Abstract
Background
Transurethral resection of the prostate (TURP) is considered the gold standard surgical intervention for prostate size less than 80 g. Prostatic artery embolization (PAE) has been suggested as a minimally invasive interventional radiological procedure in the management of benign prostatic hyperplasia (BPH), especially by using the PErFecTED technique. We aim through our study to evaluate the efficacy and safety of PAE compared with those of monopolar transurethral resection of prostate (M-TURP) and bipolar transurethral resection of prostate (B-TURP) in treating lower urinary tract symptoms (LUTSs) secondary to BPH.
Methods
We randomized 60 patients into 3 equal groups representing M-TURP, B-TURP, and PAE. Patients were followed up at 1 and 6 months postoperatively with regard to the International prostate symptom score (IPSS) score; uroflowmetry; prostate volume by transrectal ultrasound; and postvoid residual urine.
Results
The mean operative time was 59, 68, and 89 minutes for the M-TURP group, the B-TURP group, and the PAE group, respectively; only one patient, who represented 5% of the M-TURP group and 1.7% of the whole study population, developed transurethral resection syndrome. Four patients of the PAE group complained of postembolization syndrome, which represented 20% of the cases. Only two patients in our study, both belonging to the PAE group, developed acute urinary retention after catheter removal, representing 10% of the PAE group and 3.33% of the whole study population. The improvement in the IPSS score, the average uroflowmetry (Q-average) score, postvoid residual urine, and prostate volume reduction was noted in all groups, with more statistically significant improvement in each of the M-TURP and the B-TURP groups than in the PAE group.
Conclusion
PErFecTED technique is a novel way of embolization, with statistically significant improvement for patients complaining of LUTSs due to BPH in terms of improvement of IPSS, uroflowmetry, prostate size, and amount of postvoid residual urine, yet these results are still not comparable with either the results of M-TURP or B-TURP that still show more effective improvement.
Keywords: Prostate, LUTS, Embolization, TURP, Urine retention, IPSS
1. Introduction
Benign prostatic hyperplasia (BPH) is one of the most common morbidities in elderly men with bladder outlet obstruction and lower urinary tract symptoms (LUTSs). It is estimated to affect 50% of men at the age of 60 years and as many as 90% of men aged 70–89 years.1,2
Transurethral resection of the prostate (TURP) is considered the gold standard surgical intervention for prostate size less than 80 g. The introduction of bipolar transurethral resection in saline has reduced the relative risks of transurethral resection syndrome (TUR syndrome), and the procedure is more appropriate for prostate size more than 80 g.3,4
Prostatic artery embolization (PAE), which was initially used in management of hematuria secondary to BPH, has been first used by Rastinehad et al. in management of BPH.19 Then, it has been adopted by other studies that showed that PAE may reduce prostate volume by about 30%, improve LUTSs, improve bladder outlet obstruction, and relieve urinary retention in patients using indwelling urinary catheters.6, 7, 8 These results were much improved with the new technique of PAE that was described by Carnevale et al in 2014 wherein proximal embolization was performed first followed by distal embolization; this technique is known as PErFecTED technique, and this technique was associated with greater prostate infarction rates.18
The rule of PAE is highly controversial in the management of BPH. We aim through our study to evaluate the efficacy and safety of PAE compared with monopolar transurethral resection of prostate (M-TURP) and bipolar transurethral resection of prostate (B-TURP) in treating LUTSs secondary to BPH.
2. Materials and methods
A total of 60 patients who suffered from LUTSs due to BPH after the failure of medical treatment were included in our study from the urology outpatient clinic of Ain Shams University Hospitals in the period from January 2016 until January 2018. Patients complained of LUTSs with an IPSS score of 8–35 (8 being moderate and 35 being severe), uroflowmetry with an average flow of ≤10 ml/sec, and a prostate volume less than 100 ml by transrectal ultrasound. Patients with elevated kidney functions (≥1.5 mg/dl), with allergy to intravenous (IV) contrast media, unfit for surgery, with prostatic adenocarcinoma, with previous history of prostatic or urethral operations, with signs of the decompensated bladder (e.g., bladder diverticulum), with signs of upper urinary tract infection revealed by pelvic abdominal ultrasound were excluded from our study.
