = 0.15. The main effect of rural/urban residence was not significant, F(1, 313) = 0.46, p = 0.5, ηp2 = 0.0. There was no significant interaction between time and rural/urban residence, F(1, 313) = 0.49, p = 0.49, ηp2 = 0.0.
Automatic thoughts
Automatic thoughts reduced over time, F(1, 318) = 29.21, p < 0.001, ηp2 = 0.08. The main effect of rural/urban residence was not significant, F(1, 318) = 0.0, p = 0.97, ηp2 = 0.0. The interaction between time and rural/urban residence was not significant, F(1, 318) = 0.48, p = 0.49, ηp2 = 0.0.
Completers analyses
Depressive symptoms
Depressive symptoms declined over time, F(1,188) = 82.78, p < 0.001, ηp2 = 0.31. The main effect of rural/urban residence was not significant, F(1,188) = 0.40, p = 0.53, ηp2 = 0.0. The interaction between time and rural/urban residence was not significant, F(1,188) = 0.13, p = 0.72, ηp2 = 0.0.
Behavioral activation
Behavioral activation increased over time, F(1,188) = 71.81, p < 0.001, ηp2 = 0.28. The main effect of rural/urban residence was not significant, F(1,188) = 0.09, p = 0.77, ηp2 = 0.0. There was no significant interaction between time and rural/urban residence, F(1,188) = 0.25, p = 0.62, ηp2 = 0.0.
Automatic thoughts
Decreases in automatic thoughts were observed over time, F(1, 190) = 33.36, p < 0.001, ηp2 = 0.15. The main effect of rural/urban residence was not significant, F(1,190) = 0.02, p = 0.90, ηp2 = 0.0. There was no significant interaction between time and rural/urban residence with automatic thoughts, F(1,190) = 0.37, p = 0.55, ηp2 = 0.0.
Discussion
Response to the MomMoodBooster intervention
The MomMoodBooster program has been evaluated in two trials, one uncontrolled (Danaher et al., 2013) and one controlled trial (Milgrom et al., 2016). Positive results were obtained in both trials. The current report describes outcomes from implementation of the MomMoodBooster program with women veterans. Because the goal was dissemination of the program nationwide, a controlled trial was not feasible. The present analyses examined whether outcomes differed across rural and urban residing veteran women, given known health disparities experienced by rural-residing individuals.
Participation in the MomMoodBooster program was associated with decreased depressive symptoms, increased behavioral activation, and decreased dysfunctional automatic thoughts. Effect sizes across all these outcomes were large (Cohen, 1988) among completers. Effect sizes were large for depressive symptoms and behavioral activation in the ITT analyses. Veteran women entering the program had significant depressive symptoms.
About 75% of the veteran women were taking antidepressant medication, and almost 90% of women had previous or current experience with psychotherapy. Average level of the PHQ-9 at program entry was over 15, which is considered “moderately severe” (Kroenke et al., 2001). More than two-thirds of women were experiencing a current major depression. In sum, the veteran women who participated in the MomMoodBooster program were experiencing significant suffering and depression morbidity that was not being sufficiently addressed by available mental health care.
The MomMoodBooster program was designed to treat postpartum depressive symptoms through a cognitive-behavioral approach. The treatment seeks to target the therapeutic processes measured in this study—behavioral activation and automatic thoughts. The changes observed across these processes are encouraging and suggests that treatment was associated with change in these areas. Of course, without a control condition it is not possible to directly attribute change to the MomMoodBooster program itself. Nevertheless, while depressive symptoms are known to change with passage of time, the BADS, for example, has demonstrated strong test–retest reliability, and such scores would not be expected to change spontaneously (Kanter et al., 2007). Moreover, postpartum depressed women in the treatment as usual condition in the Milgrom et al. (2016) trial only had about a 0.4 SD change from baseline to follow-up for both the BADS and the ATQ, providing some indication that the passage of time may not explain the results in the current study.
