Highlights
-
•
Digital health tool has been employed to increase access to care for the patient with SUD during COVID 19 pandemic.
-
•
E-consult, a mobile-friendly tool, connects remote health care providers (HCPs) with addiction specialists.
-
•
Consultation for the cases, as well as educative materials, was offered to the HCPs.
-
•
This asynchronous telepsychiatry may be more suited for a busy specialist from a developing country like India.
Keywords: Telepsychiatry, Substance use disorders, COVID 19, Health care providers (HCPs)
Abstract
Objectives
The COVID 19 pandemic has created challenges in providing timely care for patients and families with Substance Use disorders (SUDs). With the difficulties in face-to-face consultations because of social distancing measures, telepsychiatry services can be beneficial. The study proposes implementing an e-consult for SUD management and measuring its acceptability among the health care providers (HCPs) in India.
Methods
The mobile-based e-consult for SUD, connecting HCPs with addiction specialists, was implemented during the COVID lockdown period in India from 25 March to 31 May (71 days). A total of 153 HCPs, i.e., doctors, nurses, counselors, consulted for 110 cases of SUD. Sixty-eight provided feedback by filling the survey form derived from the Service User Technology Acceptability Questionnaire (SUTAQ).
Result
More than 60% of HCPs reported overall high satisfaction. More than 98% providers reported high acceptability concerning"access to specialist care," "trusted to work appropriately", "saving time," "would like torecommend to others," easier to get touch with a specialist." The doctors reported significantly high acceptability about "access to specialist care," "satisfied with recommendations,"recommend to others" compared to other HCPs.
Conclusion
During COVID 19 pandemic lockdown in India, e-consult was an acceptable tool in managing SUDs. The majority of HCPs could discuss their cases with addiction experts. There is a need to expand this further in other mental health conditions.
1. Introduction
The COVID 19 pandemic continues to create havoc across the world, including India. Psychological symptoms relating to COVID-19 have been on the rise. There is a report of increased suicide rates, substance use disorders, domestic abuse, anxiety, and depressive disorders across the world (Tandon, 2020a, 2020b). With the difficulties in face-to-face consultations, telepsychiatry services can be an appropriate and practical strategy for the support of patients, family members, and health service providers during this pandemic (Ransing et al., 2020).
Telepsychiatry is broadly divided into traditional synchronous telepsychiatry (STP) and asynchronous telepsychiatry [ATP]. Simultaneous or live technologies (like video conferencing or phone calls) connect providers and patients in real-time for direct care delivery. Asynchronous telepsychiatry (ATP) transmits clinical data from a primary care provider or patient to a psychiatrist through secure electronic communication. It thereby allows the specialist to review the data, i.e., images, electronic health records, video recording, etc. at a later point (Forum, 2017). There are numerous studies on telepsychiatry's effectiveness in various mental health conditions like anxiety, depression, PTSD, eating disorder, etc (Hilty et al., 2015). Still, there is minimal literature on telemedicine delivered Substance use disorder (SUD) treatment. Lewei (Allison) Lin et al. (Lin et al., 2019), in a recent review, found 13 studies on tele-SUD, of which there were seven randomized controlled trials (including several pilots), one quasi-experimental research, two non-randomized pilot studies, and three retrospective studies (Lin et al., 2019).
Despite the potential for telepsychiatry delivered SUD treatment, especially during COVID 19, many countries were not entirely prepared to adopt this resource (Ramalho et al., 2020). In most settings, it was mainly limited to private practice, and there was no adequate training (Ramalho et al., 2020). SUDs is a growing public health problem in India (Murthy et al., 2010). The prevalence of harmful or dependent alcohol use requiring treatment is estimated to be 5.2%, or 5.7 crore individuals. About one crore each of cannabis and opioid harmful use or dependent require treatment (Ambekar et al., 2019).The treatment gap for SUD care is reported as high as 75% in India (Ambekar et al., 2019).
During the nationwide COVID 19 lockdown period, the local and interstate transportation was closed to contain virus transmission. Lockdown is defined as an emergency measure in which individuals are restricted from certain areas in an attempt to control exposure or transmission of disease. Hence, people with SUDs could not come to treatment centers, and many tertiary centers were closed or also converted to COVID care facility. Many patients develop complicated alcohol withdrawal (Narasimha et al., 2020) as well as could not assess the long term treatment like opioid substitution therapy (Arya and Gupta, 2020).