Informed consent was obtained from all patients participating in our study before they were randomly allocated into 3 equal groups using the sealed envelope method, i.e., groups A, B, and C representing patients who underwent M-TURP, B-TURP, and PAE, respectively.
In the M-TURP group, the procedure was performed using a 26-Fr continuous flow resectoscope, Storz single-wire loop using 175 W cutting power, a 75 W coagulation power and 1.5% glycine solution for irrigation. And in the B-TURP group, the procedure was performed using the ERBE VIO 300 D equipment bipolar generator set at 200–280 W and a coagulation mode setting of 80–120 W and using normal saline solution for irrigation.
In the PAE group, the procedure was performed as described by Carnevale et al in 2014. Under local anesthesia, access to the internal iliac artery is achieved; then, selective angiography of the internal iliac artery is performed to assess the blood supply to the prostate. The microcatheter must be placed distal to any collateral branch to the bladder, rectum, corpus cavernosum, gonad, or penis directly into the prostatic artery before it branches into urethral and capsular groups. To each 2-mL syringe of microspheres, 10 mL of iodinated contrast medium and 10 mL of saline were added, resulting in a total volume of 22 ml. The mixture is injected in high dilution in a slow manner to ensure diffuse gland ischemia and avoid vessel injury.18
Then, the microcatheter is advanced into the urethral and capsular intraprostatic groups of arteries until they are embolized separately. The urethral group of arteries is embolized first followed by the intraprostatic branches. The microcatheter is then retracted to the origin of the inferior vesical artery, and contrast is injected for final control in a search for additional prostatic branches. These procedures are repeated on the contralateral side. The patient is then discharged on the same day after the procedure and is maintained on α-blockers with the urethral catheter, which is removed on the fifth day postoperatively.9
The patients were followed up at 1 and 6 months postoperatively with regard to the IPSS score , uroflowmetry, prostate volume by transrectal ultrasound, and Post-voiding residula urine (PVRU) volume.
3. Results
The demographic data for patients in the 3 groups were nearly the same, with a mean age of 63 years. The preoperative prostate size ranged from 25 to 99 grams, 30 to 99 grams, and 31 to 95 grams in the M-TURP, B-TURP, and PAE groups, respectively.
Regarding intraoperative time, it ranged from 25 to 115 minutes, with a mean of 59 minutes, in the M-TURP group, and from 30 to 103 minutes, with a mean of 68 minutes, in the B-TURP group, while in the PAE group, it ranged from 62 minutes to 115 minutes, with a mean of 89 minutes. There is a statistically significant difference between the PAE and TURP groups, with a p-value ≤0.001, whereas there are no statistically significant results between the M-TURP and B-TURP groups.
There were no statistically significant results in postoperative hemoglobin level in all groups with no need for perioperative blood transfusion.
Regarding Na+ level, in the M-TURP group, only one patient (representing 5% of the M-TURP group and 1.7% of the whole study population) developed TUR syndrome that manifested in the form of disturbed conscious level and decreased serum Na+ level of 123 mEq/L postoperatively, which required IV hypertonic saline infusion and monitoring.
Regarding catheter removal time, for both the M-TURP group and B-TURP groups, the catheter was removed on the third postoperative day, whereas for the PAE group, it was removed on the fifth postoperative day. Two patients in the PAE group developed acute urinary retention after catheter removal (representing 10% of the PAE group and 3.33% of the whole study population); both underwent surgical intervention.
Four of the patients of the PAE group complained of postembolization syndrome (representing 20% of the PAE group) in the form of severe perianal pain, which was relieved with analgesics after 2–3 weeks.