Uptake and use of MomMoodBooster among rural and urban veteran women
One of the goals of the MomMoodBooster program was to disseminate services to rural residing women who because of access limitations or cultural issues might not readily seek mental health treatment. Regarding access to services, the general erosion of health care services in rural areas has contributed to a longstanding shortage of mental health care providers in those regions. The National Institute of Mental Health (NIMH, 2018) indicated that 60% of rural Americans live in mental health professional shortage areas. With respect to veterans specifically, Teich et al. (2017) indicated that rural veterans with a mental health diagnosis are less likely than their urban counterparts to receive any mental health treatment. Also, rural veterans are less likely to receive specialty mental health care (Cully et al., 2010).
As noted earlier, approximately 25% of veterans live in rural America. The MomMoodBooster program reached out to all eligible veteran postpartum women, regardless of rural/urban residence, and surprisingly, only 17.8% of the 8,435 eligible veteran women resided in rural areas. One potential explanation for this seemingly under-representation of rural veteran women in our overall pool is that the VA database only contained the records of veteran women whose maternity care was paid for by VA. Although VA maternity care coordinators provide prenatal care to pregnant veteran women, VA does not provide obstetrical services. Veteran women invariably receive obstetrical care from non-VA providers who are paid by VA. Many veteran women have private insurance or choose not to afford themselves of VA-supported private care. As a result, women who do not utilize VA-supported private care are not included in the database that served as the basis for recruitment. This raises the possibility that rural veteran women are using VA paid maternity care at a much lower rate than their urban counterparts or the possibility that veteran women of childbearing age are more likely to live in urban areas than veterans as a whole. Furthermore, the data regarding veteran rural/urban residence is reported across genders, so it cannot be determined whether the representation of rural women in this study aligns with veteran women nationwide [U.S. Department of Veterans Affairs (VA), 2020]. Participation in the MomMoodBooster program largely tracked the overall representation of veteran women in the pool, suggesting that rural veteran women were not less likely to stay the course through the MomMoodBooster program.
There were no differences in response to the MomMoodBooster program between rural and urban dwelling veteran women. In the current context, it is reassuring that rural dwelling veteran women are as likely to participate in and benefit from an online, coach supported program for postpartum depression as urban dwelling women. Cultural issues regarding acceptability of psychotherapy, whether provided face-to-face or in the context of an internet-based intervention, appear not to have significantly impacted the outcomes across rural and urban residing veterans. However, there was one area in which rural and urban dwelling women did differ significantly: time in contact with the phone coach. For both average minutes per call and the total number of minutes across all calls with a coach, rural-dwelling veteran women spent significantly less time. This difference may be at least partially explained by the rural agrarian value system which has been associated with distrust of science and technology (Heath, 2020) and the distinct cultural aspects of rural identity that include a skepticism of outsiders (Slama, 2004). Time spent with coaches may have also been related to the rural values of self-reliance and stoicism. For example, Robinson et al. (2012) argued that these interpersonal approaches to life mean that consulting a mental health professional carries a great deal of stigma, which is a barrier to receiving services. In one study addressing rural low-income women, the prevalence rate of major and minor depression was 38%, and yet only 2.3% of those with a diagnosis were receiving counseling (Price & Proctor, 2009). It may be that rural women are less comfortable with discussing psychological symptom management in general or feel reluctant to discuss personal matters with an unfamiliar provider. Rural women may therefore have derived more benefit from the anonymity of the online content than the phone coaching.
Other literature indicates that rural residents are more likely to rely on informal support systems like family and primary care physicians rather than mental health care professionals (Robinson et al., 2012). Rural women in our sample may not have engaged as much with coaching because of these relatively more well-developed social support systems. Social support has been inversely associated with depressive symptoms. Ross et al. (2011) found that rural women have higher levels of social network diversity which was significantly related to lower postpartum EPDS scores. With respect to reliance on primary care physicians for mental health care, it is important to note that integration of mental health services into rural primary care settings has been suggested for addressing disparities in access to care. Women have expressed that they prefer to have depression treatment considered part of prenatal care (Bhat et al., 2018). However, with less than one-fifth of rural communities having local obstetrics care (Nidey et al., 2020), additional options such as remote care provisions like MomMoodBooster may be vital to closing the rural–urban gap. Having demonstrated similar effectiveness for rural women makes this a promising option.