Considering the need, the Centre of Addiction Medicine, NIMHANS, initiated an e-consultation portal between the HCPs and Addiction Specialists. There are no reported existing telemedicine services for SUD in India. The telemedicine guidelines were gazetted and legalized recently in March 2020 by the Ministry of Health and Family Welfare, Govt of India (MOHFW, 2020). It has described the modes of communication, i.e., text/video/audio, time of notifications, real-time or emails, the purpose of the consult, i.e., first consult or follow up consult, and individuals involved in the consultation, i.e., patient to doctor or doctor to doctor, etc (Ghosh et al., 2020).
Since 2014, NIMHANS Digital Academy (NDA) has been involved in capacity building for the remote HCPs in the management of addiction and mental health by using the tele-ECHO model (Chand et al., 2014; Mehrotra et al., 2018; Sagi et al., 2018). There were more than seven thousand HCPs connected through NDA (Ganesh et al., 2020; Gangadhar, 2019).
The objectives of the current study were: (1) to employ a tele-SUD intervention by using e-consult, an asynchronous telepsychiatry between HCPs and addiction specialists (2) To measure its acceptability among the end-users, i.e., health care providers (HCPs).
2. Methodology
2.1. Design
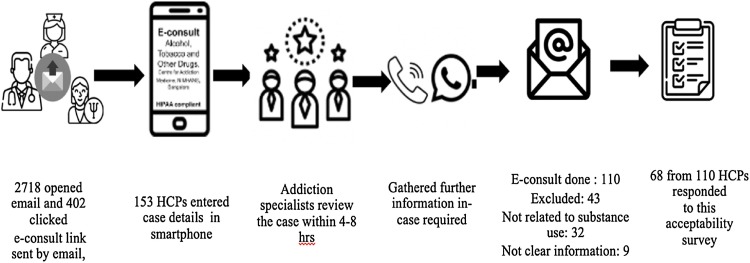
An asynchronous telepsychiatry platform, i.e., e-consult for SUD, was developed using a secure and mobile-friendly electronic platform (Fig. 1 ). An e-consult is an asynchronous consultative communication between health care providers with a specialist over a secured electronic health record or web-based platform to obtain rapid input and often prevent the need for a face-to-face patient visit (Vimalananda et al., 2020). It consists of case consultations as well as sharing of personalized educative materials between HCP and specialists (Vimalananda et al., 2015). The details of the step of development have already been published (Ganesh et al., 2020).
Fig. 1.
Flow of the events.
The e-consult consisted of 13 questions and two sections. The first part was information about the HCP, place, email, and consent for teleconsultation. Documented consent is mandatory for the teleconsultation between a doctor and another medical specialist (MOHFW, 2020). The second section consisted of the patient's socio-demographic details, the reason for consultation, substance use pattern (in the last three months), comorbid medical or psychiatric illness, etc. The doctors can also upload or share the screenshot of the past treatment details into the e-consult form. It was advised not to seek consultation for emergency cases.
2.2. Procedure
On 26 March, two days into the complete lockdown, we sent out the email with e-consult link to 7411 HCPs, i.e., 3959 docs, 1191 nurses & 2261 counselors, from the NDA database. The emails were transmitted by the bulk mail services of the NDA to the subscribers i.e. HCPs. This service also provides the information to the sender about the number of emails opened, clicked orbounced. The receiver can unsubscribe at any time. We conformed to the telemedicine practice guideline, India, during this consultation process (MOHFW, 2020).
Following e-consultation, all HCPs received a questionnaire on the acceptability of this telepsychiatry model. There is no consensus related to the definition of acceptability in mobile health (mHealth) or telehealth research. Often acceptability has been equated to satisfaction. A survey form was used for this study to assess acceptability, and this was derived from the Service User Technology Acceptability Questionnaire (SUTAQ) (Hirani et al., 2017). The SUTAQ has been used to measure acceptability and identify the characteristics of persons who were likely to reject technological health services. The questionnaire has a total of 22 items rated on a 6-point Likert scale covering domains such as accessibility, comfort, usability, privacy and security, confidentiality, satisfaction,convenience, health benefits, and self-care. The wording of the 22 items in both positive and negative, thus reducing related biases. Each subscale's result indicates the degree of average internal agreement to it (6 = strong agreement and 1 = strong disagreement). The intermediate value 3.5 is a point of neutrality (Dario et al., 2016).
