Abstract
Objectives
The outbreak of novel coronavirus-2019 (COVID-19) has affected Turkey very seriously, as well as all around the world. Many urgent and radical measures were taken due to the high contagious risk and mortality rate of the outbreak. It is noteworthy that isolation recommendations and the provision of health services for pandemic have a negative impact on Physical Medicine and Rehabilitation (PMR) services. In this study, we aimed to evaluate the effects of COVID-19 on the PMR services and physiatrists immediately after the first month of pandemic in Turkey.
Patients and methods
An online survey consisting of 45 items was sent to the members of the Turkish Society of Physical Medicine and Rehabilitation. The main goal of the survey was to evaluate the changes in the provided service of PMR and conditions of physiatrists one month after the first reported COVID-19 case in Turkey.
Results
A total of 606 PMR specialists and residents responded to the survey. The mean number of the patients visited the outpatient clinics was 148.2±128.5 per week before the pandemic, it significantly decreased to 23.4±33.1 per week after the first month of the reported first COVID-19 case. Similarly, the mean number of the patients of inpatient service significantly decreased from 21.7±39.3 per week to 2.5±10.0 per week after the first month of the pandemic. Most of the residents (69%) reported that their training was seriously affected due to pandemic. From the economic aspect, 69.2% of the participants who were working at private hospitals reported a decrease in their monthly salary, and 21% of them were sent to an unpaid vacation. A total of 21.9% of private-practice institutions paused their services. During the first month, 46.9% of the participants were assigned to the different services such as COVID-19 inpatient service, emergency or COVID-19 outpatient clinics. According to the Republic of Turkey, Ministry of Health guideline and algorithm, 15.7% of the physicians were in the category of healthcare workers with suspected COVID-19.
Conclusion
The COVID-19 pandemic affected seriously both the services and the PMR physicians as early as the first month. This effect is expected to become worse, when the duration of pandemic prolongs. Proper arrangements and measures should be planned to ameliorate the negative effects of the pandemic on the patients and PMR physicians.
Keywords: Coronavirus, COVID-19, pandemic, physical medicine and rehabilitation
Introduction
In December 2019, an increasing number of cases of pneumonia with an unknown etiology was reported in Wuhan City, Hubei Province of China. The Chinese authorities identified a new type of coronavirus, which was isolated on January 7th, 2020. The first death from novel coronavirus-2019 (COVID-19) was reported in China on January 11th, 2020.[1]
The outbreak was also followed closely by the Republic of Turkey, Ministry of Health. The Coronavirus Scientific Advisory Board was officially established on January 10th, 2020 with the affiliation of the Ministry of Health of Turkey. Meanwhile, the number of patients increased rapidly in China and the high mortality rate was reported. Unfortunately, the disease was unable to be prevented to spread rapidly all over the world. The World Health Organization (WHO) described the epidemic as pandemic for the first time on March 11th, 2020. Despite all efforts, no proven method has been found in the prevention or treatment of the disease until now.
In Turkey, the Coronavirus Scientific Advisory Board conducted its first guideline on January 14th, 2020.[2] In this guideline, possible scenarios and case descriptions were provided and initially 25 hospitals were identified as the centers of pandemic across the country. The first case of COVID-19 in Turkey was identified on March 11th, 2020. Within the framework of the measures taken by the Ministry of Health, the citizens were called to stay at home, and the importance of social isolation was emphasized. The hospitalized patients were discharged gradually, and inpatient bed occupancy rate was dramatically reduced from 70 to 30% to be prepared for an increasing number of COVID-19 patients. Elective surgical procedures were also postponed to reduce the burden of intensive care units (ICUs). Meanwhile, the Turkish Society of Physical Medicine and Rehabilitation (TSPMR) published the consensus about the instructions for outpatient clinics, rehabilitation units, and inpatient rehabilitation services to reduce the infection rate on March 18th, 2020. In this guideline, it was recommended to postpone the treatment of patients with comorbidities and elderly, due to the high mortality rate of COVID-19, particularly in these patients. The Coronavirus Scientific Advisory Board regularly updated the guidelines, and the latest version was published on April 14th, 2020.[3] From the first published guideline to the latest, it is remarkable that the Committee has made all efforts to develop a standard approach in a wide medical spectrum from protection to intensive care. In addition, there have been recent other strict regulations about isolation. All schools were closed during this period, and the services of pediatric rehabilitation centers such as special education centers were interrupted.
