Abstract
The SARS-CoV-2 pandemic has highlighted the crucial role of pathologists in the health care system at a time of significant decline in the number of US medical students matching to pathology residency positions. To understand this decline, a national survey of fourth-year US allopathic medical students was conducted to assess experiences, knowledge, and attitudes of pathology and factors that impact specialty choice. Participating in a separate pathology course did not increase the probability of choosing pathology. Experiences significantly associated with choosing pathology included clinical or research opportunities in pathology during the last 2 years of medical school, autopsy observation/participation, and participation in pathology interest groups. Many respondents felt they were not sufficiently exposed to pathology to consider it as a specialty. Those who considered pathology but did not choose it were less likely to report understanding the activities of pathologists and being recruited by pathology faculty and more likely to express a preference for more direct patient contact as compared to those entering pathology. In general, respondents agreed that pathology has a good work–life balance and a satisfying degree of intellectual challenge. On the other hand, respondents generally agreed that information on social media and perception of the pathology job market do not seem to be positive and few agreed that pathology is a highly regarded specialty. We identify steps to address these issues and increase the number of US medical students choosing pathology as a specialty crucial to the future of medicine and public health.
Keywords: career choices, pathology, pathology residency, specialty choice, medical student
Introduction
There has been a significant decrease in the number of graduating US medical students matching to pathology residency positions. Based on Match data published by the National Resident Matching Program (NRMP), the percentage of pathology positions filled by US seniors over the past 6 years has fairly steadily declined with numbers of US seniors filling the following percentages of postgraduate year 1 pathology positions offered through the Match: 2015—46.6%, 2016—42.8%, 2017—35.9%, 2018—36.6%, 2019—33.4%, and 2020—33.8%.1,2 Pathology also ranks lower in attracting US seniors in comparison to other specialties. For example, in the 2020 Match, US seniors accounted for 40.2% of categorical internal medicine positions, 68.3% of anesthesiology positions, 67.3% of categorical surgery positions, 60.4% of categorical pediatric positions, 75.5% of obstetrics-gynecology positions, 40.7% of diagnostic radiology positions, and 80.8% of orthopedic surgery positions.2
In the late 1980s and early 1990s, there appears to have been a similar issue with recruiting trainees as well as concerns over trainee and practicing pathologist attrition.3 At that time, factors influencing students against choosing a career in pathology included a perceived job shortage, negative statements about the specialty from other physicians and pathologists, the addition of a fifth year of training, and a lack of patient contact.4,5 Positive pathologist role models were found to be a positive influence and a valuable resource for recruitment.5 Based on anecdotal evidence, the current decline may be related to changes in the undergraduate medical school curriculum over the past decade that have resulted in decreased exposure to pathology and pathologists, a negative perception of the current pathology job market, and negative feedback about the specialty posted on social media platforms.
Multiple studies from Canada have explored similar issues with recruitment to pathology in that country in the 2000s. One survey found that in addition to a lack of significant direct patient contact, some students cited insufficient or inadequate experience in pathology or misconceptions or stereotypes about the profession as reasons why they did not choose pathology.6 Another focus group based study found that pathology was “utterly invisible in clinical practice” and it wasn’t that students had rejected pathology, it was that the specialty was ignored. This study suggested that promoting experiences in pathology may improve recruitment.7 A third earlier study looking specifically at the impact of a change to problem-based learning (PBL) curriculum found that graduates from non-PBL and PBL curriculums were equally likely to choose pathology as a career.8
Given the projected shortage of pathologists in the near future, it is important to identify factors that may be contributing to this decline in interest to optimize recruitment efforts.9 By surveying graduating allopathic medical students about their knowledge, experiences, and attitudes about pathology, we may identify why US medical graduates are not choosing a career in pathology. Understanding factors and influences that may negatively or positively impact selection of pathology as a career choice may result in strategies to combat the current trend in decreasing applications to pathology residencies by US medical graduates.
Materials and Methods
We conducted a national survey of fourth-year US allopathic medical students graduating in spring 2019 to evaluate their experience with pathology in their medical school curriculum, the factors that impacted their specialty choice, and their knowledge of and interest in the field of pathology. The purpose of this survey was to better understand factors that influence medical students’ decision surrounding specialty choice to develop recommendations for improving recruitment of medical students into pathology. The institutional review board of The University of Oklahoma Health Sciences Center approved the study.
An email explaining the purpose of the survey and including a link to the survey instrument was sent to the Associate Dean of Student Affairs (or other relevant administrator) at US allopathic medical schools with a request to forward the survey to all graduating medical students at their respective institutions. The Chair of the Department of Pathology for each institution was also copied on the email request. The survey was administered through Survey Monkey and the survey was open from April 19, 2019, through May 16, 2019. A follow-up email was sent at the midpoint of the survey window to encourage participation. As an incentive to participate, deans were also offered the opportunity to receive aggregate survey data for their school upon request as this information may be beneficial for purposes of career advising, which is a Liaison Committee on Medical Education required standard for accreditation.10
The specialty choice interest survey was developed by the College of American Pathologists Graduate Medical Education Committee (CAP GMEC) and was designed to make comparisons between those students who considered a career in pathology (ie, researched the specialty and made a conscious decision to either include or not include pathology in their rank list) versus those who did not consider the specialty. The survey asked specifically about the students’ experiences and exposure to pathology in their medical school curriculum, factors that influenced specialty choice and timing of their decision-making, and attitudes about and knowledge of the field of pathology.
Responses were summarized using descriptive statistics. One-way analysis of variance and 2-way χ2 tests were used to compare results between groups of respondents. Statistical analyses were performed using IBM SPSS Statistics for Windows, version 25.0 (IBM Corp).
Results
Respondent Demographics
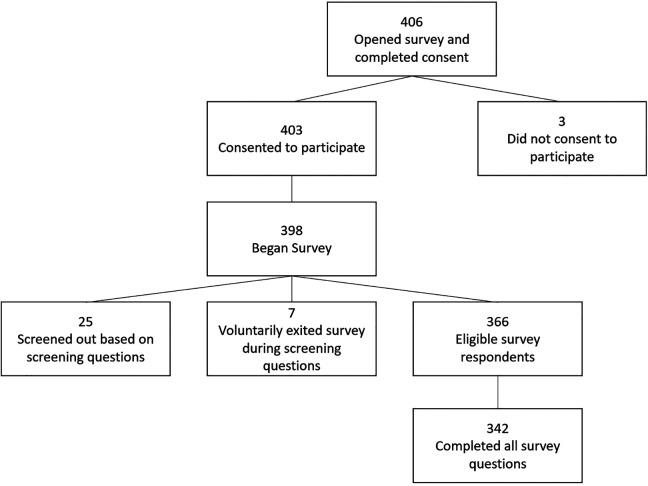
Deans at 137 US allopathic medical schools received emails requesting the survey be forwarded to graduating medical students at their institutions. Survey responses reflect participation from students at 30 different medical schools for a response rate of at least one student respondent from 22% (N = 30 of 137) of US allopathic schools surveyed. Four hundred and six students opened the survey, of which, 398 students agreed to participate and began the survey. Twenty-five students did not meet the survey eligibility requirements (ie, graduating in spring 2019 and participated in a match process) and were screened out. This resulted in 366 eligible survey respondents, and 342 of these students completed all survey questions (see Figure 1). Among those respondents who chose to answer demographic questions, approximately half were female and half were male with the majority identifying as white and between the ages of 25 and 29 years (Table 1).
Figure 1.
Medical student survey participation.
Table 1.