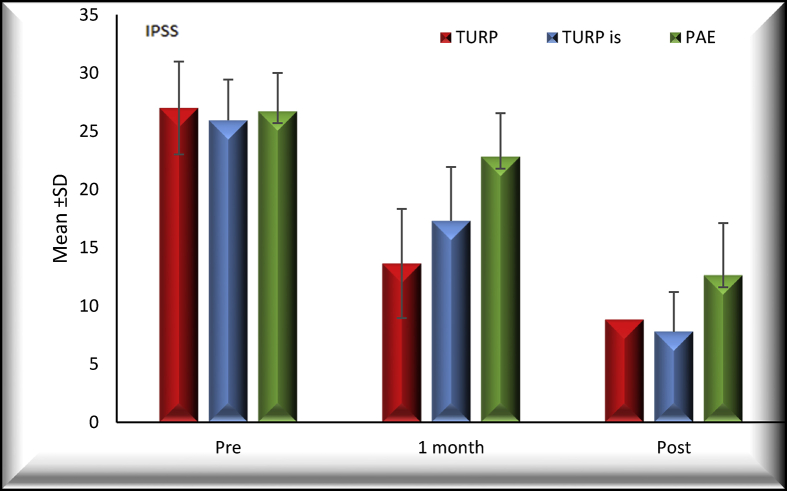
Regarding the IPSS questionnaire, the decrease in the mean score in the 3 groups was as follows: in the first month of follow-up, the decline in the mean score was 13, 9, and 4 for the M-TURP, B-TURP, and PAE groups, respectively, with a statistically significant difference in all the 3 groups compared with the preoperative score.
Comparing the preoperative and the 6-month follow-up postoperative IPSS results, the differences in means between the three groups were 18, 18, and 14 for the M-TURP, B-TURP, and PAE groups, respectively, as shown in Fig. 1. Improvement in the IPSS score was statistically significant in each of the M-TURP and B-TURP groups compared with the PAE group.
Fig. 1.
Comparison of the differences in mean and standard deviations between the preoperative, 1-month follow-up, and 6-month follow-up International prostate symptom score (IPSS) score results for the patients of the three groups: M-TURP, B-TURP, and PAE. M-TURP = monopolar transurethral resection of the prostate; B-TURP = bipolar transurethral resection of the prostate; PAE = prostatic artery embolization; SD = standard deviation.
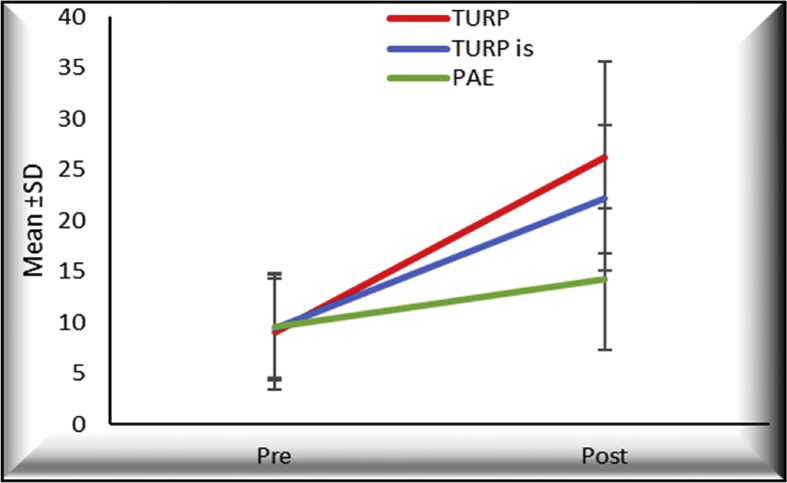
The differences in means between the preoperative and postoperative average uroflowmetry (Q-average) score in the three groups were 9, 7, and 3 for the M-TURP group, B-TURP group, and PAE group, respectively, as shown in Fig. 2. This improvement was statistically significant in the 3 groups, with a p-value <0.001. There was a statistically significant difference in average uroflowmetry improvement between the M-TURP and B-TURP groups on the one hand and the PAE group on the other hand, with a p-value <0.001, but there was no statistically significant difference between the M-TURP and B-TURP groups.
