Abstract
Previous research has demonstrated that the burden of household food insecurity is disproportionately high among racial/ethnic minority groups, yet no peer-reviewed studies have systematically examined racial/ethnic disparities in household food insecurity in the context of the COVID-19 pandemic. This cross-sectional study on household food insecurity during COVID-19 used data from a nationally representative sample of US households through the 2020 Household Pulse Survey (HPS) (including all 50 states and the District of Columbia, n = 74,413 households). Six generalized estimating equation (GEE) models were estimated, and the results indicated that households headed by Blacks, Asians, Hispanics, or other racial/ethnic minorities were not significantly more food insecure than White households during the pandemic. However, among food-insecure households, Black households were more likely to report that they could not afford to buy more food; Asian and Hispanic households were more likely to be afraid to go out to buy food; Asian households were more likely to face transportation issues when purchasing food; while White households were more likely to report that stores did not have the food they wanted. Moreover, racial/ethnic minorities were significantly less confident about their household food security for the next 4 weeks than Whites. The coronavirus pandemic crisis has exposed and exacerbated the food injustice in American society. Policymakers and local officials should take concerted actions to improve the capacity of food supply and ensure food equality across all racial/ethnic groups.
Keywords: Food insecurity, Race/ethnicity, Household pulse survey, COVID-19
Introduction
Household food insecurity, defined as the limited or uncertain ability to acquire adequate food for one or more household members [1], remains an issue of great concern among American families. According to a recent US Department of Agriculture (USDA) report, in 2018, about 11.1% of US households experienced food insecurity at least part of the time, which equates to 37.2 million people, including 11.2 million children [2]. The salience of food insecurity has been underscored by its links to adverse health and social outcomes. People from food-insecure households, for example, tend to report poorer physical health [3–5], symptoms of anxiety or depression [6, 7], lower self-esteem [8], and poorer overall mental health status [9, 10]. Particularly, children who live in food-insecure homes are more likely to have emotional distress, decreased quality of life, and worse academic performance [11–14]. Annually, food insecurity has caused at least 160 billion dollars of economic burden in the USA [15]. Therefore, some scholars refer to food insecurity as “a symptom of a complex and multidimensional social disease” [16].
Household Food Insecurity During the COVID-19 Pandemic
While the prevalence of household food insecurity in the US has been slowly decreasing in the years following the Great Recession, reaching a pre-recession level in 2018 [2], the ongoing COVID-19 pandemic crisis has worsened the situation. Caused by the novel coronavirus SARS-CoV-2, COVID-19 was identified in December 2019 and declared a pandemic by the World Health Organization (WHO) on March 11th, 2020 [17]. The pandemic and social distancing efforts implemented to slow its spread have disrupted global and local food supply chains [18]. Due to the unprecedented rise in unemployment, many households are experiencing income shocks, which led to an inability to afford food. A Marketplace report concluded that the US is now facing its worst food insecurity challenge [19].
The most striking revelation of the pandemic and food insecurity is that a significant portion of previously food-secure households is facing food insecurity for the first time. According to the Marketplace report, approximately 40% of the increase in food bank usage comes from individuals experiencing food insecurity for the first time [19, 20]. On the other hand, food scarcity at grocery stores, as well as income and labor insecurity, is hindering the already adverse situations of more vulnerable groups. Indeed, poor or low-income and pre-pandemic food-insecure households are facing greater food hardship during the pandemic [21]. It is clear that the COVID-19 tragedy has devastatingly threatened the food security of American families, and we still have much to learn about the characteristics of household food insecurity during this crisis, including racial/ethnic disparities.
Race/Ethnicity and Household Food Insecurity
The burden of household food insecurity is not distributed equally, as this burden is disproportionately high among racial/ethnic minority groups [3, 22–25]. For example, even though food insecurity in 2018 had reached the pre-recession level, households headed by Blacks and Hispanics remained disproportionately affected by food insecurity at a rate of 21.2% and 16.2%, respectively, while the national average was 11.1% [2]. The relationship between race/ethnicity and food insecurity is complex, as it intertwines with other risk factors, such as poverty and unemployment. Previous research suggests that the concentration of social and economic disadvantage among racial/ethnic minorities is a significant predictor of their higher rates of food insecurity [26].
However, despite the intersectionality of race/ethnicity and other social or economic factors of food insecurity, some studies noted that the higher risk of food insecurity among people of color continues even after the effects of other confounders are removed [10, 27–30]. It is possible that racial discrimination and racism play a role in creating food inequalities across racial/ethnic groups. For example, Burke et al. [31] investigated the association between lifetime racial discrimination and food insecurity among Black food-insecure households with children in South Carolina. They found that even after adjusting for other demographic and socioeconomic confounders, every unit increase in the frequency of racial discrimination was associated with a 5% increase in the odds of being very low food secure [31].
To the best of our knowledge, no peer-reviewed studies have systematically examined racial/ethnic disparities in household food insecurity in the context of the COVID-19 pandemic. Yet, there is evidence suggesting that the ongoing crisis has more adverse implications on racial/ethnic minorities [32–34]. Based on the previous research on food insecurity, we hypothesize that during the COVID-19 pandemic, racial/ethnic minority households experience higher levels of food insecurity than White households. We analyzed data of a nationally representative sample of US households through the 2020 Household Pulse Survey (HPS). The generalized estimating equation (GEE) procedure was utilized to select the best fitting models to test the hypothesis. To disentangle the independent effect of race/ethnicity on household food insecurity from other confounders, we adjusted for demographic characteristics, household structure, socioeconomic status (SES), and health in all models. These four areas were selected based on a review of the literature on the determinants of household food insecurity [2, 3, 35–38]. Specifically, for demographic characteristics, we included sex and age, which have been shown to affect food insecurity [22, 35, 39]. Household structure factors, including household size, marital status, and the number of children, are also associated with food insecurity [3, 36]. Since SES is a crucial predictor of food insecurity [36], in our models, we included four SES variables: poverty, education, housing tenure, and employment status. Finally, the general health status has been linked to household food insecurity [40, 41].
Material and Methods
Data
This study is a secondary analysis of cross-sectional data, and measures were derived from the 2020 Household Pulse Survey (HPS). To understand the impacts of the COVID-19 pandemic on American households, the US Census Bureau developed and implemented the HPS in partnership with five federal statistical partner agencies, including the Bureau of Labor Statistics, the National Center for Health Statistics, the United States Department of Agriculture’s Economic Research Service, the National Center for Education Statistics, and the Department of Housing and Urban Development. The Census Bureau selected a large nationally representative sample for the HPS by utilizing its Master Address File (MAF), which is considered the gold standard frame for US statistics [42]. In fact, the HPS is one of the first nationally representative surveys that provide comprehensive and timely information on the social and economic implications of COVID-19 [42].
Data collection of the HPS began on April 23, 2020, and was conducted by an Internet questionnaire through the online survey platform Qualtrics, with survey links sent by email. The HPS questionnaire includes questions on employment status, spending patterns, food security, housing, physical and mental health, access to health care, and educational disruption during the pandemic. For the week-one sample, there were 74,413 respondents in total [42]. On May 20, 2020, data pertaining to the week-one sample were released through tables, interactive data tools, and microdata files accessible from the US Census Bureau’s Experimental Data webpage (https://www.census.gov/programs-surveys/household-pulse-survey/datasets.html). We used the week-one HPS microdata files for this study. Overall, our analyses included 74,413 American households across the 50 states and the District of Columbia. Due to the HPS’ complex sampling design, we applied the recommended sampling weight to adjust for differential probabilities of selection for each household [42]. The sampling design of HPS and our survey-weighted analyses allow for generalization to households in the US.
Variables
Table 1 provides descriptive statistics for each analytical variable. Together, our analyses included six dependent variables, and the independent variables were grouped into two categories: focal independent variables and control variables.
Table 1.
