Abstract
This ecological study investigated the association between COVID-19 distribution and air quality index (AQI), comorbidities and sociodemographic factors in the USA. The AQI factors included in the study are total AQI, ozone, carbon monoxide, sulfur dioxide, and nitrogen dioxide (NO2). Other demographic, socioeconomic, and geographic variables were included as covariates. The correlations of COVID-19 variables—proportion of cases and deaths in each population, as well as case fatality rate with independent variables were determined by Pearson and Spearman correlation and multiple linear regression analyses. The results revealed that AQI-NO2, population density, longitude, gross domestic product per capita, median age, total death of disease, and pneumonia per population were significantly associated with the COVID-19 variables (P < 0.05). Air pollutants, especially NO2 in the US case, could be addressed as an important factor linked with COVID-19 susceptibility and mortality.
Keywords: COVID-19, Air quality index, Comorbidities, Population density, Longitude, Income
Introduction
The new coronavirus disease (COVID-19) pandemic has claimed more than 500,000 lives globally, causing massive public health and economic challenges (Liang et al. 2020; Conticini et al. 2020). This infectious disease, emerging in Wuhan, China, causes severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The methods of contagion SARS-CoV-2 is not yet well understood, including what key modifiable parameters may contribute to spread of the virus. The risk factors for COVID-19 -associated severity and death are still under investigation, but some environmental and demographic factors such as air pollution (particle matter, nitrogen dioxide (NO2), ozone (O3)) (Coccia 2020; Fattorini and Regoli 2020; Frontera et al. 2020; Liang et al. 2020), atmospheric patterns (temperature, humidity) (Sajadi et al. 2020; Sarmadi et al. 2020b), and comorbidities (cardiovascular and cerebrovascular disease, and cancer) (Richardson et al. 2020; Tian et al. 2020) might play a plausible role for both susceptibility and vulnerability of populations. The impact of mentioned parameters on excessive morbidity and mortality attributed to other respiratory or chronic diseases has been well-established in recent years (Liu et al. 2019; Shi et al. 2016; Wang et al. 2019; Grande et al. 2020). In order to investigate the correlation between air pollution indicators and various diseases, air quality index (AQI) can be considered as an important parameter that involves many air pollution elements. An analysis of 55 provinces capital in Italy recently revealed that increase in symptomatic COVID-19 infected cases was associated with variations in air pollution level (Coccia 2020). Also, other studies found that prevalence of comorbidities plays a key role in higher mortality of COVID-19 (Richardson et al. 2020; Tian et al. 2020; Ravi 2020). It also has been proven that some medical conditions like diabetes and heart diseases can increse the risk of death in COVID-19 patient (Richardson et al. 2020; Coccia 2020). Additionally, race and ethnicity were associated with the rate of death in different societies (Rentsch et al. 2020; Gross et al. 2020).
Regarding the possible contribution of air pollution and comorbidities in the risk of COVID-19 infection and mortality, this study aimed to assess the association between air pollutants and infection and mortality rate and whether race and comorbidities act modify the spread of COVID-19.
Materials and methods
Study area, data, and sources
This ecological study was conducted based on data from COVID-19 patients in all 50 US states; the District of Columbia (DC) and Puerto Rico. The USA (24–71°N, 67–172°E) is situated at the North of America continent, covers an area of 9,833,520 km2, and has a population about 328,239,523.
For this analysis, data was acquired from the Centers for Disease Control and Prevention (CDC) as the main source of COVID-19 descriptive statistics, including the proportion of cases per 105 persons (PCP), deaths per 105 persons (PDP), and case fatality rate (CFR).
Measures of the study
Parameters such as weighted distribution of population (%) for race and comorbidities include septicemia, malignant neoplasms, diabetes mellitus, Alzheimer disease, influenza and pneumonia, chronic lower respiratory diseases, other diseases of the respiratory system, nephritis, nephrotic syndrome and nephrosis, diseases of heart, and cerebrovascular diseases compiled from the CDC for 22 weeks prior to June 6, 2020. Air quality and socioeconomic and demographic indicators were determined from the US Environmental Protection Agency’s (EPA) AQI (USEPA 2020) and World Population Review website (World Population Review 2020), respectively.