Fig. 2.
Comparison of the differences in means and standard deviations for preoperative and postoperative maximum uroflow results for the three groups: M-TURP, B-TURP, and PAE. M-TURP = monopolar transurethral resection of the prostate; B-TURP = bipolar transurethral resection of the prostate; PAE = prostatic artery embolization; SD = standard deviation.
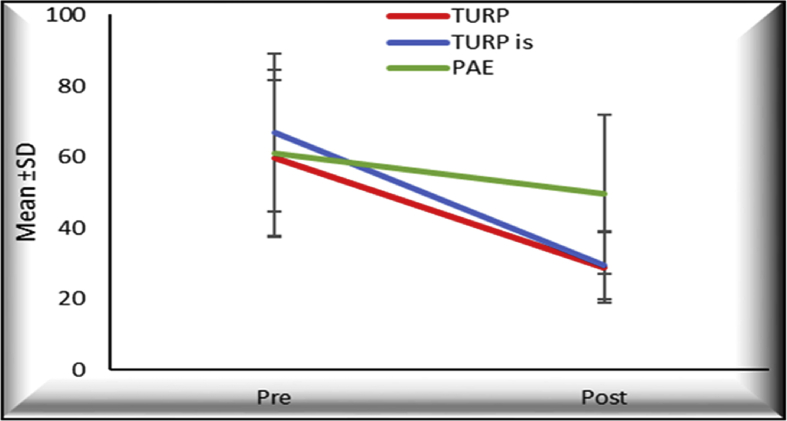
The mean of prostate size reduction in the three groups were 31, 37, and 11 grams for the M-TURP, B-TURP, and PAE groups, respectively, as shown in Fig. 3, with a significant difference between the PAE group and both the M-TURP and B-TURP groups with a p-value <0.001, whereas there was no statistically significant difference between the M-TURP and B-TURP groups.
Fig. 3.
Comparison of the differences in means and standard deviations for preoperative and postoperative prostate size results for the three groups: M-TURP, B-TURP, and PAE. M-TURP = monopolar transurethral resection of the prostate; B-TURP = bipolar transurethral resection of the prostate; PAE = prostatic artery embolization; SD = standard deviation.
Postvoid residual urine showed marked improvement in all groups; the mean postoperative results were 35 ml, 33 ml, and 88 ml for the M-TURP, B-TURP, and PAE groups, respectively. The differences in means between the preoperative and postoperative results in the three groups were 85, 109, and 95 for the M-TURP, B-TURP, and PAE groups, respectively, with a statistically significant difference between the preoperative and postoperative values in the three groups and no statistically significant difference between each of the groups.
4. Discussion
In our study, we evaluated the rule of M-TURP, B-TURP, and PAE in the management of LUTSs due to BPH with regard to the intraoperative time, immediate postoperative hemoglobin and serum sodium levels, postoperative complications, uroflowmetry, prostate size, postvoid residual urine, and IPSS score up to six months after the intervention.
Regarding mean intraoperative time, it was much longer in the PAE group, with 89.85 minutes compared with 59.7 minutes and 68.25 minutes for the M-TURP group and the B-TURP group, with a statistically significant difference; this may be attributed to the anatomy of the pelvic vessels to achieve selective embolization and avoid untargeted embolization and also to the unfamiliarity of the intervention radiologist with the new technique which demands a higher learning curve than the standard way of embolization.
Regarding intraoperative blood loss, it was more in the M-TURP group than that seen in the other two groups, with a significant difference between the M-TURP and PAE groups. However, no patients in any group required blood transfusion. In a prospective randomized study, Stucki et al10 compared bleeding complications of M-TURP and B-TURP procedures. The authors could not find any statistically significant difference between the 2 procedures, and none of the patients required a blood transfusion; this was concomitant with our results.10
Regarding the serum Na+ level, TUR syndrome occurred in one patient the M-TURP group (representing 5% of the M-TURP group and 1.7% of the whole study population); it did not occur in any of the patients of the other two groups. However, the decrease in the level of serum Na+ postoperatively was not statistically significant between the three groups.
