Abstract
Objective
The primary aim of the present study was to compare the ‘cross-legged foetal sitting position’ (CFSP) with the ‘sitting foetal position’ (SFP) sonographically. The secondary aim was to compare their comfort.
Methods
A randomised, consecutive controlled, single-blinded trial was performed in Yeditepe University. A total of 50 healthy volunteers were included in the study. Exclusion criteria were body mass index (BMI) >40 kg m-2, lumbar hernia, scoliosis, history of spine surgery, lower back pain or trauma, especially pelvic or knee problems related to arthropathy and not able to do one/both of the two position techniques. The two positioning techniques were evaluated by ultrasonography (USG) and 5-point Numerical Rating Scale (5-NRS) patient satisfaction of comfort questionnaire. Seven outcomes via USG were evaluated, subcutaneous tissue (ST), skin to spinous process (S–SP), transverse diameters of right and left paraspinal muscles (RPM and LPM), interspinous gap opening (ISGO), mean of bilateral paraspinal muscle (MPM) and CFSP–SFP change (CFSP–SFP). Stretcher comfort, position comfort, lumbar comfort (LC) and abdominal comfort (AC) were evaluated by participants with the 5-NRS.
Results
In the CFSP, the mean ST and S–SP were significantly (p<0.0001) shorter, and LPM, RPM and MPM were significantly (p<0.0001) wider. The mean ISGO in the CFSP was significantly (p<0.0001) broader. The CFSP was significantly more comfortable than the SFP according to the LC (p=0.02). Only ISGO was found to be significantly broader in the male participant group (p=0.01) and in the BMI ≥25 group (p=0.02) according to CFSP–SFP.
Conclusion
Considering all ultrasonographic anatomical measurements and according to the 5-NRS related to LC, the CFSP appears to be more advantageous than the SFP as a neuraxial positioning technique.
Keywords: Conduction anaesthesia, diagnostic imaging, lumbar vertebrae, patient positioning, patient satisfaction
Introduction
The failure rate of conduction anaesthesia (neuraxial anaesthesia) is still a concern and ranges from 2% to 20% (1). Success is related to a calm and comforted patient and a skilled professional operator. Therefore, to ease the needle replacement, the patient and operator must cooperate for the body position. A successful neuraxial anaesthesia implementation requires a proper body positioning which provides an adequate interspinous gap opening (ISGO). A prosperous positioning of the patient widens the ISGO that ensures an increased chance of successful needle placement (2). Therefore, alternative positioning techniques are still being described (3). The sitting foetal position (SFP) technique is one of the best, by providing not only an adequate ISGO but also patient comfort (4).
For the last two decades, various studies have been published about the techniques of neuraxial anaesthesia and the aids (tools, land-marking and levelling techniques by assessment or by ultrasound imaging (USI) and positioning techniques) (5, 6). USI before or during the implementation of neuraxial anaesthesia has been used since the 1990s (7). As anatomical landmarks based on physical assessment were shown to be misleading in >30% of the cases, USI of adult or paediatric patients during implementation has become a necessity for proper identification (8).
The primary aim of the present study was to compare two different neuraxial anaesthesia positioning techniques, the ‘cross-legged foetal sitting position’ (CFSP) and the SFP, according to lumbar anatomical measurements evaluated via ultrasonography (USG). The secondary aim was to compare the comfort of the two positions by 5-point Numerical Rating Scale (5-NRS) patient satisfaction of comfort questionnaire. The hypothesis is that the CFSP could be more comfortable than the SFP. In addition, the CFSP could be as advantageous as the SFP regarding the sonographic comparison of the L4–L5 vertebrae interspinous gap, the surrounding tissues and the muscles.
Methods
Ethical approval for this prospective, randomised, consecutive controlled clinical trial (no.: 885) was provided by the Yeditepe University Clinical Trials Ethical Committee, Istanbul, Turkey (Chairperson Prof T. Çelik) on 16 May 2018. This study is registered at ClinicalTrials.gov (NCT03741465) in November 2018.
Clinical trial procedures were explained briefly to 150 healthy respondents by the senior author. A pilot study was made with 10 (5 male and 5 female) volunteers. Written informed consent was obtained from each participant. Diagnostic data were as shown mean age 31.5±4.9 standard deviation (SD) years, mean weight 64±22.6 SD kg, mean height 171±10 SD cm and mean body mass index (BMI) 21.7±5.8 SD kg m−2. However, a sample size of 38 was determined by the ultrasonographic ISGO measurements of the two positioning techniques with millimetres (CFSP: 21.5±3.7 SD mm and SFP: 17.8±2.3 SD mm), within the inputs of α err prob=0.05 and power (1−β err prob)=0.95. To comply with the secondary aim of the study, we decided to include 48 participants to represent a population of 50 people with a 95% confidence level and 3% confidence interval, in pursuance of Cohen, Manion and Morrison’s table of sample size. Fifty participants were included in the study for compensation of the possible losses. Systematic random sampling was performed according to the number of neuraxial anaesthesia that is performed in the clinic in a year (approximately 600 patients); the sample size required for a random sample of those 600 patients with 95% confidence level was a minimum of 235 related to Cohen, Manion and Morrison’s table of sample size (9), and the frequency interval is 2.6, which rounds up to 3. Therefore, volunteers were picked to the trial by the senior author as 1st, 4th, 7th, 10th and so on till the desired sample has been achieved. Written informed consent was obtained from all participants who were assigned to the trial by the senior author.