Program participants opened an average of about four of the six program modules and overall completed about 61% of the program lessons. Fifty percent of program participants completed at least 80% of modules. There were no differences across groups. These rates are somewhat lower than two previous MomMoodBooster trials (Danaher et al., 2013; Milgrom et al., 2016), but only a total of 74 postpartum depressed women had been included in these two trials. The number of postpartum depressed women in the MomMoodBooster program was nearly five times that of the two previous two trials together. Moreover, rather than representing just a few communities where the other studies were conducted, women in the VA MomMoodBooster program were very diverse in race, ethnicity, rurality, and geographic locale, and represented 46 of the 50 states and the District of Columbia. Participants had very favorable overall ratings of the program (3.21 on a 4-point scale) and the coaches (3.20 on a 4-point scale), though urban veterans rated coaches more highly than did rural veterans. It will be important for phone coaches and staff to recognize the diversity in postpartum depressed veteran women, reflect on cultural opportunities (Hayes et al., 2015), and adjust coaching accordingly to maximize participants’ engagement in the program.
Limitations
Program staff were able to reach out by letter to 8,435 postpartum veteran women over the course of several years (see Figure #1). However, program staff were unable to make phone contact with 3051 of these women. Many of these women may have been reluctant to answer a call from an unfamiliar number even though they were alerted by the program introductory letter that a call would be forthcoming. Additionally, 2375 women declined to participate. These women were most likely to be feeling well and had no need for the MomMoodBooster program. Another 1966 women were ineligible for different reasons. Other women were eligible at screening but were lost along the way. More work is needed to understand the unique barriers to initiation, engagement, and completion for both urban and rural dwelling veteran women.
Strengths
One important positive feature of the MomMoodBooster program had little to do with its impact on the mental health of veteran women who utilized the program. Staff reached out by letter to a very large number of postpartum veteran women over a 5-year period, signaling to women whether they were well or experiencing mood symptoms in the postpartum period that the VA recognized their vulnerability and was offering a free mental health program that was accessible to them no matter where they lived. Relatedly, program staff were trained to assess postpartum depression and related conditions, addressing previously reported shortfalls in screening and detection of perinatal mood disorders (Ashford et al., 2016). The MomMoodBooster program for veteran women recruiting strategy provides a layer of screening otherwise unavailable to postpartum veterans, thereby increasing the chances that women in need of services will have access to much needed support. The national reach of the recruiting strategy opens new possibilities for reaching women in rural locations who might otherwise struggle to connect with specialized services. MomMoodBooster is a efficacious (Danaher et al., 2013; Milgrom et al., 2016) and accessible option that for some may be the sole option for managing postpartum symptoms and for others may be one level of a stepped-care model of treatment for PPD (O’Mahen et al., 2013). The format of the online content is highly structured and interactive, which, when combined with supportive coaching, increases acceptance and reduces attrition (van Ballegooijen et al., 2014).
Initiation of the program was slightly higher than what has previously been reported in the literature as the help-seeking average (33–42%) among those with a diagnosis of depression. Of those screened eligible, 48.1% received a welcome call from a coach, 44.86% engaged with the first session and 36.72% engaged with the first coaching call. This suggests that the personal contact with eligible women makes a difference in comfort and willingness to engage in services. These results are consistent with previous literature that demonstrates that tailoring interventions to the specific concerns of the perinatal period increases engagement (O’Mahen et al., 2012). Finally, the size of this sample gives us relative certainty of the reported effects.