The original SUTAQ is primarily meant for assessment of the acceptability of health technology, i.e., tracker, health app, etc (Newman et al., 2011; Torbjørnsen et al., 2018). Hence, following multiple iterations with two subject specialists and two technology experts, twelve out of 22 items were selected for this study (Appendix 1: supplementary).
Each health provider was sent three emails and one phone call to facilitate the submission of the survey form following completion of e-consultation. The institute ethics review committee had approved this study.
2.3. Analysis
The data were checked for normality distribution by visual inspection of the histogram, Q-Q plot, kurtosis, skewness, and Shapiro-Wilk's test. The data was not following a normal distribution. Hence median was taken for analysis. Mann Whitney U test was used for between-group comparison. We compared the median score of SUTAQ items among the Doctors (n = 38) and Counsellors/Nurses (N = 30).
3. Results
Two thousand seven hundred eighteen (36.68 %) out of 7411 opened the email. Among those who opened, 402 (14.79 %) clicked on the e-consult link at least once. In total, 153 (5.6 %) used e-consult serviced during the study period, i.e., 71 days of nationwide lockdown. About 38.05 % of those who visited the e-consult page used this service. Sixty-eight out of 110 HCPs i.e. 61.8 % filled up the acceptability for the e-consult survey (Fig. 1)
3.1. Profile of the HCPs and the cases for e-consult (Table 1)
Table 1.
Profile of the HCPs and Cases e-consulted.
| Profiles | N (%) |
|---|---|
| Profession | |
| Doctor | 81 (52.94) |
| Nurse | 15 (9.80) |
| Counsellor | 57 (37.25) |
| Gender | |
| Male | 106 (69.3) |
| Female | 47 (30.7) |
| Reason for e-Consult # | |
| Help with diagnosis | 87 (56.86) |
| Help with medications | 84 (54.93) |
| Help with psychosocial intervention | 130 (84.96) |
| Types of substance use among cases (N = 110)* | |
| Alcohol | 58 (52.72) |
| Nicotine | 40 (36.36) |
| Opioid | 10 (9.09) |
| Benzodiazepine | 6 (5.45) |
| Cannabis | 5 (4.54) |
| Behavioral addiction | 4 (3.63) |
| Clinical Presentation | |
| Primary Withdrawal Features | |
| Alcohol | 42(38.18) |
| Nicotine | 33(30.00) |
| Opioids | 9(8.18) |
| Benzodiazepine | 6(5.45) |
| Comorbid Psychiatric disorder | 11 (10) |
| Mood disorder | 8 (7.27) |
| Anxiety disorder | 3 (2.73) |
| Nature of consultation provided by experts | |
| Diagnosis | 110 |
| Pharmacotherapy | 99 |
| Counseling (Brief Intervention) | 110 |
# reason for e-consult may be more than one *more than one substance use for some cases.
In total, 153 health care providers (HCPs) sought consultation for their patients in this asynchronous telepsychiatry platform during the COVID-19 lockdown. In eleven records, the available information was inadequate to make any diagnosis. We could not get more details despite reaching out to HCPs. Thirty-two patient consultations records were not related to substance use (they were about COVID testing, symptoms of COVID, etc.). Finally, one hundred and ten case consultations were associated with SUDs and included in this study.
The doctors used the e-consultation most frequently, followed by counselors and nurses.TThe mean distance between HCP and specialist was 1263.24 km (±781.84). The majority of consultation is to receive guidance in the area of psychosocial management. Five HCPs consulted more than once. The majority of the 110 case consultations were about male patients with a mean age of 39.06 (12.06) years. Alcohol, nicotine, and opioids were the most prevalent form of substance abuse. Alcohol (52.52%) and nicotine use disorders (36.36%) were the most commonly reported symptoms (Table 1 ).