Healthy participants between aged 18 and 45 years who were able to do two positioning techniques (the CFSP and the SFP) were selected according to the trial eligibility criteria. Participants who have a BMI >40 kg m−2, lumbar hernia, scoliosis, a history of spine surgery, lower back pain or trauma, especially pelvic or knee problems related to arthropathy, and who could not be able to do one or both of the two neuraxial position techniques were excluded from the study. Eventually, none of the participants left the trial or were discriminated.
Demographic data of the participants were recorded as age, height, weight, BMI and gender. The trial was performed in USG rooms of the Radiology Department, consisting of the same conditions as darkness, stretcher and ultrasound device (General Electric LOGIQ E9 (CISPR11 Group 1 Class A), Wauwatosa, WI, USA) and probe (9 L-broadband linear array probe), with 2.4–10 MHz.
Each participant sat on the stretcher in two different neuraxial anaesthesia positioning techniques (SFP and CFSP) one after another. In the CFSP, the participants sat on the same part of the stretcher with legs crossed. The forearms of the participants were on the lap, the hands were on the knees and the position was completed with the back curved in the foetal position (Figure 1). In the SFP, the participants sat on the middle side of the stretcher facing the wall of the sonography room and turned their backs to the consultant radiologist with the legs hanging freely. The forearms of the participants were on the lap, and the hands were on the knees. The position was completed with the back curved in the foetal position (Figure 2).
Figure 1. a, b.
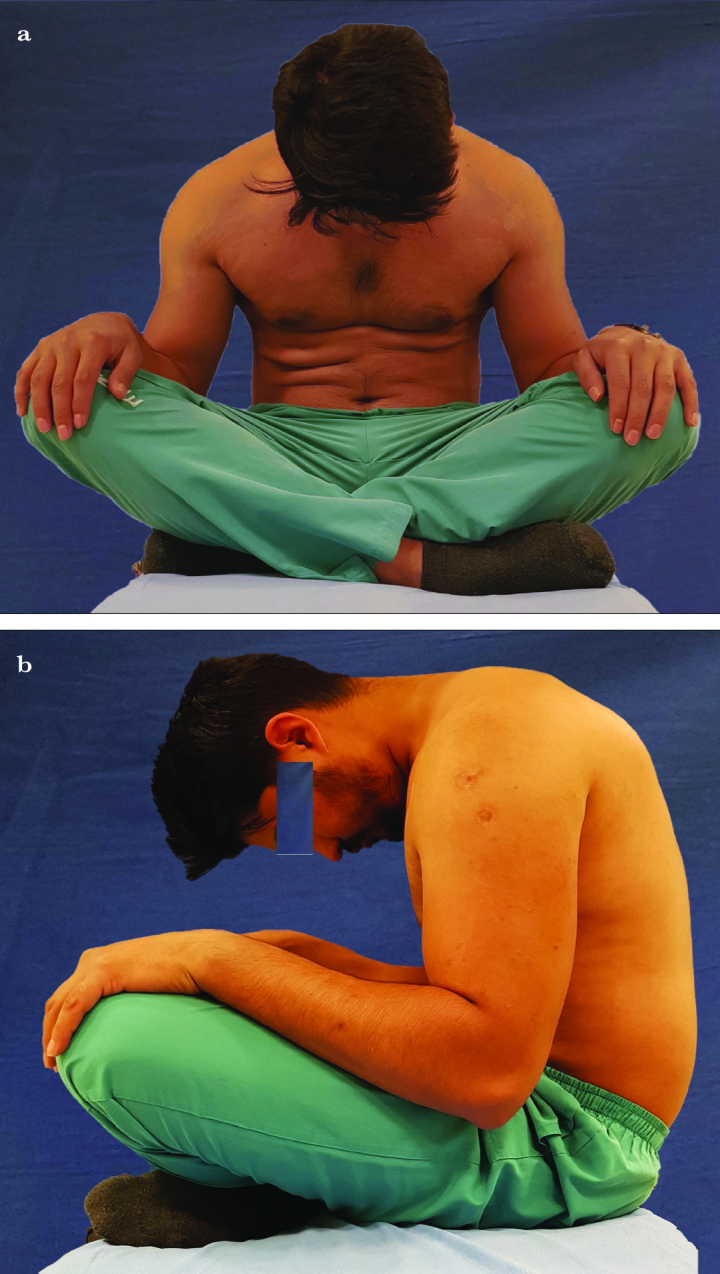
The cross-legged foetal sitting position
Forearms are on the lap and hands on the knees, completed with the back curved in the foetal position
Figure 2.