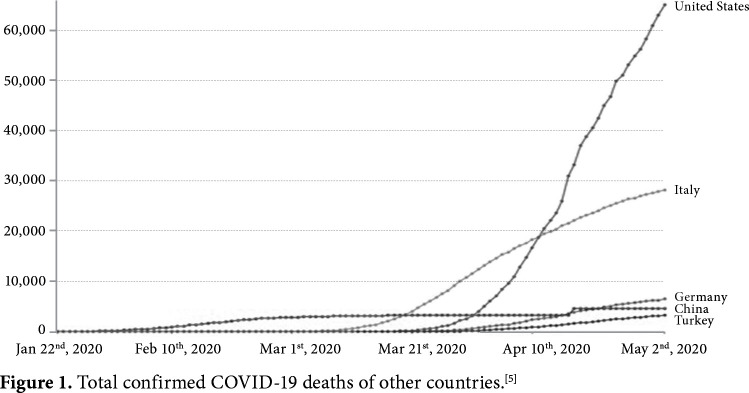
On March 23rd, 2020, a very critical decision was taken from the Ministry of Health. All hospitals who were specialists in Infectious Diseases and Clinical Microbiology and Chest Diseases or Internal Medicine and having the 3rd level adult ICUs were accepted as pandemic hospitals. Based on this decision, the number of pandemic centers were increased to overcome the burden of pandemic. Despite the early and gradually increased measures, Turkey reached a total of 124,375 cases and 3,336 deaths on May 2nd, 2020.[4] Despite the high number of confirmed cases, Turkey has still a lower mortality rate compared to other countries (Figure 1). The Ministry of Health has attributed the lower mortality rate to two main causes: the reservation of inpatient services and ICUs for COVID-19 patients and the effective use of healthcare providers, including physicians and nurses.
Figure 1. Total confirmed COVID-19 deaths of other countries.[5].
It is undoubtedly true that these measures have negative consequences on the management of diseases other than COVID-19. The healthcare services provided to patients in the field of Physical Medicine and Rehabilitation (PMR) has been also affected adversely as in other specialties. In addition, PMR physicians has started to be employed in various positions for fight against the pandemic. In this study, we aimed to evaluate the effects of COVID-19 on the PMR services and physiatrists immediately after the first month of pandemic in Turkey.
Patients and Methods
The TSPMR established the COVID-19 Study Group after the pandemic to provide recommendations rehabilitation of COVID-19 patients and to inform PMR physicians and the public with updated literature. This study was conducted by the TSPMR/COVID-19 Study Group. A survey was created to evaluate the effects of the pandemic. The survey consisted of 45 items in five main subheadings. The first subheading was about demographic data and academic degrees of the participants (5 items). The second subheading was the PMR services prior to pandemics (11 items). The third subheading was about the job descriptions and service profile in the first month of the pandemics (15 items). The fourth subheading included six items for preventive measures and the fifth subheading included eight items on socioeconomical burden of pandemics on PMR specialists. We attempted to obtain objective data about the proportional change in numbers of patients examined in outpatient clinics, receiving physical therapy in physical therapy units, and hospitalized patients in hospitals. In addition, the impact of the pandemic on education, working conditions and monthly income, and the extent of the exposure of PMR physicians to the risk of infection were also questioned. A written informed consent was obtained from each participant. The study protocol was approved by both of the Ethics committee of Zonguldak Bülent Ecevit University (2020/08) and Republic of Turkey, Ministry of Health. The study was conducted in accordance with the principles of the Declaration of Helsinki.