The following medications were commonly advised during e-consultation. Benzodiazepines were recommended for alcohol withdrawal, baclofen/ naltrexone/ acamprosate, anti-craving agents for alcohol use disorder, nicotine gum and patch (Nicotine replacement therapy NRT) for nicotine use disorders. Tramadol was the most commonly recommended medication for opioid withdrawal and for those who could not procure prescription buprenorphine due to lockdown. There was almost no access to Buprenorphine maintenance treatment. Long-acting diazepam was advised to manage withdrawal symptoms in benzodiazepine dependence. Appropriate mood stabilizers, anti-psychotic, anti-depressants were recommended for the SUD cases with a co-occurring psychiatric diagnosis. Around 71.89 % of HCPs advised to use brief interventions, motivational interviewing components, and relapse prevention strategies with their patients of SUDs (Humeniuk et al., 2010; Menon and Kandasamy, 2018; Murthy, 2018). Almost 85 % of HCPs also received educational material related to the medical and psychosocial management of the concerned substance, along with recommendations.
3.2. Acceptability of e-consult among HCPs (Table 2a, Table 2b, Table 2c)
Table 2a.
Acceptability on various SUTAQ items by HCPs.
| SUTAQ Items (score) | Strongly disagree (1) | Moderately disagree (2) | Mildly Disagree (3) | Mildly Agree (4) | Moderately Agree (5) | Strongly Agree (6) |
|---|---|---|---|---|---|---|
| 1. Saving time | 0 | 0 | 1 (1.47%) | 4 (5.88%) | 19 (27.94%) | 44 (64.70%) |
| 2. Access to specialist care | 0 | 0 | 0 | 10 (14.70%) | 19 (27.94%) | 39 (57.35%) |
| 3. Satisfied with recommendations | 0 | 1 (1.47%) | 1 (1.47%) | 6 (8.82%) | 21 (30.88%) | 40 (58.82%) |
| 4. Recommend to others | 0 | 1 (1.47%) | 0 | 6 (8.82%) | 16 (23.52%) | 45 (66.17%) |
| 5. Not as suitable as regular face to face consultations** | 7 (10.29%) | 5 (7.35%) | 7 (10.29%) | 18 (26.47%) | 22 (32.35%) | 9 (13.23%) |
| 6. Easier to get in touch with Addiction Specialist | 1 (1.47%) | 0 | 0 | 3 (4.41%) | 25 (36.76%) | 39 (57.35%) |
| 7. Interferes with the continuity of the care** | 11 (16.18%) | 8 (11.76%) | 8 (11.76%) | 13 (19.18%) | 19 (27.94%) | 9 (13.23%) |
| 8. Invaded my patient's privacy** | 24 (35.29%) | 7 (10.29%) | 9 (13.23%) | 6 (8.82%) | 13 (19.12%) | 9 (13.23%) |
| 9. Trusted to work appropriately | 0 | 0 | 0 | 9 (13.23%) | 21 (30.88%) | 38 (55.88%) |
| 10. Made me Feel uncomfortable** | 29 (42.64%) | 15 (22.05%) | 7 (10.29%) | 8 (11.76%) | 7 (10.29%) | 1 (1.47%) |
| 11. Concerned about level of Expertise of Specialists** | 12 (17.65%) | 7 (10.29%) | 6 (8.82%) | 8 (11.76%) | 18 (26.47%) | 16 (23.53%) |
| 12. Certainly, be a good addition to my regular consultation | 2 (2.94%) | 0 | 2 (2.94%) | 6 (8.82%) | 17 (25%) | 40 (58.82%) |
Items 5, 7, 8, 10, 11 were suggestive of dissent; therefore the scores are inverted; thus, a low value implies a positive view towards these aspects of e-consult.
Table 2b.
Comparison of Acceptability among HCPs (Doctor: 38 and Counsellor:30).