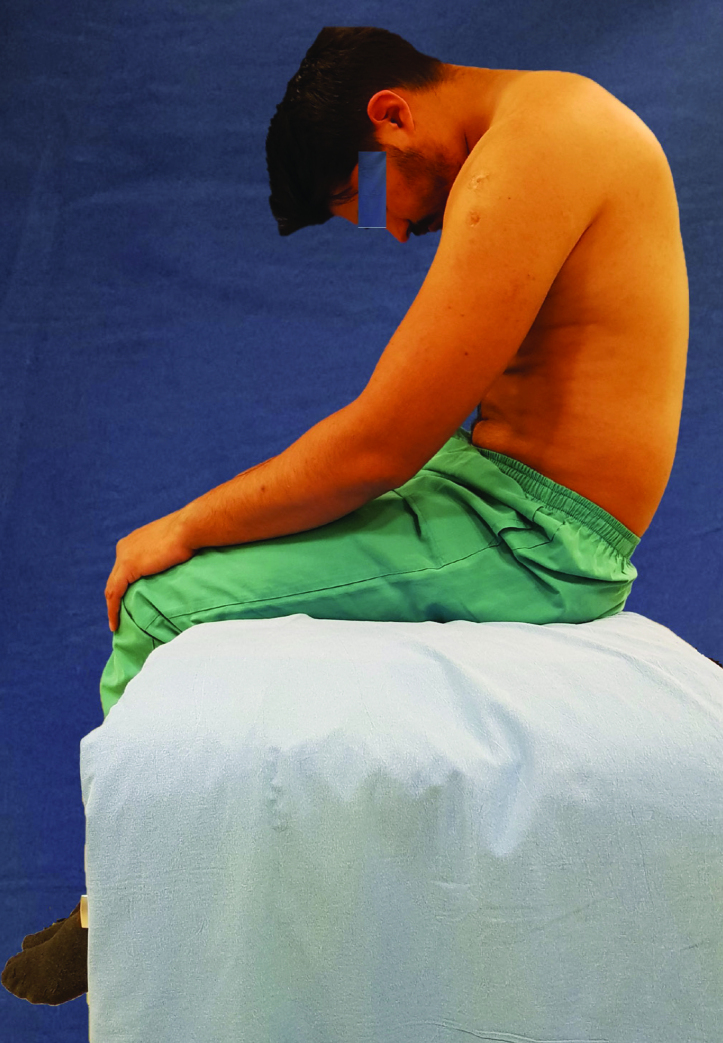
The sitting foetal position
Forearms are on the lap and hands on the knees, completed with the back curved in the foetal position while the legs are hanging freely
The senior author had every participant perform the correct neuraxial positioning and checked out the participant’s consistency before the radiological examination. All sonographic examinations were made with the same device and by the same consultant doctor of the Radiology Department who did not know the aim of the current trial. After hydrophilic anti-allergic ultrasound transmission gel (Aquasonic 100; Parker Laboratories Inc., Fairfield, NJ, USA) was applied to the lower back of the participant skin, scanning was started from the sacrum to the cephalad, aiming to identify the best scene of the L4–L5 in a depth of 5 cm. Five different parameters were recorded during ultrasonographic evaluation of the two positioning techniques, including subcutaneous tissue (ST), skin to spinous process (S–SP), transverse diameters of left and right paraspinal muscles (LPM and RPM) in the axial plane (Figure 3) by the paramedian approach and ISGO in the sagittal plane (Figure 4). The mean of bilateral paraspinal muscle (MPM) was calculated from outcomes.
Figure 3. a–c.