Conclusion
The MomMoodBooster program showed clear value for treatment of PPD in rural and urban settings. Continuing to work toward improving initiation and retention of women as well as dissemination of the program through partnerships with community providers may further improve access for under-served veteran women.
More work is needed to understand the specific aspects of the program and coaching that contribute to positive outcomes for women, as well as to further understand the unique experiences and barriers of both rural life and women experiencing postpartum depression. Additional options for treatment and prevention during the antenatal period may help to further reduce the mental health burden of perinatal depression. Finally, the move to telemedicine associated with COVID-19 makes the availability of programs like MomMoodBooster even more important as a viable alternative to face-to-face care.
Acknowledgements
The following individuals were instrumental in the administration of the project through logistical support, program management, recruiting, coaching, and data management: Bruce Alexander, Caroline Boyd-Rogers, Charles Brunette, Nicole Dietrich, Lindsey Greth, Michael Hallin, Jaclyn Kamradt, Taylor Magnuson, Kristen Merkitch, Michelle Miller, Graham Nelson, Brianne Richson, Anne Roche, Amarilys Saldana, Francesca Scheiber, Neevetha Sivagurunathan, Manny Stegall, Staff of the Veterans Rural Health Resource Center-Iowa City. The US Department of Veterans Affairs had no role in the analysis or interpretation of data or the decision to report these data in a peer-reviewed journal. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government. MomMoodBooster (MomMoodBooster.com) was developed by an international team in the US (Brian G. Danaher PhD, Milagra Tyler MS, and John R. Seeley PhD; Oregon Research Institute & Influents Innovations) plus Scott Stuart, MD (University of Iowa) and in Australia (Jeannette Milgrom PhD, Alan W Gemmill PhD, and colleagues; Parent-Infant Research Institute—PIRI). We especially thank Danaher and Tyler for their work in adapting the program to fit the requirements of our VA trial and for providing support/training.
Author contributions
All authors contributed to the implementation of the intervention, data analysis, and preparation of the manuscript. Recruiting, data collection, and intervention management were performed by PJH. Application of the intervention, data collection, and data analysis were performed by CLS. Data analysis was performed by EBK. Conceptualization, study design, and supervision of the intervention was performed by MWO’. The first draft of the manuscript was written by CLS, and all authors contributed to the writing and editing process. All authors read and approved of the final manuscript.
Funding
This research was supported by the U.S. Veterans Health Administration (VHA) Office of Rural Health, Veterans Rural Health Resource Center-Iowa City (Award # 15023) and the VHA Office of Women’s Health Services. Visit www.ruralhealth.va.gov to learn more.
Compliance with ethical standards
Conflict of interest
Michael O’Hara served as a paid consultant for “Responsive eHealth Intervention for Perinatal Depression in Healthcare Settings” (MH109191; PI: Brian Danaher). Cara Solness, Emily Kroska, and Paul Holdefer declare no conflicts of interest.