| SUTAQ items | Median (S.D.) | Doctor versus Counsellors Variance (Mann Whitney U test) |
|---|---|---|
| 1. Saving time | 6 (0.678) | U = 535.00, p= 0.607 |
| 2. Access to specialist care | 6 (0.739) | U = 425.00, p =0 .043* |
| 3. Satisfied with recommendations | 6 (0.781) | U = 329.500, p = 0.001* |
| 4. Recommend to others | 6 (0.781) | U = 433.00, p = 0.043* |
| 5. Not as suitable as regular face to face consultations | 3 (1.486) | U = 431.00, p = 0.077 |
| 6. Easier to get in touch with an Addiction Specialist | 6 (0.801) | U = 497.00, p= 0.302 |
| 7. Interferes with the continuity of the care | 3 (1.676) | U = 483.00, p= 0.273 |
| 8. Invaded my patient's privacy | 4 (1.9) | U = 505.00, p= 0.408 |
| 9. Trusted to work appropriately | 6 (0.96) | U = 534.00, p= 0.623 |
| 10. Made me feel uncomfortable | 5 (1.562) | U = 493.00, p= 0.318 |
| 11. Concerned about the level of expertise of specialists | 2 (1.864) | U = 540.00, p= 0.705 |
| 12. Certainly, be a good addition to my regular consultation | 6 (1.262) | U = 443.00, p = 0.077 |
p < 0.05.
Table 2c.
Comparison of Subscales among HCPs (Doctor: 38 and Counsellor:30).
| Subscale | Median (Interquartile Range) | Doctor and Counsellors variance (Mann Whitney U test) |
|---|---|---|
| Enhanced care | 5.7 (5.3-6) | 432.5, p = 0.076 |
| Increased accessibility | 5.5 (5-6) | 434.0, p = 0.075 |
| Privacy and discomfort | 4.5 (3-6) | 499.0, p = 0.372 |
| Care personnel concerns | 3 (2-4) | 487.0, p = 0.305 |
| E-consult as substitution | 3 (2-4) | 431.0, p = 0.077 |
| Satisfaction | 5.5 (5-6) | 400.0, p = 0.026* |
Sixty-eight of 110 (61.8%) HCPs, i.e., Thirty-eight doctors, twenty-seven counselors, and three nurses, filled up the feedback form. The majority (85%) felt it was easy to navigate the e-consult pathway.
There was a high degree of acceptability for: "access to specialist care" (100 %), "trusted to work appropriately (100 %)", "Saving time (98.53 %)", "recommend to others" (98.53 %)," easier to get touch with the specialist (98.53 %) "satisfied with recommendations" (97.06 %) and "a good addition to my regular consultation (94.12 %) (Table 2a ).
Low acceptability was reported for "suitability compared to face to face consultation" (72.05 %), "concerned with the level of expertise" (61.76 %), "interfere with the continuity of care (60.35 %)).(Table 2b )
Among HCPs, doctors reported significantly high acceptability with regard to "access to specialist care," "satisfied with recommendations, "recommend to others" compared to others (Table 2b).
Three subscales, "enhanced care," "increased accessibility," and "satisfaction" indicated a high degree of acceptability of this service. (Table 2c ) HCPs did not express any specific concerns about an invasion of privacy and confidentiality issues during this electronic consultation. They shared a positive view of these aspects of electronic consultation.
4. DISCUSSION
During the COVID 19 lockdown, e-consult for patients with SUDs was implemented as face to face visits were not possible. A majority of HCPs reported easy access to the specialist, trusted the consultation, and were satisfied with the recommendations. Many felt this saves time for their patients and agreed with this as a useful addition to the regular consultation. The most frequent reason for consultation in this study was for the management of Alcohol and Nicotine use disorders, which are commonly used substances in India, as reported in household surveys. The National Mental Health Survey, 2016, suggests nicotine addiction as the most prevalent (20.9 %) followed by alcohol (4.6 %) and other substances (0.6 %) (Gururaj et al., 2016). Similarly, due to the restriction of travel and closure of sale, it can explain substance-related withdrawal symptoms as the most common reason for consultation.
More than 60 % of the HCPs reporting overall high satisfaction, and more than 98 % providers reported high acceptability for "access to specialist care," "trusted to work appropriately", "saving time," "would like to recommend to others," easier to get touch with a specialist." They scored high in the subscales of "enhanced care," "increased accessibility to specialist," and "satisfaction in consultation." Studies from other health conditions have shown that HCP satisfaction was generally good for e-consults, with 70–95 % providers reporting high satisfaction (Vimalananda et al., 2015). The HCPs reported satisfaction in terms of convenience, educational value, rapid turnaround, improved access to specialty input, better provider-provider communication, avoidance of unnecessary patient travel, and the perception of shorter waiting times for patients ultimately referred to face-to-face visits (Vimalananda et al., 2020).