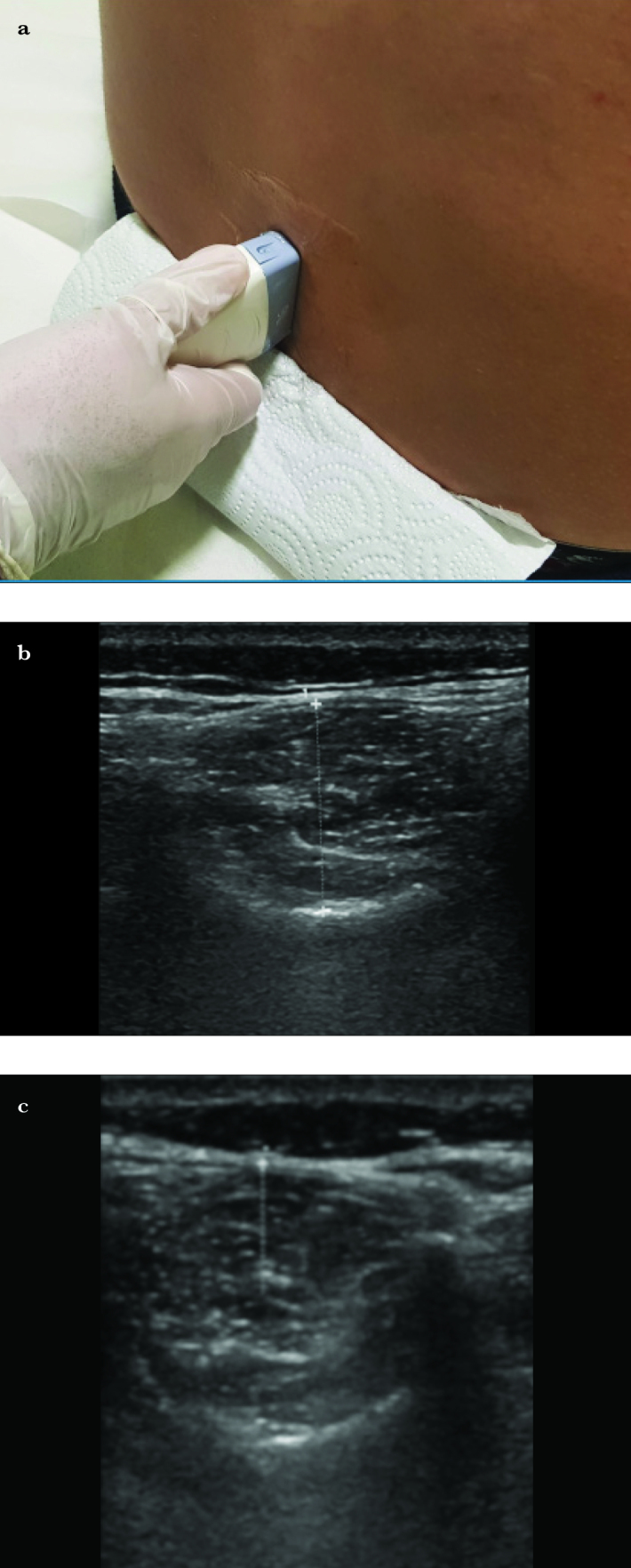
Ultrasound imaging in the axial plane
Left paraspinal muscle and right paraspinal muscle evaluation
Figure 4. a, b.
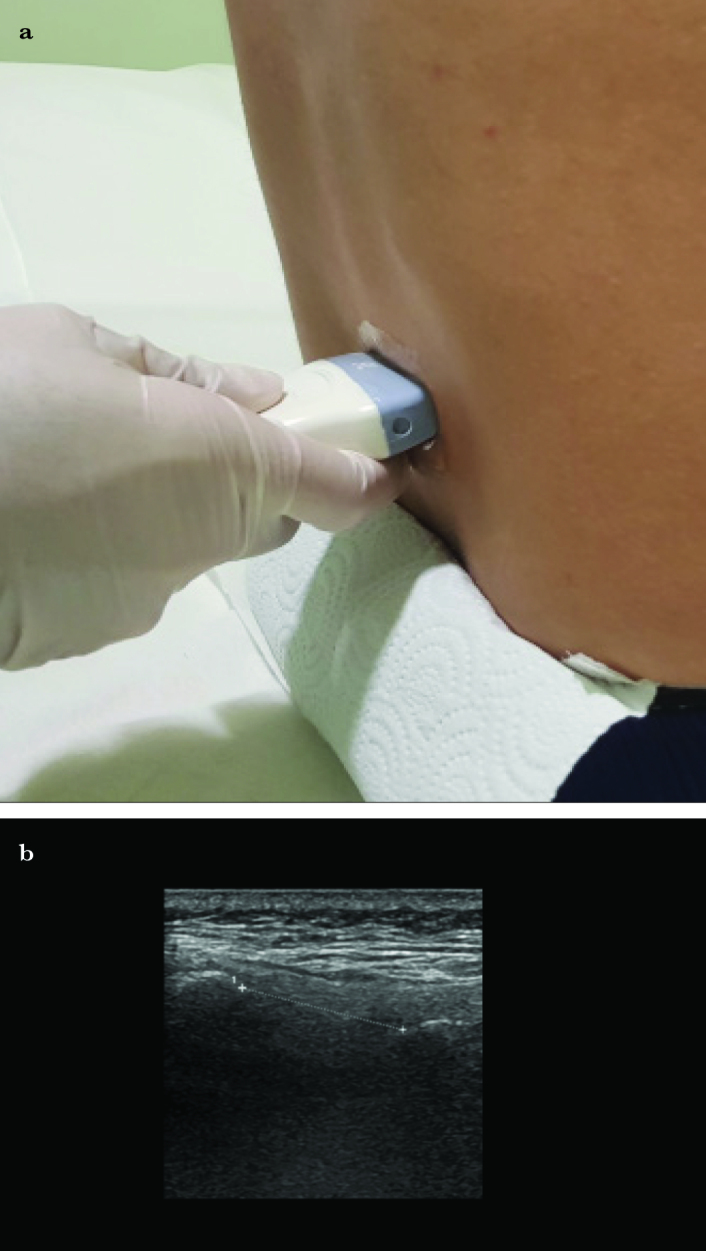
Ultrasound imaging in the sagittal plane
Interspinous gap opening evaluation
The 5-point NRS was used for measurement of comfort in each positioning technique. The participants compared each position after sonographic examination from 1 to 5, with 1 representing the least comfortable level as ‘poor’, 3 as ‘normal’ and 5 representing the most comfortable level as ‘very good’. The participants evaluated stretcher comfort (SC), position comfort (PC) (the SFP and CFSP comfort), lumbar comfort (LC) and abdominal comfort (AC).