Descriptive statistics for analytical variables (n = 74,413)
| Variables | Frequency | % missing | Mean | SD |
|---|---|---|---|---|
| Dependent variables: | ||||
| Household food insecurity level | 1.70 | 0.535 | 0.722 | |
| Causes of household food insecurity | ||||
| Couldn’t afford to buy more food | 11,565 | 0.00 | ||
| Afraid or did not want to go out to buy food | 7998 | |||
| Couldn’t get out to buy food due to transportation, mobility, or health issues | 3049 | |||
| The stores did not have the food they wanted | 15,812 | |||
| Household food security confidence level | 8.37 | 3.036 | 1.012 | |
| Independent variables: | ||||
| Household food insecurity level prior to March 13, 2020 | 1.67 | 0.383 | 0.685 | |
| Demographic Characteristics | ||||
| Age | 0.00 | 48.236 | 16.805 | |
| Sex | ||||
| Female | 38,417 | 0.00 | ||
| Male | 35,996 | |||
| Race/ethnicity | ||||
| White | 46,720 | 0.00 | ||
| Black | 8546 | |||
| Asian | 3804 | |||
| Hispanic | 12,479 | |||
| Other racial/ethnic groups | 2864 | |||
| Household Structure | ||||
| Total number of people in household | 0.00 | 3.482 | 1.949 | |
| Married and had children | 18,135 | 0.71 | ||
| Unmarried and had children | 11,571 | |||
| Married and no children | 23,133 | |||
| Unmarried and no children | 21,044 | |||
| SES | ||||
| Household income | 13.57 | 78,817.35 | 53,466.46 | |
| Educational attainment | 0.00 | 4.348 | 1.593 | |
| Housing Tenure | ||||
| Owned | 14,769 | 10.71 | ||
| Rented | 21,343 | |||
| Mortgage or loan | 30,333 | |||
| Employed for the last 7 days | 38,727 | 0.70 | ||
| You or anyone in your household might experience a loss of employment income in the next 4 weeks because of the COVID-19 pandemic | 28,680 | 0.74 | ||
| Received free groceries or a free meal during the past 7 days | 5422 | 1.97 | ||
| Health | ||||
| General health status | 9.37 | 3.543 | 1.039 | |
Results presented in Table 1 were weighted based on the HPS recommended sampling weights
Dependent Variables
The USDA Household Food Security Survey Module (HFSSM) uses a multi-item scale to assess a variety of aspects of a household’s access to food, which becomes a standard measure of food insecurity in the USA [2]. Instead of including any items from the HFSSM scale, the HPS collected a different measure of food insecurity by asking respondents to choose a statement that best described the food eaten situation in their households over the past 7 days [42]. A recent research report confirmed that the HPS measure is a good indicator of household food insecurity and aligns with the HFSSM measure [43]. We used responses to the HPS question to construct a variable measuring the level of household food insecurity during the COVID-19 pandemic, which ranges from 0 = food secure (“enough of the kinds of food I/we wanted to eat”) to 3 = severely food insecure (“often not enough to eat”). The greater the value, the higher level of food insecurity of the household. The average level of food insecurity of our sample was 0.54.
For those households that self-reported being food insecure, HPS asked the specific reasons why they did not have enough food. Based on the responses, we created four binary variables (each coded as 0 = no; 1 = yes) to measure different causes of food insecurity. They are as follows: (1) could not afford to buy more food; (2) afraid or did not want to go out to buy food; (3) could not get out to buy food due to transportation, mobility, or health issues; and (4) the stores did not have the food they wanted. Among the 30,534 food-insecure households in our sample, 38% of them could not afford to buy more food, 26% were afraid or did not want to go out to buy food, 10% could not go out to buy food, and 52% reported that stores did not have the food they wanted.
Finally, respondents rated their levels of confidence about food security of their households for the next 4 weeks, based on a 4-point Likert-type scale (from 1 = “not at all confident” to 4 = “very confident”). We used responses to this question to create the food security confidence variable. The average level of food security confidence of our sample was 3.04.
Focal Independent Variables
Race/ethnicity variables were our focal independent variables. An HPS-provided variable indicating the respondent’s race/ethnicity was used, and we recorded it into five binary variables (each coded as 0 = no; 1 = yes), including White, non-Hispanic; Black/African American, non-Hispanic; Asian, non-Hispanic; Hispanic; and other racial/ethnic groups, non-Hispanic. White was used as the reference group in the analyses. In our sample, 63% of respondents were White, 11% were Black, 5% were Asian, 17% were Hispanic, and 4% were from other racial/ethnic groups.
Control Variables
Preexisting Household Food Insecurity
The HPS asked respondents’ household food security status before March 13, 2020. Using responses to this question, we developed a variable to measure the level of preexisting household food insecurity status, and its value ranged from 0 = food secure to 3 = severely food insecure. For our sample, the average level of preexisting household food insecurity was 0.38.
Demographic Characteristics
The respondent’s age in years was calculated based on the reported date of birth. We used the respondent sex variable from the HPS: females were coded as 1, and males were coded as 0. The average age of all respondents included in this study was 48 years old, and about 52% of respondents were female.
Household Structure
The HPS provided the total number of people (adults and children) currently living in each household. For all households included in the sample, the average household size was 3 people. Depending on the respondent’s marital status and whether he/she had child/ren, we created four binary variables (each coded as 0 = no; 1 = yes): (1) married and had child/ren; (2) unmarried and had child/ren; (3) married without child/ren; (4) unmarried without child/ren. Respondents who were married and had child/ren were used as the reference group in the analyses. Among all respondents, 25% of them were currently married and had children, 16% were unmarried and had children, 31% were married but did not have children, and 28% were unmarried and did not have children.
Socioeconomic Status (SES)
Total household income before taxes was provided by the HPS. The average household income for our sample was 78,817 dollars. Based on the federal poverty thresholds, household income, household size, and numbers of children, we categorized all households into three groups: above low income, low income, and poor. In terms of educational attainment, each respondent reported his/her highest degree completed, ranging from 1 = less than high school to 7 = graduate degree. For the sample, the average educational attainment level was 4.35.
For housing tenure, we created three binary variables (each coded as 0 = no; 1 = yes): 1) the respondent owned the house/apartment without a mortgage or loan; (2) the respondent owned the house/apartment with a mortgage or loan; and (3) the respondent rented the house/apartment. Respondents who owned their houses/apartments without a mortgage/loan were used as the reference group. Together, about 30% of the households included in this study owned their houses or apartments without a mortgage or loan, 41% had a mortgage/loan, and 29% rented their houses or apartments.
For employment status, we used the survey question about whether the respondent did any work for either pay or profit during the past 7 days (0 = no; 1 = yes). In our sample, 52% of respondents were employed. Moreover, employment expectation was measured by whether the respondent expected him/her or anyone in the household to experience a loss of employment income in the next 4 weeks because of the pandemic. About 47% of households expected to experience a loss of employment income due to COVID-19. In addition, the free meal variable indicated whether the respondent or anyone in the household received free groceries or meals during the past 7 days (0 = no; 1 = yes). In the sample, 7% of households reported receiving free groceries or meals.
Health
Respondents rated their health, in general, using a 5-point Likert-type scale (1 = poor; 5 = excellent). The average general health scores reported by the respondents was 3.54.
Analytic Strategy and Modeling Plan
We analyzed the dataset using generalized estimating equations (GEEs). GEEs are appropriate for this study for two main reasons: first, like other generalized linear models, GEEs relax the assumptions of traditional regression models, such as normality of variable distribution [44–46]; second, GEEs are better than other generalized linear models when used to analyze clustered data [47], and our data has a clustered structure: the 74,413 households in our sample were clustered within the 50 states and the District of Columbia. GEEs have also been used to analyze clustered data in other studies [48–50].
In total, six GEE models were estimated. In Model 1, we included all households (n = 74,413) and used the level of household food insecurity as the dependent variable, race/ethnicity as focal independent variables, and the level of preexisting household food insecurity, demographic characteristics, household structure, SES, and health as control variables. For Models 2–5, we only included households that self-reported as food insecure (n = 30,534). The four causes of household food insecurity were dependent variables, and independent variables were the same as those in Model 1. Finally, in Model 6, the level of food security confidence was the dependent variable. Independent variables were similar to those in Model 1, except that employment expectation was included as an additional control variable.
In terms of the intracluster dependency correlation matrix of GEEs, in this study, we specified the exchangeable correlation matrix, which assumes constant intracluster dependency, such that all off-diagonal elements of the correlation matrix are equal [45, 46]. We used this specification in other studies (e.g., 49, 50, 52), and it fits better than other applicable specifications (i.e., independent and unstructured) for the six GEE models.
To select the best fitting models, for Model 1 and Model 6, we tested normal, gamma, and inverse Gaussian distributions for dependent variables with logarithmic (log) and identity link functions [51]. We selected the inverse Gaussian with the identity link function for Model 1 and the inverse Gaussian with the log link function for Model 6. For Models 2–5, since dependent variables were dichotomous, we selected binomial distributions with a logit link function [51]. Those specifications were selected because they yielded the lowest quasi-likelihood under the independence criterion (QIC) values, meaning they were the best fitting models.