Human rights statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the University of Iowa Institutional Review Board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Andersson G, Cuijpers P. Internet-based and other computerized psychological treatments for adult depression: A meta-analysis. Cognitive Behaviour Therapy. 2009;38:196–205. doi: 10.1080/16506070903318960. [DOI] [PubMed] [Google Scholar]
- Andrews G, Cuijpers P, Craske MG, McEvoy P, Titov N. Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: A meta-analysis. PLoS ONE. 2010;5:e13196. doi: 10.1016/j.janxdis.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrilla CHA, Patterson DG, Garberson LA, Coulthard C, Larson EH. Geographic variation in the supply of selected behavioral health providers. American Journal of Preventive Medicine. 2018;54:S199–S207. doi: 10.1016/j.amepre.2018.01.004. [DOI] [PubMed] [Google Scholar]
- Appolomio KK, Fingerhut R. Postpartum depression in a military sample. Military Medicine. 2008;173:1085–1091. doi: 10.7205/MILMED.173.11.1085. [DOI] [PubMed] [Google Scholar]
- Ashford MT, Olander EK, Ayers S. Computer-or web-based interventions for perinatal mental health: A systematic review. Journal of Affective Disorders. 2016;197:134–146. doi: 10.1016/j.jad.2016.02.057. [DOI] [PubMed] [Google Scholar]
- Bhat A, Reed S, Mao J, Vredevoogd M, Russo J, Unger J, Rowles R, Unützer J. Delivering perinatal depression care in a rural obstetric setting: A mixed methods study of feasibility, acceptability and effectiveness. Journal of Psychosomatic Obstetrics and Gynecology. 2018;39:273–280. doi: 10.1080/0167482X.2017.1367381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark DM. Implementing NICE guidelines for the psychological treatment of depression and anxiety disorders: The IAPT experience. International Review of Psychiatry. 2011;23:318–327. doi: 10.3109/09540261.2011.606803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Cuijpers P, van Straten A, Warmerdam L. Behavioral activation treatments of depression: A meta-analysis. Clinical Psychology Review. 2007;27:318–326. doi: 10.1016/j.cpr.2006.11.001. [DOI] [PubMed] [Google Scholar]
- Cully JA, Jameson JP, Phillips LL, Kunik ME, Fortney JC. Use of psychotherapy by rural and urban veterans. The Journal of Rural Health. 2010;26:225–233. doi: 10.1111/j.1748-0361.2010.00294.x. [DOI] [PubMed] [Google Scholar]
- Danaher BG, Milgrom J, Seeley JR, Stuart S, Schembri C, Tyler MS, Ericksen J, Lester W, Gemmill AW, Lewinsohn P. Web-based intervention for postpartum depression: Formative research and design of the MomMoodBooster program. JMIR Research Protocols. 2012;1:e18. doi: 10.2196/resprot.2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danaher BG, Milgrom J, Seeley JR, Stuart S, Schembri C, Tyler MS, Ericksen J, Lester W, Gemmill AW, Kosty DB, Lewinsohn P. MomMoodBooster web-based intervention for postpartum depression: Feasibility trial results. Journal of Medical Internet Research. 2013;15:e242. doi: 10.2196/jmir.2876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn HA, Blow FC, Marcus SM. Rates and predictors of depression treatment among pregnant women in hospital-affiliated obstetrics practices. General Hospital Psychiatry. 2006;28:289–295. doi: 10.1016/j.genhosppsych.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Fox J, Merwin E, Blank M. De facto mental health services in the rural south. Journal of Health Care for the Poor and Underserved. 1995;6:434–469. doi: 10.1353/hpu.2010.0003. [DOI] [PubMed] [Google Scholar]
- Fuhr K, Hautzinger M, Krisch K, Berking M, Ebert DD. Validation of the Behavioral Activation for Depression Scale (BADS): Psychometric properties of the long and short form. Comprehensive Psychiatry. 2016;66:209–218. doi: 10.1016/j.comppsych.2016.02.004. [DOI] [PubMed] [Google Scholar]
- Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): A diagnostic meta-analysis. Journal of General Internal Medicine. 2007;22:1596–1602. doi: 10.1007/s11606-007-0333-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes JA, Owen J, Bieschke KJ. Therapist differences in symptom change with racial/ethnic minority clients. Psychotherapy. 2015;52:308–314. doi: 10.1037/a0037957. [DOI] [PubMed] [Google Scholar]
- Heath, F. E. (2020). Britannica. https://www.britannica.com/topic/agrarianism
- Henshaw, E., Sabourin, B., & Warning, M. (2013). Treatment‐seeking behaviors and attitudes survey among women at risk for perinatal depression or anxiety. Journal of Obstetric, Gynecologic & Neonatal Nursing, 42, 168–177. 10.1111/1552-6909.12014 [DOI] [PubMed]
- Hollon SD, Kendall PC. Cognitive self-statements in depression: Development of an automatic thoughts questionnaire. Cognitive Therapy and Research. 1980;4:383–395. doi: 10.1007/BF01178214. [DOI] [Google Scholar]
- Judd F, Jackson H, Komiti A, Murray G, Fraser C, Grieve A, Gomez R. Help-seeking by rural residents for mental health problems: The importance of agrarian values. Australian and New Zealand Journal of Psychiatry. 2006;40:769–776. doi: 10.1111/j.1440-1614.2006.01882.x. [DOI] [PubMed] [Google Scholar]
- Kanter JW, Mulick PS, Busch AM, Berlin KS, Martell CR. The Behavioral Activation for Depression Scale (BADS): Psychometric properties and factor structure. Journal of Psychopathology and Behavioral Assessment. 2007;29:191–202. doi: 10.1007/s10862-006-9038-5. [DOI] [Google Scholar]
- Kintzle S, Schuyler AC, Ray-Letourneau D, Ozuna SM, Munch C, Xintarianos E, Hasson AM, Castro CA. Sexual trauma in the military: Exploring PTSD and mental health utilization in female veterans. Psychological Services. 2015;12:394–401. doi: 10.1037/ser0000054. [DOI] [PubMed] [Google Scholar]
- Klaman SL, Turner K. Prevalence of perinatal depression in the military: A systematic review of the literature. Maternal and Child Health Journal. 2016;20:52–65. doi: 10.1007/s10995-016-2172-0. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavender TJ, Ebert L, Jones D. An evaluation of perinatal mental health interventions: An integrative literature review. Women and Birth. 2016;29:399–406. doi: 10.1016/j.wombi.2016.04.004. [DOI] [PubMed] [Google Scholar]
- Le H-N, Perry DF, Sheng X. Using the internet to screen for postpartum depression. Maternal and Child Health Journal. 2009;13:213–221. doi: 10.1007/s10995-008-0322-8. [DOI] [PubMed] [Google Scholar]
- Lee EW, Denison FC, Hor K, Reynolds RM. Web-based interventions for prevention and treatment of perinatal mood disorders: A systematic review. BMC Pregnancy and Childbirth. 2016;16:1–8. doi: 10.1186/s12884-016-0831-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazzucchelli T, Kane R, Rees C. Behavioral activation treatments for depression in adults: A meta-analysis and review. Clinical Psychology Science and Practice. 2009;16:383–411. doi: 10.1111/j.1468-2850.2009.01178.x. [DOI] [Google Scholar]
- McCarthy JF, Blow FC, Ignacio RV, Ilgen MA, Austin JL, Valenstein M. Suicide among patients in the veterans affairs health system: Rural-urban differences in rates, risks, and methods. American Journal of Public Health. 2012;102:S111–S117. doi: 10.2105/AJPH.2011.300463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milgrom J, Danaher BG, Gemmill AW, Holt C, Holt CJ, Seeley JR, Tyler MS, Ross J, Ericksen J. Internet cognitive behavioral therapy for women with postnatal depression: A randomized controlled trial of MumMoodBooster. Journal of Medical Internet Research. 2016;18:e54. doi: 10.2196/jmir.4993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair U, Armfield NR, Chatfield MD, Edirippulige S. The effectiveness of telemedicine interventions to address maternal depression: A systematic review and meta-analysis. Journal of Telemedicine and Telecare. 2018;24:639–650. doi: 10.1177/1357633X18794332. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (NICE). (2020). Antenatal and postnatal mental health [NICE Guideline no. 192]. https://www.nice.org.uk/guidance/cg192 [PubMed]