Statistical analysis
IBM Statistical Packages for the Social Sciences 22.0 programme (IBM SPSS Corp.; Armonk, NY, USA) was used for analysis. Descriptive statistics were expressed as minimum–maximum, SD, median, frequency and rate values. The distribution of the variables was measured by the coefficient of variation, skewness–kurtosis, histogram, detrended and the normality test of Shapiro–Wilk. Data were determined as parametric if three or more over five positivity occurred in the tests mentioned above. The t-test of the paired sample was used to compare the LPM, RPM, MPM and ISGO sonographic results of the two positioning techniques. The Wilcoxon test was used to compare the ST and S–SP sonographic results of the two positioning techniques. Sonographic measurements of the two positioning techniques were calculated as mean difference and named as ‘CFSP–SFP change’ (CFSP–SFP).
The Mann–Whitney U test was used to compare the changes of the two positioning techniques’ sonographic measurements according to gender and BMI. The marginal homogeneity test was used to compare the comfort of the two positioning techniques according to the 5-point NRS. A p-value of <0.05 was considered to be statistically significant.
Results
Demographic characteristics of 50 participants who were evaluated in the two positioning techniques ultrasonographically from June 2018 to November 2018 are shown in Table 1. The mean ST and S–SP measurements in the CFSP technique were significantly (p<0.0001) shorter than those in the SFP technique as follows: ST (5.6±2.6 mm and 5.9±2.6 mm, respectively) and S–SP (11.0±5.5 mm and 11.8±5.6 mm, respectively). The mean measurements of the LPM, RPM and MPM in the CFSP technique were significantly (p<0.0001) broader than those in the SFP technique as follows: LPM (21.3±6.2 mm and 17.5±5.7 mm, respectively), RPM (21.0±6.1 mm and 17.1±5.4 mm, respectively) and MPM (21.1±6.1 mm and 17.3±5.6 mm, respectively). The mean of ISGO measurement in the CFSP technique was significantly (p<0.0001) wider than that in the SFP technique as follows: 22.3±4.2 mm and 19.0±3.0 mm, respectively (Table 2).
Table 1.
Demographic data of the participants
| n=50 | Median (min–max) | Mean±SD |
|---|---|---|
|
| ||
| Age, years | 28 (19–45) | 30.2±7.2 |
| Weight, kg | 72 (47–125) | 73.3±17.9 |
| Height, cm | 170.5 (156–187) | 171.9±0.1 |
| BMI, kg m−2 | 24.1 (17.5–38.8) | 24.6±4.8 |
n: number of participants; min: minimum; max: maximum; SD: standard deviation
Table 2.
Ultrasonographic measurements
| Mean±SD (min–max) | p | |
|---|---|---|
|
| ||
| ST | ||
| SFP | 5.9±2.6 (2–14.4) | 0.0001w |
| CFSP | 5.6±2.6 (1.8–15.3) | |
| S–SP | ||
| SFP | 11.8±5.6 (4.7–37) | 0.0001w |
| CFSP | 11±5.5 (4.6–38.5) | |
| LPM | ||
| SFP | 17.5±5.7 (7.3–32.8) | 0.0001t |
| CFSP | 21.3±6.2 (9.2–35.8) | |
| RPM | ||
| SFP | 17.1±5.4 (7–30) | 0.0001t |
| CFSP | 21±6.1 (8.9–35.3) | |
| MPM | ||
| SFP | 17.3±5.6 (7.2–31.4) | 0.0001t |
| CFSP | 21.1±6.1 (9.1–35.6) | |
| ISGO | ||
| SFP | 19±3 (12–25.5) | 0.0001t |
| CFSP | 22.3±4.2 (13.4–35.4) | |
min: minimum; max: maximum; SD: standard deviation; t: paired t-test; w, Wilcoxon test; SFP: sitting foetal position; CFSP: cross-legged foetal sitting position; ST: subcutaneous tissue; S–SP: skin to spinous process; LPM: left paraspinal muscle; RPM: right paraspinal muscle; MPM: mean of bilateral paraspinal muscle; ISGO: interspinous gap opening
According to the 5-point NRS comfort results, there was no significant difference of the SC, AC and PC between the CFSP technique and the SFP technique (p>0.05). The CFSP technique was significantly more comfortable than the SFP technique related to the LC (p=0.02) (Table 3).
Table 3.