Demographic Data.
| Frequency | Percent | |
|---|---|---|
| Sex | ||
| Male | 167 | 50 |
| Female | 168 | 50 |
| Total respondents | 335 | |
| Age | ||
| <25 years old | 6 | 2 |
| 25-29 years old | 275 | 82 |
| 30-34 years old | 46 | 14 |
| 35-39 years old | 7 | 2 |
| 40-44 years old | 2 | 1 |
| >44 years old | 1 | 0 |
| Total respondents | 337 | |
| Ethnicity | ||
| White | 230 | 71 |
| Hispanic or Latino | 15 | 5 |
| Black or African American | 11 | 3 |
| Asian | 47 | 15 |
| American Indian or Alaskan Native | 3 | 1 |
| Middle Eastern or North African | 5 | 2 |
| Native Hawaiian or Pacific Islander | 0 | 0 |
| Other (please specify)* | 13 | 4 |
| Total respondents | 324 | |
| Education | ||
| Undergraduate degree† | ||
| Biology | 130 | 40 |
| Biochemistry | 31 | 9 |
| Neuroscience/Neurobiology | 30 | 9 |
| Chemistry | 23 | 7 |
| Psychology | 22 | 7 |
| Total respondents | 327 | |
| Graduate degree | ||
| PhD‡ | 15 | 26 |
| MS | 22 | 39 |
| MPH | 16 | 28 |
| MBA | 1 | 2 |
| JD | 0 | 0 |
| Other§ | 6 | 11 |
| Total respondents | 57 |
* Other included the following responses: Black/white, Caucasian/Hispanic/Middle Eastern, Jewish, Mixed race, Pakistani, white and Middle Eastern, white and Asian, and white/subcontinental Indian.
† These responses were open-ended and only degrees noted by >5% of respondents are listed.
‡ PhD fields included the following responses: Biochemistry and Molecular Biology, Bioinformatics, Biomedical Engineering, Biomedical Sciences with concentration in Neuroscience, Cancer Immunology, Immunology, Multiple Sclerosis Research, Neuropathology, and Neuroscience.
§ Other degrees included the following: Master of Arts, Master of Arts in Medical Sciences, Master of Health Science, and Master of Forensic Science.
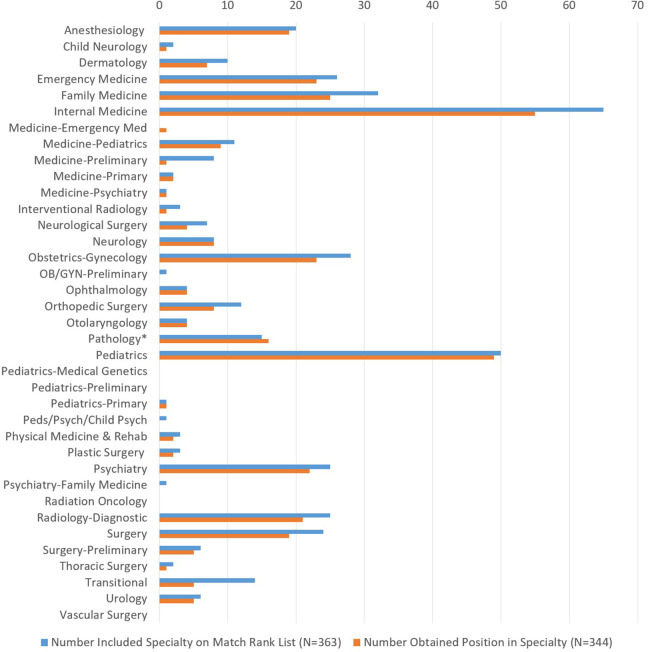
Respondent Specialty Choice
Most respondents (88%, N = 328 of 374) participated in the NRMP Match to obtain a residency position, with the Military Match being the most common alternative match process. Respondents (85%, N = 310 of 365) most frequently included one medical specialty on their Match rank list. Most respondents (96%, N = 345 of 361) obtained a residency position through a match process. Eleven (69%) of the 16 respondents who did not obtain a position in the main NRMP Match considered a different specialty in the Supplemental Offer and Acceptance Program (SOAP) of the NRMP Match. The most common specialty considered in the SOAP was Family Medicine (45%, N = 5 of 11). Pathology, Internal Medicine, and Surgery—Preliminary were each considered by 3 (27%) respondents (N = 3 of 11). Figure 2 shows the number of respondents who ranked programs in each medical specialty as compared to the number who ultimately obtained positions in the specialty. With regard to pathology, the 15 respondents represented in Figure 2 only ranked pathology programs in the Match and did not rank other specialties.
Figure 2.
National Resident Matching Program (NRMP) Match preferences and outcome. One respondent who obtained a position in pathology did not provide data on the specialties included on his/her Match rank list. Therefore, for pathology, the number included specialty on Match rank list value is less than the number obtained position in specialty.
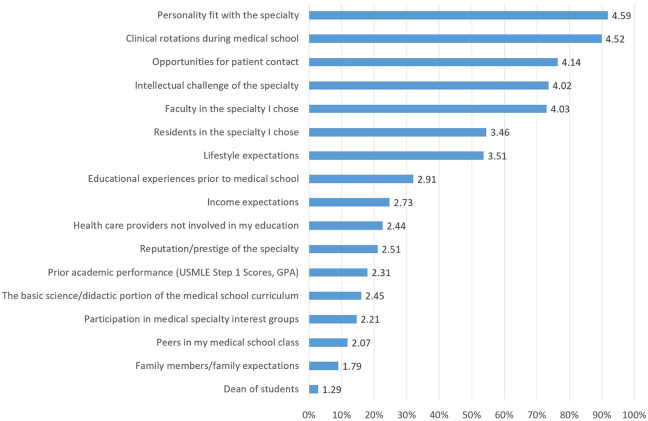
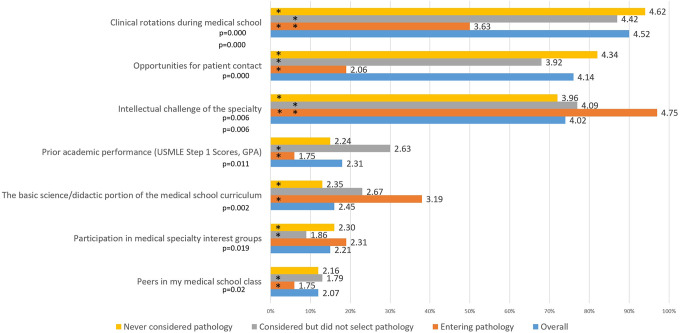
Timing and Factors Influencing Specialty Choice
Over half of the respondents (55%, N = 202 of 364) decided on their medical specialty during their third year of medical school, and 18% (N = 66 of 364) made their decision during their fourth year. Another 16% (N = 58 of 364) had decided on their specialty prior to entering medical school. For students entering pathology, 25% (N = 4 of 16) decided to enter the field of pathology prior to starting medical school, while 25% (N = 4 of 16) and 13% (N = 2 of 16) decided on pathology during their third or fourth year of medical school, respectively. Figure 3 illustrates respondents’ self-reports of the extent to which various specialty characteristics and educational and personal factors influenced their medical specialty choice. Personality fit with the specialty and clinical rotations during medical school had the greatest influence on specialty choice for respondents as a whole. Figure 4 indicates statistically significant differences when comparing influence factors for students who never considered pathology, students who considered pathology but ultimately selected another specialty, and those students who chose to enter pathology. Students entering pathology rated the didactic portion of the medical school curriculum (F 2,347 = 6.123, P = .002) and the intellectual challenge of the specialty chosen (F 2,347 = 5.236, P = .006) as having a greater influence on their specialty decision as compared to those who did not consider pathology. Those entering pathology rated opportunities for patient contact (F 2,347 = 46.611, P = .000) and clinical rotations during medical school (F 2,347 = 14.488, P = .000) as less important factors compared to both other groups, and prior academic performance (F 2,347 = 4.524, P = .011) as less important compared to those who considered but did not select pathology.
Figure 3.