After catheter removal, two patients from the PAE group (representing 10% of the PAE group and 3.33% of the whole study population) developed acute urinary retention, necessitating catheterization, and they both underwent surgical intervention.
Four of the patients of the PAE group (representing 20% of the PAE group and 6.66% of the whole study population) complained of severe perianal pain, which was relieved with analgesics after 2–3 weeks. Up to 6 months of follow-up, the noticed complications in our study population were limited to urine retention and postembolization syndrome in the form of pain and dysuria, as mentioned in the Results section.
Gao et al11 in their study stated that commonly observed minor complications in the PAE group were postembolization syndrome (11.1%) and acute urinary retention (25.9%), but in their study, acute urinary retention resolved within three days, requiring no more than just a urinary catheter, attributing that to urethral compression by ischemic edema of the prostate after PAE. Compared with our results, we had a higher rate of incidence of postembolization syndrome, and the patients who developed retention required catheterization and another way of intervention.11
The IPSS scores was significantly improved at one and six months of follow-up for the three groups, yet this improvement was statistically more significant in the M-TURP than B-TURP groups and was more in the two groups than that in the PAE group. The mean IPSS score decreased from 27, 26, and 26 to 9, 8, and 12 at 6-month follow-up for the M-TURP, B-TURP, and PAE groups, respectively. Despite the variation in prostate size reduction after intervention between the 3 groups, IPSS score improvement was nearly similar in all groups; this may be due to asymptomatic prostatic inflammation that affects the LUTSs as mentioned by Cakir et al.12 In addition, the subjectivity of IPSS score and patient to patient variability and the different education level as mentioned by Taneja et al13 2017, that education level may be affected and the visual prostate symptom score would be more appropriate in comparison to IPSS.
Regarding maximum uroflow rate, there was a statistically significant improvement in all three groups, with more improvement in the M-TURP and B-TURP groups than in the PAE group.
Demirdage et al14 stated that irrespective of the energy type used, M-TURP operation can be successfully performed to relieve the complaints of patients who had lower urinary tract obstruction. In their study, the mean preoperative IPSS values were 25 in both the M-TURP and B-TURP groups, and these values fell to 6.6 and 6.7 at the postoperative sixth month, and regarding mean flow rate, in the M-TURP group, it increased from 8.6 mL/min to 20.1 mL/min, whereas it increased from 9.2 mL/min to 21.8 mL/min in the B-TURP group.14 These results were similar and comparable with our results in comparing M-TURP and B-TURP with a consensus on the effectiveness in relieving LUTSs due to BPH.
Shim et al16 stated that analyzing the efficacy of PAE in a single arm reveals significant improvements in IPSS scores, maximum uroflowmetry, PVRU, and prostate volume. However, in their systematic review with meta-analysis, they concluded that PAE should still be considered as an experimental treatment modality. In terms of efficacy, it is still inferior to standard treatment methods. However, PAE may offer other benefits to patients as being a minimally invasive procedure with a shorter hospital stay, faster return to normal activities, reduction in some adverse effects, and with a symptomatic benefit in management of LUTSs due to BPH.15, 16, 17
Carnevale et al18 in their study found a significant difference in terms of maximum uroflowmetry and prostate size yet not in IPSS questionnaire scores and stated that M-TURP results in significantly higher Q-max values and significantly smaller prostate volume than PAE, but there was no significant difference between postoperative IPSS scores.