The 5-point NRS comfort questionnaire scores
| Comfort evaluation of SFP and CFSP related to four different parameters | Median (min–max) | p |
|---|---|---|
|
| ||
| SC | ||
| SFP | 4.0 (1.0–5.0) | 0.25M-h |
| CFSP | 4.0 (1.0–5.0) | |
| PC | ||
| SFP | 4.0 (1.0–5.0) | 0.06M-h |
| CFSP | 4.0 (1.0–5.0) | |
| LC | ||
| SFP | 4.0 (1.0–5.0) | *0.02M-h |
| CFSP | 4.0 (1.0–5.0) | |
| AC | ||
| SFP | 4.0 (1.0–5.0) | 0.09M-h |
| CFSP | 4.0 (1.0–5.0) | |
p<0.05.
NRS: Numerical Rating Scale; min: minimum; max: maximum; M-h: marginal homogeneity test; SFP: sitting foetal position; CFSP: cross-legged foetal sitting position; SC: stretcher comfort; PC: position comfort; LC: lumbar comfort; AC: abdominal comfort
CFSP–SFP was compared according to the BMI (<25 to ≥25 kg/m2) and gender groups. The male participant group’s only ISGO measurement was found to be significantly wider (p=0.012) than the female group (Table 4). Only ISGO measurement was found to be significant (p=0.02) in the BMI ≥25 group (Table 5). In both of the BMI-related groups and the gender-related groups, the 5-point NRS results were determined to be nonsignificant (p>0.05).
Table 4.
CFSP–SFP change according to gender
| CFSP-SFP | Male (n=25) | Female (n=25) | p | ||
|---|---|---|---|---|---|
|
| |||||
| Mean±SD | Median | Mean±SD | Median | ||
|
| |||||
| ST | −0.37±0.51 | −0.4 | −0.4±0.55 | −0.4 | 0.984m |
| S–SP | −0.48±1.35 | −0.4 | −1.04±1.33 | −0.8 | 0.143m |
| LPM | 3.47±1.82 | 3.2 | 4±2.35 | 3.4 | 0.472m |
| RPM | 3.68±1.72 | 3.3 | 4.22±2.19 | 4 | 0.473m |
| MPM | 3.58±1.74 | 3.3 | 4.11±2.23 | 3.95 | 0.491m |
| ISGO | 2.42±1.95 | 2.2 | 4.18±2.73 | 3.7 | *0.01m |
p<0.05.
n: number; SD: standard deviation; m: Mann–Whitney U test; CFSP–SFP: cross-legged foetal sitting position to sitting foetal position change; ST: subcutaneous tissue; S–SP: skin to spinous process; LPM: left paraspinal muscle; RPM: right paraspinal muscle; MPM: mean of bilateral paraspinal muscle; ISGO: interspinous gap opening
Table 5.
CFSP–SFP change according to body mass index
| CFSP-SFP | BMI <25 kg m−2 | BMI ≥25 kg m−2 | p | ||
|---|---|---|---|---|---|
|
| |||||
| Mean±SD | Median | Mean±SD | Median | ||
|
| |||||
| ST | −0.39±0.4 | −0.4 | −0.38±0.74 | −0.55 | 0.624m |
| S–SP | −0.61±0.83 | −0.4 | −1.09±2.07 | −0.75 | 0.154m |
| LPM | 3.55±1.98 | 3.2 | 4.14±2.35 | 3.9 | 0.486m |
| RPM | 3.81±2 | 3.3 | 4.25±1.92 | 4.25 | 0.308m |
| MPM | 3.68±1.96 | 3.3 | 4.19±2.09 | 4.25 | 0.339m |
| ISGO | 2.75±2.21 | 2.2 | 4.47±2.76 | 4.3 | *0.02m |
p<0.05.
m: Mann–Whitney U test; BMI: body mass index; CFSP–SFP: cross-legged foetal sitting position to sitting foetal position change; ST: subcutaneous tissue; S–SP: skin to spinous process; LPM: left paraspinal muscle; RPM: right paraspinal muscle; MPM: mean of bilateral paraspinal muscle; ISGO: interspinous gap opening
Discussion
The main findings of the current study were about the anatomical measurements of the two neuraxial positioning techniques which were measured via USI. ISGO, LPM, RPM and MPM measurements in the CFSP were wider, whereas ST and S–SP measurements were thinner than those in the SFP. Moreover, the participants were more comfortable in the CFSP than in the SFP in comparison to LC. Although AC and PC scores in the 5-point NRS of comfort were clinically relevant in the CFSP, they were not statistically significant.
Additionally, the male participant group and the BMI ≥25 group had a broader ISGO in the CFSP. To the best of our knowledge, this is the first study that includes paraspinal muscle measurements by 9L linear array probe via USG and a consultant radiologist performed sonographic measurements. Paraspinal muscle relaxation, as shown sonographically as paraspinal muscles transverse diameter widening, appears to be also related to LC.
Ultrasonography is very useful for neuraxial anaesthesia implementations. According to a recent meta-analysis published by Perlas et al. (10), neuraxial USG significantly improves the precision and efficacy of neuraxial anaesthesia techniques. Although there are more reliable and sensitive imagining modalities than sonography, such as magnetic resonance, computed tomography or plain radiography, none of them is as safe and practical as USG. USG could also be performed by other medical doctors, such as anaesthesiologists.