Factors impacting specialty choice. The numbers labeling each bar indicate the mean rating across all respondents. The percentage on the x-axis designates the percent responding very much so (5) or for the most part (4).
Figure 4.
Factors impacting specialty choice: Statistically significant differences between respondent groups. Significance was tested via 1-way analysis of variance. *The groups demonstrating significant differences in responses for each factor. The numbers labeling each bar indicate the mean rating across all respondents. The percentage on the x-axis designates the percent responding very much so (5) or for the most part (4).
Respondent Pathology Exposure
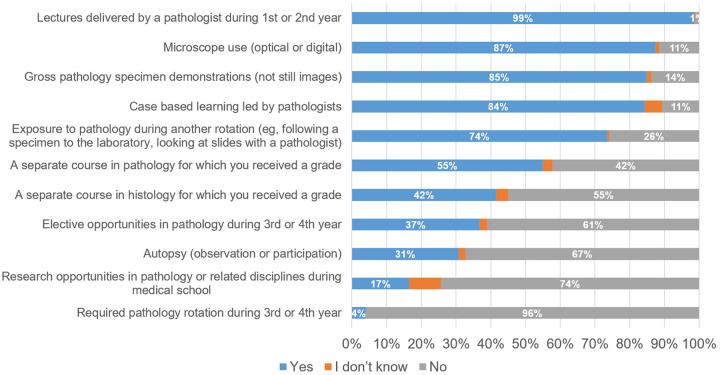
Figure 5 provides detailed information on student exposure to pathology and pathologists in their medical school curricula. Nearly all respondents (99%, N = 346 of 351) participated in lectures delivered by a pathologist during their first or second year of medical school. Fifty-five percent (N = 193 of 351) had completed a separate course in pathology as part of their curriculum as opposed to an integrated curriculum. Very few respondents participated in a required pathology clinical rotation during the third or fourth year of medical school (4%, N = 14 of 351), while a greater percentage reported participation in elective opportunities in pathology (37%, N = 129 of 351) during their third or fourth year of medical school. Nearly two-thirds of respondents (64%, N = 225 of 351) selected I don’t know when asked if their medical school offered a post-sophomore fellowship in pathology, while only 13% (N = 45 of 351) responded Yes to this question representing 7 different medical schools (25% or N = 7 of 28 schools with responses to this question). Only 3 (1%) of 349 respondents had participated in a post-sophomore pathology fellowship during their medical education. Fifty-five percent of respondents (N = 193 of 351), representing 21 medical schools (N = 21 of 28 or 75% of schools with responses to the question), indicated their medical school had a pathology interest group. A notable percentage (40%, N = 139 of 351) of respondents did not know if their medical school had a pathology interest group. Notably, 32% of respondents (N = 94 of 298) from schools with a pathology interest group stated that they did not know if their school had a pathology interest group and 4% of respondents (N = 11 of 298) from these schools stated they did not have a pathology interest group. This suggests these students were unaware or misinformed about the presence of an interest group at their medical school.
Figure 5.
Integration of pathology in medical school curriculum.
A small number of respondents had a friend, family member, or mentor who was a pathologist (19%, N = 65 of 349) or clinical/medical laboratory scientist (23%, N = 82 of 349). Similarly, few respondents reported prior education or work experience in related fields with 17% (N = 61 of 350) indicating they had worked in a clinical/hospital laboratory handling specimens, 3% (N = 10 of 350) reporting a degree in medical or clinical laboratory science or medical technology, and 1% (N = 4 of 349) reporting a degree or work in the field of forensics.
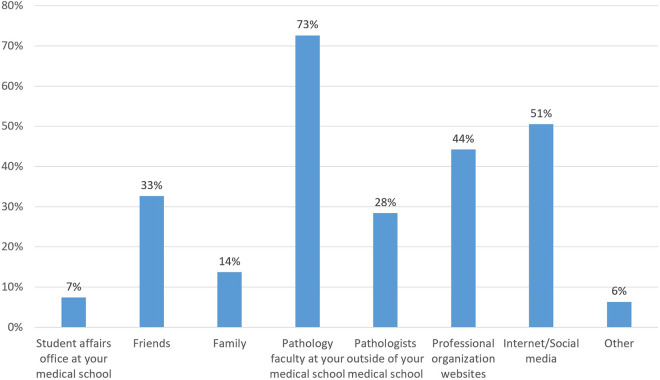
Of the 350 respondents, 94 (27%) indicated they had considered a career in pathology. Figure 6 shows the percentage of these respondents who used different resources to research the field of pathology. The 3 most common resources selected by respondents included pathology faculty at their medical school, the internet/social media, and professional organization websites. Respondents who used the internet/social media to research pathology were asked to list the sites used. Thirty-five (73%) of 48 respondents commented. Sites utilized included Student Doctor Network (26%, N = 9 of 35), American Association of Medical Colleges (AAMC; 20%, N = 7 of 35), CAP (20%, N = 7 of 35), Google (20%, N = 7 of 35), and Reddit (17%, N = 6 of 35).
Figure 6.
Resources used to research pathology. Respondents selecting “other” most commonly described an experience during medical school.
Respondent Perceptions of Pathology
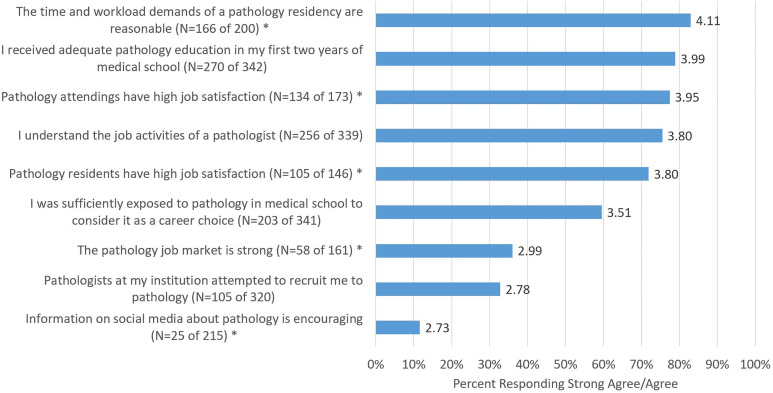
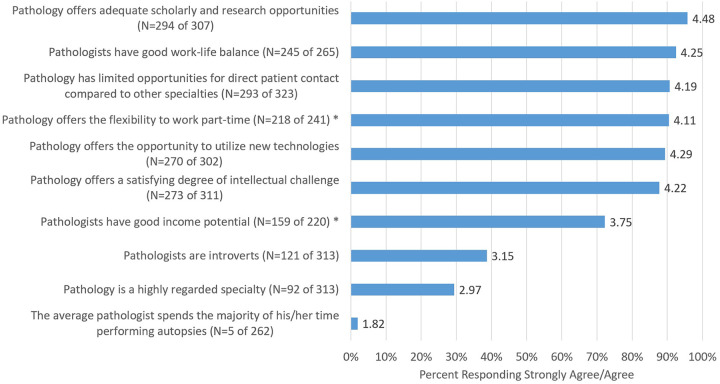
All respondents were asked to rate statements concerning their perceptions of their exposure to the field of pathology (Figure 7) and their perceptions of pathology as a medical specialty (Figure 8). Statements were rated on a scale ranging from strongly disagree (1) to strongly agree (5). Respondents were also given the option to choose “NA/Don’t know enough about pathology to answer” as opposed to rating the statement. Agreement varied across items; however, many students were not sufficiently exposed to pathology to consider it as a specialty, information on social media and perception of the pathology job market do not seem to be positive, and few respondents agreed that pathology is a highly regarded specialty. On the other hand, many students responded that pathologists have a good work–life balance and pathology offers a satisfying degree of intellectual challenge. It should also be noted that a sizable number of respondents reported they do not know enough about pathology to rate many statements, reinforcing the perception of a lack of exposure to the field (see Supplemental Table 1).