Data analysis procedure
A descriptive analysis was conducted on all the data. Here, t test and one-way ANOVA test were used to compare proportion of cases (PCI), proportion of deaths (PCD), and CFR values between states categories. Pearson and Spearman correlation, as well as linear regression analysis were conducted to assess the association between AQI, comorbidities, and demographic data and the number of cases and deaths from COVID-19 per 100,000 people. We have used log-transformed PCI and PCD as a dependent variable and mean AQI, weighted distribution of population in each state (%), and number of previously mentioned diseases of interest in each population as independent variables. All the statistical analyses were 2-tailed and performed at a 5% significance level using SPSS 16 and Prism version 6 (GraphPad).
Results and discussion
While precise discussions about factors contributing to the novel coronavirus pandemic distribution are inconclusive, some plausible reasons for our findings were reviewed. Air pollution, comorbidities, and socioeconomic–demographic are main factors in contributing to the infection and mortality of COVID-19 spread in-between states of USA.
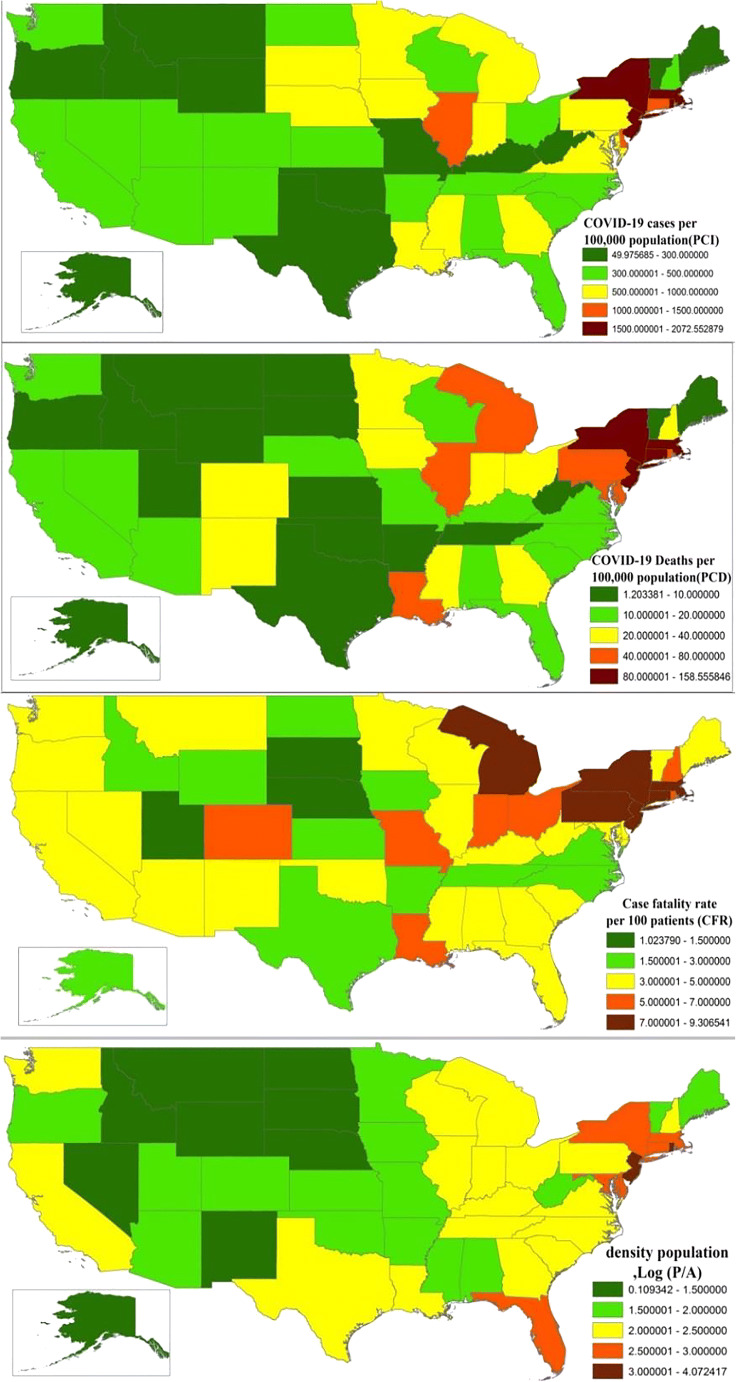
The number of cases and reported deaths per population in New York was much higher compared with other states (402,914 cases of 2,074,852 individuals and 30,824 of 114,967 deaths) (Fig. 1). Table 1 showed the association of COVID-19 variables (PCI, PCD, and CFR) and some plausible factors contributing to the inter-states COVID-19 distribution. The association between AQI-NO2 and COVID-19 variables was statistically significant (r = 0.51 for PCD, r = 0.46 for PCI, and r = 0.40 for CFR; P < .05). Also, population density (log density) and total mortality over 22 weeks were positively associated with PCI, PCD, and CFR (P < .001), whereas longitude was inversely associated (Table 2 and Appendix). The correlations were stronger among AQI-NO2, pneumonia deaths, population density, longitude, and PCD, suggesting these potential key factors may have considerably increased mortality rates.