About three fourth of the providers in the current study received personalized, case-based educational materials. These materials were designed to provide useful information regarding managing similar cases in the future. Recent studies in e-consult have described a full educational benefit to less-experienced HCPs. Nurse practitioners, physician assistants, trainee physicians, and physicians with less than ten years of experience reported improved clinical skills compared to physicians with longer experience (Kwok et al., 2018). HCPs managing mental health conditions, reported significant improvement in perceived support for diagnosis, treatment decisions, and changing treatment during six months of e-consult (Golberstein et al., 2018). In our study, although the HCPs did not find e-consult a satisfactory substitute for regular 'face to face' consultation but considered it as an useful addition to their regular practice.
Broadly there are three methods of asynchronous technology used teleconsultations i.e., messaging, video recording, and electronic health records (Chan et al., 2018). The current study would fall into the category of electronic health records or electronic consultations or e-consult. The advantage of e-consult is that, unlike curbside consultation (telephone/message/Whatsapp), a HIPPA compliant secured electronic form was used to review the documented data provided by HCPs. This also does not require videoconferencing facility nor the simultaneous presence of both HCP and the specialists. We have signed a business associate agreement (BAA) with the online survey provider to make sure that all the information are encrypted and protected health information (PHI) remain secured.
The response to the email invitation to use the e-consult was 5.6 %. In a study from developed country, researchers invited teenagers to evaluate a smoking cessation website. They were also offered 20 $ gift for participation in the survey. The result showed that only 5 out of 2109 delivered emails i.e. 0.24 % completed the questionnaire (Koo and Skinner, 2005). Internet provides a tremendous opportunities for innovative research but there are many other variables i.e. participants interest, technology and content which can play the part in engagement. The poor response of opening the email in our study can be explained by the fact that all the participants may not be interested in SUD or not providing care to SUDs. Hence they may not find this as useful. At the same time, one out of three who visited the e-consult link, used this and discussed their case with addiction specialist.
More than 60 % of HCPs who used e-consultation, completed the SUTAQ questionnaire regarding acceptability. This survey response rate is double than that of similar survey among HCPs who availed e-consult with a mental health specialist (Golberstein et al., 2018). The response rate on feedback at the baseline and follow up from HCP was 30 % and 27 % respectively reported by the previous study (Golberstein et al., 2018).
This study could not able to get the feedback on e-consult directly from the patients, treated by the HCPs. Besides, very few HCPs used this tool during a COVID lockdown period. We cannot conclusively comment on the translation of the e-consult recommendations to their patients. However, despite these limitations, this was well accepted by those who used it in their practice. The future research should explore the use of e-consult in other areas of mental health.
5. CONCLUSION
The COVID-19 pandemic has catapulted the widespread use of technology in medicine practice. The e-consult holds a promise for improving SUD care in the community by formalizing the consultation between HCP and addiction specialist as both do not need to meet real time. In a developing country like India, addiction specialists are very few, located in public sector teaching hospital and are busy in clinical services. The educative component of e-consult is also an useful tool to empower the HCPs for future and greater confidence in the continued care. This study provided positive evidence related to accessibility, enhanced clinical care, and clinician satisfaction among HCPs. Future rigorous studies on e-consult can help in understanding its impact on patient clinical outcome in different health facilities. This information will establish e-consult programs as a cost-effective option to improve accessibility of speciality care in the health care system.