Figure 7.
Perceptions of pathology exposure. The numbers labeling each bar indicate the mean rating across all respondents. The percentage on the x-axis designates the percent responding strongly agree (5) or agree (4). *>100 respondents answered “NA/Don’t know enough about pathology to answer.”
Figure 8.
Perceptions of pathology as a medical specialty. The numbers labeling each bar indicate the mean rating across all respondents. The percentage on the x-axis designates the percent responding strongly agree (5) or agree (4). *>100 respondents answered “NA/Don’t know enough about pathology to answer.”
Comparison Between Respondents Considering Pathology Versus Those Not Considering the Field
Comparisons of responses were made between those who considered pathology for a career versus those who did not consider the specialty. Table 2 compares integration of pathology into the curriculum as experienced between the 2 groups. Notably, items that were likely elective or extracurricular experiences demonstrated statistically significant differences in terms of participation. These included elective opportunities in pathology during the third or fourth year of medical school (χ2(1) = 26.593, P < .001), observation or participation in an autopsy (survey did not ask if this was elective or mandatory; χ2(1) = 22.952, P < .001), research opportunities in pathology or a related discipline during medical school (χ2(1) = 19.660, P < .001), and pathology interest group/activities (χ2(1) = 23.591, P < .001). Notably, there was no statistical difference observed between groups for the curriculum elements of having separate histology or pathology courses. When further subdividing respondents into those who entered pathology, those who considered but did not select pathology, and those who never considered pathology, curriculum factors including elective opportunities in pathology during the third or fourth year of medical school (χ2(2) = 39.415, P = .000), observation or participation in an autopsy (χ2(2) = 38.730, P = .000), research opportunities in pathology or a related discipline during medical school (χ2(2) = 32.770, P = .000), and pathology interest group/activities (χ2(2) = 24.930, P = .000) remained significantly different between all groups. Those respondents who considered but did not select pathology had much lower participation in all of these activities as compared to students who chose pathology. This finding may suggest that many students interested in pathology are not participating in important curriculum opportunities that might lead them to choose a career in the specialty.
Table 2.
Comparison of Integration of Pathology Into the Medical School Curriculum for Those Respondents Who Considered Pathology as a Career Choice Versus Those Who Did Not.
| Did you participate in the following during medical school? | Pathology considered | Pathology not considered | Significance* | |
|---|---|---|---|---|
| A separate course in histology for which you received a grade | Total N | 90 | 247 | χ2(1) = .101, P = .75 |
| Yes | 44% (40) | 43% (105) | ||
| No | 56% (50) | 57% (142) | ||
| A separate course in pathology for which you received a grade | Total N | 90 | 249 | χ2(1) = .564, P = .45 |
| Yes | 60% (54) | 55% (138) | ||
| No | 40% (36) | 45% (111) | ||
| Lectures delivered by a pathologist during first or second year | Total N | 94 | 254 | χ2(1) = 1.085, P = .30 |
| Yes | 98% (92) | 99% (252) | ||
| No | 2% (2) | 1% (2) | ||
| Required pathology rotation during third or fourth year | Total N | 94 | 255 | χ2(1) = 1.186, P = .28 |
| Yes | 2% (2) | 5% (12) | ||
| No | 98% (92) | 95% (243) | ||
| Elective opportunities in pathology during third or fourth year | Total N | 92 | 249 | χ2(1) = 26.593, P < .001 |
| Yes | 60% (55) | 29% (73) | ||
| No | 40% (37) | 71% (176) | ||
| Autopsy (observation or participation) | Total N | 92 | 250 | χ2(1) = 22.952, P < .001 |
| Yes | 51% (47) | 24% (60) | ||
| No | 49% (45) | 76% (190) | ||
| Microscope use (optical or digital) | Total N | 93 | 252 | χ2(1) = 2.055, P = .15 |
| Yes | 93% (86) | 87% (219) | ||
| No | 7% (7) | 13% (33) | ||
| Gross pathology specimen demonstrations (not still images) | Total N | 94 | 249 | χ2(1) = .438, P = .51 |
| Yes | 88% (83) | 86% (213) | ||
| No | 12% (11) | 14% (36) | ||
| Case based learning led by pathologists | Total N | 89 | 242 | χ2(1) = 1.441, P = .23 |
| Yes | 85% (76) | 90% (218) | ||
| No | 15% (13) | 10% (24) | ||
| Research opportunities in pathology or related disciplines during medical school | Total N | 89 | 228 | χ2(1) = 19.660, P < .001 |
| Yes | 34% (30) | 12% (28) | ||
| No | 66% (59) | 88% (200) | ||
| Exposure to pathology during another rotation (eg, following a specimen to the laboratory, looking at slides with a pathologist) | Total N | 93 | 254 | χ2(1) = .433, P = .51 |
| Yes | 76% (71) | 73% (185) | ||
| No | 24% (22) | 27% (69) |
* Significance was tested via 2-way χ2 test.
Table 3 compares other educational activities and personal factors for those respondents who considered pathology as a career choice versus those who did not. Of interest, a significantly greater percentage of medical students who considered pathology had a friend, family member, or mentor who was a pathologist (χ2(1) = 23.599, P < .001). However, there was not a statistically significant relationship between having a friend, family member, or mentor who was a clinical or medical/laboratory scientist and interest in pathology as a career choice. Understandably, respondents interested in pathology were significantly more likely to have participated in a pathology interest group activity (χ2(1) = 23.591, P < .001).
Table 3.
Comparison of Other Educational Activities and Personal Factors for Those Respondents Who Considered Pathology as a Career Choice Versus Those Who Did Not.
| Other educational activities or personal factors | Pathology considered | Pathology not considered | Significance* | |
|---|---|---|---|---|
| Does your medical school have a post-sophomore pathology fellowship? | Total N | 41 | 84 | χ2(1) = 5.226, P = .02 |
| Yes | 22% (9) | 43% (36) | ||
| No | 78% (32) | 57% (48) | ||
| Does your medical school have a pathology interest group? | Total N | 65 | 145 | χ2(1) = .210, P = .65 |
| Yes | 92% (60) | 90% (131) | ||
| No | 8% (5) | 10% (14) | ||
| Have you participated in pathology interest group activities? | Total N | 60 | 131 | χ2(1) = 23.591, P < .001 |
| Yes | 48% (29) | 15% (20) | ||
| No | 52% (31) | 85% (111) | ||
| Do you have a friend, family member, or mentor in the following roles? Pathologist | Total N | 93 | 255 | χ2(1) = 23.599, P < .001 |
| Yes | 36% (33) | 13% (32) | ||
| No | 64% (60) | 87% (223) | ||
| Do you have a friend, family member, or mentor in the following roles? Clinical/medical laboratory scientist | Total N | 93 | 255 | χ2(1) = 2.108, P = .15 |
| Yes | 29% (27) | 22% (55) | ||
| No | 71% (66) | 78% (200) | ||
| Do you have previous experience working in a clinical/hospital laboratory handling patient specimens? | Total N | 94 | 255 | χ2(1) = .825, P = .36 |
| Yes | 20% (19) | 16% (41) | ||
| No | 80% (75) | 84% (214) |
* Significance was tested via 2-way χ2 test.