The survey was published online on April 10th, 2020, and the members of TSPMR were invited to participate in the survey two times by electronic mail (e-mail). The participants agreed that their information could be used in a publication before starting to fill the survey. The survey was finalized on April 17th, 2020.
Statistical analysis
Current number of PMR physicians in Turkey is estimated to be around of 3,250. The research sample was selected from the members of the TSPMR. The TSPMR has officially 2,400 members. The sample size estimation performed based on the theoretical constant of 1.96 with 20% probable incidence value. The sample size was calculated as 222 according to formula, and at least 250 physicians were planned to participate in the study to overcome the design-related dropout risk.
Statistical analysis was performed using the IBM SPSS version 23.0 software (IBM Corp., Armonk, NY, USA). The normal distribution of numerical data was evaluated by the Shapiro-Wilk test. The Student’s t-test was used for the comparison of two independent variables with normal distribution. Categorical variables were evaluated using the Pearson chi-square test. A one-sample t-test was used to examine significant differences in the means of variables between the study groups. A p value of <0.05 was considered statistically significant.
Results
Totally, 790 participants registered to the survey through the online system. Participants who did not complete all the 45-items were excluded from the analysis (n=184). The study was completed with 606 participants.
Demographic data
The distribution of the participants according to the provinces is demonstrated in Table 1. Participation was implemented in a total of 71 provinces of Turkey, representing the overall population of the country. The highest three participation rates were from Istanbul (27.4%), Ankara (12.2%), and Bursa (7.9%). The mean age was 40.3±10.2 (range, 24 to 73) years and the summary of academic degrees is presented in Table 2.
Table 1. The distribution of provinces.
| The number of participants | Province |
| 1 | Amasya, Bayburt, Bilecik, Burdur, Çorum, Düzce, Elâzığ, Erzurum, Kastamonu, Kırklareli, Kilis, Mardin, Sivas, Yalova, Yozgat |
| 2 | Aksaray, Artvin, Bartın, Bingöl, Kars, Muş, Niğde, Rize, Siirt, Sinop, Şırnak |
| 3 | Ağrı, Batman, Çanakkale, Diyarbakır, Eskişehir, Karabük, Kırşehir, Muğla, Nevşehir, Ordu, Şanlıurfa, Uşak, Van |
| 4 | Afyonkarahisar, Kahramanmaraş, Malatya |
| 5 | Balıkesir, Bolu, Denizli, Hatay, Sakarya, Tekirdağ |
| 6 | Giresun, Isparta, Kırıkkale, Kocaeli, Zonguldak |
| 8 | Gaziantep, Manisa, Mersin, Samsun, Trabzon |
| 9 | Tokat |
| 10 | Kütahya |
| 11 | Aydın, Kayseri |
| 12 | Edirne |
| 14 | Adana |
| 20 | Antalya |
| 21 | İzmir, Konya |
| 48 | Bursa |
| 74 | Ankara |
| 166 | İstanbul |
| Total: 606 participants | Total: 71 cities |
Table 2. The academic degrees of the participants.
| Academic degree | n | % |
| Resident | 91 | 15.02 |
| Specialist | 365 | 60.23 |
| Assistant Professor | 34 | 5.61 |
| Associate Professor | 46 | 7.59 |
| Professor | 70 | 11.55 |
| Total | 606 | 100.0 |
The effect of the pandemic on the service profile
Clinical and academic work settings can considerably vary among PMR physicians. The areas and work settings of PMR physicians prior to pandemic were questioned. Most of the PMR physicians worked in the settings of outpatient clinics, outpatient rehabilitation units, and inpatient rehabilitation services. Before the pandemic, 15.7% of the participants were also working in the ICUs for rehabilitation purpose. A total of 12.9% of them were also working in traditional and complementary medical units, while 6.6% contributed on-call duties in the emergency service.