Financial Disclosure
Nothing to disclose
Declaration of Competing Interest
None
Acknowledgment
Health care providers engaged in NIMHANS Digital Academy, Virtual Knowledge Network ECHO with a mission of providing SUD care for underserved population
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ajp.2020.102451.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Ambekar A., Agrawal A., Rao R., Mishra A., Khandelwal S., Chadda R. National Survey on Extent and Pattern of Substance Use in India. In: Ambekar A., Agrawal A., Rao R., Mishra A., Khandelwal S., Chadda R., editors. National Survey on Extent and Pattern of Substance Use in India (2019) Ministry of Social Justice and Empowerment, Government of India and NDDTC, AIIMS; New Delhi, New Delhi: 2019. [Google Scholar]
- Arya S., Gupta R. COVID-19 outbreak: Challenges for Addiction services in India. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan S., Li L., Torous J., Gratzer D., Yellowlees P.M. Review of Use of Asynchronous Technologies Incorporated in Mental Health Care. Curr Psychiatry Rep. 2018;20(10):85. doi: 10.1007/s11920-018-0954-3. PMID:30155593. [DOI] [PubMed] [Google Scholar]
- Chand P., Murthy P., Gupta V., Kandasamy A., Jayarajan D., Sethu L., Benegal V., Varghese M., Komaromy M., Arora S. Technology enhanced learning in addiction mental health: developing a virtual knowledge network: NIMHANS ECHO. 2014 IEEE Sixth International Conference on Technology for Education; IEEE; 2014. pp. 229–232. [Google Scholar]
- Dario C., Luisotto E., Dal Pozzo E., Mancin S., Aletras V., Newman S., Gubian L., Saccavini C. Assessment of patients’ perception of telemedicine services using the service user technology acceptability questionnaire. Int. J. Integr. Care. 2016:16. doi: 10.5334/ijic.2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forum N.Q. National Quality Forum Washington; DC: 2017. Creating a Framework to Support Measure Development for Telehealth. [Google Scholar]
- Ganesh A., Sahu P., Nair S., Chand P. A smartphone based e-Consult in addiction medicine: An initiative in COVID lockdown. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gangadhar B. Distance training for the delivery of psychiatric services in primary care. Ind. J. Psychiatr. 2019;61:115. doi: 10.4103/psychiatry.IndianJPsychiatry_38_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh A., Gupta R., Misra A. Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: guidelines for physicians. Diab. Metab. Synd. Clin. Res. Rev. 2020 doi: 10.1016/j.dsx.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golberstein E., Kolvenbach S., Carruthers H., Druss B., Goering P. Effects of electronic psychiatric consultations on primary care provider perceptions of mental health care: survey results from a randomized evaluation. Healthcare. 2018:17–22. doi: 10.1016/j.hjdsi.2017.01.002. Elsevier. [DOI] [PubMed] [Google Scholar]
- Gururaj G., Varghese M., Benegal V., Rao G., Pathak K., Singh L., Misra R. National Institute of Mental Health and Neurosciences; Bengaluru: 2016. National mental health survey of India, 2015-16: Summary. [Google Scholar]
- Hilty D., Yellowlees P.M., Parrish M.B., Chan S. Telepsychiatry: effective, evidence-based, and at a tipping point in health care delivery? Psychiatr. Clin. 2015;38:559–592. doi: 10.1016/j.psc.2015.05.006. [DOI] [PubMed] [Google Scholar]
- Hirani S.P., Rixon L., Beynon M., Cartwright M., Cleanthous S., Selva A., Sanders C., Newman S.P. Quantifying beliefs regarding telehealth: development of the whole systems demonstrator service user technology acceptability questionnaire. J. Telemed. Telecare. 2017;23:460–469. doi: 10.1177/1357633X16649531. [DOI] [PubMed] [Google Scholar]
- Humeniuk R., Henry-Edwards S., Ali R., Poznyak V., Monteiro M.G., Organization W.H. 2010. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): manual for use in primary care. [Google Scholar]
- Koo M., Skinner H. Challenges of internet recruitment: a case study with disappointing results. J. Med. Int. Res. 2005;7:e6. doi: 10.2196/jmir.7.1.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok J., Olayiwola J.N., Knox M., Murphy E.J., Tuot D.S. Electronic consultation system demonstrates educational benefit for primary care providers. J. Telemed. Telecare. 2018;24:465–472. doi: 10.1177/1357633X17711822. [DOI] [PubMed] [Google Scholar]