Fig. 1.
Geographical distribution of the proportion of cases (PCI), deaths (PCD) per 100,000 population, case fatality rate (%) (updated June 12, 2020) and density population (logarithm population per area (km2)
Table 1.
Correlation (r) between COVID-19 variables and independent variables
| Variable | Log PCI | Log PCD | CFR |
|---|---|---|---|
| Air pollution | |||
| AQI-total | 0.110 | 0.079 | 0.035 |
| AQI-Ozone | − 0.252 | − 0.283 | − 0.233 |
| AQI-SO4 | 0.005 | 0.079 | 0.160 |
| AQI-CO | 0.225 | 0.272 | 0.175 |
| AQI-NO2 | 0.464** | 0.513** | 0.399* |
| Race | |||
| Non-Hispanic Black or African American | 0.119 | 0.112 | 0.035 |
| Non-Hispanic American Indian or Alaska Native | − 0.281 | − 0.403** | − 0.370* |
| Non-Hispanic Asian | 0.112 | 0.135 | 0.078 |
| Comorbidities | |||
| Total deathsa | 0.286* | 0.366** | 0.328* |
| Pneumonia deathsa | 0.647** | 0.719** | 0.642** |
| Influenza and pneumoniaa | 0.355* | 0.297* | 0.295* |
| Nephritis nephrotic syndrome and nephrosisa | 0.235 | 0.306* | 0.294* |
| Other diseases of respiratory systema | 0.383** | 0.465** | 0.411** |
| Septicemiaa | 0.219 | 0.358** | 0.358** |
| Socioeconomic-demographic | |||
| Log density | 0.564** | 0.652** | 0.524** |
| HDI | 0.230 | 0.218 | 0.188 |
| GDP ($US) | 0.395** | 0.375** | 0.224 |
| Median age | − 0.084 | 0.131 | 0.357** |
| Longitude (°) | − 0.569** | − 0.612** | − 0.446** |
Other race or comorbidities not significant with low correlation coefficient. ** P < 0.01, *P < 0.05
AQI air quality index, PCP proportion of cases to population per 105, PDP proportion of deaths to population per 105, CFR case fatality rate (%), HDI human development index, GDP gross domestic product per capita ($US)
aDeaths for 22 weeks as up June 6, 2020, per 105 population
Table 2.
multivariable linear regression analysis between independent variables and COVID-19 variables (adjusted with HDI)
| Variables | PCI | PCD | CFR | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F-test | B (SE) | R2 | Sig. | F-test | B (SE) | R2 | Sig. | F-test | B (SE) | R2 | Sig. | |
| AQI-NO2 | 5.10 | 0.02(0.005) | 0.25 | 0.003 | 5.94 | 0.03(0.008) | 0.28 | 0.002 | 4.34 | 0.08(0.04) | 0.22 | 0.04 |
| Log density | 8.65 | 0.24(0.06) | 0.26 | < 0.001 | 19.47 | 0.45(0.008) | 0.44 | < 0.001 | 16.18 | 1.77(0.36) | 0.40 | < 0.001 |
| Median age | 0.93 | 0.022(0.02) | 0.04 | 0.24 | 1.50 | 0.03(0.027) | 0.06 | 0.34 | 8.44 | 0.35(0.11) | 0.26 | 0.003 |
| Longitude (°) | 9.81 | − 0.009(0.002) | 0.29 | < 0.001 | 20.45 | − 0.02(0.003) | 0.46 | < 0.001 | 16.55 | − 0.06(0.01) | 0.40 | < 0.001 |
| Total deathsa | 5.71 | 0.002(0.001) | 0.19 | 0.002 | 18.90 | 0.005(0.001) | 0.45 | < 0.001 | 24.67 | 0.02(0.004) | 0.50 | < 0.001 |
| Pneumonia deathsa | 14.70 | 0.01(0.002) | 0.38 | < 0.001 | 32.40 | 0.02(0.002) | 0.76 | < 0.001 | 24.31 | 0.08(0.01) | 0.50 | < 0.001 |
| Influenza and pneumoniaa | 0.23 | 0.006(0.008) | 0.02 | 0.44 | 1.63 | 0.012(0.011) | 0.06 | 0.29 | 4.24 | 0.08(0.07) | 0.15 | 0.13 |
| Nephritis nephrotic syndrome and nephrosisa | 0.62 | − 0.001(0.008) | 0.03 | 0.93 | 1.67 | 0.005(0.012) | 0.07 | 0.69 | 3.84 | 0.07(0.05) | 0.14 | 0.2 |
| Other diseases of respiratory systema | 2.22 | 0.021(0.01) | 0.11 | 0.04 | 8.37 | 0.05(0.02) | 0.26 | 0.001 | 11.60 | 0.27(0.07) | 0.33 | < 0.001 |
| Septicemiaa | 2.44 | 0.03(0.01) | 0.10 | 0.04 | 7.57 | 0.07(0.02) | 0.26 | 0.001 | 14.48 | 0.35(0.08) | 0.40 | < 0.001 |
AQI air quality index, PCP proportion of cases to population per 105, PDP proportion of deaths to population per 105, CFR case fatality rate (%), HDI human development index
**P < 0.01, *P < 0.05
aDeaths for 22 weeks as up June 6, 2020, per 105 population