Tables 4 and 5 compare perceptions of exposure to pathology and pathology as a medical specialty for those respondents who considered pathology as a career choice versus those who did not. Respondents considering pathology as a career choice expressed statistically greater agreement when rating statements indicating that they understood the job activities of a pathologist (t(206.993) = 5.397, P < .001), that pathologists at their institution attempted to recruit them (t(317) = 6.604, P < .001), and that residents and attending pathologists had high job satisfaction (Residents—t(137.287) = 4.162, P < .001; Attendings—t(170) = 3.561, P < .001). They were also more likely to express statistically greater agreement in statements indicating that pathology is a highly regarded specialty (t(310) = 2.449, P = .02; although this was rated low in both groups), that pathology offers a satisfying intellectual challenge (t(309) = 3.594, P < .001), and that pathology offers adequate opportunity for scholarly activity (t(304) = 2.715, P = .01). When further subdividing respondents into those who entered pathology, those who considered but did not select pathology, and those who never considered pathology, significant differences between groups were observed for the statements regarding receiving adequate pathology education during the first 2 years of medical school (F 2,339 = 5.314, P = .005), understanding the job activities of a pathologist (F 2,336 = 18.898, P = .000), and pathologists attempting to recruit students (F 2,317 = 23.487, P = .000). Students who considered pathology but chose another specialty were more likely to feel that their pathology education was adequate as compared to students entering pathology (F 2,339 = 5.314, P = .005), but less likely to report understanding the activities of pathology (F 2,336 = 18.898, P = .000) and being recruited by faculty as compared to those entering pathology (F 2,317 = 23.487, P = .000). Again, this finding suggests that medical students considering but not choosing pathology may not be receiving the information they need about the specialty to make an informed choice or benefiting from a pathologist mentor.
Table 4.
Comparison of Perceptions of Exposure to Pathology for Those Respondents Who Considered Pathology as a Career Choice Versus Those Who Did Not.
| Please rate your level of agreement with each of the following statements about pathology | Pathology considered | Pathology not considered | Significance* | ||||
|---|---|---|---|---|---|---|---|
| N | Mean | Top box %† | N | Mean | Top box %† | ||
| I understand the job activities of a pathologist | 92 | 4.13 | 90% | 246 | 3.68 | 70% | t(206.993) = 5.397, P < .001 |
| I received adequate pathology education in my first 2 years of medical school | 92 | 3.96 | 77% | 249 | 4.00 | 80% | t(339) = −.403, P = .69 |
| I was sufficiently exposed to pathology in medical school to consider it as a career choice | 92 | 3.61 | 62% | 248 | 3.47 | 59% | t(338) = 1.087, P = .28 |
| Information on social media about pathology is encouraging | 68 | 2.85 | 19% | 147 | 2.67 | 8% | t(213) = 1.474, P = .14 |
| The pathology job market is strong | 62 | 2.97 | 35% | 99 | 3.00 | 36% | t(159) = −.188, P = .85 |
| Pathologists at my institution attempted to recruit me to pathology | 90 | 3.39 | 56% | 229 | 2.53 | 24% | t(317) = 6.604, P < .001 |
| Pathology residents have high job satisfaction | 56 | 4.13 | 84% | 89 | 3.60 | 64% | t(137.287) = 4.162, P < .001 |
| The time and workload demands of a pathology residency are reasonable | 81 | 4.22 | 89% | 118 | 4.03 | 79% | t(197) = 1.815, P = .07 |
| Pathology attendings have high job satisfaction | 69 | 4.19 | 87% | 103 | 3.80 | 71% | t(170) = 3.561, P < .001 |
* Significance was tested via independent samples t tests.
† Values in this column are the percent selecting strongly agree or agree.
Table 5.
Comparison of Perceptions of Pathology as a Medical Specialty for Those Respondents Who Considered Pathology as a Career Choice Versus Those Who Did Not.
| Please rate your level of agreement with each of the following statements about pathology | Pathology considered | Pathology not considered | Significance* | ||||
|---|---|---|---|---|---|---|---|
| N | Mean | Top box† % | N | Mean | Top box† % | ||
| Pathology is a highly regarded specialty | 90 | 3.17 | 41% | 222 | 2.89 | 25% | t(310) = 2.449, P = .02 |
| Pathology offers the flexibility to work part-time | 77 | 4.18 | 92% | 163 | 4.08 | 90% | t(238) = 1.178, P = .24 |
| Pathologists have good work–life balance | 87 | 4.33 | 95% | 177 | 4.21 | 91% | t(262) = 1.632, P = .10 |
| Pathologists have good income potential | 79 | 3.75 | 72% | 140 | 3.75 | 73% | t(217) = −.028, P = .98 |
| The average pathologist spends the majority of his/her time performing autopsies | 84 | 1.69 | 0% | 177 | 1.89 | 3% | t(259) = −2.367, P = .02 |
| Pathology has limited opportunities for direct patient contact compared to other specialties | 91 | 4.07 | 88% | 231 | 4.24 | 92% | t(320) = −1.934, P = .05 |
| Pathologists are introverts | 89 | 2.98 | 29% | 223 | 3.22 | 43% | t(180.376) = −2.053, P = .04 |
| Pathology offers a satisfying degree of intellectual challenge | 91 | 4.45 | 95% | 220 | 4.13 | 85% | t(309) = 3.594, P < .001 |
| Pathology offers adequate scholarly and research opportunities | 85 | 4.64 | 96% | 221 | 4.42 | 95% | t(304) = 2.715, P = .01 |
| Pathology offers the opportunity to utilize new technologies | 88 | 4.39 | 92% | 213 | 4.25 | 88% | t(299) = 1.582, P = .12 |
* Significance was tested via independent samples t tests.
† Values in this column are the percent selecting strongly agree or agree.
Differences in Responses by Gender
There was no relationship between identified gender and consideration of pathology as a career choice, with both female and male respondents considering pathology in similar numbers (χ2(1) = .808, P = .369). There were some statistically significant differences in responses between genders for both factors influencing specialty choice and perceptions of pathology. Females were more likely to rate opportunities for patient contact as a more important factor in specialty choice (mean rating 4.32 vs 3.98; t(333) = −2.980, P = .003), while males rated lifestyle expectations (mean rating 3.71 vs 3.28; t(325.751) = 3.350, P = .001), income expectations (mean rating 3.01 vs 2.42; t(332) = 4.608, P = .000), reputation/prestige of the specialty (mean rating 2.68 vs 2.38; t(333) = 2.109, P = .036), and prior academic performance (mean rating 2.47 vs 2.14; t(330.753) = 2.433, P = .016) as being more influential factors. Female respondents were more likely to rate statements on the strength of the pathology job market (mean rating 3.18 vs 2.79; t(153) = −2.330, P = .021), the reputation of pathology on social media (mean rating 2.90 vs 2.59; t(200.706) = −2.659, P = .008), and the income potential of pathology (mean rating 3.90 vs 3.62; t(195.995) = −2.658, P = .009) more positively as compared to male respondents. Male respondents were more likely to feel that pathology has limited opportunities for direct patient contact compared to other specialties (mean rating 4.29 vs 4.10; t(314) = −2.294, P = .022), to feel that they received adequate pathology education during their first 2 years of medical school (mean rating 4.01 vs 3.89; t(331) = 2.410, P = .016), and to feel that pathology offers adequate scholarly research opportunities (mean rating 4.57 vs 4.38; t(298) = 2.745, P = .006) as compared to females.
Free-Text Responses Regarding Specialty Choice
Survey respondents who did not consider a career in pathology were asked to comment as to why they did not consider pathology as a career option. Two hundred and nineteen of 256 or 86% of respondents in this group provided free-text comments in response to this question. Thematic analysis of these comments identified 4 common themes among respondents including preference for more patient contact (68%, N = 148 of 219), interest in a different specialty (11%, N = 25 of 219), lack of interest/perception pathology is boring (11%, N = 24 of 219), and not interested in working in a laboratory/using a microscope (9%, N = 20 of 219).