Based on the variance inflation factor (VIF) and tolerance, inferences from the six GEE models were not affected by multicollinearity. Missing data was not an issue for this study, as the missing values of the main variables we included in the analyses (age, sex, race/ethnicity, educational attainment, household size, whether the respondent had child/ren) were already imputed by the HPS [42]. Other variables we used had low levels of missing data (< 14%). Therefore, in the analyses, the listwise deletion was implemented to handle missing data.
Results
Descriptive Results
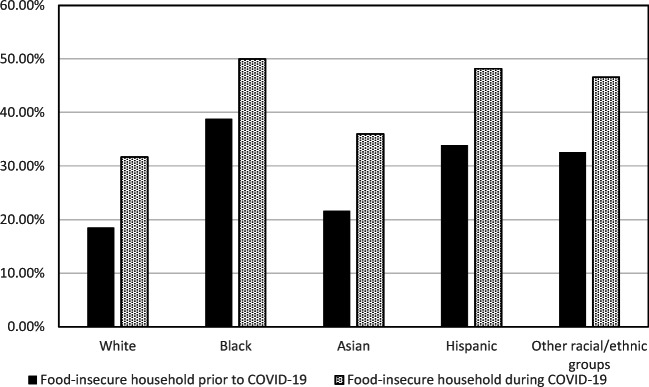
Based on a nationally representative sample of US households, we found that the overall prevalence of household food insecurity has been increasing as the pandemic evolves. Before March 13, 2020, about 30% of households in our sample self-reported as food insecure, while the number rapidly increased to 43% in late April 2020. As shown in Fig. 1, among the five racial/ethnic groups, the percentage of food-insecure households has raised more than 14% for Asian and Hispanic households and more than 13% for White households. Until late April, about half Black and Hispanic households in our sample were food insecure. In terms of SES, 11% Black and 9% Hispanic households were poor, compared to 2% for White and 3% for Asian households. About 65% Asians were employed for the last 7 days, which was higher than Whites (56%), Blacks (57%), Hispanics (57%), and other racial/ethnic groups (57%). On average, Asians had the highest educational attainment level (5.85), while Hispanics had the lowest level (4.69).
Fig. 1.
The percentage of food-insecure households before and during COVID-19 by race/ethnicity
Multivariate Results
Table 2 reports the results from Model 1, predicting the level of food insecurity during the COVID-19 pandemic among the 74,413 households. Households headed by Blacks, Asians, or Hispanics were not significantly more food insecure than White households during the pandemic (p > 0.05). Households with higher levels of preexisting food insecurity experienced higher levels of food insecurity during the pandemic (p < 0.0001). In terms of demographic characteristics, Model 1 suggests that older respondents reported significantly lower levels of household food insecurity than younger respondents during the pandemic (p < 0.0001), while sex was not a significant predictor (p = 0.125). For household structure, we found that households with a larger size tended to be significantly more food insecure during the pandemic (p = 0.047). Unmarried respondents with (p = 0.036) or without (p = 0.018) children had higher levels of food insecurity than married respondents who had children. For SES variables, low-income households had significantly higher levels of food insecurity than above-low-income households (p = 0.036), while there was no significant difference between poor and above-low-income households (p = 0.141). As compared to households that owned their houses/apartments without a mortgage/loan, households that had a mortgage/loan (p = 0.002) or rented their houses/apartments (p = 0.002) experienced significantly higher levels of food insecurity during COVID-19. People who were employed were less food insecure than people who did not work for pay for the past 7 days (p < 0.0001), and households that received free meals/groceries for the past 7 days were significantly more food insecure than households that did not receive free meals/groceries (p < 0.0001). Finally, the healthier the respondents reported being, the more food secure their households were (p < 0.0001).
Table 2.
Results of the GEE model predicting the level of household food insecurity during the COVID-19 pandemic (n = 74,413)
| Variables | Model 1 | |||
|---|---|---|---|---|
| B | SE | CI | p | |
| Intercept | 1.647*** | 0.045 | (1.558; 1.735) | < 0.0001 |
| Household food insecurity level prior to March 13, 2020 | 0.652*** | 0.010 | (0.633; 0.672) | < 0.0001 |
| Demographic characteristics: | ||||
| Age | − 0.004*** | 0.000 | (− 0.005; − 0.004) | < 0.0001 |
| Female | 0.009 | 0.006 | (− 0.003; 0.021) | 0.125 |
| Race/ethnicity | ||||
| White | ref | ref | ref | ref |
| Black | 0.022 | 0.015 | (− 0.007; 0.051) | 0.133 |
| Asian | − 0.012 | 0.011 | (− 0.033; 0.010) | 0.293 |
| Hispanic | 0.041 | 0.027 | (− 0.012; 0.094) | 0.127 |
| Other racial/ethnic groups | 0.040* | 0.020 | (0.002; 0.079) | 0.041 |
| Household structure: | ||||
| Total number of people in household | 0.009* | 0.005 | (0.000; 0.018) | 0.047 |
| Married and had children | ref | ref | ref | ref |
| Unmarried and had children | 0.028* | 0.013 | (0.002; 0.054) | 0.036 |
| Married and no children | 0.017 | 0.016 | (− 0.015; 0.049) | 0.307 |
| Unmarried and no children | 0.027* | 0.012 | (0.005; 0.050) | 0.018 |
| SES: | ||||
| Above-low-income household | ref | ref | ref | ref |
| Low-income household | 0.039* | 0.018 | (0.003; 0.075) | 0.036 |
| Poor household | 0.045 | 0.031 | (− 0.015; 0.106) | 0.141 |
| Educational attainment | 0.002 | 0.003 | (− 0.005; 0.009) | 0.580 |
| Housing Tenure | ||||
| Owned | ref | ref | ref | ref |
| Rented | 0.044** | 0.014 | (0.016; 0.072) | 0.002 |
| Mortgage or loan | 0.022** | 0.007 | (0.008; 0.036) | 0.002 |
| Employed for the last 7 days | − 0.070*** | 0.014 | (− 0.098; − 0.042) | < 0.0001 |
| Received free groceries or a free meal during the past 7 days | 0.090*** | 0.022 | (0.047, 0.133) | < 0.0001 |
| Health: | ||||
| General health status | − 0.068*** | 0.004 | (− 0.075, − 0.060) | < 0.0001 |
*** p < 0.001,** p < 0.01, * p < 0.05
Results presented in Table 2 were weighted based on the HPS recommended sampling weights
Inverse Gaussian distribution with the identity link function
Tables 3 and 4 report the results for Models 2–5, predicting the causes of food insecurity among those food-insecure households (n = 30,534). The results of Model 2 suggest that when all control variables were held constant, as compared to White food-insecure households, Black food-insecure households (p < 0.0001) or food-insecure households that were headed by other races/ethnicities (p = 0.006) were more likely to report that they could not afford to buy more food during the pandemic. Model 3 indicates that Asian (p < 0.0001) and Hispanic (p = 0.001) food-insecure households were more likely to report that they were afraid or did not want to go out to buy food during COVID-19 than White food-insecure households. According to Model 4, as compared to White food-insecure households, Asian food-insecure households (p = 0.003) and food-insecure households headed by other races/ethnicities (p = 0.016) were more likely to report that they could not go out to buy food due to transportation, mobility, or health issues during the pandemic. Finally, the results from Model 5 demonstrate that when compared to Black (p < 0.0001), Asian (p < 0.0001), and Hispanic (p < 0.0001) food-insecure households, White food-insecure households were significantly more likely to report that the stores did not have the food they wanted. Please see Tables 3 and 4 for detailed results of the control variables.
Table 3.