With regard to high basic reproductive number (R0) of COVID-19, it is apparent that states with high population density have a higher proportion of infected individuals and consequently high mortality rate, as described in previous studies (Wu et al. 2020; Rocklöv and Sjödin 2020). The number of total COVID-19 deaths (per population) is correlated with the population density, which is a troublesome issue. Increase in implemented control measures accompanied with increased hospital capacity and testing of asymptomatic patients could also impact the distribution scale of the virus between states (Lau et al. 2020; Conticini et al. 2020). Between January 19th (report first case) and June 12th, the results showed major infected cases and death numbers of COVID-19 to New York and New Jersey. At the same time (January 1st and June 6th), an explosion of total and pneumonia deaths per population within New Jersey State was detected. This state has the second highest density in the USA.
Air pollution elements such as PM2.5, PM10, NO2, and O3 are known to play an important role in both infectious and non-infectious diseases (Wang et al. 2019; Liu et al. 2019; Grande et al. 2020; Lin et al. 2007; Chang et al. 2020; Ciencewicki and Jaspers 2007). Some studies have also investigated the association between air pollution and incidence and distribution of COVID-19 in different other countries (Frontera et al. 2020; Fattorini and Regoli 2020). The air pollution associations revealed in this study were similar to that of prior studies in USA (Liang et al. 2020). A higher value of CFR and PCD was significantly associated with exposure to NO2, but not O3 and PM2.5 (Liang et al. 2020; Anil and Alagha 2020; Islam et al. 2020). On the other hand, Wu et al. 2020 showed that only 1 μg/m3 increase in PM2.5 was associated with an eighth percent increase in the COVID-19 death rate. This study suggested that air pollution exposure may suppress early immune response to infection through inflammation and cellular damage (Wu et al. 2020), in line with other infectious diseases such as SARS (Cui et al. 2003).
The results of current study showed that longitude was negatively correlated with COVID-19 variables (Appendix). In fact, states in the western USA (high longitude) had lower median age, comorbidities, and air pollution as well as population density (Fig. 1). On the other hand, GDP per capita was positively correlated with PCI and PCD. It appears that the investment in health systems of regions with higher income may support screening programs and tests for fast and high volume diagnosis of patients infected with COVID-19 and/or asymptomatic individuals, and vice versa (Chattu and Yaya 2020; Vasquez et al. 2020; Sarmadi et al. 2020a). Additionally, it seems that prevalence of comorbidities plays a determinative role in COVID-19 incidence and mortality. Similarly, prevalence of heart disease and diabetes was positively associated with risk of death in other studies (Richardson et al. 2020; Coccia 2020).
We acknowledge that there are some limitations to this study as follows: The data for number of cases and deaths attributed to COVID-19 are invariably different in each state due to differences in diagnosis criteria, variation in the number of available tests in each state, different sensitivity and specificity of each test, and reporting protocols. Other potential factors discussed in the studies (Sajadi et al. 2020; Sarmadi et al. 2020b). It is also suggested that future studies should address the effect of quarantine policies, adherence, and effectiveness, public awareness, social distancing, length of hospitalization, migration, and other chronic disease.