The UK-ROPE study included 305 patients, 216 patients of whom underwent PAE, and concluded that PAE provides a significant improvement in the IPSS score; although some of these improvements were less than those observed with the TURP arm, PAE has the advantage of higher safety and earlier return to daily activities. Regarding prostate volume, there was a 28% reduction in prostate volume in the PAE group. In our study, the reduction in prostate size was 11.5% only, which may be attributed to the follow-up point, which was limited to 6 months after the intervention.15
5. Conclusion
B-TURP is as effective as M-TURP, with less blood loss and decrease in the possibility of occurrence of TUR syndrome.
PAE performed using the PErFecTED technique is an advanced way of embolization that requires a high level of expertise and shows improvement in patients complaining of LUTSs due to BPH, yet these results are still not comparable with either M-TURP or B-TURP results. However, it represents a good treatment option in highly selective patients who are unfit for surgery that can be performed as an outpatient setting, requiring less hospitalization with earlier return to daily activities.
More studies regarding PAE are needed to discuss the long-term efficacy, the effect on erection, ejaculation, the need for retreatment again and cost-effectiveness; studies are also needed to evaluate the economic benefits of PAE.
Conflicts of interest
The authors have no conflict of interest to declare.
Contributor Information
Ahmed Radwan, Email: Ahmedradwan67@gmail.com.
Ahmed Farouk, Email: dr_farouk77@yahoo.com.
Ahmed Higazy, Email: ahmedmaherhigazy@gmail.com.
Younan R. Samir, Email: dr-yona@med.asu.edu.eg.
Ahmed M. Tawfeek, Email: Drahmedtawfeek@med.asu.edu.eg.
Mohamed A. Gamal, Email: dr.mohgamal@gmail.com.
References
- 1.Oelke M., Bachmann A., Descazeaud A., Emberton M., Gravas S., Michel M. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2013;64(1):118–140. doi: 10.1016/j.eururo.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 2.Roehrborn C.G. ILC IN THE TREATMENT OF BPH Benign Prostatic Hyperplasia: An Overview. Rev Urol. 2005;7:3–14. [PMC free article] [PubMed] [Google Scholar]
- 3.Gravas S., Cornu J.N., Drake M.J., Gacci CG M., Herrmann T.R.W., Madersbacher CM S. EAU Guidelines Panel on Treatment of Non-neurogenic Male LUTS Guidelines: Management of Non-Neurogenic Male Lower Urinary Tract Symptoms (LUTS), incl. Benign Prostatic Obstruction (BPO) Eur Assoc Urol. 2018;36(4):575–584. doi: 10.1007/s00345-018-2220-z. http://uroweb.org/wp-content/uploads/EAU-Guidelines-on-the-Management-of-Non-neurogenic-Male-LUTS-2018-large-text.pdf [DOI] [Google Scholar]
- 4.Avins A.L., Barry M.J., Bruskewitz R.C., Donnell R.F., Foster H.E., Gonzalez C.M. BPH); 2010. American Urological Association Guideline: Management of Benign Prostatic Hyperplasia (BPH) AUA Staff: Chapter 1: Guideline on the Management of Benign Prostatic Hyperplasia. [Google Scholar]
- 6.Somani B.K., Hacking N., Bryant T. Prostate artery embolization (PAE) for benign prostatic hyperplasia (BPH) BJU Int. 2014;114(5):639–640. doi: 10.1111/bju.12672. [DOI] [PubMed] [Google Scholar]
- 7.Bagla S., Martin C.P., Breda A Van, Sheridan M.J., Sterling K.M., Papadouris D. Early Results from a United States Trial of Prostatic Artery Embolization in the Treatment of Benign Prostatic Hyperplasia. J Vasc Intervent Radiol. 2014:1–6. doi: 10.1016/j.jvir.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 8.Pisco J.M., Tinto H.R., Campos L. 2013. Embolisation of prostatic arteries as treatment of moderate to severe lower urinary symptoms ( LUTS ) secondary to benign hyperplasia : results of short- and mid-term follow-up; pp. 2561–2572. [DOI] [PubMed] [Google Scholar]