Results of the GEE models predicting the causes of food insecurity among food-insecure households during the pandemic (n = 30,534)
| Variables | Model 2 (Could not afford to buy more food) |
Model 3 (Afraid to go or did not want to go out to buy food) |
||||||
|---|---|---|---|---|---|---|---|---|
| B | SE | CI | p | B | SE | CI | p | |
| Intercept | 0.271 | 0.190 | (− 0.102; 0.644) | 0.154 | − 0.598** | 0.1952 | (− 0.980; − 0.215) | 0.002 |
|
Household food insecurity level prior to March 13, 2020 |
0.659*** | 0.046 | (0.570; 0.749) | < 0.0001 | − 0.267*** | 0.0344 | (− 0.335; − 0.200) | < 0.0001 |
| Demographic characteristics: | ||||||||
| Age | − 0.022*** | 0.002 | (− 0.027; − 0.018) | < 0.0001 | − 0.011*** | 0.0017 | (− 0.014; − 0.007) | < 0.0001 |
| Female | 0.158* | 0.078 | (0.006; 0.311) | 0.042 | 0.130* | 0.0627 | (0.007; 0.253) | 0.038 |
| Race/ethnicity | ||||||||
| White | ref | ref | ref | ref | ref | ref | ref | ref |
| Black | 0.526*** | 0.073 | (0.384; 0.668) | < 0.0001 | − 0.100 | 0.0958 | (− 0.287; 0.088) | 0.298 |
| Asian | 0.001 | 0.141 | (− 0.275; 0.278) | 0.993 | 1.303*** | 0.1220 | (1.064; 1.542) | < 0.0001 |
| Hispanic | 0.037 | 0.158 | (− 0.273; 0.348) | 0.814 | 0.378** | 0.1099 | (0.163; 0.594) | 0.001 |
| Other racial/ethnic groups | 0.265** | 0.096 | (0.076; 0.454) | 0.006 | 0.257* | 0.1270 | (0.009; 0.506) | 0.043 |
| Household structure: | ||||||||
|
Total number of people in household |
0.012 | 0.019 | (− 0.025; 0.050) | 0.518 | − 0.008 | 0.0307 | (− 0.068; 0.052) | 0.800 |
| Married and had children | ref | ref | ref | ref | ref | ref | ref | ref |
| Unmarried and had children | − 0.038 | 0.121 | (− 0.275; 0.198) | 0.751 | 0.017 | 0.0634 | (−0.107; 0.142) | 0.785 |
| Married and no children | − 0.058 | 0.121 | (− 0.295; 0.179) | 0.631 | − 0.116 | 0.0724 | (− 0.258; 0.026) | 0.109 |
| Unmarried and no children | 0.049 | 0.089 | (− 0.126; 0.224) | 0.584 | 0.150 | 0.1077 | (− 0.061; 0.361) | 0.163 |
| SES: | ||||||||
| Above-low-income household | ref | ref | ref | ref | ref | ref | ref | ref |
| Low-income household | 0.570*** | 0.069 | (0.434; 0.705) | < 0.0001 | 0.035 | 0.0787 | (− 0.119; 0.190) | 0.654 |
| Poor household | 0.515*** | 0.098 | (0.323; 0.706) | < 0.0001 | − 0.190 | 0.1860 | (− 0.555; 0.175) | 0.307 |
| Educational attainment | − 0.134*** | 0.030 | (− 0.193; − 0.076) | < 0.0001 | 0.142*** | 0.0157 | (0.111; 0.173) | < 0.0001 |
| Housing Tenure | ||||||||
| Owned | ref | ref | ref | ref | ref | ref | ref | ref |
| Rented | 0.492*** | 0.074 | (0.346; 0.637) | < 0.0001 | − 0.285* | 0.1112 | (− 0.503; − 0.067) | 0.010 |
| Mortgage or loan | 0.080 | 0.070 | (−0.057; 0.217) | 0.250 | −0.067 | 0.1059 | (− 0.275; 0.140) | 0.526 |
| Employed for the last 7 days | − 0.299* | 0.125 | (− 0.543; − 0.055) | 0.016 | − 0.042 | 0.0625 | (− 0.164; 0.081) | 0.503 |
| Received free groceries or a free meal during the past 7 days | 0.564*** | 0.150 | (0.269; 0.858) | < 0.0001 | − 0.144* | 0.0710 | (− 0.283; − 0.005) | 0.042 |
| Health: | ||||||||
| General health status | − 0.148*** | 0.033 | (− 0.213; − 0.083) | < 0.0001 | − 0.111*** | 0.0247 | (− 0.159; − 0.062) | < 0.0001 |
*** p < 0.001,** p < 0.01, * p < 0.05
Results presented in Table 3 were weighted based on the HPS recommended sampling weights
Binomial distributions with a logit link function
Table 4.
Results of the GEE models predicting the causes of food insecurity among food-insecure households during the pandemic (n = 30,534)
| Variables | Model 4 (Could not go out to buy food) |
Model 5 (The stores did not have the food I wanted) |
||||||
|---|---|---|---|---|---|---|---|---|
| B | SE | CI | p | B | SE | CI | p | |
| Intercept | − 1.832** | 0.5770 | (− 2.963; − 0.701) | 0.001 | 0.621** | 0.2154 | (− 1.043; − 0.198) | 0.004 |
| Household food insecurity level prior to March 13, 2020 | 0.011 | 0.0475 | (− 0.082; 0.104) | 0.817 | − 0.534*** | 0.0430 | (− 0.618; − 0.449) | < 0.0001 |
| Demographic characteristics: | ||||||||
| Age | − 0.005 | 0.0051 | (− 0.015; 0.004) | 0.279 | − 0.003 | 0.0024 | (− 0.008; 0.001) | 0.173 |
| Female | 0.192 | 0.0984 | (− 0.001; 0.384) | 0.052 | 0.050 | 0.0579 | (− 0.063; 0.164) | 0.386 |
| Race/ethnicity | ||||||||
| White | ref | ref | ref | ref | ref | ref | ref | ref |
| Black | − 0.164 | 0.1504 | (− 0.459; 0.131) | 0.275 | − 0.814*** | 0.1054 | (− 1.021; − 0.608) | < 0.0001 |
| Asian | 0.494** | 0.1656 | (0.169; 0.819) | 0.003 | − 1.111*** | 0.1228 | (− 1.352; − 0.870) | < 0.0001 |
| Hispanic | 0.020 | 0.1305 | (− 0.236; 0.276) | 0.879 | − 0.547*** | 0.0882 | (− 0.720; − 0.374) | < 0.0001 |
| Other racial/ethnic groups | 0.324* | 0.1348 | (0.059; 0.588) | 0.016 | − 0.266* | 0.1155 | (− 0.492; − 0.040) | 0.021 |
| Household structure: | ||||||||
|
Total number of people in household |
− 0.045 | 0.0416 | (− 0.126; 0.037) | 0.283 | 0.009 | 0.0285 | (− 0.047; 0.064) | 0.765 |
| Married and had children | ref | ref | ref | ref | ref | ref | ref | ref |
| Unmarried and had children | 0.445* | 0.2059 | (0.041; 0.848) | 0.031 | − 0.277** | 0.0890 | (− 0.452; − 0.103) | 0.002 |
| Married and no children | 0.100 | 0.1487 | (− 0.191; 0.392) | 0.500 | 0.051 | 0.1070 | (− 0.159; 0.261) | 0.635 |
| Unmarried and no children | 0.596** | 0.1777 | (0.248; 0.944) | 0.001 | − 0.242* | 0.1047 | (− 0.447; − 0.036) | 0.021 |
| SES: | ||||||||
| Above-low-income household | ref | ref | ref | ref | ref | ref | ref | ref |
| Low-income household | 0.202 | 0.1377 | (− 0.067; 0.472) | 0.141 | − 0.420*** | 0.0574 | (− 0.533; − 0.308) | < 0.0001 |
| Poor household | 0.471** | 0.1504 | (0.176; 0.766) | 0.002 | − 0.476*** | 0.1317 | (− 0.734; − 0.217) | < 0.0001 |
| Educational attainment | 0.144*** | 0.0270 | (0.091; 0.197) | < 0.0001 | 0.075*** | 0.0152 | (0.045; 0.105) | < 0.0001 |
| Housing Tenure | ||||||||
| Owned | ref | ref | ref | ref | ref | ref | ref | ref |
| Rented | 0.418*** | 0.0991 | (0.224; 0.612) | < 0.0001 | − 0.301*** | 0.0676 | (− 0.434; − 0.169) | < 0.0001 |
| Mortgage or loan | 0.246 | 0.1422 | (− 0.032; 0.525) | 0.083 | − 0.067 | 0.0817 | (− 0.227; 0.093) | 0.410 |
| Employed for the last 7 days | − 0.180* | 0.0892 | (− 0.355; − 0.006) | 0.043 | 0.567*** | 0.0826 | (0.405; 0.729) | < 0.0001 |
| Received free groceries or a free meal during the past 7 days | − 0.072 | 0.1689 | (− 0.403; 0.259) | 0.670 | − 0.239 | 0.1236 | (− 0.482; 0.003) | 0.053 |
| Health: | ||||||||
| General health status | − 0.450*** | 0.0493 | (− 0.547; − 0.353) | < 0.0001 | 0.078** | 0.0298 | (0.020; 0.136) | 0.009 |
*** p < 0.001,** p < 0.01, * p < 0.05
Results presented in Table 4 were weighted based on the HPS recommended sampling weights
Binomial distributions with a logit link function
Table 5 reports the results from Model 6, predicting the level of food security confidence among the 74,413 households. There were significant racial/ethnic findings: Black (p < 0.0001), Asian (p < 0.0001), Hispanic (p < 0.0001) respondents, and respondents from other racial/ethnic groups (p = 0.003) were all significantly less confident about their household food security for the next 4 weeks than White respondents. The results of Model 6 also suggest that respondents from households that were more food insecure prior to COVID-19 had significantly lower levels of food security confidence (p < 0.001). In terms of household structure, as compared to people who were married and had children, those who were married but without children were significantly more confident about their household food security for the next 4 weeks (p < 0.0001). For SES variables, both low-income (p < 0.0001) and poor (p < 0.0001) households had significantly lower levels of food security confidence than above-low-income households. Educational attainment (p < 0.0001) were significantly and positively associated with food security confidence. People who rented their houses/apartments (p < 0.0001), unemployed (p < 0.0001), or expected to lose their jobs (p < 0.0001) were significantly less confident about their household food security. Finally, people who self-reported as healthy were significantly more confident about their household food security for the next four weeks (p < 0.0001).