Conclusion
Despite the inherent limitations of the ecological study design utilized and our subsequent inability to assess associations at an individual and temporal level, our study suggested that air pollution components, especially NO2, could be contributing factors in the interstate distribution of COVID-19. Population density might be also an effective factor in COVID-19 outbreak. Alongside demographic factors, wearing facemasks and adhering to social and physical distancing guideline are imperative to limit spreading the disease. We also acknowledge that higher incidence rates in some states reflect economic differences, which may impact access and availability of diagnostic services and healthcare provisions. It also seems that Non-Hispanic American Indian or Alaska Native are more resistant against COVID-19. Finally, we believe that health managers and policymakers in the USA should consider the implemented measurements based on social distancing, school closures, and funding for hospital infrastructure, which has the ability to slow the spread of disease, with special attention to providing education and resources to vulnerable and historically marginalized populations with disproportionate exposures to air pollution.
Acknowledgments
The authors would like to thank the Torbat Heydariyeh University of Medical Sciences for their support for performing this research.
Abbreviations
- AQI
air quality index
- CDC
The Centers for Disease Control and Prevention
- CFR
case fatality rate
- COVID-19
coronavirus disease 2019
- EPA
Environmental Protection Agency
- GDP
gross domestic product
- NO2
nitrogen dioxide
- O3
ozone
- PCP
proportion of cases per population
- PDP
proportion of death per population
- PM
particle matter
- SARS-CoV-2
severe acute respiratory syndrome coronavirus 2
- USA
United States of America
Appendix
Scatter plots show standardize coefficients of liner regression model between COVID-19 and independent variables
Fig. 2.

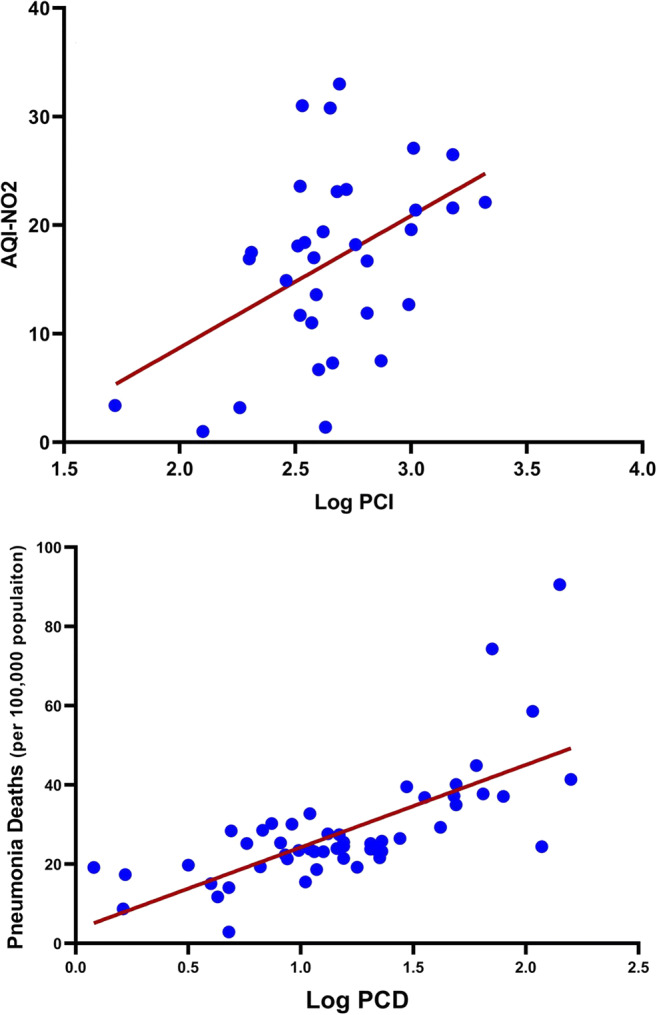
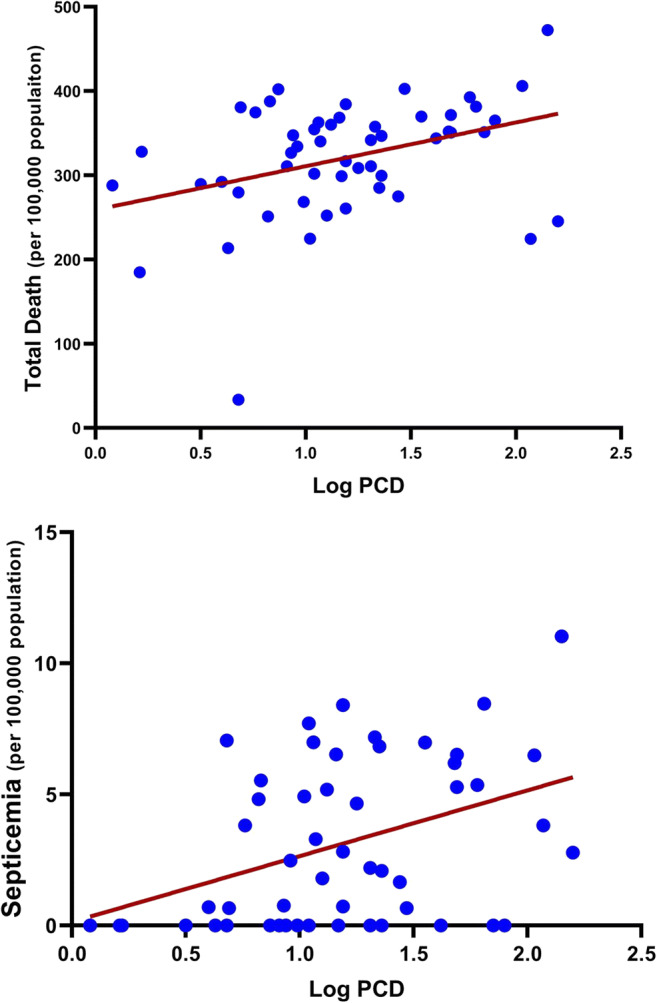
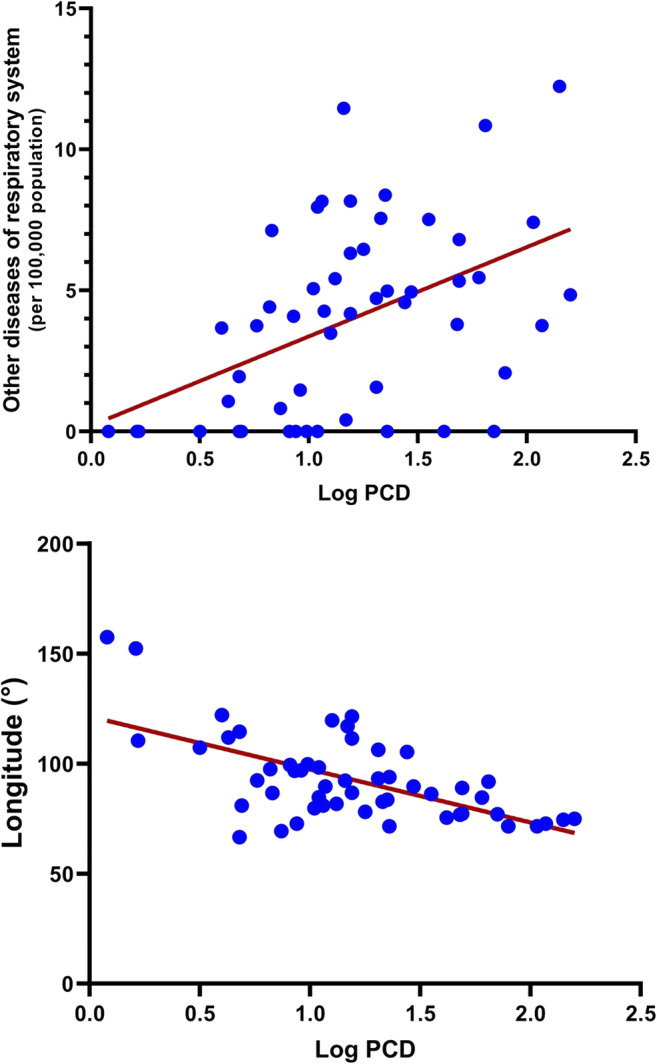







Scatter plots show liner regression model between COVID-19 and independent variables AQI air quality index, PCP proportion of cases to population per 105, PDP proportion of deaths to population per 105, CFR case fatality rate (%), HDI human development index, GDP gross domestic product per capita ($US)
Authors’ contributions
Mohammad Sarmadi: conceptualization, methodology, formal analysis, investigation, project administration, resources, data curation, writing—original draft, writing—review and editing, supervision. Vahid Kazemi Moghadam: conceptualization, investigation, writing—original draft, writing—review and editing. Aisha S. Dickerson: methodology, formal analysis, investigation, writing—original draft, writing—review and editing. Luigi Martelletti: investigation, writing—original draft, writing—review and editing. All authors read and approved the manuscript.