- Lin L.A., Casteel D., Shigekawa E., Weyrich M.S., Roby D.H., McMenamin S.B. Telemedicine-delivered treatment interventions for substance use disorders: A systematic review. J. Subst. Abuse Treat. 2019;101:38–49. doi: 10.1016/j.jsat.2019.03.007. [DOI] [PubMed] [Google Scholar]
- Mehrotra K., Chand P., Bandawar M., Sagi M.R., Kaur S., Aurobind G., Raj A., Jain S., Komaromy M., Murthy P. Effectiveness of NIMHANS ECHO blended tele-mentoring model on Integrated Mental Health and Addiction for counsellors in rural and underserved districts of Chhattisgarh, India. Asian J. Psychiatr. 2018;36:123–127. doi: 10.1016/j.ajp.2018.07.010. [DOI] [PubMed] [Google Scholar]
- Menon J., Kandasamy A. Relapse prevention. Ind. J. Psychiatr. 2018;60:S473. doi: 10.4103/psychiatry.IndianJPsychiatry_36_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MOHFW . Ministry of Health and Family Welfare, Govt of India, Ministry of Health and Family Welfare; 2020. Telemedicine Practice Guidelines. [Google Scholar]
- Murthy P. Guidelines for psychosocial interventions in addictive disorders in India: An introduction and overview. Ind. J. Psychiatry. 2018;60:S433. doi: 10.4103/psychiatry.IndianJPsychiatry_35_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murthy P., Manjunatha N., Subodh B., Chand P.K., Benegal V. Substance use and addiction research in India. Ind. J. Psychiatr. 2010;52:S189. doi: 10.4103/0019-5545.69232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narasimha V.L., Shukla L., Mukherjee D., Menon J., Huddar S., Panda U.K., Mahadevan J., Kandasamy A., Chand P.K., Benegal V. Complicated alcohol withdrawal—an unintended consequence of COVID-19 lockdown. Alcohol Alcohol. (Oxford, Oxfordshire) 2020 doi: 10.1093/alcalc/agaa042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman S., Rixon L., Hirani S., Cartwright M., Beynon M., Cleanthous S., Selva A. Quantifying beliefs regarding telehealth: development of the SUTAQ service user technology acceptability questionnaire. Invited talk, Renewing Health conference; Tromso, Norway; 2011. [DOI] [PubMed] [Google Scholar]
- Ramalho R., Adiukwu F., Bytyçi D.G., El Hayek S., Gonzalez-Diaz J.M., Larnaout A., Grandinetti P., Kundadak G.K., Nofal M., Pereira-Sanchez V. Telepsychiatry and healthcare access inequities during the COVID-19 pandemic. Asian J. Psychiatr. 2020 doi: 10.1016/j.ajp.2020.102234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ransing R., Adiukwu F., Pereira-Sanchez V., Ramalho R., Orsolini L., Teixeira A.L.S., Gonzalez-Diaz J.M., da Costa M.P., Soler-Vidal J., Bytyçi D.G. Early career psychiatrists’ perspectives on the mental health impact and care of the COVID-19 pandemic across the world. Asian J. Psychiatr. 2020 doi: 10.1016/j.ajp.2020.102085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagi M.R., Aurobind G., Chand P., Ashfak A., Karthick C., Kubenthiran N., Murthy P., Komaromy M., Arora S. Innovative telementoring for addiction management for remote primary care physicians: A feasibility study. Ind. J. Psychiatr. 2018;60:461. doi: 10.4103/psychiatry.IndianJPsychiatry_211_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tandon R. COVID-19 and mental health: Preserving humanity, maintaining sanity, and promoting health. Asian J. Psychiatr. 2020 doi: 10.1016/j.ajp.2020.102256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tandon R. The COVID-19 pandemic, personal reflections on editorial responsibility. Asian J. Psychiatr. 2020;50 doi: 10.1016/j.ajp.2020.102100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torbjørnsen A., Småstuen M.C., Jenum A.K., Årsand E., Ribu L. The service user technology acceptability questionnaire: Psychometric evaluation of the norwegian version. JMIR human factors. 2018;5 doi: 10.2196/10255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vimalananda V.G., Gupte G., Seraj S.M., Orlander J., Berlowitz D., Fincke B.G., Simon S.R. Electronic consultations (e-consults) to improve access to specialty care: a systematic review and narrative synthesis. J. Telemed. Telecare. 2015;21:323–330. doi: 10.1177/1357633X15582108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vimalananda V.G., Orlander J.D., Afable M.K., Fincke B.G., Solch A.K., Rinne S.T., Kim E.J., Cutrona S.L., Thomas D.D., Strymish J.L. Electronic consultations (E-consults) and their outcomes: a systematic review. J. Am. Med. Inform. Associat. 2020;27:471–479. doi: 10.1093/jamia/ocz185. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.