Table 5.
Results of the GEE model predicting the level of food security confidence during the COVID-19 pandemic (n = 74,413)
| Variables | Model 6 | |||
|---|---|---|---|---|
| B | SE | CI | p | |
| Intercept | 0.917*** | 0.041 | (0.838; 0.997) | < 0.0001 |
| Household food insecurity level prior to March 13, 2020 | − 0.177*** | 0.006 | (− 0.189; − 0.165) | < 0.0001 |
| Demographic characteristics: | ||||
| Age | 0.001 | 0.000 | (0.000; 0.001) | 0.123 |
| Female | − 0.012 | 0.010 | (− 0.031; 0.007) | 0.204 |
| Race/ethnicity | ||||
| White | ref | ref | ref | ref |
| Black | − 0.061*** | 0.014 | (− 0.088; − 0.033) | < 0.0001 |
| Asian | − 0.067*** | 0.010 | (− 0.087; − 0.047) | < 0.0001 |
| Hispanic | − 0.060*** | 0.008 | (− 0.077; − 0.044) | < 0.0001 |
| Other Racial/ethnic groups | − 0.053** | 0.018 | (− 0.088, − 0.017) | 0.003 |
| Household structure: | ||||
| Total number of people in household | 0.006 | 0.003 | (− 0.001; 0.011) | 0.053 |
| Married and had children | ref | ref | ref | ref |
| Unmarried and had children | − 0.016 | 0.010 | (− 0.035; 0.004) | 0.110 |
| Married and no children | 0.040*** | 0.010 | (0.021; 0.059) | < 0.0001 |
| Unmarried and no children | 0.012 | 0.009 | (− 0.005; 0.029) | 0.175 |
| SES: | ||||
| Above-low-income household | ref | ref | ref | ref |
| Low-income household | − 0.090*** | 0.009 | (− 0.108; − 0.072) | < 0.0001 |
| Poor household | − 0.101*** | 0.018 | (− 0.138; −0.065) | < 0.0001 |
| Educational attainment | 0.020*** | 0.003 | (0.014; 0.026) | < 0.0001 |
| Housing Tenure | ||||
| Owned | ref | ref | ref | ref |
| Rented | − 0.059*** | 0.016 | (− 0.090; − 0.029) | < 0.0001 |
| Mortgage | − 0.026 | 0.014 | (− 0.053; 0.000) | 0.052 |
| Employed for the last 7 days | 0.034*** | 0.006 | (0.022; 0.046) | < 0.0001 |
| You or anyone in your household might experience a loss of employment income in the next 4 weeks because of the COVID-19 pandemic | − 0.152*** | 0.009 | (− 0.169; −0.134) | < 0.0001 |
| Received free groceries or a free meal during the last 7 days | − 0.030* | 0.013 | (− 0.055; −0.006) | 0.015 |
| Health: | ||||
| General health status | 0.061*** | 0.004 | (0.054; 0.068) | < 0.0001 |
*** p < 0.001,** p < 0.01, * p < 0.05
Results presented in Table 5 were weighted based on the HPS recommended sampling weights
Inverse Gaussian distribution with the log link function
Discussion
Race/ethnicity is a key factor contributing to the production of food insecurity [3, 22, 24]. There are few, if any, published studies using empirical evidence to systematically examine racial/ethnic disparities in household food insecurity in the context of the COVID-19 pandemic. This critical knowledge gap exists, despite the reality that millions of American households are now struggling to feed their families. This paper contributes to the small number of studies documenting the characteristics of US household food insecurity during COVID-19 [42], and we are the first to focus on racial/ethnic disparities.
To test the hypothesis, six GEE models were estimated. We first noted that during the pandemic, the level of household food insecurity did not significantly differ across racial/ethnic groups, when demographic characteristics, household structure, SES, and health were controlled. This finding initially appears to contradict earlier studies suggesting that racial/ethnic minorities, especially Blacks and Hispanics, are disproportionately affected by food insecurity [3, 23]. A possible explanation is that with a noticeable increase of White food-insecure households during COVID-19, the racial/ethnic gap seems less evident. In other words, we found no support for the hypothesis when all households were included in the model.
However, the hypothesis holds when we examined the four different causes of food insecurity among households self-reported as food insecure during the pandemic. Specifically, as compared to White food-insecure households, Black food-insecure households were more likely to report that they could not afford to buy more food during the pandemic. This finding is unsurprising in light of previous research that the individuals and families from Black communities are often at the risk of suffering food insecurity [3, 22] due to their social and economic disadvantages, such as lower SES [52, 53], racial discrimination [31], and residential segregation [54–56]. The current study contributes further evidence demonstrating that the gap between Black and White households in food insecurity is persistent throughout the pandemic. One putative explanation is that as compared to Whites and other racial/ethnic groups, Blacks are the most likely to work in industries that are affected by the pandemic, which worsened the long-standing economic hardship Black families have been facing [32].
Part of the substantive novelty of this study lies in our findings on Asian and Hispanic households. We discovered that Asian food-insecure households were more afraid to go out to buy food than White food-insecure households. Not being able to leave the house to purchase food could negatively affect the food supply for the family. Because during the early pandemic period, online grocery stores were overloaded and often failed to meet the sudden demand [57, 58]. Many households, especially those with less income and education, could not afford or did not have the knowledge or skills to purchase groceries online. We are unaware of previous findings on the impacts of COVID-19 on food insecurity among Asian households. However, there is evidence indicating that racial hatred and discrimination towards Asian Americans have been increasing since the beginning of the pandemic. Often referred to as the “Chinese virus” or “kung flu,” COVID-19 was used to rationalize anti-Asian xenophobia, stoking public hysteria and racist attacks. Since mid-March, for example, an incident-reporting center founded by the Asian Pacific Policy and Planning Council has received more than 1800 reports of pandemic-related harassment or violence targeting Asian Americans across multiple states [59]. Those racially driven attacks could very likely instill fear among Asian communities. During the COVID-19 crisis, people are already reluctant to leave their homes because of the fear of contracting the coronavirus, while Asian families are experiencing additional anxiety about dealing with racist incidents, which intensified their food insecurity.
We also noted that as compared to White food-insecure households, Asian food-insecure households had higher odds of reporting that they could not go out to buy food because they had transportation, mobility, or health issues. Although Asian Americans, especially first-generation immigrants, have shown to experience transportation barriers and health disparities [60, 61], those factors have not been linked to food insecurity among Asian households. Indeed, the lack of attention paid to the food security of Asian communities likely relates to the model minority myth, which assumes that Asian Americans have unparalleled achievements in education and success [62] and thus suffer little health disparities. Yet, studies have demonstrated that such a myth has led to internalized racialism and further resulting in adverse environmental and health outcomes (e.g., 51, 65, 66). Becerra et al. [63] argued that Asian Americans are facing an overlooked burden of food insecurity; thus, there is an imperative need for more research on understanding the barriers to ensuring food security among Asian families. Following this line of thinking, our study documented the specific food barriers Asian households are facing during the pandemic.