Data availability
All data generated or analyzed during this study are included in this published article.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Anil I, Alagha O. The impact of COVID-19 lockdown on the air quality of Eastern Province. Saudi Arabia: Air Qual Atmos Health; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang Q, Zhang H, Zhao Y. Ambient air pollution and daily hospital admissions for respiratory system–related diseases in a heavy polluted city in Northeast China. Environ Sci Pollut Res. 2020;27:10055–10064. doi: 10.1007/s11356-020-07678-8. [DOI] [PubMed] [Google Scholar]
- Chattu VK, Yaya S. Emerging infectious diseases and outbreaks: implications for women’s reproductive health and rights in resource-poor settings. Reprod Health. 2020;17:43. doi: 10.1186/s12978-020-0899-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciencewicki J, Jaspers I (2007) Air pollution and respiratory viral infection. Inhal Toxicol 19:1135–1146 [DOI] [PubMed]
- Coccia M (2020) Factors determining the diffusion of COVID-19 and suggested strategy to prevent future accelerated viral infectivity similar to COVID. Sci Total Environ. 729–138474. 10.1016/j.scitotenv.2020.138474 [DOI] [PMC free article] [PubMed]
- Conticini E, Frediani B, Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ Pollut. 2020;261:114465. doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui Y, Zhang Z-F, Froines J, Zhao J, Wang H, Yu, S.-Z. & Detels, R. Air pollution and case fatality of SARS in the People's Republic of China: an ecologic study. Environ Health. 2003;2:15. doi: 10.1186/1476-069X-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fattorini D, Regoli F. Role of the chronic air pollution levels in the Covid-19 outbreak risk in Italy. Environ Pollut. 2020;264:114732. doi: 10.1016/j.envpol.2020.114732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frontera A, Martin C, Vlachos K, Sgubin G. Regional air pollution persistence links to COVID-19 infection zoning. J Inf Secur. 2020;S0163-4453(20):30173. doi: 10.1016/j.jinf.2020.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grande G, Ljungman PL, Eneroth K, Bellander T, Rizzuto D. Association between cardiovascular disease and long-term exposure to air pollution with the risk of dementia. JAMA Neurol. 2020;77:9. doi: 10.1001/jamaneurol.2019.4914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross CP, Essien UR, Pasha S, Gross JR, Wang SY, Nunez-Smith M (2020) Racial and ethnic disparities in population-level covid-19 mortality. Journal of general internal medicine, 1-3. [DOI] [PMC free article] [PubMed]
- Islam MS, Tusher TR, Roy S, Rahman M. Impacts of nationwide lockdown due to COVID-19 outbreak on air quality in Bangladesh: a spatiotemporal analysis. Air Qual Atmos Health. 2020 doi: 10.1007/s11869-020-00940-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau H, Khosrawipour V, Kocbach P, Mikolajczyk A, Ichii H, Zacharski M, Bania J, Khosrawipour T. The association between international and domestic air traffic and the coronavirus (COVID-19) outbreak. J Microbiol Immunol Infect. 2020;53:467–472. doi: 10.1016/j.jmii.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang D, Shi L, Zhao J, Liu P, Schwartz J, Gao S, Sarnat J, Liu Y, Ebelt S, Scovronick N (2020) Urban Air Pollution May Enhance COVID-19 Case-Fatality and Mortality Rates in the United States. The Innovation 100047. 10.1016/j.xinn.2020.100047 [DOI] [PMC free article] [PubMed]