There were statistically significant changes of the service profile in the first month of the pandemic. The number of physicians working in all services related to PMR decreased significantly compared to before the pandemic, while the number of physicians assigned to the emergency service increased. Pandemic-related units were introduced into the healthcare system and PMR specialists were commonly assigned into these units. In addition, 90 (14.9%) of our colleagues worked in COVID-19 emergency triage, 140 (23.1%) in COVID-19 outpatient clinics, and 191 (31.5%) in COVID-19 inpatient services (Table 3).
Table 3. Comparison of PMR services before pandemic and in first month of pandemic (Participants who answered “Yes” are included in the table).
| Before the pandemic | First month of pandemic | |||||
| Service area | n | % | n | % | χ2 | p* |
| PMR outpatient clinics | 571 | 94.2 | 491 | 81.0 | 89.96 | 0.001 |
| Outpatient rehabilitation service | 520 | 85.8 | 245 | 40.4 | 34.52 | 0.001 |
| Inpatient rehabilitation service | 435 | 71.8 | 153 | 25.2 | 59.65 | 0.001 |
| ICU | 95 | 15.7 | 60 | 9.9 | 167.47 | 0.001 |
| TCMS | 78 | 12.9 | 33 | 5.4 | 204.53 | 0.001 |
| On-call ED | 40 | 6.6 | 58 | 9.6 | 91.19 | 0.001 |
| ED Covid triage | 0 | 0 | 90 | 14.9 | ||
| Covid outpatient clinic | 0 | 0 | 140 | 23.1 | ||
| Covid inpatient clinic | 0 | 0 | 191 | 31.5 | ||
| PMR: Physical Medicine and Rehabilitation; ICU: Intensive care unit; TCMS: Traditional and complementary medical center; ED: Emergency depart- ment; * p<0.05 indicates significant difference. | ||||||
When the service profile of the pandemic was categorically analyzed by academic degrees, the residents and specialists were mostly affected. A total of 91.2% of residents and 56.4% of the specialists began to work in either COVID-19 triage, COVID-19 inpatient, or COVID-19 outpatient services. The mean number of the shift increased from 1.1±2.0 (range, 0 to 10) to 1.8±2.6 (range, 0 to 13) for all participants. The increase in the mean number of shifts was directly associated with the increased number of shift of specialists, assistant professors, and professors (p=0.001, p=0.007, and p=0.013, respectively).
The effect of pandemic on the number of patients requiring PMR services
In the first month of pandemic, the number of patients in the outpatient clinics, outpatient rehabilitation units, and inpatient services statistically significantly decreased, compared to pre-pandemic setting (Table 4).
Table 4. The effect of pandemic on the number of patients in rehabilitation facilities.
| Setting | February 24-29, 2020 | April 6-11, 2020 | p* |
| PMR outpatient clinics | 148.2±128.5 | 23.4±33.1 | 0.001 |
| Outpatient rehabilitation service | 89.8±123.1 | 6.8±15.2 | 0.001 |
| Inpatient rehabilitation service | 21.7±39.3 | 2.5±10.0 | 0.001 |
| PMR: Physical Medicine and Rehabilitation; * One-sample t-test (*p<0.05 indicates significant difference). | |||
The effect of pandemic on training
The effect of the pandemic on PMR training was assessed in 147 participants who had educational duties and 91 residents of PMR. Of 147 trainers, 14 (9.5%) were mildly (range, 0 to 25%); 13 (8.8%) were moderately (range, 26 to 50%), 30 (20.4%) were severely (range, 51 to 75%), and 90 (61.2%) were very severely (range, 76 to 100%) affected from pandemic on the basis of PMR educational activities. Residents also confirmed the negative effects of the pandemic on their training. Of 91 residents, five (5.5%) were mildly, five (5.5%) were moderately, 12 (13.2%) were severely, and 69 (75.8%) very severely affected in terms of the level of training programs which they received (Table 5).