- National Research Council and Institute of Medicine. (2009). Depression in parents, parenting, and children: Opportunities to improve identification, treatment, and prevention. Committee on Depression, Parenting Practices, and the Healthy Development of Children. Board on Children, Youth, and Families. Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press. [PubMed]
- NIMH. (2018). Mental health and rural America: Challenges and opportunities. https://www.nimh.nih.gov/news/media/2018/mental-health-and-rural-america-challenges-and-opportunities.shtml
- Netemeyer RG, Williamson DA, Burton S, Biswas D, Jindal S, Landreth S, Mills G, Primeaux S. Psychometric properties of shortened versions of the Automatic Thoughts Questionnaire. Educational and Psychological Measurement. 2002;62:111–129. doi: 10.1177/0013164402062001008. [DOI] [Google Scholar]
- Nguyen S, LeardMann CA, Smith B, Conlin AS, Slymen DJ, Hooper TI, Ryan MAK, Smith TC. Is military deployment a risk factor for maternal depression? Journal of Women’s Health. 2013;22:9–18. doi: 10.1089/jwh.2012.3606. [DOI] [PubMed] [Google Scholar]
- Nidey N, Tabb KM, Carter KD, Bao W, Strathearn L, Rohlman DS, Wehby G, Ryckman K. Rurality and risk of perinatal depression among women in the United States. The Journal of Rural Health. 2020;36:9–16. doi: 10.1111/jrh.12401. [DOI] [PubMed] [Google Scholar]
- O’Mahen HA, Flynn HA. Preferences and perceived barriers to treatment for depression during the perinatal period. Journal of Women's Health. 2008;17:1301–1309. doi: 10.1089/jwh.2007.0631. [DOI] [PubMed] [Google Scholar]
- O'Mahen HA, Woodford J, McGinley J, Warren FC, Richards DA, Lynch TR, Taylor RS. Internet-based behavioral activation-treatment for postnatal depression (Netmums): A randomized controlled trial. Journal of Affective Disorders. 2013;150:814–822. doi: 10.1016/j.jad.2013.03.005. [DOI] [PubMed] [Google Scholar]
- O’Mahen H, Fedock G, Henshaw E, Himle JA, Forman J, Flynn HA. Modifying CBT for perinatal depression: What do women want? Cognitive and Behavioral Practice. 2012;19:359–371. doi: 10.1016/j.cbpra.2011.05.005. [DOI] [Google Scholar]
- Parikh SV, Segal ZV, Grigoriadis S, Ravindran AV, Kennedy SH, Lam RW. Canadian network for mood and anxiety treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. II. Psychotherapy alone or in combination with antidepressant medication. Journal of Affective Disorders. 2009;117:S15–S25. doi: 10.1016/j.jad.2009.06.042. [DOI] [PubMed] [Google Scholar]
- Price SK, Proctor EK. A rural perspective on perinatal depression: Prevalence, correlates, and implications for help-seeking among low-income women. The Journal of Rural Health. 2009;25:158–166. doi: 10.1111/j.1748-0361.2009.00212.x. [DOI] [PubMed] [Google Scholar]
- Renton T, Tang H, Ennis N, Cusimano MD, Bhalerao S, Schweizer TA, Topolovec-Vranic J. Web-based intervention programs for depression: A scoping review and evaluation. Journal of Medical Internet Research. 2014;16:e209. doi: 10.2196/jmir.3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riding-Malon R, Werth JL., Jr Psychological practice in rural settings: At the cutting edge. Professional Psychology: Research and Practice. 2014;45:85–91. doi: 10.1037/a0036172. [DOI] [Google Scholar]
- Robinson WD, Springer PR, Bischoff R, Geske J, Backer E, Olson M, Jarzynka K, Swinton J. Rural experiences with mental illness: Through the eyes of patients and their families. Families, Systems, & Health. 2012;30:308–321. doi: 10.1037/a0030171. [DOI] [PubMed] [Google Scholar]