Ultrasonography provides better diagnostic view and could be able to show the anatomic landmarks and measurements related to spine anatomy in skilled and experienced consultant’s hands, even if the patient is overweight or pregnant (11, 12). Shaikh et al. (13) reported in their meta-analysis that USI and land-marking are performed by a study investigator who had adequate expertise in USG. The reliability of USG is related to the clinical knowledge of the investigator; therefore, in the current study, USI was performed by a consultant radiologist. USI with the 9L linear array probe that was used in the current study is available for superficial tissue imaging, providing a better diagnostic anatomical evaluation, especially in small depths. There was no need for a curved probe to achieve an appropriate USI in >5 cm depth because there was no insertion of a needle or placement of a catheter in the present study.
Several kinds of neuraxial positioning techniques, such as lateral, traditional sitting, hamstring stretch, sitting legs parallel on the table, pendant, Oxford and mid-calf, have been recently evaluated by USG (3, 4, 14–16). Within those positioning techniques, the traditional sitting position (TSP) appears to be a better choice for ease and success of the manoeuvre. The only difference between the TSP and the SFP was that the legs were not supported; therefore, the knees were not flexed. The SFP was used by Dimaculangan et al. (4) and compared to five other positions. In their study, they found that sitting foetal, lying foetal and hugging a ball positions provided the widest L3–L4 interlaminar openings. Therefore, the CFSP was compared to the SFP sonographically but from the L4 to L5 interlaminar openings.
Only one study compared the success of spinal needle placement between the crossed-leg sitting position (CLSP) and the TSP. In their research, Manggala et al. (15) kept the patients in the CLSP by hugging a pillow. They used neither an imaging technique nor a patient comfort score. Although the success rate of the first attempt in the CLSP was higher than that in the TSP (63% and 56%, respectively), they determined that the rate of successful spinal needle placement was not significantly different. They said that even though the CLSP was more stable and relieved abdominal muscles better than the TSP, the position would not be so comfortable if the patient had a lower back problem. In contrast to CLSP, the participants sat cross-legged with their arms on the lap and their hands on the knees with the back curved in the foetal position in the CFSP technique.
According to the results of the 5-point NRS of comfort, the comparison of the two positioning techniques related to SC (the survey control question) was not significant as to be expected. While performing USG, the CFSP was thought to be less comfortable than the SFP due to the thinner ST. However, the LC was significantly better in the CFSP, which could be explained by paraspinal muscle relaxation, as shown sonographically as paraspinal muscles transverse diameter widening, and it appears to be related to LC.
In addition to all of the findings above, by relaxation of the paraspinal muscles, the CFSP provides patient comfort which would achieve the patient compatibility, a better stabilisation at the position that would ease the manipulation of the needle insertion. The paraspinal muscle relaxation and the contraction of interspinous ligaments in the CFSP could also be a benefit for a qualified diagnostic view, ensuring a straight anatomical land-marking. Facilitation of the neuraxial anaesthesia manoeuvre in the CFSP might increase the success of the blockade compared to other positioning techniques, relevant to the broader ISGO.
The present study has several limitations. The study population did not reflect the real community due to BMI >40 kg m−2 and >45 years of age. Participants who could have lower back or knee problems were excluded. The new CFSP technique was not compared to other traditional positioning techniques, such as the lateral foetal position. Single masking was made to the outcomes assessor (the consultant radiologist). The consultant did not know which position was for the control and which one was for the study, but the consultant saw the positions because there is no way to hide the positions of the participants. Although there are some limitations, the strengths of the study are nearly unique; to the best of our knowledge, there is no neuraxial positioning technique described before as the CFSP, and there is no study that includes a comparison of the paraspinal muscle measurements via USI in different neuraxial positioning techniques. The participants did all detailed comfort evaluations via the 5-point NSR of comfort after each positioning technique. In this current prospective study, ultrasonographic measurements were performed by a consultant radiologist M.D., and the sample size of the study was adequate. Further studies should be performed about the comfort and the success of the CFSP technique in elderly, overweight patients.
Conclusion
All ultrasonographic measurements of the CFSP were more convenient than those of the SFP in all of the participants. The CFSP is more comfortable than the SFP regarding LC. The CFSP appears to be advantageous, in patients without back, hip and knee problems, as a neuraxial anaesthesia positioning technique due to the broader ISGO which increases the success of the blockade. The decrease in the depth between the ST and the spinous process could also be beneficial while performing neuraxial anaesthesia in overweight patients.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Yeditepe University (no.: 885).