Table 5. The effect of the pandemic on education.
| Degree of influence | Instructor (n=147) | Residents (n=91) | ||
| n | % | n | % | |
| 0-25% affected | 14 | 9.5 | 5 | 5.5 |
| 26-50% affected | 13 | 8.8 | 5 | 5.5 |
| 51-75% affected | 30 | 20.4 | 12 | 13.2 |
| 76-100% affected | 90 | 61.2 | 69 | 75.8 |
Prior training for pandemic and preventive measures
The answers given to the questions about readiness of PMR physicians to pandemic and the use of personnel protective measures are presented in Table 6. Totally, 64% of the participants had a training about the COVID-19 before the pandemics and personal preventive training was given to 58% of the participants. Thirty-one percent of the participants were unable to apply personal protective equipment (PPE) adequately. Of 188 (31%) participants who did not apply PPE adequately, 105 (55.9%) of them reported that it was due to the lack of PPE, 13 (6.9%) due to the lack of information, and 70 (37.2%) due to both of the lack of PPE and information.
Table 6. Personnel protective measures and information.
| n | % | |
| Have you training about COVID-19 infection before pandemic? | 388 | 64.0 |
| Have you been trained for personal protective measures? | 354 | 58.4 |
| Were you able to implement personal protective measures adequately? | 418 | 69.0 |
According to the Republic of Turkey, Ministry of Health guideline and algorithm, 95 physicians (15.7%) were in the category of healthcare workers with suspected COVID-19. The percentage of COVID-19 during this period was 11.2% (n=68).
The answers given to the four questions investigating the professional life and economic impact of the pandemic are presented in Table 7. Overall 46.9% of the participants were working in an area where they were not trained in, while job description and scope changed in 68.2%. A total of 62% of all PMR physicians were economically impacted.
Table 7. The professional working and economic effects of the pandemic.
| fn | % | |
| I was economically affected | 376 | 62.0 |
| My job description and scope has changed | 413 | 68.2 |
| I had to work in an area which I was not trained for | 284 | 46.9 |
| Mine continue medical education was affected | 249 | 41.1 |
The effect of pandemic on private hospital employees
Since the economic impact of the pandemic was expected to be different for private hospital employees than those working for the state hospitals, specific questions were asked for private hospital employees. Totally, 292 of 606 individuals (48.18%) who participated in the survey worked in the private institutes, and 202 of them (69.2%) reported that their income decreased, compared to pre-pandemic. Sixty-four (21.92%) of 292 participants working in the private sector stated that their institution was closed, or their services were suspended. Similarly, 61 of them (20.89%) were sent to an unpaid vacation and unfortunately three (1.03%) PMR specialists became unemployed.
Discussion
Throughout the history, humankind has been struggled with epidemic diseases. Plague, cholera, typhus, smallpox, Ebola, and influenza epidemics have caused great losses worldwide. The WHO previously scripted what would happen under a flu epidemic. According to this scenario, if there is an epidemic in a country, the agent which causes epidemic is first detected and identified. While analyzing the new epidemic agent, it becomes the subject of current news and begins to spread and starts to be seen in the neighbor countries. By taking precautions, travel restrictions are introduced, and schools are closed. When the agent has just been determined in the epidemic, there is no vaccine and drug resources are not sufficient. Disease is seen in aircraft passengers who travel from countries where epidemic is identified. The epidemic begins to spread. The health institutions become unable to meet the increasing workload. The number of working staff decreases due to illness. The ICUs become fully, and healthcare and public service organizations become desperate.[6] Unfortunately for COVID-19, a similar picture of this scenario appears to have taken place literally in many countries. However, the rate of spread has been much faster, and it is understood health systems are fragile and not ready for this kind of pandemic.