- 9.Antunes A.A. 2014. The ‘“ PErFecTED Technique ”’: Proximal Embolization First , Then Embolize Distal for Benign Prostatic Hyperplasia; pp. 1602–1605. [DOI] [PubMed] [Google Scholar]
- 10.Stucki P., Marini L., Mattei A., Xafis K., Boldini M., Danuser H. Bipolar versus monopolar transurethral resection of the prostate: A prospective randomized trial focusing on bleeding complications. J Urol. 2015;193(4):1371–1376. doi: 10.1016/j.juro.2014.08.137. [DOI] [PubMed] [Google Scholar]
- 11.Gao Y., Huang Y., Zhang R., Yang Y., Zhang Q., Hou M. Benign Prostatic Hyperplasia: Prostatic Arterial Embolization versus Transurethral Resection of the Prostate—A Prospective, Randomized, and Controlled Clinical Trial. Radiology. 2014;270(3):920–928. doi: 10.1148/radiol.13122803. [DOI] [PubMed] [Google Scholar]
- 12.Cakir S.S., Polat E.C., Ozcan L., Besiroglu H., Ötunctemur A., Ozbek E. The effect of prostatic inflammation on clinical outcomes in patients with benign prostate hyperplasia. Prostate Int. 2018;6(2):71–74. doi: 10.1016/j.prnil.2017.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Taneja Y., Ram P., Kumar S., Kumar S., Raj K., Singh C. Comparison of Visual Prostate Symptom Score and International Prostate Symptom Score in the evaluation of men with benign prostatic hyperplasia: A prospective study from an Indian population. Prostate Int. 2017;5(4):158–161. doi: 10.1016/j.prnil.2017.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Demirdag C., Citgez S., Tunc B., Simsekoglu F., Can G., Onal B. The Clinical Effect of Bipolar and Monopolar Transurethral Resection of the Prostate More Than 60 Milliliters. Urology. 2016;98:132–137. doi: 10.1016/j.urology.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 15.Ray A.F., Powell J., Speakman M.J., Longford N.T., DasGupta R., Bryant T. Efficacy and safety of prostate artery embolization for benign prostatic hyperplasia: An observational study and propensity-matched comparison with transurethral resection of the prostate (the UK-ROPE study) BJU Int. 2018:270–282. doi: 10.1111/bju.14249. [DOI] [PubMed] [Google Scholar]
- 16.Shim S.R., Kanhai K.J.K., Ko Y.M., Kim J.H. Efficacy and Safety of Prostatic Arterial Embolization: Systematic Review with Meta-Analysis and Meta-Regression. J Urol. 2017;197(2):465–479. doi: 10.1016/j.juro.2016.08.100. [DOI] [PubMed] [Google Scholar]
- 17.Christidis D., Clarebrough E., Ly V., Perera M., Woo H., Lawrentschuk N. Prostatic artery embolization for benign prostatic obstruction: assessment of safety and efficacy. World J Urol. 2018;36(4):575–584. doi: 10.1007/s00345-018-2220-z. [DOI] [PubMed] [Google Scholar]
- 18.Carnevale F.C., Iscaife A., Yoshinaga E.M., Moreira A.M., Antunes A.A., Srougi M. Transurethral Resection of the Prostate (TURP) Versus Original and PErFecTED Prostate Artery Embolization (PAE) Due to Benign Prostatic Hyperplasia (BPH): Preliminary Results of a Single Center, Prospective, Urodynamic-Controlled Analysis. Cardiovasc Intervent Radiol. 2016;39(1):44–52. doi: 10.1007/s00270-015-1202-4. [DOI] [PubMed] [Google Scholar]
- 19.Roehrborn C.G., Rosen R.C. Medical therapy options for aging men with benign prostatic hyperplasia: Focus on alfuzosin 10 mg once daily. Clin Interv Aging. 2008;3(3):511–524. doi: 10.2147/cia.s3635. [DOI] [PMC free article] [PubMed] [Google Scholar]