Survey respondents who did consider a career in pathology were asked to comment as to why they ultimately did (14 respondents) or did not (68 respondents) choose pathology as a career. Thematic analysis of these comments identified common themes among respondents. For those respondents who chose pathology for their career, the most common reasons included perceived “fit” (29%, N = 4 of 14), preference for diagnostic medicine (29%, N = 4 of 14), and intellectual stimulation (21%, N = 3 of 14). For those respondents who had considered pathology but ultimately chose another specialty, the most common reasons for not choosing pathology included preference for more patient contact (54%, N = 37 of 68), greater interest in a different specialty (24%, N = 16 of 68), job market concerns (19%, N = 13 of 68), not interested in pathology (12%, N = 8 of 68), limited exposure to the specialty (10%, N = 7 of 68), and income (9%, N = 6 of 68).
Discussion
The process by which medical students make career decisions and the factors that play into it are not fully understood; however, there is some literature that begins to address this complex decision-making process. Querido et al propose that factors influencing medical students’ career choices can be grouped into 5 major categories: “(1) medical school characteristics (e.g., curriculum structure), (2) student characteristics (e.g., age, personality), (3) student values (e.g., personal preference), (4) career needs to be satisfying (e.g., expected income, status, work-life balance), and (5) perception of specialty characteristics (e.g., extracurricular or curricular experiences).”11(p18) Importantly, they argue that career decision-making among medical students is an evolutionary process along the continuum of undergraduate medical training, implying that influences, factors, and realizations during medical school inform the ultimate career choice that students make.11
In our study of graduating US allopathic medical students, our goal was to evaluate many of the factors proposed by Querido et al as they relate to the field of pathology, specifically querying students after their career choice had been made, in an effort to better understand what influenced students in their choice. As NRMP data indicate, there has been a decline over the past few years in US medical student interest in pathology with decreasing numbers of graduates matching into the specialty. Leading hypotheses among the CAP GMEC members surrounding this shift mirror those from studies of previous decades, including a perceived poor job market and poor perception of the specialty. Other hypothesis considered by our group also centered on the educational experience of students and how this has changed over the past decade with a move to a more integrated curriculum in US allopathic medical schools.
In regard to curriculum, it was hypothesized that a shift in curriculum to a more integrated approach with elimination of the traditional histology and pathology courses would result in decreasing interest in the specialty by students due to decreased or more episodic exposure as opposed to longitudinal exposure to pathologists in the basic sciences years. Also, there was a concern that without a more traditional, lecture-based standalone course, the recognition of pathology as a distinct discipline might also be lost. Previous studies suggest that the basic science curriculum may not be as influential as assumed, or at least not in its traditional format. In a study by Ford, he found that Canadian medical students were about equally as likely to rank pathology first in residency applications whether or not they studied in a school with a PBL- or non-PBL-based curriculum. In this study, the curriculum wasn’t well-defined and the curriculum designation was based on whether or not the school described their curriculum as having a dominant component of PBL. Another study by Holland and Bosch surveyed second-year medical students at multiple medical schools over 2 time points in the 1990s and early 2000s at the beginning and end of their second-year pathology course and found that the course was “ineffective at influencing students’ perceptions of pathology.”12 In this study, participating in a pathology course did not positively impact students’ probability of becoming a pathologist. Students generally had a somewhat better understanding of what a pathologist does as part of their job, particularly in anatomic pathology, but they had not changed how they viewed pathology as a career.12
In our study, the vast majority of students indicated that they had participated in lectures (99%, N = 346 of 351) or case-based learning activities (84%, N = 296 of 351) led by pathologists. Most had also used a microscope (optical or digital; 87%, N = 307 of 351) and/or participated in gross pathology specimen demonstrations (85%, N = 297 of 350). The majority of students (74%, N = 258 of 351) had also been exposed to pathology on a rotation in another specialty, which likely better highlights the job of a pathologist as compared to the pathology content in a didactic curriculum. These data suggest that students still do have significant, or at least memorable, exposure to pathologists and tools of the specialty within their medical school experience despite changes in the curriculum. Interestingly, there was no difference in rates of students who considered pathology versus those who did not based on medical school curriculum, with similar rates of interest in students from schools that were reported to have standalone pathology or histology courses versus those that reportedly did not. This does not support the hypothesis that a change in curriculum to an integrated approach has negatively impacted US allopathic medical students’ interest in pathology.
In evaluating the impact of curriculum beyond the first 2 years of medical school, pathology is much less visible as a specialty with fewer students participating in pathology rotations or pathology-related activities such as autopsy or pathology research. Clinical rotations during medical school were listed to be the second highest rated factor in impacting students’ specialty choice and fully 73% of students chose their specialty in the third or fourth year of medical school—a time at which pathology is not represented for most students in their medical education. Alarmingly, students who considered pathology but did not choose the specialty for their career reported less participation in elective opportunities in pathology in the third and fourth year of medical school as compared to their colleagues who chose pathology and were less likely to indicate pathology faculty at their institutions attempted to recruit them into the specialty as compared to those students who were entering the field. These data suggest that not only are we missing those students who may not have the exposure to pathology to even consider it as a career choice, we are also not identifying students with potential interest and giving them the experiences to make an informed decision about the profession.
In our study, the second most common source medical students use to learn about pathology is the internet to include social media sites. When asked to rate the statement “Information on social media about pathology is encouraging,” only 12% of respondents (N = 25 of 215) rated it agree or strongly agree. In an attempt to change this, the CAP Residents Forum (RF) is adding content on the CAP website to help educate medical students (https://www.cap.org/member-resources/residents/cap-for-medical-students). This content includes informational decks, videos on aspects of pathology, and posts that discuss why pathology is a rewarding specialty. Some of these posts directly take on misconceptions that are present on social media sites. The CAP RF is also using Twitter to educate medical students and debunk misconceptions about pathology.
One misconception is that the pathology job market is not strong. In our study, only 36% (58 of 161 respondents) agreed that the pathology job market is strong. Free-text comments on our survey also highlighted the impression that the pathology job market is not strong. Some of these comments include “perceived saturation of pathology (would have to live somewhere undesirable to get a good job)” and “I also was told anecdotally that the job market is hard from a…fellow who I worked with.” This perception is present on some social media sites and among some pathologists and other physicians. However, recent studies by our group show that the job market for graduating pathology residents and fellows has actually been fairly stable over much of the last decade and the perceived difficulty in finding a job is decreasing.13-15
Another finding in our survey is that pathology is not necessarily well thought of as a specialty by medical students. Only 29% (92 of 313 respondents) agreed that pathology is a highly regarded specialty, and this sentiment was also expressed in multiple respondents’ free-text comments. Likewise, pathology may not be seen as competitive or may perhaps be viewed as a fall back. This was highlighted in one respondent’s comment that their academic performance was adequate to consider another specialty. These perceptions have also been found in another study that evaluated Canadian students’ and residents’ impressions of pathology as a career. In that study, negative stereotypes of pathology and pathologists included low prestige of the specialty and perceptions that practicing pathology was a waste of medical skills and that pathologists were eccentric and lacked social competence.16 Who is perpetuating these perceptions? There are several possibilities. Pathologists who are unhappy with their career choice or situation may communicate this to their students. Other clinical specialty colleagues may also have these perceptions. Communication of these ideas to students may be direct and verbal but often is more covert and part of the hidden curriculum. The hidden curriculum is a type of informal learning that is not explicitly intended but is taught through the words and actions (or inactions) that occur in the clinical or learning environment. It is also knowledge gained from observing the medical culture at an institutional level through often unintentional comments or actions.17 How a physician in one specialty interacts with a physician in another specialty, such as pathology, can teach a medical student much about how pathologists are viewed by other physicians. Offhand comments and dismissive remarks can also communicate disregard for a clinical specialty. Pathologists who are unhappy in their job can also communicate this to students through words, body language, and emotional state.
The findings in this study are very similar to those that were done previously.3-7 A large number of the respondents in our study who did not choose pathology commented that they wanted to have more direct patient care than pathology would provide. Previous studies have shown the same finding. Likewise, previous studies also showed concerns about finding jobs after completing residency, insufficient experience with diagnostic pathology, and negative perceptions of pathology as a specialty.