Although the pandemic is a global problem, the fight against the pandemic is usually at the national level. Turkey is one of the countries which took early measures regarding COVID-19. For instance, the Ministry of Health, Coronavirus Scientific Advisory Board was established only 10 days after the first case was seen in China. Many measures were implemented after the index case was seen on March 11th, 2020. One of the main measures affecting the results of this study was the decision to postpone elective surgeries and dental practices on March 16th, 2020. In addition, restrictions on leave, resignation, and assignation were introduced to enable more efficient and controlled use of health workers in the public and private sectors and all healthcare workers took part in combating the pandemic.
Based on the results of our study, a significant number of the respondents worked in Istanbul. Istanbul is the city which COVID-19 cases were most frequently detected. This result is, therefore, not surprising, as PMR physicians of Istanbul seemed to be more affected from other cities. The sample size of our study was calculated as 250 and filling out the questionnaire by 606 physicians was a strong aspect of the study. The fact that there were participants from each academic degree and that they represented the private or public sector separately suggests that the study reflects working PMR physicians of Turkey.
The areas served by the PMR departments are very diverse. This diversity can be seen, when the data before the pandemic is examined. In the first month of the pandemic, a very important part (46.9%) of PMR physicians started working in COVID-19 inpatient and outpatient services, and emergency triage for COVID-19, in addition to or after cancelling their current duties. Many physicians with changes of job description worked in hospitals of Ministry of Health and state universities.
Although outpatient services continued, there was a sharp decline in the number of admitted patients to the department of PMR. The mean number of daily admitted patients decreased from 148 to 23. Similarly, the mean daily patient number in the outpatient rehabilitation services decreased from 89.7 to 6.7, since appointments in the outpatient rehabilitation services were postponed for elective cases. Probably, the most important issue was the decrease in the number of beds for inpatient services. Most of the beds were completely or partially transferred for the use of COVID-19 patients, with the mean number of inpatient beds declining from 21.6 to 2.5. This service interruption would have further consequences to be felt in the forthcoming months.
Failure to provide of healthcare, particularly in outpatient services and PMR treatment sessions where chronic diseases are followed and treated, would increase the level of disability in the future. As an example, it has become very difficult to find any inpatient rehabilitation bed for some serious diseases such as stroke or spinal cord injury. In a multi-national study confirming this situation, it was reported that only 7.4% of patients with spinal cord injuries could receive rehabilitation treatment as before the outbreak. Unfortunately, 50.4% of patients were treated at home. As a solution, 47% of the respondents reported that telemedicine models were used.[7] Although there was information about telemedicine confirming the situation for various rehabilitation needs in the media, there is still very little information about how important this issue may be. Again, our individual observation is that patients are unwilling to postpone their treatment. The most important result of our study was that there was a great service deficit in the PMR field from the very beginning of the pandemic, and a huge potential for post-pandemic accumulation has started. The PMR physicians began to experience negative repercussions of the situation, while participating in the fight against the pandemic. At first, PMR training is a hand on and cannot be performed by using the online education model. Moreover, most of residents currently serve in another services and units unrelated to their medical specialty. The operation of PMR curriculum program has come to a stagnation point and the specializing theses has been interrupted. The question of how long this situation would last puts burden on residents. Therefore, when the number of cases begins to decrease in our country, it is very important to make urgent plans and necessary changes in residency programs.
Although the Ministry of Health of Turkey took the precautions early, the precautions in some subjects were not fully reflected on the field. Approximately 36% of the respondents received no in-service training about COVID-19. In addition, the training of personal preventive measures was provided in 58% of the participants. Interestingly, 31% of PMR physicians were unable to apply PPE adequately. Of 188 respondents who did not apply personal protective measures adequately, 105 (55.9%) reported that it was due to the lack of PPE or lack of information (n=13, 6.9%), and both (n=70, 37.2%).