Informed Consent: Written informed consent was obtained from each participant who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – F.F.K., E.K.; Design – F.F.K.; Supervision – F.F.K., N.K., Ö.K.; Resources – F.F.K., E.K.; Materials – F.F.K., E.K.; Data Collection and/or Processing – F.F.K., E.K.; Analysis and/or Interpretation – F.F.K., N.K., Ö.K.; Literature Search – F.F.K., N.K., Ö.K.; Writing Manuscript – F.F.K., N.K.; Critical Review – F.F.K., Ö.K.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Perna P, Gioia A, Ragazzi R, Volta CA, Innamorato M. Can pre-procedure neuroaxial ultrasound improve the identification of the potential epidural space when compared with anatomical landmarks? A prospective randomized study. Minerva Anestesiol. 2017;83:41–9. doi: 10.23736/S0375-9393.16.11399-9. [DOI] [PubMed] [Google Scholar]
- 2.Shankar H, Rajput K, Murugiah K. Correlation between spinous process dimensions and ease of spinal anaesthesia. Indian J Anaesth. 2012;56:250–4. doi: 10.4103/0019-5049.98769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schultz J, Njaa M, Spahn T, Auyong D, Habib A, Panni M. Mid-calf position-an improved technique to place neuraxial anaesthesia. Br J Anaesth. 2006;97:583–4. doi: 10.1093/bja/ael231. [DOI] [PubMed] [Google Scholar]
- 4.Dimaculangan DP, Mazer JA, Maracaja-Neto LF. Sonographic evaluation of lumbar interlaminar space opening in a variety of patient body positions for optimal neuraxial anesthesia delivery. J Clin Anesth. 2016;34:159–5. doi: 10.1016/j.jclinane.2016.03.045. [DOI] [PubMed] [Google Scholar]
- 5.Chin KJ, Karmakar MK, Peng P. Ultrasonography of the Adult Thoracic and Lumbar Spine for Central Neuraxial Blockade. Anesthesiology. 2011;114:1459–85. doi: 10.1097/ALN.0b013e318210f9f8. [DOI] [PubMed] [Google Scholar]
- 6.Grau T. The evaluation of ultrasound imaging for neuraxial anesthesia. Can J Anesth. 2003;50(Suppl 1):30. doi: 10.1007/BF03018153. [DOI] [Google Scholar]
- 7.Bonazzi M, Bianchi De Grazia L, Di Gennaro S, Lensi C, Migliavacca S, Marsicano M, et al. Ultrasonography-guided identification of the lumbar epidural space. Minerva Anestesiol. 1995;61:201–5. [PubMed] [Google Scholar]
- 8.Duniec L, Nowakowski P, Kosson D, Łazowski T. Anatomical landmarks based assessment of intravertebral space level for lumbar puncture is misleading in more than 30% Anaesthesiol Intensive Ther. 2013;45:1–6. doi: 10.5603/AIT.2013.0001. [DOI] [PubMed] [Google Scholar]
- 9.Cohen L, Manion L, Morrison . Research Methods in Education. Sixth Edition. 2007. p. 104. [Google Scholar]
- 10.Perlas A, Chaparro L, Chin K. Lumbar Neuraxial Ultrasound for Spinal and Epidural Anesthesia. Obstetric Anesthesia Digest. 2016;36:126–7. doi: 10.1097/01.aoa.0000489444.91016.8c. [DOI] [PubMed] [Google Scholar]
- 11.Srinivasan KK, Iohom G, Loughnane F, Lee PJ. Conventional Landmark-Guided Midline Versus Preprocedure Ultrasound-Guided Paramedian Techniques in Spinal Anesthesia. Anesth Analg. 2015;121:1089–6. doi: 10.1213/ANE.0000000000000911. [DOI] [PubMed] [Google Scholar]
- 12.Locks GD, Almeida MC, Pereira AA. Use of the Ultrasound to Determine the Level of Lumbar Puncture in Pregnant Women. Rev Bras Anestesiol. 2010;60:13–9. doi: 10.1590/S0034-70942010000100002. [DOI] [PubMed] [Google Scholar]
- 13.Shaikh F, Brzezinski J, Alexander S, Arzola C, Carvalho JC, Beyene J, et al. Ultrasound Imaging for Lumbar Punctures and Epidural Catheterizations. Obstetric Anesthesia Digest. 2014;34:71–2. doi: 10.1097/01.aoa.0000446285.45372.0a. [DOI] [PubMed] [Google Scholar]
- 14.Sandoval M, Shestak W, Stürmann K, Hsu C. Optimal patient position for lumbar puncture, measured by ultrasonography. Emerg Radiol. 2004;10:179–81. doi: 10.1007/s10140-003-0286-3. [DOI] [PubMed] [Google Scholar]
- 15.Manggala SK, Tantri AR, Satoto D. Comparison of Successful Spinal Needle Placement Between Crossed-Leg Sitting Position and Traditional Sitting Position in Patients Undergoing Urology Surgery. Anesth Pain Med. 2016;6:e39314. doi: 10.5812/aapm.39314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Soltani Mohammadi S, Piri M, Khajehnasiri A. Comparing Three Different Modified Sitting Positions for Ease of Spinal Needle Insertion in Patients Undergoing Spinal Anesthesia. Anesth Pain Med. 2017;7:e55932. doi: 10.5812/aapm.55932. [DOI] [PMC free article] [PubMed] [Google Scholar]