From these findings, we feel there are a number of steps that can be taken in an attempt to increase the number of allopathic medical students who choose to go into pathology. Given that most respondents said they chose their specialty in the third and fourth year of medical school, increasing the visibility of and exposure to pathology in the clinical years could attract more students. Exposure to pathology in the basic science curriculum and through pathology interest groups is not enough as seen in our survey and that of Holland and Bosch.12 Students need to see and understand the role of pathology in diagnostic medicine and in the patient care team. Requiring a pathology rotation in the last 2 years of medical school could achieve this but finding time and support for this in the clinical curriculum may be difficult especially since pathology is such a small clinical specialty. Also, pathology departments may not have the resources to be able to support this. As diagnostic radiology also has a low percentage of allopathic medical students entering the specialty and has sparse patient contact similar to pathology, a combined radiology/pathology clinical experience in the third year of medical school could be more acceptable to curriculum deans and be beneficial to both specialties. Other ways to achieve visibility of pathology include increasing medical student exposure to pathology residents and attendings. This could be done by requiring medical students to follow specimens to the frozen section room while on surgery rotations, attending an autopsy on a patient they cared for, going to the laboratory to review a surgical pathology, peripheral blood smear, or microbiology specimen taken from one of their patients. Attendance at tumor boards to see the crucial role of the pathologist in diagnosis and treatment decisions would also increase visibility of the specialty. These would take coordination with our direct care clinical colleagues but knowledge of what pathologists do and can offer and their role in the clinical care team would be beneficial for students going into almost any specialty. It could also help to improve laboratory utilization, stewardship of resources, quality of care, and patient safety.
Improving the quality of interactions between pathologists (attendings and residents) and medical students is another step that can be taken. Pathologists need to be aware that how they interact with medical students can directly affect career decisions as well as what students, and eventually future physicians, think about the specialty of pathology. Willingness to teach students over the microscope, at an autopsy, in tumor board, or in the clinical laboratory can have an effect. Showing enthusiasm and excitement about what one is doing in the care of the patient will speak loudly to students. Each interaction is an opportunity to change perceptions and create good will.
Talking and advocating for our worth as pathologists with our colleagues in other specialties will be important in changing perceptions of pathology. Students pick up these perceptions from multiple sources but one source is likely our clinical colleagues through the hidden curriculum that occurs during clinical rotations. This issue is bigger than just recruiting medical students and would help the specialty in general. Pathologists need to be visible and seen by their colleagues as crucial members of the patient care team. By doing so, it is possible that perceptions of pathologists in both students and physicians in other specialties may change.
Identifying and mentoring medical students who show an interest in pathology is crucial. In our survey, respondents who considered pathology but chose another specialty showed a significantly lower agreement with the statement that pathologists recruited them into the specialty compared to students who chose pathology. This is also shown in comments where respondents said they were recruited by other specialties but not by pathologists and that they did not have a good understanding of what a pathologist does. Faculty development on identifying prospective residents among students, explaining what pathologists do, and providing effective mentoring of students is needed. Every interaction a pathologist has with a medical student is a chance to spark an interest in pathology, to further increase interest that is already there, or to educate about the job of a pathologist. Talking with students, whether in the classroom, over the microscope, in the laboratory, or after a tumor board conference is an opportunity to teach what pathologists do and to encourage and mentor students trying to decide what specialty to choose.
Our survey shows the internet, including social media, is a significant source of information for medical students wishing to learn about pathology. There needs to be support for the development of resources to provide quality, accurate information about the specialty to help counter negative messaging on some social media sites. Pathology specialty organizations and other stakeholders need to develop high-quality materials in the media that the current generation of medical students uses. The CAP RF is already working to do this with their short videos, blog posts, and Twitter feeds but more information and sources on different platforms and media would be useful.
As shown by our survey, there continues to be concern about a difficult pathology job market and low pathologist income even though recent publications by the CAP GMEC refute this.13-15 This continues to be a sustained interest and high priority of our committee and it is committed to continue providing data, particularly if it can be used to support the case to pursue the specialty and demonstrate residents are finding jobs.
There are several limitations of our study. This survey only measured a single point in time, in particular a point shortly after Match results were received. Thus, the survey does not capture the evolution of decision-making on specialty choice. Also, as we only surveyed one graduating class of allopathic medical students, we cannot assess for changes in opinions, attitudes, and experiences over time that may provide more insight into the decreasing number of US allopathic medical students choosing pathology. Another limitation is that we did not survey osteopathic students and this is planned for the near future. The sample size is small: 340 medical students responded representing only 22% of medical schools. Likewise, the number of respondents entering pathology residency is small (N = 16). Despite these, the age range represented by our sample is similar to that for US medical school graduates per AAMC data.18 Respondents are from schools representing all regions of the country and all sizes of medical schools. Compared with the racial makeup of the graduating class of 2019 according to AAMC data, our survey has a higher percentage of white respondents (71% vs 48%) and a lower percentage of African American (3% vs 8%) and Asian (15% vs 21%) respondents.19
When asking about autopsy participation, we did not ask if it was required or elective. Thus, we cannot determine whether elective versus required autopsy participation makes a difference in interest in our perception of pathology. We also did not ask about perceptions on the length of pathology residency. However, from several comments stating fellowships are required to get a job, it is possible that students perceive the specialty training period as too long and as a deterrent to choosing the specialty.
We tried to prevent bias by inviting all students at all allopathic medical schools through the Associate Deans and Chairs of Pathology. Because there was information and informed consent provided before the survey was started, students were informed the survey was asking about pathology. This may have selected for more students who had stronger feelings about pathology, in particular for those with more positive perceptions. As osteopathic medical school graduates fill 11% of allopathic pathology residency training positions, we feel it would be of value to undertake a survey of osteopathic medical students in the future.
The percentage of US medical students choosing pathology residency has fluctuated over time (Table 6).20 When the percentage has decreased in the past, concerns have been raised in the literature and within the specialty and efforts were undertaken to improve this.3-5 This has also happened in Canada.6,7 We are again at a point where the number of US medical students going into pathology has dropped to a low level. Based on our survey and review of the literature, many of the reasons given by our survey respondents are the same as those in the past: lack of direct patient care, concerns about finding jobs after completing residency, insufficient experience with diagnostic pathology, and negative perceptions of pathology as a specialty. We cannot do much about the first reason except to show potential residents where pathologists can have direct patient contact and how our work directly affects patient care. For the other reasons, we have identified steps that can be taken for improvement. It will not be easy but we have been successful in increasing the number of US medical students choosing pathology in the past and can be again. The SARS-CoV-2 pandemic has shown the need for a deep bench of pathologists to bring up, validate, and operationalize molecular and serologic testing in the face of a pandemic. A study of allopathic medical school pathology departments who produce high and low numbers of pathology residents is ongoing and may help identify additional ways to increase the number of student choosing pathology.
Table 6.