As already known, healthcare professionals are at the front line of COVID-19 outbreak and are mostly affected by the epidemic. In such a disease with a high contagious rate, it is a must to apply personal protective measures. The Turkish Medical Association announced that a total of 3,474 healthcare workers were diagnosed with COVID-19 on April 4th, 2020 and 38% of them were physicians.[8] The number of physicians who died until this date was 17.[8] The Ministry of Health of Turkey also released a guideline and algorithm for health professionals on March 27th, 2020.[9] According to this guideline, 95 participants (15.7%) of the study were evaluated in the category of contact healthcare professionals. Some of our physicians were also infected with COVID-19. As the reported numbers cannot be generalized to the entire country, it can be predicted that the number would be much higher, when the pandemic ends.
From the economic aspect, 62% of the physicians reported that their monthly income level decreased compared to the previous month. Physicians who worked at the private hospitals were affected from the outbreak at varying degrees, unlike those in the state and university hospitals. Nearly 21% of the private hospitals interrupted or closed their services in the first month. Staff physicians working at these private facilities were sent for unpaid leave. Of note, it is thought-provoking that three specialists were unemployed in the first month of pandemic.
Nonetheless, there are some limitations to this study. The answers given to some questions are likely to change in the forthcoming periods, as we were able to evaluate the answers within only a certain time frame. Indeed, the number of COVID-19 test capacity has yet reached the desired level. In addition, controversial opinions on the use of PPE earlier seem to be minimized nowadays. Thus, repeating the questionnaire in the next few months may cause positive or negative changes in some items. Therefore, it is planned to repeat the questionnaire after some time to track these changes.
In conclusion, to the best of our knowledge, this is the first study to evaluate the effect of pandemic on PMR. It is intended to contribute to the planning of PMR services in the near future during the days in which a highly dynamic process is experienced. After the isolation of the first case, PMR physicians fulfilled their responsibilities and, as the outbreak increases, they would continue to perform expected duties, even if these duties are beyond their specialties. Our expectation from the health authorities is to plan the steps which would meet the expectations of both our patients and staff physicians in the process of normalization of pandemics.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1. Available at: https://wwwwho.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019- ncov.pdf?sfvrsn=20a99c10_4 . [Accessed: May 2, 2020]
- 2. Available at: https://covid19bilgi.saglik.gov.tr/depo/rehberler/COVID-19_Rehberi.pdf. [Accessed: May 2, 2020]
- 3. T.C. Sağlık Bakanlığı, Halk Sağlığı Genel Müdürlüğü, Covid-19 (SARS-CoV-2) Rehberi (Bilim Kurulu Çalışması). Available at: https://covid19bilgi.saglik.gov.tr/depo/rehberler/Covid-19_Rehberi.pdf. [Accessed: April 14, 2020] [Google Scholar]
- 4. Available at: https://covid19bilgi.saglik.gov.tr/tr/ [Accessed: May 03, 2020]
- 5. Available at: https://ourworldindata.org/covid-deaths. [Accessed: May 2, 2020]
- 6.Eccleston-Turner M, Phelan A, Katz R. Preparing for the Next Pandemic - The WHO’s Global Influenza Strategy. N Engl J Med. 2019;381:2192–2194. doi: 10.1056/NEJMp1905224. [DOI] [PubMed] [Google Scholar]
- 7.Stillman MD, Capron M, Alexander M, Di Giusto ML, Scivoletto G. COVID-19 and Spinal Cord Injury and Disease: Results of an International Survey. Spinal Cord Ser Cases. 2020;6:21–21. doi: 10.1038/s41394-020-0275-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Available at: https://www.ttb.org.tr/kollar/userfiles/files/ ttbCovid-saglik-calisanlari_-EN-SON.pdf. [Accessed: May 2, 2020]
- 9. Available at: https://covid19bilgi.saglik.gov.tr/depo/tedavi/COVID19-TemasiOlanSaglikCalisanlarininDegerlendirilmesi.pdf. [Accessed: May 2, 2020]