Similarly, Hispanic food-insecure households also reported that they were afraid or did not want to leave their homes to purchase food. The food security gap between Hispanic and White populations is long-standing [2, 23, 64], and previous research suggests that deportation fears might be one of the leading causes of food insecurity among Hispanic households, especially those with immigrant members [65, 66]. During the coronavirus outbreak, federal, state, and local authorities have become more involved in enforcing immigration restrictions, and those efforts have largely targeted Hispanic communities [67, 68]. Hence, it is possible that as the fears of deportation, family separation, and police harassment intensified during the pandemic, many Hispanic families did not feel comfortable to leave their homes to buy food.
As mentioned, the prevalence of food insecurity has rapidly increased among White households. In stark contrast to Black, Asian, or Hispanic food-insecure households, White food-insecure households were more likely to report that stores did not have the food they wanted. What can be made of this finding? Clearly, it implies that the main food access barrier that White households were facing during COVID-19 was more likely to be temporary. During the early pandemic period, stores experienced shortages for certain food items due to logistics issues, market shifts, labor shortages, or customers’ hoarding behaviors. However, there is evidence suggesting that grocery stores’ supply shortages have been greatly improved since May [69]. In contrast, the burdens of food insecurity among minority households will last longer because they are caused by systemic economic hardship, interpersonal racial discrimination, and structural racism. Consequently, as suggested by our last model, all racial/ethnic minority groups were significantly less confident about their household food security for the next 4 weeks than Whites. During this ongoing crisis, minorities were more stressed about feeding their families because their struggle with food was not just temporarily triggered by COVID-19; rather, it is “a symptom of a social disease” [16], deeply rooted within our social systems.
A number of studies have identified age, household size, poverty, employment status, housing tenure, and health as key factors in the production of household food insecurity [2, 3, 35–38, 70]. Those findings were confirmed in our study. We also found that only a small proportion of households in our sample reported receiving free food: among all households, 7% received free food; and among food-insecure households, 10% received free food. As the pandemic persists, more coordinated efforts are desperately needed to provide food support to American families, especially those experiencing food insecurity.
Study Limitations and Avenues for Further Research
The results of this study should be interpreted in the context of limitations. First, food security is defined as a multidimensional concept internationally. According to the Committee on World Food Security (CFS), food security exists “when all people at all times have physical and economic access to sufficient, safe and nutritious food to meet their dietary needs and food preferences for an active and healthy life” [71]. According to the CFS, there are four dimensions of food security: availability, access, stability, and utilization. Following the USDA’s definition of food security [2], the current paper focuses on the second dimension, food access. Future studies could explore other dimensions of food security in the context of COVID-19. Second, the USDA used a Rasch measurement model to develop its food security scale [72] which is a unidimensional item-response-theory model based on all HFSSM items. Due to the HPS’ different food insecurity measure, we were unable to estimate the Rasch measurement model in this study. Hence, our estimates on the prevalence of household food insecurity are not strictly comparable to estimates provided by the USDA. Third, this study does not account for nutritional outcomes of food insecurity. During the pandemic, less nutrient-rich foods have become cheaper than more nutritious foods, so people with less resources might switch to those more affordable but less healthy foods [69]. In other words, even when people were able to buy the food they wanted, they might still suffer negative nutritional consequences. However, since the HPS did not ask food prices or the types of food people purchased, we could not investigate nutritional disparities among racial/ethnic groups during the pandemic in this study. Fourth, due to the limitation of the HPS data, we were unable to disaggregate Asian and Hispanic categories into subgroups based on country of origin (e.g., Chinese, Vietnamese, Mexican, Cuban), which might mask substantial diversity that exists within Asian and Hispanic populations and conceal disparate food insecurity risks experienced by particular subgroups. For example, a previous study found the highest prevalence of food insecurity among Vietnamese Americans and the lowest prevalence among Japanese Americans [63]. Fifth, based on previous research and existing evidence, we provided explanations on why Asian and Hispanic households might be afraid to leave their homes to buy food. However, we acknowledge that in the HPS questionnaire, respondents were not asked why they were afraid or did not want to go out to buy food. The direct links between COVID-19, racial discrimination, mobility, and food insecurity need to be future investigated by future studies. Sixth, COVID-19 is an unpredictable and fast-moving crisis, so it is possible that some of our findings might become outdated as the pandemic evolves. However, we believe that documenting and understanding people’s struggle with food during the period of a major crisis is itself important.
This study also illuminated several future research directions. In this paper, we rely on the cross-sectional research design and week-one HPS microdata. Future researchers can use the weekly released HPS data to conduct longitudinal studies to investigate how patterns suggested by our study vary over time. Further, the first-week HPS questionnaire did not include specific questions on receipt of Food Stamps or access to the Coronavirus Aid, Relief, and Economic Security (CARES) stimulus package. Yet, access to social protection plays a vital role in reducing household food insecurity. Interestingly, our results indicated that there was no significant difference in food insecurity between poor and above-low-income households. We hypothesize that receiving Food Stamps or the CARES stimulus package might have protected poor families from food insecurity during COVID-19. Recent findings suggest that the CARES Act has the potential to reduce poverty in the USA [73, 74]. Future research should explore whether and how the CARES Act affected household food insecurity during the pandemic. Moreover, future researchers should seek to collect data on household geographic locations and investigate how location-related variables (e.g., rural vs. urban) affect household food insecurity during COVID-19. Factors at the state level should also be taken into consideration. Finally, the effects of interactions between demographic characteristics, household structure, SES, and health variables on household food insecurity should be future investigated.
Conclusions
The coronavirus pandemic crisis, and the resulting economic crash, has exposed and exacerbated food injustice in American society. This paper provides one of the first assessments of household food insecurity across racial/ethnic groups in the USA during the period of a pandemic, with the HPS being one of the few to provide national-level data on the social impacts of COVID-19. To ensure adequate food availability for all households, policymakers and local officials should accelerate efforts to improve the capacity of the food supply chain, increase the number of food assistance programs, and make those programs more accessible. At the same time, concerted action is needed to ensure food equality across all racial/ethnic groups. For example, legislators could consider providing income support for households that are facing financial hardship, especially those from Black communities, and urgent steps should be taken to prevent racial attacks and xenophobic violence targeting Asian and Hispanic populations. Without such action, the current health crisis could become a social crisis that will have long-term consequences for American families.
Availability of Data and Material
Not applicable.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Code Availability
Not applicable.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Danielle Xiaodan Morales, Email: xdeng2@utep.edu.
Stephanie Alexandra Morales, Email: smorales12@miners.utep.edu.
Tyler Fox Beltran, Email: tfbeltran@miners.utep.edu.
References
- 1.Anderson SA. Core indicators of nutritional state for difficult-to-sample populations. J Nutr. 1990;120:1555–1600. doi: 10.1093/jn/120.suppl_11.1555. [DOI] [PubMed] [Google Scholar]
- 2.Coleman-Jensen, A, Rabbitt M, Gregory CA, Singh A. Household food security in the United States in 2018. ERR-270, U.S. Department of Agriculture, Economic Research Service. 2019. https://www.ers.usda.gov/webdocs/publications/94849/err-270.pdf?v=7154.9.