Percentage of US Seniors Matched to Postgraduate Year 1 Pathology Positions 1986 to 2020.20
| Year | Percentage | Year | Percentage | Year | Percentage | Year | Percentage | Year | Percentage |
|---|---|---|---|---|---|---|---|---|---|
| 1986 | 1.4 | 1993 | 2.2 | 2000 | 0.9 | 2007 | 2.1 | 2014 | 1.6 |
| 1987 | 1.5 | 1994 | 2.0 | 2001 | 1.3 | 2008 | 2.1 | 2015 | 1.7 |
| 1988 | 1.4 | 1995 | 2.1 | 2002 | 1.5 | 2009 | 2.2 | 2016 | 1.5 |
| 1989 | 1.9 | 1996 | 1.8 | 2003 | 2.0 | 2010 | 2.2 | 2017 | 1.2 |
| 1990 | 1.9 | 1997 | 1.0 | 2004 | 2.2 | 2011 | 1.7 | 2018 | 1.2 |
| 1991 | 2.2 | 1998 | 0.9 | 2005 | 2.4 | 2012 | 1.7 | 2019 | 1.1 |
| 1992 | 1.9 | 1999 | 1.1 | 2006 | 2.2 | 2013 | 1.6 | 2020 | 1.1 |
Supplemental Material
Supplemental Material, Supplemental_Table_1_-_Count_on_'Don't_know'_Answers for Factors Influencing US Allopathic Medical Students to Choose Pathology as a Specialty by Cindy B. McCloskey, Kristen Johnson, Mark Brissette, Richard Conran, John Childs, Melissa George, Dita Gratzinger, Victor G. Prieto, Amyn M. Rojiani, Irene Shyu, Charles Timmons Jr and Robert Hoffman in Academic Pathology
Acknowledgments
Dr McCloskey would like to thank the University of Oklahoma College of Medicine Academy of Teaching Scholar’s Health Education Research Organization (HERO) for development of this research idea and Dr Christopher Williams for assistance in preparing figures for the manuscript.
Authors’ Note: For Drs Brissette and Childs: The views and opinions expressed in this manuscript are those of the authors and do not reflect the official policy or position of the Department of Army/Navy/Air Force, Department of Defense or the United States Government. Department/Institution to which the work should be attributed: College of American Pathologists, Graduate Medical Education Committee, 325 Waukegan Road, Northfield, IL 60093.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding and support for the College of American Pathologists Graduate Medical Education Committee (CAP GMEC) are provided by the College of American Pathologists in the form of educational staff support (author K.J.), travel reimbursement for current and former committee members (authors C.B.M., M.B., R.C., J.C., M.G., D.G., V.G.P., A.M.R., I.S., C.T., and R.H.), and funding for publication.
ORCID iD: Richard Conran  https://orcid.org/0000-0002-4053-1784
https://orcid.org/0000-0002-4053-1784
Dita Gratzinger  https://orcid.org/0000-0002-9182-8123
https://orcid.org/0000-0002-9182-8123
Charles Timmons Jr  https://orcid.org/0000-0002-5274-8569
https://orcid.org/0000-0002-5274-8569
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Results and Data: 2019 Main Residency Match. National Resident Matching Program. Published 2019 Accessed June 13, 2020 https://mk0nrmp3oyqui6wqfm.kinstacdn.com/wp-content/uploads/2019/04/NRMP-Results-and-Data-2019_04112019_final.pdf.
- 2. Results and Data: 2020 Main Residency Match. National Resident Matching Program. Published 2020 Accessed June 13, 2020. https://mk0nrmp3oyqui6wqfm.kinstacdn.com/wp-content/uploads/2020/05/MM_Results_and-Data_2020.pdf.
- 3. Vance RP, Prichard RW, Smith RD. Pathology trainee manpower: APC program directors’ questionnaire, 1989 results. Hum Pathol. 1991;22:1067–1076. [DOI] [PubMed] [Google Scholar]
- 4. Smith RD, Prichard RW. A survey of first-year pathology residents: factors in career choice. Hum Pathol. 1987;18:1089–1096. [DOI] [PubMed] [Google Scholar]
- 5. Vance RP, Prichard RW, Smith RD. Recruitment of pathology trainees. Recent trends from the 1989 Association of Pathology Chairmen’s Survey of first-year pathology residents. Arch Pathol Lab Med. 1991;115:1097–1106. [PubMed] [Google Scholar]
- 6. Ford JC. If not, why not? Reasons why Canadian postgraduate trainees chose—or did not choose—to become pathologists. Hum Pathol. 2010;41:566–573. [DOI] [PubMed] [Google Scholar]
- 7. Hung T, Jarvis-Selinger S, Ford JC. Residency choices by graduating medical students: why not pathology? Hum Pathol. 2011;42:802–807. [DOI] [PubMed] [Google Scholar]
- 8. Ford JC. Influence of a problem-based learning curriculum on the selection of pathology as a career: evidence from the Canadian match of 1993-2004. Hum Pathol. 2005;36:600–604. [DOI] [PubMed] [Google Scholar]
- 9. Robboy SJ, Weintraub S, Horvath AE, et al. Pathologist workforce in the United States: I. Development of a predictive model to examine factors influencing supply. Arch Pathol Lab Med. 2013;137:1723–1732. [DOI] [PubMed] [Google Scholar]
- 10. Functions and Structure of a Medical School: Standards for Accreditation of Medical Education Programs Leading to the MD Degree 2019-2020. Liason Committee on Medical Education. Published 2018 Accessed June 13, 2020 https://lcme.org/publications/.
- 11. Querido SJ, Vergouw D, Wigersma L, Batenburg RS, De Rond ME, Ten Cate OT. Dynamics of career choice among students in undergraduate medical courses. A BEME systematic review: BEME Guide No. 33. Med Teach. 2016;38:18–29. [DOI] [PubMed] [Google Scholar]
- 12. Holland L, Bosch B. Medical students’ perceptions of pathology and the effect of the second-year pathology course. Hum Pathol. 2006;37:1–8. [DOI] [PubMed] [Google Scholar]
- 13. Gratzinger D, Johnson KA, Brissette MD, et al. The recent pathology residency graduate job search experience: a synthesis of 5 years of College of American Pathologists job market surveys. Arch Pathol Lab Med. 2018;142:490–495. [DOI] [PubMed] [Google Scholar]
- 14. George MR, Johnson KA, Gratzinger DA, et al. Will I need to move to get my first job? Geographic relocation and other trends in the pathology job market. Arch Pathol Lab Med. 2020;144:427–434. [DOI] [PubMed] [Google Scholar]
- 15. Timmons CF, Black-Schaffer WS, Naritoku WY, et al. Entry of graduates of US Pathology Residency Programs into the workforce: cohort data between 2008 and 2016 remain positive and stable. Acad Pathol. 2020:7 doi:10.1177/2374289520901833. Accessed June 13, 2020 https://journals.sagepub.com/doi/10.1177/2374289520901833. [DOI] [PMC free article] [PubMed]
- 16. Raphael S, Lingard L. Choosing pathology: a qualitative analysis of the changing factors affecting medical career choice. Med Sci Educ. 2005;15:81–90. [Google Scholar]
- 17. Hafferty FW, Franks R. The hidden curriculum, ethics teaching, and the structure of medical education. Acad Med. 1994;69:861–871. [DOI] [PubMed] [Google Scholar]
- 18. Table A-6: Age of Applicants to US Medical Schools at Anticipated Matriculation by Sex and Race/Ethnicity, 2014-2015 through 2017-2018. American Association of Medical Colleges. Published 2017 Accessed June 13, 2020 https://www.aamc.org/system/files/d/1/321468-factstablea6.pdf.
- 19. Table A-8: Applicants to US Medical Schools by Selected Combinations of Race/Ethnicity and Sex, 2016-2017 through 2019-2020. American Association of Medical Colleges. Published 2019 Accessed June 13, 2020 https://www.aamc.org/system/files/2019-11/2019_FACTS_Table_A-8.pdf.
- 20. Report Archives: Results and Data: Main Residency Match—1986-2020. National Resident Matching Program. Published 1986-2020 Accessed June 13, 2020 http://www.nrmp.org/report-archives/.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, Supplemental_Table_1_-_Count_on_'Don't_know'_Answers for Factors Influencing US Allopathic Medical Students to Choose Pathology as a Specialty by Cindy B. McCloskey, Kristen Johnson, Mark Brissette, Richard Conran, John Childs, Melissa George, Dita Gratzinger, Victor G. Prieto, Amyn M. Rojiani, Irene Shyu, Charles Timmons Jr and Robert Hoffman in Academic Pathology