- Lin H-H, Ezzati M, Murray M. Tobacco smoke, indoor air pollution and tuberculosis: a systematic review and meta-analysis. PLoS Med. 2007;4:17. doi: 10.1371/journal.pmed.0040020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C, Chen R, Sera F, Vicedo-Cabrera AM, Guo Y, Tong S, Coelho MS, Saldiva PH, Lavigne E, Matus P. Ambient particulate air pollution and daily mortality in 652 cities. N Engl J Med. 2019;381:705–715. doi: 10.1056/NEJMoa1817364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravi K. Ethnic disparities in COVID-19 mortality: are comorbidities to blame? Lancet. 2020;396(10243):22. doi: 10.1016/S0140-6736(20)31423-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rentsch CT, Kidwai-Khan F, Tate JP, Park LS, King JT, Skanderson M, Hauser RG, Schultze A, Jarvis CI, Holodniy M, Lore V, Akgun KM, Crothers K, Taddei TH, Freiberg MS, Justice AC (2020) Covid-19 by race and ethnicity: a national cohort study of 6 million United States veterans. medRxiv: The Preprint Server for Health Sciences. 10.1101/2020.05.12.20099135
- Richardson S, Hirsch JS, Narasimhan M, Crawford JM, Mcginn T, Davidson KW, Consortium ATNCR. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocklöv J, Sjödin H. High population densities catalyse the spread of COVID-19. J Travel Med. 2020;27:2. doi: 10.1093/jtm/taaa038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sajadi MM, Habibzadeh P, Vintzileos A, Shokouhi S, Miralles-Wilhelm F, Amoroso A. Temperature, humidity, and latitude analysis to estimate potential spread and seasonality of coronavirus disease 2019 (COVID-19) JAMA Netw Open. 2020;3:e2011834–e2011834. doi: 10.1001/jamanetworkopen.2020.11834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarmadi M, Kakhki S, Foroughi M, Abadi TSH, Nayyeri S, Moghadam VK, Ramezani M. Hospitalization period of COVID-19 for future plans in hospital. BJS (Brit J Surg) 2020;107:e427–e428. doi: 10.1002/bjs.11871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarmadi M, Marufi N, Kazemi Moghaddam V. Association of COVID-19 global distribution and environmental and demographic factors: an updated three-month study. Environ Res. 2020;188:109748. doi: 10.1016/j.envres.2020.109748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L, Zanobetti A, Kloog I, Coull BA, Koutrakis P, Melly SJ, Schwartz JD. Low-concentration PM2. 5 and mortality: estimating acute and chronic effects in a population-based study. Environ Health Perspect. 2016;124:46–52. doi: 10.1289/ehp.1409111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian J, Yuan X, Xiao J, Zhong Q, Yang C, Liu B, Cai Y, Lu Z, Wang J, Wang Y, Liu S, Cheng B, Wang J, Zhang M, Wang L, Niu S, Yao Z, Deng X, Zhou F, Wei W, Li Q, Chen X, Chen W, Yang Q, Wu S, Fan J, Shu B, Hu Z, Wang S, Yang X-P, Liu W, Miao X, Wang Z. Clinical characteristics and risk factors associated with COVID-19 disease severity in patients with cancer in Wuhan, China: a multicentre, retrospective, cohort study. Lancet Oncol. 2020;21:893–903. doi: 10.1016/S1470-2045(20)30309-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- USEPA (2020) Air data: air quality data collected at outdoor monitors across the US [online]. USA. Available: https://www.epa.gov/outdoor-air-quality-data [Accessed 15 June 2020]
- Vasquez L, Sampor C, Villanueva G, Maradiegue E, Garcia-Lombardi M, Gomez-García W, Moreno F, Diaz R, Cappellano AM, Portilla CA. Early impact of the COVID-19 pandemic on paediatric cancer care in Latin America. Lancet Oncol. 2020;21:753–755. doi: 10.1016/S1470-2045(20)30280-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M, Hou Z-H, Xu H, Liu Y, Budoff MJ, Szpiro AA, Kaufman JD, Vedal S, Lu B. Association of estimated long-term exposure to air pollution and traffic proximity with a marker for coronary atherosclerosis in a nationwide study in China. JAMA Netw Open. 2019;2:e196553–e196553. doi: 10.1001/jamanetworkopen.2019.6553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Population Review (2020) Median Age by State 2020 [Online]. Available: https://worldpopulationreview.com/states/median-age-by-state/ [Accessed 15June 2020]
- Wu X, Nethery RC, Sabath BM, Braun D, Dominici F (2020) Exposure to air pollution and COVID-19 mortality in the United States. medRxiv: The Preprint Server for Health Sciences. 10.1101/2020.04.05.20054502
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.