- 3.Bruening M, MacLehose R, Loth K, Story M, Neumark-Sztainer D. Feeding a family in a recession: food insecurity among Minnesota parents. Am J Public Health. 2012;102:520–526. doi: 10.2105/AJPH.2011.300390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duffy M, Jackson TL, Cooper T. Food insecurity among Rhode Island adults. R I Med J. 2019:46–8. [PubMed]
- 5.Franklin B, Jones A, Love D, Puckett S, Macklin J, White-Means S. Exploring mediators of food insecurity and obesity: a review of recent literature. J Community Health. 2013;37:253–264. doi: 10.1007/s10900-011-9420-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leung CW, Epel ES, Willett WC, Rimm EB, Laraia BA. Household food insecurity is positively associated with depression among low-income supplemental nutrition program participants and income-eligible nonparticipants. J Nutr. 2014;145:622–627. doi: 10.3945/jn.114.199414. [DOI] [PubMed] [Google Scholar]
- 7.Siefert K, Heflin CM, Corcoran ME, Williams DR. Food insufficiency and the physical and mental health of low-income women. Women Health. 2001;32:159–177. doi: 10.1300/J013v32n01_08. [DOI] [PubMed] [Google Scholar]
- 8.Laraia BA, Siega-Riz AM, Gundersen C, Dole N. Psychosocial factors and socioeconomic indicators are associated with household food insecurity among pregnant women. J Nutr. 2006;136:177–182. doi: 10.1093/jn/136.1.177. [DOI] [PubMed] [Google Scholar]
- 9.Pryor L, Lioret S, Van der Waerden J, Fombonne E, Falissard B, Melchior M. Food insecurity and mental health problems among a community sample of young adults. Soc Psychiatr Epidemiol. 2016;51:1073–1081. doi: 10.1007/s00127-016-1249-9. [DOI] [PubMed] [Google Scholar]
- 10.Stuff JE, Casey PH, Szeto KL, Gossett JM, Robbins JM, Simpson PM, Connell C, Bogle ML. Household food insecurity is associated with adult health status. J Nutr. 2004;134:2330–2335. doi: 10.1093/jn/134.9.2330. [DOI] [PubMed] [Google Scholar]
- 11.Casey PH, Szeto KL, Robbins JM, Stuff JE, Connell C, Gossett JM, Simpson PM. Child health-related quality of life and household food security. Arch Pediatr Adolesc Med. 2005;159:51–56. doi: 10.1001/archpedi.159.1.51. [DOI] [PubMed] [Google Scholar]
- 12.Cook JT, Frank DA, Berkowitz C, Black MM, Casey PH, Cutts DB, Meyers AF, Zaldivar N, Skalicky A, Levenson S, Heeren T, Nord M. Food insecurity is associated with adverse health outcomes among human infants and toddlers. J Nutr. 2004;134:1432–1438. doi: 10.1093/jn/134.6.1432. [DOI] [PubMed] [Google Scholar]
- 13.Grineski SE, Morales DX, Collins TW, Rubio R. Transitional dynamics of household food insecurity impact children’s developmental outcomes. J Dev Behav Pediatr. 2018;39:715–725. doi: 10.1097/DBP.0000000000000598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jyoti DF, Frongillo EA, Jones SJ. Food insecurity affects school children’s academic performance, weight gain, and social skills. J Nutr. 2005;135:2831–2839. doi: 10.1093/jn/135.12.2831. [DOI] [PubMed] [Google Scholar]
- 15.Shepard DS, Setren E, Cooper D. Hunger in America [Internet]. Center for American Progress. 2011 [Cited 8 July 2020]. Available from https://www.americanprogress.org/issues/poverty/reports/2011/10/05/10504/hunger-in-america/.
- 16.Roncarolo F, Potvin L. Food insecurity as a symptom of a social disease: analyzing a social problem from a medical perspective. Can Fam Phys. 2016;62. [PMC free article] [PubMed]
- 17.Rolling updates on coronavirus disease (COVID-19) [Internet]. World Health Organization. 2020 [Cited 8 July 2020]. Available from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen.
- 18.Regional emergency response to mitigate the impact of COVID-19 [Internet]. United Nations [Cited 16 July 2020]. 2020.
- 19.Fields S. 44% of Americans fear they won’t be able to afford food, poll finds [Internet]. Marketplace. 2020 [Cited 14 July 2020]. Available from https://www.marketplace.org/2020/05/07/44-of-americans-fear-they-wont-be-able-to-afford-food-poll-finds/.
- 20.Fields S. “Record levels” of food insecurity in the U.S. because of COVID-19 [Internet]. Marketplace. 2020 [Cited 14 July 2020]. Available from https://www.marketplace.org/2020/05/22/record-levels-of-food-insecurity-in-the-u-s-because-of-covid-19/.
- 21.Wolfson J, Leung C. Food insecurity and COVID-19: disparities in early effects for US adults. Nutr. 2020;12. 10.3390/nu12061648. [DOI] [PMC free article] [PubMed]
- 22.Nam Y, Huang J, Heflin C, Sherraden M. Racial and ethnic disparities in food insufficiency: evidence from a statewide probability sample. J Soc Soc Work Res. 2015;6:201–228. doi: 10.1086/681574. [DOI] [Google Scholar]
- 23.Nord M, Coleman-Jensen A, Andrews M, Carlson S. Household food security in the United States in 2009. ERR-108, U.S. Department of Agriculture, Economic Research Service. 2010. https://www.ers.usda.gov/webdocs/publications/44776/7024_err108_1_.pdf?v=4464.8.
- 24.Odoms-Young A, Bruce MA. Examining the impact of structural racism on food insecurity: implications for addressing racial/ethnic disparities. Fam Community Health. 2018;41:S3–S6. doi: 10.1097/FCH.0000000000000183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ribar DC, Hamrick KS. Dynamics of poverty and food sufficiency. FANRR-36, U.S. Department of Agriculture, Economic Research Service. 2003. https://www.ers.usda.gov/webdocs/publications/46753/15939_fanrr36_1_.pdf?v=2571.1.
- 26.Shapiro TM. The hidden cost of being African American: how wealth perpetuates inequality. USA: Oxford University Press; 2004. [Google Scholar]
- 27.Bartfeld J, Dunifon R, Nord M, Carlson S. What factors account for state-to-state differences in food security? ERR. EIB-20, USDA. 2006.
- 28.Gundersen C. Measuring the extent, depth, and severity of food insecurity: an application to American Indians in the USA. J Popul Econ. 2008;21:191–215. doi: 10.1007/s00148-007-0152-9. [DOI] [Google Scholar]
- 29.Kaiser L, Baumrind N, Dumbauld S. Who is food-insecure in California? Findings from the California women’s health survey, 2004. Public Health Nutr. 2007;10:574–581. doi: 10.1017/S1368980007382542. [DOI] [PubMed] [Google Scholar]
- 30.Yu M, Lombe M, Nebbitt VE. Food stamp program participation, informal supports, household food security and child food security: a comparison of african american and caucasian households in poverty. Child Youth Serv Rev. 2010;32:767–773. doi: 10.1016/j.childyouth.2010.01.015. [DOI] [Google Scholar]
- 31.Burke MP, Jones SJ, Frongillo EA, Fram MS, Blake CE, Freedman DA. Severity of household insecurity and lifetime racial discrimination among African-American households in South Carolina. Ethn Health. 2018;23:276–292. doi: 10.1080/13557858.2016.1263286. [DOI] [PubMed] [Google Scholar]
- 32.Bottemiller Evich H. Stark racial disparities emerge as families struggle to get enough food [Internet]. POLITICO. 2020 [Cited 2020 July 8]. Available from: https://www.politico.com/news/2020/07/06/racial-disparities-families-struggle-food-348810.
- 33.Kurtzleben D. Job losses higher among people of color during coronavirus pandemic. In: NPR. 2020 [Cited 15 July 2020]. Available from: https://www.npr.org/2020/04/22/840276956/minorities-often-work-these-jobs-they-were-among-first-to-go-in-coronavirus-layo.
- 34.Weller C. Systemic racism makes Covid-19 much more deadly for African-Americans. Forbes. 2020 [Cited 10 July 2020] Available from https://www.forbes.com/sites/christianweller/2020/06/18/systemic-racism-makes-covid-19-much-more-deadly-for-african-americans/#44c2a5257feb.