- Ross LE, Villegas L, Dennis CL, Bourgeault IL, Cairney J, Grigoriadis S, Steele LS, Yudin MH. Rural residence and risk for perinatal depression: A Canadian pilot study. Archives of Women's Mental Health. 2011;14:175–185. doi: 10.1007/s00737-011-0208-4. [DOI] [PubMed] [Google Scholar]
- Rost K, Smith GR, Taylor JL. Rural-urban differences in stigma and the use of care for depressive disorders. Journal of Rural Health. 1993;9:57–62. doi: 10.1111/j.1748-0361.1993.tb00495.x. [DOI] [PubMed] [Google Scholar]
- Schachman K, Lindsey L. A resilience perspective of postpartum depressive symptomatology in military wives. Journal of Obstetric, Gynecologic and Neonatal Nursing. 2013;42:157–167. doi: 10.1111/1552-6909.12007. [DOI] [PubMed] [Google Scholar]
- Searle AK, Van Hooff M, McFarlane AC, Davies CE, Tran T, Hodson SE, Benassi HP, Steele NM. Screening for depression and psychological distress in a currently serving military population: The diagnostic accuracy of the K10 and the PHQ9. Assessment. 2019;26:1411–1426. doi: 10.1177/1073191117745124. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of Clinical Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- Sidebottom AC, Harrison PA, Godecker A, Kim H. Validation of the Patient Health Questionnaire (PHQ)-9 for prenatal depression screening. Archives of Women's Mental Health. 2012;15:367–374. doi: 10.1007/s00737-012-0295-x. [DOI] [PubMed] [Google Scholar]
- Slama K. Rural culture is a diversity issue. Minnesota Psychologist. 2004;53:9–13. [Google Scholar]
- Smith MV, Shao L, Howell H, Wang H, Poschman K, Yonkers KA. Success of mental health referral among pregnant and postpartum women with psychiatric distress. General Hospital Psychiatry. 2008;31:155–162. doi: 10.1016/j.genhosppsych.2008.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teich J, Ali MM, Lynch S, Mutter R. Utilization of mental health services by veterans living in rural areas. The Journal of Rural Health. 2017;33:297–304. doi: 10.1111/jrh.12221. [DOI] [PubMed] [Google Scholar]
- Thomas L, Gandhi S, Parel JT. Interventions for mothers with postpartum depression: A systematic review. International Journal of Depression and Anxiety. 2018;1:1–8. doi: 10.23937/IJDA-2017/1710002. [DOI] [Google Scholar]
- Watson D, O’Hara MW, Chmielewski M, McDade-Montez EA, Koffel E, Naragon K, Stuart S. Further validation of the IDAS: Evidence of convergent, discriminant, criterion, and incremental validity. Psychological Assessment. 2008;20:248–259. doi: 10.1037/a0012570. [DOI] [PubMed] [Google Scholar]
- Watson D, O’Hara MW, Naragon-Gainey K, Koffel E, Chmielewski M, Kotov R, Stacik SM, Ruggero CJ. Development and validation of new anxiety and bipolar symptom scales for an expanded version of the IDAS (the IDAS-II) Assessment. 2012;19:399–420. doi: 10.1177/1073191112449857. [DOI] [PubMed] [Google Scholar]
- Watson D, O'Hara MW, Simms LJ, Kotov R, Chmielewski M, McDade-Montez EA, Gamez W, Stuart S. Development and validation of the inventory of depression and anxiety symptoms (IDAS) Psychological Assessment. 2007;19:253–268. doi: 10.1037/1040-3590.19.3.253. [DOI] [PubMed] [Google Scholar]
- Weeks WB, Wallace AE, West AN, Heady HR, Hawthorne K. Research on rural veterans: An analysis of the literature. The Journal of Rural Health. 2008;24:337–344. doi: 10.1111/j.1748-0361.2008.00179.x. [DOI] [PubMed] [Google Scholar]
- Van Ballegooijen W, Cuijpers P, van Straten A, Karyotaki E, Andersson G, Smit JH, Riper H. Adherence to internet-based and face-to-face cognitive behavioural therapy for depression: A meta-analysis. PLoS ONE. 2014;9:e100674. doi: 10.1371/journal.pone.0100674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veterans Administration. (2020). About Rural Veterans. Available at: https://www.ruralhealth.va.gov/aboutus/ruralvets.asp. Accessed May 2, 2020.