- 35.Arteaga I, Potochnick S, Parsons S. Decomposing the household food insecurity gap for children of U.S.-born and foreign-born hispanics: evidence from 1998 to 2011. J Immigr Minority Health. 2017;19:1050–1058. doi: 10.1007/s10903-017-0561-0. [DOI] [PubMed] [Google Scholar]
- 36.Huet C, Ford JD, Edge VL, Shirley J, King N, Harper SL. Food insecurity and food consumption by season in households with children in an Arctic city: a cross-sectional study. BMC Public Health. 2017;17:578. doi: 10.1186/s12889-017-4393-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Raj A, McDougal LP, Silverman JG. Gendered effects of siblings on child malnutrition in South Asia: cross-sectional analysis of demographic and health surveys from Bangladesh, India, and Nepal. Matern Child Health J. 2015;19:217–226. doi: 10.1007/s10995-014-1513-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rubio RL, Grineski SE, Morales DX, Collins TW. The role of parents’ nativity in shaping differential risks of food insecurity among US first graders. Matern Child Health J. 2019;23:910–918. doi: 10.1007/s10995-018-02717-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hadley C, Lindstorm D, Tessema F, Belachew T. Gender Bias in the food insecurity experience of Ethiopian adolescents. Soc Sci Med. 2007;66:427–438. doi: 10.1016/j.socscimed.2007.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Casey P, Goolsby S, Berkowitz C, Frank D, Cook J, Cutts D, Black MM, Zaldivar N, Levenson S, Heeren T, Meyers A. Children’s sentinel nutritional assessment program study group. Maternal depression, changing public assistance, food security, and child health status. Pediatr. 2004;113:298–204. doi: 10.1542/peds.113.2.298. [DOI] [PubMed] [Google Scholar]
- 41.Knowles M, Rabinowich J, De Cuba SE, Cutts DB, Chilton M. “Do you wanna breathe or eat?”: parent perspectives on child health consequences of food insecurity, trade-offs, and toxic stress. Matern Child Health J. 2016;20:25–32. [DOI] [PMC free article] [PubMed]
- 42.Fields JF, Hunter-Childs J, Tersine A, Sisson J, Parker E, Velkoff V, Logan C, Shin H. Design and operation of the 2020 household pulse survey, 2020. U.S. Census Bureau. Forthcoming. 2020. Accessed 07 Jul 2020.
- 43.Schanzenbach D, Pitts A. Food insecurity in the census household pulse survey data tables. Institute for Policy Research 2020; 1–15. Available from https://www.ipr.northwestern.edu/documents/reports/ipr-rapid-research-reports-pulse-hh-data-1-june-2020.pdf.
- 44.Diggle PJ, Heagerty P, Liang K, Zegger SL. Analysis of longitudinal data. 2. Oxford: Oxford University Press; 2002. [Google Scholar]
- 45.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. doi: 10.1093/biomet/73.1.13. [DOI] [Google Scholar]
- 46.Zeger S, Liang K. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. doi: 10.2307/2531248. [DOI] [PubMed] [Google Scholar]
- 47.Zorn C. Generalized estimating equation models for correlated data: a review with applications. Am J Pol Sci. 2001;45:470–490. doi: 10.2307/2669353. [DOI] [Google Scholar]
- 48.Collins TW, Grineski SE, Morales DX. Environmental injustice and sexual minority health disparities: a national study of inequitable health risks from air pollution among same-sex partners. Soc Sci Med. 2017;191:38–47. doi: 10.1016/j.socscimed.2017.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Morales DX, Grineski SE, Collins TW. Increasing research productivity in undergraduate research experiences: exploring predictors of collaborative faculty–student publications. CBE—Life Sci Educ. 2017;16:ar42. doi: 10.1187/cbe.16-11-0326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grineski S, Morales DX, Collins T, Hernandez E, Fuentes A. The burden of carcinogenic air toxics among Asian Americans in four US metro areas. Popul Environ. 2019;40:257–282. doi: 10.1007/s11111-018-0308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Garson GD. Generalized linear models and generalized estimating equations. Asheboro:Statistical Associates Publishing; 2012. Accessed 23 Jul 2020.
- 52.DeNavas-Walt C, Proctor BD, Smith JC. Income, poverty, and health insurance coverage in the United States: 2012. US Census Bureau Current Population Reports. 2013:60–245 https://www.census.gov/prod/2013pubs/p60-245.pdf.
- 53.Kena G, Aud S, Johnson F, Wang X, Zhang J, Rathbun A, Wilkinson-Flicker S, Kristapovich P. The condition of education 2014. NCES 2014–083. 2014. https://eric.ed.gov/?id=ED545122.
- 54.Dutko P, Ver Ploeg M, Farrigan T. Characteristics and influential factors of food deserts. Economic Research Service. ERR-140, USDA. 2012.
- 55.Grigsby-Toussaint DS, Lipton R, Chavez N, Handler A, Johnson TP, Kubo J. Neighborhood socioeconomic change and diabetes risk: findings from the Chicago childhood diabetes registry. Diabetes Care. 2010;33:1065–1068. doi: 10.2337/dc09-1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the US. Am J Prev Med. 2009;36:74–81. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 57.Budiu R. Online shopping for food and groceries during Covid-19: workflow issues impact the Ecommerce customer experience [Internet]. Nielsen Norman Group. 2020 [Cited 20 Sept 2020]. Available from https://www.nngroup.com/articles/food-shopping-covid19/.
- 58.Cannuscio CC, Tappe K, Hillier A, Buttenheim A, Karpyn A, Glanz K. Urban food environements and residents’ shopping behaviors. Am J Prev Med. 2013;45:606–614. doi: 10.1016/j.amepre.2013.06.021. [DOI] [PubMed] [Google Scholar]
- 59.Kambhampaty AP. ‘I will not stand silent.’ 10 Asian Americans reflect on racism during the pandemic and the need for equality [Internet]. TIME. 2020 [Cited 14 July 2020]. Available from https://time.com/5858649/racism-coronavirus/.
- 60.Chen MS., Jr Cancer health disparities among Asian Americans: what we know and what we need to do. Cancer. 2005;104:2895–2902. doi: 10.1002/cncr.21501. [DOI] [PubMed] [Google Scholar]
- 61.Lee S, Juon HS, Martinez G, Hsu CE, Robinson ES, Bawa J, et al. Model minority at risk: expressed needs of mental health by Asian American young adults. J Community Health. 2009;34. 10.1007/s10900-008-9137-1. [DOI] [PMC free article] [PubMed]
- 62.Chou RS, Feagin JR. The myth of the model minority: Asian Americans facing fascism. 2. New York: Routledge; 2015. [Google Scholar]
- 63.Becerra MB, Mshigeni SK, Becerra BJ. The overlooked burden of food insecurity among Asian Americans: results from the California health interview survey. Int J Environ Res Public Health. 2018;15:1684. doi: 10.3390/ijerph15081684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Carney M. Compounding crises of economic recession and food insecurity: a comparative study of three low-income communities in Santa Barbara County. Agric Human Values. 2012;29:185–201. doi: 10.1007/s10460-011-9333-y. [DOI] [Google Scholar]
- 65.Landale NS, Hardie JH, Oropesa RS, Hillemeier MM. Behavioral functioning among Mexican-origin children: does parental legal status matter? J Health Soc Behav. 2015;56:2–18. doi: 10.1177/0022146514567896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yoshikawa H. Immigrants raising citizens: undocumented parents and their children. New York: Russell Sage Foundation; 2011. [Google Scholar]
- 67.Chishti M, Pierce S. Crisis within a crisis: immigration in the United States in a time of COVID-19 [Internet]. The Immigrant Learning Center. 2020 [Cited 8 July 2020]. Available from https://www.immigrationresearch.org/node/2978.
- 68.Loweree J, Reichlin-Melnick A, Ewing W. The Impact of COVID-19 on Noncitizens and Across the U.S. Immigration System [Internet]. In American Immigration Council. 2020. Available from https://www.americanimmigrationcouncil.org/research/impact-covid-19-us-immigration-system. Accessed 15 Jul 2020.
- 69.Laborde D, Martin W, Swinnen J, Vos R. COVID-19 risks to global food security. Science. 2020;369:500–2. [DOI] [PubMed]
- 70.Gundersen C, Ziliak J. Research report: childhood food insecurity in the U.S.: trends, causes, and policy options. Futur Child. 2014; 1–19. Available from www.jstor.org/stable/26304695. Accessed 05 Aug 2020.
- 71.Committee on World Food Security. Coming to terms with terminology [Internet]. In Food and Agriculture Organization. 2012; 1–14. Available from http://www.fao.org/3/MD776E/MD776E.pdf.
- 72.Bickel G, Nord M, Price Cristofer, Hamilton W, Cook J. Guide to measuring household food security. USDA. 2000; 1–76.
- 73.Jeehoon H, Meyer BD, Sullivan JX. Income and poverty in the COVID-19 pandemic. Brook Pap Econ Act 2020. Available from https://www.brookings.edu/wp-content/uploads/2020/06/Han-et-al-conference-draft.pdf.
- 74.Parolin Z, Curran M, Wimer C. The CARES ACT and poverty in the COVID-19 crisis: promises and pitfalls of the recovery rebates and expanded unemployment benefits. Center Pov Soc Pol. 2020;4:1–18. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.